Abstract
Lateral epicondylalgia is a commonly encountered musculoskeletal complaint. Currently, there is no agreement regarding the exact underlying pathoanatomical cause or the most effective management strategy. Various forms of joint manipulation have been recommended as treatment. The purpose of this study was to systematically review available literature regarding the effectiveness of manipulation in treating lateral epicondylalgia. A comprehensive search of Medline, CINAHL, Health Source, SPORTDiscus, and the Physiotherapy Evidence Database ending in November 2007 was conducted. Thirteen studies, both randomized and non-randomized clinical trials, met inclusion criteria. Articles were assessed for quality by one reviewer using the 10-point PEDro scale. Quality scores ranged from 1–8 with a mean score of 5.15 ± 1.85. This score represented fair quality overall; however, trends indicated the presence of consistent methodological flaws. Specifically, no study achieved successful blinding of the patient or treating therapist, and less than 50% used a blinded outcome assessor. Additionally, studies varied significantly in terms of outcome measures, follow-up, and comparison treatments, thus making comparing results across studies difficult. Results of this review support the use of Mulligan's mobilization with movement in providing immediate, short-, and long-term benefits. In addition, positive results were demonstrated with manipulative therapy directed at the cervical spine, although data regarding long-term effects were limited. Currently, limited evidence exists to support a synthesis of any particular technique whether directed at the elbow or cervical spine. Overall, this review identified the need for further high-quality studies using larger sample sizes, valid functional outcome measures, and longer follow-up periods.
KEYWORDS: Joint Manipulation, Lateral Epicondylalgia, Systematic Review, Tennis Elbow
Lateral epicondylalgia (LE), also known as tennis elbow, is a common musculoskeletal complaint that is frequently encountered by physical therapists. Prevalence of the disorder ranges from 2.8% in the general population with increases up to 7.4% in the engineering industry1,2. Despite being widely known as tennis elbow, more cases can be attributed to mechanical stress related to occupation than to tennis1,3. Overall trends indicate that rates of injury increase in populations whose occupation involves repetitive use of the upper extremity4,5. Peak incidence occurs between 45–54 years of age with the dominant arm typically affected2,4. Some indicate that LE has been described as a self-limiting condition with 89% of those diagnosed reporting decreases in pain at 1 year6, whereas others have estimated as much as 40% of those diagnosed experience prolonged symptoms leading to impaired function4.
The exact underlying pathological process contributing to LE has been the topic of much debate, and there still exists no consensus4. Current evidence following surgical intervention indicates that LE is a chronic disorder demonstrated by the presence of degenerative changes, such as increased fibroblasts and disorganized collagen, as opposed to inflammatory cells5,7–9. These findings are contradictory to the widely used term epicondylitis, which describes an inflammatory condition9. It has recently been recommended that the term epicondylitis be replaced with epicondylosis, a more accurate descriptor of the underlying degenerative process, or the generalized term epicondylalgia9,10.
A significant number of treatments are offered for LE, ranging from medical interventions such as surgery and medication to physical therapy including modalities, exercise, and manual therapy3,5,11,12. Given the complexity surrounding the identification of an underlying cause, it is not surprising that no agreement exists as to which method is most effective in treating this disorder3,12,13. In addition, evidence regarding treatment effectiveness for LE is also lacking. A review conducted by Labelle et al14 in 1992 concluded that evidence was lacking to support any current treatment and that the existing studies were of low quality. An updated review by Smidt et al15 in 2003 shared similar conclusions to those of Labelle et al14. Most recently, a review conducted by Bisset et al16 highlighted initial benefits provided by manipulative therapy and concluded that further studies were warranted. This conclusion regarding manipulative therapy, however, was based on the results of 4 studies. Due to inclusion of meta-analyses in their design, Bisset and colleagues excluded studies not achieving a 50% or higher quality score so as to prevent studies of low quality from affecting calculated effect sizes. Other studies examining manipulative therapy may have been excluded for not satisfying the minimum quality criteria. Therefore, a review including not only studies published after the review by Bisset et al16 but also including those that may have been excluded is warranted to aid in further defining manipulation's role and effectiveness in treating LE.
Manipulation has been a recommended treatment for LE since the 1920s, beginning with techniques advocated by Mills and Cyriax12. Further manipulative techniques include Kaltenborn and Stoddard's varus thrust, Mennell's extension thrust, and Mulligan's mobilization with movement17–19. Given the history of manipulation's role in treating LE combined with Bisset et al's16 conclusions, a review of available literature focusing on the role of manipulative therapy is indicated. The objective of this systematic review was to examine the effectiveness of manipulative therapy in treating patients with LE.
Methods
Search Strategy
A comprehensive search of the following databases with no restrictions was conducted (CH): Medline (1966–November 2007), Cumulative Index of Nursing and Allied Health Literature (1981–November 2007), Health Source (1975–November 2007), SPORTDiscus (1985–November 2007), and the Physiotherapy Evidence Database (1929–November 2007). Key terms used during these searches included tennis elbow, lateral epicondylitis, lateral epicondylalgia, mobilization, manipulation, manual therapy, mobilization with movement, MWM, Cyriax, and Mill's manipulation. The Boolean operator AND was used to link terms describing diagnosis (tennis elbow, lateral epicondylitis, etc.) with terms describing manipulative intervention (mobilization, manipulation, etc.).
Selection Criteria
Articles were selected for this review if they met the following criteria: English language, experimental design, comparison between at least two treatment conditions, subjects with clinical diagnosis of LE, use of at least one patient-centered outcome, and inclusion of manipulative treatment in least one group. For the purpose of this review, manipulative treatment was defined as any joint manipulation or mobilization technique applied to treat LE. Mobilization and manipulation are defined by the Guide to Physical Therapist Practice20 as manual therapy techniques delivered with the goal of increasing tissue extensibility, improving range of motion (ROM), and modulating pain.
No restrictions were placed regarding the area of the body undergoing manipulation. Articles involving Cyriax physiotherapy were included only if friction massage was followed by the application of Mill's manipulation. Application of friction massage alone would not satisfy the operational definition of manipulative treatment used in this review. Details regarding the application of Cyriax physiotherapy, including Mill's manipulation, are described by Kushner and Reid17. Patient-centered outcomes were defined as those deemed important to the patient such as pain, ROM, strength, work status, and relevant functional questionnaires. Aside from not meeting inclusion criteria, articles were also excluded if manipulative techniques were used in conjunction with modes of treatment not normally delivered by physical therapists such as injection or anesthesia. Relevant studies were included regardless of methodological quality scores so as to include those articles that may have been excluded from past reviews. Abstracts of articles identified with the above search strategy were reviewed for inclusion. Full-text copies were requested for any abstract determined to fulfill the inclusion criteria. If determination could not be made based on the abstract, full text was requested and the full article was reviewed for inclusion.
Data Extraction and Analysis
A standardized set of data was gathered from each selected article. Data collected included that regarding demographics of the patient sample, manipulative technique studied, treatment frequency, outcome measures, results, and follow-up. Comparison between individual studies as well as conclusions regarding the entire sample were based on total Physiotherapy Evidence Database (PEDro) scores as well as scores on individual items 2–11 on the scale.
Quality Assessment
Assessment of methodological quality of selected articles was performed using the PEDro scale. The PEDro scale consists of an 11-item checklist designed to score the quality of randomized clinical trials. Interrater reliability has been reported as fair to good with an ICC of .55 (95% CI .41–.72) for individual raters21. Items 2–11 are concerned with internal validity while item 1 deals with external validity. Each item on the checklist is scored yes or no with those items marked yes receiving a score of 1 and those marked no receiving a score of 0.
All selected papers were read and scored by one individual (CH). To ensure accuracy, published operational definitions of PEDro scale items21 were reviewed prior to scoring. Total scores were determined by adding the total number of items marked yes with a maximum score of 10/10 possible points. Item 1 was excluded from the total score as it does not relate to the internal validity of the study. Following scoring, the mean score and standard deviation were calculated for the entire sample of articles. Considering the relative impossibility of successfully blinding treating therapists and subjects in trials involving manual therapy, it was hypothesized that the maximum achievable PEDro score would be 8/10. A quality score of 50% or better has been used as a benchmark to define acceptable quality in past systematic reviews15,16. Therefore, for the purposes of this review, studies were regarded as high quality if they scored 6 or higher, fair quality if they scored 4–5, and poor quality if they scored 3 or below.
Results
Study Selection and Characteristics
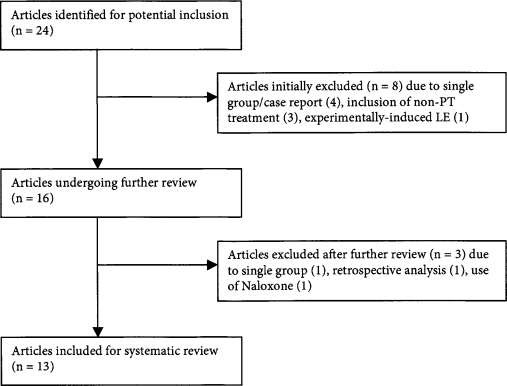
The results of the search strategy are presented in Figure 1. A total of 24 articles were initially identified for potential inclusion. Upon further review, 13 studies were deemed as having met inclusion criteria. The other 11 studies were excluded for the following reasons: 6 were a case study design, single group design, or retrospective analysis22–27; 3 combined manipulation with treatment options not readily available to physical therapists28–30; 1 used a sample with experimentally-induced LE31; and 1 administered the endorphin-blocking drug naloxone32.
FIGURE 1.
Study selection following literature search.
All 13 included studies used patient samples made up of men and women with a diagnosis of LE. Sample demographics are presented in Table 1. The two most frequently used outcome measures were pain-free grip strength and patient-reported rating of change or global improvement. A complete list of outcome measures including frequency of use is presented in Table 2. Regarding follow-up, 4 studies33–36 collected outcome data immediately following treatment with no further follow-up, 5 studies37–41 performed short-term follow-up of 3 months or less, and 4 studies42–45 included long-term follow-up of 6 months or greater with 2 studies42,45 collecting outcomes at one year.
TABLE 1.
Patient sample demographics.
| Study | n | M/F | Age (years) | Symptom Duration |
|---|---|---|---|---|
| Bisset et al42 | 198 | 128/70 | 47.6 (7.8) | 22 weeks (median) |
| Verhaar et al45 | 106 | 56/147 | 43 (9) | 33 weeks |
| Stasinopoulos & Stasinopoulos44 | 75 | 46/29 | 40.4 (5.6), 40.4 (5.6), 40.1 (6.2) | 5 months |
| Kochar & Dogra39 | 66 | 36/30 | 41 | not stated |
| Baltaci et al37 | 38 | 18/20 | 40.8, 35.5 | 5 months |
| Struijs et al41 | 28 | 15/13 | 46.3, 47.5 | 14.2(12.3), 9.3(6.1)weeks |
| Vicenzino et al34 | 24 | 11/13 | 49 | 6.2 (5.1) months |
| Paungmali et al33 | 24 | 17/7 | 48.5 (7.2) | 8.9 (8.4) months |
| Vicenzino et al36 | 24 | 14/10 | 46.43 (1.68) | 8.33 (1.71) months |
| Drechsler et al38 | 18 | 8/10 | 0–57 | not stated |
| Vicenzino et al35 | 15 | 7/8 | 44 | 8 (2) months |
| Langen-Pieters et al40 | 13 | 8/5 | 46.1, 49.7 | 16.6 (12.5) weeks |
| Cleland et al43 | 10 | 5/5 | 40.4 | 13.4 (4.9) weeks |
*Ages are presented as a mean or range with SD in ( ). Multiple means represent those of each treatment group when sample mean not available. Symptom duration reported as mean values with SD in ( ) unless otherwise indicated. Multiple means represent symptom duration for each group when sample mean not available.
TABLE 2.
Outcome measures used in 13 studies identified for review.
| Outcome Measure | Studies | Measurement Type |
|---|---|---|
| Pain-free grip strength | 9 | Physical impairment |
| Patient-reported rate of change | 5 | Self-reported change in function |
| Pain with VAS | 5 | Physical impairment |
| Maximum grip strength | 4 | Physical impairment |
| Pressure pain threshold | 4 | Physical impairment |
| ULTT2b | 3 | Physical impairment |
| Function with VAS | 3 | Self-reported functional level |
| Sympathetic nervous system function | 2 | Clinician-monitored changes in SNS activity |
| Termal pain threshold | 2 | Physical impairment |
| Pain-free function lat. Epicondylitis questionnaire | 2 | Self-report functional questionnaire |
| ADL inconvenience scale 0–11 | 1 | Self-reported difficulty with ADLs |
| Assessor's rating of severity | 1 | Clinician-reported symptom level |
| Wrist extensor strength (weight test) | 1 | Physical impairment |
| Elbow and wrist ROM & MMT results | 1 | Physical impairment |
| DASH questionnaire | 1 | Self-reported functional questionnaire |
| Pain with NPRS | 1 | Physical impairment |
| Occupation and recreation questionnaire | 1 | Self-reported functional questionnaire |
*Abbreviations: VAS = visual analog scale, ULTT2b = upper limb tension test 2b, ADL = activities of daily living, ROM = range of motion, MMT = manual muscle test, DASH = disabilities of the arm, shoulder and hand, NPRS = numeric pain rating scale.
Methodological Quality
Quality scores for the included articles ranged from 1–8 with a mean score of 5.2 (SD 1.9). PEDro criteria most frequently satisfied were comparison between groups (100%), reporting of point measures and variability (92%), and random allocation (85%). No study was found to have satisfied criteria 5 and 6 regarding blinding of subjects and of treating clinicians. Successful blinding of patients and therapists proves to be difficult when applying a manual treatment. Low rates of satisfaction among the sample of articles were also identified for intention to treat analysis for at least one outcome measure (15%), concealment of group allocation (38%), and blinding of the outcome assessor (46%). A full breakdown of PEDro scores by criteria for each article is available in Table 3.
TABLE 3.
Breakdown of PEDro scoring for each study.
| Criteria | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Score |
| Bisset et al42 | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Paungmali et al33 | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Struijs et al41 | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7/10 |
| Verhaar et al45 | Y | Y | Y | N | N | N | Y | N | Y | Y | 6/10 |
| Cleland et al43 | Y | Y | Y | N | N | N | Y | N | Y | Y | 6/10 |
| Drechsler et al38 | Y | N | Y | N | N | N | Y | N | Y | Y | 5/10 |
| Langen-Pieters et al40 | Y | N | Y | N | N | N | Y | N | Y | Y | 5/10 |
| Stasinopoulos & Stasinopoulos44 | N | N | Y | N | N | Y | Y | N | Y | Y | 5/10 |
| Vicenzino et al36 | Y | N | N | N | N | Y | Y | N | Y | Y | 5/10 |
| Kochar & Dogra39 | Y | N | Y | N | N | N | N | N | Y | Y | 4/10 |
| Vicenzino et al35 | Y | N | N | N | N | Y | N | N | Y | Y | 4/10 |
| Vicenzino et al34 | Y | N | N | N | N | N | N | N | Y | Y | 3/10 |
| Baltaci et al37 | |||||||||||
|
N |
N |
N |
N |
N |
N |
N |
N |
Y |
N |
1/10 |
|
| Total by criteria | 11/13 | 5/13 | 9/13 | 0/13 | 0/13 | 6/13 | 9/13 | 2/13 | 13/13 | 12/13 | |
*PEDro criteria: (2) random allocation to groups; (3) allocation was concealed; (4) group similarity at baseline; (5) blinding of subjects; (6) blinding of therapists; (7) blinding of outcome assessors; (8) measurement of at least one key outcome obtained from at least 85% of the group; (9) intention-to-treat analysis for at least one key outcome; (10) between group comparison for at least one key outcome; (11) reported point measurements and measurements of variability for at least one key outcome.
Mobilization with Movement (MWM)
Four studies33,36,39,42 examined the use of MWM directed at the elbow as described by Mulligan18 (Table 4). PEDro scores ranged from 4–8 with a mean quality score of 6.25. Two studies33,36 compared MWM with a placebo technique and a no-treatment control, while two39,42 compared MWM with other treatment regimens. The immediate positive effects of MWM were demonstrated by Vicenzino et al36 and Paungmali et al33, whose studies showed significant increases in pain-free grip following application of MWM as opposed to the placebo or control conditions. The addition of MWM to ultrasound (US) + exercise was found to provide benefits in the short term (3 months or less) by Kochar and Dogra39, whose results showed significant improvements in visual analog scale (VAS) pain, grip strength, patient assessment, and weight test performance when compared to a US + exercise group and/or no treatment control. Bisset and colleagues42 favored MWM over wait-and-see but not corticosteroid injection at 6 weeks. However, MWM was favored over the injection group during follow-up past 6 weeks as the steroid group experienced a high rate of recurrence (72%). Long-term follow-up displayed similar outcomes for those in the MWM and wait-and-see groups who were not significantly different at 52 weeks. Overall, MWM was shown, by studies of fair to high quality, to provide favorable outcomes over the short and long term when compared to placebo or other modes of treatment.
TABLE 4.
Studies examining MWM.
| Study | Design/Score | Treatment | Frequency | Outcomes | Results | F/U |
|---|---|---|---|---|---|---|
| Bisset et al42 |
|
MWM & exercise; injection; wait-and-see |
|
Global change, PFGS, VAS-pain, PFF questionnaire, assessor's rating | MWM 65% reported success @ 6 weeks, 94% @ 52 weeks; favored over wait-and-see @ 6 weeks; MWM over injection favored @ 52 weeks (NNT=4); injection group 72% recurrence rate; MWM group 8% recurrence rate | 6 and 52 wks |
| Paungmali et al33 |
|
MWM; placebo; control | Each subject experienced each treatment in randomized order with 48-hour washout between sessions | PFGS, PPT, TPT, SNS activity | MWM 47.5% inc. PFGS, PPT increase from 281.4 kPa to 300.8 kPa, measurable increase in SNS function | Outcomes captured during and immediately afer treatment |
| Vicenzino et al36 |
|
MWM; placebo; control | Each subject experienced each treatment in randomized order with 48-hour washout between sessions | PFGS, PPT | MWM 58% increase in PFGS, 10% increase in PPT | Outcomes captured during and immediately afer treatment |
| Kochar & Dogra39 |
|
MWM+ US+Ex; US+Ex; no treatment control | 10 treatments over 3 weeks | VAS-pain, grip strength, weight test, patient assessment over last 24 hrs. | 12 weeks: MWM group 5.9cm dec. VAS-pain, 4.04 kg. Weight test increase, 8.83kg increase in grip strength, greater pt. Assessment scores; MWM group had significantly better outcomes when compared to other 2 groups | 1, 2, 3, and 12 wks. |
*Abbreviations: MWM = mobilization with movement, PFGS = pain-free grip strength, VAS = visual analog scale, PFF = pain-free function, PPT = pressure pain threshold, TPT = thermal pain threshold, SNS = sympathetic nervous system, US = ultrasound, NNT = number needed to treat.
Mobilization of the Cervical Spine
Three studies34,35,43 examined the effect of mobilization directed at the cervical spine on LE symptoms. Descriptions outlining technique and application can be found in each respective study's methods section (Table 5). PEDro scores ranged from 3–6 with an average quality score of 4.3. Two studies34,35 of poor and fair quality compared the use of cervical spine mobilization versus placebo and control conditions while one study compared two treatment regimens, one that included cervical spine mobilization and one that did not. Two studies found significant improvements in pain-free grip strength, pressure pain threshold, and upper limb tension test 2b (ULTT2b) position immediately following cervical mobilization34,35. One high-quality study43 demonstrated that the addition of cervical spine mobilization to a treatment regimen including manual therapy and exercise directed at the elbow and wrist resulted in significant improvements in pain-free grip, numeric pain rating scale (NPRS), Disabilities of the Arm, Shoulder and Hand (DASH) scores, and global rating of change scores. Outcomes for the cervical mobilization group were found to be superior both at discharge (6 weeks) and at 6-month follow-up.
TABLE 5.
Studies examining cervical spine mobilization.
| Study | Design/Score | Treatment | Frequency | Outcomes | Results | F/U |
|---|---|---|---|---|---|---|
| Cleland et al43 |
|
C-spine + local treatment local treatment alone | 2 × week × 4 weeks followed by 1 × week × 2 weeks, 10 visits over 6-week period | NPRS, PFGS, DASH questionnaire GROC @ 6 months | @ D/C: c-spine group scored 10 points better on DASH, 1.6 better on NRPS, 14.6 kg better PFGS @ 6 months: C-spine group scored 14.4 points better better on NPRS, and 19.6 kg better PFGS GROC scores @ 6 months showed greater improvement in c-spine group | Discharge (6 weeks) and 6 months |
| Vicenzino et al35 |
|
C-spine mobilization; placebo; control | All subjects experienced each treatment in randomized order over 3-day period | PFGS, PPT, VAS-pain, ULTT2b, VAS functional scale | C-spine mobilization: 7 degree increase in ULTT2b, 33.2 N increase in PFGS, 45 kPa increase in PPT, 1.9cm improvement in VAS-pain, no significant difference in VAS-function between groups | Outcomes captured immediately afer treatment and 24 hrs. Later for pain and function |
| Vicenzino et al34 |
|
C-spine mobilization; placebo; control | Each subject experienced each treatment in randomized order with 48-hour washout between sessions | ULTT2b, PPT, TPT, PFGS, SNS activity | C-spine mobilization: 6.89 degree increase in ULTT2b, 75.74 kPa increase in PPT, 13.98 N increase PFGS | Outcomes captured immediately afer treatment |
*Abbreviations: NRPS = numeric pain rating scale, PFGS = pain-free grip strength, DASH = disabilites of the arm, shoulder and hand, GROC = global rating of change, PPT = pressure pain threshold, VAS = visual analog scale, ULTT2b = upper limb tension test 2b, TPT = thermal pain threshold, SNS = sympathetic nervous system
Cyriax Physiotherapy
Three studies37,44,45 examined the effectiveness of Cyriax physiotherapy (Table 6). PEDro scores ranged from 1–6 with an average quality score of 4. All of the included studies compared the use of Cyriax physiotherapy with another mode of treatment. One study37 of poor quality supported the effectiveness of Cyriax physiotherapy. Baltaci et al37 found that Cyriax physiotherapy combined with the use of an elbow band led to greater improvements in pain and ROM when compared to a group receiving conventional treatment including stretching, exercise, and modalities. One high-quality study45 found that corticosteroid injection led to greater improvements in grip strength and patient satisfaction at 6 weeks. One fair-quality study44 favored supervised exercise over both Cyriax physiotherapy and polarized polychromatic non-coherent light therapy for improvements in pain, pain-free grip strength, and function.
TABLE 6.
Studies examining Cyriax physiotherapy.
| Study | Design/Score | Treatment | Frequency | Outcomes | Results | F/U |
|---|---|---|---|---|---|---|
| Verhaar et al45 |
|
Cyriax physiotherapy; local corticosteroid injection |
|
Grip strength, patient assessment of satisfaction |
|
6 and 52 weeks |
| Stasinopoulos & Stasinopoulos 44 |
|
Cyriax physiotherapy; supervised exercise; polarized polychromatic non-coherent light therapy (Bioptron) | 3 × week for 4 weeks | VAS-pain, VAS-function, PFGS |
|
4, 8, 16, and 28 weeks |
| Baltaci et al37 |
|
Cyriax physiotherapy with elbow band; conventional physiotherapy | Not clearly stated | VAS-pain, VAS-function, ROM, grip strength, MMT | Cyriax group scored significantly better on VAS-pain, VAS-function, grip strength, and wrist extension, flexion, pronation and supination MMT | Not clearly stated |
*Abbreviations: VAS = visual analog scale, PFGS = pain-free grip strength, ROM = range of motion, MMT = manual muscle test
Other Manipulative Techniques
Three studies38,40,41 were included that dealt with other forms of manipulative therapy directed at treating LE. Descriptions outlining technique and application can be found in each respective study's methods section (Table 7). One high-quality study41 examined the effectiveness of wrist manipulation compared to a treatment consisting of US, friction massage, and exercise. Results favored the wrist manipulation group for the outcome of global improvement at 3 weeks and pain reported during the day at 6 weeks. Differences in global improvement were no longer statistically significant at 6 weeks. One fair-quality study38 examined the effectiveness of a neural tension treatment including ULTT2b neural mobilization combined with radial head mobilizations when indicated compared to standard treatment. Results favored those who received radial head mobilization for improved occupational status measured at discharge and recreational status measured at discharge and 3-month follow-up. One-fair quality study40 examined the effectiveness of manipulation according to restrictions found during exam combined with exercise compared with ultrasound alone. Results favored the group receiving ultrasound for improved pain and Pain-free Function Tennis Elbow questionnaire scores.
TABLE 7.
Studies examining other manipulative techniques.
| Study | Design/Score | Treatment | Frequency | Outcomes | Results | F/U |
|---|---|---|---|---|---|---|
| Struijs et al41 |
|
|
|
Global improvement pain, inconvenience of ADLs, PFGS, max grip strength |
|
3 and 6 weeks |
| Drechsler et al38 |
|
|
2 × week for 6–8 weeks | Grip strength, ULTT2b position (degrees), occupation and recreation self-report questionnaires | Recreational status improved at d/c and follow-up in neural tension group, recreational status improved in standard group at d/c but not at follow-up; ULTT2b improved in neural tension group at d/c and follow-up; no significant changes in grip strength for either group | Assessed @ discharge and 3 months |
| Langen-Pieters et al40 |
|
|
2 × week for 6 weeks | PFGS, VAS-pain, PFF tennis elbow questionnaire overall improvement |
|
3 and 6 weeks |
*Abbreviations: US = ultrasound, ADL = activities of daily living, PFGS = pain-free grip strength, ULTT2b = upper limb tension test 2b, VA S = visual analog scale, PFF = pain-free function
Discussion
No other systematic reviews specifically focusing on manipulative therapy directed at treating LE were identified during the literature search. Previous reviews15,16 have included studies dealing with manipulation; however, some studies were excluded from the results of these studies because standards of quality for inclusion were not met or the study was not yet published, as in the case of Bisset et al42. Minimum levels of quality for inclusion were not used in this review for the purpose of including those studies that may have been excluded from past reviews.
The results of published studies should be viewed objectively as the validity and generalizability of these results are a function of the study's overall quality. Assessment of quality is essential as it directly affects conclusions that are made regarding how an individual study influences clinical decision-making and contributes to the overall body of evidence. The average quality score for the 13 articles included in this review was 5.15/10 points, representing fair and acceptable quality. Trends in PEDro criteria scoring for the group showed significant methodological flaws; for example, no study met the PEDro criteria for blinding of patients or treating therapists. Regardless of the apparent difficulty in achieving successful blinding in trials involving manual treatment, lack of blinding may introduce expectation bias as well as the potential for cointervention on the part of the treating therapist46,47. Cointervention is a term that describes when a treatment that can affect outcomes is not equally administered to all groups46. In the absence of patient/therapist blinding, it is recommended that blinded outcome assessors be used to account for investigator bias48. Less then 50% of included studies used a blinded assessor to capture outcomes. This has been found to lead to greater reports of treatment effect49, and results should be interpreted cautiously.
A total of 17 different measures were used at varying frequencies to assess outcomes in the group of studies. The measure most frequently used was pain-free grip strength with 69% of studies including it as one of their outcomes. Pain-free grip strength has been established as a valid method for capturing change in LE50. While measurements of physical impairments, like pain-free grip, may be sensitive to change, they may not have a linear correlation with a patient's level of function51. The relationship between impairments and function or disability is often times complicated and involves many other factors51.
The inclusion of functional outcome questionnaires can provide additional important information regarding function, disability, and overall quality of life. The use of these tools has been recommended as an effective adjunct to gauge outcomes in patients with low back pain52. Unfortunately, the use of specific functional questionnaires was only reported in 4 of the studies38,40,42,43 examined here. Formulating a relationship between treatment and functional impact is difficult to establish. Aside from regional questionnaires such as the DASH and Upper Extremity Functional Index (UEFI), the Patient-rated Tennis Elbow Evaluation Questionnaire (PRTEE) is a condition-specific outcome measure developed for patients with LE53 that is valid and reliable and has been recommended as a primary outcome measure for patients with LE53.
In terms of specific techniques, Mulligan's mobilization with movement was the most frequently studied. In addition, that group of studies had the highest mean quality score (6.25/10) as well. Mulligan's technique was shown to provide benefits both immediate and at short- and long-term follow-up, although these results should be generalized to the clinical population with care. Specifically, care should be taken when interpreting the results of Vicenzino et al36 and Paungmali et al33, whose goals were to examine the pain-relieving effects of the technique. Paungmali and colleagues33 noted, for example, that their purpose was not to determine the effect that the technique had on patient function but rather to describe the physiological effects following application.
Mobilization directed at the cervical spine was also found to provide benefits in those with LE24,34,35. However, the results of those studies may have low generalizability as 2 out of the 3 were only concerned with the immediate effects following application of the technique. Cleland and colleagues43 examined outcomes of cervical spine mobilization as an adjunct to therapy already directed at the elbow and wrist and found favorable results. However, generalizability is again in question due to the small sample size as well as the requirement of cervical and thoracic spine joint restrictions for inclusion in the study.
Isolated manipulation of the wrist41 was found to provide superior short-term outcomes compared to multi-modal intervention. The results of this high-quality study encourages future research that examines the effect when manipulation of the wrist as part of a multi-modal treatment as opposed to being implemented alone. Cleland et al43 provided an example wherein manual therapy directed at the wrist was an included technique; it was listed as part of the local treatment directed at the elbow and wrist in their study examining cervical spine mobilization.
Limitations
A possible limitation to this review was the exclusion of articles using single group design. Although lower on the evidence hierarchy, the inclusion of these articles may have made a worthy contribution to this review as the number of available RCTs was limited. Another potential limitation was the use of a single person (CH) who was responsible for determining appropriateness for inclusion; this may have contributed to selection bias. The increased variability regarding manipulative technique, comparison interventions, follow-up, and outcome measures also made it very difficult to compare results across studies and draw relevant conclusions. Finally, no attempt was made to locate and obtain unpublished data, which introduces the potential for publication bias. These sources can prove to be difficult to identify and obtain when not indexed in databases such as Medline54. Lack of indexing is a significant barrier to successfully incorporating unpublished data into the search methodology, and for this reason it was not included in this review.
Conclusion
The current body of evidence regarding the use of manipulation in treating LE varies significantly in regards to technique and comparison treatments. Currently, there are not enough published studies to support a systematic review focusing on any particular technique. The results of this review support and build upon the conclusions reached by Bisset et al16. Current evidence supports Mulligan's mobilization with movement in providing not only immediate benefits but also improving outcomes at short- and long-term follow-up. There exists a potential for improvement with cervical spine mobilization, indicating the need for further research. Perhaps a subgroup of patients with LE exists who would benefit from treatment directed at the cervical spine. Future studies are warranted that use larger sample sizes, valid functional outcome questionnaires such as the PRTEE, short- and long-term patient follow-up, and inclusion of comparison treatments that are currently used in clinical practice.
REFERENCES
- 1.Dimberg L. The prevalence and causation of tennis elbow (lateral humeral epicondylitis) in a population of workers in an engineering industry. Ergonomics. 1987;30:573–580. doi: 10.1080/00140138708969746. [DOI] [PubMed] [Google Scholar]
- 2.Shiri R, Viikari-Juntura E, Varonen H, Heliovaara M. Prevalence and determinants of lateral and medial epicondylitis: A population study. Am J Epidemiol. 2006;164:1065–1074. doi: 10.1093/aje/kwj325. [DOI] [PubMed] [Google Scholar]
- 3.Murphy KP, Giuliani JR, Freedman BA. The diagnosis and management of lateral epicondylitis. Curr Opin Orthop. 2006;17:134–138. [Google Scholar]
- 4.Vicenzino B, Wright A. Lateral epicondylalgia I: A review of epidemiology, pathophysiology, aetiology and natural history. Phys Ther Rev. 1996;1:23–34. [Google Scholar]
- 5.Vicenzino B. Lateral epicondylalgia: A musculoskeletal physiotherapy perspective. Man Ther. 2003;8:66–79. doi: 10.1016/s1356-689x(02)00157-1. [DOI] [PubMed] [Google Scholar]
- 6.Smidt N, Lewis M, van der Windt D, Hay EM, Bouter LM, Croft P. Lateral epicondylitis in general practice: Course and prognostic indicators of outcome. J Rheumatol. 2006;33:2053–2059. [PubMed] [Google Scholar]
- 7.Chard MD, Cawston TE, Riley GP, Gresham GA, Hazleman BL. Rotator cuff degeneration and lateral epicondylitis: A comparative histological study. Ann Rheum Dis. 1994;53:30–34. doi: 10.1136/ard.53.1.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Potter HG, Hannafin JA, Morwessel RM, DiCarlo EF, O'Brien SJ, Altchek DW. Lateral epicondylitis: Correlation of MR imaging, surgical, and histopathologic findings. Radiology. 1995;196:43–46. doi: 10.1148/radiology.196.1.7784585. [DOI] [PubMed] [Google Scholar]
- 9.Waugh EJ. Lateral epicondylalgia or epicondylitis: What's in a name? J Orthop Sports Phys Ther. 2005;35:200–202. doi: 10.2519/jospt.2005.0104. [DOI] [PubMed] [Google Scholar]
- 10.Bishai SK, Plancher KD. The basic science of lateral epicondylosis: Update for the future. Tech Orthop. 2006;21:250–255. [Google Scholar]
- 11.Kaminsky SB, Baker CL. Lateral epicondylitis of the elbow. Tech Hand Up Extrem Surg. 2003;7:179–189. doi: 10.1097/00130911-200312000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Wright A, Vicenzino B. Lateral epicondylalgia II: Therapeutic management. Phys Ther Rev. 1997;2:39–48. [Google Scholar]
- 13.Haker E. Lateral epicondylalgia: Diagnosis, treatment, and evaluation. Critical Reviews in Physical and Rehabilitation Medicine. 1993;5:129–154. [Google Scholar]
- 14.Labelle H, Guibert R, Newman N, Fallaha M, Rivard CH. Lack of scientific evidence for the treatment of lateral epicondylitis of the elbow: An attempted meta-analysis. J Bone Joint Surg. 1992;74B:646–651. doi: 10.1302/0301-620X.74B5.1388172. [DOI] [PubMed] [Google Scholar]
- 15.Smidt N, Assendelft W, Arola H, et al. Effectiveness of physiotherapy for lateral epicondylitis: A systematic review. Ann Med. 2003;35:51–62. doi: 10.1080/07853890310004138. [DOI] [PubMed] [Google Scholar]
- 16.Bisset L, Paungmali A, Vicenzino B, Beller E. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med. 2005;39:411–422. doi: 10.1136/bjsm.2004.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kushner S, Reid D. Manipulation in the treatment of tennis elbow. J Orthop Sports Phys Ther. 1986;7:264–272. doi: 10.2519/jospt.1986.7.5.264. [DOI] [PubMed] [Google Scholar]
- 18.Mulligan B. Manual Therapy: NAGS, SNAGS, MWMS, etc, 5th ed. Wellington, NZ: Plane View Services; 2006. [Google Scholar]
- 19.Vicenzino B, Cleland JA, Bisset L. Joint manipulation in the management of lateral epicondylalgia: A clinical commentary. J Man Manip Ther. 2007;15:50–56. doi: 10.1179/106698107791090132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Physical Therapy Association Guide to Physical Therapist Practice. 2nd ed. Phys Ther. 2001;81:9–746. [PubMed] [Google Scholar]
- 21.Maher C, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–721. [PubMed] [Google Scholar]
- 22.Abbott JH. Mobilization with movement applied to the elbow affects shoulder range of movement in subjects with lateral epicondylalgia. Man Ther. 2001;6:170–177. doi: 10.1054/math.2001.0407. [DOI] [PubMed] [Google Scholar]
- 23.Abbott JH, Patla CE, Jensen RH. The initial effects of an elbow mobilization with movement technique on grip strength in subjects with lateral epicondylalgia. Man Ther. 2001;6:163–169. doi: 10.1054/math.2001.0408. [DOI] [PubMed] [Google Scholar]
- 24.Cleland JA, Whitman J, Fritz J. Effectiveness of manual physical therapy to the cervical spine in the management of lateral epicondylalgia: A retrospective analysis. J Orthop Sports Phys Ther. 2004;34:713–724. doi: 10.2519/jospt.2004.34.11.713. [DOI] [PubMed] [Google Scholar]
- 25.Kaufman R. Conservative chiropractic care of lateral epicondylitis. J Manipulative Physiol Ther. 2000;23:619–622. doi: 10.1067/mmt.2000.110942. [DOI] [PubMed] [Google Scholar]
- 26.Paungmali A, Vicenzino B, Smith M. Hypoalgesia induced by elbow manipulation in lateral epicondylalgia does not exhibit tolerance. J Pain. 2003;4:448–454. doi: 10.1067/s1526-5900(03)00731-4. [DOI] [PubMed] [Google Scholar]
- 27.Vicenzino B, Wright A. Effects of a novel manipulative physiotherapy technique on tennis elbow: A single case study. Man Ther. 1995;1:30–35. doi: 10.1054/math.1995.0247. [DOI] [PubMed] [Google Scholar]
- 28.Hashemi K, Blakeley C. Elbow manipulation combined with steroid injection: An effective treatment for resistant cases of tennis elbow. Journal One-Day Surgery. 2007;17:45–48. [Google Scholar]
- 29.Madan S, Jowett R. Lateral epicondylalgia: Treatment by manipulation under anaesthetic and steroid injection and operative release. Acta Orthopaedica Belgica. 2000;66:449–454. [PubMed] [Google Scholar]
- 30.Rompe JD, Riedel C, Betz U, Fink C. Chronic lateral epicondylitis of the elbow: A prospective study of low-energy shockwave therapy plus manual therapy of the cervical spine. Arch Phys Med Rehabil. 2001;82:578–582. doi: 10.1053/apmr.2001.22337. [DOI] [PubMed] [Google Scholar]
- 31.Slater H, Arendt-Nielsen L, Wright A, Graven-Nielsen T. Effects of a manual therapy technique in experimental lateral epicondylalgia. Man Ther. 2006;11:107–117. doi: 10.1016/j.math.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 32.Paungmali A, O'Leary S, Souvlis T, Vicenzino B. Naloxone fails to antagonize initial hypoalgesic effect of a manual therapy treatment for lateral epicondylalgia. J Manipulative Physiol Ther. 2004;27:180–185. doi: 10.1016/j.jmpt.2003.12.022. [DOI] [PubMed] [Google Scholar]
- 33.Paungmali A, O'Leary S, Souvlis T, Vicenzino B. Hypoalgesic and sympathoexcitatory effects of mobilization with movement for lateral epicondylalgia. Phys Ther. 2003;83:374–383. [PubMed] [Google Scholar]
- 34.Vicenzino B, Collins D, Benson H, Wright A. An investigation of the interrelationship between manual therapy-induced hypoalgesia and sympatheoexcitation. J Manipulative Physiol Ther. 1998;21:448–453. [PubMed] [Google Scholar]
- 35.Vicenzino B, Collins B, Wright A. The initial effects of a cervical spine manipulative physiotherapy treatment on the pain and dysfunction of lateral epicondylalgia. Pain. 1996;68:69–74. doi: 10.1016/S0304-3959(96)03221-6. [DOI] [PubMed] [Google Scholar]
- 36.Vicenzino B, Paungmali A, Buratowski S, Wright A. Specific manipulative therapy treatment for chronic lateral epicondylalgia produces uniquely characteristic hypoalgesia. Man Ther. 2001;6:205–212. doi: 10.1054/math.2001.0411. [DOI] [PubMed] [Google Scholar]
- 37.Baltaci G, Ergun N, Tunay VB. Effectiveness of Cyriax manipulative therapy and elbow band in the treatment of lateral epicondylitis. Eur J Sport Traumatol Rel Res. 2001;23:113–118. [Google Scholar]
- 38.Drechsler W, Knarr JF, Snyder-Mackler L. A comparison of two treatment regimens for lateral epicondylitis: A randomized trial of clinical interventions. J Sport Rehabil. 1997;6:226–234. [Google Scholar]
- 39.Kochar M, Dogra A. Effectiveness of a specific physiotherapy regimen on patients with tennis elbow. Physiotherapy. 2002;88:333–341. [Google Scholar]
- 40.Langen-Pieters P, Weston P, Brantingham JW. A randomized, prospective pilot study comparing chiropractic care and ultrasound for the treatment of lateral epicondylitis. Euro J Chiro. 2003;50:211–218. [Google Scholar]
- 41.Struijs PA, Damen PJ, Bakker E, Blankevoort L, Assendelft W, van Dijk CN. Manipulation of the wrist for management of lateral epicondylitis: A randomized pilot study. Phys Ther. 2003;83:608–616. [PubMed] [Google Scholar]
- 42.Bisset L, Beller E, Jull G, Brooks P, Darnell R, Vicenzino B. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: Randomized trial. BMJ. 2006;333:939. doi: 10.1136/bmj.38961.584653.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cleland JA, Flynn TW, Palmer JA. Incorporation of manual therapy directed at the cervicothoracic spine in patients with lateral epicondylalgia: A pilot clinical trial. J Man Manip Ther. 2005;13:143–151. [Google Scholar]
- 44.Stasinopoulos D, Stasinopoulos I. Comparison of effects of Cyriax physiotherapy: A supervised exercise program and polarized polychromatic non-coherent light (Bioptron light) for the treatment of lateral epicondylitis. Clin Rehabil. 2006;20:12–23. doi: 10.1191/0269215506cr921oa. [DOI] [PubMed] [Google Scholar]
- 45.Verhaar JA, Walenkamp GH, van Mameren H, Kester AD, van der Liden AJ. Local corticosteroid injection versus Cyriax-type physiotherapy for tennis elbow. J Bone Joint Surg. 1996;78B:128–132. [PubMed] [Google Scholar]
- 46.Guyatt G, Rennie D. Users' Guide to the Medical Literature: A Manual for EvidenceBased Clinical Practice. Chicago, IL: AMA Press; 2002. [Google Scholar]
- 47.Helewa A, Walker JM. Critical Evaluation of Research in Physical Rehabilitation. Philadelphia, PA: Saunders; 2000. [Google Scholar]
- 48.Licciardone JC, Russo DP. Blinding protocols, treatment credibility, and expectancy: Methodological issues in clinical trials of osteopathic manipulative treatment. JAOA. 2006;106:457–463. [PubMed] [Google Scholar]
- 49.Poolman RW, Struijs PA, Krips R, et al. Reporting of outcomes in orthopaedic randomized trials: Does blinding of outcome assessors matter? J Bone Joint Surg. 2007;89A:550–558. doi: 10.2106/JBJS.F.00683. [DOI] [PubMed] [Google Scholar]
- 50.Stratford PW, Levy DR, Gowland C. Evaluative properties of measures used to assess patients with lateral epicondylitis at the elbow. Physiother Can. 1993;45:160–164. [Google Scholar]
- 51.Jette AM. Outcomes research: Shifting the dominant research paradigm in physical therapy. Phys Ther. 1995;75:965–970. doi: 10.1093/ptj/75.11.965. [DOI] [PubMed] [Google Scholar]
- 52.Resnik L, Dobrzykowsi E. Guide to outcomes measurements for patients with low back pain syndromes. J Orthop Sports Phys Ther. 2003;33:307–315. doi: 10.2519/jospt.2003.33.6.307. [DOI] [PubMed] [Google Scholar]
- 53.Rompe JD, Overend TJ, MacDermid JC. Validation of the patient-rated tennis elbow evaluation questionnaire. J Hand Ther. 2007;20:3–11. doi: 10.1197/j.jht.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 54.Banks M. Connections between open access publishing and access to gray literature. J Med Libr Assoc. 2004;92:164–166. [PMC free article] [PubMed] [Google Scholar]