Abstract
Background/aims
The issue of spontaneous relapse of hepatitis in anti-HBe positive asymptomatic HBsAg carriers was rarely reported before and deserves further exploration.
Methods
A total of 1241 anti-HBe positive asymptomatic adult HBsAg carriers were prospectively followed up. Of these, 661 (53%) were males, and the mean (±SD) age was 35.6 ± 9.1 years. Relapse of hepatitis was defined as elevation of ALT more than twice the upper limit of normal accompanied by detectable serum HBV DNA by hybridization assays.
Results
During a mean follow up of 12.3 years, hepatitis relapsed in 211 patients with an annual rate of 1.46%. The cumulative probabilities of hepatitis relapse were 10.2%, 17.4%, 19.3%, 20.2%, and 20.2%, respectively, after 5, 10, 15, 20, and 25 years of follow up. Multivariate analyses showed that the probability of hepatitis relapse correlated significantly with male sex (P < 0.0001) and age at entry (P = 0.007). The cumulative probability of hepatitis relapse after 20 years was 26.9% for males and only 12.5% for females, and was 13.1% for those of age <30 years at entry but increased to 29.4% for those of age 40–49 years at entry.
Conclusion
Hepatitis relapsed in about 20% of asymptomatic HBsAg carries during 25 years of follow up. Relapse of hepatitis occurred more frequently during earlier years of follow up. Males were more likely to have relapse of hepatitis than females. In addition, relapse of hepatitis was significantly less frequent in patients who were younger than 30 years at study entry, possibly implicating more favorable outcome of earlier HBeAg seroconversion.
Keywords: Age, Anti-HBe, HBeAg seroconversion, Gender
Introduction
The epidemiological and clinical features of hepatitis B virus (HBV) infection vary between high and low HBV endemic areas [1]. In high endemic areas such as Southeast Asia and Taiwan, HBV infection occurs predominantly in the perinatal period or early childhood with high-rate of persistent infection [1]. The natural history of chronic HBV infection consists of three chronological phases: an initial immune tolerant phase (hepatitis B e antigen [HBeAg] positive and normal alanine aminotransferase [ALT] levels), followed by immune clearance phase (HBeAg positive and abnormal ALT levels), and finally the low replication phase (hepatitis B e antibody [anti-HBe] positive and normal ALT levels) [2, 3]. Patients in the third phase usually have HBV DNA undetectable by hybridization assays and are termed “inactive HBsAg carriers”. The ultimate outcome of chronic HBV infection appears to depend on the duration of the immune clearance phase as well as on the severity of liver damage during this phase [4, 5]. In addition, hepatitis may relapse after HBeAg seroconversion that also significantly contributes to the development of cirrhosis [6–8]. There were two published studies from Taiwan that prospectively followed up the natural course after spontaneous HBeAg seroconversion [6, 7]. The annual rates of relapse of hepatitis (ALT > twice the upper normal limit and detectable serum HBV DNA by hybridization assays) were 3.3% in the study involving patients with chronic hepatitis B [6] and 2.2% in the study involving asymptomatic patients [7].
HBV infection is highly endemic in Taiwan, where the HBsAg carrier rates in the general population are high up to 15–20% before the era of universal nation-wide neonatal HBV vaccination [9–11]. Most HBsAg carriers are incidentally identified during blood donation or health check up. Among them, the great majority is negative for HBeAg and has normal ALT. For example, in one large series of 10,431 asymptomatic adult HBsAg carriers from Taiwan, 19.6% were HBeAg positive and 80.4% were HBeAg negative. Of the latter, only 16.2% had abnormal ALT. It is thus estimated that 67% of incidentally recognized asymptomatic HBsAg carriers in Taiwan are HBeAg negative with normal ALT [12]. The natural course of chronic HBV infection in these inactive HBsAg carriers, however, is rarely reported.
Recently, we have noted that there was an appreciably high-rate of spontaneous HBsAg seroclearance in anti-HBe positive asymptomatic adult HBsAg carriers during a long-term follow up and that HBsAg carriers with sustained remission of hepatitis were 2.2 times more likely to have spontaneous HBsAg seroclearance than those with relapse of hepatitis [13]. In that study, the annual rate of spontaneous relapse of hepatitis was 1.6%, which correlated positively with male sex and age at entry [13]. However, the issue of spontaneous relapse of hepatitis was not particularly addressed. In this study, we tried to further analyze in more detail and discuss the rates, determinants and clinical implication of spontaneous relapse of hepatitis in 1241 anti-HBe positive asymptomatic adult HBsAg carriers from Taiwan.
Materials and methods
Patients
From 1980, asymptomatic adults who were incidentally identified as HBsAg carriers during blood donation or health check up were recruited into the present study if they fulfilled the following criteria: (1) HBsAg positive for at least one year; (2) HBeAg negative, anti-HBe positive, normal ALT (0–36 U/l), no evidence of cirrhosis based on the clinical ground and liver ultrasonography [14] and no concomitant infection with hepatitis C virus or hepatitis D virus at baseline; (3) no anti-viral or immunomodulatory therapy before entry and during follow up; (4) regular follow up at least every year and for a minimum of 3 years; (5) available for follow up through 2005. Patients who had alcohol or drugs that might be possible etiological agents of hepatitis were excluded. No patient in this cohort admitted intravenous drug abuse or homosexuality.
Clinical data at baseline and during follow up
At entry, the patients were tested for liver biochemical tests, virological markers (HBsAg, HBeAg, anti-HBe, antibody against hepatitis C virus [anti-HCV], and antibody against hepatitis D virus [anti-HDV]), α-fetoprotein, and liver ultrasonography. Liver biochemical tests were assayed every 6 months if ALT levels were normal, and every 1–3 months or more often if ALT levels were elevated. HBsAg, HBeAg, anti-HBe, and α-fetoprotein were assayed every 6 months or more often if clinically indicated. Liver ultrasonography was assayed every 6–12 months or more often if clinically indicated. Assays for anti-HCV and anti-HDV were repeated if ALT levels elevated to more than twice the normal upper limit. Serum HBV DNA was not routinely assayed but was measured when ALT levels elevated to more than twice the normal upper limit.
Methods
HBsAg, HBeAg, anti-HBe, and anti-HDV were assayed by radioimmunoassay (Abbott Diagnostics, North Chicago, Ill.). Anti-HCV was tested by a second- or third-generation enzyme immunoassay (Abbott Diagnostics). Hepatitis B virus DNA was tested by sandwich molecular hybridization assays using a Digene Hybrid Capture System (Digene Diagnostics, Inc., Beltsville, Md.). The detection sensitivity was 0.5 pg/ml.
Relapse of hepatitis was diagnosed when ALT levels elevated to more than twice the normal upper limit, accompanied by positive serum HBV DNA by hybridization assays [6–8]. Patients that remained positive for anti-HBe with normal ALT through the course of follow up were defined as sustained remission.
Statistical analysis
To compare characteristics between groups, either chi-squared test or Fisher exact test was used for analysis of categorical variables and Student t test or Wilcoxon nonparametric test was used for analysis of continuous variables. Estimates on the rate of hepatitis relapse were calculated by the actuarial analysis method, and the difference was determined by the long-rank test. Univariate and multivariate analyses were performed to identify factors associated with relapse of hepatitis. Variables found to be significant in the univariate models were tested in a multivariate setting using the Cox proportional hazards regression models. Statistical procedures were performed with SPSS statistical software (version 13.0; SPSS, Chicago, IL). P values <0.05 were considered significant.
Results
A consecutive series of 1241 anti-HBe positive asymptomatic adult HBsAg carriers were enrolled in this study. Their baseline and follow-up data were summarized in Table 1. The mean (±SD) age at entry was 35.6 ± 9.1 years (median, 34.5; range, 16–76 years), and 661 (53%) were men.
Table 1.
Baseline and follow-up characteristics of study patients
| Characteristics | N = 1241 |
|---|---|
| Mean ± SD or number (%) (range) | |
| Age at entry (years) | 35.6 ± 9.1 (16–76) |
| Men:women | 661:580 |
| Follow up duration (years) | 12.3 ± 5.5 (3–26) |
| Male | 12.6 ± 5.7 (3–26) |
| Female | 12.0 ± 5.3 (3–25) |
| Relapse of hepatitis | 211(17.0) |
| Male | 154(23.3) |
| Female | 57(9.8) |
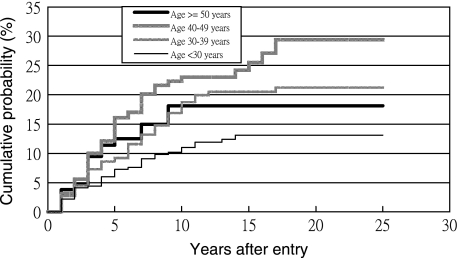
During 14,484 person-years of follow up, relapse of hepatitis occurred in 211 patients (154 males and 57 females). The calculated rate of hepatitis relapse was 1.46% per year. The cumulative probabilities of hepatitis relapse were 10.2%, 17.4%, 19.3%, 20.2%, and 20.2%, respectively, after 5, 10, 15, 20, and 25 years. Multivariate analyses using the Cox proportional hazards regression models showed that the probability of hepatitis relapse correlated positively with male sex (hazard ratio [95%CI] = 2.41 [1.78–3.27], P < 0.0001) and age at entry (hazard ratio [95%CI] = 1.22 [1.06–1.41] per decade increase, P = 0.007). The person-years of follow up and the events of hepatitis relapse in each age group are illustrated in Table 2. The annual rates of hepatitis relapse increased significantly with increasing age at entry. The cumulative probability of hepatitis relapse according to gender is shown in Fig. 1, and according to age at entry is shown in Fig. 2. Relapse of hepatitis was significantly more frequent in males than in females. In addition, relapse of hepatitis was least likely in carriers of age younger than 30 years and most likely in those of age 40–50 years at study entry.
Table 2.
Calculated rates of relapse of hepatitis and cirrhosis in 1241 anti-HBe positive asymptomatic adult HBsAg carriers according to age at entry
| Age at entry | N | Person-years of follow-up | No. (%/years) of patients with relapse of hepatitis | No (%/year) of patients with cirrhosis |
|---|---|---|---|---|
| <30 years | 320 | 4,176 | 37(0.89%)* | 1(0.03%)# |
| 30–39 years | 563 | 6,565 | 101(1.53%)* | 17(0.25%)# |
| 40–49 years | 251 | 2,620 | 56(2.14%)* | 14(0.53%)# |
| ≥50 years | 107 | 1,123 | 17(1.51%)* | 8(0.71%)# |
| Total | 1241 | 14,484 | 211(1.46%) | 40(0.28%) |
*, # P < 0.0001 by chi-square test for trend
Fig. 1.
Actuarial analysis of the cumulative probability of spontaneous relapse of hepatitis in 1241 anti-HBe-positive asymptomatic adult HBsAg carriers according to gender (P < 0.0001)
Fig. 2.
Actuarial analysis of the cumulative probability of spontaneous relapse of hepatitis in 1241 anti-HBe-positive asymptomatic adult HBsAg carriers according to age at entry (P = 0.0007)
Forty patients were found to progress to cirrhosis based on the clinical ground and liver ultrasonography [14] until the last visit. Of these, four subsequently developed hepatocellular carcinoma. The annual rate of progression to cirrhosis was 1.14% (33 during 2,887 person-years of follow up) for patients with relapse of hepatitis and 0.06% (7 during 11,597 person-years of follow up) for those without (P < 0.0001). The rates of progression to cirrhosis also increased progressively with increasing age at entry, as shown in Table 2.
Discussion
The present study showed that annual rate of spontaneous relapse of hepatitis in anti-HBe-positive asymptomatic adult HBsAg carriers was approximately 1.5%. This figure was substantially lower compared to the rates of 2.2% and 3.3%, respectively, in two previous studies reported from our unit [6, 7]. It should be pointed out that the previous two studies followed up the patients starting from the time of HBeAg seroconversion, while the onset of HBeAg seroconversion in this cohort of patients was unknown. In one of these studies, the cumulative probability of HBeAg negative hepatitis after spontaneous HBeAg serocoinversion was 14%, 18%, 22%, respectively, at 3, 5, and 10 years of follow up [6]. These data indicate that more than half of relapse of hepatitis occurred during the first 3 years after HBeAg seroconversion. The mean age at entry of the patients in this cohort was 35.6 years, while previous studies revealed that the mean age of HBeAg seroconversion for HBeAg-positive HBsAg carriers from endemic areas was 31–33 years [7, 15–17]. These data probably suggest that HBsAg carriers in this cohort were enrolled into this study 2–4 years after HBeAg seroconversion, which may explain the relatively lower rates of relapse of hepatitis in the present series than in the previous series. Moreover, the present results showed that the risk of spontaneous relapse of hepatitis tended to decease with the time of follow up. The cumulative probability of spontaneous relapse of hepatitis was 10.2% after 5 years of follow up. However, the rates tended to progressively become low 5 years thereafter compared to the first 5 years: the cumulative probability of relapse of hepatitis increased to 17.4% after 10 years (7.2% increase from 6th to 10th year of follow up), 19.3% after 15 years (1.9% increase from 11th to 15th year of follow up), and 20.2% after 20 years (0.9% increase from 16th to 20th year of follow up). Notably, the risk of relapse of hepatitis became negligible, if any, after 20 years of follow up (Fig. 1).
Two factors independently associated with spontaneous relapse of hepatitis in anti-HBe positive asymptomatic adult HBsAg carriers were identified in this study. In keeping with the previous observations that relapse of hepatitis after HBeAg seroconversion was significantly more frequent in male carriers than in female carriers [7], the present study showed that male carriers were 2.4 times more likely to have spontaneous relapse of hepatitis than female carriers. As shown in Fig. 1, the cumulative probability of spontaneous hepatitis relapse after 20 years of follow up was 26.4% for male carriers but was only 12.5% for female carriers (P < 0.0001). Because HBsAg carriers with relapse of hepatitis were about 20 times more likely to progress to cirrhosis compared to those with sustained remission of hepatitis, as previously observed [7] and in this cohort of carriers, the high risk of relapse of hepatitis in male gender may account for the male predominance among patients with HBV related cirrhosis [18], despite of little male sex dominance in asymptomatic HBsAg carriers in high endemic areas, as shown in this cohort.
One interesting finding of the present study is that spontaneous relapse of hepatitis correlated significantly with the age at entry. As shown in Table 2 and Fig. 2, spontaneous relapse of hepatitis occurred much less frequently in patients who were younger than 30 years at study entry. The cumulative probability of spontaneous relapse of hepatitis after 20 years of follow up was only 13.1% for carriers of age less than 30 years at entry. The cumulative probability increased much with increasing age at entry, peaked to 29.4% in those of age 40–49 years and then declined in those of age over 50 years at entry. While the onset of HBeAg seroconversion for patients of age over 30 years at entry was unknown, HBsAg carriers of age less than 30 years at entry in this cohort can be considered as those with early HBeAg seroconversion. The present results possibly implicate that HBeAg seroconversion before age 30 years may be associated with a decreased risk of spontaneous relapse of hepatitis, compared to that after age 30 years. Further studies are indicated to clarify this issue.
With regard to viral factors possibly associated with spontaneous relapse of hepatitis, the results of previous studies from Taiwan and Hong Kong have suggested that relapse of hepatitis was significantly more frequent in genotype C infection than in genotype B infection [8, 17]. Unfortunately, data on HBV genotype and HBV DNA levels at entry were not available in this study, because the majority of patients in this cohort entered into follow up long before the significance of HBV genotype and viral load [19, 20] have been explored and no adequate serum samples were available for study retrospectively. Further studies are indicated to clarify the impact of HBV genotype as well as other viral factors such as precore stop mutant and basal core promoter mutant in spontaneous relapse of hepatitis in anti-HBe positive asymptomatic carries.
In conclusion, the annual rate of spontaneous relapse of hepatitis in anti-HBe positive asymptomatic adult HBsAg carriers is estimated to be 1.5%. Approximately 20% of these carries have spontaneous relapse of hepatitis during 25 years of follow up. Relapse of hepatitis occurs relatively more frequently during the first 5- to 10- year follow up. Male carriers are 2.4 times more likely to have relapse of hepatitis than females. In addition, relapse of hepatitis is significantly less likely to occur in patients who are younger than 30 years at study entry. The latter finding may implicate more favorable outcome of earlier HBeAg seroconversion in chronic HBV infection.
Abbreviations
- HBV
Hepatitis B virus
- HBeAg
Hepatitis B e antigen
- ALT
Alanine aminotransferase
- Anti-HBe
Antibody against hepatitis B e antigen
- HBsAg
Hepatitis B surface antigen
- Anti-HCV
Antibodies against hepatitis C virus
- Anti-HDV
Antibody against hepatitis D virus
Footnotes
See related editorial: 10.1007/s12072-007-9004-7
References
- 1.Chu CM, Liaw YF. Natural history differences in perinatally versus adult-acquired disease. Curr Hepatitis Rep 2004;3:123–31. [DOI]
- 2.Chu CM, Karayiannis P, Fowler MJ, Monjardino J, Liaw YF, Thomas HC. Natural history of chronic hepatitis B virus infection in Taiwan: studies of hepatitis B virus DNA in serum. Hepatology 1985;5:431–4. [DOI] [PubMed]
- 3.Chu CM. Natural history of chronic hepatitis B virus infection in adults with emphasis on the occurrence of cirrhosis and hepatocellular carcinoma. J Gastroenterol Hepatol 2000;15 Suppl:E25–30. [DOI] [PubMed]
- 4.Liaw YF, Tai DI, Chu CM, Chen TJ. The development of cirrhosis in patients with chronic type B hepatitis: a prospective study. Hepatology 1988;8:493–6. [DOI] [PubMed]
- 5.Fattovich G, Brollo L, Giustina G, Noventa F, Pontisso P, Alberti A, Realdi G, Ruol A. Natural history and prognostic factors for chronic hepatitis type B. Gut 1991;32:294–8. [DOI] [PMC free article] [PubMed]
- 6.Hsu YS, Chien RN, Yeh CT, Sheen IS, Chiou HY, Chu CM, Liaw YF. Long-term outcome after spontaneous HBeAg seroconversion in patients with chronic hepatitis B. Hepatology 2002;35:1522–7. [DOI] [PubMed]
- 7.Chu CM, Hung SJ, Lin J, Tai DI, Liaw YF. Natural history of hepatitis B e antigen to antibody seroconversion in patients with normal serum aminotransferase levels. Am J Med 2004;116:829–34. [DOI] [PubMed]
- 8.Chu CM, Liaw YF. Genotype C hepatitis B virus infection is associated with a higher risk of reactivation of hepatitis B, progression to cirrhosis than genotype B: a longitudinal study of hepatitis B e antigen-positive patients with normal aminotransferase levels at baseline. J Hepatol 2005;43:411–7. [DOI] [PubMed]
- 9.Chen DS, Sung JL, Lai MY. A seroepidemiologic study of hepatitis B virus infection in Taiwan. Taiwan Yi Xue Hui Za Zhi 1978;77:908–18. [PubMed]
- 10.Wu JS, Chen CH, Chiang YH, Lee YC, Lee MH, Ko YC, Hu HT. Hepatitis B virus infection in Taiwan with reference to anti-HBc versus HBsAg and anti-HBs. Taiwan Yi Xue Hui Za Zhi 1980;79:760–7. [PubMed]
- 11.Sung JL, Chen DS, Lai MY, Yu JY, Wang TH, Wang CY, Lee CY, Chen SY, Ko TM. Epidemiology study on hepatitis B virus infection in Taiwan. Chin J Gastroenterol 1984;1:1–9.
- 12.Chu CM, Sheen IS, Lin SM, Liaw YF. Sex difference in chronic hepatitis B viStudies of serum HBeAg and alanine aminotransferase levels in 10431 asymptomatic Chinese HBsAg carriers. Clin Infect Dis 1993;16:709–13. [DOI] [PubMed]
- 13.Chu CM, Liaw YF. HBsAg seroclearance in asymptomatic carriers of high endemic areas: appreciably high rates during a long-term follow up. Hepatology 2007;45:1187–1192. [DOI] [PubMed]
- 14.Lin DY, Sheen IS, Chiu CT, Lin SM, Kuo YC, Liaw YF. Ultrasonographic changes of early liver cirrhosis in chronic hepatitis B: a longitudinal study. J Clin Ultrasound 1993;21:303–8. [DOI] [PubMed]
- 15.Kao JH, Chen PJ, Lai MY, Chen DS. Hepatitis B virus genotypes and spontaneous hepatitis B e antigen seroconversion in Taiwanese hepatitis B carriers. J Med Virol 2004;72:363–9. [DOI] [PubMed]
- 16.Yuen MF, Yuan HJ, Wong DK, Yuen JC, Wong WM, Chan AO, Wong BC, Lai KC, Lai CL. Prognostic determinants for chronic hepatitis B in Asians: therapeutic implications. Gut 2005;54:1610–4. [DOI] [PMC free article] [PubMed]
- 17.Chu CJ, Hussain M, Lok AS. Hepatitis B virus genotype B is associated with earlier HBeAg seroconversion compared with hepatitis B virus genotype C. Gastroenterology 2002;122:1756–62. [DOI] [PubMed]
- 18.Chu CM, Liaw YF, Sheen IS, Lin DY, Huang MJ. Sex difference in chronic hepatitis B virus infection: an appraisal based on the status of hepatitis B e antigen and antibody. Hepatology 1983;3:947–50. [DOI] [PubMed]
- 19.Iloeje UH, Yang HI, Su J, Jen CL, You SL, Chen CJ. Risk evaluation of viral load elevation and associated liver disease/cancer-In HBV (the REVEAL-HBV) study group. Predicting cirrhosis risk based on the level of circulating hepatitis B viral load. Gastroenterology 2006;130:678–86. [DOI] [PubMed]
- 20.Chen CJ, Yang HI, Su J, Jen CL, You SL, Lu SN, Huang GT, Iloeje UH. REVEAL-HBV Study Group. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA 2006;295:65–73. [DOI] [PubMed]