Abstract
Background
Very few prospective studies examine the relationship between childhood sleep problems and subsequent substance use. In this study, we examined how sleep problems at ages 3–8 predicted onset of alcohol, cigarette, and marijuana use in adolescence. We also investigated the relationships between childhood sleep problems and adolescent internalizing and externalizing problems.
Methods
Study participants were 292 boys and 94 girls from a community sample of high-risk families and controls in an ongoing longitudinal study.
Results
Controlling for parental alcoholism, sleep problems at ages 3–8 predicted onset of alcohol, cigarette, and marijuana use among boys and onset of alcohol use among girls. Childhood sleep problems were related to maternal ratings of internalizing and externalizing problems during adolescence for both boys and girls. Adjusting for these problems did not weaken the effects of sleep problems on onset of substance use.
Conclusions
This is to our knowledge the first study that prospectively examines gender differences in the relationship between sleep problems and early onset of substance use. Childhood sleep problems predicted early onset of substance use for boys but not girls. If childhood sleep problems indeed increase the probability of substance use onset, greater attention by parents to sleep problems in children and adolescents would potentially have ameliorative long-term effects. Parents are encouraged to explore different ways to help their children sleep better, including obtaining information and suggestions from their primary care physicians.
Keywords: sleep problems, onset of alcohol use, onset of drug use, behavioral problems
1. Introduction
Sleep problems, especially insomnia, have been shown to predict subsequent onset of alcohol and other drug use disorders among adults [1–3]. Much less is known about the prospective relationship between sleep problems in childhood and substance use in adolescence. Several cross-sectional epidemiological studies indicate that sleep pattern irregularities and sleep problems are associated with increased alcohol, cigarette, and other drug use during adolescence [4–6]. However, cross-sectional studies do not allow testing of temporal order or inferring the causal relationship between sleep problems and substance use.
Very few prospective studies exist on the relationship between sleep problems early in life and subsequent substance use. In an earlier report by our group based on 257 boys from a community-recruited sample of children of alcoholics and controls, Wong et al. [7] found that maternal ratings of children’s sleep problems at ages 3–5 predicted onset of any use of alcohol, marijuana, and illicit drugs, as well as onset of occasional or regular use of cigarettes by age 14. Moreover, while early childhood sleep problems predicted attention problems as well as anxiety and depression in late childhood, those problems did not explain the sleep-substance use onset relationship. In this paper, we extended the earlier analyses to include girls as well as additional boys and focused on possible gender differences in the relations between childhood problems and onset of substance use.
Gender differences regarding the relations between sleep problems and onset of substance use have not been widely studied. Existing cross-sectional studies seem to show inconsistent results. Vignau et al. [6] found that poor sleep was related to alcohol inebriation in 763 French adolescents, regardless of gender. However, poor sleep was related to illicit drugs use in boys but not girls. Tynjala et al [5] reported that perceived tiredness was related to the use of psychoactive substances in 4187 Finnish adolescents. Boys who were tired were more likely to drink excessively and smoked while girls who were tired were more likely to smoke. In a study of 13,381 U.S. adolescents, Johnson and Breslau [4] found a stronger association between sleep problems and substance use (including use of cigarettes, alcohol and any illicit drug) among girls than among boys. However, adjusting for internalizing or externalizing problems eliminate the gender differences. A recent study of 1,014 U.S. adolescents showed that the relationship between DSM-IV primary insomnia and substance use disorders were the same for the two sexes [8]. Given these inconsistent results, it would be important to ascertain whether there are any gender differences in the relations between sleep problems and substance use in a longitudinal study.
Previous studies appear to indicate that sleep problems are related to internalizing and externalizing problems. Wong et al. [7] reported an association between sleep problems in early childhood and internalizing problems in late childhood. Two other prospective studies also found a relationship between childhood sleep problems and internalizing problems. In one longitudinal study of 490 children, after controlling for childhood internalizing problems, a composite measure of sleep problems at 4 years old (e.g., sleepwalking, nightmares, unusual sleep duration) predicted an increase in internalizing problems in mid-adolescence [9]. Another study examining 943 children showed that after controlling for childhood internalizing problems, parental reports of persistent childhood sleep problems (i.e., reporting sleep problems at 5 or 7 years old and again at nine years old) predicted adult anxiety disorders but not adult depression [10].
Prospective studies on the relationship between sleep problems and externalizing problems are rare. Wong et al. [7] reported a prospective association between early childhood sleep problems and aggressive behavior in late childhood. Existing cross-sectional data show a relationship between sleep problems and externalizing problems. For instance, inattention and hyperactivity were associated with sleep-related breathing disorders among children referred to sleep centers [11, 12] and children who were seen in child psychiatry and general pediatric clinics [13]. Conduct problems were positively related to symptoms of sleep-disordered breathing, restless legs syndrome, or periodic leg movements during sleep among children at two general clinics [14].
Sleep disturbances may lower one’s ability to regulate, control, or inhibit emotion and behavior [15, 16]. It is possible that poor sleep contributes to an elevated level of internalizing and externalizing problems. Both problems have been known to predict alcohol use and problems among adolescents and young adults [17–20]. Could internalizing and externalizing problems (e.g., anxiety, aggression) explain the association between sleep problems and adolescent substance use? Controlling for internalizing and externalizing problems, do childhood sleep problems still significantly predict onset of substance use in adolescence?”
This paper has three goals. First, we examined possible gender differences in the relations between childhood problems and onset of substance use. While Wong et al. [7] focused on onset of substance use by a certain age (14 years old) among boys, this paper examined onset of substance use from childhood to adolescence (3–17 years old) in both boys and girls. Thus this paper offers a more thorough analysis of the relation between sleep problems and substance use onset. Second, we analyzed the relationship between sleep problems and the developmental trajectories of internalizing and externalizing problems from childhood to adolescence. These analyses were absent from previous longitudinal studies [7,9,10]. Third, we examined whether childhood sleep problems predicted adolescent substance use after controlling for the developmental trajectories of internalizing and externalizing problems.
2. Methods
2.1 Participants
The present study is part of an ongoing longitudinal family study of the development of risk for alcohol and other substance use disorders [21–25]. The larger study recruited a population-based sample of 311 alcoholic men, their partners (whose substance use disorder was free to vary), and their initially 3–5-year-old sons. The 3–11-year-old daughters in the families were also invited to participate in the longitudinal study after the study began. The majority of these girls joined the project between ages 6 to 11.
Alcoholic men were identified by population sampling methods involving (a) a canvass of all courts in a four-county-wide area for drunk drivers with high blood alcohol levels (BAL > 0.15%); (b) a neighborhood canvass in the areas where the court-selected alcoholics lived to recruit additional alcoholics. The neighborhood canvass also recruited a control group of children and their families who resided in the same neighborhood as the alcoholic families, but whose parents had no lifetime history of substance abuse/dependence. Offspring of control families were age matched to the male child in the alcoholic family residing in the same neighborhood [21, 23]. Both biological parents were required to be living together in the same household (either as married couples or domestic partners) and to have a 3 to 5-year old son living with them at the time of recruitment. The presence of fetal alcohol syndrome was an exclusionary criterion [26, 27]. Analyses of benchmark indicators reported by Zucker et al. [23] showed that the level of psychiatric comorbidity among alcoholic men in this sample is higher than that in the general U.S. population of alcoholics, but somewhat lower than that found in clinical populations.
The current sample consists of 292 boys and 94 girls and both of their biological parents. They were selected from the original study because data on both sleep problems and substance use were present. This represents 94% of the total sample. 75% of participants (223 boys; 67 girls) had at least one parent who was a lifetime alcoholic when they were 3–8 years old; and 25% of participants were controls.
All families were Caucasian-Americans, because less than 4 percent of the population in the study sampling area that met inclusion criteria was non-Caucasian. Given the study’s sample size, if non-Caucasian ethnic/racial groups were included, the number available would not permit any effective analysis to be done. As there is an extensive literature showing a relationship between substance abuse and ethnic/racial status [28, 29], including such variation in the study without being able to statistically model its effects would only contribute to error. Therefore, the investigators originally opted to exclude this variation. The study is currently recruiting an additional sample of both African-American and Hispanic families using parallel recruitment criteria.
2.2 Procedures
Trained interviewers who were blind to family diagnostic status collected the data. The contact time for each family varied, depending on the data collection wave. Typically, each parent was involved for 9–10 hours and each child for seven hours spread over seven sessions. A variety of age-appropriate tasks (e.g., questionnaires, semi-structured interviews, and interactive tasks) were administered, and most of the contacts occurred in the families’ homes. Special arrangement was made to collect data from families who had relocated. No families were lost due to relocation.
Participants and their parents were interviewed at three-year intervals. Participants were 3–5 years old at Time 1, 6–8 years old at Time 2, 9–11 years old at Time 3, 12–14 years old at Time 4 and 15–17 years old at Time 5. Additionally, participants were interviewed annually between the ages of 11 and 17 years old on questions regarding alcohol and drug use. The data presented in this paper include five regular waves and seven annual waves of the study. Data on the sleep problems measures were collected at Time 1 and 2. Data on internalizing and externalizing problems were collected at Time 1 through Time 4. Data on substance use were collected from Time 4 through Time 5 as well as the annual waves.
2.3 Measures
Sleep problems
Childhood sleep problems (ages 3–8) were measured by mothers’ ratings on the Child Behavior Checklist (CBCL) [30]. The CBCL is a widely used instrument that measures common behavioral problems. Its’ reliability and validity have been demonstrated [31, 32].
Two items were used to indicate sleep problems: having trouble sleeping, and overtiredness. Responses to each item were scored on a three-point rating scale (0=not true; 1=somewhat or sometimes true; 2=very true or often true). A relatively small percentage of the sample had a score of 2 on either item (e.g., trouble sleeping at ages 3–8: 7.8% had a score of 1 and 3.6% had a score of 2; overtiredness at ages 3–8: 25.4% had a score of 1 and 1.6 % had a score of 2). Therefore each item was recoded as a dichotomous variable (0=not true, 1=sometimes or often true). Children who were rated as having problems sleeping were also more likely to be rated as overtired (χ2 (1)=13.41, p <.001). Given this relationship, in most analyses, the two items were combined to form a composite indicator of sleep problems (0=absence of both problem; 1=presence of either problem).
Onset of substance use
Substance use was assessed by the Drinking and other Drug Use History Questionnaire – Youth Version (DDHQ-Y; [33]) and the Diagnostic Interview Schedule – Child Version (DISC; [34]) at ages 11–17. All of the items in DDHQ-Y have been extensively used in a variety of survey and clinical settings. The questionnaire measures the frequency and quantity of alcohol use and problems, and the frequency of other drug use and problems.
Information about onset of substance use was collected between ages 11 to 17. Information on onset of drinking was gathered by an item in the DDHQ-Y, “How old were you the first time you ever took a drink (not just a sip)?” Information about onset of smoking was gathered by the DDHQ-Y and DIS-C. Participants were asked, “Have you ever smoked cigarettes?” and if yes, “How old were you the first time you smoked a cigarette?” Onset of marijuana use was measured by one question in DDHQ-Y, “How old were you when you first used marijuana?” Onset of use of other illicit drugs (other than marijuana) was not examined in this paper because of the low occurrence rates among the participants.
Internalizing and externalizing problems
Maternal ratings of internalizing and externalizing problems at ages 3–14 were measured by the CBCL – Parental version [30]. To make sure that internalizing and externalizing problems were measuring behaviors that are separated from sleep problems and substance use, internalizing problem items related to sleep problems and externalizing problem items related to substance use were eliminated from the analyses.
Parental alcoholism
Parental lifetime alcoholism (alcohol abuse or alcohol dependence) when the child was 3–8 years old was assessed by three instruments: the Short Michigan Alcohol Screening Test [35] the Diagnostic Interview Schedule Version III [36], and the Drinking and Drug History Questionnaire [37]. Base on information collected by these instruments, a trained clinician made diagnoses of parental alcoholism using DSM-IV criteria. The availability of three sources of information collected over three different sessions, separated sometimes by as much as several months, served as an across method validity check on respondent replies. In cases of discrepant information, the data represented by the majority of information sources was used in establishing the diagnosis. Inter-rater reliability for the diagnosis was excellent (kappa = 0.81). Children were coded as having an alcoholic parent if either parent met lifetime criteria for alcohol abuse or dependence at ages 3–8. Lifetime parental alcoholism may change over time and therefore may be different for siblings within the same family.
2.4 Analytic plan
Discrete-time survival analyses were conducted to estimate the hazard probability of onset of alcohol, cigarette and marijuana use [38, 39]. This method was chosen over continuous-time survival analyses because age of onset information was gathered in discrete numbers (e.g., 14 years old). The model for onset of first alcohol use is specified as follows:
where h(tj) is the hazard probability of first alcohol use at age j, αj is the baseline logit hazard function, β1PA is the effect of parental alcoholism on the logit hazard function, and β2SLEEP is the effect of early childhood sleep problems on the logit hazard function. Similar models were used to estimate the probability of first cigarette and marijuana use. Parental alcoholism has been shown to affect onset of drinking and other drug use. Thus its effects on substance use were controlled for in all analyses. We first tested whether sleep problems significantly interacted with parental alcoholism to affect each substance use outcome among boys and girls. It did not, so the interaction term was dropped from all subsequent analyses.
Multiple-group analyses were used to test for possible gender differences in the effects of sleep problems on onset of alcohol, cigarette and marijuana use. For each outcome, two sets of nested models were compared. In model 1, the effects of sleep problems on the outcome were constrained to be the same in both groups. In model 2 the effects of sleep problem were allowed to be different. If the difference in the deviance statistics of the two models reached a critical value (p <.05) in the χ2 test, model 1 could be rejected [39](Singer & Willet, 2003), indicating that the effect of sleep problems on the outcome was different for boys and girls.
To assess whether childhood sleep problems were related to the development of internalizing and externalizing problems, we first used latent growth modeling (LGM) to analyze individual differences in the developmental trajectories of the two problems [40–43]. We then tested the effects of sleep problems on these trajectories. In all analyses, age was used as the metric of time [39, 44–46]. Gender differences in the developmental trajectories of internalizing and externalizing problems were assessed by multiple group analyses. We also tested the effect of sleep problems on these trajectories. Gender differences in the effect of sleep problems on either the intercept or the slope factor of the trajectories were tested by multiple group analyses.
Finally, we examined whether controlling for the developmental trajectories of internalizing and externalizing problems would reduce the relationship between childhood sleep problems and adolescent substance use. One set of analyses included childhood parental alcoholism, sleep problems and externalizing problems as predictors while another set of analyses included parental alcoholism, sleep problems and internalizing problems as predictors. Because internalizing and externalizing problems show a moderate to high correlation empirically [32, 47, 48], they were not used in the same model to avoid problems of estimation.
Lastly, it is useful to note that some participants in our study came from the same family. On the average, each family has 1.77 children participated in the study. Based on the rule of thumb suggested by Muthen & Satorra [49] and Muthen [50], this type of clustering did not significantly bias our analysis. All analyses described above were carried out using MPLUS 4.0 [51].
3. Results
3.1 Descriptive statistics
At ages 3–8, about one-tenth of children (11%) were rated by their mothers as having trouble sleeping and more than one quarter (27%) were rated as overtired. One-third (33%) of the children had either sleep problem. The percentage of boys and girls who had sleep problems did not differ (χ2 (1) = 0.01, p = 0.94). Having an alcoholic parent at ages 3–8 did not significantly increase the risk of childhood sleep problems (χ2 (1) = 0.70, p = 0.40). By age 14, one-third of the participants (32%) had started drinking, nearly 30% had started smoking cigarettes and 18% had used marijuana.
3.2 Childhood sleep problems and age of onset of substance use
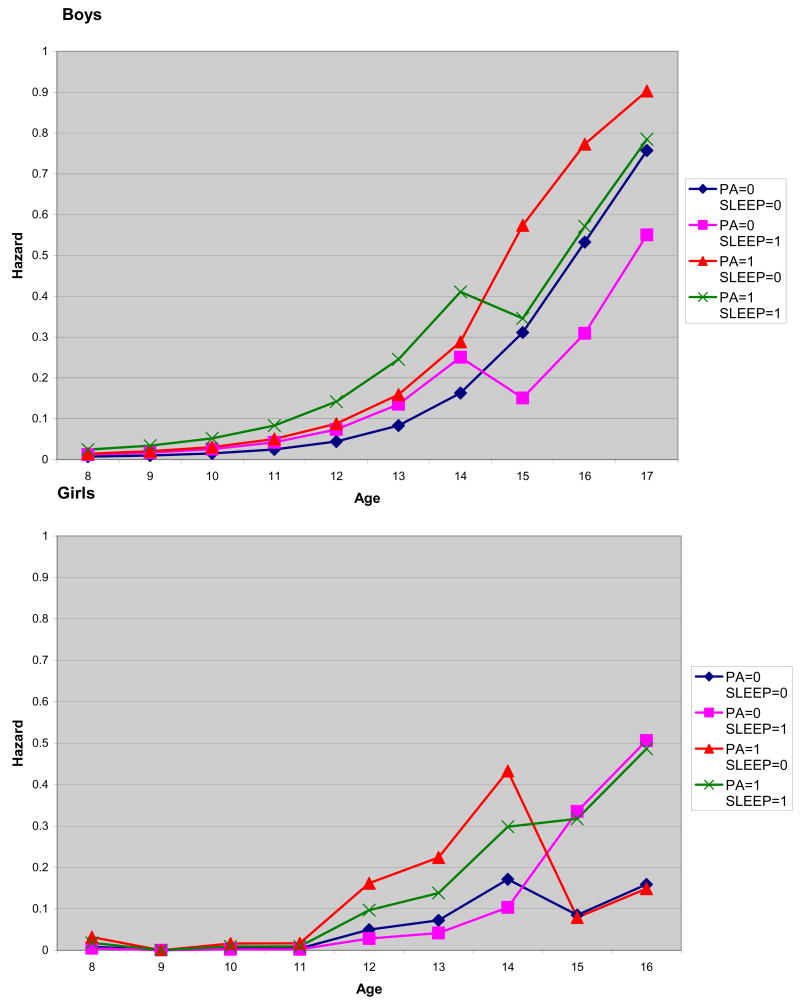
Age of onset of first alcohol use (Table 1 and Figure 1)
Table 1.
Parameter Estimates and Standard Errors Predicting Age of Onset of Alcohol Use
| Boys | Girls | |||||
|---|---|---|---|---|---|---|
| Predictor variables | Parameter | SE | ORa | Parameter | SE | ORa |
| Age 3–14 | ||||||
| Parental alcoholism | 0.73** | 0.26 | 2.08 | 1.31** | 0.49 | 3.69 |
| Sleep problems | 0.54** | 0.20 | 1.72 | −0.59 | 0.41 | -- |
| Age 15–17 | ||||||
| Parental alcoholism | 1.09** | 0.43 | 2.98 | −0.08 | 0.87 | -- |
| Sleep problems | −0.94 | 0.55 | -- | 1.69* | 0.83 | 5.42 |
| Age 3–14 | ||||||
| Parental alcoholism | 0.79* | 0.27 | 2.19 | 0.99 | 0.53 | -- |
| Sleep problems | 0.64* | 0.26 | 1.90 | −0.44 | 0.45 | -- |
| Age 15–17 | ||||||
| Parental alcoholism | 1.18** | 0.45 | 3.28 | −0.40 | 0.89 | -- |
| Sleep problems | −0.90 | 0.57 | -- | 1.75* | 0.86 | 5.75 |
| Externalizing prob. intercept | 0.03 | 0.02 | -- | 0.03 | 0.02 | -- |
| Externalizing prob. slope | 0.89** | 0.34 | 2.44 | 0.89** | 0.34 | 2.44 |
| Age 3–14 | ||||||
| Parental alcoholism | 0.73** | 0.26 | 2.08 | 1.11* | 0.52 | 3.04 |
| Sleep problems | 0.56* | 0.24 | 1.75 | −0.42 | 0.44 | -- |
| Age 15–17 | ||||||
| Parental alcoholism | 1.01** | 0.43 | 3.00 | −0.30 | 0.89 | -- |
| Sleep problems | −0.92 | 0.56 | -- | 1.84* | 0.85 | 6.30 |
| Internalizing prob. interceptb | -- | -- | -- | -- | -- | -- |
| Internalizing prob. slope | 0.11 | 0.81 | -- | 0.87 | 0.75 | -- |
Note. Three sets of results were presented here. The first model estimated how onset of alcohol use was predicted by parental alcoholism and sleep problems. The second model added externalizing problems as a predictor. The third model used internalizing problems instead of externalizing problems as the additional predictor.
Estimated odds of event occurrence when the respective explanatory variable increased by one unit. Estimated odds were calculated only when the variable was statistically significant.
Internalizing problems intercept was dropped from the analyses because (i) it has no significant relationship with onset of marijuana use and (ii) including it in the analyses led to non-convergence of model.
p < 0.05,
p < 0.01.
Figure 1.
Estimated hazard probabilities of onset of alcohol use
Note: PA = parental alcoholism (0=no and 1=yes); sleep = childhood sleep problems (0=no and 1=yes). No girls reported onset of alcohol use at age 17.
Controlling for parental alcoholism, early sleep problems significantly increased the probability of onset of drinking from ages 8 to 14 among boys. Childhood sleep problems had no relationship with onset of drinking at or prior to 14 years old among girls. Multiple group analyses showed that this difference was statistically significant (χ2 (1) = 6.41, p = 0.01). Sleep problems significantly increased the probability of drinking onset in girls from ages 15 to 17 years old. No such effect was observed in boys. Again, this difference was statistically significant (χ2 (1) = 7.50, p < 0.01). Having an alcoholic parent significantly increased the probability of alcohol use in all participants. Age of onset of cigarette use (Table 2). Sleep problems predicted onset of cigarette use from ages 7 to 11 among boys. Seep problems did not predict onset of cigarette use among girls. This gender difference was statistically significant (χ2 (1) = 6.59, p = 0.01). Having an alcoholic parent did not significantly increase the probability of onset of cigarette use in all participants.
Table 2.
Parameter Estimates and Standard Errors Predicting Age of Onset of Cigarette Use
| Boys | Girls | |||||
|---|---|---|---|---|---|---|
| Predictor variables | Parameter | SE | ORa | Parameter | SE | ORa |
| Age 7–11 | ||||||
| Parental alcoholism | 0.17 | 0.40 | -- | 3.23* | 1.23 | 25.20 |
| Sleep problems | 0.82* | 0.38 | 2.28 | −1.64 | 1.08 | -- |
| Age 12–17 | ||||||
| Parental alcoholism | 0.49 | 0.33 | -- | 2.82** | 1.06 | 16.78 |
| Sleep problems | 0.05 | 0.32 | -- | −0.53 | 0.55 | -- |
| Age 7–11 | ||||||
| Parental alcoholism | 0.37 | 0.46 | -- | 2.34 | 1.34 | -- |
| Sleep problems | 1.16* | 0.51 | 3.19 | −0.98 | 1.14 | -- |
| Age 12–17 | ||||||
| Parental alcoholism | 0.71 | 0.39 | -- | 2.19 | 1.14 | -- |
| Sleep problems | 0.49 | 0.47 | -- | −0.27 | 0.65 | -- |
| Externalizing prob. intercept | 0.07* | 0.03 | 1.07 | 0.07* | 0.03 | 1.07 |
| Externalizing prob. slope | 2.33*** | 0.59 | 10.28 | 2.33*** | 0.59 | 10.28 |
| Age 7–11 | ||||||
| Parental alcoholism | 0.10 | 0.42 | -- | 3.09* | 1.25 | 21.98 |
| Sleep problems | 1.14* | 0.44 | 3.13 | −1.54 | 1.10 | -- |
| Age 12–17 | ||||||
| Parental alcoholism | 0.41 | 0.35 | -- | 2.72* | 1.07 | 15.18 |
| Sleep problems | 0.39 | 0.39 | -- | −0.48 | 0.56 | -- |
| Internalizing prob. interceptb | -- | -- | -- | -- | -- | -- |
| Internalizing prob. slope | 1.08 | 0.65 | -- | 1.08 | 0.65 | -- |
Note. Three sets of results were presented here. The first model estimated how onset of cigarette use was predicted by parental alcoholism and sleep problems. The second model added externalizing problems as a predictor. The third model used internalizing problems instead of externalizing problems as the additional predictor.
Estimated odds of event occurrence when the respective explanatory variable increased by one unit. Estimated odds were calculated only when the variable was statistically significant.
Internalizing problems intercept was dropped from the analyses because (i) it has no significant relationship with onset of marijuana use and (ii) including it in the analyses led to non-convergence of model.
p < 0.05,
p < 0.01, p < 0.001.
Age of onset of marijuana use (Table 3)
Table 3.
Parameter Estimates and Standard Errors Predicting Age of Onset of Marijuana Use
| Boys | Girls | |||||
|---|---|---|---|---|---|---|
| Predictor variables | Parameter | SE | ORa | Parameter | SE | ORa |
| Age 7–15 | ||||||
| Parental alcoholism | 1.00** | 0.32 | 2.72 | 2.17** | 0.79 | 8.76 |
| Sleep problems | 0.49* | 0.24 | 1.63 | −0.95 | 0.51 | -- |
| Age 16–17 | ||||||
| Parental alcoholism | 1.01* | 0.41 | 2.75 | 0.20 | 1.21 | -- |
| Sleep problems | −0.85 | 0.54 | -- | 0.04 | 1.38 | -- |
| Age 7–15 | ||||||
| Parental alcoholism | 1.09** | 0.36 | 2.97 | 2.24* | 0.97 | 9.39 |
| Sleep problems | 0.77* | 0.37 | 2.16 | −1.49 | 0.81 | -- |
| Age 16–17 | ||||||
| Parental alcoholism | 1.14* | 0.45 | 3.13 | 0.20 | 1.31 | -- |
| Sleep problems | −0.54 | 0.63 | -- | −0.69 | 1.55 | -- |
| Externalizing prob. intercept | 0.02 | 0.03 | -- | 0.17* | 0.09 | 1.19 |
| Externalizing prob. slope | 1.38** | 0.49 | 3.97 | 1.38** | 0.49 | 3.97 |
| Age 7–15 | ||||||
| Parental alcoholism | 1.05** | 0.34 | 2.86 | 1.90* | 0.83 | 6.69 |
| Sleep problems | 0.30 | 0.31 | -- | −0.72 | 0.56 | -- |
| Age 16–17 | ||||||
| Parental alcoholism | 1.07* | 0.43 | 2.92 | −0.13 | 1.26 | -- |
| Sleep problems | −1.03 | 0.57 | -- | 0.16 | 1.43 | -- |
| Internalizing prob. interceptb | -- | -- | -- | -- | -- | -- |
| Internalizing prob. slope | −1.06 | 1.02 | -- | 1.82 | 1.08 | -- |
Note. Three sets of results were presented here. The first model estimated how onset of marijuana use was predicted by parental alcoholism and sleep problems. The second model added externalizing problems as a predictor. The third model used internalizing problems instead of externalizing problems as the additional predictor.
Estimated odds of event occurrence when the respective explanatory variable increased by one unit. Estimated odds were calculated only when the variable was statistically significant.
Internalizing problems intercept was dropped from the analyses because (i) it has no significant relationship with onset of marijuana use and (ii) including it in the analyses led to non-convergence of model.
p < 0.05,
p < 0.01.
Sleep problems predicted onset of marijuana use from 7 to 15 years old among boys. This effect was absent in girls. The difference was statistically significant (χ2 (1) = 6.99, p < 0.01). Having an alcoholic parent significantly increased the probability of marijuana use for both boys and girls
3.3 Childhood sleep problems and behavioral problems
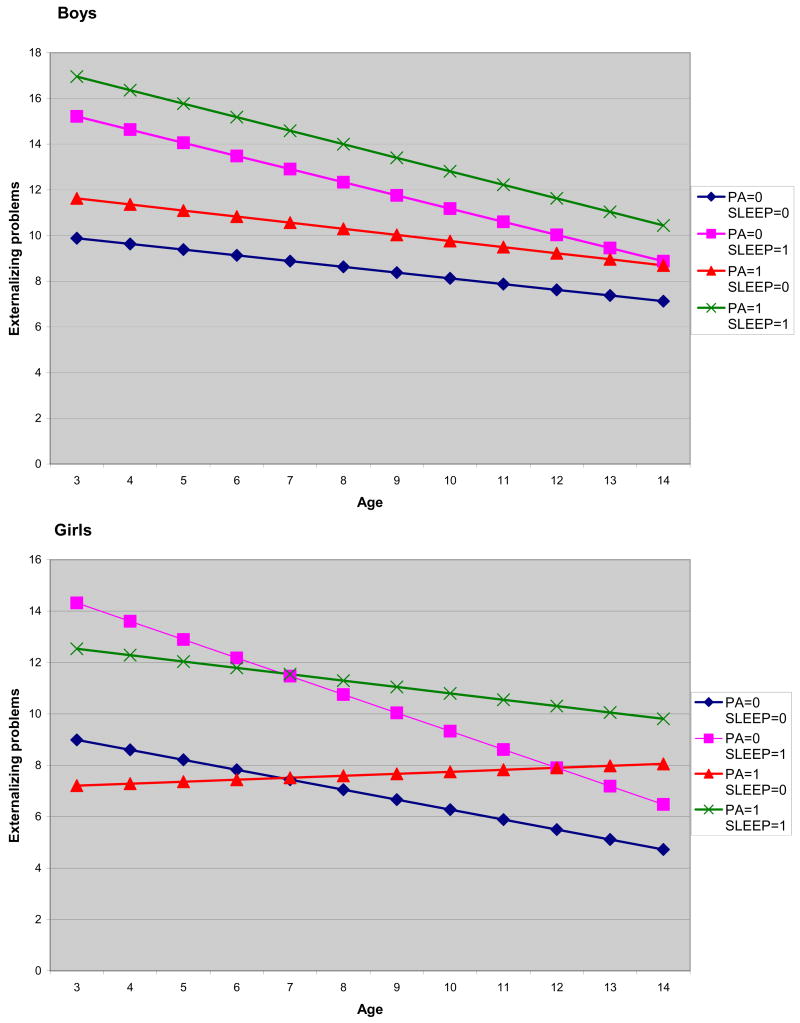
Externalizing problems
Multiple-group analyses indicated that boys had a higher externalizing problems intercept than girls. The model that allowed the intercept to be different in the two groups was significantly better than the model that constrained the coefficient to be the same (χ2 (1) = 10.87, p <.001). In contrast, the analyses could not reject that boys and girls have the same externalizing problems slope (χ2 (1) = 2.12, p =.15). Among boys, the average intercept of externalizing problems at the initial assessment period was 13.64 (ûa1 = 13.64 (.48), p <.001), with a decreasing linear slope of 0.32 unit per year (ûβ1 = −0.32 (.04), p <.001). There were significant individual differences in the initial status ( , p <.001) and the rate of change ( , p <.001), indicating participants are different in their growth trajectories. Among girls, the average intercept of externalizing problems at the initial assessment period was 11.13 (ûa1= 11.13 (.66), p <.001, with a decreasing linear slope of 0.32 unit per year (ûβ1 = −0.32 (.04), p <.001). There were significant individual differences in the initial status ( , p <.001) and the rate of change ( , p <.01).
Next we examined whether parental alcoholism and sleep problems predicted the developmental trajectories of externalizing problems from age 3 to 14. Controlling for parental alcoholism, there were no gender differences in the effect of sleep problems on the initial status (χ2 (1) = 0.24, p =.63) and rate of change (χ2 (1) = 2.20, p =.14) of externalizing problems. Regardless of gender, those with sleep problems had a higher level of externalizing problems in the initial assessment period (β = 6.30 (.91), p <.001) and a faster rate of decrease in externalizing problems over time (β = −.33 (.09), p <.001). Although participants with sleep problems had a faster rate of decrease in externalizing problems, further analyses showed that controlling for parental alcoholism, their scores remain higher than participants without sleep problems from ages 3 to 17 (Figure 2). Compared to girls without an alcoholic parent, girls with an alcoholic parent had similar level of externalizing problems at the initial assessment period (β = −3.18 (1.90), p =.10). However, they were more likely to show a slower rate of decrease in externalizing problems (β =.47 (.19), p =.01). There was no relationship between parental alcoholism and the development of externalizing problem in boys (intercept: β = 1.79 (1.12), p =.11; slope: β = −.02 (.11), p =.88).
Figure 2.
Development of externalizing problems
Note: PA = parental alcoholism (0=no and 1=yes); sleep = childhood sleep problems (0=no and 1=yes).
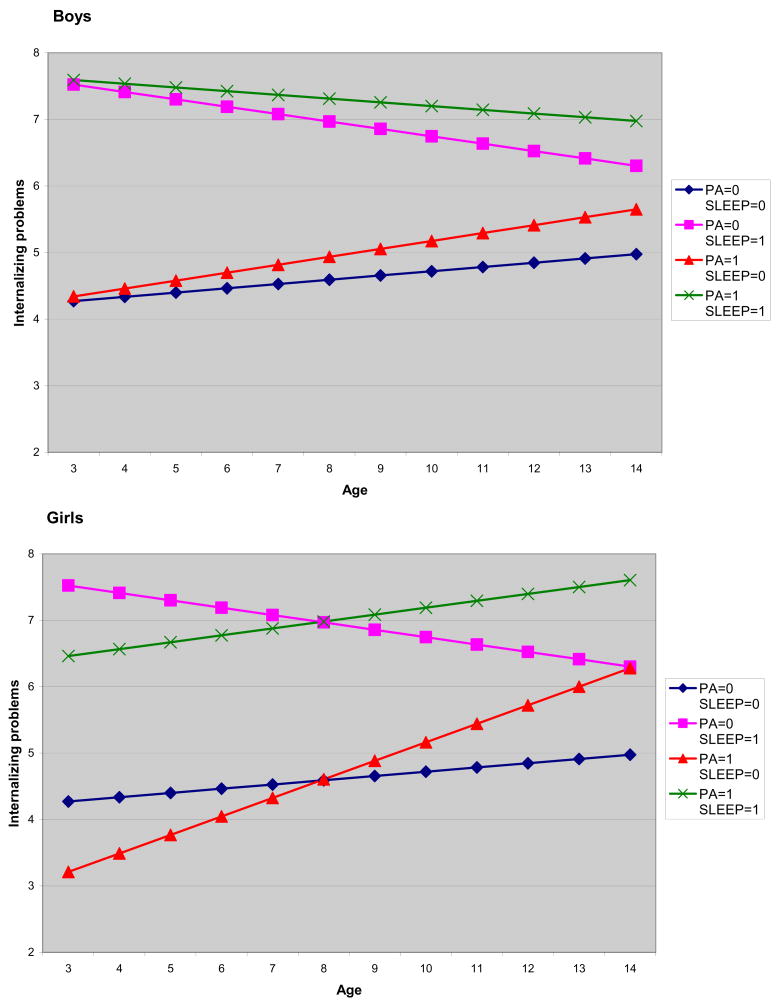
Internalizing problems
Multiple-group analyses indicated that there were no gender differences in either the initial level (χ2 (1) =.37, p =.53) or rate of change in internalizing problems (χ2 (1) =.01, p =.94). For all participants, the average intercept of internalizing problems at the initial assessment period was 4.94 (ûa2 = 4.94 (.32), p <.001, with an increasing linear slope of.07 unit per year (ûβ2 =.07 (.03), p <.05). Among boys, there were significant individual differences in both the initial status ( , p <.001) and the rate of change ( , p <.05). Among girls, there was little variation among girls in the initial status of internalizing problems ( , p =.14). However, there were significant individual differences in the rate of change ( , p <.01).
Controlling for parental alcoholism, there were no gender differences in the effect of sleep problems on the initial status (χ2 (1) =.06, p =.81) and rate of change (χ2 (1) =.45, p =.50) of internalizing problems. Regardless of gender, those with sleep problems have a higher level of internalizing problems in the initial assessment period (β = 3.78 (0.66), p <.001) and a slower rate of increase in internalizing problems over time (β = −.18 (.07), p<.05). Although participants with sleep problems had a slower rate of increase in internalizing problems, further analyses showed that their internalizing problems in adolescence remained higher than participants without sleep problems (Figure 3). Girls with an alcoholic parent had similar level of internalizing problems at the initial assessment period (β = −1.71 (1.01), p =.09) when compared to girls without an alcoholic parent. However, they were more likely to show a faster rate of increase in internalizing problems (β =.22 (.11), p <.05). There was no relationship between parental alcoholism and the development of internalizing problem in boys (intercept: β= −.10 (.76), p =.90; slope: β=.06 (.08), p =.48).
Figure 3.
Development of internalizing problems
Note: PA = parental alcoholism (0=no and 1=yes); sleep = childhood sleep problems (0=no and 1=yes).
3.4 Did controlling for internalizing or externalizing problems reduce the relationship between childhood sleep problems and onset of adolescent substance use?
Analyses in the previous sections showed that childhood sleep problems were related to the developmental trajectories of externalizing and internalizing problems. Controlling for these two problems, would the effect of childhood sleep problems on substance use reduce? We included the growth factors of externalizing and internalizing problems as predictors in the survival analysis models of substance use. As seen in Tables 1–3, there was no indication that internalizing or externalizing problems reduced the effects of sleep problems on substance use. Although a higher initial level of externalizing problems predicted earlier onset of alcohol and cigarette use and a slower rate of decrease in externalizing problems predicted earlier onset of alcohol, cigarette, and marijuana use, including externalizing problems in the analyses did not weaken the relationship between childhood sleep problems and adolescent substance use outcomes. The coefficients for sleep problems remained largely the same (i.e., significant coefficients remain significant), regardless of whether externalizing problems were in the model. Finally, internalizing problems were not related to any of the three substance use outcomes for all participants. Including internalizing problems in the model did not weaken the relationship between sleep problems and substance use.
4. Discussion
This study examined how childhood sleep problems might affect adolescent substance use and behavioral problems. It tested whether controlling for internalizing and externalizing problems would reduce the relationship between childhood sleep problems and adolescent substance use.
Childhood sleep problems appear to be a robust marker for substance use in adolescence for boys but generally are not for girls. Sleep problems significantly increased the risk of early onset of alcohol, cigarette, and marijuana use in boys. However, sleep problems predicted only the risk of onset of alcohol use in girls. To the best of our knowledge, our study was the first to report gender differences on the effects of sleep problems and onset of substance use. More longitudinal studies are necessary to understand whether the findings reported here can be generalized to other populations. Our findings appear to parallel the results of at least two cross-sectional studies [5, 6]. Both studies show that sleep problems have a stronger relationship with substance use among boys than among girls. However, a cautionary note is in order. In the Vignau et al study, sleep disturbances were associated with alcohol inebriation in both boys and girls; among boys only, sleep disturbances were also associated with the use of other drugs. These results seem to be consistent with the findings of the current study. However, in the Tynjala et al study, perceived tiredness was associated with alcohol use and smoking in boys while perceived tiredness was associated with smoking only in girls. More work needs to be done before we know why there are inconsistencies in the results from these studies.
Two important issues need to be addressed in future work. One has to do with possible gender differences in the development of sleep problems from childhood to adolescence. A recent epidemiological study of 1,014 adolescents reported that girls experienced significant changes in sleep habits and patterns subsequent to the onset of menses [8]. Girls were not significantly different from boys in rates of insomnia before onset of menses. However, a significant gender difference emerged after menses onset. Onset of menses was associated with an increase of risk of insomnia. However, physical maturation was not associated with rates of insomnia in boys. If girls’ sleep habits and patterns indeed undergo a great deal of change in adolescence, one must examine the nature of these changes in order to fully understand the relationships between sleep problems and substance use among girls. Future studies could examine how sleep problems develop over time and how those changes may affect the relationship between childhood sleep problems and substance use in the two sexes.
Another issue that remains to be explored is the kind of substances used by those with sleep problems. Previous research [5, 6] and this study indicate a stronger relationship among sleep problems and substance use outcomes for boys than for girls. However, the specific substances used by boys and girls are inconsistent in these studies. Sleep problems could cause physical distress and a decrease in motivation to engage in everyday activities [52], which may result in an increase in stress and negative affect experienced by the individual. Existing data indicate that male social drinkers appear to be more likely than female social drinkers to report using alcohol to cope with distress and negative feelings (see Nolen-Hoeksema [53] for a review). If sleep problems indeed lead to an increase in distress and negative affect, there may be gender differences in the tendency to use different kinds of substances (including alcohol) to cope with sleep problems. The results in this study indicate that such differences exist. Future work could (i) ascertain the robustness of these differences in nationally representative samples with longitudinal data; (ii) systematically examine the factors that may explain such differences. These factors may include peer network [54], availability of substances (e.g., substances offered to the adolescent by peers; alcohol available in the adolescent’s home if adults at home use alcohol; [54]), gender roles [55, 56] as well as drinking motives (e.g., drinking to cope with distress; [53, 57]) and expectancies (e.g., expecting that alcohol will reduce tension; [58, 59]).
Internalizing and externalizing problems have been shown to precede early use of alcohol and other drugs [17–19]. Would controlling for these problems in the analyses change the relationship between sleep problems and onset of substance use? Sleep problems were associated with the developmental trajectories of internalizing and externalizing problems for all participants. However, there was no evidence that the effect of sleep problems on substance use reduced after adjusting for these developmental trajectories. Sleep problems remained a significant predictor of substance use in the presence of externalizing problems or internalizing problems (Tables 1–3).
Internalizing and externalizing problems did not seem to explain the relationship between early sleep problems and onset of substance use. It is important to note that this study used maternal ratings of internalizing and externalizing problems. Sleep problems could result in mild to moderate levels of negative affect and deficits in self-regulation in adolescents that may not be noticeable to parents. Future studies could use other measures of internalizing and externalizing problems. For instance, self-report of these problems in adolescence may better explain the relation between sleep problems and onset of substance use. Additionally, future studies need to consider other neurological, cognitive, or emotional processes that may explain the relationship between childhood sleep problems and adolescent substance use. These processes may include deficits in self-regulation, lower levels of executive functioning, increase in subjective distress, impulsive decision-making and using substances as a sleep aid (see Dahl & Lewin, [52] for a review).
To summarize, childhood sleep problems had a robust relationship with the risk of early substance-use onset in boys. Other studies indicate that early onset of alcohol use is one of the most robust predictors of subsequent alcohol problems in adolescence [60–62] as well as alcohol use disorders in adulthood [63–65]. Moreover, early onset of alcohol and other drugs use is associated with adolescent risky behaviors, such as early sexual intercourse and teenage pregnancy [66–67]. Thus early use of substances may have serious consequences for adolescents.
Our findings provide evidence that the markers of adolescent alcohol and other drug use are detectable very early in the life course. The results indicate that one potential pathway (i.e., sleep to early substance-use onset) can be identified among boys. Substance abuse and dependence are major public health problems. The availability of easily assessed markers of very early risk represents a potentially important public health contribution.
Results of this study may have implications for prevention and intervention work in adolescent substance use. If childhood sleep problems indeed predict early onset of substance use, greater attention by parents to sleep problems in children and adolescents would potentially have ameliorative long-term effects. Parents are encouraged to explore different ways to help their children sleep better, including obtaining information and suggestions from their primary care physicians. For recalcitrant difficulties, a recommendation to seek specialty-level professional help is recommended. Health care providers may want to be aware of the potential serious consequences of childhood sleep problems and provide treatment when sleep disturbances are clinically indicated. Such treatment could include sleep hygiene, behavior therapy, and/or medication.
The current study has several limitations. First, maternal ratings were used as the sole indicator of childhood sleep problems. These ratings may reflect disturbances in the mother-child relationship related to early infant and toddler sleep patterns, rather than to child sleep problems per se. Such disturbances may be shaped by both the characteristics of the mother (e.g., her own alcohol problems, depression, or lack of experience) as well as those of her toddler. Arguing against this, however, is the fact that we controlled for the effect of parental alcoholism (a significant psychopathology) and still observed a positive relationship between sleep problems and substance use.
Second, we have fewer girls than boys in the sample (94 girls, 292 boys). Thus it is essential that the results concerning gender differences be replicated in other longitudinal studies. Third, our analyses did not include any information prior to ages 3 to 5. Data pertaining to prenatal development and sleep-wakefulness information in the first three years of life are necessary for a thorough analysis of sleep problems in early childhood. Fourth, our sample of alcoholic and control families was deliberately selected so that offspring were at the middle-to-high end of the risk for alcohol use disorder continuum. These findings need to be evaluated in other samples at high risk for substance abuse as well as in general population samples. Fifth, our measures of sleep problems were limited to two items and they did not fully capture the spectrum of childhood sleep problems. Overtiredness in childhood may be caused by factors other than sleep problems, such as inadequate nutrition. In addition, the sleep problem indicators we used were maternal ratings. It is therefore important to establish that the observed differences reflect true sleep problems, rather than subjective experience of them. Studies using polysomnographic or actigraphic measures in addition to sleep questionnaires are needed. One such project is currently under way in our own group. We also did not analyze the two sleep items separately. Due to the small sample size, combining both items allow us to have the maximum statistical power to examine the theoretical issues we are interested in. We plan to systematically examine the effect of each sleep item on substance use in future work as more data become available
This study provides preliminary evidence on gender differences in the relationship between early childhood sleep problems and onset of adolescent substance use. Given the public health importance of both sleep and substance-related problems, and given that there may be different risk pathways that link sleep problems to substance use for boys and girls, it is important that the present work be replicated in larger samples of girls and in longitudinal studies where data are collected beyond early adolescence. At the same time, it is possible that the effects of early childhood sleep problems on onset of substance use among girls may not show up until later in development.
Acknowledgments
This work was supported in part by grants from the National Institute on Alcohol Abuse and Alcoholism awarded to R. A. Zucker (R37 AA07065) and K. J. Brower (K24 AA00304) and by a grant from Idaho State University Faculty Research Committee awarded to M. M. Wong. Correspondence concerning this article should be addressed to Maria M. Wong, Department of Psychology, Idaho State University, Pocatello, ID 83209-8112; E-mail: wongmari@isu.edu or to
Contributor Information
Maria M. Wong, Department of Psychology, Idaho State University
Kirk J. Brower, Department of Psychiatry, University of Michigan
Robert A. Zucker, Departments of Psychiatry & Psychology, University of Michigan
References
- 1.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39:411–418. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 2.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbance and psychiatric disorders. Journal of the American Medical Association. 1989;262:1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 3.Weissman MM, Greenwald S, Nino-Murcia G, Dement WC. The morbidity of insomnia uncomplicated by psychiatric disorders. General Hospital Psychiatry. 1997;19:245–250. doi: 10.1016/s0163-8343(97)00056-x. [DOI] [PubMed] [Google Scholar]
- 4.Johnson EO, Breslau N. Sleep problems and substance use in adolescence. Drug and Alcohol Dependence. 2001;64:1–7. doi: 10.1016/s0376-8716(00)00222-2. [DOI] [PubMed] [Google Scholar]
- 5.Tynjala J, Kannas L, Levalahti E. Perceived tiredness among adolescents and its association with sleep habits and use of pyschoactive substances. Journal of Sleep Research. 1997;6:189–198. doi: 10.1046/j.1365-2869.1997.00048.x. [DOI] [PubMed] [Google Scholar]
- 6.Vignau J, Bailly D, Duhamel A, Vervaecke P, Beuscart R, Collinet C. Epidemiologic study of sleep quality and troubles in French secondary school adolescents. Journal of Adolescent Health. 1997;21:343–350. doi: 10.1016/S1054-139X(97)00109-2. [DOI] [PubMed] [Google Scholar]
- 7.Wong MM, Brower KJ, Fitzgerald HE, Zucker RA. Sleep Problems in Early Childhood and Early Onset of Alcohol and Other Drug Use in Adolescence. Alcohol Clin Exp Res. 2004;28:578–587. doi: 10.1097/01.alc.0000121651.75952.39. [DOI] [PubMed] [Google Scholar]
- 8.Johnson EO, Roth T, Schultz L, Breslau N. Epidemiology of DSM-IV insomnia in adolescence: Lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. 2006;117:247–256. doi: 10.1542/peds.2004-2629. [DOI] [PubMed] [Google Scholar]
- 9.Gregory AM, O’Connor TG. Sleep problems in childhood: A longitudinal study of developmental change and association with behavioral problems. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:964–971. doi: 10.1097/00004583-200208000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Gregory AM, Caspi A, Eley TC, Moffitt TE, O’Connor TG, Poulton R. Prospective Longitudinal Associations Between Persistent Sleep Problems in Childhood and Anxiety and Depression Disorders in Adulthood. Journal of Abnormal Child Psychology. 2005;33:157–163. doi: 10.1007/s10802-005-1824-0. [DOI] [PubMed] [Google Scholar]
- 11.Guilleminault C, Korobkin R, Winkle R. A review of 50 children with obstructive sleep apnea syndrome. Lung. 1981;159:275–287. doi: 10.1007/BF02713925. [DOI] [PubMed] [Google Scholar]
- 12.Guilleminault C, Winkle R, Korobkin R, Simmons B. Children and nocturnal snoring: Evaluation of the effects of sleep related respiratory resistive load and daytime functioning. European Journal of Pediatrics. 1982;139:165–171. doi: 10.1007/BF01377349. [DOI] [PubMed] [Google Scholar]
- 13.Chervin RD, Dillon JE, Bassetti C, Ganoczy DA, Pituch KJ. Symptoms of sleep disorders, inattention, and hyperactivity in children. Sleep. 1997;20:1185–1192. doi: 10.1093/sleep/20.12.1185. [DOI] [PubMed] [Google Scholar]
- 14.Chervin RD, Dillon JE, Archbold KH, Ruzicka DL. Conduct problems and symptoms of sleep disorders in children. American Academy of Child and Adolescent Psychiatry. 2003;42:201–208. doi: 10.1097/00004583-200302000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Dahl RE. The regulation of sleep and arousal: Development and psychopathology. Development & Psychopathology. 1996;8:3–27. [Google Scholar]
- 16.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Development. 1998;69:875–887. [PubMed] [Google Scholar]
- 17.Caspi A, Moffit TE, Newman DL, Silva PA. Behavioral observations at age 3 years predict adult psychiatric disorders: Longitudinal evidence from a birth cohort. Archives of General Psychiatry. 1996;53:1033–1039. doi: 10.1001/archpsyc.1996.01830110071009. [DOI] [PubMed] [Google Scholar]
- 18.Chassin L, Pitts SC, DeLucia C, Todd M. A longitudinal study of children of alcoholics: Predicting young adult substance use disorders, anxiety, and depression. Journal of Abnormal Psychology. 1999;108:106–119. doi: 10.1037//0021-843x.108.1.106. [DOI] [PubMed] [Google Scholar]
- 19.Hussong AM, Hicks RE, Levy SA, Curran PJ. Specifying the relations between affect and heavy alcohol use among young adults. Journal of Abnormal Psychology. 2001;110:449–461. doi: 10.1037//0021-843x.110.3.449. [DOI] [PubMed] [Google Scholar]
- 20.Zucker RA. The development of alcohol problems: Exploring the biopsychosocial matrix of risk. Rockville, MD: Department of Health and Human Services; 1994. Pathways to alcohol problems and alcoholism: A developmental account of the evidence for multiple alcoholisms and for contextual contributions to risk; pp. 255–289. Vol. NIAAA Research Monograph 26; NIH Publication No. 94–3495. [Google Scholar]
- 21.Zucker RA, Ellis DA, Bingham CR, Fitzgerald HE. The development of alcoholic subtypes: Risk variation among alcoholic families during early childhood years. Alcohol Health & Research World. 1996;20:46–54. [PMC free article] [PubMed] [Google Scholar]
- 22.Zucker RA, Fitzgerald HE. Early developmental factors and risk for alcohol problems. Alcohol Health and Research World. 1991;15:18–24. [Google Scholar]
- 23.Zucker RA, Fitzgerald HE, Refior SK, Puttler LI, Pallas DM, Ellis DA. The clinical and social ecology of childhood for children of alcoholics: Description of a study and implicatioons for a differentiated social policy. In: Fitzgerald HE, Lester BM, Zuckerman BS, editors. Children of addiction: Research, health, and policy issues. New York: Routledge Falmer; 2000. pp. 109–141. [Google Scholar]
- 24.Zucker RA, Ellis DA, Bingham CR, Fitzgerald HE. The development of alcoholic subtypes: Risk variation among alcoholic families during early childhood. Alcohol Health & Research World. 1996;20:46–54. [PMC free article] [PubMed] [Google Scholar]
- 25.Zucker RA, Fitzgerald HE, Refior SK, Puttler LI, Pallas DM, Ellis DA. The clinical and social ecology of childhood for children of alcoholics: Description of a study and implicatioons for a differentiated social policy. In: Zuckerman BS, editor. Children of addiction: Research, health, and policy issues. New York: Garland Press; 2000. pp. 1–30. [Google Scholar]
- 26.Fitzgerald HE, Sullivan LA, Ham HP, Zucker RA, Bruckel S, Schneider AM. Predictors of behavioral problems in three-year-old sons of alcoholics: Early evidence for onset of risk. Child Development. 1993;64:110–123. doi: 10.1111/j.1467-8624.1993.tb02898.x. [DOI] [PubMed] [Google Scholar]
- 27.Fitzgerald HE, Zucker RA, Yang H-Y. Developmental systems theory and alcoholism: Analyzing patterns of variation in high risk families. Psychology of Addictive Behaviors. 1995;9:8–22. [Google Scholar]
- 28.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 29.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, Correlates, Disability, and Comorbidity of DSM-IV Alcohol Abuse and Dependence in the United States: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 30.Achenbach T. Manual for the child behavior checklist/4–18 and 1991 profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 31.Achenbach T. Burlington, VT: University Associates in Psychiatry; 1991. [Google Scholar]
- 32.Achenbach T, Edelbrock C. Manual for the child behavior checklist and revised child behavior profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1983. [Google Scholar]
- 33.Zucker RA, Fitzgerald HE. Family study of risk for alcoholism over the life course. Appendix 9.3 Assesment protocol: Description of instruments and copies of contact schedules, 2002.
- 34.Shaffer D, Fisher P, Lucas C, Dulcan MK, Schwab-Stone M. NIMH Diagnostic Interview Schedule for Children, Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 35.Selzer ML, Vinokur A, van Rooijen L. A self-administered Short Michigan Alcoholism Screening Test (SMAST) Journal of Studies on Alcohol. 1975;36:117–126. doi: 10.15288/jsa.1975.36.117. [DOI] [PubMed] [Google Scholar]
- 36.Robins LN, Helzer JE, Croughan JL, Ratcliff KS. The NIMH Diagnostic Interview Schedule: Its history, characteristics and validity. St. Louis, MO: Washington University School of Medicine; 1980. [Google Scholar]
- 37.Zucker RA, Fitzgerald HE, Noll RB. Drinking and drug history (rev. ed., version 4) East Lansing, MI: Michigan State University; 1990. Unpublished instrument. [Google Scholar]
- 38.Muthen B, Masyn K. Discrete-time survival mixture analysis. Journal of Educational and Behavioral Statistics. 2005;30:27–58. [Google Scholar]
- 39.Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- 40.Curran PJ. A latent curve framework for the study of developmental trajectories in adolescent substance use. In: Rose JS, Chassin L, Presson CC, Sherman SJ, editors. Multivariate applications in substance use research: New methods for new questions. Mahwah, NJ: Erlbaum; 2000. pp. 43–78. [Google Scholar]
- 41.Meredith W, Tisak J. Latent curve analysis. Psychometrika. 1990;55:107–122. [Google Scholar]
- 42.Muthen B. Analysis of longitudinal data using latent variable models with varying parameters. In: Horn JL, editor. Best methods for the analysis of change. Washington, DC: American Psychological Association; 1991. pp. 1–17. [Google Scholar]
- 43.McArdle JJ, Epstein D. Latent growth curves within developmental structural equation models. Child Development. 1987;58:110–133. [PubMed] [Google Scholar]
- 44.Mehta PD, West SG. Putting the individual back into individual growth curves. Psychol Meth. 2000;5:23–43. doi: 10.1037/1082-989x.5.1.23. [DOI] [PubMed] [Google Scholar]
- 45.Metha PD, West SG. Putting the individual back into individual growth curves. Psychological Methods. 2000;5:23–43. doi: 10.1037/1082-989x.5.1.23. [DOI] [PubMed] [Google Scholar]
- 46.Singer JD, Willet JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. A framework for investigating change over time; pp. 3–15. [Google Scholar]
- 47.Kruger RF, Capsi A, Moffitt TE, Silva PA. The structure and stability of common mental dissorders (DSM-III-R): A longitudinal epidemiological study. Journal of Abnormal Psychology. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 48.Wong MM, Zucker RA, Fitzgerald HE. Developmental trajectories of internalizing and externalizing problems in sons of alcoholics: Effects of parent psychopathology, parent daily negative affect, and child temperament. 2007 Unpublished manuscript. [Google Scholar]
- 49.Muthen BO, Satorra A. Complex sample data in structural equation modeling. Sociological Methodology. 1995;25:267–316. [Google Scholar]
- 50.Muthen B. Methodological issues in randoem coefficient growth modeling using a latent variable framework: Applications to the development of heavy drinking ages 18–37. In: Rose JS, Chassin L, Presson CC, Sherman SJ, editors. Multivariate applications in substance use research: New methods for new questions. Mahwah, NJ: Erlbaum; 2000. [Google Scholar]
- 51.Muthen BO, Muthen LK. Mplus. Los Angeles, CA: Muthen & Muthen; 2006. [Google Scholar]
- 52.Dahl RE, Lewin DS. Pathways to adolescent health: Sleep regulation and behavior. Journal of Adolescent Health. 2002;31(Suppl6):175–184. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- 53.Nolen-Hoeksema S, Harrell ZAT. Rumination, depression, and alcohol use: Tests of gender differences. Journal of Cognitive Psychotherapy: An International Quarterly. 2002;16:391–404. [Google Scholar]
- 54.Zucker RA. Alcohol use and alcohol use disorders: A developmental-biopsychosocial system formulation covering the life course. In: Cicchetti D, Cohen DJ, editors. Developmental psychopathology: Disorder and adaptation. Vol. 3. New York: Wiley; 2006. [Google Scholar]
- 55.Huselid RF, Cooper ML. Gender roles as mediators of sex differences in adolescent alcohol use and abuse. J Health Soc Behav. 1992;33:348–362. [PubMed] [Google Scholar]
- 56.White HR, Huselid RF. Gender differences in alcohol use during adolescence. In: Wilsnack RW, Wilsnack SC, editors. Gender and alcohol: Individual and social perspectives. Piscataway, NJ: Rutgers Center of Alcohol Studies; 1997. pp. 176–198. [Google Scholar]
- 57.Park CL, Levenson MR. Drinking to cope among college students: Prevalence, problems and coping processes. Journal of Studies on Alcohol. 2002;63:486–497. doi: 10.15288/jsa.2002.63.486. [DOI] [PubMed] [Google Scholar]
- 58.Bartholow BD, Sher KJ, Strathman A. Moderation of the expectancy-alcohol use relation by private selfconsciousness: Data from a longitudinal study. Personality and Social Psychology Bulletin. 2000;26:1409–1420. [Google Scholar]
- 59.Cooper ML, Russell M, Frone MR. Work stress and alcohol effects: A test of stress-induced drinking. J Health Soc Behav. 1990;31:260–276. [PubMed] [Google Scholar]
- 60.Ellickson PL, Tucker JS, Klein DJ. Ten-year prospective study of public health problems associated with early drinking. Pediatrics. 2003;111:949–955. doi: 10.1542/peds.111.5.949. [DOI] [PubMed] [Google Scholar]
- 61.Gruber E, DiClemente RJ, Anderson MM, Lodico M. Early drinking onset and its association with alcohol use and problem behavior in late adolescence. Preventive Medicine: An International Journal Devoted to Practice & Theory. 1996;25:293–300. doi: 10.1006/pmed.1996.0059. [DOI] [PubMed] [Google Scholar]
- 62.Hawkins JD, Graham JW, Maguin E, Abbott R, Hill KG, Catalano RF. Exploring the effects of age of alcohol use initiation and psychosocial risk factors on subsequent alcohol misuse. Journal of Studies on Alcohol. 1997;58:280–290. doi: 10.15288/jsa.1997.58.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chou SPRPP. Early onset of drinking as a risk factor for lifetime alcohol-related problems. British Journal of Addiction. 1992;87:1199–1204. doi: 10.1111/j.1360-0443.1992.tb02008.x. [DOI] [PubMed] [Google Scholar]
- 64.DeWit DJ, Adlaf EM, Offord DR, Ogborne AC. Age of first alcohol use: A risk factor for the development of alcohol disorders. American Journal of Psychiatry. 2000;157:745–750. doi: 10.1176/appi.ajp.157.5.745. [DOI] [PubMed] [Google Scholar]
- 65.Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: Results from the National Longitudinal Alcohol Epidemiological Survey. Journal of Substance Abuse. 1997;10:59–73. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- 66.Urdy JR, Campbell BC. Getting started on sexual behavior. In: Rossi AS, editor. Sexuality across the life course. Chicago: University of Chicago Press; 1994. pp. 187–208. [Google Scholar]
- 67.Miller B, Moore K. Adolescent sexual behavior, pregnancy, and parenting: Research through the 1980s. Journal of Marriage and the Family. 1990;52:1025–1044. [Google Scholar]