Abstract
Background:
Although physicians sometimes use the futility rationale to limit the use of life-sustaining treatments, little is known about how surrogate decision makers view this rationale. We sought to determine the attitudes of surrogates of patients who are critically ill toward whether physicians can predict futility and whether these attitudes predict surrogates' willingness to discontinue life support when faced with predictions of futility.
Methods:
This multicenter, mixed qualitative and quantitative study took place at three hospitals in California from 2006 to 2007. We conducted semistructured interviews with surrogate decision makers for 50 patients who were critically ill and incapacitated that addressed their beliefs about medical futility and inductively developed an organizing framework to describe these beliefs. We used a hypothetical scenario with a modified time–trade-off design to examine the relationship between a patient's prognosis and a surrogate's willingness to withdraw life support. We used a mixed-effects regression model to examine the association between surrogates' attitudes about futility and their willingness to limit life support in the face of a very poor prognosis. Validation methods included the use and integration of multiple data sources, multidisciplinary analysis, and member checking.
Results:
Sixty-four percent of surrogates (n = 32; 95% confidence interval [CI], 49 to 77%) expressed doubt about the accuracy of physicians' futility predictions, 32% of surrogates (n = 16; 95% CI, 20 to 47%) elected to continue life support with a < 1% survival estimate, and 18% of surrogates (n = 9; 95% CI, 9 to 31%) elected to continue treatment when the physician believed that the patient had no chance of survival. Surrogates with religious objections to the futility rationale (n = 18) were more likely to request continued life support (odds ratio, 4; 95% CI, 1.2 to 14.0; p = 0.03) than those with secular or experiential objections (n = 15; odds ratio, 0.95; 95% CI, 0.3 to 3.4; p = 0.90).
Conclusions:
Doubt about physicians' ability to predict medical futility is common among surrogate decision makers. The nature of the doubt may have implications for responding to conflicts about futility in clinical practice.
Physicians' use of medical futility judgments as a rationale to withdraw life-sustaining treatments over the objections of surrogate decision makers remains controversial. Much of the debate from the past few years1 has focused on who has the authority to determine what goals of treatment are worthwhile. This trend recognizes that many disputes about futility are in fact disagreements between clinicians and surrogates about what is a valuable health state and at what cost it should be pursued. Although attempts2 have been made to craft substantive rather than purely procedural guidelines to define circumstances in which life-sustaining treatment should be withdrawn, such policies have not been widely accepted.3–5
Nonetheless, general consensus5 is that physicians need not provide treatments that will not accomplish their intended goal. The validity of this definition of the futility rationale rests in part on an assumption that physicians can predict with absolute certainty that an intervention will not accomplish its intended goal. However, prior studies6 of patients (not surrogates) have revealed that a small, but significant proportion question this rationale. Our clinical experience and recent research7 suggest that this questioning also may occur within the hospital ICU setting. However, few systemically gathered empirical data examine surrogates' perspectives about physician futility judgments within clinical practice. Therefore, we conducted a mixed qualitative and quantitative study to explore the attitudes of surrogates for patients who are critically ill about whether physicians can predict futility and whether these attitudes predict surrogates' willingness to discontinue life support when physicians assert that it will be ineffective.
Materials and Methods
Between June 2006 and March 2007, we conducted a multicenter, mixed qualitative and quantitative study in three hospitals in California, including a Veterans Affairs hospital, a tertiary academic hospital, and a public county hospital. All study procedures were approved by the institutional review board at each participating hospital.
Study investigators identified eligible surrogates of patients who were critically ill by screening 1 day per week at each institution with a systematic sampling technique in which we made a standardized pass through each ICU and screened the first patient-surrogate pair we encountered. At each institution where data collection was performed, beds are filled on a first-come, first-served basis. Participants were eligible if they spoke English well enough not to require the use of an interpreter to interact with health-care providers, were at least 18 years of age, and were involved in decision making for a patient who was critically ill and incapacitated. Prior to approaching any potential participants, we obtained permission from the patient's attending physician to do so. All surrogates provided written consent, completed a demographic questionnaire, and participated in a one-on-one semistructured interview that was audiotaped and transcribed.
Semistructured Interviews
At the beginning of the interview, participants were read a standardized prompt (Table 1). The interviewer used techniques of cognitive interviewing8 to pursue and clarify emergent themes as they arose. The goals were to quantify the proportion of surrogates who expressed doubt about physicians' ability to predict futility and qualitatively understand the nature of the doubt. The interviewer followed up surrogates' responses, pursued themes as they arose, and sought clarification or elaboration.
Table 1.
Standardized Interview Prompts
| Prompt Read to Surrogates Prior to Standardized Interview | Prompt Read to Surrogates Prior to Modified Time–Trade-Off Scenario |
|---|---|
| I'd like you to imagine the following situation: Your loved one is admitted to the ICU with a life-threatening illness. S/he is on a breathing machine and can't speak for him/herself and you are asked to make decisions for him/her. The doctors sit down to discuss your loved one's situation with you and say that your loved one will not survive the hospitalization. If the doctor thought there was absolutely no chance for your loved one to survive the hospitalization, would you believe the doctor? Why or why not? | Imagine that for the past 2 weeks, your loved has been in the ICU because of a life-threatening illness. During this time, s/he has been on a mechanical ventilator because s/he is not able to breathe on his/her own. A ventilator is a machine that breathes for your loved one. It involves a tube being placed through your loved one's mouth and into their windpipe. While on the ventilator your loved one has not been able to eat, talk, or get out of bed. S/he has been fed through a tube placed through his/her mouth and into his/her stomach. Friends and family have been able to visit your loved one, but they have not been able to stay with them all the time. The ventilator occasionally has been uncomfortable for your loved one, but doctors have given him/her medicines to help. The medicines have kept your loved one sleepy most of the time. The main doctor comes to you and explains that your loved one has not improved as quickly as hoped. He informs you that in order to have any chance of surviving, your loved one will need to remain in the ICU for 1 month followed by 1 month of rehabilitation in a nursing facility. This plan of care would involve the placement of a surgical breathing tube in his/her neck. In addition, a surgical feeding tube would be placed into his/her stomach through their skin. If your loved one survived, the doctors think that he/she would be able to return to the same level of functioning s/he had before this hospitalization. |
Modified Time–Trade-Off Technique
Following the semistructured interview, surrogates were presented with a standardized scenario (Table 1). They were told that the patient's estimated chance of survival was “x%,” with x = 100, 80, 50, 20, 10, 5, 1, <1, and 0. For each value of x, surrogates were shown a “wall of people” to supplement the numeric presentation of risk with a visual depiction of the survival estimate.9–11 For example, a surrogate was asked the following question as he or she was shown the graphic depiction of 100% chance of survival: “Do you think it would be appropriate to pursue the treatments I just mentioned for your loved one if the doctors felt there was a 100% chance of survival?” If the surrogate answered “yes,” the question was repeated with an 80% chance of survival. This process continued down to a 0% chance of surviving or until the surrogate indicated that he or she believed that it would be appropriate to stop life-sustaining treatments. Although several methods12 exist to assess treatment preferences, including the standard gamble and time trade-off, there is no consensus that one method is best. We chose the modified time–trade-off technique to allow comparison of our data to similar studies.13
Qualitative Data Analysis
Development of the Coding Framework:
The audiotaped interviews were transcribed verbatim by a medical transcriptionist. We used constant comparative methods to develop a framework to describe surrogates' attitudes about physicians' futility predictions. Constant comparison is a general qualitative methodology14,15 for developing theory inductively from data that are systematically gathered and analyzed and often is used when existing conceptual frameworks for the topics under study are inadequate. To develop the preliminary coding scheme, two investigators independently read and performed open (line-by-line) coding of a subset of the transcripts to identify themes and concepts relating to surrogates' attitudes about medical futility. As concepts accumulated and distinctions between concepts became more refined, similar concepts were grouped into conceptual categories. These categories were developed further by comparing the categories among transcripts. All investigators reviewed this preliminary framework and, through a series of investigator meetings, arrived at a consensus on the coding framework.14,16 We modified the framework iteratively over the study period when interviews yielded new themes or ideas.
For the purposes of coding, we defined skepticism about physicians' futility predictions as any statement by a surrogate during the qualitative interview that indicated doubt about physicians' ability to accurately predict futility. We defined acceptance of futility as the absence of expression of skepticism or doubt about the ability of physicians to accurately predict futility.
Reliability of the Coding:
Using the final coding framework, one investigator coded all the interviews by listening to the audiotapes and reading the transcripts. To assess intercoder reliability, another investigator coded a random sample of 20% of the transcripts. Both coders were blinded to the demographic characteristics of the surrogates and to each other's coding. The average κ statistic for assigning individual codes in the transcripts was 0.95 (range, 0.91 to 1.00). A κ value > 0.8 represents excellent interrater reliability.17
Validity of the Findings:
We used two techniques18,19 to ensure the validity of our findings. First, we used a multidisciplinary approach in developing the qualitative coding framework. Areas of investigator expertise are bioethics, critical care medicine, general internal medicine, physician-patient communication, and end-of-life care. A multidisciplinary approach minimizes the chance that individual bias threatens the validity of the findings. Second, we used multiple types of data to pursue the research question, including qualitative interview data and quantitative data from the modified time–trade-off analysis. Near the end of the study, we presented the preliminary conceptual framework to study participants for confirmation and modification, a process known as member checking.19
Quantitative Analysis
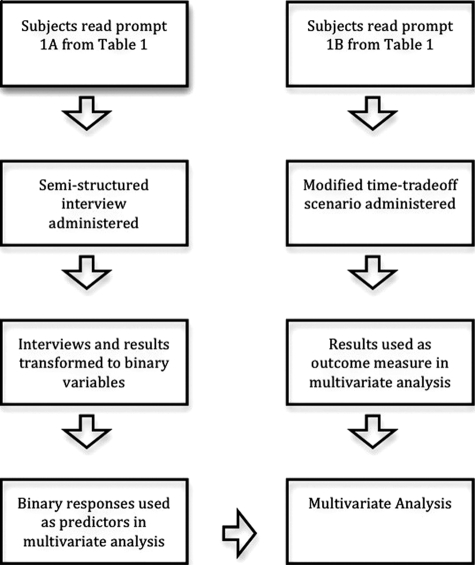
We transformed the results of the qualitative interview into quantitative (binary) data to determine whether the presence and nature of doubt about physicians' predictions of futility were associated with an unwillingness to withdraw life support in the face of a very poor prognosis (Fig 1). For example, if a surrogate revealed during the interview that he or she doubted physicians' prognostications because he or she believed in miracles, this was transformed into the presence of a religious objection to futility. We used a mixed-effects logistic regression model to examine the association between surrogates' attitudes on physicians' ability to predict futility and their willingness to withdraw life support in the face of a very poor prognosis. A mixed-effects model permits appropriate analysis of clustered data. All analyses were performed with statistical software (STATA, version 9.0; StataCorp LP; College Station, TX). All reported p values are two-sided, with statistical significance set at p < 0.05.
Figure 1.
Flow diagram of data collection and analysis.
Results
Participant Characteristics
Of 58 eligible surrogates, 50 were included in the study, for an enrollment rate of 86%. Their demographic characteristics are described in Table 2. For nine patients, we enrolled two individuals who indicated that they were sharing responsibilities for surrogate decision making; for four patients, three individuals indicating that they were sharing responsibility were enrolled into the study. Table 3 describes the patients' demographic characteristics.
Table 2.
Demographic Characteristics of Surrogate Decision Makers
| Characteristics | Values |
|---|---|
| Age,* yr | 55.2 (13.4) |
| Gender | |
| Male | 16 (32) |
| Female | 34 (68) |
| Race or ethnicity† | |
| White | 20 (40) |
| Black | 12 (24) |
| Hispanic | 10 (20) |
| Asian | 5 (10) |
| Native American | 2 (4) |
| Pacific Islander | 1 (2) |
| Other or undocumented | 1 (3) |
| Relationship to patient | |
| Spouse or partner | 14 (28) |
| Sibling | 11 (22) |
| Child | 8 (16) |
| Parent | 5 (13) |
| Other relative | 5 (13) |
| Friend | 4 (8) |
| Other | 3 (6) |
| Level of education | |
| Eighth grade or less | 0 (0) |
| Some high school | 4 (8) |
| High school diploma or general equivalency diploma | 15 (30) |
| Some college or trade school | 17 (34) |
| A 4-year college degree | 5 (10) |
| Graduate or professional school | 9 (18) |
| Primary language‡ | |
| English | 48 (96) |
| Spanish | 6 (12) |
| Cantonese | 3 (6) |
| Mandarin | 1 (2) |
| French | 1 (2) |
| German | 1 (2) |
| Armenian | 1 (2) |
| Religious preference | |
| Christian | 17 (34) |
| Catholic | 8 (16) |
| Protestant | 6 (12) |
| No religious affiliation | 4 (8) |
| Declined response | 4 (8) |
| Baptist | 3 (6) |
| Methodist | 3 (6) |
| Lutheran | 2 (4) |
| Jewish | 1 (2) |
| Seventh Day Adventist | 1 (2) |
| Apostolic | 1 (2) |
| Importance of religion in everyday life§ | |
| Declined response | 4 (8) |
| Not at all important | 2 (4) |
| Not too important | 7 (14) |
| Fairly important | 17 (34) |
| Very important | 20 (40) |
Values are given as No. (%), unless otherwise indicated. Total No. of surrogates, 50.
*Values are given as the mean (SD).
†Sums are > 50 surrogates because some individuals identified with more than one race or ethnicity.
‡Sums are > 50 surrogates because some individuals cited more than one primary language.
§Surrogates' religiosity was assessed with the following question, with the answer rated using a 4-point Likert scale: How important are religious or spiritual beliefs to your everyday life?
Table 3.
Demographic Characteristics of Patients in the Hospital ICU
| Characteristics | Values |
|---|---|
| Age,* yr | 65.2 (19.7) |
| Gender | |
| Male | 21 (68) |
| Female | 10 (32) |
| Race or ethnicity† | |
| White | 15 (48) |
| Black | 6 (19) |
| Hispanic | 4 (13) |
| Asian | 2 (6) |
| Native American | 2 (6) |
| Pacific Islander | 1 (3) |
| Other or undocumented | 1 (3) |
| Admitting diagnosis | |
| Cardiac failure or myocardial infarction | 9 (29) |
| Intracranial aneurysm or hemorrhage | 4 (13) |
| Sepsis or infection | 3 (10) |
| Respiratory failure | 3 (10) |
| Trauma | 2 (6) |
| Renal failure | 2 (6) |
| GI bleed | 2 (6) |
| Other | 6 (19) |
Values are given as No. (%), unless otherwise indicated. Total No. of patients, 31.
*Values are given as the mean (SD).
†Sums are > 31 patients because some individuals identified with more than one race or ethnicity.
Surrogates' Attitudes About Predicting Physiologic Futility
Sixty-four percent of surrogates expressed a reluctance or unwillingness to believe physicians' futility predictions. They provided the following four main explanations for this belief: a skepticism about physicians' ability to achieve complete prognostic certainty, a need to see for themselves that a patient was incapable of recovery, a need to triangulate multiple information sources before believing physicians, and a belief that God could intervene to change the course of an illness. Next, we describe the four main themes in detail.
Skepticism About Physicians' Prognostic Abilities:
The most common concern raised by surrogates (n = 20) was that predicting the future with the certainty required for a futility judgment is beyond physicians' capabilities. For many, this idea was based on a belief that some aspects of life are mysterious even to physicians. The elderly wife of a patient who was intubated explained, “I have been around too long, seen too many things to know that we really don't know what's gonna happen. People can come from their deathbed back. Or, sometimes they can, from one day to the next, pass away. I never understood that, I don't think doctors understand that or can predict that either.”
For other surrogates, this belief arose from prior experiences with inaccurate prognostication. The son of a woman with critical illness superimposed on cancer referred to her long battle with cancer as, “My mom is a case. I think she was given 6, maybe 18 months before she was absolutely supposed to die … and she's lived 9 years. She had cancer. She did chemo, she had fluid in her lungs, and she had the fluid taken out …. And she's lived 9 years.”
A Need To See for Themselves:
Some surrogates (n = 12) described how their own observations of the patient would allow them to determine whether further medical intervention would be futile. One surrogate believed that he would be able to identify futility because he had “seen death with his own eyes” and knew “what to look for in a person when a person is dying.” The mother of a young trauma patient described how she would observe her son's physical appearance and determine whether treatment was futile, describing, “I'm looking to see … if there are any physical signs that I can see, like moaning, crying … or tubes coming all off their body. [I'm looking to see if] they are just a vegetable.”
Other surrogates emphasized the need to observe the patient's condition over time to assess whether the situation was truly hopeless. One father who was making decisions for his middle-aged daughter with end-stage renal disease needed to “give it a little time to see if anything changes.” When asked what he would need to see before accepting a futility prediction, he remarked, “If they are laying there like a vegetable, and you don't see no improvement for days … then what the doctor says is gonna happen, is gonna happen.”
Triangulation of Multiple Sources of Information:
Roughly one third of surrogates (n = 14) described a process of synthesizing multiple types and sources of information to determine the gravity of the patient's condition. In the following statement, the adult child of a patient with heart failure described the importance of consistent prognostication from different physicians: “I always want a second opinion. I'd want check and balance. In other words, I'm not going to believe everything that [the physician] tells me … I still need a second opinion. Another expert opinion tells me that, yeah, you know, he's right and there's no hope.”
Another surrogate described the following process of triangulating three distinct information sources to determine his impression of the accuracy of a futility prediction: prior experiences with illness, information from the physician, and visual observation of the patient, saying, “I'm trying to be … unemotional about what I'm hearing. I'm trying to assess everything through my personal experiences, through the doctor's explanations, and with my own eyes. And taking all these things into account, I'm trying to come up with an accurate judgment about what is going to happen to the patient.”
God Can Intervene in a Hopeless Situation:
Based on religious grounds, roughly one third of surrogates (n = 18) doubted physicians' ability to predict futility. These individuals believed that God was capable of miraculously healing patients regardless of the severity of their illness. One surrogate summed up this belief by stating, “[The patient] may be really sick, but there may be a miracle …. God might decide it's not their time.” These surrogates believed that miracles occur without the understanding or foresight of physicians. One described her perception of the role of miracles in healing patients who are critically ill, saying, “I don't think miracles happen often, but they do happen. They definitely don't happen regularly or in a set way, so no one knows when they will occur …. Doctors don't know when they are going to happen because they are people like everyone else. But they can happen, and they do happen.”
Survival Estimates in Surrogate Decisions To Withhold Treatment
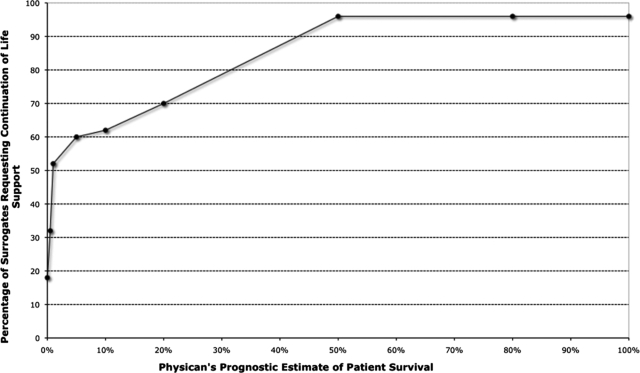
Figure 2 illustrates the percentage of surrogates who requested continuation of life support with decreasing chances of survival to hospital discharge. Surrogate willingness to consent to treatment declined as the prognosis worsened. Notably, 32% (n = 16; 95% confidence interval [CI], 20 to 47%) elected to continue treatment with a < 1% survival estimate, and 18% (n = 9; 95% CI, 9 to 31%) elected to continue treatment when the physician believed that there was no chance of survival.
Figure 2.
Percentage of surrogates requesting continuation of life support based on physicians' survival estimates.
The Impact of Religious vs Secular or Experiential Reasons for Doubt on Treatment Decisions
Surrogates who doubted physician's futility predictions clustered into the following two general groups: those whose doubt was based on religious beliefs (n = 18); and those whose doubt was based on secular considerations (n = 15), such as past experiences with inaccurate prognostication, a secular belief that future-telling is inherently inaccurate, and a need to triangulate physicians prognostications with other sources before accepting the prognosis as true. Surrogates who doubted physicians' futility predictions on religious grounds were more likely to request continued life support in the face of a very poor prognosis (odds ratio, 4; 95% CI, 1.2 to 14.0; p = 0.03), whereas those whose doubt was based on secular concerns were not (odds ratio, 0.95; 95% CI, 0.3 to 3.4; p = 0.90).
Discussion
Our findings provide new insight about the perspectives of surrogate decision makers on the medical futility rationale and point to practical considerations that may help to refine how physicians approach discussions about futility with surrogates. Most surrogates we interviewed were reluctant to immediately accept physicians' predictions of medical futility. We identified several explanations for this finding, including beliefs that individual physicians' predictions may be unreliable, a need for surrogates to see for themselves the futility of a situation before accepting physicians' prognostications, and the possibility that God will intercede to change patients' outcomes. Those surrogates who objected to the futility rationale based on a belief in miracles were more likely to insist on continued life support in the face of a very poor prognosis, whereas those who objected based on secular or experiential grounds were not.
Prior commentaries20,21 have proposed the following two main sources of conflict around medical futility: misunderstandings about prognosis; and religiously grounded objections. Our data revealed several new types of objections by surrogates to the futility rationale that merit further investigation, most importantly nonreligious doubts about the accuracy of physicians' predictions and the need for surrogates to see futility for themselves rather than rely solely on physicians' prognostications. These findings not only are important sociological observations, but also may be valuable in helping physicians to diagnose the true nature of the conflict about futility and respond skillfully. For example, by understanding that a religious objection is at the heart of a conflict, physicians may avoid using more strident attempts at scientific explanations to convince surrogates of the prognosis and instead enlist the help of a chaplain or a representative of the surrogate's religion to help mediate the conflict. Seeking the input of multiple senior clinicians may help to mitigate conflict with surrogates who have nonreligious concerns about the accuracy of prognostic estimates. A careful explanation of the prognostic significance (or lack thereof) of the physical appearance of the patient may help surrogates to see for themselves the gravity of the patient's illness.
An interesting preliminary finding from the study is that the precise nature of surrogates' doubt in physicians' futility predictions appears to have different implications for surrogates' willingness to forego life support. Those surrogates with religious objections to the futility rationale were more adamant about continuing life support, but those with secular or experiential concerns were no more likely to continue life support than those without concerns about physicians' prognostic accuracy. Although it is perhaps not surprising that surrogates who endorsed strong religious reasons for doubting futility predictions were more likely to request ongoing life support, we were surprised that those with secular doubts were not. These findings highlight the importance of understanding the true nature of the surrogates' skepticism about futility because the prospect for conflict resolution seems to partly hinge on this point. For cases of religiously based objection, high-quality communication from clinicians may be necessary but insufficient, and early involvement of pastoral care providers may be warranted.21 The ethical dilemma that arises, for which our empirical data provide no answer, is whether it is appropriate to override a surrogate's deeply held religious belief that conflicts with the physician's considered judgments about futility. A careful ethical analysis of this question cannot be undertaken here, but others21,22 have addressed it in detail.
We speculate that our findings provide a measure of validation for process-based approaches to futility that have been advocated.23,24 The individual components of the recommended processes address several of the issues the surrogates in this study highlighted as important. For example, the recommended early consultation of an ethics committee may allow for a more precise understanding of the nature of the conflict. The delay in decision making that is built into a deliberative due-process mechanism may allow surrogates to observe the patients' disease over time. The requirement for an independent prognostic assessment allows surrogates to triangulate multiple perspectives about the patient's prognosis.
This study has several limitations. First, our sample size was relatively small due to the in-depth, qualitative nature of the study. Second, we used specific hypothetical scenarios to prompt surrogates to discuss their attitudes about futility and to determine the threshold at which they believed it appropriate to withdraw life-sustaining treatment. It is possible that surrogates' responses to these hypothetical situations do not reflect the breadth of perspectives about futility. Further, the possibility of a “social desirability bias” exists in that surrogates may have provided what they believed to be socially expected answers rather than their true attitudes. Although we cannot fully exclude the possibility of social desirability bias, the diversity of perspectives that we found provides new insight. Third, although our cohort was diverse, we only enrolled English-speaking surrogates and, therefore, did not capture the views of individuals who do not speak English. Fourth, it is possible that surrogates' attitudes about futility predictions vary over a patient's illness trajectory. The cross-sectional design of our study did not permit us to assess changes over time. Nonetheless, we believe that these findings provide new insight into the perspectives surrogates hold at the time the patient is in the hospital ICU. Finally, our data presuppose no prior relationship between the physician and surrogate decision makers. It is possible that surrogates' attitudes about physicians' ability to predict futility could be different when they have established a trusting relationship with the physician over time. However, the current structure of critical care often requires that physicians discuss futility with surrogates whom they have only recently met.
Although the use of the medical futility rationale remains controversial in the care of patients with advanced illness,2,25 its use in clinical practice seems unlikely to disappear. Physicians should be aware that even with a clear understanding of their beliefs about the futility of a situation, many surrogates may object to the medical futility rationale. The grounds for these objections are diverse and include deeply held religious beliefs, nonreligious skepticism about physicians' ability to make a prognosis with certainty, and surrogates' need for a more experiential understanding of the patient's prognosis. Understanding these issues may open the way for a more nuanced approach to addressing futility in clinical practice.
Abbreviation:
- CI
confidence interval
Footnotes
This project was supported by a grant from the University of California, Berkeley-University of California, San Francisco Joint Medical Program (Mr. Zier), a grant from the University of California, San Francisco Dean's Office Medical Student Research Program (Mr. Zier), and a grant from the National Center for Research Resources [KL2 RR024130], a component of the National Institutes of Health and the National Institutes of Health Roadmap for Medical Research (Dr. White). Dr. White is also supported by a grant from the Greenwall Foundation Faculty Scholars Program.
The authors have reported to the ACCP that no significant conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians ( www.chestjournal.org/site/misc/reprints.xhtml ).
References
- 1.Burns JP, Truog RD. Futility: a concept in evolution. Chest. 2007;132:1987–1993. doi: 10.1378/chest.07-1441. [DOI] [PubMed] [Google Scholar]
- 2.Schneiderman LJ, Jecker NS, Jonsen AR. Medical futility: its meaning and ethical implications. Ann Intern Med. 1990;112:949–954. doi: 10.7326/0003-4819-112-12-949. [DOI] [PubMed] [Google Scholar]
- 3.Cantor M, Braddock C, Derse AR, et al. Do-not-resuscitate orders and medical futility. Arch Intern Med. 2003;163:2689–2694. doi: 10.1001/archinte.163.22.2689. [DOI] [PubMed] [Google Scholar]
- 4.Christakis N. Death foretold: prophecy and prognostication in medical care. Chicago, IL: University of Chicago Press; 1999. [Google Scholar]
- 5.Society of Critical Care Medicine. Consensus statement of the Society of Critical Care Medicine's ethics committee regarding futile and other possibly inadvisable treatments. Crit Care Med. 1997;25:887–891. doi: 10.1097/00003246-199705000-00028. [DOI] [PubMed] [Google Scholar]
- 6.Curtis JR, Patrick DL, Caldwell E, et al. The attitudes of patients with advanced AIDS towards use of the medical futility rationale in decisions to forego mechanical ventilation. Arch Intern Med. 2000;160:1597–1601. doi: 10.1001/archinte.160.11.1597. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs LM, Burns K, Jacobs BB. Trauma death: views of the public and trauma professionals on death and dying from injuries. Arch Surg. 2008;143:730–735. doi: 10.1001/archsurg.143.8.730. [DOI] [PubMed] [Google Scholar]
- 8.DeMaio TJ, Rothgeb JM. Cognitive interviewing techniques: in the lab and in the field. In: Schwarz N, Sudman S, editors. Answering questions: methodology for determining cognitive and communicative processes in survey research. San Francisco, CA: Jossey-Bass; 1996. pp. 177–196. [Google Scholar]
- 9.Edwards A, Elwyn G, Mulley A. Explaining risks: turning numerical data into meaningful pictures. BMJ. 2002;324:827–830. doi: 10.1136/bmj.324.7341.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paling J. Strategies to help patients understand risks. BMJ. 2003;327:745–748. doi: 10.1136/bmj.327.7417.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fagerlin A, Ditto PH, Danks JH, et al. Projection in surrogate decisions about life-sustaining medical treatments. Health Psychol. 2001;20:166–175. [PubMed] [Google Scholar]
- 12.Sox H, Blatt M, Higgins M, et al. Medical decision making. Boston, MA: Butterworth; 1988. [Google Scholar]
- 13.Lloyd CB, Nietert PJ, Silvestri GA. Intensive care decision making in the seriously ill and elderly. Crit Care Med. 2004;32:649–654. doi: 10.1097/01.ccm.0000115636.29294.2f. [DOI] [PubMed] [Google Scholar]
- 14.Strauss AL, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- 15.Glaser BG, Strauss AL. Discovery of grounded theory. Chicago, IL: Adline; 1967. [Google Scholar]
- 16.Charmaz KC. Constructing grounded theory: a practical guide through qualitative analysis. Thousand Oaks, CA: Sage; 2006. [Google Scholar]
- 17.Sackett DL, Haynes RB, Tugwell P, et al. Clinical epidemiology: a basic science for clinical medicine. 2nd ed. Boston, MA: Little, Brown; 1991. [Google Scholar]
- 18.Patton MQ. Enhancing the quality and credibility of qualitative analysis. Health Serv Res. 1999;34:1189–1208. [PMC free article] [PubMed] [Google Scholar]
- 19.Giacomini MK, Cook DJ. Users' guides to the medical literature: XXIII; Qualitative research in health care A—are the results of the study valid? Evidence-Based Medicine Working Group. JAMA. 2000;284:357–362. doi: 10.1001/jama.284.3.357. [DOI] [PubMed] [Google Scholar]
- 20.Brett AS. Futility revisited: reflections on the perspectives of families, physicians, and institutions. HEC Forum. 2005;17:276–293. doi: 10.1007/s10730-005-5154-y. [DOI] [PubMed] [Google Scholar]
- 21.Brett AS, Jersild P. “Inappropriate” treatment near the end of life: conflict between religious convictions and clinical judgment. Arch Intern Med. 2003;163:1645–1649. doi: 10.1001/archinte.163.14.1645. [DOI] [PubMed] [Google Scholar]
- 22.Truog RD. Tackling medical futility in Texas. N Engl J Med. 2007;357:1–3. doi: 10.1056/NEJMp078109. [DOI] [PubMed] [Google Scholar]
- 23.Council on Ethical and Judicial Affairs, American Medical Association. Medical futility in end-of-life care: report of the Council on Ethical and Judicial Affairs. JAMA. 1999;281:937–941. [PubMed] [Google Scholar]
- 24.Fine RL, Mayo TW. Resolution of futility by due process: early experience with the Texas Advance Directives Act. Ann Intern Med. 2003;138:743–746. doi: 10.7326/0003-4819-138-9-200305060-00011. [DOI] [PubMed] [Google Scholar]
- 25.Waisel DB, Truog RD. The cardiopulmonary resuscitation-not-indicated order: futility revisited. Ann Intern Med. 1995;122:304–308. doi: 10.7326/0003-4819-122-4-199502150-00011. [DOI] [PubMed] [Google Scholar]