Abstract
Gastrointestinal involvement of endometriosis has been found in 3%-37% of menstruating women and exclusive localization on the ileum is very rare (1%-7%). Endometriosis of the distal ileum is an infrequent cause of intestinal obstruction, ranging from 7% to 23% of all cases with intestinal involvement. We report a case in which endometrial infiltration of the small bowel caused acute obstruction requiring emergency surgery, in a woman whose symptoms were not related to menses. Histology of the resected specimen showed that endometriosis was mainly prevalent in the muscularis propria and submucosa and that the mucosa was not ulcerated but had inflammation and glandular alteration. Endometrial lymph node involvement, with a cystic glandular pattern was also detected.
Keywords: Endometriosis, Small bowel, Ileum, Obstruction, Abdominal pain, Intestinal resection
INTRODUCTION
Endometriosis is characterized by the presence of functional endometrial tissue consisting of glands and/or stroma located outside the uterus[1]. It is a painful chronic disease occurring in 5%-15% of menstruating women[1–3].
The reported prevalence of endometriosis is 1%-20% in asymptomatic women, 10%-25% in infertile patients and 60%-70% in women with chronic pelvic pain[4,5].
Endometriosis can be divided into intra- and extra-peritoneal sites. In decreasing order of frequency, the intra-peritoneal locations are ovaries (30%), uterosacral and large ligaments (18%-24%), fallopian tubes (20%), pelvic peritoneum, pouch of Douglas, and gastrointestinal (GI) tract. Extra-peritoneal locations include cervical portio (0.5%), vagina and rectovaginal septum, round ligament and inguinal hernia sac (0.3%-0.6%), navel (1%), abdominal scars after gynaecological surgery (1.5%) and caesarian section (0.5%). Endometriosis rarely affects extra-abdominal organs such as the lungs, urinary system, skin and the central nervous system[6–9].
GI involvement of endometriosis has been found in 3%-37% of women, most commonly in the sigmoid colon, rectum and terminal ileum[10–13].
We report a case in which endometrial infiltration of the small bowel caused acute obstruction, requiring emergency surgery. Diagnosis of ileal endometriosis was made by pathological examination of the resected specimen.
CASE REPORT
A 44-year old woman was referred to our unit because of diffuse abdominal pain, associated with diarrhoea alternating with constipation.
The patient began complaining of mild abdominal discomfort nine months earlier. Episodes of pain relapsed irregularly, lasted a few hours and were not related to menses. She had two normal labors at the age of 30 and 32 years, regular menses and no history of dyspareunia. No other symptoms were present. Her past medical history was unremarkable.
Three months earlier, evaluation by her primary care physician revealed normal blood tests, and an abdominal ultrasound examination was unremarkable. Faecal analysis was negative for both parasites and occult blood. Antispasmodic drugs were administered, but the patient experienced a progressive worsening of the cramping abdominal pain and the onset of constipation.
Physical examination showed mild diffuse abdominal tenderness. No abdominal masses or enlarged lymph nodes were noted. Auscultation detected an increase of bowel sounds and peristaltic rushes. Colonoscopy and abdominal computed tomography (CT) scan were planned. However, 48 h later, the patient required emergency admission for small bowel occlusion. Abdominal X-ray examination showed dilated loops of the small intestine with no air in the colon, and CT scan revealed an irregular mass involving the ileum with dilation of the small intestine. A colonoscopy was performed to refine the diagnosis. The colon was normal, but the ileum, at about 5 cm from the ileocecal valve, showed a tight extrinsic compression with intact mucosa.
Surgery was immediately carried out and an obstructing mass 5 cm in length involving the distal ileum was detected, with diffuse dilation of the small intestine. A right hemicolectomy with resection of 25 cm of ileum was performed. There was no evidence of macroscopic lesions in other abdominal and pelvic organs. The post-operative course was uneventful and the patient left the hospital 9 d later.
Histology of the resected specimen showed endometriosis involving the ileum and causing a stricture. The bowel wall was infiltrated, but the mucosa was not ulcerated. Endometriosis was mainly prevalent in the muscularis propria and submucosa. The mucosal involvement showed inflammation and glandular alteration (Figure 1). Immunocytochemistry with cytokeratin (CK) of different molecular weight (CK7 and CK20) was performed. Endometrioid glands and the intestinal epithelium were positive for CK7 and CK20, respectively (Figure 2). Endometrial lymph node involvement, with a cystic glandular pattern, was also detected (Figure 3).
Figure 1.
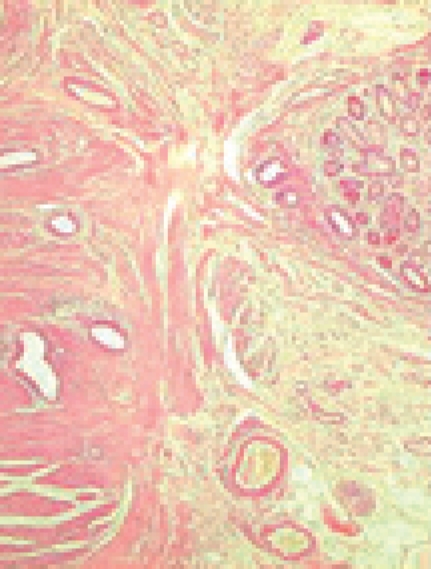
Histology of ileal wall showing endometrial tissue in the muscular layer, with foci of mucosal involvement.
Figure 2.
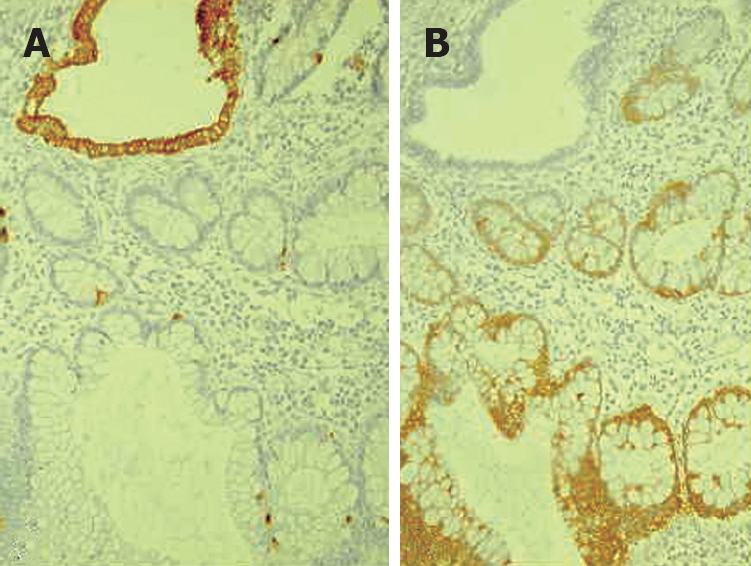
Histopathology showing CK20 immunostaining of intestinal epithelium (A) and CK 7 immunostaining of endometrioid glands (B).
Figure 3.
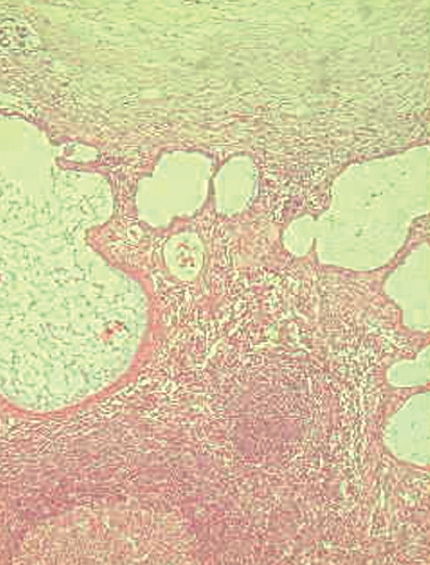
Endometriosis involving lymph nodes with a cystic glandular pattern.
DISCUSSION
Endometriosis is a common disease of unknown etiology. Many theories have been proposed to explain this condition. The most widely accepted is Sampson’s retrograde menstruation theory: during menstruation, endometrial tissue refluxes through the fallopian tubes, implanting and growing on the serosal surface of abdominal and pelvic organs[14,15].
Alternatively, extrauterine growth of endometriotic tissue could occur as a result of metaplastic transformation of pluripotential peritoneal mesothelium (Minh’s theory)[16].
Another theory implies the migration of cells through the lymphatic system or via hematogenous spread[17]. Donnez et al[18] hypothesized that endometrial nodules may develop from metaplasia of mullerian remnants. In some cases, they could result from iatrogenic displacement of the decidua during a caesarean section[19].
The “neurologic hypothesis” is a new concept in the pathogenesis of endometriosis: the lesions seem to infiltrate the large bowel wall along the nerves, at a distance from the primary lesion[20]. However, other factors, immunological, genetic and familial, could be involved in the pathogenesis of this disease[21–23].
Endometriosis usually becomes apparent in the reproductive years when the lesions are stimulated by ovarian hormones. Forty percent of the patients present symptoms in a cyclic manner, which are usually related with menses[24]. In our patient, symptoms relapsed irregularly and were not related with menses.
At present, superficial endometriosis is considered a normal phenomenon in women at the childbearing age, whereas deep infiltrative endometriosis (DIE) and endometrial ovarian cysts are the severe and painful manifestations of the condition[25]. DIE occurs in 30%-40% of the patients with endometriosis[26].
Pelvic pain, infertility and dyspareunia are the characteristic symptoms of the disease[25], but the clinical presentation is often non-specific.
Extra-pelvic endometriosis affects the GI tract of 5% of women with this condition[27]. The rectosigmoid is the most common site for intestinal endometriosis, accounting for 70% of all cases, while small bowel involvement, usually confined to the distal ileum, is less frequent (1%-7%) and exclusive localization on the ileum is very rare (1%-7%)[13]. Different incidence rates of endometriosis at different sites may be due to the fact that endometriosis is often an incidental finding at surgery[9].
In a review of 1000 women who underwent laparotomy for gynecological symptoms, Jubanyik et al[28] described 181 (18%) cases of GI endometriosis, but only one patient had small bowel involvement. Melody et al[29] reported distal ileum involvement in 35 out of 36 patients. In a radiologic study, Scarmato et al[30] detected endometriosis of the terminal and mid-ileum in four patients and one patient, respectively. Endometriosis in the jejunum[31] and proximal ileum has also been documented[32]. Anaf et al[20], considering bowel endometriosis an “infiltration or invasion phenomenon”, found that there is a histological continuity between the superficial and underlying deep lesions of the large bowel wall, suggesting that lesions originating from the serosa progressively invade the muscularis propria. The mucosa is rarely involved as it is poorly innervated. Pelvic, pericolonic and para-aortic lymph node involvement of endometriosis has also been reported, often coexisting with endometriosis of the bowel wall[33]. Lymph node involvement may be a consequence of lymphatic dissemination from endometrial foci in the intestinal wall[34,35].
Symptoms are initially cyclical but may become permanent when the lesions progress.
It is difficult to establish a preoperative diagnosis of GI endometriosis, because GI tract symptoms can mimic a wide spectrum of diseases, including irritable bowel syndrome, infectious diseases, ischemic enteritis/colitis, inflammatory bowel disease and neoplasm[10,30,36,37]. GI endometriosis patients present with relapsing bouts of abdominal pain, abdominal distention, tenesmus, constipation and diarrhoea[9]. Rectal bleeding and pain during defecation may also occur[38].
Endometriosis infiltrating the muscularis propria may lead to localized fibrosis in the bowel wall, strictures, and small or large bowel obstruction[9,10].
The true incidence of endometriosis causing bowel obstruction is unknown[11], although complete obstruction of the bowel lumen occurs in less than 1% of cases[39].
Endometriosis of the distal ileum is an infrequent cause of intestinal obstruction, ranging from 7% to 23% of all cases with intestinal involvement[31,33,40,41].
The incidence of intestinal resection for bowel obstruction is 0.7% among patients undergone surgical treatment for abdominopelvic endometriosis[39].
In our case, as in others previously reported in the literature, it was impossible to establish a timely and accurate preoperative diagnosis for the vagueness of symptoms, similar to other cases of bowel obstruction.
However, endometriosis of the small bowel should be suspected in young, nulliparous patients with abdominal pain, in conjunction with signs of obstruction[12]. Mussa et al[42] reported a case of small bowel endometriosis with intestinal obstruction, protein-losing enteropathy and anasarca. Wong et al[43] described a case of endometriosis of the small bowel mimicking pancreatitis.
Rarely, intestinal endometriosis may occur with perforation[44,45]. Malignancy has been reported in 0.7%-1% of patients and 78.7% of the cases occur in the ovary[46]. The colorectum is involved in only 5% of patients[47].
The differential histologic diagnosis of endometrioid adenocarcinoma (AC) and colonic AC is difficult because colonic AC has a significant mucosal component, while endometrioid AC usually involves the outer layers of the colon[45,47,48]. Immunohistochemical staining for CK7 and CK20 seems to be useful in differentiating colonic and endometrioid AC[49,50]. Approximately, 75%-95% of primary colonic AC cases have a CK7-negative and CK20-positive phenotype, whereas 80%-100% of endometrial AC cases have a CK7-positive and CK20-negative phenotype[50]. Although endoscopic diagnosis of colonic endometriosis has been reported[51], the mucosa is usually normal or shows minimal mucosal abnormalities[45,47,48], friability[52], extrinsic process or fibrosed stenoses[53].
Rectal bleeding may be caused by mucosal injury during the passage of stools through a stenosed colon with the intramural endometriotic tissue increased at the time of menses if it occurs. Colonic mucosa heals rapidly and no signs are detectable at endoscopy[54].
Endoscopic biopsies usually yield insufficient tissue for a definitive pathologic diagnosis as endometriosis involves the deep layers of the bowel wall. Endometriosis can induce mucosal changes without any specific pattern, which mimic findings of other diseases such as inflammatory bowel disease, ischemic colitis or neoplasm[55].
Radiologically, lesions of endometriosis are either of constricting and polypoid type or both[54]. On barium studies, radiographic findings caused by implants in the ileum are similar to those in the colon. Rectosigmoid or cecal endometriosis on double contrast barium enema studies is seen as an extrinsic mass with spiculation and tethering of folds[30,56].
The diagnosis of endometriosis may be suspected on the basis of the clinical history[30]. Less than 50% of patients have concurrent pelvic endometriosis[57].
CT is not the primary imaging modality for evaluation of bowel endometriosis, although it can occasionally demonstrate a stenosing rectosigmoid mass[58].
Multislice CT (MSCT) has a great potential for detecting alterations in the intestinal wall, especially if it is combined with enteroclysis (MSCTe). Biscaldi et al[59] carried out a study on 98 women with symptoms suggestive of colorectal endometriosis and MSCTe identified 94.8% of bowel endometriotic nodules.
Magnetic resonance imaging (MRI) has a high sensitivity (77%-93%) in the diagnosis of bowel endometriosis[60,61].
The depth of rectal wall infiltration by endometriosis is poorly defined by MRI. A combination of MRI and rectal endoscopic ultrasonography (EUS) has recently been proposed[62]. When retroperitoneal infiltration is present, it is mandatory to know if the bowel wall is involved in order to identify patients requiring bowel resection.
Both rectal EUS sensitivity and negative predictive value range from 92% to 100%. The specificity and positive predictive value are rather poor, which are 66% and 64%, 83% and 94%, respectively, as reported in two different studies[63,64].
There is a great interest in the use of serum markers to diagnose endometriosis, but they are not sufficiently accurate for use in clinical practice[65].
Cancer antigen CA-125 has been used to monitor the progress of endometriosis[66]. CA19-9 has a lower sensitivity than CA-125, and cytokine interleukin-6 may be more sensitive and specific than CA-125.
Surgery is the choice of treatment for intestinal endometriosis in most cases. For the accidental finding without symptoms of obstruction, hormone therapy with danazol or gonadotrophin-releasing hormone (GnRH) analogs may be considered[9]. Surgical treatment should be indicated for women with pain, bleeding, changes in bowel habits and intestinal obstruction[51]. In the small bowel, the treatment of endometriosis is surgical resection of the involved bowel, while medical therapy is only a temporary treatment[12].
Intestinal endometriosis may be active in the peri- and post- menopausal years and even surgery may be necessary for these patients[54].
In this paper, we report an unusual presentation of endometriosis characterized by abrupt onset of small bowel occlusion. The present report points out that endometriosis remains a challenging condition for clinicians, especially, as in our case, when the symptoms are not related to menses. Intestinal endometriosis should be considered in patients with epigastric, abdominal and/or pelvic pain, in conjunction with signs of obstruction.
Peer reviewers: Kazuma Fujimoto, Professor, Department of Internal Medicine, Saga Medical School, Nabeshima, Saga, Saga 849-8501, Japan; Amado S Peña, Professor, Department of Pathology, Immunogenetics, VU University Medical Centre, De Boelelaan 1117, PO Box 7057, Amsterdam 1007 MB, The Netherlands
S- Editor Li DL L- Editor Wang XL E- Editor Ma WH
References
- 1.Olive DL, Schwartz LB. Endometriosis. N Engl J Med. 1993;328:1759–1769. doi: 10.1056/NEJM199306173282407. [DOI] [PubMed] [Google Scholar]
- 2.Lu PY, Ory SJ. Endometriosis: current management. Mayo Clin Proc. 1995;70:453–463. doi: 10.4065/70.5.453. [DOI] [PubMed] [Google Scholar]
- 3.Keane TE, Peel AL. Endometrioma. An intra-abdominal troublemaker. Dis Colon Rectum. 1990;33:963–965. doi: 10.1007/BF02139106. [DOI] [PubMed] [Google Scholar]
- 4.Abrao MS, Podgaec S, Filho BM, Ramos LO, Pinotti JA, de Oliveira RM. The use of biochemical markers in the diagnosis of pelvic endometriosis. Hum Reprod. 1997;12:2523–2527. doi: 10.1093/humrep/12.11.2523. [DOI] [PubMed] [Google Scholar]
- 5.Pritts EA, Taylor RN. An evidence-based evaluation of endometriosis-associated infertility. Endocrinol Metab Clin North Am. 2003;32:653–667. doi: 10.1016/s0889-8529(03)00045-8. [DOI] [PubMed] [Google Scholar]
- 6.Bergqvist A. Different types of extragenital endometriosis: a review. Gynecol Endocrinol. 1993;7:207–221. doi: 10.3109/09513599309152504. [DOI] [PubMed] [Google Scholar]
- 7.Frackiewicz EJ, Zarotsky V. Diagnosis and treatment of endometriosis. Expert Opin Pharmacother. 2003;4:67–82. doi: 10.1517/14656566.4.1.67. [DOI] [PubMed] [Google Scholar]
- 8.Fox H, Buckley CH. Current concepts of endometriosis. Clin Obstet Gynaecol. 1984;11:279–287. [PubMed] [Google Scholar]
- 9.Lin YH, Kuo LJ, Chuang AY, Cheng TI, Hung CF. Extrapelvic endometriosis complicated with colonic obstruction. J Chin Med Assoc. 2006;69:47–50. doi: 10.1016/S1726-4901(09)70111-X. [DOI] [PubMed] [Google Scholar]
- 10.Yantiss RK, Clement PB, Young RH. Endometriosis of the intestinal tract: a study of 44 cases of a disease that may cause diverse challenges in clinical and pathologic evaluation. Am J Surg Pathol. 2001;25:445–454. doi: 10.1097/00000478-200104000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Paksoy M, Karabicak I, Ayan F, Aydogan F. Intestinal obstruction due to rectal endometriosis. Mt Sinai J Med. 2005;72:405–408. [PubMed] [Google Scholar]
- 12.Orbuch IK, Reich H, Orbuch M, Orbuch L. Laparoscopic treatment of recurrent small bowel obstruction secondary to ileal endometriosis. J Minim Invasive Gynecol. 2007;14:113–115. doi: 10.1016/j.jmig.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 13.Macafee CH, Greer HL. Intestinal endometriosis. A report of 29 cases and a survey of the literature. J Obstet Gynaecol Br Emp. 1960;67:539–555. doi: 10.1111/j.1471-0528.1960.tb09211.x. [DOI] [PubMed] [Google Scholar]
- 14.Quinn M. Endometriosis: the consequence of neurological dysfunction? Med Hypotheses. 2004;63:602–608. doi: 10.1016/j.mehy.2004.03.032. [DOI] [PubMed] [Google Scholar]
- 15.Witz CA. Current concepts in the pathogenesis of endometriosis. Clin Obstet Gynecol. 1999;42:566–585. doi: 10.1097/00003081-199909000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Minh HN, Smadja A, Orcel L. [An integrated histogenetic concept of internal and external endometriosis] J Gynecol Obstet Biol Reprod (Paris) 1986;15:29–35. [PubMed] [Google Scholar]
- 17.Audebert AJ. [External endometriosis: histogenesis, etiology and natural course] Rev Prat. 1990;40:1077–1081. [PubMed] [Google Scholar]
- 18.Donnez J, Spada F, Squifflet J, Nisolle M. Bladder endometriosis must be considered as bladder adenomyosis. Fertil Steril. 2000;74:1175–1181. doi: 10.1016/s0015-0282(00)01584-3. [DOI] [PubMed] [Google Scholar]
- 19.Luisi S, Gabbanini M, Sollazzi S, Calonaci F, Razzi S, Petraglia F. Surgical scar endometriosis after Cesarean section: a case report. Gynecol Endocrinol. 2006;22:284–285. doi: 10.1080/09513590600777578. [DOI] [PubMed] [Google Scholar]
- 20.Anaf V, El Nakadi I, Simon P, Van de Stadt J, Fayt I, Simonart T, Noel JC. Preferential infiltration of large bowel endometriosis along the nerves of the colon. Hum Reprod. 2004;19:996–1002. doi: 10.1093/humrep/deh150. [DOI] [PubMed] [Google Scholar]
- 21.Dmowski WP, Gebel HM, Rawlins RG. Immunologic aspects of endometriosis. Obstet Gynecol Clin North Am. 1989;16:93–103. [PubMed] [Google Scholar]
- 22.De Falco M, Ragusa M, Oliva G, Miranda A, Parmeggiani D, Sperlongano P, Accardo M, Calzolari F, Misso C, Monacelli M, Avenia N. Is extrauterine endometriosis confined to the gynecological sphere? A critical review of the experience in a general surgery unit. G Chir. 2007;28:83–92. [PubMed] [Google Scholar]
- 23.Moen MH, Magnus P. The familial risk of endometriosis. Acta Obstet Gynecol Scand. 1993;72:560–564. doi: 10.3109/00016349309058164. [DOI] [PubMed] [Google Scholar]
- 24.Badawy SZ, Freedman L, Numann P, Bonaventura M, Kim S. Diagnosis and management of intestinal endometriosis. A report of five cases. J Reprod Med. 1988;33:851–855. [PubMed] [Google Scholar]
- 25.Amaral VF, Ferriani RA, Sa MF, Nogueira AA, Rosa e Silva JC, Rosa e Silva AC, Moura MD. Positive correlation between serum and peritoneal fluid CA-125 levels in women with pelvic endometriosis. Sao Paulo Med J. 2006;124:223–227. doi: 10.1590/S1516-31802006000400010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cornillie FJ, Oosterlynck D, Lauweryns JM, Koninckx PR. Deeply infiltrating pelvic endometriosis: histology and clinical significance. Fertil Steril. 1990;53:978–983. doi: 10.1016/s0015-0282(16)53570-5. [DOI] [PubMed] [Google Scholar]
- 27.Prystowsky JB, Stryker SJ, Ujiki GT, Poticha SM. Gastrointestinal endometriosis. Incidence and indications for resection. Arch Surg. 1988;123:855–858. doi: 10.1001/archsurg.1988.01400310069011. [DOI] [PubMed] [Google Scholar]
- 28.Jubanyik KJ, Comite F. Extrapelvic endometriosis. Obstet Gynecol Clin North Am. 1997;24:411–440. doi: 10.1016/s0889-8545(05)70311-9. [DOI] [PubMed] [Google Scholar]
- 29.Melody GF. Endometriosis causing obstruction of the ileum. Obstet Gynecol. 1956;8:468–472. [PubMed] [Google Scholar]
- 30.Scarmato VJ, Levine MS, Herlinger H, Wickstrom M, Furth EE, Tureck RW. Ileal endometriosis: radiographic findings in five cases. Radiology. 2000;214:509–512. doi: 10.1148/radiology.214.2.r00fe35509. [DOI] [PubMed] [Google Scholar]
- 31.Martimbeau PW, Pratt JH, Gaffey TA. Small-bowel obstruction secondary to endometriosis. Mayo Clin Proc. 1975;50:239–243. [PubMed] [Google Scholar]
- 32.Rio FW, Edwards DL, Regan JF, Schmutzer KJ. Endometriosis of the small bowel. Arch Surg. 1970;101:403–405. doi: 10.1001/archsurg.1970.01340270051014. [DOI] [PubMed] [Google Scholar]
- 33.Cameron IC, Rogers S, Collins MC, Reed MW. Intestinal endometriosis: presentation, investigation, and surgical management. Int J Colorectal Dis. 1995;10:83–86. doi: 10.1007/BF00341202. [DOI] [PubMed] [Google Scholar]
- 34.Lorente Poyatos R, Palacios Perez A, Bravo Bravo F, Lopez Caballero FJ, Bouhmidi A, Huertas Nadal C, Ruiz Escolano E. Rectosigmoid endometriosis with lymph node involvement. Gastroenterol Hepatol. 2003;26:23–25. [PubMed] [Google Scholar]
- 35.Sheikh HA, Krishnamurti U, Bhat Y, Rajendiran S. A 42-year-old woman with a 7-month history of abdominal pain. A, endometriosis involving ileocecal junction and 2 pericolonic lymph nodes; B, intranodal benign glandular inclusions. Arch Pathol Lab Med. 2005;129:e218–e221. doi: 10.5858/2005-129-e218-AYWWAM. [DOI] [PubMed] [Google Scholar]
- 36.Cappell MS, Friedman D, Mikhail N. Endometriosis of the terminal ileum simulating the clinical, roentgenographic, and surgical findings in Crohn's disease. Am J Gastroenterol. 1991;86:1057–1062. [PubMed] [Google Scholar]
- 37.Dimoulios P, Koutroubakis IE, Tzardi M, Antoniou P, Matalliotakis IM, Kouroumalis EA. A case of sigmoid endometriosis difficult to differentiate from colon cancer. BMC Gastroenterol. 2003;3:18. doi: 10.1186/1471-230X-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Conio M, Buscarini E, Blanchi S, Lapertosa G, Zambelli A. Sigmoid endometriosis. Gastrointest Endosc. 2004;60:434–435. doi: 10.1016/s0016-5107(04)01701-8. [DOI] [PubMed] [Google Scholar]
- 39.de Bree E, Schoretsanitis G, Melissas J, Christodoulakis M, Tsiftsis D. Acute intestinal obstruction caused by endome-triosis mimicking sigmoid carcinoma. Acta Gastroenterol Belg. 1998;61:376–378. [PubMed] [Google Scholar]
- 40.Riaz N, Khurshaidi N. Acute small bowel obstruction secondary to ileal endometrioma. J Coll Physicians Surg Pak. 2007;17:228–229. [PubMed] [Google Scholar]
- 41.Ridha JR, Cassaro S. Acute small bowel obstruction secondary to ileal endometriosis: report of a case. Surg Today. 2003;33:944–947. doi: 10.1007/s00595-003-2613-4. [DOI] [PubMed] [Google Scholar]
- 42.Mussa FF, Younes Z, Tihan T, Lacy BE. Anasarca and small bowel obstruction secondary to endometriosis. J Clin Gastroenterol. 2001;32:167–171. doi: 10.1097/00004836-200102000-00017. [DOI] [PubMed] [Google Scholar]
- 43.Wong LS, Mahendrakumar R, Bullen BR. Small-bowel endometriosis masquerading as pancreatitis. J R Soc Med. 1999;92:17–18. doi: 10.1177/014107689909200106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Varras M, Kostopanagiotou E, Katis K, Farantos CH, Angelidou-Manika Z, Antoniou S. Endometriosis causing extensive intestinal obstruction simulating carcinoma of the sigmoid colon: a case report and review of the literature. Eur J Gynaecol Oncol. 2002;23:353–357. [PubMed] [Google Scholar]
- 45.Yantiss RK, Clement PB, Young RH. Endometriosis of the intestinal tract: a study of 44 cases of a disease that may cause diverse challenges in clinical and pathologic evaluation. Am J Surg Pathol. 2001;25:445–454. doi: 10.1097/00000478-200104000-00003. [DOI] [PubMed] [Google Scholar]
- 46.Heaps JM, Nieberg RK, Berek JS. Malignant neoplasms arising in endometriosis. Obstet Gynecol. 1990;75:1023–1028. [PubMed] [Google Scholar]
- 47.Chen KT. Endometrioid adenocarcinoma arising from colonic endometriosis mimicking primary colonic carcinoma. Int J Gynecol Pathol. 2002;21:285–288. doi: 10.1097/00004347-200207000-00014. [DOI] [PubMed] [Google Scholar]
- 48.Zanetta GM, Webb MJ, Li H, Keeney GL. Hyperestrogenism: a relevant risk factor for the development of cancer from endometriosis. Gynecol-Oncol. 2000;79:18–22. doi: 10.1006/gyno.2000.5905. [DOI] [PubMed] [Google Scholar]
- 49.Han AC, Hovenden S, Rosenblum NG, Salazar H. Adenocarcinoma arising in extragonadal endometriosis: an immunohistochemical study. Cancer. 1998;83:1163–1169. [PubMed] [Google Scholar]
- 50.Chu P, Wu E, Weiss LM. Cytokeratin 7 and cytokeratin 20 expression in epithelial neoplasms: a survey of 435 cases. Mod Pathol. 2000;13:962–972. doi: 10.1038/modpathol.3880175. [DOI] [PubMed] [Google Scholar]
- 51.Bozdech JM. Endoscopic diagnosis of colonic endometriosis. Gastrointest Endosc. 1992;38:568–570. doi: 10.1016/s0016-5107(92)70518-5. [DOI] [PubMed] [Google Scholar]
- 52.Averbach M, Abrao MS, Podgaec S, Correa P. Rectal endometriosis. Gastrointest Endosc. 2005;62:978–979; discussion 979. doi: 10.1016/j.gie.2005.07.054. [DOI] [PubMed] [Google Scholar]
- 53.Korber J, Grammel S, Lobeck H, Weidemann H. [Stenosis of the terminal ileum. Endometriosis as the differential diagnosis of Crohn's disease] Dtsch Med Wochenschr. 1997;122:926–929. doi: 10.1055/s-2008-1047710. [DOI] [PubMed] [Google Scholar]
- 54.Bartkowiak R, Zieniewicz K, Kaminski P, Krawczyk M, Marianowski L, Szymanska K. Diagnosis and treatment of sigmoidal endometriosis--a case report. Med Sci Monit. 2000;6:787–790. [PubMed] [Google Scholar]
- 55.Langlois NE, Park KG, Keenan RA. Mucosal changes in the large bowel with endometriosis: a possible cause of misdiagnosis of colitis? Hum Pathol. 1994;25:1030–1034. doi: 10.1016/0046-8177(94)90061-2. [DOI] [PubMed] [Google Scholar]
- 56.Gordon RL, Evers K, Kressel HY, Laufer I, Herlinger H, Thompson JJ. Double-contrast enema in pelvic endometriosis. AJR Am J Roentgenol. 1982;138:549–552. doi: 10.2214/ajr.138.3.549. [DOI] [PubMed] [Google Scholar]
- 57.Croom RD 3rd, Donovan ML, Schwesinger WH. Intestinal endometriosis. Am J Surg. 1984;148:660–667. doi: 10.1016/0002-9610(84)90347-7. [DOI] [PubMed] [Google Scholar]
- 58.Fishman EK, Scatarige JC, Saksouk FA, Rosenshein NB, Siegelman SS. Computed tomography of endometriosis. J Comput Assist Tomogr. 1983;7:257–264. doi: 10.1097/00004728-198304000-00010. [DOI] [PubMed] [Google Scholar]
- 59.Biscaldi E, Ferrero S, Fulcheri E, Ragni N, Remorgida V, Rollandi GA. Multislice CT enteroclysis in the diagnosis of bowel endometriosis. Eur Radiol. 2007;17:211–219. doi: 10.1007/s00330-006-0364-5. [DOI] [PubMed] [Google Scholar]
- 60.Bazot M, Darai E, Hourani R, Thomassin I, Cortez A, Uzan S, Buy JN. Deep pelvic endometriosis: MR imaging for diagnosis and prediction of extension of disease. Radiology. 2004;232:379–389. doi: 10.1148/radiol.2322030762. [DOI] [PubMed] [Google Scholar]
- 61.Takeuchi H, Kuwatsuru R, Kitade M, Sakurai A, Kikuchi I, Shimanuki H, Kinoshita K. A novel technique using magnetic resonance imaging jelly for evaluation of rectovaginal endometriosis. Fertil Steril. 2005;83:442–447. doi: 10.1016/j.fertnstert.2004.08.021. [DOI] [PubMed] [Google Scholar]
- 62.Roseau G, Dumontier I, Palazzo L, Chapron C, Dousset B, Chaussade S, Dubuisson JB, Couturier D. Rectosigmoid endometriosis: endoscopic ultrasound features and clinical implications. Endoscopy. 2000;32:525–530. doi: 10.1055/s-2000-9008. [DOI] [PubMed] [Google Scholar]
- 63.Delpy R, Barthet M, Gasmi M, Berdah S, Shojai R, Desjeux A, Boubli L, Grimaud JC. Value of endorectal ultrasonography for diagnosing rectovaginal septal endometriosis infiltrating the rectum. Endoscopy. 2005;37:357–361. doi: 10.1055/s-2005-861115. [DOI] [PubMed] [Google Scholar]
- 64.Camagna O, Dhainaut C, Dupuis O, Soncini E, Martin B, Palazzo L, Chosidow D, Madelenat P. [Surgical management of rectovaginal septum endometriosis from a continuous series of 50 cases] Gynecol Obstet Fertil. 2004;32:199–209. doi: 10.1016/j.gyobfe.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 65.Mounsey AL, Wilgus A, Slawson DC. Diagnosis and management of endometriosis. Am Fam Physician. 2006;74:594–600. [PubMed] [Google Scholar]
- 66.Bedaiwy MA, Falcone T. Laboratory testing for endometriosis. Clin Chim Acta. 2004;340:41–56. doi: 10.1016/j.cccn.2003.10.021. [DOI] [PubMed] [Google Scholar]


