Abstract
BACKGROUND
Reduced nocturnal blood pressure (BP) dipping is more prevalent among blacks living in the United States than whites and is associated with increased target organ damage and cardiovascular risk. The primary aim of this study was to determine whether socioeconomic and psychosocial factors help to explain racial differences in dipping. In order to address the limited reproducibility of dipping measures, we investigated this question in a sample of participants who underwent multiple ambulatory BP monitoring (ABPM) sessions.
METHODS
The study sample included 171 black and white normotensive and mildly hypertensive participants who underwent three ABPM sessions, each 1 month apart, and completed a battery of questionnaires to assess socioeconomic and psychosocial factors.
RESULTS
As expected, blacks showed less dipping than whites, after adjusting for age, sex, body mass index (BMI), and mean 24 h BP level (mean difference = 3.3%, P= 0.002). Dipping was related to several of the socioeconomic and psychosocial factors examined, with higher education and income, being married, and higher perceived social support, each associated with a larger dipping percentage. Of these, marital status and education were independently associated with dipping and together accounted for 36% of the effect of race on dipping.
CONCLUSIONS
We identified a number of socioeconomic and psychosocial correlates of BP dipping and found that reduced dipping among blacks vs. whites is partially explained by marital status (being unmarried) and lower education among blacks. We also present results suggesting that repeated ABPM may facilitate the detection of associations between dipping and other variables.
Blacks living in the United States suffer from disproportionately high rates of hypertension compared with whites.1,2 In addition to significant differences in casual daytime blood pressure (BP), studies using ambulatory BP monitoring (ABPM) to examine diurnal BP patterns have found that blacks also have higher nocturnal BP than whites and show smaller declines in nocturnal BP relative to daytime BP.3 The nocturnal decline represents the normal diurnal pattern of BP,4 and disruption of this pattern appears to be an important prognostic factor. Individuals whose nocturnal BP declines <10% of their mean daytime BP are typically classified as nondippers5 and have greater target organ damage and increased risk of cardiovascular disease morbidity and mortality.6–9 A number of studies have demonstrated that the reproducibility of dipping status is poor,10 which may reduce the likelihood of detecting associations with other measures. The use of >1 ABPM may facilitate the identification of predictors or outcomes of dipping but has rarely been done.
Mechanisms underlying the observed race differences in BP dipping are not well understood. The finding that African blacks show greater dipping than US blacks—to a level similar to that observed among whites11—suggests that environmental and psychosocial factors may play an important role. A number of such factors have been associated with the amount of BP dipping, including socioeconomic status,12 stressful life events,13 anger and hostility,14 perceived racism,15 marital status,16 and aspects of social integration and social support.13,17 Some of these factors have been found to partially mediate black–white differences in dipping, but to our knowledge, the independent contributions of each have not yet been examined using >1 ABPM recording.
The purpose of this study was to determine the extent to which socioeconomic and psychosocial factors help to explain race differences in BP dipping in a sample of normotensive and mildly hypertensive adults who completed three ABPM sessions.
METHODS
Study population
The present study was conducted as part of a larger investigation of psychological and behavioral mechanisms of white coat hypertension. The sample includes normotensive and mildly hypertensive participants who were recruited between 1998 and 2003 using advertisements and physician referrals at the Weill Cornell Hypertension Center of New York Presbyterian Hospital and Mount Sinai Medical Center in New York City. The study was approved by the hospitals’ Institutional Review Boards. The eligibility criteria were age 18–80 years; English-speaking; no previous cardiovascular event, diabetes, or other serious health problems; screening BP below 160/100mmHg; and participants willing, with physician’s permission, to stop antihypertensive medication for a 10-week period (including the 2 weeks prior to enrollment). A total of 226 black and white participants who enrolled in the study and completed the first ABPM session were eligible for inclusion in the present set of analyses. Of these, 171 participants (76%) completed all three ABPM sessions and formed the sample for the primary analysis.
Procedure
Participants attended an initial recruitment visit during which eligibility was determined, informed consent was obtained, and height and weight were measured for calculation of body mass index (BMI). Following the recruitment visit, participants completed three assessments, each of which involved two visits on consecutive days. The assessments were scheduled at 1-month intervals; the median time between the first and second assessments was 34 days (25th, 75th percentiles: 28, 41) and between the second and third assessments was 30 days (25th, 75th percentiles: 26, 35).
On the first day of each assessment, participants were instrumented with an ABPM arm cuff on the nondominant arm and were instructed to wear the monitor for the remainder of the day, during sleep, and throughout the following day. Participants were given take-home questionnaire packets and diaries in which to record sleep/wake times. The second assessment day involved a clinic visit during which a physician obtained BP measurements using the opposite arm. Participants left the clinic still wearing the ABPM, which they removed at bedtime and returned via prepaid mailer.
Measures
Ambulatory BP (ABP)
ABPM was performed using the Spacelabs 90207 ABP monitor (Spacelabs Healthcare, Redmond, WA). Validation procedures followed the British Hypertension Society guidelines.18 The ABPM took measurements every 30min throughout the monitoring period for three-quarters of subjects, and every 15min during the day (6 am–10 pm) and 30min at night (10 pm–6 am) for the remaining subjects. ABP data were edited to eliminate out-of-range readings (systolic BP (SBP) <70mmHg or >220mmHg, diastolic BP <40mmHg or >150mmHg) and errors due to motion artifacts or equipment problems. The average daytime and nocturnal ABP for each monitoring period was computed from the actual sleep/ wake times. Conservative time periods were used to compute daytime (10 am–9 pm) and sleep (1 am–5:30 pm) ABP for 6% of ABP recordings for which participants did not report sleep/wake times. The mean number of awake and sleep ABP measurements taken cumulatively over the three sessions were 107.3 ± 23.3 and 42.1 ± 8.7, respectively.
Self-report measures
The take-home packets included questionnaires to obtain the following demographic and socioeconomic data: age, sex, race, years of education, annual gross household income, marital status, and parental status (having biological or adopted children). Participants also completed a battery of psychosocial measures, each of which has been widely used and had good internal reliability in our sample: trait anxiety was assessed using the 20-item subscale (α = 0.90) of the State-Trait Anxiety Inventory;19 trait anger was assessed using the 10-item subscale (α = 0.86) of the State-Trait Anger Expression Inventory;20 hostility was assessed using the 50-item (α = 0.90) Cook–Medley Hostility Scale;21 neuroticism was assessed using the 12-item subscale (α = 0.86) of the NEO Five-Factor Inventory;22 perceived social support was assessed using the 40-item (α = 0.93) Interpersonal Support Evaluation List;23 and life stress was assessed using the Life Experiences Survey,24 a 60-item checklist of life events.
Statistical analysis
The mean awake and sleep BPs were computed by taking the average of all awake and sleep readings, respectively, across the three ABPM sessions. The mean BPs were quite stable (see Table 1), and results of repeated measures analyses of variance indicated that any differences across the sessions were not statistically significant. The primary outcome measure was the average SBP dipping, calculated as 1 minus the ratio of the mean sleep SBP divided by the mean awake SBP, expressed as a percentage. For descriptive purposes, we defined nondippers as participants whose average dipping percentage was <10%, the standard cutoff.5
Table 1.
Reproducibility of ABP measures
| Awake SBP | Sleep SBP | |
|---|---|---|
| Session 1, mean ± s.d. | 134 ± 14 | 119 ± 15 |
| Session 2, mean ± s.d. | 134 ± 14 | 119 ± 14 |
| Session 3, mean ± s.d. | 134 ± 14 | 120 ± 14 |
| r, Sessions 1/2 | 0.85 | 0.72 |
| r, Sessions 2/3 | 0.80 | 0.76 |
| r, Sessions 1/3 | 0.85 | 0.76 |
r = Pearson correlation coefficient; all r s significant at P < 0.001.
ABP, ambulatory blood pressure; SBP, systolic blood pressure.
The baseline characteristics of black and white participants were compared using t-tests for continuous variables and χ2 tests for categorical variables. Multivariable regression was used to examine the effect of race and the set of socioeconomic and psychosocial factors on the mean dipping percentage after adjusting for age, sex, BMI, and mean 24-h SBP. We controlled for 24-h SBP rather than awake or sleep SBP given that the latter two are used to define dipping. Two-way interaction terms of interest were entered on the final step of the regression equation. Because white participants were significantly more likely than black participants to be recruited via physician referrals (49% vs. 27%, P = 0.02), and therefore were more likely to be hypertensive, we also examined the interaction between race and recruitment method.
A bootstrap strategy25,26 was used to test whether socioeconomic and psychosocial factors mediated the association between race and dipping. Specifically, 10,000 random samples were drawn, with replacement, from the analysis sample, each with the same number of subjects as the analysis sample. For each sample, two regression equations were estimated, before and after inclusion of the potential mediator, and it was determined whether the race coefficient was attenuated in the model that included the mediator. If attenuation occurred in >95% of the bootstrap samples, we rejected the null hypothesis of “no mediation” at the α = 0.05 level. We also calculated the percent reduction in the race coefficient after including the identified mediators in the regression equation. All analyses were performed using SPSS v.16 (SPSS, Chicago, IL) and SAS v.9.13 (SAS Institute, Cary, NC).
RESULTS
Sample characteristics
Sample characteristics are presented in Table 2. Blacks were significantly younger (P < 0.001) and had higher BMI (P = 0.001), on average, than whites. Blacks were also less likely than whites to be married (P = 0.04) and reported less education (P < 0.001), lower income (P < 0.001), more life events (P = 0.008), and greater hostility (P = 0.001). Regarding BP variables, blacks showed a smaller dipping percentage compared with whites (P = 0.004), as expected. However, whites had somewhat higher awake SBP (P = 0.08) and were more likely to have been diagnosed as hypertensive (P = 0.01) than blacks, likely due to the difference in recruitment method described above.
Table 2.
Participant characteristics
| Variable | Range | Total sample (N = 171) | Black (N = 41) | White (N =130) | P value |
|---|---|---|---|---|---|
| Age | 19.0–80.5 | 52.9 ± 14.4 | 44.7 ± 11.7 | 55.5 ± 14.2 | <0.001 |
| Female sex | 0–1 | 55.6% (95) | 51.2% (21) | 56.9% (74) | 0.52 |
| BMI | 17.8–47.6 | 26.7 ± 5.8 | 29.9 ± 6.6 | 25.7 ± 5.3 | 0.001 |
| Hypertensivea | 0–1 | 50.6% (84) | 32.4% (12) | 55.8% (72) | 0.01 |
| Anti-HTN drugs | 0–1 | 11.1% (19) | 9.8% (4) | 11.5% (15) | 0.75 |
| 24-h SBP | 101–177 | 129 ± 13 | 127 ± 13 | 130 ± 12 | 0.28 |
| Awake SBP | 107–178 | 134 ± 13 | 131 ± 13 | 135 ± 13 | 0.08 |
| Sleep SBP | 90–170 | 119 ± 13 | 119 ± 14 | 119 ± 12 | 0.95 |
| Dipping percent | −3.6–26.0 | 11.1 ± 5.4 | 9.1 ± 4.9 | 11.8 ± 5.4 | 0.004 |
| Nondipper status | 0–1 | 42.7% (73) | 53.7% (22) | 39.2% (51) | 0.10 |
| Education, years | 6–18 | 15.4 ± 2.4 | 14.0 ± 2.8 | 15.9 ± 2.2 | <0.001 |
| Income, $ | 5,000–150,000 | 55,818 ± 47,116 | 29,595 ± 22,403 | 63,770 ± 49,753 | <0.001 |
| Married | 0–1 | 32.7% (56) | 19.5% (8) | 36.9% (48) | 0.04 |
| Parentb | 0–1 | 48.3% (71) | 63.0% (17) | 45.0% (54) | 0.09 |
| Social support | 4–40 | 31.0 ± 8.0 | 30.2 ± 9.0 | 31.2 ± 7.7 | 0.52 |
| Life events | 0–59 | 11.8 ± 13.9 | 18.4 ± 17.6 | 9.7 ± 11.9 | 0.008 |
| Hostility | 2–35 | 16.5 ± 7.6 | 20.3 ± 6.6 | 15.3 ± 7.5 | 0.001 |
| Trait anxiety | 0–41 | 18.3 ± 9.4 | 18.3 ± 8.2 | 18.3 ± 9.8 | 0.98 |
| Trait anger | 0–19 | 6.2 ± 4.5 | 6.7 ± 5.4 | 6.0 ± 4.1 | 0.44 |
| Neuroticism | 0–44 | 19.5 ± 8.2 | 18.1 ± 6.3 | 19.9 ± 8.7 | 0.26 |
Mean ± s.d. shown for continuous variables. % (N) shown for dichotomous variables.
BMI, body mass index; HTN, hypertension; SBP, systolic blood pressure.
“Hypertensive” indicates subjects with session 1 clinic BP ≥140/90mmHg (missing for five subjects) and/or taking anti-HTN drugs prior to study enrollment.
“Parent” indicates subjects with ≥1 child (missing for 24 subjects).
The study sample of 171 was also compared with the 55 participants (24%) who were excluded due to missing the second and/or third ABPM sessions. Included and excluded participants did not differ significantly with regard to sex, hypertension status, use of antihypertensive medications, session 1 awake BP, sleep BP, dipping status or percentage, or psychosocial factors. Those excluded were, however, more likely to be black (P < 0.001), younger (P = 0.009), report lower education (P = 0.005) and income (P = 0.006), and have a higher mean BMI (P = 0.002).
Reproducibility of BP measures
Correlations among the continuous dipping measures across the three ABPM sessions ranged from 0.42 to 0.48 (Ps < 0.001); these are similar to previous reports,27,28 but are likely attenuated due to the sampling variability that results from having a limited number of sleep readings each night.29 Results of a repeated measures analysis of variance indicated that the amount of dipping did not change significantly across the sessions. As expected, reproducibility of the dichotomous dipping measure across sessions was more limited (kappas from 0.26 to 0.42, Ps < 0.01).
Race differences in BP dipping
A regression equation predicting dipping was estimated with age, sex, BMI, and mean 24-h SBP entered as covariates on the first step and race entered on the second step. Results were consistent with the unadjusted analysis and showed that race was a significant predictor (P = 0.002), with SBP dipping 3.3% more in whites than in blacks. None of the covariates were significantly associated with dipping. Given the differential exclusion of blacks vs. whites from the sample (due to missing the second and/or third ABPM sessions), we repeated this analysis using dipping measures from the first session only for all 226 participants. Race remained a significant predictor of dipping (P = 0.03).
We also examined the interaction between race and recruitment method. This interaction was not statistically significant (P = 0.24), suggesting that despite whites having been more likely than blacks to be recruited via physician referrals vs. advertisements, this difference did not substantially affect the observed race-dipping relationship.
Associations of socioeconomic and psychosocial factors with race and BP dipping
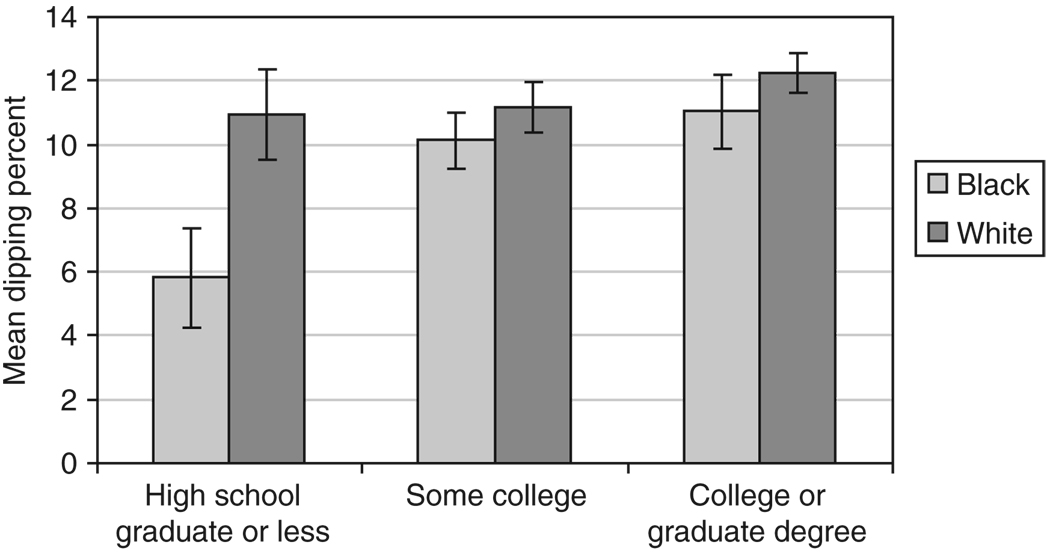
We next examined associations between dipping and each of the socioeconomic and psychosocial variables. Greater dipping was associated with more education (r = 0.26, P = 0.001), higher income (r = 0.28, P < 0.001), being married (t = −3.95, P < 0.001), and was marginally associated with higher perceived social support (r = 0.16, P = 0.06). In order to identify factors that were independently associated with dipping, these variables were entered on the second step of a regression equation, following the entry of race and the set of covariates. Results indicated that more education and being married were each associated with greater dipping. To rule out the possibility that multicollinearity among the predictors influenced these results, we repeated the analysis using stepwise entry of the predictors. Consistent with the previous analysis, only education (P = 0.03) and marital status (P < 0.001) entered the equation. Interactions of race with marital status and education were not statistically significant, although Figure 1 shows some indication of greater race differences in dipping at low education levels.
Figure 1.
Mean blood pressure dipping percentage by race and education level. Standard error bars are shown for each mean.
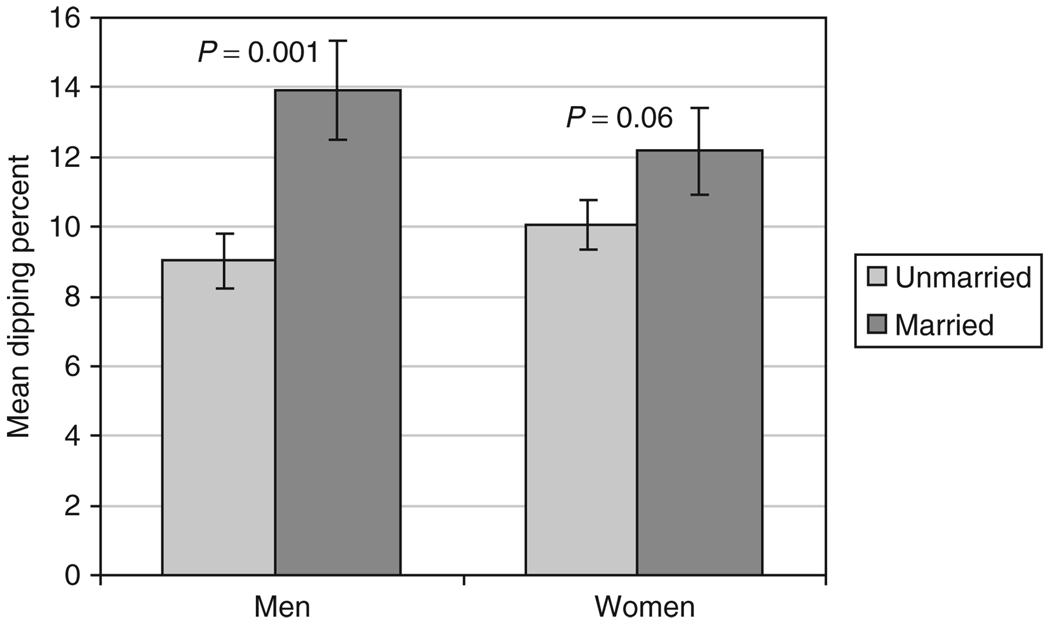
Given previous literature demonstrating greater health benefits of marriage for men than women,30 we also tested whether the effect of marital status on dipping differed by sex. Results indicated that a marginally significant sex by marital status interaction existed (P = 0.11), so we next examined the effect of marital status on dipping in separate regression equations for men and women. Being married was more strongly associated with greater dipping in men (P = 0.001) than in women (P = 0.06). A plot of this interaction is shown in Figure 2.
Figure 2.
Mean blood pressure dipping percentage by marital status and sex. The sex × marital status interaction was marginally significant (P = 0.11). The figure shows the mean dipping percentage for each group, adjusted for age, body mass index, mean 24-h systolic blood pressure, race, and education. P values in the figure represent the significance of the effect of marital status in men and women separately.
Do socioeconomic or psychosocial factors mediate the race-dipping association?
We next examined whether education and marital status, which were each independently associated with dipping, mediated the race-dipping association. The estimated effect of race decreased by 21% when education was added to the equation that also controlled for age, sex, BMI, and 24-h SBP. The mediation hypothesis was supported by the bootstrap analysis at the P = 0.02 level of significance. Similarly, the estimated effect of race decreased by 14% when marital status was added to the equation that also controlled for the covariates. The bootstrap analysis supported this mediation hypothesis at the P = 0.04 level of significance. Together, education and marital status accounted for 36% of the effect of race on dipping. When the mediators and covariates were all controlled in the regression equation, the statistical significance of the race coefficient was reduced from P = 0.002 to P = 0.05.
Analysis of first ABPM session
A unique element of this study was the use of three ABPM sessions, which we believe is important given that the limited reliability of BP dipping when based on a single 24-h recording is likely to reduce the likelihood of detecting associations with other variables. We conducted additional analyses to evaluate whether the results presented above based on all three sessions were comparable to those obtained when analyzing only the first session in the same sample of 171 participants. Although the pattern of results was similar, the association between race and dipping became somewhat weaker; the statistical significance of the association was reduced from P = 0.002 to P = 0.03. Thus, it appears that the use of a single ABPM session does indeed limit the ability to detect associations between dipping and other variables that become evident when repeated monitoring is conducted.
DISCUSSION
As previously reported, we found that blacks showed significantly less BP dipping than did whites and were more likely to be classified as nondippers. Examination of a group of socioeconomic and psychosocial factors revealed that being unmarried and having less education were independent predictors of less dipping and together accounted for 36% of the effect of race on dipping. Marriage and higher socioeconomic status are associated with positive health outcomes,31,32 and these effects are thought to result from both a better health behavior profile and the buffering of psychological and physiological effects of stress, which could involve lower exposure to stress as well as the availability of greater resources with which to cope with stress.30,33 We also found that being married was more strongly associated with dipping among men than women, which is consistent with previous research regarding sex differences in the beneficial health effects of marriage.30
The use of three ABPM sessions is an important and unique feature of this study. Our results suggest that improving the reliability of diurnal BP changes through repeated monitoring facilitates the detection of associations between dipping and other factors. Another strength of the present study is the simultaneous examination of a range of socioeconomic and psychosocial factors, which allowed us to assess the independent contribution of several factors that have previously been examined in isolation. This may help to explain discrepancies with previous studies. For example, the studies that have reported associations between perceived social support and dipping13,17 did not assess marital status, and it is unknown whether the effect of perceived support would have been reduced when both were included in the analyses for those studies. In the present study, the association between perceived support and dipping became stronger, although not statistically significant, when marital status was excluded from the analysis, suggesting that this may be a plausible explanation for the difference in findings.
Notwithstanding the race differences in ABPM completion—which were found to have little effect on our results—the generalizability of these findings is enhanced by the inclusion of both normotensives and hypertensives and participants of a wide age range and varied socioeconomic profile. Ituarte et al.13 examined a comparable set of factors and found that being a parent was the only independent predictor of less dipping. However, all participants were married or living with a partner, were high school graduates, employed full-time, nonsmokers, normotensive, and were similar with regard to socioeconomic status. Therefore, the authors were not able to evaluate the role of marital status and were underpowered to evaluate the role of education, the two socioeconomic factors that were found to be most important in our study.
Several limitations of the study must be noted when interpreting these findings. First, the number of blacks in the sample was relatively small. In addition, blacks were less likely to complete the second and/or third ABPM sessions than whites, and therefore a greater proportion of blacks were excluded from the analysis sample. Also, blacks were less likely to have been recruited for the study via physician referrals than whites and were less likely to be hypertensive. However, we have shown that these factors did not substantially influence the results. Still, efforts to reduce such enrollment biases will enhance the generalizability of findings of future studies in this area.
The lack of information regarding baseline medical status is an important limitation. Although participants reported no major health problems, we were unable to evaluate the role of possible confounds (e.g., creatinine level, glomerular filtration rate) using objective data. Similarly, lack of data regarding lifestyle factors is a limitation. Although recent studies suggest that race differences in dipping are not explained by dietary factors34 or sleep quality,35 other factors such as smoking and alcohol use may be important. We also did not assess marital quality or exposure to racism, which have both been related to dipping in previous studies.15,16
In conclusion, the present study contributes to the growing body of research focused on understanding race differences in BP dipping. Our findings suggest that marital status and socioeconomic status may help to explain the disparity between blacks and whites in BP dipping, an important predictor of cardiovascular disease outcomes. Additional research is needed to further explore the pathways between race and dipping using longitudinal designs that include a comprehensive assessment of possible mediators to determine the relative importance of the various factors that have been shown to influence dipping.
Acknowledgments
Preparation of this article was supported in part by the National Heart, Lung, and Blood Institute, National Institutes of Health, grants HL47540 and HL76857, T.G.P., principal investigator, and HL86734, T.M.S., principal investigator. The sponsors had no role in the study design, in the collection, analysis, or interpretation of the data, in the writing of the present report, or in the decision to submit the manuscript for publication.
Footnotes
Disclosure: The authors declared no conflict of interest.
References
- 1.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165:2098–2104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 2.Wang X, Poole JC, Treiber FA, Harshfield GA, Hanevold CD, Snieder H. Ethnic and gender differences in ambulatory blood pressure trajectories: results from a 15-year longitudinal study in youth and young adults. Circulation. 2006;114:2780–2787. doi: 10.1161/CIRCULATIONAHA.106.643940. [DOI] [PubMed] [Google Scholar]
- 3.Profant J, Dimsdale JE. Race and diurnal blood pressure patterns. A review and meta-analysis. Hypertension. 1999;33:1099–1104. doi: 10.1161/01.hyp.33.5.1099. [DOI] [PubMed] [Google Scholar]
- 4.Pickering TG, Harshfield GA, Kleinert HD, Blank S, Laragh JH. Blood pressure during normal daily activities, sleep, and exercise. Comparison of values in normal and hypertensive subjects. JAMA. 1982;247:992–996. [PubMed] [Google Scholar]
- 5.Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. N Engl JMed. 2006;354:2368–2374. doi: 10.1056/NEJMra060433. [DOI] [PubMed] [Google Scholar]
- 6.Ingelsson E, Björklund-Bodegård K, Lind L, Arnlöv J, Sundström J. Diurnal blood pressure pattern and risk of congestive heart failure. JAMA. 2006;295:2859–2866. doi: 10.1001/jama.295.24.2859. [DOI] [PubMed] [Google Scholar]
- 7.Cuspidi C, Macca G, Sampieri L, Fusi V, Severgnini B, Michev I, Salerno M, Magrini F, Zanchetti A. Target organ damage and non-dipping pattern defined by two sessions of ambulatory blood pressure monitoring in recently diagnosed essential hypertensive patients. J Hypertens. 2001;19:1539–1545. doi: 10.1097/00004872-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Ben-Dov IZ, Kark JD, Ben-Ishay D, Mekler J, Ben-Arie L, Bursztyn M. Predictors of all-cause mortality in clinical ambulatory monitoring: unique aspects of blood pressure during sleep. Hypertension. 2007;49:1235–1241. doi: 10.1161/HYPERTENSIONAHA.107.087262. [DOI] [PubMed] [Google Scholar]
- 9.Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, Matsubara M, Hashimoto J, Hoshi H, Araki T, Tsuji I, Satoh H, Hisamichi S, Imai Y. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002;20:2183–2189. doi: 10.1097/00004872-200211000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Parati G, Staessen JA. Day-night blood pressure variations: mechanisms, reproducibility and clinical relevance. J Hypertens. 2007;25:2377–2380. doi: 10.1097/HJH.0b013e3282f2d116. [DOI] [PubMed] [Google Scholar]
- 11.Fumo MT, Teeger S, Lang RM, Bednarz J, Sareli P, Murphy MB. Diurnal blood pressure variation and cardiac mass in American blacks and whites and South African blacks. Am J Hypertens. 1992;5:111–116. doi: 10.1093/ajh/5.3.111. [DOI] [PubMed] [Google Scholar]
- 12.Stepnowsky CJ, Jr, Nelesen RA, DeJardin D, Dimsdale JE. Socioeconomic status is associated with nocturnal blood pressure dipping. Psychosom Med. 2004;66:651–655. doi: 10.1097/01.psy.0000138124.58216.6c. [DOI] [PubMed] [Google Scholar]
- 13.Ituarte PH, Kamarck TW, Thompson HS, Bacanu S. Psychosocial mediators of racial differences in nighttime blood pressure dipping among normotensive adults. Health Psychol. 1999;18:393–402. doi: 10.1037//0278-6133.18.4.393. [DOI] [PubMed] [Google Scholar]
- 14.Thomas KS, Nelesen RA, Dimsdale JE. Relationships between hostility, anger expression, and blood pressure dipping in an ethnically diverse sample. Psychosom Med. 2004;66:298–304. doi: 10.1097/01.psy.0000126196.82317.9d. [DOI] [PubMed] [Google Scholar]
- 15.Brondolo E, Libby DJ, Denton EG, Thompson S, Beatty DL, Schwartz J, Sweeney M, Tobin JN, Cassells A, Pickering TG, Gerin W. Racism and ambulatory blood pressure in a community sample. Psychosom Med. 2008;70:49–56. doi: 10.1097/PSY.0b013e31815ff3bd. [DOI] [PubMed] [Google Scholar]
- 16.Holt-Lunstad J, Birmingham W, Jones BQ. Is there something unique about marriage? The relative impact of marital status, relationship quality, and network social support on ambulatory blood pressure and mental health. Ann Behav Med. 2008;35:239–244. doi: 10.1007/s12160-008-9018-y. [DOI] [PubMed] [Google Scholar]
- 17.Rodriguez CJ, Burg MM, Meng J, Pickering TG, Jin Z, Sacco RL, Boden-Albala B, Homma S, Di Tullio MR. Effect of social support on nocturnal blood pressure dipping. Psychosom Med. 2008;70:7–12. doi: 10.1097/PSY.0b013e31815aab4e. [DOI] [PubMed] [Google Scholar]
- 18.O’Brien E, Petrie J, Littler W, de Swiet M, Padfield PL, Altman DG, Bland M, Coats A, Atkins N. An outline of the revised British Hypertension Society protocol for the evaluation of blood pressure measuring devices. J Hypertens. 1993;11:677–679. doi: 10.1097/00004872-199306000-00013. [DOI] [PubMed] [Google Scholar]
- 19.Spielberger CD. Manual for the State-Trait Anxiety Inventory (STAI) Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 20.Spielberger CD, Jacobs GA, Russell S, Crane RS. Assessment of anger:the State-Trait Anger Scale. In: Butcher JN, Spielberger CD, editors. Advances in Personality Assessment. Vol 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1983. pp. 159–187. [Google Scholar]
- 21.Cook W, Medley D. Proposed hostility and pharisaic-virtue scales for the MMPI. J Appl Psychol. 1954;38:414–418. [Google Scholar]
- 22.Costa PT, McCrae RR. Revised NEO Personality Inventory and NEO Five-Factor Inventory Professional Manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- 23.Cohen S, Mermelstein R, Kamarck T, Hoberman H. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors. Social Support: Theory, Research and Applications. The Hague, Netherlands: Martinus Nijhoff; 1985. pp. 73–94. [Google Scholar]
- 24.Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: development of the Life Experiences Survey. J Consult Clin Psychol. 1978;46:932–946. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- 25.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 27.Dimsdale JE, von Känel R, Profant J, Nelesen R, Ancoli-Israel S, Ziegler M. Reliability of nocturnal blood pressure dipping. Blood Press Monit. 2000;5:217–221. doi: 10.1097/00126097-200008000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Ben-Dov IZ, Ben-Arieh L, Mekler J, Bursztyn M. Blood pressure dipping is reproducible in clinical practice. Blood Press Monit. 2005;10:79–84. doi: 10.1097/00126097-200504000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Schwartz J, Grossman S, Warren K, Pickering TG. How stable is the awake-sleep difference in mean ambulatory blood pressures? Paper presented at American Society for Hypertension. 1997 [Google Scholar]
- 30.Kiecolt-Glaser JK, Newton TL. Marriage and health: his and hers. Psychol Bull. 2001;127:472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- 31.Johnson NJ, Backlund E, Sorlie PD, Loveless CA. Marital status and mortality: the National Longitudinal Mortality Study. Ann Epidemiol. 2000;10:224–238. doi: 10.1016/s1047-2797(99)00052-6. [DOI] [PubMed] [Google Scholar]
- 32.Kaplan GA, Keil JE. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88(4 Pt 1):1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 33.Ross CE, Wu C-L. The links between education and health. Am Sociol Rev. 1995;60:719–745. [Google Scholar]
- 34.Jehn ML, Brotman DJ, Appel LJ. Racial differences in diurnal blood pressure and heart rate patterns: results from the Dietary Approaches to Stop Hypertension (DASH) trial. Arch Intern Med. 2008;168:996–1002. doi: 10.1001/archinte.168.9.996. [DOI] [PubMed] [Google Scholar]
- 35.Hughes JW, Kobayashi I, Deichert NT. Ethnic differences in sleep quality accompany ethnic differences in night-time blood pressure dipping. Am J Hypertens. 2007;20:1104–1110. doi: 10.1016/j.amjhyper.2007.05.005. [DOI] [PubMed] [Google Scholar]