Abstract
Ectopic varices (EcV) comprise large portosystemic venous collaterals located anywhere other than the gastro-oesophageal region. No large series or randomized-controlled trials address this subject, and therefore its management is based on available expertise and facilities, and may require a multidisciplinary team approach. EcV are common findings during endoscopy in portal hypertensive patients and their bleeding accounts for only 1–5% of all variceal bleeding. EcV develop secondary to portal hypertension (PHT), surgical procedures, anomalies in venous outflow, or abdominal vascular thrombosis and may be familial in origin. Bleeding EcV may present with anaemia, shock, haematemesis, melaena or haematochezia and should be considered in patients with PHT and gastrointestinal bleeding or anaemia of obscure origin. EcV may be discovered during panendoscopy, enteroscopy, endoscopic ultrasound, wireless capsule endoscopy, diagnostic angiography, multislice helical computed tomography, magnetic resonance angiography, colour Doppler-flow imaging, laparotomy, laparoscopy and occasionally during autopsy. Patients with suspected EcV bleeding need immediate assessment, resuscitation, haemodynamic stabilization and referral to specialist centres. Management of EcV involves medical, endoscopic, interventional radiological and surgical modalities depending on patients’ condition, site of varices, available expertise and patients’ subsequent management plan.
Keywords: Ano-rectal varices, Biliary varices, Colonic varices, Duodenal varices, Intra-abdominal varices, Isolated gastric varices type 2, Stomal varices
Introduction
The term “ectopic varices” (EcV) describes dilated portosystemic collateral veins located in unusual sites other than the gastro-oesophageal (G-O) region including the ectopic isolated gastric varices type 2 (IGV2). This definition has previously been given to any gastrointestinal mucosa-associated abnormally dilated tortuous veins that may lead to gastrointestinal bleeding. In addition, the term has also been given to any portosystemic collateral veins located in the abdominal wall or in the retroperitoneal space.
As no randomized-controlled trials (RCTs) have previously addressed the therapeutic modalities of EcV, most of the available knowledge about this entity is obtained from small case series, case reports and mini-reviews. Awareness of the existence and the therapeutic options of EcV is essential for any physician dealing with patients with gastrointestinal bleeding. This is crucial not only because EcV represent up to 5% of all variceal bleeding episodes [1] but also because of the difficulty in their management and the high mortality secondary to their initial bleeding (up to 40%) [2].
Nowadays, EcV are diagnosed more frequently because of the recent advances in radiological and endoscopic techniques such as double-balloon enteroscopy (DBE) and video capsule endoscopy (PillCam). Indeed, about 8.1% of patients with portal hypertension (PHT) who underwent capsule endoscopy have small-bowel varices [3]. In this review, we present the currently available knowledge relating to the sites, types, pathogenesis, diagnosis and management of EcV.
Sites
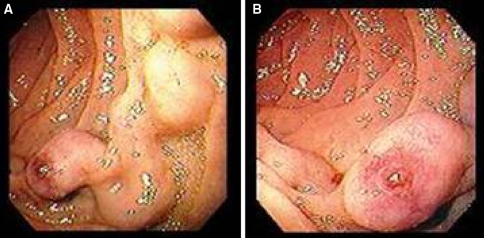
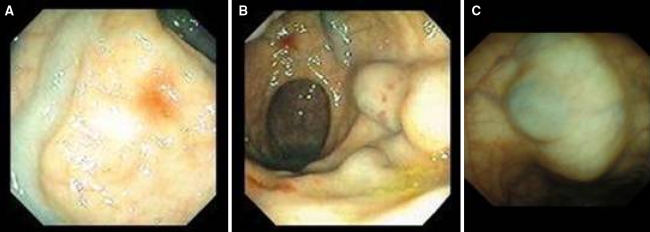
Although EcV occur at several sites (Table 1), the bleeding EcV are most commonly found in the duodenum (Fig. 1), jejunum, ileum, colon, ano-rectal region (Fig. 2), biliary tract, umbilicus, peritoneum or at the sites of previous bowel surgery including stomas (peristomal varices) and trans-anastomotic porto-portal varices. Other infrequent sites include the peritoneum, ovary and vagina.
Table 1.
Recognized sites of EcV
| Duodenum |
| Jejunum |
| Ileum |
| Colon |
| Rectum |
| Peristomal area |
| Biliary tree |
| Peritoneum |
| Around the falciform ligament |
| Umbilicus |
| Urinary bladder |
| Along the splenic ligament |
| Ovary |
| Vagina |
| Right diaphragm |
Fig. 1.
(a) Upper endoscopy picture showing serpiginous varices in the postbulbar duodenum with a focus on intermittent bleeding. (b) Close-up view
Fig. 2.
Sigmoidoscopy (a, b) and colonoscopy (c) pictures showing dilated venous collaterals and spider angiomas in a patient with liver cirrhosis and PHT
Norton et al. [4] reviewed 169 cases of bleeding from EcV. Twenty-six of them were peristomal in origin, 17% in the duodenum, 17% in the jejunum or ileum, 14% in the colon, 8% in the rectum, 9% in the peritoneum, and few were located in other rare sites such as the vagina and the ovary [4]. Another rare site of EcV include the right diaphragm. On rupture, these varices present with acute dyspnoea and right-sided bloody pleural effusion [5]. Trans-anastomotic porto-portal varices are rare. They usually develop in the presence of extrahepatic PHT and presumably arise within the peri-anastomotic inflammatory tissue. Such varices may be difficult to manage and their prognosis is poor if they are bleeding [6].
Prevalence
EcV account for only 1–5% of all variceal bleeding episodes [1, 2, 7]. EcV represent a relatively common finding during endoscopy in patients with PHT. The prevalence of EcV varies according to the modality used for their detection, the patient population studied and the aetiology of PHT. For example, duodenal varices were detected in 40% of patients with intrahepatic PHT undergoing angiography [7], whereas ano-rectal varices have been reported in 10–40% of patients with liver cirrhosis undergoing colonoscopy [8, 9]. Colonic varices were reported in 3.4% of patients with intrahepatic PHT [10]. In addition, a recent study of 37 patients with liver cirrhosis who underwent capsule endoscopy, 3 (8.1%) were found to have small-bowel varices [3].
On upper endoscopy, most patients with duodenal varices have extrahepatic PHT. In fact, most patients with portal or splenic vein thrombosis on angiography are likely to show duodenal varices [4, 11–14]. Intestinal varices have also been reported in a patient with prehepatic PHT secondary to cavernous malformation of the portal vein (portal cavernoma) and were associated with oesophageal varices (OV) [15]. Varices in other parts of the small bowel (jejunum and ileum) and in the colon are commonly seen in patients with intrahepatic PHT who have previously undergone abdominal surgery [11].
Stomal varices, particularly common in patients with intrahepatic PHT, are caused by primary sclerosing cholangitis [11]. Because of the low prevalence of extrahepatic PHT in the western countries, most cases of bleeding from EcV reported in the West are usually associated with intrahepatic PHT [11, 16]. These varices usually bleed at hepatic venous pressure gradients of 12 mmHg or less [17]. Similar to gastric varices (GV), a possible explanation for the lower portal pressure in patients with EcV could be the development of spontaneous spleno-renal shunts or a reduced portal collateral resistance [18]. The bleeding can be massive enough to cause mortality, and the source in such cases can only be identified at autopsy [19].
Table 2 shows the estimated prevalence of EcV in different studies. To the best of our knowledge, data regarding the incidence and/or severity of bleeding in each site are not currently available. A proposed international Web-based EcV registry would be very valuable in this respect.
Table 2.
Estimated prevalence of EcV in different studies
| References | Author(s) | Diagnostic modality | Patient population | n | n (% ) EcV | Sites |
|---|---|---|---|---|---|---|
| [1] | Kinkhabwala et al. | Transhepatic portography | Predominantly IHPHT | 500 | 25 (5) | Ileal |
| [3] | De Palma et al. | Capsule endoscopy | IIHPHT | 37 | 3 (8.1) | Small bowel |
| [7] | Stephan and Miething | Arteriography | IHPHT | 73 | 1 (1.4) | Duodenum |
| [7] | Stephan and Miething | Arteriography | EHPHT | 33 | 9 (27.3) | Duodenum |
| [10] | McCormack et al. | Colonoscopy | Predominantly IHPHT | 102 | 4 (3.6) | Rectal |
| [12] | Salam et al. | Arteriography | GI bleeders | 200 | 6 (3) | GIT and GB |
| [13] | Wilson et al. | Arteriography | GI bleeding | 309 | 5 (1.6) | GIT |
| [14] | Itzchak and Glickman | Arteriography | EHPHT | 20 | 8 (40) | Duodenum |
| [17] | Tripathi et al. | Portography | TIPS patients | 472 | 12 (2.5) | GIT |
| [131] | Sarin et al. | Endoscopy | IHPHT and EHPHT | 1,128 | 53 (4.6) | IGV2 |
EHPHT, extrahepatic portal hypertension; GI, gastrointestinal tract other than the O-G area; IHPHT, intrahepatic portal hypertension
Aetiology and pathogenesis
As shown in Table 3, EcV may develop secondary to PHT, including the idiopathic PHT [20], surgical procedures involving abdominal organs and vessels, anomalies in the venous outflow vessels, abdominal vascular thrombosis, hepatocellular carcinoma, and may be familial in origin [21]. It has also been reported that duodenal and rectal varices develop as a result of band ligation of varices in the oesophago-gastric (OG) junction [22, 23].
Table 3.
Recognized causes of EcV
| PHT (intrahepatic and extrahepatic) |
| Surgical procedures involving abdominal organs and vessels |
| Anomalies in the venous outflow vessels |
| Abdominal vascular thromboses |
| Hepatocellular carcinoma |
| Secondary to band ligation of O-G junction varices |
| Familial |
Most of EcV represent natural portosystemic shunts that develop as a result of high portal pressure anywhere in the gut, around the ovaries, the biliary tree and the bare area of the liver. Under normal circumstances, such collaterals remain collapsed. However, in portal hypertensive patients, the portosystemic collaterals open in a trial to reduce the increased intrahepatic vascular resistance.
Any surgical operation involving apposition of abdominal structures (drained by the systemic veins) to the bowel (drained by the portal tributaries) may result in the formation of collateral vessels at an unusual site. An example is the development of ileostomy varices (stomal varices) in patients with primary sclerosing cholangitis who have undergone colectomy for ulcerative colitis [24]. In addition, bleeding jejunal varices were detected in a case of severe extrahepatic portal vein stenosis secondary to pancreaticoduodenectomy with portal vein resection and intraoperative radiotherapy [25].
Colonic varices may develop in the absence of PHT because of the anomalies in portal venous outflow as in patients with congenital anomalies of portosystemic anastomoses [26], abnormal vessel structure [27], arteriovenous fistulae [28] or they may be familial in origin [21, 27]. In addition, rectal varices may occur secondary to intra-abdominal vascular thrombosis [29].
Because tension in the varix wall is proportional to the radius of the vessel and the transmural pressure across the vessel wall, the major determinants of rupture of EcV are mostly vessel size, portal pressure and varix wall tension [30]. In addition, the prevalence of haemorrhage from rectal varices was shown to be significantly higher in patients with rectal varices of advanced form and/or with a positive “red-colour” sign [31].
Diagnosis
Table 4 provides a list of the recognized presentations of patients with bleeding EcV. Fortunately, “luminal EcV”, that is, those occurring within the gastrointestinal tract lumen, are more common, usually easier to detect and manifest earlier than the “non-luminal EcV”, that is, those elsewhere in the abdominal cavity or the pelvis.
Table 4.
Recognized presentations of bleeding from EcV
| Overt gastrointestinal bleeding of obscure origin |
| Occult gastrointestinal bleeding |
| Accidental finding |
| Iron-deficiency anaemia |
| Haematemesis |
| Haematochezia |
| Internal haemorrhage (haemoperitoneum) |
| Hypovolaemic shock |
| Haemorrhagic pleural effusion |
| At autopsy |
Patients with duodenal varices may present with haematemesis, or massive lower gastrointestinal bleeding [32]. In addition, EcV located distal to the duodenum present mostly with melaena or haematochezia [33]. Moreover, the presence of EcV should be considered in all patients with PHT and gastrointestinal bleeding if both upper and lower gastrointestinal endoscopies failed to show a definite source of bleeding.
Many other cases are discovered accidentally, especially those presenting with anaemia of obscure origin, melaena or positive faecal occult blood testing. EcV can also be detected during routine endoscopy, diagnostic transfemoral or transhepatic angiography [23], Technetium TC-99m red blood cell scintigraphy [34], video capsule endoscopy [3], computed tomography (CT) angiography [35], multislice helical CT [36], CT-enteroclysis [37], contrast-enhanced 3D magnetic resonance angiography [38], endoscopic ultrasound (EUS) [39], laparoscopy or laparotomy (Table 5). In addition, colour Doppler-flow imaging has been used to demonstrate gallbladder varices in three cases of extrahepatic portal venous obstruction (EPVO) and obstructive jaundice [40]. Occasionally, the presence of EcV can be confirmed only at autopsy [41]. It should be noted that EcV can appear as filling defects in barium studies of the colon or small bowel and may be misdiagnosed as polyps or tumours [21]. This emphasizes the importance of endoscopic and angiographic modalities.
Table 5.
Methods of detection of EcV
| Oesophagogastroduodenoscopy |
| Push and DBE |
| Wireless video capsule endoscopy |
| Colonoscopy |
| EUS |
| Colour Doppler-flow imaging |
| Multislice helical CT |
| CT-enteroclysis |
| Contrast-enhanced 3D magnetic resonance angiography |
| TC-99m red blood cell scintigraphy |
| Multidimensional-CT |
| Angiography and CT-angiography |
| During laparotomy or laparoscopy |
| At autopsy |
Varices in the abdominal wall usually rupture externally and can easily be diagnosed, whereas those located around the falciform ligament of the liver, in the diaphragm, in the rectovesical region, or on the splenic ligament may rupture into the peritoneal cavity causing internal bleeding and can be fatal [42, 43]. Diagnosis of cases with internal bleeding needs a high index of clinical suspicion and often presents with rapid accumulation of ascites associated with signs of hypovolaemic shock and a reduction in the haematocrit value. The diagnosis is further indicated by CT scan, which detects retroperitoneal varices and intra-abdominal bleeding or collections, and can be confirmed by the detection of a heavily bloodstained ascitic fluid tap.
Various techniques can be used to reveal the extent of portosystemic collaterals, the direction of flow and the pressure in the portal venous system. These include splenic portography, umbilical vein catheterization, percutaneous transhepatic portography and transjugular transhepatic portography at the time of or after transjugular intrahepatic portosystemic shunt (TIPS) insertion [44–46]. The last three modalities allow direct and selective access to the main tributaries of the portal vein, including the coronary-azygous collaterals, which represent a dominant mechanism in patients with PHT [47].
Role of capsule endoscopy (PillCam)
About 8.1% of patients with PHT who have undergone capsule endoscopy have small-bowel varices [3]. This number reflects a prevalence that is generally higher than expected and points to the role of capsule endoscopy as a non-invasive tool in the workup of patients with obscure gastrointestinal bleeding, including those with chronic liver diseases. Also, a case report by Fix et al. [48] has shown the significance of PillCam in diagnosing obscure gastrointestinal bleeding from mesenteric varices. It has also been found to be beneficial in detecting small-bowel varices in a patient after Whipple’s operation [49]. Furthermore, PillCam as an alternative to upper endoscopy has been tested in 32 patients with liver cirrhosis for the detection of OG varices and portal hypertensive gastropathy [50]. In one patient, PillCam detected small varices that were not seen at endoscopy, and the overall concordance between both modalities was 96.9 and 90.6% for the diagnosis of varices and gastropathy, respectively, without any adverse effects related to PillCam [50]. A large-scale trial is underway to validate and expand these findings.
Role of DBE
At ileocolonoscopy, 18% of patients with liver cirrhosis and PHT have ileal varices [51]. DBE has the potential to visualize the whole small bowel, take biopsy specimens, and perform all necessary endoscopic interventions [52]. Hekmat et al. [53] have recently demonstrated a successful obliteration of a jejunal varix by using N-butyl-2-cyanoacrylate (Histoacryl) in a lesion found ∼240 cm from the ligament of Treitz. This signifies the therapeutic benefit of DBE over capsule endoscopy in small-bowel EcV. The widespread use of this modality in the future would help detect such varices and allow therapeutic intervention, and hence reduce rebleeding, transfusions, and may be mortality.
Management of bleeding EcV
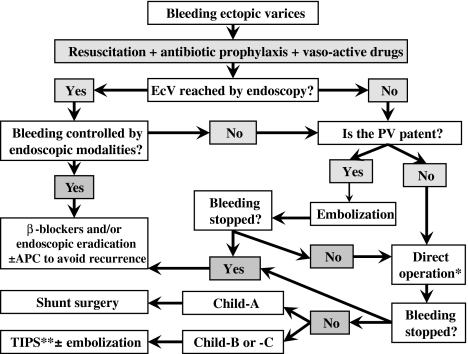
The management of EcV is difficult and may require a multidisciplinary team of endoscopists, hepatologists, surgeons and interventional radiologists (Table 6). It is very difficult to draw guidelines for the treatment of EcV because of the diversity of their location, presentation, complications and diagnostic and therapeutic options. However, the optimal therapeutic modality depends mainly on the location of varices, patient’s condition, the locally available expertise and facilities, and the cause of PHT. Management essentially includes prompt resuscitation, immediate workup to localize the site/source of bleeding, followed by application of the suitable treatment modality or immediate transfer to tertiary referral centres. A proposed systematic approach for any patient presenting with bleeding from possible EcV is shown in Fig. 3.
Table 6.
Therapeutic options for EcV
| Endoscopic |
| Band ligation |
| Injection sclerotherapy |
| Argon plasma coagulation |
| Medical: β-blockers |
| Interventional radiology |
| Embolization |
| TIPS ± embolization |
| B-RTO ± TIO |
| Surgical |
B-RTO, balloon-occluded retrograde transvenous obliteration; TIO, transiliocolic obliteration; TIPS; transjugular intrahepatic portosystemic stent shunt
Fig. 3.
Schematic of the management of bleeding EcV. APC, argon plasma coagulation; EcV, ectopic varices; PV, portal vein; TIPS, transjugular intrahepatic portosystemic shunt. * A direct operation or local devascularization of the EcV is a useful procedure even if portal vein is not patent or the patients have Child-Pugh B or C cirrhosis. ** Use TIPS with caution in patients with Child-Pugh C cirrhosis and weigh the benefit of stopping bleeding against the risk of encephalopathy and deterioration in liver function
Initial management
Similar to acute OG variceal bleeding, clinical assessment, resuscitation, haemodynamic stabilization, antibiotic prophylaxis and referral to specialist centres should be started as soon as possible in patients with suspected EcV bleeding.
The use of vasoactive drugs such as octreotide and terlipressin to reduce splanchnic blood flow and variceal pressure may be of benefit as in patients with bleeding from OG varices [54, 55]. The role of these vasoactive drugs in the control of bleeding from EcV has not been addressed.
All subjects with suspected variceal bleeding should undergo emergency upper endoscopy as a first-line investigation. If it fails to show the source of upper gastrointestinal bleeding, colonoscopy after a rapid colonic purge (3 litres of polyethylene glycol solution delivered via a nasogastric tube) should be the second step of investigation because in a series of 22% of French patients with EcV, bleeding was reported from the colon or rectum [8]. Colonic and rectal varices appear as serpiginous, dilated bluish vessels projecting into the lumen. However, if panendoscopy fails to identify and localize a variceal or a non-variceal source of bleeding, capsule endoscopy, DBE, transfemoral angiography or TC-99m red blood cell scintigraphy or other modalities, as mentioned above, would be the third step of the investigation.
Endoscopic treatment
The use of endoscopic modalities has been reported both in the setting of controlling acute bleeding from EcV and in the secondary prophylaxis. Therefore, depending on the currently available data, primary prophylaxis of EcV bleeding should not be recommended.
Band ligation
Only a few reports are available regarding the successful use of band ligation of EcV mainly in the rectum and duodenum [56–60]. It has also been reported that band ligation, together with balloon-occluded retrograde transvenous obliteration (B-RTO), is beneficial in the management of bleeding duodenal varices [59]. However, if the entire varix cannot be banded, there might be a high risk of developing a wide defect in the varix, especially after sloughing, rendering the banding technique unsafe for large EcV. It has been recommended that banding can be done only if the varix diameter does not exceed the diameter of the endoscope [4].
Injection sclerotherapy
Most EcV are within reach of standard endoscopy [11] or DBE [54]. Several studies have reported successful treatment of duodenal and rectal varices with sclerosant injection [61, 62]. The response to injection sclerotherapy can be unsatisfactory, especially with rectal and colonic varices, probably due to excessive dilution of the sclerosant in large varices beyond a concentration adequate to obliterate the varix. Therefore, a combination of sclerotherapy with banding in such a situation can be attempted [63]. Also, successful control of bleeding from duodenal, jejunal, colonic and rectal varices after injecting with cyanoacrylate, thrombin or any other combination of sclerosants has also been reported [53, 64–67].
Argon plasma coagulation
The use of argon plasma coagulation (APC) as a supplemental treatment in the eradication and prevention of recurring oesophageal variceal after band ligation has been shown to be both effective and safe, and better than band ligation alone [68–70]. APC of EcV has been reported to be effective in stopping bleeding and eradicating ileocolonic anastomotic varices in a 65-year-old male patient [71]. The use of APC in preventing recurrence of endoscopically accessible EcV should be tested in more patients after initial eradication with other modalities such as band ligation or sclerotherapy.
Embolization therapy
Embolization, via intervention radiological techniques, of steel coils, thrombin, gel foam, collagen or autologous blood clot [72], either alone or in combination with band ligation or TIPS, is an effective short-term therapy for bleeding OG varices. The goal of this therapy is not to occlude the bleeding site itself but to occlude the feeding vein (i.e., the vein on the portal venous side) to the EcV. Steel coils are the preferred embolic materials because they lead to a permanent focal occlusion and are available in a variety of sizes, and allow occlusion of large veins without difficulty. The rate of bleeding control has been reported to reach 94% [73, 74]. Unfortunately, embolization does not decompress the portal venous system, resulting in high 1-year rebleeding rates [73]. The feeding veins can be reached via percutaneous transhepatic or transjugular routes.
Percutaneous embolization of bleeding EcV has been reported in the literature as case reports or case series [75–78]. The transhepatic approach is usually preferred, especially in patients with active bleeding, because access to the portal venous system is faster than the transjugular approach. On the other hand, the transhepatic approach may be difficult in patients with portal vein occlusion, but is usually preferred if a subsequent TIPS is planned after variceal embolization [79–81]. Macedo et al. presented a retrospective review of 14 patients, 12 of whom had an abdominal surgery 2–38 years earlier, who underwent transhepatic embolization of coils into the draining veins for the management of bleeding EcV. Rebleeding occurred within 72 h in two patients, and recurrent bleeding from 23 days to 27 months after initial intervention was identified in nine patients. Therefore, it can be concluded that percutaneous coil embolization is a simple and safe treatment for bleeding EcV; however, recurrent bleeding is frequent and repeated intervention is often required. TIPS usually offers good control of bleeding at the expense of a more complex procedure and increased risk of encephalopathy [72]. Okasaki et al. [82] have recently reported a case of obliteration of bleeding giant rectal varices with the use of modified percutaneous transhepatic obliteration with sclerosant.
Medical treatment
The role of β-blockers in the primary and secondary prophylaxis of bleeding from OG varices is well established. However, no solid data exist regarding the use of β-blockers or nitrates in the long-term management of patients with EcV. Although an earlier study in 1986 had shown that β-blocker therapy was not effective in the management of peristomal varices [22], a recent report of three cases had shown their effectiveness [83]. Another case report suggests that β-blockers can be effective as secondary prophylaxis of duodenal variceal rebleeding, especially after simple oversewing of duodenal variceal veins [84]. It seems logical that this modality could be tried in patients with EcV, especially after the implementation of emergency endoscopic or surgical modalities or when patients cannot undergo a surgical shunt [85].
Surgical treatment
If endoscopic modalities or interventional embolization fail to control bleeding from EcV, creating a TIPS or proceeding with surgery is the optimal option depending on the availability of expertise, liver function and the cause of PHT. Direct surgery or local devascularization of the EcV is a useful minimally invasive procedure that does not take much time, does not involve resection of long segments of the small intestine and can be done even if the portal vein is not patent or if the patient has Child B or C cirrhosis [84, 86].
Surgery is preferred both in patients with Child-Pugh class A cirrhosis and in patients with an EPVO. Other surgical interventions reported to control EcV include simple oversewing of the duodenal varices through a duodenotomy [87], duodenal dearterialization and stapling [79], circumferential-stapled anoplasty [88] and double selective shunting [89].
The non-selective portosystemic shunts, such as mesocaval, portocaval or central splenorenal shunt, adequately decompress the portal circulation, but because they are considered major surgical procedures, they are not commonly used nowadays. Also, non-conventional portosystemic shunts using large collateral vessels may be performed in patients with EPVO, for example, children with extensive thrombosis of the portal venous system [90].
Transjugular intrahepatic portosystemic shunt
Many recent publications have addressed the role of TIPS in the successful control of bleeding EcV caused by intrahepatic PHT unresponsive to conservative or endoscopic management [17, 40, 91–102]. The largest four series involved 12, 9, 24 and 21 patients who received TIPS for bleeding EcV [40, 100, 101, 103]. Although TIPS offers a highly effective modality for controlling bleed, the long-term survival of patients is mainly dependent on their liver function. The high efficacy of TIPS has to be balanced against the potential for increased encephalopathy and the procedure-related morbidity.
TIPS together with variceal embolization has the advantage of being effective, minimally invasive, can be performed in one session, does not preclude subsequent liver transplantation, and therefore may be used during the acute situation both as a bridge to transplantation and as the definitive therapy in patients unfit for surgery.
Balloon-occluded retrograde transvenous obliteration
B-RTO is a recent therapeutic technique for the management of patients with large GV. The technique is valuable in patients who bleed at lower portal pressures, patients with hepatic encephalopathy, and when the portal vein is not patent. Recently, B-RTO—alone or in combination with transiliocolic obliteration of vein—has also been shown to be effective in controlling bleeding of duodenal varices that failed endoscopic therapy in poor surgical candidates, without complications or recurrence for a period of up to 3 years [104–108]. However, its use is currently limited because of its low availability and lack of technical expertise, and caution is required in patients with large OV. Most of the available literature addressing this method originates from the Far East, mainly Japan, and the early results are promising. B-RTO might be a difficult procedure, but it works well if the doctors are familiar with the procedure.
Special types of EcV
Intra-abdominal varices
Varices in the abdominal wall usually rupture externally and therefore are easily recognized and treated with local compression and surgical ligation. Many cases of veins around the falciform ligament of the liver that rupture into the peritoneal cavity have been reported and are characterized by a rapid increase in ascites, particularly in the presence of abdominal pain, and associated with a decrease in the haematocrit value. Management of this situation is difficult because transhepatic obliteration of the varices is relatively contraindicated because of the accompanying ascites. Other modes of therapy include transjugular, intrahepatic embolization of the portal venous system, TIPS placement, and emergency surgical ligation of the bleeding varix, but this results in high mortality [109].
Stomal varices
The term “ectopic stomal varices” refers to abnormally dilated veins that have developed in the stomal mucosa. Stomal varices are commonly seen in patients with ileostomies after proctocolectomy for inflammatory bowel disease associated with primary sclerosing cholangitis and PHT [24]. Stomal varices are recognized by the purplish hue around the stoma. As the patient is usually aware of the bleed early in the clinical course, he or she may be taught how to control the bleeding with pressure. Therefore, mortality from bleeding stomal varices is relatively low (3–4%) [92]. A case report from Korea described the use of 2D reformatted and 3D volume rendered images by multidimensional-CT in a patient with an episode of acute bleeding from the colonic stoma [110]. Local measures, such as epinephrine-soaked gauze, pressure dressings, suture ligation, gel foam or refashioning the stoma, have all been applied successfully in controlling the initial bleeding episode [93, 111]. Injection sclerotherapy has also been tried, but it may cause mucosal ulceration, stomal orifice stricture and peristomal skin necrosis [112]. In patients with uncontrolled or recurrent bleeding, a portosystemic procedure should be contemplated. TIPS—alone on in combination with embolization therapy—is preferred to a surgical portosystemic shunt because patients with stomal varices may be candidates for liver transplantation [111, 113–116].
Biliary tract varices
The development of biliary tract varices is a rare complication of PHT and sometimes is referred to as “pseudocholangiocarcinoma” or “pseudosclerosing cholangitis” or “portal hypertensive bilopathy”. In a series of 42 patients with EPVO, gallbladder varices were detected by Doppler ultrasonography in 11 patients and choledochal varices in 9 patients [117]. Another study showed varices around the gallbladder and/or the biliary channels in 30% of patients [118]. Biliary varices are usually asymptomatic, often discovered accidentally, in the absence of other signs of PHT [119], but can lead to silent fatal outcomes [120]. Occurrence of varices around the common bile duct can result in extrahepatic biliary obstruction, cholangitis and haemobilia. The appearances of a biliary tree on endoscopic retrograde cholangiopancreatography may mimic those of primary sclerosing cholangitis [121]. Also, EUS can serve to diagnose biliary varices in patients with EPVO and jaundice. Although biliary varices are mainly asymptomatic, they may cause obstructive jaundice when they are located in the wall of the common bile duct. EUS can also detect unrecognized malignant tumours in patients with EPVO of undetermined origin [39]. Smith et al. [122] reported a case of severe gastrointestinal bleeding due to jejunal-biliary anastomotic varices. The anastomotic site was the location of the pressure gradient, from the high-pressure small-bowel varices to the low-pressure biliary tract. This was successfully treated by disconnection of the anastomosis and bile duct repair. Therapeutic modalities of biliary varices include surgical portosystemic shunt and endoscopic, radiological or even surgical biliary drainage procedures.
Ano-rectal varices
The misdiagnosis of ano-rectal varices as haemorrhoids can sometimes have devastating consequences. Therefore, it is important to differentiate anal varices from haemorrhoids. The former collapse with digital pressure, whereas the latter do not. Rectal varices are enlarged portosystemic collateral veins, which develop in patients with PHT as a pathway for portal venous blood flow from the superior haemorrhoidal veins (portal) to and through the middle and inferior haemorrhoidal veins (systemic). Massive bleeding from ano-rectal varices has been reported, but such reports are infrequent [123–125]. On the other hand, haemorrhoids represent a common cause of rectal bleeding, but their prevalence in patients with PHT is not higher than the general population [126]. Weinshel et al. [127] have published an excellent review of the differentiation, pathogenesis and management of these two entities.
Ectopic IGV type 2
GV may be primary or secondary in origin. The former refers to those varices that are present at the initial endoscopic examination in a patient who never underwent variceal sclerotherapy or band ligation for OV, whereas the latter refers to GV that develop after endoscopic therapy for OV. Many classification systems have been proposed for GV on the basis of their location, size, colour, form and relation to OV. However, the most widely used classification system is that proposed by Sarin et al. [128, 129] and recommended by the Baveno III consensus working group [130], and categorizes GV on the basis of their location in the stomach and their relationship with OV (Table 7).
Table 7.
Classification of GVa
| IGV (GV occurring in the absence of OV) | G-OV (GV extending from OV into the stomach) | ||
|---|---|---|---|
| Type 1 (IGV1) | Type 2 (IGV2) | Type 1 (G-OV1) | Type 2 (G-OV2) |
| Varices located in the fundus that are often tortuous and complex in shape | EcV in the antrum, corpus and around the pylorus | Varices continuous with OV and extending along the lesser curve for about 2–5 cm below the G-O junction | Often long, tortuous, varices extending from the oesophagus below the G-O junction towards the fundus |
| 8% | 2% | 74% | 16% |
IGV2 are present either in the body or on the antrum of the stomach or upper duodenum. Sarin et al. [131] have described the prevalence, natural history and clinical significance of these varices in a prospective study involving 1,128 patients with PHT. Of these patients, 53 (4.7%) had IGV2. These IGV2 were predominantly (84.9%) secondary in origin and located in the antrum (53%), duodenum (32%) or at both sites (11%), and rarely in the corpus or fundus (4%). Bleeding due to IGV2 was seen only in three (5.7%) patients during a mean follow-up of 36.3 ± 12.1 months and could be successfully managed with endoscopic ligation or obliteration [131].
Recommended future research
Because of the low incidence of EcV and the lack of valid reproduced RCTs addressing this complication, we recommend the establishment of an international Web-based EcV case registry through which a more precise epidemiologic, diagnostic, prognostic, prophylactic and therapeutic data can be obtained. Major referral centres should be encouraged to participate and register their cases and subsequently be involved in multicentre RCTs concentrating on the management of such patients. Also, comparative haemodynamic studies between patients with G-O varices and those with EcV are warranted.
Concluding remarks
Most of the available data about EcV are obtained from case reports or short series of cases.
EcV are being recognized more frequently nowadays because of the continuous advances in the endoscopic and imaging techniques.
Ectopic variceal bleeding is reported in patients with internal haemorrhage, hypovolaemic shock, occult gastrointestinal bleeding, anaemia or bleeding from the gut of obscure origin, especially in patients with PHT, following abdominal surgical procedures, in cases with extrahepatic venous obstruction or thrombosis, or anomalies of the portal venous system.
It is difficult to recommend general guidelines for the management of EcV and each case should be dealt with depending on the site and severity of bleeding and according to available expertise and facilities.
Patients with EcV bleeding must be considered difficult, should be managed in specialized canters, and have to be approached with a multidisciplinary team involving intensivists, gastroenterologists, surgeons and interventional radiologists.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Abbreviations
- APC
Argon plasma coagulation
- B-RTO
Balloon-occluded retrograde transvenous obliteration
- CT
Computed tomography
- EcV
Ectopic varices
- EUS
Endoscopic ultrasound
- EPVO
Extrahepatic portal venous obstruction
- G-O
Gastro-oesophageal
- GV
Gastric varices
- IGV
Isolated gastric varices
- OV
Oesophageal varices
- OG
Oesophago-gastric
- PHT
Portal hypertension
- RCT
Randomized-controlled trials
- TIPS
Transjugular intrahepatic portosystemic shunt
Footnotes
An erratum to this article can be found at http://dx.doi.org/10.1007/s12072-008-9089-7
References
- 1.Kinkhabwala M, Mousavi A, Iyer S, Adamsons R. Bleeding ileal varicosity demonstrated by transhepatic portography. AJR Am J Roentgenol. 1977;129:514–6. [DOI] [PubMed]
- 2.Khouqeer F, Morrow C, Jordan P. Duodenal varices as a cause of massive upper gastrointestinal bleeding. Surgery. 1987;102:548–52. [PubMed]
- 3.De Palma GD, Rega M, Masone S, Persico F, Siciliano S, Patrone F, et al. Mucosal abnormalities of the small bowel in patients with cirrhosis and portal hypertension: a capsule endoscopy study. Gastrointest Endosc. 2005;62:529–34. [DOI] [PubMed]
- 4.Norton ID, Andrews JC, Kamath PS. Management of EcV. Hepatology. 1998;28:1154–8. [DOI] [PubMed]
- 5.Matsui M, Kojima A, Kakizaki S, Nagasaka K, Sohara N, Sato K, et al. Ectopic varices in a right diaphragm that ruptured into the pleural cavity. Acta Med Okayama. 2006;60:229–32. [DOI] [PubMed]
- 6.Mitchell AW, Jackson JE. Trans-anastomotic porto-portal varices in patients with gastrointestinal haemorrhage. Clin Radiol. 2000;55:207–11. [DOI] [PubMed]
- 7.Stephan G, Miething R. Rontgendiagnostik varicoser Duodenal veranderungen bei portaler Hypertension. Der Radiol. 1968;3:90–5. [PubMed]
- 8.Hosking SW, Smart HL, Johnson AG, Triger DR. Anorectal varices, hemorrhoids and portal hypertension. Lancet. 1989;1:349–52. [DOI] [PubMed]
- 9.Naveau S, Poynard T, Pauphilet C, Aubert A, Chaput JC. Rectal and colonic varices in cirrhosis. Lancet. 1989;1:624. [DOI] [PubMed]
- 10.McCormack TT, Bailey HR, Simms JM, Johnson AG. Rectal varices are not piles. Br J Surg. 1984;71:163. [DOI] [PubMed]
- 11.Lebrec D, Benhamou JP. Ectopic varices in portal hypertension. Clin Gastroenterol. 1985;14:105–21. [PubMed]
- 12.Salam AA, Goldman M, Smith D, Hill HL. Gastric, intestinal, and gallbladder varices: hemodynamic and therapeutic considerations. South Med J. 1979;72:402–8. [DOI] [PubMed]
- 13.Wilson SE, Stone RT, Christie JP, Passaro E. Jr. Massive lower gastrointestinal bleeding from intestinal varices. Arch Surg. 1979;114:1158–61. [DOI] [PubMed]
- 14.Itzchak Y, Glickman MG. Splenic vein thrombosis in patients with a normal size spleen. Invest Radiol. 1977;12:158–63. [DOI] [PubMed]
- 15.Sorrentino D, Labombarda A, Debiase F, Trevisi A, Giagu P. Cavernous transformation of the portal vein associated to multiorgan developmental abnormalities. Liver Int. 2004;24:80–3. [DOI] [PubMed]
- 16.Tanaka T, Kato K, Taniguchi T, Takagi D, Takeyama N, Kitazawa Y. A case of ruptured duodenal varices and review of the literature. Jpn J Surg. 1988;18:595–600. [DOI] [PubMed]
- 17.Tripathi D, Helmy A, Macbeth K, Balata S, Lui HF, Stanley AJ, et al. Ten years’ follow-up of 472 patients following transjugular intrahepatic portosystemic stent-shunt insertion at a single centre. Eur J Gastroenterol Hepatol. 2004;16:9–18. [DOI] [PubMed]
- 18.Watanabe K, Kimura K, Matsutani S, Ohto M, Okuda K. Portal hemodynamics in patients with gastric varices. A study in 230 patients with esophageal and/or gastric varices using portal vein catheterization. Gastroenterology. 1988;95:434–40. [DOI] [PubMed]
- 19.Machida T, Sato K, Kojima A, Takezawa J, Sohara N, Kakizaki S, et al. Ruptured duodenal varices after endoscopic ligation of esophageal varices: an autopsy case. Gastrointest Endosc. 2006;63:352–4. [DOI] [PubMed]
- 20.Francois F, Tadros C, Diehl D. Pan-colonic varices and idiopathic portal hypertension. J Gastrointestin Liver Dis. 2007;16:325–8. [PubMed]
- 21.Zaman L, Bebb JR, Dunlop SP, Jobling JC, Teahon K. Familial colonic varices: a cause of “polyposis” on barium enema. Br J Radiol. 2008;81:17–9. [DOI] [PubMed]
- 22.Wu WC, Wang LY, Yu FJ, Wang WM, Chen SC, Chuang WL, et al. Bleeding duodenal varices after gastroesophageal varices ligation: a case report. Kaohsiung J Med Sci. 2002;18:578–81. [PubMed]
- 23.Katakura K, Irisaw A, Obara K, Saito A, Shishido H, Shibukawa G, et al. Appearance of rectal varices in extrahepatic portal obstruction after treatment for esophago-gastric varices: a case report. Fukushima J Med Sci. 2002;48:51–6. [DOI] [PubMed]
- 24.Weisner RH, LaRusso NF, Dozois RR. Peristomal varices after proctocolectomy in patients with primary sclerosing cholangitis. Gastroenterology. 1986;90:316–22. [DOI] [PubMed]
- 25.Sakai M, Nakao A, Kaneko T, Takeda S, Inoue S, Yagi Y, et al. Transhepatic portal venous angioplasty with stenting for bleeding jejunal varices. Hepatogastroenterology. 2005;52:749–52. [PubMed]
- 26.Feldman M, Smith VM, Warner CG. Varices of the colon: report of 3 cases. JAMA. 1962;179:729–30. [DOI] [PubMed]
- 27.Iredale JP, Ridings P, McGinn FP, Arthur MJ. Familial and idiopathic colonic varices: an unusual cause of lower gastrointestinal haemorrhage. Gut. 1992;33:1285–8. [DOI] [PMC free article] [PubMed]
- 28.Wheeler HB, Warren R. Duodenal varices due to portal hypertension due to arteriovenous aneurysm. Ann Surg. 1957;146:229–38. [DOI] [PMC free article] [PubMed]
- 29.Ryu SH, Chang HS, Myung SJ, Yang SK. Rectal varices caused by thrombosis of intra-abdominal vessels. Gastrointest Endosc. 2002;55:409. [DOI] [PubMed]
- 30.Groszmann RJ. Reassessing portal venous pressure measurements. Gastroenterology. 1984;86:1611–4. [PubMed]
- 31.Shudo R, Yazaki Y, Sakurai S, Uenishi H, Yamada H, Sugawara K. Clinical study comparing bleeding and nonbleeding rectal varices. Endoscopy. 2002;34:189–94. [DOI] [PubMed]
- 32.Khan MQ, Al-Momen S, Alghssab A. Duodenal varices causing massive lower gastrointestinal hemorrhage. Ann Saudi Med. 1999;19:440–3. [DOI] [PubMed]
- 33.Khan AA, Sarwar S, Alam A, Butt AK, Shafqat F, Tarique S, et al. Ectopic intestinal varices as a rare cause of lower gastrointestinal haemorrhage. J Coll Physicians Surg Pak. 2003;13:526–7. [PubMed]
- 34.Bykov S, Becker A, Koltun L, Yudko E, Garty I. Massive bleeding from jejunal varices in a patient with thalassemia major detected by TC-99m red blood cell scintigraphy. Clin Nucl Med. 2005;30:457–9. [DOI] [PubMed]
- 35.Kakizaki S, Ishikawa T, Koyama Y, Yamada H, Kobayashi R, Sohara N, et al. Primary biliary cirrhosis complicated with sigmoid colonic varices: the usefulness of computed tomographic angiography. Abdom Imaging. 2003;28:831–4. [DOI] [PubMed]
- 36.Weishaupt D, Pfammatter T, Hilfiker PR, Wolfensberger U, Marincek B. Detecting bleeding Duodenal varices with multislice helical CT. AJR Am J Roentgenol. 2002;178:399–401. [DOI] [PubMed]
- 37.Jain TP, Gulati MS, Makharia GK, Paul SB. Case of the season: detection of duodenal varices by CT enteroclysis. Semin Roentgenol. 2005;40:204–6. [DOI] [PubMed]
- 38.Handschin AE, Weber M, Weishaupt D, Fried M, Clavien PA. Contrast-enhanced three-dimensional magnetic resonance angiography for visualization of ectopic varices. Dis Colon Rectum. 2002;45:1541–4. [DOI] [PubMed]
- 39.Palazzo L, Hochain P, Helmer C, Cuillerier E, Landi B, Roseau G, et al. Biliary varices on endoscopic ultrasonography: clinical presentation and outcome. Endoscopy. 2000;32:520–4. [DOI] [PubMed]
- 40.Gulati G, Pawa S, Chowdhary V, Kumar N, Mittal SK. Colour Doppler flow imaging findings in portal biliopathy. Trop Gastroenterol. 2003;24:116–9. [PubMed]
- 41.Hashiguchi M, Tsuji H, Shimono J, Azuma K, Fujishima M. Ruptured duodenal varices: an autopsy case report. Hepatogastroenterology. 1999;46:1751–4. [PubMed]
- 42.Olusola BF, McCashland TM, Seemayer TA, Sorrell MF. Rectovesical ectopic varix intraperitoneal hemorrhage with fatal outcome. Am J Gastroenterol. 2002;97:504. [DOI] [PubMed]
- 43.Ramchandran TM, John A, Ashraf SS, Moosabba MS, Nambiar PV, Shobana Devi R. Hemoperitoneum following rupture of ectopic varix along splenorenal ligament in extrahepatic portal vein obstruction. Indian J Gastroenterol. 2000;19:91. [PubMed]
- 44.Turner MD, Sherlock S, Steiner RE. Splenic venography and intrasplenic pressure measurement in the clinical investigation of the protal venous system. Am J Med. 1957;23:846–59. [DOI] [PubMed]
- 45.Kessler RE, Tice DA, Zimmon DS. Value, complications, and limitations of umbilical vein catheterization. Surg Gynecol Obstet. 1973;136:529–35. [PubMed]
- 46.Smith-Laing G, Camilo ME, Dick R, Sherlock S. Percutaneous transhepatic portography in the assessment of portal hypertension. Clinical correlations and comparison of radiographic techniques. Gastroenterology. 1980;78:197–205. [PubMed]
- 47.Bosch J, Groszmann RJ. Measurement of azygos venous blood flow by a continuous thermal dilution technique: an index of blood flow through gastroesophageal collaterals in cirrhosis. Hepatology. 1984;4:424–9. [DOI] [PubMed]
- 48.Fix OK, Simon JT, Farraye FA, Oviedo JA, Pratt DS, Chen WT, et al. Obscure gastrointestinal hemorrhage from mesenteric varices diagnosed by video capsule endoscopy. Dig Dis Sci. 2006;51:1169–74. [DOI] [PubMed]
- 49.Hellmig S, Seeger M, Stüber E, Kiehne K, Schreiber S, Fölsch UR. Endoscopic-guided capsule endoscopy in a patient with small-bowel varices after Whipple’s operation. Gastrointest Endosc. 2005;62:166–9. [DOI] [PubMed]
- 50.Eisen GM, Eliakim R, Zaman A, Schwartz J, Faigel D, Rondonotti E, et al. The accuracy of PillCam ESO capsule endoscopy versus conventional upper endoscopy for the diagnosis of esophageal varices: a prospective three-center pilot study. Endoscopy. 2006;38:31–5. [DOI] [PubMed]
- 51.Misra SP, Dwivedi M, Misra V, Gupta M. Ileal varices and portal hypertensive ileopathy in patients with cirrhosis and portal hypertension. Gastrointest Endosc. 2004;60:778–83. [DOI] [PubMed]
- 52.Heine GD, Hadithi M, Groenen MJ, Kuipers EJ, Jacobs MA, Mulder CJ. Double-balloon enteroscopy: indications, diagnostic yield, and complications in a series of 275 patients with suspected small-bowel disease. Endoscopy. 2006;38:42–8. [DOI] [PubMed]
- 53.Hekmat H, Al-toma A, Mallant MP, Mulder CJ, Jacobs MA. Endoscopic N-butyl-2-cyanoacrylate (Histoacryl) obliteration of jejunal varices by using the double balloon enteroscope. Gastrointest Endosc. 2007;65(2):350–2. [DOI] [PubMed]
- 54.Besson I, Ingrand P, Person B, Boutroux D, Heresbach D, Bernard P, et al. Sclerotherapy with or without octreotide for acute variceal bleeding. N Engl J Med. 1995;333:555–60. [DOI] [PubMed]
- 55.Silvain C, Carpentier S, Sautereau D, Czernichow B, Métreau JM, Fort E, et al. Terlipressin plus transdermal nitroglycerin versus octreotide in the control of acute bleeding from esophageal varices: a multicenter randomized trial. Hepatology. 1993;18:61–5. [PubMed]
- 56.Shudo R, Yazaki Y, Sakurai S, Uenishi H, Yamada H, Sugawara K, et al. Combined endoscopic variceal ligation and sclerotherapy for bleeding rectal varices associated with primary biliary cirrhosis: a case showing a long-lasting favorable response. Gastrointest Endosc. 2001;53:661–5. [DOI] [PubMed]
- 57.Firoozi B, Gamagaris Z, Weinshel EH, Bini EJ. Endoscopic band ligation of bleeding rectal varices. Dig Dis Sci. 2002;47:1502–5. [DOI] [PubMed]
- 58.Bosch A, Marsano L, Varilek GW. Successful obliteration of duodenal varices after endoscopic ligation. Dig Dis Sci. 2003;48:1809–12. [DOI] [PubMed]
- 59.Akazawa Y, Murata I, Yamao T, Yamakawa M, Kawano Y, Nomura N, et al. Successful management of bleeding duodenal varices by endoscopic variceal ligation and balloon-occluded retrograde transvenous obliteration. Gastrointest Endosc. 2003;58:794–7. [DOI] [PubMed]
- 60.Fayad N, Nammour F, Elfant A. Endoscopic variceal ligation for bleeding duodenal varices. J Clin Gastroenterol. 2004;38:467. [DOI] [PubMed]
- 61.Barbish AW, Ehrinpreis MN. Successful endoscopic injection sclerotherapy of a bleeding duodenal varix. Am J Gastroenterol. 1993;88:90–2. [PubMed]
- 62.Yamanaka T, Shiraki K, Ito T, Sugimoto K, Sakai T, Ohmori S, et al. Endoscopic sclerotherapy (ethanolamine oleate injection) for acute rectal varices bleeding in a patient with liver cirrhosis. Hepatogastroenterology. 2002;49:941–3. [PubMed]
- 63.Ikeda K, Konishi Y, Nakamura T, Nabeshima M, Yamamoto S, Migihashi R, et al. Rectal varices successfully treated by endoscopic injection sclerotherapy after careful hemodynamic evaluation: a case report. Gastrointest Endosc. 2001;54:788–91. [DOI] [PubMed]
- 64.Sans M, Llach J, Bordas JM, Andreu V, Reverter JC, Bosch J, et al. Thrombin and ethanolamine injection therapy in arresting uncontrolled bleeding from duodenal varices. Endoscopy. 1996;28:403. [DOI] [PubMed]
- 65.Bhasin DK, Sharma BC, Sriram PV, Makharia G, Singh K. Endoscopic management of bleeding ectopic varices with histoacryl. HPB Surg. 1999;11:171–3. [DOI] [PMC free article] [PubMed]
- 66.Schafer TW, Binmoeller KF. Argon plasma coagulation for the treatment of colonic varices. Endoscopy. 2002;34:661–3. [DOI] [PubMed]
- 67.Chen WC, Hou MC, Lin HC, Chang FY, Lee SD. An endoscopic injection with N-butyl-2-cyanoacrylate used for colonic variceal bleeding: a case report and review of the literature. Am J Gastroenterol. 2000;95:540–2. [DOI] [PubMed]
- 68.Ryu SH, Moon JS, Kim I, Kim YS, Lee JH. Endoscopic injection sclerotherapy with N-butyl-2-cyanoacrylate in a patient with massive rectal variceal bleeding: a case report. Gastrointest Endosc. 2005;62:632–5. [DOI] [PubMed]
- 69.Cipolletta L, Bianco MA, Rotondano G, Marmo R, Meucci C, Piscopo R. Argon plasma coagulation prevents variceal recurrence after band ligation of esophageal varices: preliminary results of a prospective randomized trial. Gastrointest Endosc. 2002;56:467–71. [DOI] [PubMed]
- 70.Furukawa K, Aoyagi Y, Harada T, Enomoto H. The usefulness of prevention consolidation therapy of esophageal varices using an argon plasma coagulation technique. Hepatol Res. 2002;23:220–5. [DOI] [PubMed]
- 71.Nakamura S, Mitsunaga A, Murata Y, Suzuki S, Hayashi N. Endoscopic induction of mucosal fibrosis by argon plasma coagulation (APC) for esophageal varices: a prospective randomized trial of ligation plus APC vs. ligation alone. Endoscopy. 2001;33:210–5. [DOI] [PubMed]
- 72.Ohnishi K, Takayasu K, Takashi M. Transhepatic obliteration of esophageal varices using stainless steel coils combined with hypertonic glucose and gelfoam. J Clin Gastroenterol. 1985;7:200–7. [DOI] [PubMed]
- 73.Smith-Lang G, Scott J, Long RG, Sherlock S. Role of percutaneous transhepatic obliteration of varices in the management of bleeding from gastroesophageal varices. Gastroenterology. 1981;80:1031–6. [PubMed]
- 74.Viamonte M Jr, Pereiras R, Russell E, Le Page J, Hutson D. Transhepatic obliteration of gastroesophageal varices in acute and non-acute bleeders. AJR Am J Roentgenol. 1977;129:237–41. [DOI] [PubMed]
- 75.Ozaki CK, Hansen M, Kadir S. Transhepatic embolization of superior mesenteric varices in portal hypertension. Surgery. 1988;105:446–8. [PubMed]
- 76.Samaraweera RN, Feldman L, Widrich WC, Waltman A, Steinberg F, Greenfield A, et al. Stomal varices: percutaneous transhepatic embolization. Radiology. 1989;170:779–82. [DOI] [PubMed]
- 77.Toumeh KK, Girardot JD, Choo IW, Andrews JC, Cho KJ. Percutaneous transhepatic embolization as treatment for bleeding ileostomy varices. Cardiovasc Intervent Radiol. 1995;18:179–82. [DOI] [PubMed]
- 78.Macedo TA, Andrews JC, Kamath PS. Ectopic varices in the gastrointestinal tract: short- and long-term outcomes of percutaneous therapy. Cardiovasc Intervent Radiol. 2005;28:178–84. [DOI] [PubMed]
- 79.Hidajat N, Stobbe H, Hosten N, Schroeder RJ, Fauth M, Vogl T, et al. Transjugular intrahepatic portosystemic shunt and transjugular embolization of bleeding rectal varices in portal hypertension. AJR Am J Roentgenol. 2002;178:362–3. [DOI] [PubMed]
- 80.lluminati G, Smail A, Azoulay D, Castaing D, Bismuth H. Association of transjugular intrahepatic portosystemic shunt with embolization in the treatment of bleeding duodenal varix refractory to sclerotherapy. Dig Surg. 2000;17:398–400. [DOI] [PubMed]
- 81.Dharancy S, Sergent G, Bulois P, Bonnal JL, Golup G, Mauroy B, et al. Bleeding stomal varices treated with embolization and transjugular porto-systemic shunt. Gastroenterol Clin Biol. 2000;24(2):232–4. [PubMed]
- 82.Okazaki H, Higuchi K, Shiba M, Nakamura S, Wada T, Yamamori K, et al. Successful treatment of giant rectal varices by modified percutaneous transhepatic obliteration with sclerosant: report of a case. World J Gastroenterol. 2006;12:5408–11. [DOI] [PMC free article] [PubMed]
- 83.Noubibou M, Douala HC, Druez PM, Kartheuzer AH, Detry RJ, Geubel AP. Chronic stomal variceal bleeding after colonic surgery in patients with portal hypertension: efficacy of beta-blocking agents? Eur J Gastroenterol Hepatol. 2006;18:807–8. [DOI] [PubMed]
- 84.Hsieh JS, Wang WM, Perng DS, Huang CJ, Wang JY, Huang T. Modified devascularization surgery for isolated gastric varices assessed by endoscopic ultrasonography. Surg Endosc. 2004;18:666–71. [DOI] [PubMed]
- 85.Cottam DR, Clark R, Hayn E, Shaftan G. Duodenal varices: a novel treatment and literature review. Am Surg. 2002;68:407–9. [PubMed]
- 86.Goyal N, Singhal D, Gupta S, Soin AS, Nundy S. Transabdominal gastroesophageal devascularization without transection for bleeding varices: results and indicators of prognosis. J Gastroenterol Hepatol. 2007;22:47–50. [DOI] [PubMed]
- 87.McAlister VC, Al-Saleh NA. Duodenal dearterialization and stapling for severe hemorrhage from duodenal varices with portal vein thrombosis. Am J Surg. 2005;189:49–52. [DOI] [PubMed]
- 88.Botterill ID, Jayne DG, Snelling AP, Ambrose NS. Correction of symptomatic ano-rectal varices with circumferential stapled anoplasty. Colorectal Dis. 2002;4:217. [DOI] [PubMed]
- 89.Sato Y, Yokoyama N, Suzuki S, Tani T, Nomoto M, Hatakeyama K. Double selective shunting for esophagogastric and rectal varices in portal hypertension due to congenital hepatic polycystic disease. Hepatogastroenterology. 2002;49:1528–30. [PubMed]
- 90.D’Cruz AJ, Kamath PS, Ramachandra C, Jalihal A. Non-conventional portosystemic shunts in children with extrahepatic portal vein obstruction. Acta Pediatr Jpn. 1995;37:17–20. [DOI] [PubMed]
- 91.D’Amico G, Pagliaro L, Bosch J. The treatment of portal hypertension: a meta-analytic review. Hepatology. 1995;22:332–54. [DOI] [PubMed]
- 92.McChesney L, Jensen D, Matalon T, Ganger D, Sankary H, Foster P, et al. Duodenal varices: a case report and review of the literature. HPB Surg. 1995;9:31–5. [DOI] [PMC free article] [PubMed]
- 93.Haskal ZJ, Scott M, Rubin RA, Cope C. Intestinal varices: treatment with the transjugular intrahepatic portosystemic shunt. Radiology. 1994;191:183–7. [DOI] [PubMed]
- 94.Johnson PA, Laurin J. Transjugular portosystemic shunt for treatment of bleeding stomal varices. Dig Dis Sci. 1997;42:440–2. [DOI] [PubMed]
- 95.Bernstein D, Yrizarry J, Reddy KR, Russell E, Jeffers L, Schiff ER. Transjugular intrahepatic portosystemic shunt in the treatment of intermittently bleeding stomal varices. Am J Gastroenterol. 1996;91:2237–8. [PubMed]
- 96.Jonnalagadda SS, Quiason S, Smith OJ. Successful therapy of bleeding duodenal varices by TIPS after failure of sclerotherapy. Am J Gastroenterol. 1998;93:272–4. [DOI] [PubMed]
- 97.Ory G, Spahr L, Megevand JM, Becker C, Hadengue A. The long-term efficacy of the intrahepatic portosystemic shunt (TIPS) for the treatment of bleeding anorectal varices in cirrhosis. A case report and review of the literature. Digestion. 2001;64:261–4. [DOI] [PubMed]
- 98.Ryu RK, Nemcek AA Jr, Chrisman HB, Saker MB, Blei A, Omary RA, et al. Treatment of stomal variceal hemorrhage with TIPS: case report and review of the literature. Cardiovasc Intervent Radiol. 2000;23:301–3. [DOI] [PubMed]
- 99.Morris CS, Najarian KE. Transjugular intrahepatic portosystemic shunt for bleeding stomal varices associated with chronic portal vein occlusion: long-term angiographic, hemodynamic, and clinical follow-up. Am J Gastroenterol. 2000;95:2966–8. [DOI] [PubMed]
- 100.Tripathi D, Jalan R. Transjugular intrahepatic portosystemic stent-shunt in the management of gastric and ectopic varices. Eur J Gastroenterol Hepatol. 2006;18:1155–60. [DOI] [PubMed]
- 101.Vidal V, Joly L, Perreault P, Bouchard L, Lafortune M, Pomier-Layrargues G. Usefulness of transjugular intrahepatic portosystemic shunt in the management of bleeding ectopic varices in cirrhotic patients. Cardiovasc Intervent Radiol. 2006;29:216–9. [DOI] [PubMed]
- 102.Almeida JR, Trevisan L, Guerrazzi F, Mesquita MA, Ferraz JG, Montes CG, et al. Bleeding duodenal varices successfully treated with TIPS. Dig Dis Sci. 2006;5:1738–41. [DOI] [PubMed]
- 103.Vangeli M, Patch D, Terreni N, Tibballs J, Watkinson A, Davies N, et al. Bleeding ectopic varices: treatment with transjugular intrahepatic porto-systemic shunt (TIPS) and embolisation. J Hepatol. 2004;41:560–6. [DOI] [PubMed]
- 104.Ohta M, Yasumori K, Saku M, Saitsu H, Muranaka T, Yoshida K. Successful treatment of bleeding duodenal varices by balloon-occluded retrograde transvenous obliteration: a transjugular venous approach. Surgery. 1999;126:581–3. [PubMed]
- 105.Tominaga K, Montani A, Kuga T, Shiba M, Watanabe T, Fujiwara Y, et al. Combined balloon-occluded embolization for treatment of concurrent duodenal, gastric, and esophageal varices: a case report. Gastrointest Endosc. 2001;53:665–8. [DOI] [PubMed]
- 106.Ota K, Okazaki M, Higashihara H, Kokawa H, Shirai Z, Anan A, et al. Combination of transileocolic vein obliteration and balloon-occluded retrograde transvenous obliteration is effective for ruptured duodenal varices. J Gastroenterol. 1999;34:694–9. [DOI] [PubMed]
- 107.Takamura K, Miyake H, Mori H, Terashima Y, Ando T, Fujii M, et al. Balloon occluded retrograde transvenous obliteration and percutaneous transhepatic obliteration for ruptured duodenal varices after operation for rectal cancer with multiple liver metastasis: report of a case. J Med Invest. 2005;52:212–7. [DOI] [PubMed]
- 108.Zamora CA, Sugimoto K, Tsurusaki M, Izaki K, Fukuda T, Matsumoto S, et al. Endovascular obliteration of bleeding duodenal varices in patients with liver cirrhosis. Eur Radiol. 2006;16:73–9. [DOI] [PubMed]
- 109.Graham AN, McAleese P, Moorehead RJ. Intraperitoneal rupture of ectopic varices—a rare complication of portal hypertension. HPB Surg. 1994;7:315–8. [DOI] [PMC free article] [PubMed]
- 110.Choi JW, Lee CH, Kim KA, Park CM, Kim JY. Ectopic varices in colonic stoma: MDCT findings. Korean J Radiol. 2006;7:297–9. [DOI] [PMC free article] [PubMed]
- 111.Kabeer MA, Jackson L, Widdison AL, Maskell G, Mathew J. Stomal varices: a rare cause of stomal hemorrhage. A report of three cases. Ostomy Wound Manage. 2007;53:20–2. [PubMed]
- 112.Wolfsen HC, Kozarek RA, Bredfeldt JE, Fenster LF, Brubacher LL. The role of endoscopic injection sclerotherapy in the management of bleeding peristomal varices. Gastrointest Endosc. 1990;36:472–4. [DOI] [PubMed]
- 113.Shibata D, Brophy DP, Gordon FD, Anastopoulos HT, Sentovich SM, Bleday R. Transjugular intrahepatic portosystemic shunt for treatment of bleeding ectopic varices with portal hypertension. Dis Colon Rectum. 1999;42:1581–5. [DOI] [PubMed]
- 114.Alkari B, Shaath NM, El-Dhuwaib Y, Aboutwerat A, Warnes TW, Chalmers N, et al. Transjugular intrahepatic porto-systemic shunt and variceal embolisation in the management of bleeding stomal varices. Int J Colorectal Dis. 2005;20:457–62. [DOI] [PubMed]
- 115.Wong RC, Berg CL. Portal hypertensive stomopathy: a newly described entity and its successful treatment by placement of a transjugular intrahepatic portosystemic shunt. Am J Gastroenterol. 1997;92:1056–7. [PubMed]
- 116.Malkan GH, Bhatia SJ, Bashir K, Khemani R, Abraham P, Gandhi MS, et al. Cholangiopathy associated with portal hypertension: diagnostic evaluation and clinical implications. Gastrointest Endosc. 1999;49:344–8. [DOI] [PubMed]
- 117.Chawla Y, Dilawari JB, Katariya S. Gallbladder varices in portal vein thrombosis. AJR Am J Roentgenol. 1994;162:643–5. [DOI] [PubMed]
- 118.Griniatsos J, Arbuckle J, Bhalla A, Karvounis E, Isla A. Bile duct varices in the absence of portal hypertension signs. Int Surg. 2003;88:76–9. [PubMed]
- 119.Chu EC, Chick W, Hillebrand DJ, Hu KQ. Fatal spontaneous gallbladder variceal bleeding in a patient with alcoholic cirrhosis. Dig Dis Sci. 2002;47:2682–5. [DOI] [PubMed]
- 120.Dilawari JB, Chawla YK. Pseudosclerosing cholangitis in extrahepatic portal venous obstruction. Gut. 1992;33:272–6. [DOI] [PMC free article] [PubMed]
- 121.Vitellas KM, Keogan MT, Freed KS, Enns RA, Spritzer CE, Baillie JM, et al. Radiologic manifestations of sclerosing cholangitis with emphasis on MR cholangiopancreatography. Radiographics. 2000;20:959–75. [DOI] [PubMed]
- 122.Smith AM, Walsh M, Henderson. M. Novel bile duct repair for bleeding biliary anastomotic varices: case report and literature review. J Gastrointest Surg. 2005;9:832–6. [DOI] [PubMed]
- 123.Johansen K, Bardin J, Orloff MJ. Massive bleeding from hemorrhoidal varices in portal hypertension. JAMA. 1980;244:2084–5. [DOI] [PubMed]
- 124.Mashiah A. Massive bleeding from hemorrhoidal varices in portal hypertension. JAMA. 1981;246:2323–4. [DOI] [PubMed]
- 125.Waxman JS, Tarkin N, Dave P, Waxman M. Fatal hemorrhage from rectal varices. Report of two cases. Dis Colon Rectum. 1984;27:749–50. [DOI] [PubMed]
- 126.Jacobs DM, Bubrick MP, Onstad GR, Hitchcock CR. The relationship of hemorrhoids to portal hypertension. Dis Colon Rectum. 1980;23:567–9. [DOI] [PubMed]
- 127.Weinshel E, Chen W, Falkenstein DB, Kessler R, Raicht RF. Hemorrhoids or rectal varices: defining the cause of massive rectal hemorrhage in patients with portal hypertension. Gastroenterology. 1986;90:744–7. [DOI] [PubMed]
- 128.Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343–9. [DOI] [PubMed]
- 129.Sarin SK, Kumar A. Gastric varices: profile, classification, and management. Am J Gastroenterol. 1989;84:1244–9. [PubMed]
- 130.Sarin SK, Primignani M, Agarwal SR. Gastric varices. In: de Franchis R, editor. Portal hypertension. Proceedings of the third Baveno International Consensus Workshop on Definitions, Methodology and Therapeutic Strategies. London: Blackwell Science; 2001. p. 76–96.
- 131.Sarin SK, Jain AK, Lamba GS, Gupta R, Chowdhary A. Isolated gastric varices: prevalence, clinical relevance and natural history. Dig Surg. 2003;20:42–7. [DOI] [PubMed]