Abstract
Liver-related autoantibodies are crucial for the correct diagnosis and classification of autoimmune liver diseases (AiLD), namely autoimmune hepatitis types 1 and 2 (AIH-1 and 2), primary biliary cirrhosis (PBC), and the sclerosing cholangitis variants in adults and children. AIH-1 is specified by anti-nuclear antibody (ANA) and smooth muscle antibody (SMA). AIH-2 is specified by antibody to liver kidney microsomal antigen type-1 (anti-LKM1) and anti-liver cytosol type 1 (anti-LC1). SMA, ANA and anti-LKM antibodies can be present in de-novo AIH following liver transplantation. PBC is specified by antimitochondrial antibodies (AMA) reacting with enzymes of the 2-oxo-acid dehydrogenase complexes (chiefly pyruvate dehydrogenase complex E2 subunit) and disease-specific ANA mainly reacting with nuclear pore gp210 and nuclear body sp100. Sclerosing cholangitis presents as at least two variants, first the classical primary sclerosing cholangitis (PSC) mostly affecting adult men wherein the only (and non-specific) reactivity is an atypical perinuclear antineutrophil cytoplasmic antibody (p-ANCA), also termed perinuclear anti-neutrophil nuclear antibodies (p-ANNA) and second the childhood disease called autoimmune sclerosing cholangitis (ASC) with serological features resembling those of type 1 AIH. Liver diagnostic serology is a fast-expanding area of investigation as new purified and recombinant autoantigens, and automated technologies such as ELISAs and bead assays, become available to complement (or even compete with) traditional immunofluorescence procedures. We survey for the first time global trends in quality assurance impacting as it does on (1) manufacturers/purveyors of kits and reagents, (2) diagnostic service laboratories that fulfill clinicians’ requirements, and (3) the end-user, the physician providing patient care, who must properly interpret test results in the overall clinical context.
Keywords: Autoantigen, Autoimmune hepatitis, Autoantibody, Primary biliary cirrhosis, Primary sclerosing cholangitis, Liver disease
INTRODUCTION
The presence of autoantibodies plays a central role in the diagnosis and classification of autoimmune liver diseases (AiLD)[1,2], but their nature and significance remain challenging in regard to pathogenesis. Such antibodies discriminate between distinct subtypes of the AiLD and facilitate diagnosis of the overlap syndromes[3]. AiLD represent a broad range of disorders that can affect one or the other of the two cellular components, namely hepatocytes in autoimmune hepatitis (AIH), and cholangiocytes in primary biliary cirrhosis (PBC), primary sclerosing cholangitis (PSC) and the autoimmune hepatitis/sclerosing cholangitis overlap syndrome of childhood, designated as autoimmune sclerosing cholangitis (ASC)[4], and discussed elsewhere in this issue.
Antibody to nuclei (ANA) and/or to smooth muscle (SMA) characterizes type 1 AIH (AIH-1) and antibody to a liver kidney microsomal constituent (anti-LKM) defines patients with type 2 AIH (AIH-2)[5]. Usually the two patterns of serology are mutually exclusive, but in the rare cases in which they coexist, the disease features resemble those of AIH-2[6]. ASC is a third form of AiLD which is similar clinically, histologically and serologically to AIH-1, but is associated with radiological changes of sclerosing cholangitis[7]. SMA, ANA and to a lesser extent anti-LKM can be found in post-transplantation de novo AIH[8]. The presence of anti-mitochondrial antibodies (AMA) with a specificity for the E2 subunit of the pyruvate complex (PDC-E2), and certain PBC-specific ANA, characterise PBC[1,9]. Perinuclear anti-neutrophil cytoplasmic antibody (p-ANCA) is the most frequent antibody reactivity in primary sclerosing cholangitis (PSC)[1,3], but per se has low specificity for diagnosis.
HISTORICAL NOTES ON AUTOIMMUNE LIVER SEROLOGY
The evolution of knowledge on AIH is discussed in another article in this issue. Here we provide a brief historical survey of the serological tests currently used by diagnostic laboratories.
Anti-nuclear antibody (ANA)
Serum antibodies with specificity for cell nuclear antigens were first described by Miescher et al in 1954[10] following the discovery of the lupus erythematosus (LE) cell by Hargraves and colleagues[11] and the recognition that the LE cell phenomenon was related to a serum factor reacting with nuclear antigens, subsequently termed “antinuclear factor” (ANF), and later antinuclear antibody (ANA). Deoxyribonucleic acid (DNA) and deoxyribonucleoprotein (DNAP) were identified in 1957 as “ANF” target antigens[11,12] and it was further shown that antibodies responsible for the LE-cell phenomenon reacted with DNA and gave a “homogenous” pattern of nuclear staining by immunofluorescence[13]. In 1956 a positive test for LE cells in blood was reported in young women with a chronic liver disease then called chronic active hepatitis (CAH), leading to the designation of “lupoid hepatitis”, an early label for what is now known as AIH-1[14,15]. Testing for ANF/ANA by immunofluorescence (IFL) supplanted the cumbersome LE cell test in the early 1960s.
Smooth-muscle autoantibody (SMA)
Antibodies binding to smooth muscle of rat stomach were initially detected in serum samples of patients with liver diseases by Johnson et al, in 1965[16]. The presence of SMA in patients with AiLD was confirmed by Whittingham et al[17]. Patients with non-AiLDs were reported as seronegative for SMA and, notably, also negative were patients with SLE. The antibody was often found in association with ANA, which was already a known marker of AIH, and tended to fade with steroid induced remission. Bottazzo et al[18] reported that the SMA staining arterial vessels (V), glomerular mesangium (G) and fibers surrounding the kidney tubules (T), responsible for the VGT pattern, was confined to an aggressive form of hepatitis now known to be AIH-1. The antigenic moiety mainly but not exclusively responsible for SMA activity in what in the 1970s was called CAH was identified as filamentous (F) actin[19–21].
Liver kidney microsomal antibody (anti-LKM)
Cytoplasmic antibodies in “CAH” were described in the laboratory of Deborah Doniach[22,23] whose group first used the expression anti-liver kidney microsomal (anti-LKM) antibodies[24]. “Microsomal” is something of a misnomer as “microsomes” are the in vitro equivalent of particles of the endoplasmic reticulum wherein the antigen is located. Other nosological entities in which anti-microsomal antibodies were evident included drug induced hepatitis, leading to the use of LKM1, LKM2, LKM3 to designate the different immunofluorescent patterns, which reflect the different targeted autoantigens[25]. The ability of anti-LKM1 antibodies to define a second serological type of AIH, i.e. AIH type 2, was proposed by Homberg et al[26]. Three groups independently identified cytochrome P450 IID6 (CYP2D6) as the molecular target of anti-LKM1 antibodies[27–29]; the group of Alvarez[27] was the first to publish its data in the form of a full-length paper.
As mentioned, other LKM antibody patterns were subsequently described. LKM2 antibodies were recognised in patients with hepatitis induced by tienilic acid[24], a uricosuric diuretic withdrawn from clinical use in 1980 and Rizzetto’s group described LKM3 antibodies in a proportion of cases of chronic hepatitis D infected patients[30]. In contrast to anti-LKM1 and LKM2 antibodies, anti-LKM3 stained human exocrine pancreas and thyroid. Anti-LKM2 reacted with CYP2C9 and anti-LKM3 with uridine diphosphate glucuronosyl transferases (UGT)[25]. A fourth type of LKM antibodies recognising CYP1A2 and CYP2A6 has been described in patients with AIH associated with autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED)[31]. The IFL pattern of the antibody is indistinguishable from that of anti-LKM1. An anti-liver microsomal antibody (anti-LM) staining the centrolobular hepatocytes but not the kidney and which recognises CYP1A2 has been described in dihydralazine-induced hepatitis and in a few cases of AIH[32–34].
Liver cytosol antibody (anti-LC1)
Anti-LC1 were originally described in association with anti-LKM1, or in isolation, by Martini et al in patients with AIH-2[35]. Lenzi et al have also found anti-LC1 antibodies in 14% anti-LKM-1 antibody positive patients suffering from chronic hepatitis C virus infection[36]. The enzyme formiminotransferase cyclodeaminase (FTCD) has been identified as the molecular target of anti-LC1 antibodies[37,38].
Mitochondrial antibody (AMA)
The first indication that PBC could be an autoimmune disease was obtained in 1958 when the serum of a woman with PBC was found to contain high titres of complement-fixing antibodies directed to tissue homogenates[39], that later, by absorption studies, were shown to be absorbed by a rat liver mitochondrial fraction[40]. A breakthrough for the clinical hepatologist was the observation in 1965 by Walker, Doniach, Roitt and Sherlock that human tissue sections rich in mitochondria give a characteristic immunofluorescence pattern when they are incubated with sera from patients with PBC but not with controls which, in that study, included patients with extra-hepatic bile duct obstruction, drug induced cholestasis and viral hepatitis[41]. In 1967, Berg et al[42] demonstrated that PBC sera reacted in vitro with a trypsin-sensitive mitochondrial antigen that was named M2 antigen, in contrast to M1, the target of anti-cardiolipin antibody. Subsequently Berg developed a nomenclature based on the types of anti-mitochondrial reactivity that spanned M3-M9, but this is no longer used. The M2 antigen was located at the inner surface of the inner mitochondrial membrane of all mitochondria tested[42–45]. The target antigens of M2 were identified in the 1980s as components of the 2-oxo-acid dehydrogenase complexes, the predominant target being the E2 subunit of pyruvate dehydrogenase complex, as judged by molecular cloning[46,47]. PBC-specific AMA were later shown to recognise other enzymes of the 2-OADC, including the E2 subunits of branched chain oxoacid dehydrogenase complex (BCOADC), the oxoglutarate dehydrogenase complex (OGDC) and the PDC-E3 binding protein[1,48].
Antibodies against soluble liver antigen/liver-pancreas antigen
Two autoantibodies, anti-soluble liver antigen (SLA) and anti-liver-pancreas (LP), both described in AIH by two independent German groups, have been shown to target the same antigen, hence the current name of anti-SLA/LP antibodies[49–51]. The LP antigen has first been reported by Berg’s group in the supernatant of liver and pancreas homogenates[50]. The SLA antigen was described by Manns and colleagues in 1987 as a component of the supernatant of liver and kidney homogenates[49]. Anti-SLA antibodies detected by a competitive ELISA were then proposed as markers of a third type of severe AIH seronegative for the conventional AIH-1 autoantibodies[49].
Anti-asialoglycoprotein receptor antibodies
Attempts to identify antigens specifically expressed on the hepatocyte surface which could serve as self targets in AiLD have led to the description of a crude liver extract preparation known as the liver specific protein (LSP) and its major component, the asialoglycoprotein receptor (ASGPR)[52,53]. ASGPR, also designated as hepatic lectin, is a type II transmembrane glycoprotein. It is the only known liver-specific autoantigen, and is constitutively expressed on the hepatocellular membrane.
RECOMMENDATIONS FOR AUTOANTIBODY DETECTION BY IMMUNOFLUORESCENCE (IFL)
IFL is the main technique for the screening of autoantibodies diagnostically relevant to liver disease. The methodology is practically unchanged from that introduced by Weller and Coons in 1954[54]. It uses unfixed, air-dried, tissue sections which are incubated with a test serum potentially containing an antibody. After removing unbound serum by washing, a fluorochrome labelled second antibody, raised in animal and specific for human immunoglobulins, is applied to detect the first tissue-bound antibody[55]. Specific patterns can then be recognised using an ultraviolet microscope. A consensus statement in 2004 from the Committee for Autoimmune Serology of the International Autoimmune Hepatitis Group (IAIHG) provided guidelines on how to test for autoantibodies relevant to AIH and concluded that indirect IFL on fresh sections of multi-organ (liver, kidney, stomach) from rodents (usually rat) should be the first line screening[55]. The recommendations of the Committee include detailed guidelines for the preparation of substrate, application of the test serum samples, optimal dilution of samples and fluorochrome-labelled revealing agents, selection of controls and identification of diagnostically relevant staining patterns[55]. The use of the three tissues enables the simultaneous detection of virtually all the autoantibodies relevant to liver disease, namely SMA, ANA, anti-LKM1, AMA and anti-LC1[55]. The first serum dilution recommended for autoantibody detection (before titration) is for adults 1:40, and for children 1:20 for ANA and SMA and 1:10 for anti-LKM1 in children[55].
Autoantibodies detected by IFL and their reactants
ANA: This autoantibody is readily detectable as nuclear staining in all the three tissues of the composite substrate. On the liver it is also possible to identify different patterns, the homogenous being typical of AIH-1[55]. A clearer definition of the different ANA patterns seen in PBC is best achieved by the use of the human larynx epithelioma cancer cell line (HEp-2) because these cells have large nuclei, and the mitotic phase of these cells permits the easy detection of anti-centromere antibodies (ACA) because they stain the chromosomes of cells in mitosis[56,57]. HEp-2 permit ready detection of the IFL patterns called multiple nuclear dot (MND) and rim-like membranous (RLM) typical of PBC[58,59]. Anti-MND stains 5-20 dots of variable size, distributed all over the nucleus but sparing the nucleoli[58]. The pattern can be confused with that of ACA but anti-MND do not stain the chromosomes of cells in mitosis whereas ACA do so[58]. Moreover, the dots of ACA are all of the same size while those of MND vary in size and number between individual cells[58]. In addition to homogenous ANA, speckled and nucleolar patterns are seen in AIH, and to a lesser extent in PBC, but are not disease-specific.
SMA: SMA of the VGT pattern is considered specific for AIH-1, though some 20%-40% of patients with AIH-1 do not have it[55]. SMA can also be detected, always by IFL, using fibroblasts or HEp-2 cells. The VGT pattern corresponds to the microfilament staining of isolated fibroblasts and represents a cable pattern across the cell[18]. Both patterns have been termed “anti-actin” though there is no molecular proof as yet that actin is indeed the only or indeed the main target of VGT SMA.
Anti-LKM1: Anti-LKM1 brightly stains the third portion of the proximal renal tubules and the cytoplasm of the hepatocytes but it spares cells of the gastric mucosa[55]. Anti-LKM1 is a frequently undiagnosed autoantibody, being commonly misinterpreted as AMA[1,60]. AMA is extremely rare in pediatric patients and PBC is extremely rare in childhood[61,62]. So, when AMA is reported in a child with clinical and histological characteristics of AIH, the serological report is almost certainly incorrect.
AMA: The confusion between AMA and anti-LKM1 occurs because both autoantibodies stain the renal tubules, though with a pattern different to a trained eye and readily appreciated when the kidney tissue section contains both distal and proximal tubules (Figure 1). AMA stains strongly the mitochondria-rich distal tubules which are smaller than the proximal tubules stained by anti-LKM1 antibodies. AMA also stains the gastric parietal cells within the stomach, which are spared by anti LKM1, whereas AMA stains hepatocytes much less brightly than does anti-LKM1. The analysis therefore of the three-tissue substrate should allow a correct serological interpretation. Some serodiagnosticians claim a utility of HEp-2 cells for recognition of AMA which gives a “string of pearls” pattern of cytoplasmic staining. Unfortunately interpretative problems are still frequent especially in those laboratories where only kidney is used as substrate, and particularly when the tissue is poorly oriented. Advice on how to orient and cut the kidney has been issued by the Autoimmune Serology Committee of IAIHG[55].
Figure 1.
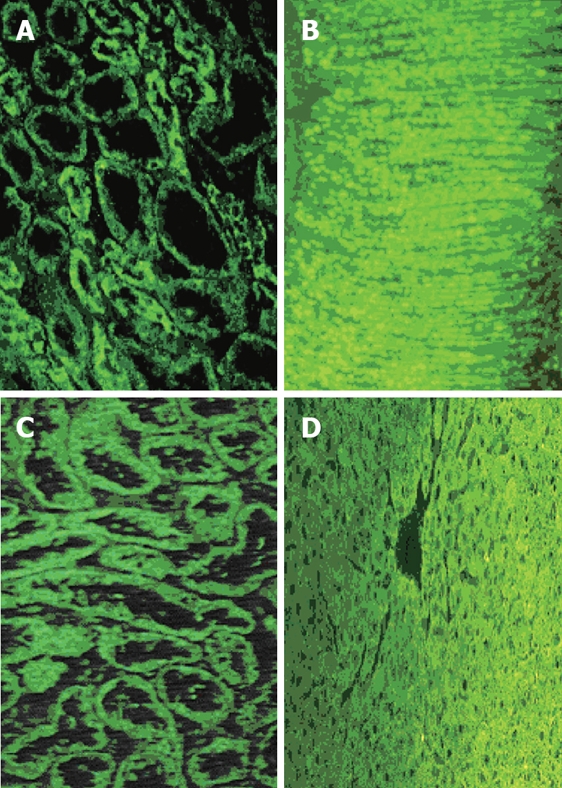
Immunofluorescence of anti-mitochondrial (A and B), and anti-liver kidney microsomal antibody (anti-LKM1) (C and D). AMA stain (A) stronger the smaller, distal tubules while anti-LKM1 the proximal tubules of the rat kidney (C). These specificities are frequently misdiagnosed, especially when only the kidney substrate is used and the sections do not contain both proximal and distal tubules. Thus, the use of rat stomach (B) and liver (D) is strongly recommended to prevent misinterpretation; AMA characteristically stain the gastric parietal cells while anti-LKM1 stain the rat liver but not the stomach.
Anti-LC1: This antibody stains the cytoplasm of hepatocytes with a zonal distribution within the liver, being particularly abundant on perivenous hepatocytes and the renal tubules. In most cases, however, anti-LC1 is obscured by the simultaneous presence of anti-LKM1[35,36]. Anti-LC1 can be also detected by gel diffusion techniques such as double dimension immunodiffusion and counter immunoelectrophoresis, techniques in which the cytosol of liver homogenate is used as antigen and the test serum is run with a positive control[63].
ANCA: ANCA is detected by indirect IFL using neutrophils as substrate and can give a cytoplasmic (c-ANCA) or perinuclear (p-ANCA) pattern[64,65]. The pattern of p-ANCA is an artifact caused by the ethanol fixation of the neutrophils which leads to the migration of some positively charged cytoplasmic antigens to the negatively charged nuclear envelope, so giving the characteristic perinuclear fluorescence staining. An atypical p-ANCA staining, unaffected by ethanol fixation, gives a perinuclear staining subtly different from the classical p-ANCA. It recognizes components of the nuclear envelope and has been described, especially in patients with PSC[66]. In view of the location of the antigen, some groups are now describing these antibodies as perinuclear anti-neutrophil nuclear antibodies (p-ANNA)[67,68].
AUTOANTIGENS OF LIVER-RELATED AUTOANTIBODIES
Nuclear antigens
No single AIH-1-specific nuclear antigen has been identified so far. A number of nuclear molecular targets has been detected, including centromere, histones, double-stranded DNA, chromatin, and ribonucleoprotein complexes with no single pattern or combination thereof being characteristic of AIH[3], although most typical is a homogenous pattern attributable to anti-chromatin.
Smooth muscle antigens
SMA giving the “anti-actin” IFL pattern has long been considered highly diagnostic for AIH type 1, its target deemed to be F-actin (noting that purified actin is a monomer G-actin, which is polymerized in the presence of ATP)[3,20,55,69]. The advent of commercial kits using highly purified F-actin as target has provided the opportunity both to test the molecular specificity of the SMA giving the IFL actin pattern and to assess the diagnostic performance of antibodies directed to molecularly pure F-actin (anti-FA)[70–75]. In Granito and Villalta’s studies, the IFL anti-actin pattern was strongly associated with AIH-1 and so was anti-FA, this latter being marginally more sensitive[70,74,75]. When disease specificity of the two reactivities was analysed the IFL pattern was found to be highly specific, being absent or extremely rare in diseases other than AIH-1. In sharp contrast, anti-FA was detectable in patients with viral hepatitis, PBC, primary sclerosing cholangitis, AIH-2 and celiac disease[70,74,75]. In a paper by Frenzler, positivity for anti-FA was found in some 75% of patients subsequently diagnosed as having AIH-1 but also in 24% non-AIH patients[71]. In an attempt to address the relatively high non-specificity of the molecular assay, Villalta et al performed a receiver operating curve (ROC) analysis, from which they deduced for this assay a cut off point giving a specificity similar to IFL: the cut off point had to be increased from the 30 arbitrary units (AU) suggested by the manufacturer to 53 AU[75]. At this cut-off point the specificity of the molecular assay was indeed comparable to that of IFL, but the sensitivity dropped by more than 10% below that of IFL.
The results obtained with the IFL and molecular assays overlap considerably, but by no means completely, with several instances of positivity with one test and not with the other[72,73,75]. With the availability of highly purified F-actin the question as to whether the antibody responsible for the anti-actin IFL pattern is directed against actin could be tested directly[70–75]. Three anti-SMA positive sera containing both reactivities were absorbed with solid phase F-actin: the reactivity against F-actin was abolished (absorbed out) but that giving the fluorescent pattern was unaltered in two of the 3 sera and reduced, but not abolished, in the third[72]. In summary, detection of the IFL anti-actin pattern continues to provide to date the best specificity/sensitivity compromise[55]. The antibody responsible for the IFL “actin” pattern targets, in addition to actin, molecules other than actin[3,72]. The question arises as to whether to maintain the tradition, and with it the term of “anti-actin” for the antibody recognised in IFL, or whether to call it anti-micro filament (MF) pattern as suggested by the Serology committee of the IAIHG[55].
LKM1 antigen
While the target antigens of ANA and SMA certainly need better molecular definition, that of anti-LKM1 in AIH-2 has been clearly identified as the microsomal enzyme cytochrome P450IID6 (CYP2D6)[5,26–28]. Its identification has enabled the establishment of assays based on the use of recombinant antigens which have proven useful in solving diagnostic uncertainties between AMA and anti-LKM1[1,60,76]. Such ELISAs, however, are not always able to detect anti-LKM1 antibodies in patients with chronic hepatitis C virus infection whereas IFL and radioligand assays can do so possibly because of their ability to identify conformational epitopes undetectable by ELISA[77–80]. Short CYP2D6 peptides used as antigenic preparations perform less well than those using full-length CYP2D6 and their diagnostic use is limited.
LC1 antigen
ELISAs for detection of antibodies to FTCD, the target of anti-LC1, have been developed and used in diagnostic laboratories and their diagnostic and clinical relevance is under investigation[37,38].
SLA/LP and ASGPR
Progress has been made in the definition of other autoantibodies frequently present in AIH but undetectable by IFL including antibodies against SLA/LP[51,81–85] and ASGPR. Most of anti-SLA/LP positive patients are also positive for ANA, SMA or anti-LKM1, but occasionally anti-SLA is present in isolation and, in this case, its detection is of diagnostic importance[81,86]. The identification of the molecular target of anti-SLA/LP antibodies as the UGA serine tRNA-associated protein has led to the development of ELISA or dot-blot assays increasingly replacing the conventional inhibition ELISA originally used for anti-SLA antibody detection[51,83]. Recent studies investigating the exact role of this protein have shown that SLA/LP is a selenocysteine synthase but how the biosynthesis of selenocysteine may relate to the pathogenesis of AIH is not known[87].
Anti-ASGPR antibody detection requires either purified or recombinant antigen. The lack of disease-specificity and the difficulty in developing a reliable molecular based assay for the detection of anti-ASGPR has limited its wider applicability in diagnostic practice.
Mitochondrial antigens
The most recent advance in the immunodiagnosis of AMA is the availability of an ELISA using the triple MIT3 hybrid antigen preparation, developed in the Gershwin laboratory. This preparation contains all three immunodominant mitochondrial antigenic epitopes, namely PDC-E2, BCOADC-E2 and OGDC-E2[88]. Although assays based on MIT3 are reported to give positive results for PBC sera that test negative for AMA by conventional IFL techniques[89,90], IFL testing for AMA should remain the screening procedure.
PBC-specific nuclear antigens
As mentioned above, major target antigens of PBC-specific ANA have been identified. These include the nuclear body speckled 100 kDa (sp100), promyelocytic leukaemia (PML), and small ubiquitin-like modifier (SUMO) proteins corresponding to the MND pattern, and proteins within the nuclear pore complex (anti-NPC) including the 210 kDa glycoprotein (gp210) and the 62 kDa nucleoporin (NUP62), the major target antigens of anti-RLM antibodies and responsible for the RLM pattern[58,59,91]. New immunoassays testing autoantibodies to sp100, PML, gp210 and NUP62 have been developed using short peptides, polypeptides or full-length proteins as targets, but they have not been fully evaluated nor standardized[91–98]. They may be of diagnostic assistance, especially in those cases where it is difficult to interpret the IFL staining patterns due to concurrent autoantibody reactivities or in true AMA-negative PBC cases[1,92,99,100]. We note also the presence of ACA reactivity in the combined PBC/CREST disease. Assays to detect multiple reactivities (multiplex) and to provide a full autoimmune serological profile of relevance to PBC are being developed[89]. At present, a lack of guidelines for the detection of PBC-specific autoantibodies by scientific bodies responsible for the standardization of autoimmune serological tests is a significant handicap and perpetuates uncertainties on which are the clinically relevant tests (see below).
Atypical p-ANCA (pANNA) antigens
These are under current investigation[66–68]. The original description of a 50 kDa neutrophil-specific nuclear protein of the nuclear pore complex as the target antigen recognised by 90% of atypical p-ANCA from patients with PSC was followed by a study from the same group suggesting that the identity of the antigen is tubulin beta chain 5 (TBB5)[101]. However, when using the molecular target for their detection anti-TTB5 antibodies were found not only in PSC but also in other AiLDs.
DIAGNOSTIC RELEVANCE OF LIVER-RELATED AUTOANTIBODIES
ANA, SMA, anti-LKM1, AMA and p-ANCA should be determined in all patients with biochemical, clinical and/or histological features suggestive of AiLD[3,5]. Autoantibody titres usually vary during the course of the disease. Hence seronegativity or low autoantibody titres on a single test cannot exclude the diagnosis of AiLD and repeat tests may allow autoantibody detection and correct disease classification. Conversely, the presence of autoantibodies even at high titres in the absence of any other clinical and laboratory features suggestive of AiLD is insufficient to make a diagnosis though a patient with high titre autoantibodies needs to be seen at regular intervals. Titres of ANA, SMA and LKM1 antibodies contribute in calculating the IAIHG diagnostic score for patients with a probable or definite diagnosis of AIH[5]. IFL titres of > 1:80 attract a +3 score; 1:80 a +2 score and 1:40 +1 score. A negative score of -4 is given to cases with hepatitic features but detectable AMA at a titre of ≥ 1:40; such mixed serology points to “overlap syndrome”, discussed in another article in this issue. In children, titres of 1:20 for ANA or SMA and 1:10 for anti-LKM1 are sufficient to support the diagnosis of AIH if accompanied by other suggestive features[5,55].
In AIH-1, ANA alone are present in 15% of patients, SMA alone in 35%, and ANA and SMA co-occur in 60%[3]. In the 5% or so of cases negative for these reactivities, anti-SLA/LP may be positive. In AIH-2 at presentation anti-LKM1 and/or anti-LC1 antibodies are positive in more than 90% of patients[25,35,36,63]. In PBC, AMA are detectable in more than 95% of patients and disease-specific ANA occur in 30%-70% of PBC patients according to different reports[9,58,59,100]. In PSC, atypical p-ANCA are present in up to 90% of patients but this reactivity also occurs in AIH (up to 70%) and PBC (5%), as well as frequently in patients with inflammatory bowel disease[66–68,102,103]. In what is termed “de novo” AIH and in post-liver transplant patients, ANA, SMA, AMA and anti-LKM have been reported, at varying frequencies[85,94]. A diagnosis of AIH-2 is strongly supported by seropositivity for anti-LKM1 and/or anti-LC1, particularly in the absence of viral hepatitis C[5]. For PBC, the presence of AMA is one of the three widely accepted diagnostic criteria[9].
Autoantibody positivity is part of the criteria used for the diagnosis of AiLD, though it is not diagnostic on its own. Elevated titres and certain patterns carry significant diagnostic connotations.
We are aware of various reports that, at first sight, might appear prejudicial to the diagnostic utility of liver-related autoantibodies[104]. Thus ANA and/or SMA are reported in PBC, PSC, de novo AIH, chronic viral hepatitides B, C and D, acute liver failure, drug-induced hepatitis, non-alcoholic steatohepatitis, alcohol-induced liver disease, hepatocellular carcinoma, and also in a variety of non-liver related diseases. Hence, the diagnostic significance of antibody positivity depends on the associated clinical features[3], as well as the level of reactivity. Anti-LKM1 and anti-LC1 are reported in a proportion of adult (0%-6%) or pediatric (0%-11%) cases with chronic hepatitis C infection[36,105–107]. AMA are present (expectedly) in patients with AIH/PBC overlap syndrome, and also in chronic hepatitis C virus infected patients[1], and most recently were described in patients with acute liver failure[108]; AMA occur also in various rheumatological disorders which may co-exist with PBC notably Sjögren’s syndrome and systemic sclerosis[1,48,108–111] and are described in non-liver related conditions with asymptomatic recurrent bacteriuria in women, pulmonary tuberculosis and leprosy[112–114]. However we would submit that in the index disease (AIH or PBC) the frequency and titre of the relevant liver-related autoantibody is substantially higher than for the contrast disease.
Anti-ASGPR antibodies are found particularly in AIH-1 (approximately 90%) but are also present in patients with PBC (14%), chronic hepatitis B and C (7%) and alcoholic hepatitis (8%)[3,52,115]. Anti-SLA antibodies can be found in occasional seronegative AIH patients i.e. those who are negative for ANA, SMA or anti-LKM-1. Anti-SLA antibodies are also frequently present (up to 50%, depending on the sensitivity of the method used) in typical cases of AIH-1 and AIH-2, and also in ASC[86]. Their high specificity for AiLD is has been questioned by reports of anti-SLA being present in some 10% of chronically infected HCV patients[115]. More recently, anti-SLA antibodies have been described in 22% of patients with acute liver failure (ALF)[111]. Since in most cases of ALF we do not know the cause, the presence of anti-SLA can either detract from their disease specificity or, alternatively, suggest an autoimmune pathogenesis (or an autoimmune component to the pathogenesis) of ALF. Monitoring of autoantibodies may be useful in the case of AIH as disappearance or sharp decrease of ANA, SMA and anti-LKM1 can be an indicator of response to immunosuppressive treatment[3,6]. AMA titres do not relate to the stage of PBC and their fluctuation over time does not seem to have pathogenic significance[1,9,116], although “activity” of the PBC process is not as readily measurable as that of AIH. Practically AMA are only tested at presentation to help establish the diagnosis and repeat tests are normally requested only in cases seronegative for AMA at presentation but with clinical or laboratory findings compatible with PBC[1,2,117].
PROGNOSTIC SIGNIFICANCE AND UTILITY OF LIVER-RELATED AUTOANTIBODIES
AIH
Both SMA and ANA tend to lower in titre and even disappear during immunosuppressive therapy in most patients with AIH-1 although neither their titre at diagnosis nor their fluctuations during the disease are thought to predict disease course and outcome[3]. However, in 2002 Gregorio et al found a positive correlation between SMA titre and AST levels over time in pediatric AIH-1 cases, suggesting a potential use of these antibodies, together with IgG levels, to monitor disease activity[118]. There are no comparable adult sequential studies; this may be a reason why no correlation has been ascertained. Nevertheless, Czaja and colleagues have suggested that adult AIH-1 patients with antibodies to anti-actin have a disease onset earlier in life, respond less well to corticosteroids and progress to liver failure or require liver transplantation more frequently compared to those without anti-actin antibodies[69]. The presence of antibodies to double stranded DNA (dsDNA) has been associated with higher levels of immunoglobulin G and higher relapse rates during immunosuppressive treatment compared to seronegative cases[119]. Seropositivity for anti-ASGPR in patients with AIH correlates with histological activity with persistence indicating unresponsiveness to immunosuppressive treatment, and re-appearance being highly suggestive of relapse especially after corticosteroid withdrawal[3,52,115,120]. Anti-SLA antibodies denote patients with a more severe course of AIH and a propensity for relapse after corticosteroid withdrawal compared to their negative counterparts[49,81,121,122]. AIH-2 patients with anti-LC1 antibodies have histologically more severe disease compared to those without anti-LC1 antibodies[35,123,124].
PBC
AMA titres do not seem to be associated with disease severity but those of the IgG3 subclass may identify patients prone to develop more severe disease compared to those without AMA-IgG3[116,125]. PBC-specific ANA have been found more frequently in patients with advanced disease in a number of cross-sectional studies. Anti-NPC seropositivity is associated with accelerated progression to advanced disease and death[94,96,100,126–129] and also, ACA may identify patients with more severe PBC according to studies from USA and Japan[96,130]. These data have obvious implications for the clinical management of PBC given that the only accepted index for estimating survival has been obtained and validated in patients with advanced PBC and hence is of limited use in early disease. Thus, anti-NPC and ACA testing may be important for identifying asymptomatic patients with a likely unfavourable disease course. Once PBC has progressed to advanced histological stages, and serum bilirubin levels have become abnormal, anti-NPC determinations do not appear to offer any additional advantage over other prognostic models such as the Mayo risk score.
PATHOGENIC RELEVANCE OF LIVER-RELATED AUTOANTIBODIES
Despite their undoubted clinical relevance in diagnosis and classification of AiLD, the pathogenic role of autoantibodies and the mechanisms through which they may cause liver damage remains a topic for further research, mainly because of the difficulty in discriminating those actively involved in the immunopathogenic cascade, from those secondary to liver cell damage. The mechanism(s) responsible for the induction of liver-related autoantibodies is currently unknown; several possibilities including molecular mimicry and immunological cross-reactivity have been suggested[78,93,106,131–145]. Most liver-related autoantibodies have limited organ specificity and this notion militates against a direct pathogenic role in highly organ-specific autoimmune injury. For antibodies with a pathogenic potential, complement-dependent and/or antibody-dependent cell-mediated cytotoxicity (ADCC) are the likely effectors of damage[131,146].
EMERGING ISSUES: DIAGNOSTIC ACCURACY, QUALITY ASSURANCE AND STANDARDIZATION PROGRAMMES FOR LIVER AUTOIMMUNE SEROLOGY
There are a number of open issues on serum autoanti-bodies in AiLD. Their diagnostic significance is unquestioned, but problems concerning autoantibody detection and interpretation have not yet been resolved and are not being addressed with sufficient vigour. Several laboratories ignore, for example, the IFL cut-off points recommended by the Committee for Autoimmune Serology of the IAIHG and use their own, thus undermining comparability between different laboratories/centres. Worryingly, the cost per test seems a major reason for arbitrary elevation of cut-off points in routine practice: selecting 1:80 or even 1:160 as a screening dilution expands the number of “negatives” albeit reducing or eliminating the need for re-testing. In patients with AiLD and relatively low autoantibody titres, such as children with AIH, a report that is inaccurately indicative of negativity for autoantibodies can delay diagnosis and, harmfully, defer treatment[76,147]. Hence rigorously performed autoantibody testing may in fact provide a more economical report than a “false negative” one if such leads the clinician to order additional costly diagnostic procedures.
Additional problems for autoantibody testing especially with IFL are intrinsic to the methodology itself. First, availability of tissue substrate comprised of freshly cut sections from cryostat blocks of unfixed liver, kidney stomach tissue is limited to relatively few specialised laboratories. Second, sections of commercial origin are of variable quality because, to lengthen shelf-life, they are treated with fixatives, which readily result in enhanced background staining[55]. Third, IFL requires highly-trained and experienced personnel, is time-consuming and cannot be automated, resulting in a low throughput and increased personnel costs leading to a significant shift from IFL towards ELISAs or blot assays based on liver-autoantibody profiles; these compared to IFL are less-time consuming, easy to perform and amenable to automation. However, the authors of this review reiterate the recommendations of the Committee for Autoimmune Serology of the IAIHG stating that the current ELISAs should complement but not replace IFL. Either technique has their pros and cons, and gives answers to different questions, such that results are not directly comparable[148–150]. Most liver-related autoantibodies can be detected by IFL when using a triple rodent tissue. HEp-2 cells can help to differentiate ANA patterns and ethanol-fixed neutrophils can be used for the detection of ANCAs. In contrast, ELISAs give answers for (usually) pre-selected individual autoantibody specificities. While the analytical sensitivity of ELISAs is satisfactory, their specificity varies according to the manufacturer[150] whereas such problems are rather infrequent by IFL testing based on a triple rodent tissue substrate[151].
Over the last decade there has been a steady increase in the use of the liver-related autoantibody tests to assist both diagnosis and clinical research into AiLD[55]. This increase has been attributed mainly to the introduction of molecularly based assays for the testing of antibodies to F-actin[70–75], CYP2D6[152] and SLA[83,122,153] in AIH, and for evaluating antibodies to sp100 and gp210 in PBC[92,94–96,154]. Of concern, results for these antibody specificities may be promulgated by laboratories without authentication from externally or independently monitored quality assurance programmes (QAP).
Quality assurance (QA) can occur at three levels. The first is at the level of commercial providers of assay kits, reagents etc who would establish QA “in house” before marketing but who often elect to participate also in QAPs for routine laboratories. The second are the formalised QAPs, run by semi-governmental agencies or other organizations, as described below. The third level, which scarcely exists, involves the end-user, the responsible clinician, who must order tests advisedly with good clinical data and interpret these in the light of the clinical information to make wise evidence-based decisions. Thus it behoves the clinician to become fully aware of the many contributions (and shortcomings) of contemporary diagnostic immunoserology.
REPRESENTATIVE QUALITY ASSURANCE PROGRAMMES FOR DIAGNOSTIC SEROLOGY IN LIVER DISEASE
USA
The College of American Pathologists (CAP, www.cap.org) runs survey programmes which allow laboratories to evaluate regularly their autoantibody testing performance. Of relevance to liver, CAP circulates coded anti-M2 AMA, anti-LKM1 and SMA samples for testing. The participating laboratories analyse the sera and return their results for evaluation. In return, each laboratory receives an anonymised report of the performance of all participating laboratories.
UK
A National External Quality Assessment Service (UK NEQAS) (www.ukneqas.org.uk) is responsible for the objective assessment of the performance of autoantibody testing. The UK NEQAS for General Autoimmune Serology incorporates one sample in each of six distributions annually for AMA, anti-LKM1 and SMA. The performance reports of the participating laboratories also provide information on kit suppliers. Participation is not limited to UK but is open to non-UK Countries (Table 1).
Table 1.
Laboratories from various countries participating to the UK National External Quality Assessment Service (UK NEQAS)
| Country | Number | Country | Number |
| Austria | 3 | Latvia | 1 |
| Belgium | 7 | Malaysia | 1 |
| Croatia | 2 | Malta | 1 |
| Cyprus | 1 | New Zealand | 3 |
| Denmark | 2 | Norway | 9 |
| Eire | 15 | Portugal | 31 |
| Estonia | 1 | Republic of Chile | 1 |
| Finland | 5 | Singapore | 1 |
| France | 29 | South Africa | 3 |
| Germany | 9 | Spain | 68 |
| Greece | 16 | Sweden | 14 |
| Hong kong | 1 | Switzerland | 7 |
| Hungary | 5 | The Netherlands | 1 |
| Israel | 8 | Turkey | 2 |
| Italy | 65 | UK | 136 |
| Kingdom of Saudi Arabia | 1 | United Arab Emirates | 1 |
| Kuwait | 1 | USA | 3 |
Germany
There are currently two regulatory and quality assurance agencies, namely INSTAND (Institut für Standardisierung, www.instandev.de) and DGKL (Deutsche Gesellschaft für Klinische Chemie und Laboratoriumsmedizin, www.dgkl.de). INSTAND circulates twice per year two samples to be tested for AMA, SMA and anti-LKM1 antibody testing. Participants (150) report results quantitatively and semi-quantitatively (from 0-4 to evaluate antibody titre; 0 = negative; 1 = borderline; 2 = low; 3 = middle; and 4 = high). There is no reference to specific manufacturers but only to test methods and overall percentage of consistent results. DGKL has a similar approach but evaluations are divided on the basis of the methods used and they provide also information in relation to the kits manufacturers. Target values are determined in two reference laboratories.
France
Quality autoantibody assessment in France is organised by the French Health Products Safety Agency (AFSSAPS, Agence Française de Sécurité Sanitaire des Produits de Santé, http://agmed.sante.gouv.fr/). This Agency has the executive responsibility for proposing relevant QAPs to clinical laboratories, whether in the private or in the public sector. An autoantibody detection survey has been running on an annual basis since 1998.
Italy
In Italy there are no formal regulatory and quality assurance programmes with several laboratories participating in the surveys by UK NEQAS or CAP. Recently, a study group has been formed (Forum Interdi-sciplinare per la Ricerca nelle Malattie Autoimmuni-FIRMA-www.grouppofirma.com). FIRMA aims to provide guidelines for autontibody testing and to identify and collect sera of different autoantibody specificities that will be available for all of its member institutions.
Finland
Labquality at Helsinki offers twice per year three samples for SMA, AMA and anti-LKM1 assessment. Qualitative target values are determined in a reference laboratory and results are listed according to manufacturer and method. Evaluation reports are confidential.
Australia and New Zealand
QAPs have been established under the auspices of the Royal College of Pathologists of Australasia (RCPA) based on the selection by RCPA of expert organizing groups which distribute batches of sera to diagnostic laboratories that voluntarily elect to participate (www.rcpaqap.com.au). Diagnostic laboratories from Australia, New Zealand, and several South East Asian countries together with manufacturers and purveyors of kits participate in this programme. The Tissue Antibodies module includes AMA, SMA and anti-LKM1 antibodies. Feedback to the laboratories is by a report to all participants in which any single laboratory can identify its own performance versus that of all other participants. The RCPA issues certification of participation in this QAP. The reports sent back to laboratories are inspected by the National Association of Testing Authorities (NATA) during laboratory assessment visits. In order to be accredited, laboratories must participate and perform satisfactorily in the relevant proficiency testing programmes. There is a ‘regulatory’ element here in that NATA certification is required for access to fees under the Medicare rebate scheme.
As expected, quality assurance programmes have highlighted difficulties encountered by peripheral laboratories. In mid-2007, UK NEQAS distributed a serum with a typical anti-LKM1 antibody staining; a substantial proportion (53 out of 356, 15%) of the laboratories reported negativity for anti-LKM1 antibody test and, among these 53 laboratories, 43 incorrectly reported positivity for AMA instead (Peter White, UK NEQAS, personal communication). Also, rather worryingly, several additional laboratories did not return reports on anti-LKM1 either because they themselves do not offer this test or because they ignore its significance (Peter White, UK NEQAS, personal communication).
It is clear that exchange of calibrated reference sera and rigorous standardization programmes on liver-related autoantibody serology are urgently needed. Such initiatives will need to involve initially researchers and laboratories with a special interest in the respective antibody specificities and subsequently clinical laboratories performing routine screening tests. To this end, efforts have been made recently by the IAIHG to arrange an exchange of sera at international level but whether such an initiative will take off depends on securing financial support. Administrative sponsorship should initially come from the International Association for the Study of Liver (IASL), the American Association for the Study of Liver Diseases (AASLD) or the European Association for the Study of Liver (EASL) or from Clinical Immunology Societies of developed countries.
In conclusion, practice guidelines on liver autoimmune serology based on consensus of experts in the field have been issued and need to be steadily updated[55]. The more the clinician is aware of these guidelines, the greater the chance of correct and clinically relevant autoantibody diagnosis. It is in the best interest of the patient to obtain eventually the highest possible commitment and coordination of all organizations, agencies, industrial partners and networks working in the field.
ACKNOWLEDGMENTS
We thank Edward T Davies, David Gillis, Sue Jovanovich, Luigi Muratori, Gary L Norman, Wolfgang Schlumberger, Giorgina Mieli-Vergani, Peter White and Bob Wilson for helpful comments.
Footnotes
S- Editor Li DL L- Editor Alpini GD E- Editor Ma WH
References
- 1.Bogdanos DP, Baum H, Vergani D. Antimitochondrial and other autoantibodies. Clin Liver Dis. 2003;7:759–777, vi. doi: 10.1016/s1089-3261(03)00104-1. [DOI] [PubMed] [Google Scholar]
- 2.Invernizzi P, Lleo A, Podda M. Interpreting serological tests in diagnosing autoimmune liver diseases. Semin Liver Dis. 2007;27:161–172. doi: 10.1055/s-2007-979469. [DOI] [PubMed] [Google Scholar]
- 3.Czaja AJ, Homburger HA. Autoantibodies in liver disease. Gastroenterology. 2001;120:239–249. doi: 10.1053/gast.2001.20223. [DOI] [PubMed] [Google Scholar]
- 4.Selmi C, Mackay IR, Gershwin ME. The immunological milieu of the liver. Semin Liver Dis. 2007;27:129–139. doi: 10.1055/s-2007-979466. [DOI] [PubMed] [Google Scholar]
- 5.Alvarez F, Berg PA, Bianchi FB, Bianchi L, Burroughs AK, Cancado EL, Chapman RW, Cooksley WG, Czaja AJ, Desmet VJ, et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999;31:929–938. doi: 10.1016/s0168-8278(99)80297-9. [DOI] [PubMed] [Google Scholar]
- 6.Gregorio GV, Portmann B, Reid F, Donaldson PT, Doherty DG, McCartney M, Mowat AP, Vergani D, Mieli-Vergani G. Autoimmune hepatitis in childhood: a 20-year experience. Hepatology. 1997;25:541–547. doi: 10.1002/hep.510250308. [DOI] [PubMed] [Google Scholar]
- 7.Gregorio GV, Portmann B, Karani J, Harrison P, Donaldson PT, Vergani D, Mieli-Vergani G. Autoimmune hepatitis/sclerosing cholangitis overlap syndrome in childhood: a 16-year prospective study. Hepatology. 2001;33:544–553. doi: 10.1053/jhep.2001.22131. [DOI] [PubMed] [Google Scholar]
- 8.Kerkar N, Hadzic N, Davies ET, Portmann B, Donaldson PT, Rela M, Heaton ND, Vergani D, Mieli-Vergani G. De-novo autoimmune hepatitis after liver transplantation. Lancet. 1998;351:409–413. doi: 10.1016/S0140-6736(97)06478-7. [DOI] [PubMed] [Google Scholar]
- 9.Kaplan MM, Gershwin ME. Primary biliary cirrhosis. N Engl J Med. 2005;353:1261–1273. doi: 10.1056/NEJMra043898. [DOI] [PubMed] [Google Scholar]
- 10.Miescher P, Fauconnet M. [Absorption of L. E. factor by isolated cell nuclei.] Experientia. 1954;10:252–253. doi: 10.1007/BF02157392. [DOI] [PubMed] [Google Scholar]
- 11.Hargraves M, Richmond H, Morton R. Presentation of two bone marrow elements: The “tart” cells and the “L.E” cell. Mayo Clin Proc. 1948;27:25–28. [PubMed] [Google Scholar]
- 12.Robbins WC, Holman HR, Deicher H, Kunkel HG. Complement fixation with cell nuclei and DNA in lupus erythematosus. Proc Soc Exp Biol Med. 1957;96:575–579. doi: 10.3181/00379727-96-23545. [DOI] [PubMed] [Google Scholar]
- 13.Holman H, Deicher HR. The reaction of the lupus erythematosus (L.E.) cell factor with deoxyribonucleoprotein of the cell nucleus. J Clin Invest. 1959;38:2059–2072. doi: 10.1172/JCI103984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cowling DC, Mackay IR, Taft LI. Lupoid hepatitis. Lancet. 1956;271:1323–1326. doi: 10.1016/s0140-6736(56)91483-0. [DOI] [PubMed] [Google Scholar]
- 15.Mackay IR, Taft LI, Cowling DC. Lupoid hepatitis and the hepatic lesions of systemic lupus erythematosus. Lancet. 1959;1:65–69. doi: 10.1016/s0140-6736(59)91136-5. [DOI] [PubMed] [Google Scholar]
- 16.Johnson GD, Holborow EJ, Glynn LE. Antibody to smooth muscle in patients with liver disease. Lancet. 1965;2:878–879. doi: 10.1016/s0140-6736(65)92505-5. [DOI] [PubMed] [Google Scholar]
- 17.Whittingham S, Irwin J, Mackay IR, Smalley M. Smooth muscle autoantibody in “autoimmune” hepatitis. Gastroenterology. 1966;51:499–505. [PubMed] [Google Scholar]
- 18.Bottazzo GF, Florin-Christensen A, Fairfax A, Swana G, Doniach D, Groeschel-Stewart U. Classification of smooth muscle autoantibodies detected by immunofluorescence. J Clin Pathol. 1976;29:403–410. doi: 10.1136/jcp.29.5.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gabbiani G, Ryan GB, Lamelin JP, Vassalli P, Majno G, Bouvier CA, Cruchaud A, Luscher EF. Human smooth muscle autoantibody. Its identification as antiactin antibody and a study of its binding to “nonmuscular” cells. Am J Pathol. 1973;72:473–488. [PMC free article] [PubMed] [Google Scholar]
- 20.Lidman K, Biberfeld G, Fagraeus A, Norberg R, Torstensson R, Utter G, Carlsson L, Luca J, Lindberg U. Anti-actin specificity of human smooth muscle antibodies in chronic active hepatitis. Clin Exp Immunol. 1976;24:266–272. [PMC free article] [PubMed] [Google Scholar]
- 21.Toh BH. Smooth muscle autoantibodies and autoantigens. Clin Exp Immunol. 1979;38:621–628. [PMC free article] [PubMed] [Google Scholar]
- 22.Rizzetto M, Swana G, Doniach D. Microsomal antibodies in active chronic hepatitis and other disorders. Clin Exp Immunol. 1973;15:331–344. [PMC free article] [PubMed] [Google Scholar]
- 23.Rizzetto M, Bianchi FB, Doniach D. Characterization of the microsomal antigen related to a subclass of active chronic hepatitis. Immunology. 1974;26:589–601. [PMC free article] [PubMed] [Google Scholar]
- 24.Smith MG, Williams R, Walker G, Rizzetto M, Doniach D. Hepatic disorders associated with liver-kidney microsomal antibodies. Br Med J. 1974;2:80–84. doi: 10.1136/bmj.2.5910.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Manns MP, Obermayer-Straub P. Cytochromes P450 and uridine triphosphate-glucuronosyltransferases: model autoantigens to study drug-induced, virus-induced, and autoimmune liver disease. Hepatology. 1997;26:1054–1066. doi: 10.1002/hep.510260438. [DOI] [PubMed] [Google Scholar]
- 26.Homberg JC, Abuaf N, Bernard O, Islam S, Alvarez F, Khalil SH, Poupon R, Darnis F, Levy VG, Grippon P. Chronic active hepatitis associated with antiliver/kidney microsome antibody type 1: a second type of “autoimmune” hepatitis. Hepatology. 1987;7:1333–1339. doi: 10.1002/hep.1840070626. [DOI] [PubMed] [Google Scholar]
- 27.Gueguen M, Meunier-Rotival M, Bernard O, Alvarez F. Anti-liver kidney microsome antibody recognizes a cytochrome P450 from the IID subfamily. J Exp Med. 1988;168:801–806. doi: 10.1084/jem.168.2.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Manns MP, Johnson EF, Griffin KJ, Tan EM, Sullivan KF. Major antigen of liver kidney microsomal autoantibodies in idiopathic autoimmune hepatitis is cytochrome P450db1. J Clin Invest. 1989;83:1066–1072. doi: 10.1172/JCI113949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zanger UM, Hauri HP, Loeper J, Homberg JC, Meyer UA. Antibodies against human cytochrome P-450db1 in autoimmune hepatitis type II. Proc Natl Acad Sci USA. 1988;85:8256–8260. doi: 10.1073/pnas.85.21.8256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Crivelli O, Lavarini C, Chiaberge E, Amoroso A, Farci P, Negro F, Rizzetto M. Microsomal autoantibodies in chronic infection with the HBsAg associated delta (delta) agent. Clin Exp Immunol. 1983;54:232–238. [PMC free article] [PubMed] [Google Scholar]
- 31.Clemente MG, Meloni A, Obermayer-Straub P, Frau F, Manns MP, De Virgiliis S. Two cytochromes P450 are major hepatocellular autoantigens in autoimmune polyglandular syndrome type 1. Gastroenterology. 1998;114:324–328. doi: 10.1016/s0016-5085(98)70484-6. [DOI] [PubMed] [Google Scholar]
- 32.Boccaccio F, Attali P, Nataf J, Ink O, Fabre M, Pelletier G. [Acute hepatitis caused by dihydralazine] Gastroenterol Clin Biol. 1987;11:614. [PubMed] [Google Scholar]
- 33.Manns M, Zanger U, Gerken G, Sullivan KF, Meyer zum Buschenfelde KH, Meyer UA, Eichelbaum M. Patients with type II autoimmune hepatitis express functionally intact cytochrome P-450 db1 that is inhibited by LKM-1 autoantibodies in vitro but not in vivo. Hepatology. 1990;12:127–132. doi: 10.1002/hep.1840120120. [DOI] [PubMed] [Google Scholar]
- 34.Bourdi M, Larrey D, Nataf J, Bernuau J, Pessayre D, Iwasaki M, Guengerich FP, Beaune PH. Anti-liver endoplasmic reticulum autoantibodies are directed against human cytochrome P-450IA2. A specific marker of dihydralazine-induced hepatitis. J Clin Invest. 1990;85:1967–1973. doi: 10.1172/JCI114660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martini E, Abuaf N, Cavalli F, Durand V, Johanet C, Homberg JC. Antibody to liver cytosol (anti-LC1) in patients with autoimmune chronic active hepatitis type 2. Hepatology. 1988;8:1662–1666. doi: 10.1002/hep.1840080632. [DOI] [PubMed] [Google Scholar]
- 36.Lenzi M, Manotti P, Muratori L, Cataleta M, Ballardini G, Cassani F, Bianchi FB. Liver cytosolic 1 antigen-antibody system in type 2 autoimmune hepatitis and hepatitis C virus infection. Gut. 1995;36:749–754. doi: 10.1136/gut.36.5.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lapierre P, Hajoui O, Homberg JC, Alvarez F. Formiminotransferase cyclodeaminase is an organ-specific autoantigen recognized by sera of patients with autoimmune hepatitis. Gastroenterology. 1999;116:643–649. doi: 10.1016/s0016-5085(99)70186-1. [DOI] [PubMed] [Google Scholar]
- 38.Muratori L, Sztul E, Muratori P, Gao Y, Ripalti A, Ponti C, Lenzi M, Landini MP, Bianchi FB. Distinct epitopes on formiminotransferase cyclodeaminase induce autoimmune liver cytosol antibody type 1. Hepatology. 2001;34:494–501. doi: 10.1053/jhep.2001.27179. [DOI] [PubMed] [Google Scholar]
- 39.Mackay IR. Primary biliary cirrhosis showing a high titer of autoantibody; report of a case. N Engl J Med. 1958;258:185–188. doi: 10.1056/NEJM195801232580407. [DOI] [PubMed] [Google Scholar]
- 40.Asherson GL, Dumonde DC. Characterization of auto-antibodies produced in the rabbit by the injection of rat liver. Br J Exp Pathol. 1962;43:12–20. [PMC free article] [PubMed] [Google Scholar]
- 41.Walker JG, Doniach D, Roitt IM, Sherlock S. Serological Tests in Diagnosis of Primary Biliary Cirrhosis. Lancet. 1965;1:827–831. doi: 10.1016/s0140-6736(65)91372-3. [DOI] [PubMed] [Google Scholar]
- 42.Berg PA, Doniach D, Roitt IM. Mitochondrial antibodies in primary biliary cirrhosis. I. Localization of the antigen to mitochondrial membranes. J Exp Med. 1967;126:277–290. doi: 10.1084/jem.126.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Berg PA, Muscatello U, Horne RW, Roitt IM, Doniach D. Mitochondrial antibodies in primary biliary cirrhosis. II. The complement fixing antigen as a component of mitochondrial inner membranes. Br J Exp Pathol. 1969;50:200–208. [PMC free article] [PubMed] [Google Scholar]
- 44.Berg PA, Roitt IM, Doniach D, Cooper HM. Mitochondrial antibodies in primary biliary cirrhosis. IV. Significance of membrane structure for the complement-fixing antigen. Immunology. 1969;17:281–293. [PMC free article] [PubMed] [Google Scholar]
- 45.Berg PA, Roitt IM, Doniach D, Horne RW. Mitochondrial antibodies in primary biliary cirrhosis. 3. Characterization of the inner-membrane complement fixing antigen. Clin Exp Immunol. 1969;4:511–525. [PMC free article] [PubMed] [Google Scholar]
- 46.Gershwin ME, Mackay IR, Sturgess A, Coppel RL. Identification and specificity of a cDNA encoding the 70 kd mitochondrial antigen recognized in primary biliary cirrhosis. J Immunol. 1987;138:3525–3531. [PubMed] [Google Scholar]
- 47.Yeaman SJ, Fussey SP, Danner DJ, James OF, Mutimer DJ, Bassendine MF. Primary biliary cirrhosis: identification of two major M2 mitochondrial autoantigens. Lancet. 1988;1:1067–1070. doi: 10.1016/s0140-6736(88)91894-6. [DOI] [PubMed] [Google Scholar]
- 48.Leung PS, Coppel RL, Ansari A, Munoz S, Gershwin ME. Antimitochondrial antibodies in primary biliary cirrhosis. Semin Liver Dis. 1997;17:61–69. doi: 10.1055/s-2007-1007183. [DOI] [PubMed] [Google Scholar]
- 49.Manns M, Gerken G, Kyriatsoulis A, Staritz M, Meyer zum Buschenfelde KH. Characterisation of a new subgroup of autoimmune chronic active hepatitis by autoantibodies against a soluble liver antigen. Lancet. 1987;1:292–294. doi: 10.1016/s0140-6736(87)92024-1. [DOI] [PubMed] [Google Scholar]
- 50.Stechemesser E, Klein R, Berg PA. Characterization and clinical relevance of liver-pancreas antibodies in autoimmune hepatitis. Hepatology. 1993;18:1–9. [PubMed] [Google Scholar]
- 51.Wies I, Brunner S, Henninger J, Herkel J, Kanzler S, Meyer zum Buschenfelde KH, Lohse AW. Identification of target antigen for SLA/LP autoantibodies in autoimmune hepatitis. Lancet. 2000;355:1510–1515. doi: 10.1016/s0140-6736(00)02166-8. [DOI] [PubMed] [Google Scholar]
- 52.McFarlane IG, Hegarty JE, McSorley CG, McFarlane BM, Williams R. Antibodies to liver-specific protein predict outcome of treatment withdrawal in autoimmune chronic active hepatitis. Lancet. 1984;2:954–956. doi: 10.1016/s0140-6736(84)91167-x. [DOI] [PubMed] [Google Scholar]
- 53.McFarlane IG, McFarlane BM, Major GN, Tolley P, Williams R. Identification of the hepatic asialo-glycoprotein receptor (hepatic lectin) as a component of liver specific membrane lipoprotein (LSP) Clin Exp Immunol. 1984;55:347–354. [PMC free article] [PubMed] [Google Scholar]
- 54.Weller TH, Coons AH. Fluorescent antibody studies with agents of varicella and herpes zoster propagated in vitro. Proc Soc Exp Biol Med. 1954;86:789–794. doi: 10.3181/00379727-86-21235. [DOI] [PubMed] [Google Scholar]
- 55.Vergani D, Alvarez F, Bianchi FB, Cancado EL, Mackay IR, Manns MP, Nishioka M, Penner E. Liver autoimmune serology: a consensus statement from the committee for autoimmune serology of the International Autoimmune Hepatitis Group. J Hepatol. 2004;41:677–683. doi: 10.1016/j.jhep.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 56.Toolan HW. Transplantable human neoplasms maintained in cortisone-treated laboratory animals: H.S. No. 1; H.Ep. No. 1; H.Ep. No. 2; H.Ep. No. 3; and H.Emb.Rh. No. 1. Cancer Res. 1954;14:660–666. [PubMed] [Google Scholar]
- 57.Moore AE, Sabachewsky L, Toolan HW. Culture characteristics of four permanent lines of human cancer cells. Cancer Res. 1955;15:598–602. [PubMed] [Google Scholar]
- 58.Szostecki C, Guldner HH, Will H. Autoantibodies against “nuclear dots” in primary biliary cirrhosis. Semin Liver Dis. 1997;17:71–78. doi: 10.1055/s-2007-1007184. [DOI] [PubMed] [Google Scholar]
- 59.Courvalin JC, Worman HJ. Nuclear envelope protein autoantibodies in primary biliary cirrhosis. Semin Liver Dis. 1997;17:79–90. doi: 10.1055/s-2007-1007185. [DOI] [PubMed] [Google Scholar]
- 60.Czaja AJ, Manns MP, Homburger HA. Frequency and significance of antibodies to liver/kidney microsome type 1 in adults with chronic active hepatitis. Gastroenterology. 1992;103:1290–1295. doi: 10.1016/0016-5085(92)91518-9. [DOI] [PubMed] [Google Scholar]
- 61.Dahlan Y, Smith L, Simmonds D, Jewell LD, Wanless I, Heathcote EJ, Bain VG. Pediatric-onset primary biliary cirrhosis. Gastroenterology. 2003;125:1476–1479. doi: 10.1016/j.gastro.2003.08.022. [DOI] [PubMed] [Google Scholar]
- 62.Hannam S, Bogdanos DP, Davies ET, Hussain MJ, Portmann BC, Mieli-Vergani G, Vergani D. Neonatal liver disease associated with placental transfer of anti-mitochondrial antibodies. Autoimmunity. 2002;35:545–550. doi: 10.1080/0891693021000054057. [DOI] [PubMed] [Google Scholar]
- 63.Muratori L, Cataleta M, Muratori P, Manotti P, Lenzi M, Cassani F, Bianchi FB. Detection of anti-liver cytosol antibody type 1 (anti-LC1) by immunodiffusion, counterimmunoelectrophoresis and immunoblotting: comparison of different techniques. J Immunol Methods. 1995;187:259–264. doi: 10.1016/0022-1759(95)00192-x. [DOI] [PubMed] [Google Scholar]
- 64.van der Woude FJ, Rasmussen N, Lobatto S, Wiik A, Permin H, van Es LA, van der Giessen M, van der Hem GK, The TH. Autoantibodies against neutrophils and monocytes: tool for diagnosis and marker of disease activity in Wegener’s granulomatosis. Lancet. 1985;1:425–429. doi: 10.1016/s0140-6736(85)91147-x. [DOI] [PubMed] [Google Scholar]
- 65.Hagen EC, Andrassy K, Chernok E, Daha MR, Gaskin G, Gross W, Lesavre P, Ludemann J, Pusey CD, Rasmussen N. The value of indirect immunofluorescence and solid phase techniques for ANCA detection. A report on the first phase of an international cooperative study on the standardization of ANCA assays. EEC/BCR Group for ANCA Assay Standardization. J Immunol Methods. 1993;159:1–16. doi: 10.1016/0022-1759(93)90136-u. [DOI] [PubMed] [Google Scholar]
- 66.Terjung B, Herzog V, Worman HJ, Gestmann I, Bauer C, Sauerbruch T, Spengler U. Atypical antineutrophil cytoplasmic antibodies with perinuclear fluorescence in chronic inflammatory bowel diseases and hepatobiliary disorders colocalize with nuclear lamina proteins. Hepatology. 1998;28:332–340. doi: 10.1002/hep.510280207. [DOI] [PubMed] [Google Scholar]
- 67.Terjung B, Spengler U, Sauerbruch T, Worman HJ. “Atypical p-ANCA” in IBD and hepatobiliary disorders react with a 50-kilodalton nuclear envelope protein of neutrophils and myeloid cell lines. Gastroenterology. 2000;119:310–322. doi: 10.1053/gast.2000.9366. [DOI] [PubMed] [Google Scholar]
- 68.Terjung B, Worman HJ, Herzog V, Sauerbruch T, Spengler U. Differentiation of antineutrophil nuclear antibodies in inflammatory bowel and autoimmune liver diseases from antineutrophil cytoplasmic antibodies (p-ANCA) using immunofluorescence microscopy. Clin Exp Immunol. 2001;126:37–46. doi: 10.1046/j.1365-2249.2001.01649.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Czaja AJ, Cassani F, Cataleta M, Valentini P, Bianchi FB. Frequency and significance of antibodies to actin in type 1 autoimmune hepatitis. Hepatology. 1996;24:1068–1073. doi: 10.1002/hep.510240515. [DOI] [PubMed] [Google Scholar]
- 70.Granito A, Muratori L, Muratori P, Pappas G, Guidi M, Cassani F, Volta U, Ferri A, Lenzi M, Bianchi FB. Antibodies to filamentous actin (F-actin) in type 1 autoimmune hepatitis. J Clin Pathol. 2006;59:280–284. doi: 10.1136/jcp.2005.027367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Frenzel C, Herkel J, Luth S, Galle PR, Schramm C, Lohse AW. Evaluation of F-actin ELISA for the diagnosis of autoimmune hepatitis. Am J Gastroenterol. 2006;101:2731–2736. doi: 10.1111/j.1572-0241.2006.00830.x. [DOI] [PubMed] [Google Scholar]
- 72.Liaskos C, Bogdanos DP, Davies ET, Dalekos GN. Diagnostic relevance of anti-filamentous actin antibodies in autoimmune hepatitis. J Clin Pathol. 2007;60:107–108. doi: 10.1136/jcp.2006.039404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zamanou A, Tsirogianni A, Terzoglou C, Balafas A, Economidou I, Lymberi P. Anti-smooth muscle antibodies (ASMAs) and anti-cytoskeleton antibodies (ACTAs) in liver diseases: a comparison of classical indirect immunofluorescence with ELISA. J Clin Lab Anal. 2002;16:194–201. doi: 10.1002/jcla.10040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Granito A, Muratori P, Muratori L, Georgios P, Lenzi M, Bianchi FB. Antifilamentous actin antibodies by ELISA for the diagnosis of type 1 autoimmune hepatitis. Am J Gastroenterol. 2007;102:1131–1132. doi: 10.1111/j.1572-0241.2007.01180_7.x. [DOI] [PubMed] [Google Scholar]
- 75.Villalta D, Bizzaro N, Da Re M, Tozzoli R, Komorowski L, Tonutti E. Diagnostic accuracy of four different immunological methods for the detection of anti-F-actin autoantibodies in type 1 autoimmune hepatitis and other liver-related disorders. Autoimmunity. 2008;41:105–110. doi: 10.1080/08916930701619896. [DOI] [PubMed] [Google Scholar]
- 76.Bogdanos DP, Mieli-Vergani G, Vergani D. Liver-kidney microsomal antibody-positive autoimmune hepatitis in the United States. Am J Gastroenterol. 2001;96:3447–3448. doi: 10.1111/j.1572-0241.2001.05382.x. [DOI] [PubMed] [Google Scholar]
- 77.Ma Y, Gregorio G, Gaken J, Muratori L, Bianchi FB, Mieli-Vergani G, Vergani D. Establishment of a novel radioligand assay using eukaryotically expressed cytochrome P4502D6 for the measurement of liver kidney microsomal type 1 antibody in patients with autoimmune hepatitis and hepatitis C virus infection. J Hepatol. 1997;26:1396–1402. doi: 10.1016/s0168-8278(97)80477-1. [DOI] [PubMed] [Google Scholar]
- 78.Bogdanos DP, Lenzi M, Okamoto M, Rigopoulou EI, Muratori P, Ma Y, Muratori L, Tsantoulas D, Mieli- Vergani G, Bianchi FB, et al. Multiple viral/self immunological cross-reactivity in liver kidney microsomal antibody positive hepatitis C virus infected patients is associated with the possession of HLA B51. Int J Immunopathol Pharmacol. 2004;17:83–92. doi: 10.1177/039463200401700112. [DOI] [PubMed] [Google Scholar]
- 79.Ma Y, Peakman M, Lobo-Yeo A, Wen L, Lenzi M, Gaken J, Farzaneh F, Mieli-Vergani G, Bianchi FB, Vergani D. Differences in immune recognition of cytochrome P4502D6 by liver kidney microsomal (LKM) antibody in autoimmune hepatitis and chronic hepatitis C virus infection. Clin Exp Immunol. 1994;97:94–99. doi: 10.1111/j.1365-2249.1994.tb06585.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Muratori L, Lenzi M, Ma Y, Cataleta M, Mieli-Vergani G, Vergani D, Bianchi FB. Heterogeneity of liver/kidney microsomal antibody type 1 in autoimmune hepatitis and hepatitis C virus related liver disease. Gut. 1995;37:406–412. doi: 10.1136/gut.37.3.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ma Y, Okamoto M, Thomas MG, Bogdanos DP, Lopes AR, Portmann B, Underhill J, Durr R, Mieli-Vergani G, Vergani D. Antibodies to conformational epitopes of soluble liver antigen define a severe form of autoimmune liver disease. Hepatology. 2002;35:658–664. doi: 10.1053/jhep.2002.32092. [DOI] [PubMed] [Google Scholar]
- 82.Volkmann M, Martin L, Baurle A, Heid H, Strassburg CP, Trautwein C, Fiehn W, Manns MP. Soluble liver antigen: isolation of a 35-kd recombinant protein (SLA-p35) specifically recognizing sera from patients with autoimmune hepatitis. Hepatology. 2001;33:591–596. doi: 10.1053/jhep.2001.22218. [DOI] [PubMed] [Google Scholar]
- 83.Baeres M, Herkel J, Czaja AJ, Wies I, Kanzler S, Cancado EL, Porta G, Nishioka M, Simon T, Daehnrich C, et al. Establishment of standardised SLA/LP immunoassays: specificity for autoimmune hepatitis, worldwide occurrence, and clinical characteristics. Gut. 2002;51:259–264. doi: 10.1136/gut.51.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ballot E, Bruneel A, Labas V, Johanet C. Identification of rat targets of anti-soluble liver antigen autoantibodies by serologic proteome analysis. Clin Chem. 2003;49:634–643. doi: 10.1373/49.4.634. [DOI] [PubMed] [Google Scholar]
- 85.Bogdanos DP, Bianchi I, Ma Y, Mitry RR, Mieli-Vergani G, Vergani D. Targets of antibodies to soluble liver antigen in patients with autoimmune hepatitis. Clin Chem. 2004;50:682–683; author reply 683-684. doi: 10.1373/clinchem.2003.027730. [DOI] [PubMed] [Google Scholar]
- 86.Vitozzi S, Djilali-Saiah I, Lapierre P, Alvarez F. Anti-soluble liver antigen/liver-pancreas (SLA/LP) antibodies in pediatric patients with autoimmune hepatitis. Autoimmunity. 2002;35:485–492. doi: 10.1080/0891693021000056712. [DOI] [PubMed] [Google Scholar]
- 87.Xu XM, Carlson BA, Mix H, Zhang Y, Saira K, Glass RS, Berry MJ, Gladyshev VN, Hatfield DL. Biosynthesis of selenocysteine on its tRNA in eukaryotes. PLoS Biol. 2007;5:e4. doi: 10.1371/journal.pbio.0050004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Moteki S, Leung PS, Coppel RL, Dickson ER, Kaplan MM, Munoz S, Gershwin ME. Use of a designer triple expression hybrid clone for three different lipoyl domain for the detection of antimitochondrial autoantibodies. Hepatology. 1996;24:97–103. doi: 10.1002/hep.510240117. [DOI] [PubMed] [Google Scholar]
- 89.Oertelt S, Rieger R, Selmi C, Invernizzi P, Ansari AA, Coppel RL, Podda M, Leung PS, Gershwin ME. A sensitive bead assay for antimitochondrial antibodies: Chipping away at AMA-negative primary biliary cirrhosis. Hepatology. 2007;45:659–665. doi: 10.1002/hep.21583. [DOI] [PubMed] [Google Scholar]
- 90.Gabeta S, Norman GL, Liaskos C, Papamichalis PA, Zografos T, Garagounis A, Rigopoulou EI, Dalekos GN. Diagnostic relevance and clinical significance of the new enhanced performance M2 (MIT3) ELISA for the detection of IgA and IgG antimitochondrial antibodies in primary biliary cirrhosis. J Clin Immunol. 2007;27:378–387. doi: 10.1007/s10875-007-9092-0. [DOI] [PubMed] [Google Scholar]
- 91.Janka C, Selmi C, Gershwin ME, Will H, Sternsdorf T. Small ubiquitin-related modifiers: A novel and independent class of autoantigens in primary biliary cirrhosis. Hepatology. 2005;41:609–616. doi: 10.1002/hep.20619. [DOI] [PubMed] [Google Scholar]
- 92.Muratori P, Muratori L, Ferrari R, Cassani F, Bianchi G, Lenzi M, Rodrigo L, Linares A, Fuentes D, Bianchi FB. Characterization and clinical impact of antinuclear antibodies in primary biliary cirrhosis. Am J Gastroenterol. 2003;98:431–437. doi: 10.1111/j.1572-0241.2003.07257.x. [DOI] [PubMed] [Google Scholar]
- 93.Bogdanos DP, Baum H, Butler P, Rigopoulou EI, Davies ET, Ma Y, Burroughs AK, Vergani D. Association between the primary biliary cirrhosis specific anti-sp100 antibodies and recurrent urinary tract infection. Dig Liver Dis. 2003;35:801–805. doi: 10.1016/s1590-8658(03)00466-3. [DOI] [PubMed] [Google Scholar]
- 94.Bogdanos DP, Liaskos C, Pares A, Norman G, Rigopoulou EI, Caballeria L, Dalekos GN, Rodes J, Vergani D. Anti-gp210 antibody mirrors disease severity in primary biliary cirrhosis. Hepatology. 2007;45:1583; author reply 1583–1583; author reply 1584. doi: 10.1002/hep.21678. [DOI] [PubMed] [Google Scholar]
- 95.Bogdanos DP, Pares A, Rodes J, Vergani D. Primary biliary cirrhosis specific antinuclear antibodies in patients from Spain. Am J Gastroenterol. 2004;99:763–764; author reply 765. doi: 10.1111/j.1572-0241.2004.04119.x. [DOI] [PubMed] [Google Scholar]
- 96.Nakamura M, Kondo H, Mori T, Komori A, Matsuyama M, Ito M, Takii Y, Koyabu M, Yokoyama T, Migita K, et al. Anti-gp210 and anti-centromere antibodies are different risk factors for the progression of primary biliary cirrhosis. Hepatology. 2007;45:118–127. doi: 10.1002/hep.21472. [DOI] [PubMed] [Google Scholar]
- 97.Bauer A, Habior A. Measurement of gp210 autoantibodies in sera of patients with primary biliary cirrhosis. J Clin Lab Anal. 2007;21:227–231. doi: 10.1002/jcla.20170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wesierska-Gadek J, Klima A, Komina O, Ranftler C, Invernizzi P, Penner E. Characterization of autoantibodies against components of the nuclear pore complexes: high frequency of anti-p62 nucleoporin antibodies. Ann N Y Acad Sci. 2007;1109:519–530. doi: 10.1196/annals.1398.058. [DOI] [PubMed] [Google Scholar]
- 99.Vergani D, Bogdanos DP. Positive markers in AMA-negative PBC. Am J Gastroenterol. 2003;98:241–243. doi: 10.1111/j.1572-0241.2003.07270.x. [DOI] [PubMed] [Google Scholar]
- 100.Invernizzi P, Selmi C, Ranftler C, Podda M, Wesierska-Gadek J. Antinuclear antibodies in primary biliary cirrhosis. Semin Liver Dis. 2005;25:298–310. doi: 10.1055/s-2005-916321. [DOI] [PubMed] [Google Scholar]
- 101.Terjung B, Gottwein J, Muennich M, Muennich M, Gottwein J, Sauerbruch T, Spengler U. Identifizierung des Zielantigens atypischer p-ANCA bei autoimmunen Lebererkrankungen als Protein der Tubulin-beta Genfamilie. Z Gastroenterol. 2005;43:Abstract. [Google Scholar]
- 102.Targan SR, Landers C, Vidrich A, Czaja AJ. High-titer antineutrophil cytoplasmic antibodies in type-1 autoimmune hepatitis. Gastroenterology. 1995;108:1159–1166. doi: 10.1016/0016-5085(95)90215-5. [DOI] [PubMed] [Google Scholar]
- 103.Mulder AH, Horst G, Haagsma EB, Limburg PC, Kleibeuker JH, Kallenberg CG. Prevalence and characterization of neutrophil cytoplasmic antibodies in autoimmune liver diseases. Hepatology. 1993;17:411–417. [PubMed] [Google Scholar]
- 104.Pratt DS, Kaplan MM. Evaluation of abnormal liver-enzyme results in asymptomatic patients. N Engl J Med. 2000;342:1266–1271. doi: 10.1056/NEJM200004273421707. [DOI] [PubMed] [Google Scholar]
- 105.Bogdanos DP, Mieli-Vergani G, Vergani D. Non-organ-specific autoantibodies in children with chronic hepatitis C virus infection. Clin Infect Dis. 2004;38:1505; author reply 1505–1506. doi: 10.1086/383578. [DOI] [PubMed] [Google Scholar]
- 106.Bogdanos DP, Mieli-Vergani G, Vergani D. Non-organ-specific autoantibodies in hepatitis C virus infection: do they matter? Clin Infect Dis. 2005;40:508–510. doi: 10.1086/427293. [DOI] [PubMed] [Google Scholar]
- 107.Bogdanos DP, Mieli-Vergani G, Vergani D. Virus, liver and autoimmunity. Dig Liver Dis. 2000;32:440–446. doi: 10.1016/s1590-8658(00)80266-2. [DOI] [PubMed] [Google Scholar]
- 108.Leung PS, Rossaro L, Davis PA, Park O, Tanaka A, Kikuchi K, Miyakawa H, Norman GL, Lee W, Gershwin ME. Antimitochondrial antibodies in acute liver failure: implications for primary biliary cirrhosis. Hepatology. 2007;46:1436–1442. doi: 10.1002/hep.21828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bogdanos DP, Liaskos C, Rigopoulou EI, Dalekos GN. Anti-mitochondrial antibodies in patients with systemic lupus erythematosus: revealing the unforeseen. Clin Chim Acta. 2006;373:183–184; author reply 185. doi: 10.1016/j.cca.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 110.Liaskos C, Bogdanos DP, Rigopoulou EI, Dalekos GN. Development of antimitochondrial antibodies in patients with autoimmune hepatitis: art of facts or an artifact? J Gastroenterol Hepatol. 2007;22:454–455. doi: 10.1111/j.1440-1746.2006.04751.x. [DOI] [PubMed] [Google Scholar]
- 111.Bernal W, Meda F, Ma Y, Bogdanos DP, Vergani D. Disease-specific autoantibodies in patients with acute liver failure: the King’s College London Experience. Hepatology. 2008;47:1096–1097; author reply 1097. doi: 10.1002/hep.22179. [DOI] [PubMed] [Google Scholar]
- 112.Butler P, Hamilton-Miller J, Baum H, Burroughs AK. Detection of M2 antibodies in patients with recurrent urinary tract infection using an ELISA and purified PBC specific antigens. Evidence for a molecular mimicry mechanism in the pathogenesis of primary biliary cirrhosis? Biochem Mol Biol Int. 1995;35:473–485. [PubMed] [Google Scholar]
- 113.Klein R, Wiebel M, Engelhart S, Berg PA. Sera from patients with tuberculosis recognize the M2a-epitope (E2-subunit of pyruvate dehydrogenase) specific for primary biliary cirrhosis. Clin Exp Immunol. 1993;92:308–316. doi: 10.1111/j.1365-2249.1993.tb03397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Gilburd B, Ziporen L, Zharhary D, Blank M, Zurgil N, Scheinberg MA, Guedes LH, Gershwin ME, Shoenfeld Y. Antimitochondrial (pyruvate dehydrogenase) antibodies in leprosy. J Clin Immunol. 1994;14:14–19. doi: 10.1007/BF01541171. [DOI] [PubMed] [Google Scholar]
- 115.Czaja AJ, Pfeifer KD, Decker RH, Vallari AS. Frequency and significance of antibodies to asialoglycoprotein receptor in type 1 autoimmune hepatitis. Dig Dis Sci. 1996;41:1733–1740. doi: 10.1007/BF02088738. [DOI] [PubMed] [Google Scholar]
- 116.Van Norstrand MD, Malinchoc M, Lindor KD, Therneau TM, Gershwin ME, Leung PS, Dickson ER, Homburger HA. Quantitative measurement of autoantibodies to recombinant mitochondrial antigens in patients with primary biliary cirrhosis: relationship of levels of autoantibodies to disease progression. Hepatology. 1997;25:6–11. doi: 10.1002/hep.510250103. [DOI] [PubMed] [Google Scholar]
- 117.Invernizzi P, Crosignani A, Battezzati PM, Covini G, De Valle G, Larghi A, Zuin M, Podda M. Comparison of the clinical features and clinical course of antimitochondrial antibody-positive and -negative primary biliary cirrhosis. Hepatology. 1997;25:1090–1095. doi: 10.1002/hep.510250507. [DOI] [PubMed] [Google Scholar]
- 118.Gregorio GV, McFarlane B, Bracken P, Vergani D, Mieli-Vergani G. Organ and non-organ specific autoantibody titres and IgG levels as markers of disease activity: a longitudinal study in childhood autoimmune liver disease. Autoimmunity. 2002;35:515–519. doi: 10.1080/0891693021000056721. [DOI] [PubMed] [Google Scholar]
- 119.Czaja AJ, Morshed SA, Parveen S, Nishioka M. Antibodies to single-stranded and double-stranded DNA in antinuclear antibody-positive type 1-autoimmune hepatitis. Hepatology. 1997;26:567–572. doi: 10.1002/hep.510260306. [DOI] [PubMed] [Google Scholar]
- 120.Treichel U, Gerken G, Rossol S, Rotthauwe HW, Meyer zum Buschenfelde KH, Poralla T. Autoantibodies against the human asialoglycoprotein receptor: effects of therapy in autoimmune and virus-induced chronic active hepatitis. J Hepatol. 1993;19:55–63. doi: 10.1016/s0168-8278(05)80176-x. [DOI] [PubMed] [Google Scholar]
- 121.Kanzler S, Weidemann C, Gerken G, Lohr HF, Galle PR, Meyer zum Buschenfelde KH, Lohse AW. Clinical significance of autoantibodies to soluble liver antigen in autoimmune hepatitis. J Hepatol. 1999;31:635–640. doi: 10.1016/s0168-8278(99)80342-0. [DOI] [PubMed] [Google Scholar]
- 122.Czaja AJ, Shums Z, Norman GL. Frequency and significance of antibodies to soluble liver antigen/liver pancreas in variant autoimmune hepatitis. Autoimmunity. 2002;35:475–483. doi: 10.1080/0891693021000054101. [DOI] [PubMed] [Google Scholar]
- 123.Abuaf N, Johanet C, Chretien P, Martini E, Soulier E, Laperche S, Homberg JC. Characterization of the liver cytosol antigen type 1 reacting with autoantibodies in chronic active hepatitis. Hepatology. 1992;16:892–898. doi: 10.1002/hep.1840160407. [DOI] [PubMed] [Google Scholar]
- 124.Muratori L, Cataleta M, Muratori P, Lenzi M, Bianchi FB. Liver/kidney microsomal antibody type 1 and liver cytosol antibody type 1 concentrations in type 2 autoimmune hepatitis. Gut. 1998;42:721–726. doi: 10.1136/gut.42.5.721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Rigopoulou EI, Davies ET, Bogdanos DP, Liaskos C, Mytilinaiou M, Koukoulis GK, Dalekos GN, Vergani D. Antimitochondrial antibodies of immunoglobulin G3 subclass are associated with a more severe disease course in primary biliary cirrhosis. Liver Int. 2007;27:1226–1231. doi: 10.1111/j.1478-3231.2007.01586.x. [DOI] [PubMed] [Google Scholar]
- 126.Invernizzi P, Podda M, Battezzati PM, Crosignani A, Zuin M, Hitchman E, Maggioni M, Meroni PL, Penner E, Wesierska-Gadek J. Autoantibodies against nuclear pore complexes are associated with more active and severe liver disease in primary biliary cirrhosis. J Hepatol. 2001;34:366–372. doi: 10.1016/s0168-8278(00)00040-4. [DOI] [PubMed] [Google Scholar]
- 127.Miyachi K, Hankins RW, Matsushima H, Kikuchi F, Inomata T, Horigome T, Shibata M, Onozuka Y, Ueno Y, Hashimoto E, et al. Profile and clinical significance of anti-nuclear envelope antibodies found in patients with primary biliary cirrhosis: a multicenter study. J Autoimmun. 2003;20:247–254. doi: 10.1016/s0896-8411(03)00033-7. [DOI] [PubMed] [Google Scholar]
- 128.Kerkar N, Choudhuri K, Ma Y, Mahmoud A, Bogdanos DP, Muratori L, Bianchi F, Williams R, Mieli-Vergani G, Vergani D. Cytochrome P4502D6(193-212): a new immunodominant epitope and target of virus/self cross-reactivity in liver kidney microsomal autoantibody type 1-positive liver disease. J Immunol. 2003;170:1481–1489. doi: 10.4049/jimmunol.170.3.1481. [DOI] [PubMed] [Google Scholar]
- 129.Wesierska-Gadek J, Penner E, Battezzati PM, Selmi C, Zuin M, Hitchman E, Worman HJ, Gershwin ME, Podda M, Invernizzi P. Correlation of initial autoantibody profile and clinical outcome in primary biliary cirrhosis. Hepatology. 2006;43:1135–1144. doi: 10.1002/hep.21172. [DOI] [PubMed] [Google Scholar]
- 130.Yang WH, Yu JH, Nakajima A, Neuberg D, Lindor K, Bloch DB. Do antinuclear antibodies in primary biliary cirrhosis patients identify increased risk for liver failure? Clin Gastroenterol Hepatol. 2004;2:1116–1122. doi: 10.1016/s1542-3565(04)00465-3. [DOI] [PubMed] [Google Scholar]
- 131.Vergani D, Mieli-Vergani G. The impact of autoimmunity on hepatocytes. Semin Liver Dis. 2007;27:140–151. doi: 10.1055/s-2007-979467. [DOI] [PubMed] [Google Scholar]
- 132.Bogdanos DP, Baum H, Sharma UC, Grasso A, Ma Y, Burroughs AK, Vergani D. Antibodies against homologous microbial caseinolytic proteases P characterise primary biliary cirrhosis. J Hepatol. 2002;36:14–21. doi: 10.1016/s0168-8278(01)00252-5. [DOI] [PubMed] [Google Scholar]
- 133.Longhi MS, Ma Y, Bogdanos DP, Cheeseman P, Mieli-Vergani G, Vergani D. Impairment of CD4(+)CD25(+) regulatory T-cells in autoimmune liver disease. J Hepatol. 2004;41:31–37. doi: 10.1016/j.jhep.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 134.Bogdanos DP, Baum H, Grasso A, Okamoto M, Butler P, Ma Y, Rigopoulou E, Montalto P, Davies ET, Burroughs AK, et al. Microbial mimics are major targets of crossreactivity with human pyruvate dehydrogenase in primary biliary cirrhosis. J Hepatol. 2004;40:31–39. doi: 10.1016/s0168-8278(03)00501-4. [DOI] [PubMed] [Google Scholar]
- 135.Bogdanos DP, Baum H, Gunsar F, Arioli D, Polymeros D, Ma Y, Burroughs AK, Vergani D. Extensive homology between the major immunodominant mitochondrial antigen in primary biliary cirrhosis and Helicobacter pylori does not lead to immunological cross-reactivity. Scand J Gastroenterol. 2004;39:981–987. doi: 10.1080/00365520410003236. [DOI] [PubMed] [Google Scholar]
- 136.Bogdanos DP, Baum H, Okamoto M, Montalto P, Sharma UC, Rigopoulou EI, Vlachogiannakos J, Ma Y, Burroughs AK, Vergani D. Primary biliary cirrhosis is characterized by IgG3 antibodies cross-reactive with the major mitochondrial autoepitope and its Lactobacillus mimic. Hepatology. 2005;42:458–465. doi: 10.1002/hep.20788. [DOI] [PubMed] [Google Scholar]
- 137.Bogdanos DP, Choudhuri K, Vergani D. Molecular mimicry and autoimmune liver disease: virtuous intentions, malign consequences. Liver. 2001;21:225–232. doi: 10.1034/j.1600-0676.2001.021004225.x. [DOI] [PubMed] [Google Scholar]
- 138.Bogdanos DP, Koutsoumpas A, Baum H, Vergani D. Borrelia Burgdorferi: a new self-mimicking trigger in primary biliary cirrhosis. Dig Liver Dis. 2006;38:781–782; author reply 782-783. doi: 10.1016/j.dld.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 139.Bogdanos DP, McFarlane IG. Cytochrome P450 2A6 meets P450 2D6: an enigma of viral infections and autoimmunity. J Hepatol. 2003;39:860–863. doi: 10.1016/s0168-8278(03)00417-3. [DOI] [PubMed] [Google Scholar]
- 140.Bogdanos DP, Pares A, Baum H, Caballeria L, Rigopoulou EI, Ma Y, Burroughs AK, Rodes J, Vergani D. Disease-specific cross-reactivity between mimicking peptides of heat shock protein of Mycobacterium gordonae and dominant epitope of E2 subunit of pyruvate dehydrogenase is common in Spanish but not British patients with primary biliary cirrhosis. J Autoimmun. 2004;22:353–362. doi: 10.1016/j.jaut.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 141.Bogdanos DP, Rigopoulou EI. Viral/self-mimicry and immunological cross-reactivity as a trigger of hepatic C virus associated autoimmune diabetes. Diabetes Res Clin Pract. 2007;77:155–156. doi: 10.1016/j.diabres.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 142.Bogdanos DP, Vergani D. Origin of cross-reactive autoimmunity in primary biliary cirrhosis. Liver Int. 2006;26:633–635. doi: 10.1111/j.1478-3231.2006.01291.x. [DOI] [PubMed] [Google Scholar]
- 143.Xu L, Shen Z, Guo L, Fodera B, Keogh A, Joplin R, O’Donnell B, Aitken J, Carman W, Neuberger J, et al. Does a betaretrovirus infection trigger primary biliary cirrhosis? Proc Natl Acad Sci USA. 2003;100:8454–8459. doi: 10.1073/pnas.1433063100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Mackay IR. The etiopathogenesis of autoimmunity. Semin Liver Dis. 2005;25:239–250. doi: 10.1055/s-2005-916330. [DOI] [PubMed] [Google Scholar]
- 145.Selmi C, Balkwill DL, Invernizzi P, Ansari AA, Coppel RL, Podda M, Leung PS, Kenny TP, Van De Water J, Nantz MH, et al. Patients with primary biliary cirrhosis react against a ubiquitous xenobiotic-metabolizing bacterium. Hepatology. 2003;38:1250–1257. doi: 10.1053/jhep.2003.50446. [DOI] [PubMed] [Google Scholar]
- 146.Vergani D, Mieli-Vergani G, Mondelli M, Portmann B, Eddleston AL. Immunoglobulin on the surface of isolated hepatocytes is associated with antibody-dependent cell-mediated cytotoxicity and liver damage. Liver. 1987;7:307–315. doi: 10.1111/j.1600-0676.1987.tb00361.x. [DOI] [PubMed] [Google Scholar]
- 147.Duchini A, McHutchison JG, Pockros PJ. LKM-positive autoimmune hepatitis in the western United States: a case series. Am J Gastroenterol. 2000;95:3238–3241. doi: 10.1111/j.1572-0241.2000.03207.x. [DOI] [PubMed] [Google Scholar]
- 148.Tan EM, Smolen JS, McDougal JS, Fritzler MJ, Gordon T, Hardin JA, Kalden JR, Lahita RG, Maini RN, Reeves WH, et al. A critical evaluation of enzyme immunoassay kits for detection of antinuclear autoantibodies of defined specificities. II. Potential for quantitation of antibody content. J Rheumatol. 2002;29:68–74. [PubMed] [Google Scholar]
- 149.Fritzler MJ, Wiik A, Tan EM, Smolen JS, McDougal JS, Chan EK, Gordon TP, Hardin JA, Kalden JR, Lahita RG, et al. A critical evaluation of enzyme immunoassay kits for detection of antinuclear autoantibodies of defined specificities. III. Comparative performance characteristics of academic and manufacturers’ laboratories. J Rheumatol. 2003;30:2374–2381. [PubMed] [Google Scholar]
- 150.Fritzler MJ, Wiik A, Fritzler ML, Barr SG. The use and abuse of commercial kits used to detect autoantibodies. Arthritis Res Ther. 2003;5:192–201. doi: 10.1186/ar782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Rondeel JM, van Gelder W, van der Leeden H, Dinkelaar RB. Different strategies in the laboratory diagnosis of autoimmune disease: immunofluorescence, enzyme-linked immunosorbent assay or both? Ann Clin Biochem. 1999;36(Pt 2):189–195. doi: 10.1177/000456329903600209. [DOI] [PubMed] [Google Scholar]
- 152.Kerkar N, Ma Y, Davies ET, Cheeseman P, Mieli-Vergani G, Vergani D. Detection of liver kidney microsomal type 1 antibody using molecularly based immunoassays. J Clin Pathol. 2002;55:906–909. doi: 10.1136/jcp.55.12.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Bogdanos DP, Gilbert D, Bianchi I, Leoni S, Mitry RR, Ma Y, Mieli-Vergani G, Vergani D. Antibodies to soluble liver antigen and alpha-enolase in patients with autoimmune hepatitis. J Autoimmune Dis. 2004;1:4. doi: 10.1186/1740-2557-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Bogdanos DP, Vergani D, Muratori P, Muratori L, Bianchi FB. Specificity of anti-sp100 antibody for primary biliary cirrhosis. Scand J Gastroenterol. 2004;39:405–406; author reply 407. doi: 10.1080/00365520310008412. [DOI] [PubMed] [Google Scholar]


