Abstract
Objective
This article compares use of pain coping strategies among older, middle-aged, and younger adults living with chronic pain and seeks to determine whether the relationship between pain severity and coping is moderated by age.
Method
Participants were 464 adults reporting chronic pain secondary to multiple sclerosis, spinal cord injury, or neuromuscular disease. Participants completed a survey including measures of pain severity and the Chronic Pain Coping Inventory.
Results
After controlling for clinical and demographic variables, older adults (older than 60) reported a wider range of frequently used strategies and significantly more frequent engagement in activity pacing, seeking social support, and use of coping self-statements than did younger or middle-aged adults. Moderation analyses suggest that, for younger adults, efforts at coping generally increased with greater pain severity, whereas this relationship did not exist for older adults.
Discussion
These data suggest differences in the quantity and quality of pain coping among age groups.
Keywords: chronic pain, older adults, SCI, MS, neuromuscular disease
Aging is associated with a number of uncontrollable stressors, including retirement, financial strain, bereavement, changes in social support, and health decline (Aldwin, 1990; Krause, Jay, & Liang, 1991; Murrell, Norris, & Hutchins, 1984). Despite this, most research has demonstrated a decline in perceived stress and increase in well-being with increasing age (e.g., Aldwin, 1991; Paykel, 1983; Silverman, Eichler, & Williams, 1987). Consistent with this observation, research during the past several decades has examined the ways that older adults cope with stressors and has noted differences in both the process and the content of coping as compared to younger adults. In general, these differences have favored older adults, suggesting more effective coping in later life. For example, from the psychodynamic or developmental perspective, Vaillant (1977) reported that middle-aged men used fewer neurotic and immature defense mechanisms as compared to their younger selves. More recently, Diehl, Coyle, and Labouvie-Vief (1996) reported that a group of older adults reported a combination of coping strategies indicative of “greater impulse control” and positive appraisal of conflict situations as compared to younger adults and adolescents. Studies of standardized measures of coping have also supported these findings, suggesting that older adults generally use less escapism and avoidant coping (Aldwin & Revenson, 1985, cited in Aldwin, 1991; Irion & Blanchard-Fields, 1987). However, findings of more effective or positive coping in older adults have not been consistent across stressors or populations. Folkman, Lazarus, Pimley, and Novacek (1987) found that older people used relatively more escape avoidance, although this effect could not be replicated by Aldwin (1991). Furthermore, very small (Aldwin, Sutton, Chiara, & Spiro, 1996) or no differences (Blanchard-Fields, Sulsky, & Robinson-Whelen, 1991) in coping across age groups have also been reported by a number of authors, particularly in the area of problem-focused coping (e.g., McCrae, 1982). One finding in several studies is that older adults appear to use fewer strategies, but use them as or more effectively, than do younger adults (Aldwin, 1991; Meeks, Carstensen, Tamsky, Wright, & Pellegrini, 1989). They also tend to use the same strategies for managing stressors across life domains (Moos, Brennan, Schutte, & Moos, 2006).
Inconsistencies in the coping literature for older adults are perhaps not surprising given the complex nature of the topic. Coping is a very broad term and can encapsulate a wide range of psychological domains, including attribution style, personality, behavior, and social engagement in reaction to stressful situations (e.g., Lazarus, 1986). It follows that various measures have attempted to incorporate a large number of coping efforts into a few limited dimensions, such as active versus passive, avoidant versus nonavoidant, and adaptive versus maladaptive (e.g., Aldwin et al., 1996). This categorical approach has been criticized in the literature, as it tends to collapse different cognitions and behaviors into a few broad categories (Martin, Rott, Poon, Courtenay, & Lehr, 2001). Whether a person employs “more” or “less” of a broad category of coping may not be a meaningful way of conceptualizing the complicated relationships among stressors and responses. For this reason, contemporary approaches to measuring coping efforts in older people have focused on a more “molecular” perspective, in which very specific coping strategies are measured in relation to very specific stressors (e.g., Martin et al., 2001).
One such stressor is chronic pain. Chronic pain is a common problem for older people, affecting as many as 70% of independently living older adults (Roy & Thomas, 1988) and 83% of those in assisted living facilities (Ferrell, Ferrell, & Osterweil, 1990; Parmelee, Smith, & Katz, 1993). Larger population-based studies have described rates around 40% to 50%, a twofold increase over younger adults (Catala et al., 2002). Although the prevalence of certain pain conditions decreases with age (e.g., headache pain; Lipton, Pfeffer, Newman, & Soloman, 1993), the high prevalence of pain in older adults likely reflects an increased risk of painful conditions, such as osteoarthritis and peripheral vascular disease (Centers for Disease Control and Prevention, 2005; Srikanth et al., 2005).
Pain can significantly interfere with quality of life in older people through associations with sleep disturbance (Ferrell et al., 1990; Magni, Marchetti, Moreschi, Merskey, & Luchini, 1993), decreased social functioning (Bookwala, Harralson, & Parmelee, 2003), increased health care utilization and cost (Gallagher, Merna, & Mossey, 2000), disability or functional dependence (Dorantes-Mendoza, Avila-Funes, Mejía-Arango, & Gutiérrez-Robledo, 2007; Edwards, 2006), and increased negative affect (e.g., Davidson, Feldman, & Crawford, 1994; Radloff & Teri, 1986; Thomas, Peat, Harris, Wilkie, & Croft, 2004). Pain is an important factor contributing to poor overall physical health states in older people (Cooper & Kohlmann, 2001; also see Edwards, 2006).
Similar to the perceived stress literature in older adults, something of a paradox exists in studies describing chronic pain in this population. Despite the increased prevalence of chronic pain and its clearly negative impact on quality of life, many studies have reported that older adults are less bothered or emotionally impacted by chronic pain than are younger adults (Molton, Jensen, Ehde, & Smith, 2007; Riley, Wade, Robinson, & Price, 2000; Rustoen et al., 2005). It would appear that some part of the aging process may be a buffer to pain-related suffering. Several hypotheses have been offered for this effect, generally centered around either greater temporal experience with pain and other life stressors (Aldwin, 1991; Molton et al., 2007) or social cognitive effects such as social comparison to less well older adults (Idler, 1993; Rakowski & Cryan, 1990) and/or beliefs about the “normalcy” of pain or activity restriction associated with aging (Cook & Thomas, 1994; Greenlee, 1991; Parmelee, 1997; Riley et al., 2000; Sofaer et al., 2005; Williamson, 1998; Williamson & Schulz, 1995).
Although these hypotheses suggest various causes for the lessened impact of pain in older people, they do not clearly specify a mechanism. One possibility may be differences in the content or process of coping. It is plausible that, as a result of a lifetime of experience or other age effects, older people make more effective use of pain coping strategies associated with well-being. However, to date only a handful of studies have specifically compared pain-related coping across age groups. One study (Sorkin, Rudy, Hanlon, Turk, & Stieg, 1990) found that younger people used twice as many “cognitive” strategies (e.g., distraction, imagery) for managing pain than did older adults. In contrast, in a community sample of 280 patients with chronic pain (LaChapelle & Hadjistavropoulos, 2005), age was negatively correlated with a variety of emotion- and problem-focused strategies, suggesting lesser frequency of coping strategies across the board in older people. No significant relationship was demonstrated between age and use of pain coping strategies in a group of patients referred to a multidisciplinary pain management program (Keefe & Williams, 1990), although methodological concerns such as low power may limit the inter-pretability of the findings from this study.
In interpreting coping differences in older adults with chronic pain, it becomes important to have some basis for judging the relative effectiveness of individual strategies. Although terms such as adaptive and maladaptive are generally too broad to be useful descriptors of coping (as described above), certain coping strategies have been repeatedly shown to be associated with negative outcomes such as greater disability and poorer psychological adjustment in patients with chronic pain (e.g., Hadjistavropoulos, MacLeod, & Asmundson, 1999; Jensen, Turner, Romano, & Lawler, 1994; Jensen, Turner, Romano, & Strom, 1995; Raichle, Hanley, Jensen, & Cardenas, 2007; Tan, Nguyen, Anderson, Jensen, & Thornby, 2005) and are generally targeted by multidisciplinary pain management programs. Therefore, some consensus exists regarding which coping strategies are considered most helpful (and should be emphasized in treatment) and which are considered unhelpful (and should be avoided). Helpful strategies include task persistence (persevering with a task despite pain), relaxation, pacing one’s activities, and coping self-statements (intentionally thinking positive or affirming thoughts about pain and one’s ability to handle it; Jensen et al., 1995). Unhelpful strategies include guarding (avoiding movement because of fear of injury; Raichle et al., 2007) pain-contingent rest (Fordyce, 1976; Jensen et al., 1994; Jensen et al., 2002), and pain-contingent social support (e.g., expecting others to foresee and respond to pain complaints; Romano et al., 1995). However, to our knowledge, no studies have investigated these coping strategies specifically in older adults.
The Present Study
The present study sought to apply a “molecular” perspective to describing pain-related coping in older adults with chronic pain secondary to disability and to compare these coping strategies to those reported by younger and middle-aged adults. Disabilities such as multiple sclerosis (MS), neuromuscular disease (NMD), and spinal cord injury (SCI) are commonly associated with a number of chronic pain problems, including muscu-loskeletal pain (Abresch, Carter, Jensen, & Kilmer, 2002; Haisma et al., 2007; Kassirer, 2000), neuropathic pain or paresthesias (Ehde et al., 2003; Finnerup, Johannesen, Sindrup, Bach, & Jensen, 2001; Frisbie & Aguilera, 1990; Jensen, Abresch, Carter, & McDonald, 2005; Jensen, Hanley, Turner, & Cardenas, 2004; Siddal & Loeser, 2001), chronic headache (Archibald et al., 1994), and painful tonic spasms (Perkins, Moxley, & Papciak, 1999). Recent evidence has suggested that the majority of patients with these disabilities report chronic painful sensations (Ehde et al., 2003; Jensen et al., 2004; Widerstrom-Noga & Turk, 2003) and that from one fourth to one third report the pain as severe (Ehde et al., 2003; Jensen et al., 2004; Widerstrom-Noga & Turk, 2003).
Chronic pain lends itself well to the “molecular” view of coping, as studies have suggested specific coping strategies that are associated with positive outcomes. Also, given the observation that differences in coping may be an artifact of different stressors faced across age groups, the use of a consistent or shared stressor such as chronic pain may be a useful way to control for such differences. Specifically, we attempted to address the following questions regarding chronic, disability-related pain:
Do older adults report using pain-related coping strategies with lesser frequency than do younger or middle-aged adults?
Do older adults use a different repertoire of pain-related coping strategies? That is, do they rely on a different “rank order” list of strategies?
Compared to younger and middle-aged adults, do older adults make more frequent use of pain coping strategies that have been associated with positive outcomes or lesser use of strategies associated with negative outcomes in other samples of people with chronic pain?
Do older adults differ from younger or middle-aged adults in pain-contingent coping? That is, as pain intensity escalates, do older adults also escalate the frequency of their coping efforts, and is this different in younger people?
Method
Participants
Participants were 214 men and 250 women (N = 464) who reported chronic pain secondary to neurodegenerative disease or injury. Diagnosis included MS (n = 125, 27.0%), NMD (n = 212, 45.7%; e.g., amyotrophic lateral sclerosis, Charcot-Marie-Tooth disease, fascioscapulohumeral dystrophy, and myotonic muscular dystrophy), or SCI (127, 27.4%). All diagnoses were confirmed by a study physician before enrollment as part of recruitment. All study participants were recruited as part of a larger study investigating chronic pain in disabilities conducted at the University of Washington. Recruitment procedures varied somewhat by medical diagnosis. Participants with SCI were recruited from a sample of participants (n = 464) who had previously responded to two previous surveys of chronic pain problems in SCI taken 2 to 6 years before the current study (this method is described in Turner & Cardenas, 1999). Eligible participants from this earlier study were recontacted and asked if they wanted to participate in the current study. Participants with MS were randomly selected from a larger pool (n = 737) of people with MS who had completed a previous survey through the Multiple Sclerosis Association of King County, Washington, and who indicated that they were willing to be contacted for future research. Participants with NMD diagnoses were recruited from two sites: (a) an NMD rehabilitation clinic at the University of Washington Medical Center and (b) an NMD rehabilitation clinic and NMD research and training center at the University of California, Davis.
Data from these research pools, particularly on the scope of pain and symptom burden in disability, have been published elsewhere (see Ehde, Osborne, Hanley, Jensen, & Kraft, 2006; Jensen, Kuehn, Amtmann, & Cardenas, 2007). However, these previous studies did not include analyses of age or coping behavior in this mixed group of individuals with neuro-logically related pain.
Procedure
All participants were first sent a postcard indicating that survey materials would be forthcoming and were provided with an option to decline further participation by telephone or postcard. Participants who did not decline then received a cover letter describing the study, a consent form, and the survey itself. Participants who returned the survey were reimbursed $25 for their time. To minimize missing data, research assistants contacted respondents via telephone as needed to complete items that were left blank or were unclear. All study procedures were approved by the University Human Subjects Review Committee.
Response Rate and Selection
A total of 1,024 surveys were mailed (SCI = 333, MS = 296, NMD = 395), and a total of 637 (SCI = 157, MS = 187, NMD = 293) were returned, yielding a response rate of 62.2%. Of these, 464 respondents reported experiencing chronic pain and were included in the present study.
Measures
Demographics
Participants provided information regarding age, ethnicity, education level, and employment status. They also completed clinical questions regarding their injury or disease, including the date of onset.
Pain intensity
Average pain intensity (for the past week) was assessed using a standard 11-point numeric rating scale (NRS) ranging from 0 (no pain) to 10 (pain as bad as could be). NRSs are commonly used in pain research, and a great deal of evidence supports their validity as measures of pain intensity across pain problems and populations (Jensen & Karoly, 2000; Jensen, Karoly, O’Riordan, Bland, & Burns, 1989).
Pain-related coping
Use of pain coping strategies to manage pain was assessed using a modified version of the Chronic Pain Coping Inventory (CPCI; Jensen et al., 1995). The original CPCI contained 64 items assessing eight coping domains that the developers saw as being relevant to pain management programs: Guarding (restricting the use or movement of a body part to prevent pain), Resting (lying down or sitting), Asking for Assistance (asking for help with a task to avoid pain), Relaxation (intentionally engaging in a specific exercise, such as meditation or deep breathing, to reduce pain), Task Persistence (persevering in a task despite pain), Exercise/Stretching (using muscle stretching or physical activity to prevent pain), Coping Self-Statements (intentionally thinking positive or affirming thoughts about pain and one’s ability to handle it), and Seeking Social Support (talking with a friend or loved on when in pain). These domains are conceptualized as being generally maladaptive and therefore discouraged (Guarding, Resting, Asking for Assistance), generally adaptive and therefore encouraged (Coping Self-Statements, Relaxation, Task Persistence, Exercise/Stretching), or neither specifically encouraged nor discouraged (Seeking Social Support) in pain treatment programs (Hadjistavropoulos et al., 1999; Jensen et al., 1995). Participants are asked to indicate how many days in the past week they used each strategy at least once to cope with pain. Internal consistency and temporal stability of this measure are quite strong (mean Cronbach’s α = .84, test–retest r = .80; Jensen et al., 1995), and predictive validity of the CPCI subscales has been demonstrated through associations with relevant outcomes such as pain interference, depression, disability, and pain severity (Hadjistavropoulos et al., 1999; Jensen et al., 1995; Tan et al., 2005).
The version used in the present study included the original 64-item, eight-subscale CPCI as well as a new 6-item subscale assessing the use of activity pacing, such as taking breaks, going slower, and separating large tasks into more manageable components (i.e., “Pacing”). This Pacing subscale has demonstrated adequate validity and reliability in older adults living with chronic pain (Cronbach’s α = .79; Ersek, Turner, & Kemp, 2006). In the present sample, the CPCI subscales demonstrated acceptable internal consistency, with Cronbach’s alphas ranging from .77 (Relaxation) to .91 (Exercise/Stretching). The median alpha was .85. Correlations among CPCI subscales in the present sample are presented in Table 1.
Table 1.
Correlation Matrix of CPCI Subscales
| Pace | Guard | Rest | Ask | Relax | Task | Exer | Social | CSS | |
|---|---|---|---|---|---|---|---|---|---|
| Pace | 1.0 | ||||||||
| Guard | .52** | 1.0 | |||||||
| Rest | .47** | .57** | 1.0 | ||||||
| Ask | .30** | .47** | .38** | 1.0 | |||||
| Relax | .40** | .30** | .37** | .26** | 1.0 | ||||
| Task | .27** | .01 | –.01 | .05 | .13** | 1.0 | |||
| Exer | .31** | .22** | .19** | .17** | .45** | .24** | 1.0 | ||
| Social | .40** | .39** | .43** | .54** | .46** | .06 | .34** | 1.0 | |
| CSS | .50** | .49** | .43** | .34** | .51** | .17** | .35** | .53** | 1.0 |
Note: CPCI = Chronic Pain Coping Inventory; Pace = Pacing; Guard = Guarding; Rest = Resting; Ask = Asking For Assistance; Relax = Relaxation; Exer = Exercise/Stretching; Social = Seeking Social Support; CSS = Coping Self-Statements.
p < .01.
Statistical Approach
Potential control variables
Prior to statistical testing for control variables, we made the decision a priori to include the following variables as controls in the CPCI analyses: sex, time since diagnosis or injury, and diagnostic group (i.e., MS, NMD, SCI; see Table 2). This decision was made in an attempt to equalize the groups as much as possible, given that sex is generally confounded with diagnostic group (men are more likely to get SCI and women to develop MS) and that age is confounded with time since diagnosis. This decision was statistically supported in the present sample, where medical diagnosis was associated with significant or trend (p < .10) differences on all CPCI subscales, sex was associated with significant or trend (p < .10) differences on seven of nine CPCI subscales, and time since diagnosis or injury was positively associated with two CPCI subscales (p < .10). Although a review of these differences is beyond the scope of the present study, generally speaking participants with MS reported greater levels of coping activation across the board (although individuals with SCI relied more on task persistence and individuals with NMD relied more on guarding and asking for assistance) and women reported greater coping activation than did men (although men did report more task persistence and more coping self-statements).
Table 2.
Clinical Variables by Age Group
| Younger (n = 99) |
Middle Aged (n = 274) |
Older (n = 84) |
||||||
|---|---|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | F | p | |
| Pain severity | 4.2 | 2.6† | 4.8 | 2.4 | 5.1 | 2.3† | 3.6 | < .05 |
| Time since diagnosis (years) | 10.9 | 7.2†‡ | 15.9 | 11.1‡* | 19.4 | 13.6†* | 14.4 | < .001 |
| χ2 | P | |||||||
| Sex | ||||||||
| Male | n = 54 | n = 120 | n = 38 | 3.4 | ns | |||
| Female | n = 45 | n = 154 | n = 46 | |||||
| Diagnosis | 4.4 | ns | ||||||
| MS | n = 20 | n = 77 | n = 28 | |||||
| NMD | n = 28 | n = 78 | n = 21 | |||||
| SCI | n = 52 | n = 124 | n = 36 | |||||
Note: MS = multiple sclerosis; NMD = neuromuscular disease; SCI = spinal cord injury.
Significant difference between younger and older groups (after Sidak correction, p < .05).
Significant difference between younger and middle-aged groups (after Sidak correction, p < .05).
Significant difference between middle-aged and older groups (after Sidak correction, p < .05).
We then selected additional control variables if they (a) significantly differed by age group and (b) were significantly related to CPCI subscales in a consistent way. Analyses for controls included chi-square tests (for categorical variables) and t tests or one-way analyses of variance for continuous variables
Age group comparisons
To compare younger, middle-aged, and older adults on CPCI subscales, we utilized a one-way analysis of covariance (ANCOVA) including control variables. Participants were divided into three groups: younger (18 to 40), middle aged (40 to 60), and older (60 to 90). These cutoffs are somewhat arbitrary but were meant to be similar to those used in previous work (e.g., Boerner, 2004; Keefe & Williams, 1990) and to represent developmentally important transition periods in life. For example, we attempted to capture a period typically associated with an early career and family raising (younger; M = 31.7); a period of career peak, family individuation and/or the early experience of an “empty nest,” and retirement planning (middle aged; M = 50.0); and a period associated with retirement and transition to older adulthood (older; M =65.8). Given unequal cellular sample sizes, we selected the Type II sum of squares approach as recommended for unbalanced designs in the literature (Langsrud, 2003). Significant F tests were followed by pairwise comparisons using the Sidak (1967) correction for familywise error.
Moderated regression analyses
To determine whether the effect of pain severity on coping was moderated by age group, we performed moderated regression analyses. Moderated regression analyses were then performed as per recommendations of Holmbeck (2002). Consistent with this approach, average pain and age were centered, and an interaction term was created using the centered data. After entry of control variables, the main effects for age and pain were entered as one block, followed by a block containing the interaction. Following significance of the R2 Δ term associated with the interaction block, post hoc regression analyses were performed to determine the effect of pain on coping for each of three levels of age (as above, younger [18 to 40], middle aged [40 to 60], and older [60 to 90]). The slopes were then individually evaluated for statistical significance.
Statistical package
All analyses were conducted using SPSS software (Version 14.0).
Results
Demographics
Participants were an average of 15.4 years from injury or diagnosis (SD = 11.2). Age ranged from 18 to 83, the mean being 48.9 years (SD = 12.14). Mean ages for the age groups were as follows: 31.7 (SD = 6.8; younger), 50.0 (SD = 5.0; middle aged), and 65.8 (SD = 5.5; older). The vast majority (98.0%) were high school graduates, and most had completed some college (74.6%). Participants were generally Caucasian (93.0%) and married or living with a partner (61.2%). Regarding employment, about half (52.8%) of participants reported being unemployed because of pain or disability, with the remainder generally working part- or full-time (34.3%).
Controls
Two employment status variables (employed full-time and unemployed because of disability, both yes or no) met the specified criteria for inclusion as controls. Younger adults were more likely to be employed full-time (χ2 = 15.39, p < .01), and full-time employment was negatively associated with frequency of coping efforts for all CPCI subscales (all t values > 1.7, all p values < .10) except Task Persistence (where full-time employment actually predicted greater frequency; t = 5.3, p < .01). Similarly, unemployment because of disability was much more common in the middle-aged group (χ2 = 11.81, p < .01) and was significantly associated with all CPCI variables (all t values > 2.2, all p values < .05) except Exercise/Stretching (t = 0.60, p > .50). Being unemployed because of disability predicted more frequent use of coping strategies in all cases except Task Persistence (where unemployment because of disability predicted less use of this strategy). Pain severity also varied by age group (F = 3.6, p < .05), with older adults reporting more pain than younger adults (M =5.1 vs. 4.2, t = –2.6, p < .05).
Based on these results and the analytic plan, controls therefore included diagnostic group (NMD, SCI, MS), time since diagnosis or injury in years, gender, full-time employment (yes or no), and unemployment because of disability (yes or no). Pain severity was also included as a control in the age group comparisons (but not the moderated regression analyses, where it served as a predictor variable).
Rank Order of Coping Strategies by Reported Frequency
The rank order of coping strategies by age group is presented in Table 3. Briefly, these results suggest that although all participants appear to use a similar repertoire of strategies, certain differences do emerge as a function of age group. For example, all people in this study reported using task persistence with the greatest frequency and rarely used exercise, relaxation, or asking for social support. However, older adults appear to rate pacing and coping self-statements as “first-line” strategies, whereas this was not true for younger adults.
Table 3.
Rank Order of Pain Coping Strategies by Age Group
| Younger (n = 99) | Middle Aged (n = 275) | Older (n = 84) | |
|---|---|---|---|
| 1 | Task persistence | Task persistence | Task persistence |
| 2 | Resting | Pacing | Pacing |
| 3 | Asking for assistance | Resting | Coping self-statements |
| 4 | Pacing | Asking for assistance | Resting |
| 5 | Guarding | Guarding | Asking for assistance |
| 6 | Coping self-statements | Coping self-statements | Guarding |
| 7 | Exercise/stretching | Exercise/stretching | Exercise/stretching |
| 8 | Seeking social support | Seeking social support | Seeking social support |
| 9 | Relaxation | Relaxation | Relaxation |
Age Group Coping Differences
After inclusion of controls, one-way ANCOVA analyses were significant for Pacing, Seeking Social Support, and Coping Self-Statements (all F values > 3.25, all p values < .05). Follow-up post hoc analyses using the Sidak (1967) correction revealed that the older adults reported performing each of these strategies more often than did their younger adult counterparts (all corrected p values < .05). The average effect size for the difference between younger and older adults on these subscales was in the medium range (Cohen’s d = .47). These results are presented in Table 4.
Table 4.
Comparison of Age Groups
| Younger (n= 99) |
Middle Aged (n = 274) |
Older (n = 84) |
Effect Size (Cohen’s d) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CPCI Subscalea | M | SE | M | SE | M | SE | F | P | Y vs. O | Y vs. M | Mvs. O |
| Task Persistence | 4.4 | 0.19 | 4.5 | 0.11 | 4.8 | 0.21 | 0.85 | ns | –.21 | –.05 | –.16 |
| Pacing | 2.6 | 0.21†,‡ | 3.3 | 0.13‡ | 3.5 | 0.23† | 5.0 | < .01 | –.43 | –.33 | –.09 |
| Guarding | 2.4 | 0.17 | 2.7 | 0.10 | 2.9 | 0.18 | 2.3 | ns | –.30 | –.18 | –.12 |
| Resting | 3.0 | 0.19 | 3.2 | 0.11 | 3.1 | 0.20 | 0.52 | ns | –.05 | –.11 | .05 |
| Asking for Assistance | 2.9 | 0.23 | 2.8 | 0.14 | 3.0 | 0.26 | 0.35 | ns | –.04 | .04 | –.08 |
| Relaxation | 1.5 | 0.14 | 1.6 | 0.09 | 1.5 | 0.16 | 0.09 | ns | .0 | –.07 | .07 |
| Exercise/Stretching | 2.2 | 0.19 | 2.2 | 0.11 | 2.3 | 0.21 | 0.14 | ns | –.05 | .0 | .05 |
| Coping Self-Statements | 2.3 | 0.19† | 2.6 | 0.11* | 3.3 | 0.21†* | 7.0 | < .001 | –.52 | –.16 | –.37 |
| Seeking Social Support | 1.6 | 0.16† | 1.8 | 0.10 | 2.2 | 0.18† | 3.2 | < .05 | –.37 | –.12 | –.24 |
Note: CPCI = Chronic Pain Coping Inventory; Y = younger; M = middle age; O = older.
Means controlling for average pain intensity in the past week, medical diagnosis, time since diagnosis or injury, gender, employment status (full-time, yes or no) and disability status (unemployment because of disability, yes or no).
Significant difference between younger and older groups (after Sidak correction, p < .05).
Significant difference between younger and middle-aged groups (after Sidak correction, p <
Significant difference between middle-aged and older groups (after Sidak correction, p <.05).
In terms of number of strategies utilized more than three times per week, a significant main effect for age group was detected (F = 7.03, p < .001). Follow-up testing revealed that the older adult group reported using more strategies at least three times per week than did younger or middle-aged adults (p < .05), even after controlling for confounds (described above). Corrected means scores (Table 4) suggest that older adults utilized five of nine strategies at least three times per week, as compared to two of nine for middle-aged adults and only one of nine for younger adults.
Moderation Analyses
Moderation analyses were performed using hierarchical multiple regression with variables entered in the following blocks: Block 1 (controls; Diagnosis Dummy 1, Diagnosis Dummy 2, time since diagnosis, gender), Block 2 (main effects; age, average pain), and Block 3 (interaction terms; average pain × age). Moderation was established by significance of the R2Δ term for Block 3.
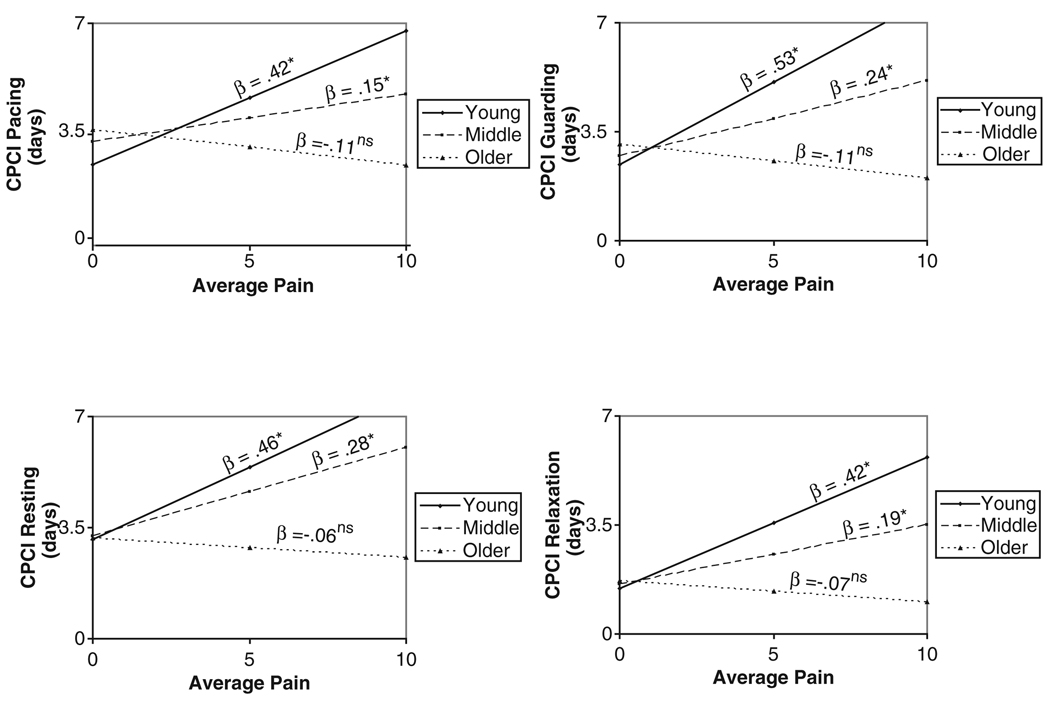
Results suggest that age moderated the pain–coping relationship for Pacing, Guarding, Resting, and Relaxation (all p values < .05). Trends were noted for Asking for Assistance (p = .07) and Exercise/Stretching (p = .08).
Coping and Pain Severity
Following the significant moderation analyses described above, we performed a post hoc linear regression analysis relating pain severity to respective CPCI subscales (i.e., Pacing, Guarding, Resting, and Relaxation) for each age group.1 A consistent pattern emerged from these analyses in which the slope for the effect of pain severity on CPCI subscales was positive and significant for the younger group, less strong (but positive and significant) for the middle-aged group, and weak and not statistically significant for the older group for all but one of the coping responses. Slopes, as well as graphic representations of the relationship between pain severity and coping strategy (Pacing, Guarding, Resting, and Relaxation) by age group, are presented in Figure 1.
Figure 1.
Chronic Pain Coping Inventory (CPCI) Subscales as Moderated by Age Group
Discussion
To our knowledge, this is the first study to look at age-related coping to pain that is secondary to disability. By comparing use of pain-related coping strategies across age groups, this study identifies a number of coping strategies used by older adults that have not been previously identified in the literature. We attempted to utilize a “molecular” perspective (Martin et al., 2001) by using a single specific stressor and a measure of coping designed specifically for that stressor. By examining these constructs in individuals with chronic pain secondary to disability, this study provides novel information about coping in this population.
Several important conclusions can be drawn from this data. First, the data suggest that older adults tend to use a wider range of strategies than do younger adults. Second, they appear to apply certain strategies (activity pacing, seeking social support, and coping self-statements) more frequently than do younger people. Finally, although these data are cross-sectional, the fact that pain was not related to coping activation for the older group suggests that they apply coping efforts regardless of overall pain level. Essentially, older people appear to use a cluster of strategies that work for them and use them consistently regardless of overall pain intensity. This is consistent with some recent work demonstrating that most aspects of the stress and coping process in older adults are comparable for different stressors across life domains (Moos et al., 2006).
In contrast to some earlier work (LaChapelle & Hadjistavropoulos, 2005; Meeks et al., 1989), we found that age was associated with greater use of certain coping strategies and that the magnitude of significant differences between younger and older adults was not inconsequential (M Cohen’s d = .44). Generally speaking, this finding is inconsistent with the limited literature on pain coping in older adults, where age has been negatively correlated with coping activation (LaChapelle & Hadjistavropoulos, 2005). By way of explanation, we note several methodological differences, including the fact that our sample was composed of older adults with physician-confirmed disability-related pain, as compared to participants from community or pain treatment settings. Also, participants in the present study were slightly younger on average than were participants in the LaChapelle and Hadjistavropoulos (2005) study (53.8 vs. 48.9 years in the present study).
In any case, we argue that the implications of mean differences in coping are not particularly useful. For example, older adults in the present study did not report greater use of task persistence, the strategy most consistently associated with better adjustment to pain (e.g., Jensen et al., 1995; Tan et al., 2005). In fact, where they did report statistically more frequent coping efforts than younger and middle-aged adults was on scales that have demonstrated either no consistent relationship with pain adjustment variables such as depression and activity (Pacing), a slight positive relationship with these variables (Seeking Social Support), or both positive and negative relationships with these variables (Coping Self-Statements) (Jensen et al., 1995; Tan et al., 2005). Also, perhaps related to a greater fear of physical injury in the elderly, older adults reported the highest levels of Guarding (although this was not significant). Clearly, it would be a misrepresentation to say that older adults were “better” at coping with pain given these mean differences alone. These results underscore, however, that mean differences may not be a very useful way to conceptualize the relationship between age and pain coping. Rather, it may be more useful to consider the frequency of reported coping strategies relative to one another and to other variables such as pain severity.
In terms of number of strategies employed, all three groups reported using each strategy an average of one day per week or more. However, qualitative differences emerged when considering the number of strategies that were reported as being used at least 3 days a week: five of nine for older adults, two of nine for middle-aged adults, and only one of nine for younger adults. These were based on means that controlled for differences in pain level and diagnosis as well as for employment status and gender. These data suggest greater consistent use of a wider range of strategies in older adults compared to younger adults.
A rank-order approach may also be helpful in understanding how these adults manage their pain. It is important that all three age groups reported task persistence as their most frequently used strategy. This is promising because task persistence has been consistently associated with good adjustment to pain in various studies (e.g., Jensen et al., 1995; Tan et al., 2005). Descriptively, although all age groups reported pain contingent “resting” about 3 days per week, younger adults reported using this strategy with a slightly greater relative frequency as compared to older adults. This strategy is widely considered to be maladaptive, as it has been associated with depression, pain interference, disability, and pain intensity (Tan et al., 2005) and is specifically targeted by a number of operant and cognitive-behavioral pain management approaches (Fordyce, 1976; Novy, 2004). Although older adults also employed this strategy, its lower ranking suggests that, perhaps as a result of aging or experience, older adults have learned that resting is not as effective for managing chronic pain as are other strategies (e.g., pacing). Positive self-statements, taking breaks, going slower, and separating large tasks into more manageable components on a non-pain-contingent basis (e.g., coping self-statements and activity pacing) seem to become more frequently used relative to other strategies with increasing age. It is also encouraging to note that this rank order list of coping strategies in older people is almost identical to one reported in a retirement community sample of older people who were administered the CPCI (Ersek et al., 2006), supporting the idea that these are the strategies most used by many older adults to manage chronic pain.
The key finding of this study is that age group moderated the relationship between pain intensity and coping response. Although this finding was statistically significant for only four subscales, trends were noted for two more. It seems statistically unlikely that these trends were the result of familywise error, given that they were in the same direction and nearly the same magnitude as significant results on other scales. In any case, it appears that younger adults reporting greater pain also utilize more coping efforts. A younger adult with a high pain level may spend considerable effort attempting to manage higher levels of pain, presumably using the top-ranked strategies for this group (i.e., task persistence, resting, and asking for assistance). A significant relationship between coping and average pain also existed for middle-aged adults, although the magnitude was weaker. However, older adults reported virtually no relationship between pain intensity and frequency of coping. That is, older adults with greater levels of pain reported no more or less coping activation than did those with lower levels of pain.
Although this interaction is cross-sectional and can therefore be interpreted in several ways, one way to interpret this finding is as evidence for better adjustment to pain in older people. In operant behavioral models of chronic pain, pain becomes reinforced when coping efforts such as rest, medication, and receiving help are pain contingent. Treatment from this perspective emphasizes engaging in healthy behaviors regardless of pain level in an attempt to break the reinforcing relationship between pain and behavior (e.g., Fordyce, 1976). Older adults, or at least the older adults in our sample, appear to have succeeded in this regard. They report using more strategies and using them more frequently, and this did not vary by pain level.
Another line of evidence supporting the problematic nature of pain-contingent coping comes from some recent work in middle-aged patients with rheumatoid arthritis (Conner et al., 2006). In this study, individuals with a history of major depression demonstrated significantly stronger relationships among pain, affect, and certain coping strategies (i.e., venting emotions), suggesting more pain-contingent well-being. This finding existed controlling for current depressive symptoms, neuroticism, and age. Our interpretation also reflects a larger literature suggesting that the ability to regulate emotions in the face of adverse events is a marker of psychological health in general (John & Gross, 2004) and in regard to pain (Davis, Zautra, & Reich, 2001; Hamilton, Zautra, & Reich, 2005). However, these last studies looked only at mood reactivity and not at pain-contingent coping per se.
As to the reason for this different (and, we argue, more efficacious) coping in older adults, several hypotheses could be offered. First, it has been suggested by our group and others that the key ingredient in positive adaptation to pain with age is temporal experience. As time goes on, individuals may learn which coping strategies are the most effective in managing their pain and employ them more consistently or to greater effect. However, in contrast to some of our earlier findings (Molton et al., 2007), effects in the present study existed even after controlling for time since injury or diagnosis. This suggests that some other factors must be at play, such as wider life experience (i.e., coping with a variety of non-pain-related stressors over the course of a lifetime) that may lead to greater general coping self-efficacy in older adults.
Another possibility may be that attributional variables, such as the belief about the “normality” of pain in aging, lead to more effective coping. Although this latter hypothesis has been suggested by many researchers to explain better psychological adjustment to pain and other physical problems in older people (e.g., Cook & Thomas, 1994; Greenlee, 1991; Parmelee, 1997), to our knowledge no direct empirical evidence has been offered to support it. In fact, given the classic conceptualization of coping provided by Lazarus (1986), an attribution that pain was a “normal” part of aging would make the stressor less threatening and thus lead to less activation of coping resources. In our data, we see the complexity of testing this hypothesis: Older adults reported greater frequency of several coping efforts overall but also less coping activation at higher levels of pain.
Some data also suggest that increasing age does not appear to consistently affect the stress appraisal process (at least for middle-aged and older men; Aldwin et al., 1996). Although acceptance of health problems has been shown to exist in older adults (Staudinger & Fleeson, 1996), it appears that this relationship manifests primarily in the very old (e.g., centenarians in Martin et al., 2001). To our knowledge, no studies have compared younger and older adults on the belief that pain is “normal” for their life context; this is a promising area for future research. In any case, we do not suspect that this attribution explains results in the present study because it seems unlikely that individuals would describe pain secondary to NMD or SCI as “normal.”
We interpret these data to suggest that when it comes to managing pain, aging is associated with an accumulation of experiences that contribute to differences in coping. These differences are not so much quantitative as they are qualitative; older people in the present study seem to use a range of techniques that work for them and do not make major changes in response to overall higher levels of pain intensity. It is possible that they have learned that certain strategies are to be avoided (resting), that certain strategies are helpful (pacing), and that pain-contingent coping reinforces pain. This may also be part of a larger process of habituation to pain in aging (Williamson & Schulz, 1995).
Strengths and Limitations
This study is preliminary and has several limitations. Most important, the data in the present study come from self-report community surveys and therefore may suffer from selection bias, response bias, or other limitations of this method. This study was also cross-sectional, which precludes causal inferences. Although a wide range of ages was reported by respondents, most were middle aged, and the older adults in our study were really the youngest old (age M = 65.8, SD = 5.5).
The fact that participants in this study came from a range of chronic neurodegenerative conditions is both a strength and a weakness of the design. Such an approach allows for greater generalizability of findings across disability groups but limits applicability to the “typical” older adult (for whom neurodegenerative disease or injury is not a common experience). This inclusion of multiple disability types also introduces the possibility that differences among illness groups contributed to the findings. For example, we did not measure posttraumatic distress that may be a salient feature for some with SCI and could also affect pain-related coping. Although we did control for medical diagnostic group in our analyses, we may not have captured these differences in their entirety.
Last, many current analyses of the associations of pain coping with pain outcomes control for general emotional state as a way of avoiding the confound of affect on pain report. Unfortunately, we did not include measure general emotional state in this way. Similarly, a measure of physical function or functional disability would be important to include in future research.
These limitations notwithstanding, we believe this study is unique in several ways. This study was able to compare coping strategies to a particular stressor (pain) using a measure specifically designed for that stressor. This “molecular” approach may limit some noise variability associated with using more general coping measures on a range of stressors. Finally, our sample size also allowed us to control for important confounding variables, such as time since injury or diagnosis and sex.
Future Directions
Clearly, the experience of pain in aging is a complicated one. Additional work is needed to understand relationships between pain and pain-related coping in older people. Further work in this area could look into beliefs about pain and aging in older people and compare these beliefs across age groups. For example, do older adults perceive their pain to be less important as a result of social comparison, gladness to be alive, high levels of coping self-efficacy, or other attributional variables? Answering this question could lead to a better understanding of the experience of pain in older people and could contribute to more effective “tailored” interventions.
Some recent work has demonstrated the importance of humor and religious coping in older people (e.g., Celso, Ebener, & Burkhead, 2003). Future work could measure these variables in the context of chronic pain. Finally, it could be argued that more effective coping in older people reflects greater “acceptance” of the pain problem. Although some promising work has been done in this area (e.g., Esteve, Ramirez-Maestre, & Lopez-Martinez, 2007), future efforts are warranted.
Acknowledgments
This research was supported by Grant P01 HD33988 from the National Institutes of Health, National Institute of Child Health and Human Development (National Center for Medical Rehabilitation Research). The authors gratefully acknowledge the contributions of Lindsay Washington, Laura Nishimura, Kevin Gertz, Emily Phelps, Kristin McArthur, Silvia Amtmann, Noel Pereyra-Johnston, Sylia Wilson, Kerry Madrone, Sarah O’Brien, Eric Weitz, Tyler Einheuser, and Sophia Purekal, University of Washington Department of Rehabilitation Medicine, in data collection and database management.
Footnotes
For clarity of visual presentation and interpretation, we performed these post hoc regressions without control variables. However, running the same regressions with the controls above did not significantly alter the pattern or magnitude of the results.
Contributor Information
Ivan Molton, University of Washington School of Medicine.
Mark P Jensen, University of Washington School of Medicine.
Dawn M. Ehde, University of Washington School of Medicine.
Gregory T. Carter, University of Washington School of Medicine.
George Kraft, University of Washington School of Medicine.
Diana D. Cardenas, University of Miami Miller School of Medicine.
References
- Abresch RT, Carter GT, Jensen MP, Kilmer DD. Assessment of pain and health-related quality of life in slowly progressive neuromuscular disease. American Journal of Hospice and Palliative Care. 2002;19:39–47. doi: 10.1177/104990910201900109. [DOI] [PubMed] [Google Scholar]
- Aldwin CM. Does age affect the stress and coping process? Implications of age differences in perceived control. Journal of Gerontology. 1991;46:174–180. doi: 10.1093/geronj/46.4.p174. [DOI] [PubMed] [Google Scholar]
- Aldwin C, Revenson T. Age differences in stress, coping, and the attribution of responsibility. Paper presented at the 93rd annual meeting of the American Psychological Association; Los Angeles. 1985. Aug, [Google Scholar]
- Aldwin CM, Sutton KJ, Chiara G, Spiro A. Age differences in stress, coping and appraisal: Findings from the Normative Aging Study. Journal of Gerontology. 1996;51B:179–188. doi: 10.1093/geronb/51b.4.p179. [DOI] [PubMed] [Google Scholar]
- Archibald CJ, McGrath PJ, Ritvo PG, Fisk JD, Bhan V, Maxner CE, et al. Pain prevalence, severity and impact in a clinic sample of multiple sclerosis patients. Pain. 1994;58:89–93. doi: 10.1016/0304-3959(94)90188-0. [DOI] [PubMed] [Google Scholar]
- Blanchard-Fields F, Sulsky L, Robinson-Whelen S. Moderating effects of age and context on the relationship between gender, sex role differences, and coping. Sex Roles. 1991;25:645–660. [Google Scholar]
- Boerner K. Adaptation to disability among middle-aged and older adults: The role of assimilative and accommodative coping. Journal of Gerontology. 2004;59B:35–42. doi: 10.1093/geronb/59.1.p35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bookwala J, Harralson T, Parmelee P. Effects of pain on functioning and well-being in older adults with osteoarthritis of the knee. Psychology of Aging. 2003;18:844–850. doi: 10.1037/0882-7974.18.4.844. [DOI] [PubMed] [Google Scholar]
- Catala E, Reig E, Artes M, Aliaga L, Lopez J, Segu J. Prevalence of pain in the Spanish population: Telephone survey in 5000 homes. European Journal of Pain. 2002;6:133–140. doi: 10.1053/eujp.2001.0310. [DOI] [PubMed] [Google Scholar]
- Celso BG, Ebener DJ, Burkhead EJ. Humor coping, health status, and life satisfaction among older adults residing in assisted living facilities. Aging & Mental Health. 2003;7:438–445. doi: 10.1080/13607860310001594691. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Lower extremity disease among persons aged > or = 40 years with and without diabetes—United States, 1999–2002. Morbidity Mortality Weekly Report. 2005;18:1158–1160. [PubMed] [Google Scholar]
- Conner TS, Tennen H, Zautra AJ, Affleck G, Armeli S, Fifield J. Coping with rheumatoid arthritis pain in daily life: Within-person analyses reveal hidden vulnerability for the formerly depressed. Pain. 2006;126:198–209. doi: 10.1016/j.pain.2006.06.033. [DOI] [PubMed] [Google Scholar]
- Cook A, Thomas M. Pain and the use of health services among the elderly. Journal of Aging and Health. 1994;6:155–172. doi: 10.1177/089826439400600202. [DOI] [PubMed] [Google Scholar]
- Cooper J, Kohlmann T. Factors associated with health status of older Americans. Age and Ageing. 2001;30:495–501. doi: 10.1093/ageing/30.6.495. [DOI] [PubMed] [Google Scholar]
- Davidson H, Feldman P, Crawford S. Measuring depressive symptoms in the frail elderly. Journal of Gerontology. 1994;49B:159–164. doi: 10.1093/geronj/49.4.p159. [DOI] [PubMed] [Google Scholar]
- Davis MC, Zautra AJ, Reich JW. Vulnerability to stress among women in chronic pain from fibromyalgia and osteoarthritis. Annals of Behavioral Medicine. 2001;23:215–226. doi: 10.1207/S15324796ABM2303_9. [DOI] [PubMed] [Google Scholar]
- Diehl M, Coyle N, Labouvie-Vief G. Age and sex differences in strategies of coping and defense across the lifespan. Psychology and Aging. 1996;1996:127–139. doi: 10.1037//0882-7974.11.1.127. [DOI] [PubMed] [Google Scholar]
- Dorantes-Mendoza G, Avila-Funes JA, Mejía-Arango S, Gutiérrez-Robledo LM. Factors associated with functional dependence in older adults: A secondary analysis of the National Study on Health and Aging, Mexico. Rev Panam Salud Publica. 2007;22:1–11. doi: 10.1590/s1020-49892007000600001. [DOI] [PubMed] [Google Scholar]
- Edwards R. Age differences in the correlates of physical functioning in patients with chronic pain. Journal of Aging and Health. 2006;18:56–69. doi: 10.1177/0898264305280976. [DOI] [PubMed] [Google Scholar]
- Ehde D, Jensen M, Engel J, Turner J, Hoffman A, Cardenas D. Chronic pain secondary to disability: A review. Clinical Journal of Pain. 2003;19:197–210. doi: 10.1097/00002508-200301000-00002. [DOI] [PubMed] [Google Scholar]
- Ehde D, Osborne T, Hanley MA, Jensen MP, Kraft GH. The scope and nature of pain in persons with multiple sclerosis. Multiple Sclerosis. 2006;12:629–638. doi: 10.1177/1352458506071346. [DOI] [PubMed] [Google Scholar]
- Ersek M, Turner JA, Kemp CA. Use of the Chronic Pain Coping Inventory to assess older adults’ pain coping strategies. Journal of Pain. 2006;7:833–842. doi: 10.1016/j.jpain.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Esteve R, Ramirez-Maestre C, Lopez-Martinez A. Adjustment to chronic pain: The role of pain acceptance, coping strategies, and pain-related cognitions. Annals of Behavioral Medicine. 2007;33:179–188. doi: 10.1007/BF02879899. [DOI] [PubMed] [Google Scholar]
- Ferrell B, Ferrell B, Osterweil D. Pain in the nursing home. Journal of the American Geriatrics Society. 1990;38:409–414. doi: 10.1111/j.1532-5415.1990.tb03538.x. [DOI] [PubMed] [Google Scholar]
- Finnerup N, Johannesen I, Sindrup S, Bach F, Jensen T. Pain and dysethesia in patients with spinal cord injury: A postal survey. Spinal Cord. 2001;39:256–262. doi: 10.1038/sj.sc.3101161. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS, Pimley S, Novacek J. Age differences in stress and coping processes. Psychology and Aging. 1987;2:171–184. doi: 10.1037//0882-7974.2.2.171. [DOI] [PubMed] [Google Scholar]
- Fordyce WE. Behavioral methods for chronic pain illness. St Louis MO: C. V. Mosby; 1976. [Google Scholar]
- Frisbie J, Aguilera E. Chronic pain after spinal cord injury: An expedient diagnostic approach. Paraplegia. 1990;28:460–465. doi: 10.1038/sc.1990.62. [DOI] [PubMed] [Google Scholar]
- Gallagher R, Merna S, Mossey J. Chronic pain: Sources of late-life pain and risk factors for disability. Geriatrics. 2000;55:40–45. [PubMed] [Google Scholar]
- Greenlee K. Pain and analgesia: Considerations for the elderly in critical care. AACN Clinical Issues in Critical Care Nursing. 1991;2:720–728. doi: 10.4037/15597768-1991-4012. [DOI] [PubMed] [Google Scholar]
- Hadjistavropoulos HD, MacLeod FK, Asmundson GJ. Validation of the Chronic Pain Coping Inventory. Pain. 1999;80:471–481. doi: 10.1016/S0304-3959(98)00224-3. [DOI] [PubMed] [Google Scholar]
- Haisma JA, van der Woude LH, Stam HJ, Bergen MP, Sluis TA, Post MW, et al. Complications following spinal cord injury: Occurrence and risk factors in a longitudinal study during and after inpatient rehabilitation. Journal of Rehabilitation Medicine. 2007;39:393–398. doi: 10.2340/16501977-0067. [DOI] [PubMed] [Google Scholar]
- Hamilton NA, Zautra AJ, Reich JW. Affect and pain in rheumatoid arthritis: Do individual differences in affective regulation and affective intensity predict emotional recovery from pain? Annals of Behavioral Medicine. 2005;29:216–224. doi: 10.1207/s15324796abm2903_8. [DOI] [PubMed] [Google Scholar]
- Holmbeck G. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Idler EL. Age differences in self assessments of health: Age changes, cohort differences, or survivorship? Journals of Gerontology. 1993;48:S289–S300. doi: 10.1093/geronj/48.6.s289. [DOI] [PubMed] [Google Scholar]
- Irion JC, Blanchard-Fields F. A cross-sectional comparison of adaptive coping in adulthood. Journal of Gerontology. 1987;42:502–504. doi: 10.1093/geronj/42.5.502. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Abresch RT, Carter GT, McDonald CM. Chronic pain in persons with neuromuscular disease. Archives of Physical Medicine and Rehabilitation. 2005;86:1155–1163. doi: 10.1016/j.apmr.2004.11.028. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Ehde DM, Hoffman AJ, Patterson DR, Czerniecki JM, Robinson LR. Cognitions, coping and social environment predict adjustment to phantom limb pain. Pain. 2002;95:133–142. doi: 10.1016/s0304-3959(01)00390-6. [DOI] [PubMed] [Google Scholar]
- Jensen M, Hanley M, Turner J, Cardenas D. Pain and other sensation in persons with spinal cord injury: Frequency and association with depression and pain interference. Psychologica. 2004;37:129–143. [Google Scholar]
- Jensen M, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R, editors. Handbook of pain assessment. 2nd ed. New York: Guilford; 2000. pp. 135–151. [Google Scholar]
- Jensen M, Karoly P, O’Riordan E, Bland F, Burns R. The subjective experience of acute pain: An assessment of the utility of 10 indices. Clinical Journal of Pain. 1989;5:153–159. doi: 10.1097/00002508-198906000-00005. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Kuehn CM, Amtmann D, Cardenas DD. Symptom burden in persons with spinal cord injury. Archives of Physical Medicine & Rehabilitation. 2007;88:638–645. doi: 10.1016/j.apmr.2007.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen MP, Turner JA, Romano JM, Lawler BK. Relationship of pain-specific beliefs to chronic pain adjustment. Pain. 1994;57:301–309. doi: 10.1016/0304-3959(94)90005-1. [DOI] [PubMed] [Google Scholar]
- Jensen MP, Turner JA, Romano JM, Strom SE. The Chronic Pain Coping Inventory: Development and preliminary validation. Pain. 1995;60:203–216. doi: 10.1016/0304-3959(94)00118-X. [DOI] [PubMed] [Google Scholar]
- John OP, Gross JJ. Healthy and unhealthy emotion regulation: Personality processes, individual differences, and life span development. Journal of Personality. 2004;72:1301–1333. doi: 10.1111/j.1467-6494.2004.00298.x. [DOI] [PubMed] [Google Scholar]
- Kassirer M. Multiple sclerosis and pain. International Journal of MS Care. 2000;2:30–38. [Google Scholar]
- Keefe FJ, Williams DA. A comparison of coping strategies in chronic pain patients across different age groups. Journal of Gerontology. 1990;45:161–165. doi: 10.1093/geronj/45.4.p161. [DOI] [PubMed] [Google Scholar]
- Krause N, Jay G, Liang J. Financial strain and psychological well-being among the American and Japanese elderly. Psychology & Aging. 1991;6:170–181. doi: 10.1037//0882-7974.6.2.170. [DOI] [PubMed] [Google Scholar]
- LaChapelle DL, Hadjistavropoulos T. Age-related differences among adults coping with pain: Evaluation of a developmental life-context model. Canadian Journal of Behavioral Science. 2005;37:123–137. [Google Scholar]
- Langsrud O. ANOVA for unbalanced data: Use Type II instead of Type III sums of squares. Statistics and Computing. 2003;13:163–167. [Google Scholar]
- Lazarus RS. Stress and coping. In: Maddox GL, editor. Encyclopedia of aging. New York: Springer; 1986. pp. 647–649. [Google Scholar]
- Lipton R, Pfeffer D, Newman L, Solomon S. Headaches in the elderly. Journal of Pain and Symptom Management. 1993;8:87–97. doi: 10.1016/0885-3924(93)90106-6. [DOI] [PubMed] [Google Scholar]
- Magni G, Marchetti M, Moreschi C, Merskey H, Luchini SR. Chronic mus-culoskeletal pain and depressive symptoms in the National Health and Nutrition Examination: I. Epidemiologic follow-up study. Pain. 1993;53:163–168. doi: 10.1016/0304-3959(93)90076-2. [DOI] [PubMed] [Google Scholar]
- Martin P, Rott C, Poon LW, Courtenay B, Lehr U. A molecular view of coping behavior in older adults. Journal of Aging and Health. 2001;13:72–91. doi: 10.1177/089826430101300104. [DOI] [PubMed] [Google Scholar]
- McCrae RR. Age differences and changes in the use of coping mechanisms. Journal of Gerontology. 1982;44B:161–169. doi: 10.1093/geronj/44.6.p161. [DOI] [PubMed] [Google Scholar]
- Meeks S, Carstensen L, Tamsky B, Wright T, Pellegrini D. Age differences in coping: Does less mean worse? International Journal of Aging and Human Development. 1989;28:127–140. doi: 10.2190/UXKQ-4J3X-TEHT-7NU2. [DOI] [PubMed] [Google Scholar]
- Molton I, Jensen M, Ehde D, Smith D. Phantom limb pain and pain interference in adults with lower extremity amputation: The moderating effects of age. Rehabilitation Psychology. 2007;52:272–279. [Google Scholar]
- Moos RH, Brennan PL, Schutte KK, Moos BS. Older adults’ coping with negative life events: Common processes of managing health, interpersonal, and financial/work stressors. International Journal of Aging and Human Development. 2006;62:39–59. doi: 10.2190/ENLH-WAA2-AX8J-WRT1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murrell SA, Norris FH, Hutchins GL. Distribution and desirability of life events in older adults: Population and policy implications. Journal of Community Psychology. 1984;64:301–311. [Google Scholar]
- Novy D. Psychological approaches for managing chronic pain. Journal of Psychopathology and Behavioral Assessment. 2004;26:279–288. [Google Scholar]
- Parmelee P. Pain and psychological function in late life. In: Mostofsky DI, Lomranz J, editors. Handbook of pain and aging. New York: Plenum; 1997. pp. 207–226. [Google Scholar]
- Parmelee P, Smith B, Katz I. Pain complaints and cognitive status among elderly institution residents. Journal of the American Geriatrics Society. 1993;41:517–522. doi: 10.1111/j.1532-5415.1993.tb01888.x. [DOI] [PubMed] [Google Scholar]
- Paykel ES. Methodological aspects of life events research. Journal of Psychosomatic Research. 1983;27:341–352. doi: 10.1016/0022-3999(83)90065-x. [DOI] [PubMed] [Google Scholar]
- Perkins FM, Moxley RT, Papciak AS. Pain in multiple sclerosis and the muscular dystrophies. In: Block AR, Kremer F, Fernandez E, editors. Handbook of pain syndromes: Biopsychosocial perspectives. Mahwah, NJ: Lawrence Erlbaum; 1999. pp. 349–370. [Google Scholar]
- Radloff L, Teri L. Use of the Center for Epidemiologic Studies Depression Scale with older adults. Clinical Gerontologist. 1986;5:119–135. [Google Scholar]
- Raichle KA, Hanley M, Jensen MP, Cardenas DD. Cognitions, coping, and social environment predict adjustment to pain in spinal cord injury. Journal of Pain. 2007;8:718–729. doi: 10.1016/j.jpain.2007.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakowski W, Cryan CD. Associations among health perceptions and health status within three age groups. Journal of Aging and Health. 1990;2:58–80. [Google Scholar]
- Riley J, Wade J, Robinson M, Price D. The stages of pain processing across the adult lifespan. Journal of Pain. 2000;1:162–170. [Google Scholar]
- Romano JM, Turner JA, Jensen MP, Friedman LS, Bulcroft RA, Hops H, et al. Chronic pain patient-spouse behavioral interactions predict patient disability. Pain. 1995;63:353–360. doi: 10.1016/0304-3959(95)00062-3. [DOI] [PubMed] [Google Scholar]
- Roy R, Thomas M. Pain, depression and illness behavior in a community sample of active elderly persons: Elderly persons with and without pain, part 2. Clinical Journal of Pain. 1988;3:207–211. [Google Scholar]
- Rustoen T, Wahl A, Banestad B, Lerdal A, Paul S, Miaskowski C. Age and the experience of chronic pain: Differences in health and quality of life among younger, middle-aged, and older adults. Clinical Journal of Pain. 2005;21:513–523. doi: 10.1097/01.ajp.0000146217.31780.ef. [DOI] [PubMed] [Google Scholar]
- Sidak Z. Rectangular confidence regions for the means of multivariate normal distributions. Journal of the American Statistical Association. 1967;62:626–633. [Google Scholar]
- Siddal P, Loeser J. Pain following spinal cord injury. Spinal Cord. 2001;39:63–77. doi: 10.1038/sj.sc.3101116. [DOI] [PubMed] [Google Scholar]
- Silverman M, Eichler A, Williams G. Self-reported stress: Findings from the 1985 National Health Interview Survey. Public Health Reports. 1987;102:47–53. [PMC free article] [PubMed] [Google Scholar]
- Sofaer B, Moore A, Holloway I, Lamberty J, Thorp T, O’Dwyer J. Chronic pain as perceived by older people: A qualitative study. Age and Ageing. 2005;34:462–466. doi: 10.1093/ageing/afi139. [DOI] [PubMed] [Google Scholar]
- Sorkin BA, Rudy TE, Hanlon RB, Turk DC, Stieg RL. Chronic pain in old and young patients: Differences appear less important than similarities. Journal of Gerontology: Psychological Sciences. 1990;45:63–68. doi: 10.1093/geronj/45.2.p64. [DOI] [PubMed] [Google Scholar]
- Srikanth C, Fryer J, Zhai G, Winzenberg T, Hosmer D, Jones G. A meta-analysis of sex differences in prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage. 2005;13:769–781. doi: 10.1016/j.joca.2005.04.014. [DOI] [PubMed] [Google Scholar]
- Staudinger UM, Fleeson W. Self and personality in old and very old age: A sample case of resilience? Development and Psychopathology. 1996;5:541–566. [Google Scholar]
- Tan G, Nguyen Q, Anderson KO, Jensen MP, Thornby J. Further validation of the Chronic Pain Coping Inventory. Journal of Pain. 2005;6:29–40. doi: 10.1016/j.jpain.2004.09.006. [DOI] [PubMed] [Google Scholar]
- Thomas E, Peat G, Harris L, Wilkie R, Croft P. The prevalence of pain and pain interference in a general population of older adults: Cross sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP) Pain. 2004;110:361–368. doi: 10.1016/j.pain.2004.04.017. [DOI] [PubMed] [Google Scholar]
- Turner J, Cardenas D. Chronic pain problems in individuals with spinal cord injuries. Seminars in Clinical Neuropsychiatry. 1999;4:186–194. doi: 10.153/SCNP00400186. [DOI] [PubMed] [Google Scholar]
- Vaillant G. Adaptation to life. Boston: Little, Brown; 1977. [Google Scholar]
- Widerstrom-Noga E, Turk D. Types and effectiveness of treatments used by people with chronic pain associated with spinal cord injuries: Influence of pain and psychosocial characteristics. Spinal Cord. 2003;41:600–609. doi: 10.1038/sj.sc.3101511. [DOI] [PubMed] [Google Scholar]
- Williamson G. The central role of restricted normal activities in adjustment to illness and disability: A model of depressed affect. Rehabilitation Psychology. 1998;43:327–347. [Google Scholar]
- Williamson G, Schulz R. Activity restriction mediates the association between pain and depressed affect: A study of younger and older adult cancer patients. Psychology & Aging. 1995;10:369–378. doi: 10.1037//0882-7974.10.3.369. [DOI] [PubMed] [Google Scholar]