Abstract
Ischemic colitis is an uncommon complication in patients with systemic lupus erythematosus (SLE). In previously reported cases of colitis caused by SLE, intestinal vasculitis is implicated as the causative process, but is rarely confirmed histologically. We described a case of a 32-year-old man with increased activity of SLE, who presented with hematochezia and abdominal pain due to ischemic colitis with small vessel vasculitis which was proven by sigmoidoscopic biopsy. The clinical course of the patient was improved after steroid and conservative management.
Keywords: Systemic lupus erythematosus, Ischemic colitis, Vasculitis
INTRODUCTION
Ischemic colitis, an acute abdominal disease, is caused by various predisposing factors. Although patients with connective tissue disorders, such as systemic lupus erythematosus (SLE), are at risk for various forms of colonic ischemia due to impairment of small vessel circulation to the large bowel caused by widespread vasculitis, ischemic colitis is an uncommon gastrointestinal complication in patients with SLE[1–8]. We report a case of ischemic colitis associated with intestinal vasculitis and presented with increased SLE activity.
CASE REPORT
A 32-year-old male with a history of SLE was admitted to our department due to a two-day history of abdominal pain and bloody stool. He was diagnosed as having SLE. He had received cyclophosphamide and steroid, had been in clinical remission since last 13 mo. At 3 mo before admission, immunologic tests showed stable SLE disease activity. On the day of admission, the vital signs were normal except for body temperature of 37.8°C. Physical examination revealed mild tenderness of the left lower abdomen but no peritoneal signs or organomegaly. Initial laboratory test results were as follows: white blood cell count, 8.7 × 109/L (normal, 4.5 × 109/L-10.5 × 109/L); hemoglobin, 14.7 g/dL; platelet count, 195 × 109/L (normal, 150 × 109/L-350 × 109/L); blood urea nitrogen, 27 mg/dL; creatinine, 1.1 mg/dL.The results of electrolytes and coagulation were normal. Immunologic test showed increased activity of SLE: ESR, 48 mm/h (normal, 0-20 mm/h); CRP, 6.79 mg/dL (normal, 0-0.3 mg/dL); antinuclear antibody (ANA), a titer of 1:200 (normal, < 1:50); C3, 108 mg/dL (normal, 84-151 mg/dL); C4, 23 mg/dL (normal, 17-40 mg/dL), antiphospholipid antibody, 2.0 U/mL (normal, < 10 U/mL); anti-Smith antibody, positive; anti-double stranded DNA antibody, 43.91 IU/mL (normal, < 5.30 IU/mL). Flexible sigmoidoscopy demonstrated severe inflammation of the mucosa extending from rectosigmoid junction to the splenic flexure, with contact bleeding and irregularly shaped ulceration (Figure 1). Rectum appeared relatively free from disease. Biopsy specimens from the sigmoid colon revealed inflammatory cell infiltration and hemorrhage in the mucosa, and small vessel wall thickening with lymphocyte infiltration, and vasculitis was considered (Figure 2). An ischemic colitis with increased SLE activity was confirmed and conservative management was done with fluids, intravenous antibiotics and intravenous steroid therapy. Clinical improvement was observed over the next three days, with stopped bloody stool and loss of abdominal pain. On the seventh day, follow-up flexible sigmoidoscopy demonstrated marked improvement of inflammation and ulceration in the sigmoid colon. On the ninth day, the patient was discharged.
Figure 1.
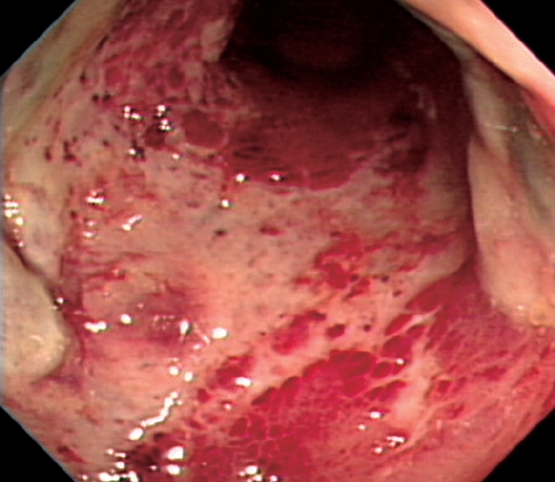
Sigmoidoscopy shows the severe erythematous friable mucosa and diffuse ulceration with dirty exudates.
Figure 2.
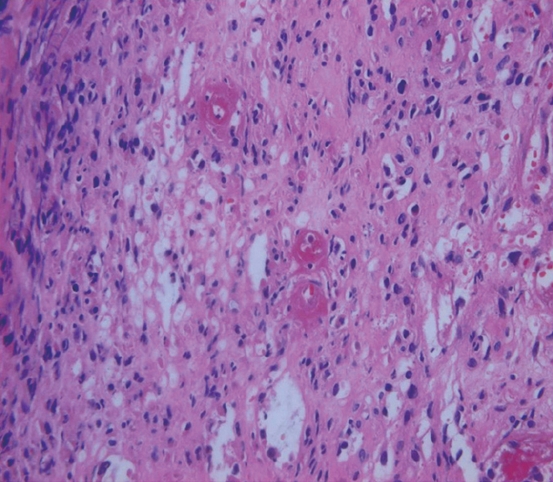
Microscopy of colon biopsies shows the thickening of small vessel wall and lymphocyte infiltration around vessels (HE, × 400).
DISCUSSION
The development of ischemic colitis in patients with SLE is an uncommon complication[1–8]. But widespread fibrinoid vasculitis, typical of SLE, is thought to be a likely predisposing factor[1]. If this vasculitis involves the colon, ischemic colitis occurs. Gastrointestinal vasculitis is one of the most serious complications of SLE, even though the occurrence of colonic lesions is rare (0.2%)[4–6]. The gastrointestinal vasculitis of SLE is consequence of tissue damage from vasculopathy mediated by immune complexes, and has been associated with SLE activity[4,5]. There are no pathognomic and histopathologic findings in SLE; however, pathologic changes associated with gastrointestinal vasculitis occur in the small vessels of the intestinal wall rather than in medium-sized mesenteric arteries[4,6]. Ischemic colitis in patients with SLE is caused by decreased blood perfusion of mesenteric vasculatures. The predisposing factors are embolism, thrombosis, vasospasm, drugs (steroids and immunosuppressive agents), vasculitis, performed colonoscopy, and enema[1,7,8]. Management of abdominal manifestations of SLE, in the absence of compelling radiographic or clinical findings suggestive of infarction or perforation, are steroid, antibiotics, and fluid therapy[2].
The present case reveals ischemic change of edematous, erythematous mucosa and ulcerations with normal mucosa except for lesions on flexible sigmoidoscopy[9,10]. Even though the patient has received immunosuppressive agents, he had stable disease activity during last 13 mo without using immunosuppressant or steroid and no procedure, such as colonoscopy or enema has been performed. Comparing with previous laboratory findings, several tests concerned with SLE disease activity demonstrated increased activity; elevated ESR, elevated CRP, positive antinuclear antibody, elevated anti-double strand DNA antibody. Under this condition, we could diagnose ischemic colitis associated with increased SLE activity and vasculitis by histopathology. Generally, a typical pattern of vasculitis is quite difficult to prove by endoscopic biopsy[11]. Therefore, some literature used the term “lupus enteritis’ rather than “gastrointestinal vasculitis” in SLE patients[5].
In conclusion, the present case is ischemic colitis associated with intestinal vasculitis and increased SLE activity, and the patient showed clinical improvement with steroid and conservative treatment. In fact, there is no simple gauge to assess the extent and degree of intestinal ischemia[2]. However, if there are abdominal manifestations, such as pain or bloody stool in patients with active SLE, ischemic colitis should be considered and suspected.
Peer reviewers: Francesco Costa, MD, Dipartimento di Medicina Interna-U.O. di Gastroenterologia, Università di Pisa-Via Roma, 67-56122-Pisa, Italy; Rami Eliakim, Professor, Department of Gastroenterology, Rambam Medical Center, p.o.b. 9602, Haifa 31096, Israel; Jean-Noel Freund, MD, INSERM 682, Str Asbourg, France, 3 Avenue Molière, Strasbourg 67200, France
S- Editor Zhong XY L- Editor Ma JY E- Editor Lin YP
References
- 1.Versaci A, Macri A, Scuderi G, Bartolone S, Familiari L, Lupattelli T, Famulari C. Ischemic colitis following colonoscopy in a systemic lupus erythematosus patient: report of a case. Dis Colon Rectum. 2005;48:866–869. doi: 10.1007/s10350-004-0837-z. [DOI] [PubMed] [Google Scholar]
- 2.Gore RM, Marn CS, Ujiki GT, Craig RM, Marquardt J. Ischemic colitis associated with systemic lupus erythematosus. Dis Colon Rectum. 1983;26:449–451. doi: 10.1007/BF02556524. [DOI] [PubMed] [Google Scholar]
- 3.Reissman P, Weiss EG, Teoh TA, Lucas FV, Wexner SD. Gangrenous ischemic colitis of the rectum: a rare complication of systemic lupus erythematosus. Am J Gastroenterol. 1994;89:2234–2236. [PubMed] [Google Scholar]
- 4.Miyahara S, Ito S, Soeda A, Chino Y, Hayashi T, Takahashi R, Goto D, Matsumoto I, Tsutsumi A, Sumida T. Two cases of systemic lupus erythematosus complicated with colonic ulcers. Intern Med. 2005;44:1298–1306. doi: 10.2169/internalmedicine.44.1298. [DOI] [PubMed] [Google Scholar]
- 5.Lee CK, Ahn MS, Lee EY, Shin JH, Cho YS, Ha HK, Yoo B, Moon HB. Acute abdominal pain in systemic lupus erythematosus: focus on lupus enteritis (gastrointestinal vasculitis) Ann Rheum Dis. 2002;61:547–550. doi: 10.1136/ard.61.6.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grimbacher B, Huber M, von Kempis J, Kalden P, Uhl M, Kohler G, Blum HE, Peter HH. Successful treatment of gastrointestinal vasculitis due to systemic lupus erythematosus with intravenous pulse cyclophosphamide: a clinical case report and review of the literature. Br J Rheumatol. 1998;37:1023–1028. doi: 10.1093/rheumatology/37.9.1023. [DOI] [PubMed] [Google Scholar]
- 7.Cappell MS. Intestinal (mesenteric) vasculopathy. II. Ischemic colitis and chronic mesenteric ischemia. Gastroenterol Clin North Am. 1998;27:827–860, vi. doi: 10.1016/s0889-8553(05)70034-0. [DOI] [PubMed] [Google Scholar]
- 8.Lafsky RD. Colonoscopy in ischemic enterocolitis. Gastrointest Endosc. 2000;52:310–311. [PubMed] [Google Scholar]
- 9.Byun JY, Ha HK, Yu SY, Min JK, Park SH, Kim HY, Chun KA, Choi KH, Ko BH, Shinn KS. CT features of systemic lupus erythematosus in patients with acute abdominal pain: emphasis on ischemic bowel disease. Radiology. 1999;211:203–209. doi: 10.1148/radiology.211.1.r99mr17203. [DOI] [PubMed] [Google Scholar]
- 10.Kim YG, Ha HK, Nah SS, Lee CK, Moon HB, Yoo B. Acute abdominal pain in systemic lupus erythematosus: factors contributing to recurrence of lupus enteritis. Ann Rheum Dis. 2006;65:1537–1538. doi: 10.1136/ard.2006.053264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Teramoto J, Takahashi Y, Katsuki S, Sato T, Sakamaki S, Kobayashi D, Watanabe N, Niitsu Y. Systemic lupus erythematosus with a giant rectal ulcer and perforation. Intern Med. 1999;38:643–649. doi: 10.2169/internalmedicine.38.643. [DOI] [PubMed] [Google Scholar]


