Abstract
Nonalcoholic fatty liver disease (NAFLD) is one of the most common chronic liver diseases and may progress to advanced hepatic fibrosis and cirrhosis in some patients. Cirrhosis due to NAFLD is considered extremely rare in children in the Asia–Pacific region. We report the characteristics of 5 children with advanced hepatic fibrosis and cirrhosis due to NAFLD. Four of them were obese, and all of them had high alanine transaminase levels and ultrasonographic evidence of fatty liver. None had diabetes mellitus or hyperlipidemia. The calculated HOMA-IR was more than two in all five cases. Liver biopsy showed stage III fibrosis in 2 patients and stage IV fibrosis (cirrhosis) in 3.
Keywords: Nonalcoholic steatohepatits, Nonalcoholic fatty liver disease, Childhood cirrhosis
Background
Nonalcoholic fatty liver disease (NAFLD) is a condition that results from pathological accumulation of triglycerides in the liver that could lead to progressive necroinflammatory disease. The histology ranges from simple steatosis through steatohepatitis to advanced fibrosis and cirrhosis. NAFLD is increasingly recognized in the absence of overt metabolic diseases [1] and is considered to be the most common liver disease in children [2]. NAFLD in children was first reported in the early 1983 [3]. Following this seminal report, a number of case series have been published describing children with nonalcoholic steatohepatitis (NASH) having the following clinical characteristics: occurrence in children and adolescents, male predominance, serum alanine transaminase (ALT) raised more than serum aspartate transaminase (AST), hypertriglyceridemia as the typical lipid abnormality and nonspecific symptoms, and a vague abdominal pain often being the reason for clinical assessment [4–8].
Obesity and type-2 diabetes in childhood are becoming alarmingly common both in developed and developing countries. With the changing socioeconomic situation, urbanization, increasing physical inactivity, and a diet rich in fat and high glycemic index, Asia is at the epicenter of this epidemic. The incidence of NAFLD in this region is increasing in both adults and children [9]. A study of 810 school children from northern Japan showed an overall prevalence of 2.6% for fatty liver diagnosed on ultrasound scan [10]. There was a strong correlation between fatty liver and body mass index. Obesity is increasingly becoming a problem in Sri Lanka. In a recent school-based study, 3.9% and 14.7% of the study subjects were obese and overweight, respectively [11].
In Western series, although fibrosis is common in pediatric NASH, cirrhosis has been described in only few cases of childhood NAFLD [6, 12, 13]. Advanced fibrosis or cirrhosis associated with NAFLD in childhood is very rare in the Asia–Pacific region [7, 14].
We report 5 children, 3 with established cirrhosis, and another 2 with advanced hepatic fibrosis, due to NAFLD. The 5 patients presented over a 4-year period from 2002.
Methods
The five children with advanced hepatic fibrosis due to NAFLD reported here were among those children who presented with non-specific abdominal pain and/or asymptomatically elevated liver enzymes, and were diagnosed as having NAFLD or NASH ultrasonographically or by liver biopsy. The routine diagnostic work-up in such children includes hepatitis screening, autoimmune screening, iron and copper studies, and ultrasonographic assessment of the liver. If NAFLD was diagnosed, fasting serum insulin and C peptide levels were measured in addition to fasting sugar levels and lipid profile. When percutaneous liver biopsy was performed, Brunt’s grading is used to stage the degree of fibrosis.
Results
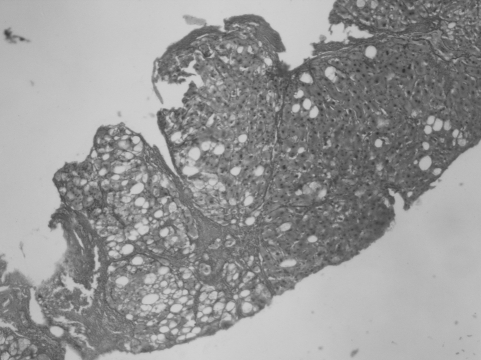
Five of the children who underwent liver biopsy in our unit had advanced fibrosis or cirrhosis due to NAFLD. There were 4 boys and a girl (median age 11 years [range 10–12 years]). Four of them were obese with body mass index more than 95th centile. All 5 had marked acanthosis nigricans, high ALT levels (more than twice the upper limit of normal), and ultrasonographic evidence of fat infiltration in the liver (at least two features of five, liver hyperechogenecity [compared to renal echogenecity], blurring of blood vessels, and deep attenuation of the signal). None of them had any other possible cause for the liver disease. None of the five had diabetes mellitus or hyperlipidemia. The calculated HOMA-IR was more than 2 in all 5 cases (Table 1). Liver biopsy showed stage III fibrosis in 2 patients and stage IV fibrosis (cirrhosis) in 3. In all 5 patients, the intra-acinar inflammation was mild (graded as <2 foci/10 objective), and portal inflammation was also mild. Ballooning degeneration and Mallory body formation were present in all biopsies. Patients with stage IV fibrosis were considered as having cirrhosis (Table 2, Fig. 1).
Table 1.
Demographic and biochemical characteristics of the 5 patients with NAFLD
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | |
|---|---|---|---|---|---|
| Age at presentation (years) | 11 | 10 | 12 | 11 | 11.5 |
| Sex | Male | Male | Male | Male | Female |
| Body mass index (kg/m2) | 26 | 31 | 28 | 26 | 21.1 |
| Body mass index centile | >95th | >95th | >95th | >95th | 85th–90th |
| Length of follow up (years) | 4 | 1.3 | 5 | 0.5 | 0.5 |
| ALT (u/l) | 171 | 183 | 218 | 100 | 86 |
| AST (u/l) | 90 | 68 | 73 | 40 | 42 |
| Albumin (g/dl) | 3.6 | 4.1 | 4.4 | 4.0 | 4.6 |
| INR | 1 | 1.2 | 1 | 1.17 | 1 |
| Hepatitis screeninga | Negative | Negative | Negative | Negative | Negative |
| Autoimmune screeningb | Negative | Negative | Negative | Negative | Negative |
| Ceruloplasmin (μmol/l) | 1.8 | 2 | 2.6 | 2.2 | 2.3 |
| Urinary Cu (μmol/24 h) | 0.3 | 0.5 | 0.28 | 0.43 | 0.38 |
| Fasting glucose (mmol/l) | 3.61 | 3.45 | 3.8 | 4.83 | 4.77 |
| Fasting insulin (μU/ml) | 12.7 | 13.1 | 12.9 | 10.01 | 11.3 |
| HOMA-IR | 2.04 | 2.01 | 2.17 | 2.17 | 2.4 |
| C peptide levels (ng/ml) | 2.0 | 2.6 | 2.8 | 2.0 | 2.7 |
| Fasting triglycerides (mg/dl) | 132 | 146 | 130 | 121 | 106 |
| Fasting cholesterol (mg/dl) | 194 | 187 | 103 | 200 | 166 |
aHepatitis screen include: Hepatitis B surface antigen, Hepatitis B core antibody and Hepatitis C antibody
bAutoimmune screening include: Anti-nuclear antibody, Anti-smooth muscle antibody and anti-KLM antibody
Table 2.
Findings of the liver biopsies of the 5 children with NAFLD
| Feature | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 |
|---|---|---|---|---|---|
| Steatosis | >66% | 40–60% | 60% | 80% | 30–40% |
| Balloon degenerationa | + | + | + | ++ | + |
| Mallory body formationa | ++ | + | + | + | + |
| Intra acinar inflammationb | + | + | + | + | + |
| Portal inflammationc | + | + | + | + | + |
| Fibrosis | Stage 4 | Stage 4 | Stage 4 | Stage 3 | Stage 3 |
| Brunt grading | Grade 3 | Grade 3 | Grade 3 | Grade 3 | Grade 1 |
| Staging | 4 | 4 | 4 | 3 | 3 |
| Cirrhosis | + | + | + | No | No |
a+ = occasional, ++ = moderate
b+ = < 2 foci per 10 objective
c+ = mild
Fig. 1.
Liver microscopy of patient 2 showing steatosis and cirrhosis (×40, reticulin with counterstaining)
Discussion
We report 5 children with advanced hepatic fibrosis or cirrhosis due to NAFLD. Three patients with cirrhosis were obese and so was the child with advanced fibrosis. The other was overweight. All 5 of them had marked acanthosis nigricans. They also had raised ALT and an ALT:AST ratio greater than 1, and a calculated HOMA-IR of more than 2, indicating insulin resistance. All 3 children with cirrhosis were males. None of them had portal hypertension. The 5 children are currently on extensive life-style modification, with dietary restriction and increased physical activity aimed at weight reduction, and are being followed up with regular monitoring.
Clinical experience with NASH in pediatric practice is limited. Although it is well recognized in the West, the epidemiology of pediatric NAFLD in Asia is not well documented. Significant fibrosis in pediatric NAFLD has been documented in previous Western case series. Baldridge and co-workers studied 14 children with NAFLD and all of them had varying degrees of inflammation and fibrosis [4]. In 2003, Schwimmer et al. [12] studied 43 children with NAFLD. Among them, only 1 child had established cirrhosis. Recently Mollesten et al. [6] described 2 children with cirrhosis and one of them had symptomatic portal hypertension. Only 2 cases of cirrhosis following NAFLD had been reported from the Asia-Pacific region. In 1984, Kinugasa et al. [7] studied 11 obese children and only one child had established cirrhosis. Similarly, Menton and co-workers reported 17 children with NASH and only one child had histological evidence of cirrhosis [14].
Conclusion
In conclusion, this report of advanced hepatic fibrosis in children underlines the fact that NAFLD in childhood may not be entirely benign. Further longitudinal studies are required to establish its natural history.
References
- 1.Marion AW, Baker AJ, Dhawan A. Fatty liver disease in children. Arch Dis Child. 2004;89:648–52. [DOI] [PMC free article] [PubMed]
- 2.Patton HM, Sirlin C, Behling C, Middleton M, Schwimmer JB, Lavine JE. Pediatric non alcoholic fatty liver disease: a critical appraisal of current data and implication for future research. J Pediatr Gastroenterol Nutr. 2006;43:413–27. [DOI] [PubMed]
- 3.Moran JR, Gishan FK, Halter SA, Greene HL. Steatohepatitis in obese children: a cause of chronic liver dysfunction. Am J Gastroenterol. 1983;78:374–7. [PubMed]
- 4.Baldrigde AD, Perez-Atayde AT, Graeme-Cook F, Higgins L, Lavin JE. Idiopathic steatohepatitis in childhood: a multicentre retrospective study. J Pediatr. 1995;127:700–4. [DOI] [PubMed]
- 5.Rashid M, Roberts EA. Non alcoholic steatohepatitis in children. J Pediatr Gastroenterol Nutr. 2000;30:48–53. [DOI] [PubMed]
- 6.Molleston JP, White F, Teckmann J, Fitzgerald JF. Obese children with steatohepatitis can develop cirrhosis in childhood. Am J Gastrenterol. 2002;97:2460–2. [DOI] [PubMed]
- 7.Kinugasa A, Sunamoto K, Furukawan N, Sawada T, Kusunoki T, Shimada N. Fatty liver and its fibrous changes found in simple obesity of children. J Pediatr Gastroenterol Nutr. 1984;3:408–14. [DOI] [PubMed]
- 8.Younossi ZM, Gramlich T, Liu YC, Matteoni C, Petrelli M, Goldblum J, et al. Nonalcoholic fatty liver disease: assessment of variability in pathologic interpretation. Mod Pathol. 1998;11:560–5. [PubMed]
- 9.Farrell GC. Non-alcoholic steatohepatitis: what is it, and why is it important in the Asia-Pacific region? J Gastroenterol Hepatol. 2003;18:124–38. [DOI] [PubMed]
- 10.Tominaga K, Kurata JH, Chen YK, Fujimoto E, Miyagawa S, Ichiro ABE, et al. Prevalence of fatty liver disease in Japanese children and relationship with obesity. An epidemiological ultrasonographic survey. Dig Dis Sci. 1995;40:2002–9. [DOI] [PubMed]
- 11.Wickramasinghe VP, Lamabadusuriya SP, Atapattu N, Satyadas G, Kuruparananthan S, Karunarathne P. Dietary and physical activity patterns of school children in an urban area of Sri Lanka. Sri Lanka J Child Health. 2005;34:44–9.
- 12.Schwimmer JB, Deutsch R, Rauch JB, Behling C, Newbury R, Levine JE. Obesity, insulin resistance, and other clinicopathological correlates of pediatric nonalcoholic fatty liver disease. J Pediatr. 2003;143:500–5. [DOI] [PubMed]
- 13.Schwimmer JB, Behling C, Newbury R, Deutsch R, Nievergelt C, Schork NJ, et al. Histology of pediatric nonalcoholic fatty liver disease. Hepatology. 2005;42:641–9. [DOI] [PubMed]
- 14.Menton ND, Lipsett J, Davidson GP, Bourne AJ, Couper RT. Non-alcoholic steatohepatitis in children and adolescents. Med J Aust. 2000;173:476–9. [DOI] [PubMed]