Abstract
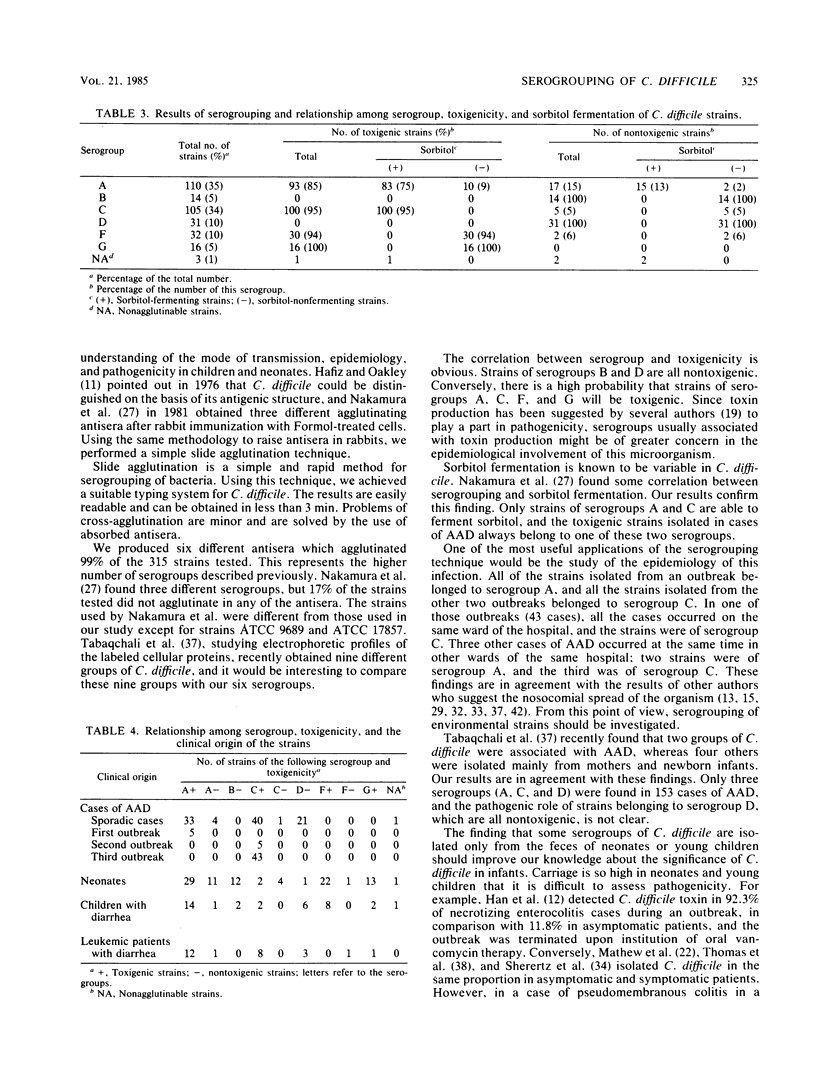
Six different agglutinating antisera were obtained by immunizing rabbits with Formol-treated strains of Clostridium difficile. After appropriate absorption, these antisera were used to define six serogroups designated by the letters A, B, C, D, F, and G. Altogether, 315 strains of C. difficile from various origins were tested for slide agglutination by these antisera; 312 (99%) of them were agglutinated by one of these antisera. A and C were the most common serogroups. An excellent correlation, ranging from 85 to 100%, was found between the serogroup and the toxigenicity of the strains. The correlation between serogroup and sorbitol fermentation was higher, ranging from 89 to 100%. The results of this typing were compared with the clinical origin of the strains. Only strains of serogroups A, C, and D were isolated in 153 cases of antibiotic-associated diarrhea. This series included strains from three outbreaks; all the strains in two of the outbreaks belonged to serogroup C, and in the third, all the strains belonged to serogroup A. Strains of serogroups B, F, and G were only found in the stools of asymptomatic neonates or young children. In the latter samples, strains of serogroups A and D were found in the same ratio as in adults with antibiotic-associated diarrhea, but strains of serogroup C were seldom isolated. In patients treated with antineoplastic drugs and suffering from diarrhea, the distribution of the strains was the same as in cases of antibiotic-associated diarrhea.
Full text
PDF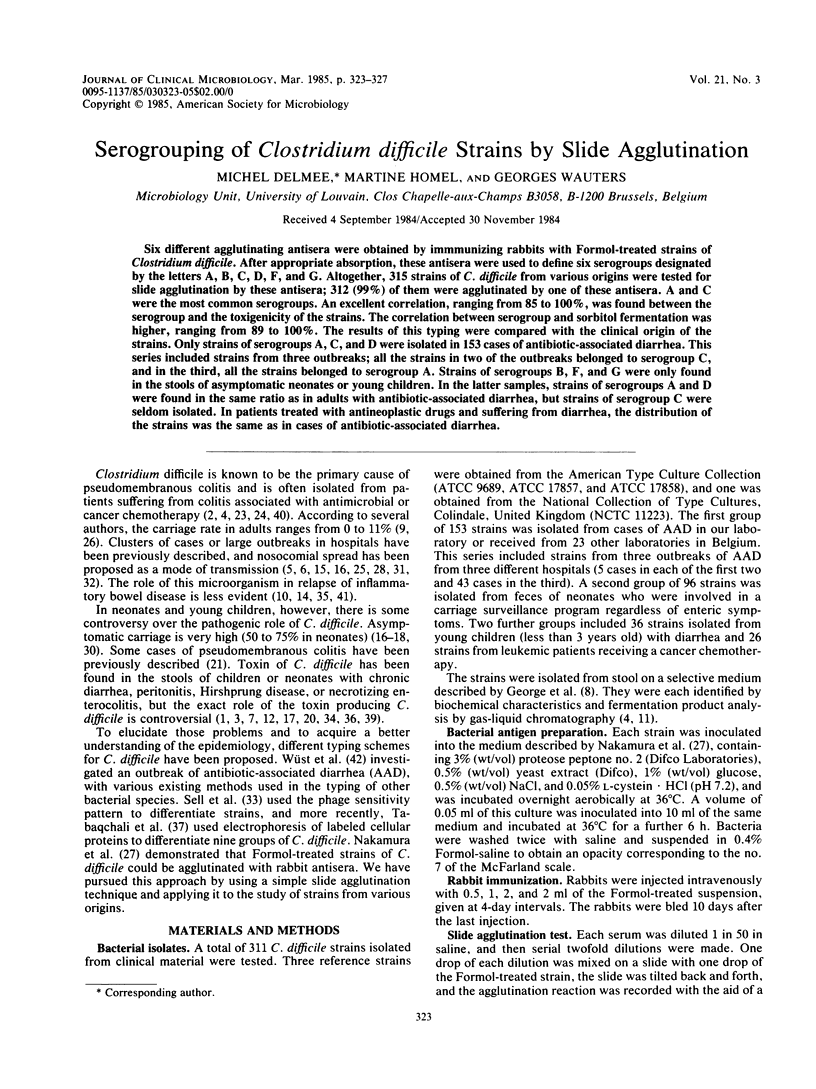

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Al-Jumaili I. J., Shibley M., Lishman A. H., Record C. O. Incidence and origin of Clostridium difficile in neonates. J Clin Microbiol. 1984 Jan;19(1):77–78. doi: 10.1128/jcm.19.1.77-78.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett J. G., Chang T. W., Gurwith M., Gorbach S. L., Onderdonk A. B. Antibiotic-associated pseudomembranous colitis due to toxin-producing clostridia. N Engl J Med. 1978 Mar 9;298(10):531–534. doi: 10.1056/NEJM197803092981003. [DOI] [PubMed] [Google Scholar]
- Cooperstock M. S. Clostridium difficile, enterocolitis, and Hirschsprung's disease. Lancet. 1982 Apr 3;1(8275):800–800. doi: 10.1016/s0140-6736(82)91843-8. [DOI] [PubMed] [Google Scholar]
- Delmée M., Wauters G. Rôle de Clostridium difficile dans les diarrhées survenant après antibiothérapie: étude de 87 cas. Acta Clin Belg. 1981;36(4):178–184. doi: 10.1080/22953337.1981.11718805. [DOI] [PubMed] [Google Scholar]
- Fekety R., Kim K. H., Batts D. H., Browne R. A., Cudmore M. A., Silva J., Jr, Toshniwal R., Wilson K. H. Studies on the epidemiology of antibiotic-associated Clostridium difficile colitis. Am J Clin Nutr. 1980 Nov;33(11 Suppl):2527–2532. doi: 10.1093/ajcn/33.11.2527. [DOI] [PubMed] [Google Scholar]
- Fekety R., Kim K. H., Brown D., Batts D. H., Cudmore M., Silva J., Jr Epidemiology of antibiotic-associated colitis; isolation of Clostridium difficile from the hospital environment. Am J Med. 1981 Apr;70(4):906–908. doi: 10.1016/0002-9343(81)90553-2. [DOI] [PubMed] [Google Scholar]
- Genta V. M., Gilligan P. H., McCarthy L. R. Clostridium difficile peritonitis in a neonate. A case report. Arch Pathol Lab Med. 1984 Jan;108(1):82–83. [PubMed] [Google Scholar]
- George W. L., Sutter V. L., Citron D., Finegold S. M. Selective and differential medium for isolation of Clostridium difficile. J Clin Microbiol. 1979 Feb;9(2):214–219. doi: 10.1128/jcm.9.2.214-219.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield C., Aguilar Ramirez J. R., Pounder R. E., Williams T., Danvers M., Marper S. R., Noone P. Clostridium difficile and inflammatory bowel disease. Gut. 1983 Aug;24(8):713–717. doi: 10.1136/gut.24.8.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hafiz S., Oakley C. L. Clostridium difficile: isolation and characteristics. J Med Microbiol. 1976 May;9(2):129–136. doi: 10.1099/00222615-9-2-129. [DOI] [PubMed] [Google Scholar]
- Han V. K., Sayed H., Chance G. W., Brabyn D. G., Shaheed W. A. An outbreak of Clostridium difficile necrotizing enterocolitis: a case for oral vancomycin therapy? Pediatrics. 1983 Jun;71(6):935–941. [PubMed] [Google Scholar]
- Hawkins C. C., Buggy B. P., Fekety R., Schaberg D. R. Epidemiology of colitis induced by Clostridium difficile in hamsters: application of a bacteriophage and bacteriocin typing system. J Infect Dis. 1984 May;149(5):775–780. doi: 10.1093/infdis/149.5.775. [DOI] [PubMed] [Google Scholar]
- Keighley M. R. Clostridium difficile and inflammatory bowel disease. J Antimicrob Chemother. 1983 Jun;11(6):493–494. doi: 10.1093/jac/11.6.493. [DOI] [PubMed] [Google Scholar]
- Kim K. H., Fekety R., Batts D. H., Brown D., Cudmore M., Silva J., Jr, Waters D. Isolation of Clostridium difficile from the environment and contacts of patients with antibiotic-associated colitis. J Infect Dis. 1981 Jan;143(1):42–50. doi: 10.1093/infdis/143.1.42. [DOI] [PubMed] [Google Scholar]
- Kim K., DuPont H. L., Pickering L. K. Outbreaks of diarrhea associated with Clostridium difficile and its toxin in day-care centers: evidence of person-to-person spread. J Pediatr. 1983 Mar;102(3):376–382. doi: 10.1016/s0022-3476(83)80652-0. [DOI] [PubMed] [Google Scholar]
- Kliegman R. M., Hack M., Jones P., Fanaroff A. A. Epidemiologic study of necrotizing enterocolitis among low-birth-weight infants. Absence of identifiable risk factors. J Pediatr. 1982 Mar;100(3):440–444. doi: 10.1016/s0022-3476(82)80456-3. [DOI] [PubMed] [Google Scholar]
- Larson H. E., Barclay F. E., Honour P., Hill I. D. Epidemiology of Clostridium difficile in infants. J Infect Dis. 1982 Dec;146(6):727–733. doi: 10.1093/infdis/146.6.727. [DOI] [PubMed] [Google Scholar]
- Libby J. M., Jortner B. S., Wilkins T. D. Effects of the two toxins of Clostridium difficile in antibiotic-associated cecitis in hamsters. Infect Immun. 1982 May;36(2):822–829. doi: 10.1128/iai.36.2.822-829.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liston T. E. Clostridium difficile toxin associated with chronic diarrhea and failure to gain weight. Clin Pediatr (Phila) 1983 Jun;22(6):458–460. doi: 10.1177/000992288302200616. [DOI] [PubMed] [Google Scholar]
- Mandal B. K., Watson B., Ellis M. Pseudomembranous colitis in a 5-week-old infant. Br Med J (Clin Res Ed) 1982 Jan 30;284(6312):345–346. doi: 10.1136/bmj.284.6312.345-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathew O. P., Bhatia J. S., Richardson C. J. An outbreak of Clostridium difficile necrotizing enterocolitis. Pediatrics. 1984 Feb;73(2):265–266. [PubMed] [Google Scholar]
- Miller S. D., Koornhof H. J. Clostridium difficile colitis associated with the use of antineoplastic agents. Eur J Clin Microbiol. 1984 Feb;3(1):10–13. doi: 10.1007/BF02032807. [DOI] [PubMed] [Google Scholar]
- Milligan D. W., Kelly J. K. Pseudomembranous colitis in a leukaemia unit: a report of five fatal cases. J Clin Pathol. 1979 Dec;32(12):1237–1243. doi: 10.1136/jcp.32.12.1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura S., Mikawa M., Nakashio S., Takabatake M., Okado I., Yamakawa K., Serikawa T., Okumura S., Nishida S. Isolation of Clostridium difficile from the feces and the antibody in sera of young and elderly adults. Microbiol Immunol. 1981;25(4):345–351. doi: 10.1111/j.1348-0421.1981.tb00036.x. [DOI] [PubMed] [Google Scholar]
- Nakamura S., Serikawa T., Mikawa M., Nakashio S., Yamakawa K., Nishida S. Agglutination, toxigenicity and sorbitol fermentation of Clostridium difficile. Microbiol Immunol. 1981;25(9):863–870. doi: 10.1111/j.1348-0421.1981.tb00091.x. [DOI] [PubMed] [Google Scholar]
- Pierce P. F., Jr, Wilson R., Silva J., Jr, Garagusi V. F., Rifkin G. D., Fekety R., Nunez-Montiel O., Dowell V. R., Jr, Hughes J. M. Antibiotic-associated pseudomembranous colitis: an epidemiologic investigation of a cluster of cases. J Infect Dis. 1982 Feb;145(2):269–274. doi: 10.1093/infdis/145.2.269. [DOI] [PubMed] [Google Scholar]
- Poxton I. R., Aronsson B., Möllby R., Nord C. E., Collee J. G. Immunochemical fingerprinting of Clostridium difficile strains isolated from an outbreak of antibiotic-associated colitis and diarrhoea. J Med Microbiol. 1984 Jun;17(3):317–324. doi: 10.1099/00222615-17-3-317. [DOI] [PubMed] [Google Scholar]
- Richardson S. A., Alcock P. A., Gray J. Clostridium difficile and its toxin in healthy neonates. Br Med J (Clin Res Ed) 1983 Sep 24;287(6396):878–878. doi: 10.1136/bmj.287.6396.878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers T. R., Petrou M., Lucas C., Chung J. T., Barrett A. J., Borriello S. P., Honour P. Spread of Clostridium difficile among patients receiving non-absorbable antibiotics for gut decontamination. Br Med J (Clin Res Ed) 1981 Aug 8;283(6288):408–409. doi: 10.1136/bmj.283.6288.408-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage A. M., Alford R. H. Nosocomial spread of Clostridium difficile. Infect Control. 1983 Jan-Feb;4(1):31–33. doi: 10.1017/s0195941700057623. [DOI] [PubMed] [Google Scholar]
- Sell T. L., Schaberg D. R., Fekety F. R. Bacteriophage and bacteriocin typing scheme for Clostridium difficile. J Clin Microbiol. 1983 Jun;17(6):1148–1152. doi: 10.1128/jcm.17.6.1148-1152.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherertz R. J., Sarubbi F. A. The prevalence of Clostridium difficile and toxin in a nursery population: a comparison between patients with necrotizing enterocolitis and an asymptomatic group. J Pediatr. 1982 Mar;100(3):435–439. doi: 10.1016/s0022-3476(82)80455-1. [DOI] [PubMed] [Google Scholar]
- Sutphen J. L., Grand R. J., Flores A., Chang T. W., Bartlett J. G. Chronic diarrhea associated with Clostridium difficile in children. Am J Dis Child. 1983 Mar;137(3):275–278. doi: 10.1001/archpedi.1983.02140290061016. [DOI] [PubMed] [Google Scholar]
- Tabaqchali S., Holland D., O'Farrell S., Silman R. Typing scheme for Clostridium difficile: its application in clinical and epidemiological studies. Lancet. 1984 Apr 28;1(8383):935–938. doi: 10.1016/s0140-6736(84)92392-4. [DOI] [PubMed] [Google Scholar]
- Thomas D. F., Fernie D. S., Bayston R., Spitz L. Clostridial toxins in neonatal necrotising enterocolitis. Arch Dis Child. 1984 Mar;59(3):270–272. doi: 10.1136/adc.59.3.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch D. F., Marks M. I. Is Clostridium difficile pathogenic in infants? J Pediatr. 1982 Mar;100(3):393–395. doi: 10.1016/s0022-3476(82)80436-8. [DOI] [PubMed] [Google Scholar]
- Willey S. H., Bartlett J. G. Cultures for Clostridium difficile in stools containing a cytotoxin neutralized by Clostridium sordellii antitoxin. J Clin Microbiol. 1979 Dec;10(6):880–884. doi: 10.1128/jcm.10.6.880-884.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu A. Spontaneous persistent pseudomembranous colitis related to Clostridium difficile in ischaemic bowel disease. Br Med J (Clin Res Ed) 1982 May 29;284(6329):1606–1607. doi: 10.1136/bmj.284.6329.1606-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wüst J., Sullivan N. M., Hardegger U., Wilkins T. D. Investigation of an outbreak of antibiotic-associated colitis by various typing methods. J Clin Microbiol. 1982 Dec;16(6):1096–1101. doi: 10.1128/jcm.16.6.1096-1101.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]


