Abstract
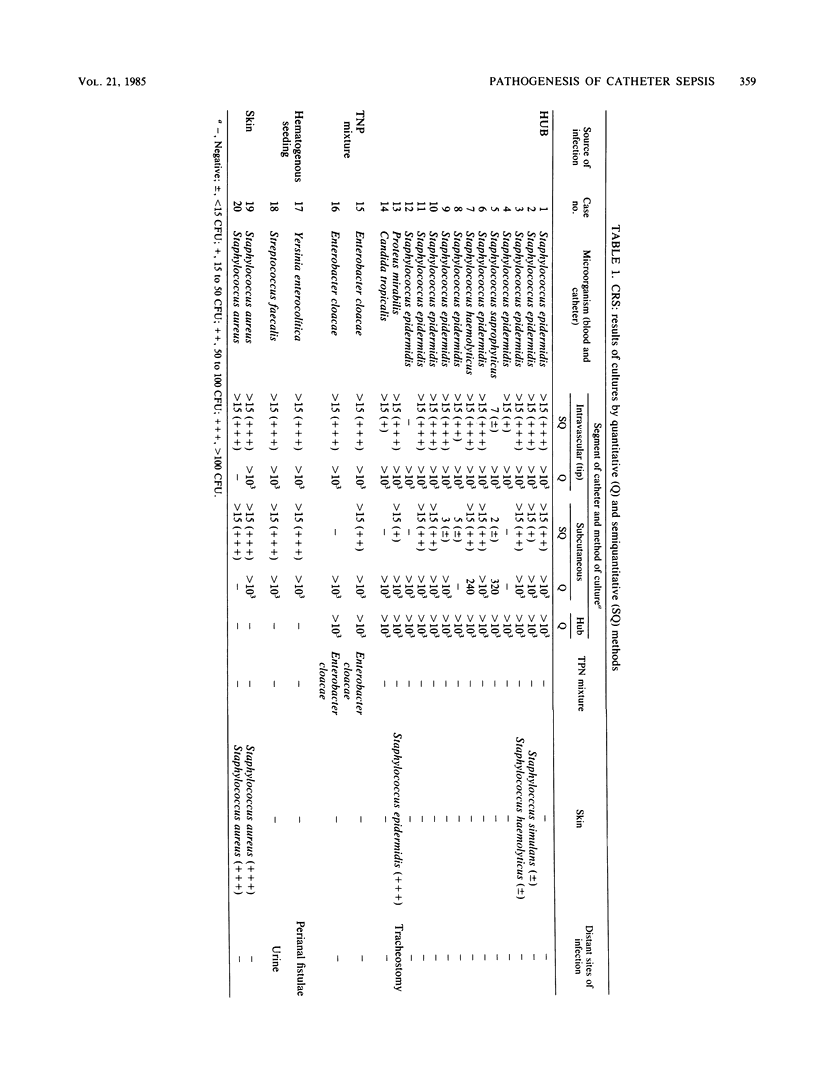
Our purpose was to study prospectively the causes, routes of infection, and frequency of catheter-related sepsis in patients on total parenteral nutrition. From January 1981 to January 1984, cultures of 135 subclavian catheters from 135 adult patients were done by quantitative and semiquantitative methods. Twenty patients (14.8%) had catheter-related sepsis. Fourteen episodes (70%) stemmed from an colonized hub. Skin infection (Staphylococcus aureus, 2 cases), total parenteral nutrition mixture contamination (Enterobacter cloacae, 2 cases), and hematogenous seeding of the catheter tip (Yersinia enterocolitica, 1 case, and Streptococcus faecalis, 1 case) accounted for the remaining six septic episodes. The catheter hub is, in our experience, the most common site of origin of organisms causing catheter tip infection and bacteremia.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bauer A. W., Kirby W. M., Sherris J. C., Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966 Apr;45(4):493–496. [PubMed] [Google Scholar]
- Bjornson H. S., Colley R., Bower R. H., Duty V. P., Schwartz-Fulton J. T., Fischer J. E. Association between microorganism growth at the catheter insertion site and colonization of the catheter in patients receiving total parenteral nutrition. Surgery. 1982 Oct;92(4):720–727. [PubMed] [Google Scholar]
- Blackett R. L., Bakran A., Bradley J. A., Halsall A., Hill G. L., McMahon M. J. A prospective study of subclavian vein catheters used exclusively for the purpose of intravenous feeding. Br J Surg. 1978 Jun;65(6):393–395. doi: 10.1002/bjs.1800650607. [DOI] [PubMed] [Google Scholar]
- Bozzetti F., Terno G., Camerini E., Baticci F., Scarpa D., Pupa A. Pathogenesis and predictability of central venous catheter sepsis. Surgery. 1982 Apr;91(4):383–389. [PubMed] [Google Scholar]
- Cleri D. J., Corrado M. L., Seligman S. J. Quantitative culture of intravenous catheters and other intravascular inserts. J Infect Dis. 1980 Jun;141(6):781–786. doi: 10.1093/infdis/141.6.781. [DOI] [PubMed] [Google Scholar]
- Deitel M., Krajden S., Saldanha C. F., Gregory W. D., Fuksa M., Cantwell E. An outbreak of Staphylococcus epidermidis septicemia. JPEN J Parenter Enteral Nutr. 1983 Nov-Dec;7(6):569–572. doi: 10.1177/0148607183007006569. [DOI] [PubMed] [Google Scholar]
- Garden O. J., Sim A. J. A comparison of tunnelled and nontunnelled subclavian vein catheters: a prospective study of complications during parenteral feeding. Clin Nutr. 1983 Apr;2(1):51–54. doi: 10.1016/0261-5614(83)90031-6. [DOI] [PubMed] [Google Scholar]
- Hesselvik F., Schildt B., Nilehn B. Long term parenteral therapy by percutaneous tunneled silicone central venous catheter--a follow-up of 300 catheters. Clin Nutr. 1982 Jul;1(2):117–124. doi: 10.1016/0261-5614(82)90033-4. [DOI] [PubMed] [Google Scholar]
- Holm I., Wretlind A. Prophylaxis against infection and septicemia in parenteral nutrition via central intravenous catheter. Acta Chir Scand. 1975;141(3):173–181. [PubMed] [Google Scholar]
- Jones R. N., Thornsberry C., Barry A. L., Gavan T. L. Evaluation of the Sceptor microdilution antibiotic susceptibility testing system: a collaborative investigation. J Clin Microbiol. 1981 Jan;13(1):184–194. doi: 10.1128/jcm.13.1.184-194.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keohane P. P., Jones B. J., Attrill H., Cribb A., Northover J., Frost P., Silk D. B. Effect of catheter tunnelling and a nutrition nurse on catheter sepsis during parenteral nutrition. A controlled trial. Lancet. 1983 Dec 17;2(8364):1388–1390. doi: 10.1016/s0140-6736(83)90922-4. [DOI] [PubMed] [Google Scholar]
- Maki D. G., Weise C. E., Sarafin H. W. A semiquantitative culture method for identifying intravenous-catheter-related infection. N Engl J Med. 1977 Jun 9;296(23):1305–1309. doi: 10.1056/NEJM197706092962301. [DOI] [PubMed] [Google Scholar]
- Ryan J. A., Jr, Abel R. M., Abbott W. M., Hopkins C. C., Chesney T. M., Colley R., Phillips K., Fischer J. E. Catheter complications in total parenteral nutrition. A prospective study of 200 consecutive patients. N Engl J Med. 1974 Apr 4;290(14):757–761. doi: 10.1056/NEJM197404042901401. [DOI] [PubMed] [Google Scholar]
- Shinozaki T., Deane R. S., Mazuzan J. E., Jr, Hamel A. J., Hazelton D. Bacterial contamination of arterial lines. A prospective study. JAMA. 1983 Jan 14;249(2):223–225. [PubMed] [Google Scholar]
- Sitges-Serra A., Jaurrieta E., Liñares J., Pérez J. L., Garau J. Bacteria in total parenteral nutrition catheters: where do they come from? Lancet. 1983 Mar 5;1(8323):531–531. doi: 10.1016/s0140-6736(83)92219-5. [DOI] [PubMed] [Google Scholar]
- Sitges-Serra A., Linares J. Tunnels do not protect against venous-catheter-related sepsis. Lancet. 1984 Feb 25;1(8374):459–460. doi: 10.1016/s0140-6736(84)91800-2. [DOI] [PubMed] [Google Scholar]
- Sitges-Serra A., Puig P., Jaurrieta E., Garau J., Alastrue A., Sitges-Creus A. Catheter sepsis due to Staphylococcus epidermidis during parenteral nutrition. Surg Gynecol Obstet. 1980 Oct;151(4):481–483. [PubMed] [Google Scholar]
- Sitges-Serra A., Puig P., Liñares J., Pérez J. L., Farreró N., Jaurrieta E., Garau J. Hub colonization as the initial step in an outbreak of catheter-related sepsis due to coagulase negative staphylococci during parenteral nutrition. JPEN J Parenter Enteral Nutr. 1984 Nov-Dec;8(6):668–672. doi: 10.1177/0148607184008006668. [DOI] [PubMed] [Google Scholar]


