Abstract
What brain reward systems mediate motivational ‘wanting’ and hedonic ‘liking’ for food rewards? And what roles do those systems play in eating disorders? This article surveys recent findings regarding brain mechanisms of hedonic ‘liking’, such as the existence of cubic-millimeter hedonic hotspots in nucleus accumbens and ventral pallidum for opioid amplification of sensory pleasure. It also considers brain ‘wanting’ or incentive salience systems important to appetite, such as mesolimbic dopamine systems and opioid motivation circuits that extend beyond the hedonic hotspots. Finally, it considers some potential ways in which ‘wanting’ and ‘liking’ might relate to eating disorders.
Keywords: Reward, Food, Ingestive behavior, Pleasure, Anorexia, Bulimia, Eating disorders, Nucleus accumbens, Ventral pallidum, Brainstem, Parabrachial nucleus, Dopamine, Opioid, Addiction
1. Introduction
Obesity, bulimia, anorexia, and related eating disorders have become more prominent in recent decades, leading to increased concern about how to deal with them. Can improved knowledge about brain reward systems help guide thinking about eating disorders and devising better treatments?
Basic brain systems for food reward carry potential implications for understanding normal eating and eating disorders. It is important to note first that brain reward systems are active participants, not just passive conduits, in the act of eating. The pleasure of sweetness arises within the brain, generated actively by neural systems that paint the pleasure onto the sensation to generate a ‘liking’ reaction —as a sort of ‘pleasure gloss’. We may be used to thinking of sweet tastes as innately pleasant, but their pleasure is not contained in the intrinsic detail of their sensation but rather in their evolved ability to act as keys that unlock activation of brain ‘liking’ systems [1–3]. This is evident by considering that if the ability to unlock hedonic brain systems is lost, a sweet taste loses its pleasure while remaining sweet as ever. For example, a particular sweet taste can become perceived as disgusting rather than nice when an individual learns a taste aversion for it after pairing with visceral illness [3–6]. Conversely, bitterness activates brain systems of aversion and disgust to be innately aversive, but tastes of cranberries, coffee, beer, gin, or opiates can become pleasant for many individuals when experience makes them into keys for hedonic brain systems.
Understanding brain substrates of pleasure and aversion may open an avenue to understanding the impact of food rewards on eating behavior. Pleasure must be translated into motivation or ‘wanting’ in order for food reward to influence actual eating behavior, as the motivation to eat involves brain mechanisms of its own.
What brain systems paint a pleasure gloss onto sensation? And what brain systems convert pleasure into a desire to eat? Answers to these questions will be described that have come primarily from animal experiments involving brain and pharmacological manipulation, supported also by human neuroimaging experiments and related studies of eating.
2. Understanding brain reward systems for food ‘wanting’ versus ‘liking’
To find brain mechanisms for ‘wanting’ and ‘liking’ first requires that those psychological components of reward be recognizable in measurable ways. This section turns to some issues regarding the brain systems that help generate ‘liking’ and ‘wanting’ for food rewards. ‘Liking’ is essentially a hedonic reaction to the pleasure of a reward. It is nearly what most people mean when they say reward. ‘Wanting’ on the other hand is not pleasure, even though also a component of reward, and may be less intuitive.
2.1. What is ‘wanting’ if it's not ‘liking’
‘Wanting’ is a shorthand term my colleagues and I use for the psychological process of incentive salience [7–10]. Incentive salience is attributed to rewards and their predictive cues, which helps determine their motivational value. Those cues then become potent triggers of ‘wanting’. In this way, cravings can be triggered by simply imagining the sight, smell and taste of palatable foods [11].
‘Wanting’ is psychologically and neurally distinguishable from ‘liking’, even if they often happen together. According to the incentive salience concept, ‘wanting’ is a mesolimbic-generated process that can tag certain stimulus representations in the brain that have Pavlovian associations with reward. When incentive salience is attributed to a reward stimulus representation, it makes that stimulus attractive, attention grabbing, and that stimulus and its associated reward suddenly become enhanced motivational targets. Because incentive salience is often triggered by Pavlovian conditioned stimuli or reward cues, it often manifests as cue-triggered ‘wanting’ for reward. When attributed to a specific stimulus, incentive salience may make an autoshaped cue light appear food-like to the autoshaped pigeon or rat that perceives it, causing the animal to try to eat the cue. In autoshaping, animals sometimes direct behavioral pursuit and consummatory responses towards the Pavlovian cue, literally trying to eat the conditioned stimulus if it is a cue for food reward [12–15].When attributed to the smell emanating from cooking, incentive salience can rivet a person's attention and trigger sudden thoughts of eating—and perhaps it can do so under some circumstances even if the person merely vividly imagines the delicious food.
But ‘wanting’ is not ‘liking’, and both together are necessary for normal reward. ‘Wanting’ without ‘liking’ is merely a sham or partial reward, without sensory pleasure in any sense. However, ‘wanting’ is still an important component of normal reward, especially when combined with ‘liking’. Reward in the full sense cannot happen without incentive salience, even if hedonic ‘liking’ is present. Hedonic ‘liking’ by itself is simply a triggered affective state—there need be no object of desire or incentive target, and no motivation for further reward. It is the process of incentive salience attribution that makes a specific associated stimulus or action the object of desire, that tags a specific behavior as the rewarded response, and that allows normal pleasure to spur desire for more. ‘Liking’ and ‘wanting’ are needed together for full reward. Fortunately, both usually happen together in human life.
2.2. Cognitive goals and ordinary wanting
Before leaving ‘wanting’ it is useful to note how the incentive salience meaning of the word ‘wanting’ (with quotation marks) as used above differs from what most people mean by the ordinary sense of the word wanting (without quotation marks). A subjective feeling of desire meant by the ordinary word wanting implies something both cognitive (involving an explicit goal) and conscious (involving a subjective feeling). When you say you want something, you usually have in mind a cognitive expectation or idea of the something-you-want: a declarative representation of your goal. Your representation is based usually on your experience with that thing in the past. Or, if you have never before experienced that thing, then, the representation is based on your imagination of what it would be like to experience. In other words, in these cases, you know or imagine cognitively what it is you want, you expect to like it, and you may even have some idea of how to get it. These are all very cognitive form of wanting, involving declarative memories of the valued goal, explicit predictions for the potential future based on those memories, and cognitive understanding of causal relationships that exist between your potential actions and future attainment of your goal.
By contrast, none of this cognition need be part of incentive salience ‘wants’ discussed above. Evidence indicates that incentive salience attributions do not need to be conscious and are mediated by relatively simple brain mechanisms [16,17]. Indeed under special circumstances like subliminal induction procedures, normal people can be made to ‘want’ to drink more of a sweet beverage than they otherwise would without becoming aware of any change in feeling or that anything has happened at all [18] (Fig. 1).
Fig.1.
Unconscious induction of ‘liking’ and ‘wanting’ to drink a sweet beverage. Thirsty people were shown subliminally fast visual presentations of either happy facial expressions or angry facial expressions that were too brief to be consciously perceived but should still have activated brain mesolimbic circuits. Then they completed a cognitive task of identifying gender of a consciously seen face (to wipe away any conscious affect engendered by the faces) before being asked to rate their own hedonic mood or to evaluate a sweet citric fruit-flavored beverage, which they could pour and ingest as they wished. No changes in hedonic ratings of subjective mood were detected after subliminal faces, but people poured and drank roughly twice as much after subliminal happy faces than after subliminal angry faces. Modified from [18].
Incentive salience ‘wants’ are triggered by foods and their cues [11,19,20]. Cue-triggered ‘wanting’ does not require understanding of causal relations about hedonic outcome. ‘Wanting’ processes can be triggered even without a person's conscious awareness that anything has happened [17].An important consequence of the difference between ‘wanting’ and more cognitive desires is that excessive incentive salience may in some cases lead to irrational ‘wants’ for outcomes that are not cognitively wanted, and that are neither liked nor even expected to be liked [21,22].
Behavioral neuroscience experiments have indicated that these forms of wanting may depend on different brain structures. For example, incentive salience ‘wanting’ depends highly on subcortical mesolimbic dopamine neurotransmission, whereas cognitive forms of wanting depend instead on cortical brain regions such as orbitofrontal cortex, prelimbic cortex and insular cortex [16,23]. The conclusion that there may be multiple kinds of psychological desire with different neural substrates has fascinating implications for disorders of desire, including the possibility of irrational desires in which individuals powerfully ‘want’ a reward that they cognitively do not want at all.
2.3. Measuring pleasure ‘liking’
Returning to the heart of reward: hedonic impact or pleasure. The practical problem in finding neural substrates for pleasure ‘liking’ is to first find a way to measure pleasure. Fortunately, pleasure ‘liking’ is a real psychological process with distinct neural mechanisms, and has objective markers in brain and behavior as well as subjective feelings [1]. The objective markers can be especially useful to give a handle on pleasure for neuroscientists, as I will describe below.
Many brain sites are activated by food pleasures in neuroimaging studies of humans. Pleasant foods activate cortical sites in the front of the brain implicated in the regulation of emotion, such as the orbitofrontal cortex and anterior cingulate cortex and insular cortex; as well as sub-cortical forebrain limbic structures such as amygdala, nucleus accumbens, and ventral pallidum; mesolimbic dopamine projections and even deep brainstem sites [8,11,24–37]. All of these brain structures may code pleasurable foods, in the sense of activating during the experience of seeing, smelling, tasting, or eating those rewards. The orbitofrontal cortex in particular has been suggested to code the pleasure of food stimuli in humans, especially along its medial edge and in a mid-anterior site that tracks changes in food pleasure during alliesthesia of hunger or satiety [28,34,35,38].
But let's also ask: which of these many brain structures actually cause or generate the pleasure of foods? Do all the neural activations generate pleasure ‘liking’ or only some? Other brain activations might reflect consequences of pleasure that were caused elsewhere. Those activations in turn might cause motivation, learning, cognition or some other function consequent to the reward, but they would not cause pleasure per se. How can the causal brain systems for pleasure be identified? Typically only by results of brain manipulation studies: a manipulation of a particular brain system will reveal pleasure causation if it produces an increase or decrease in ‘liking’ reactions to food pleasure (Fig. 2).
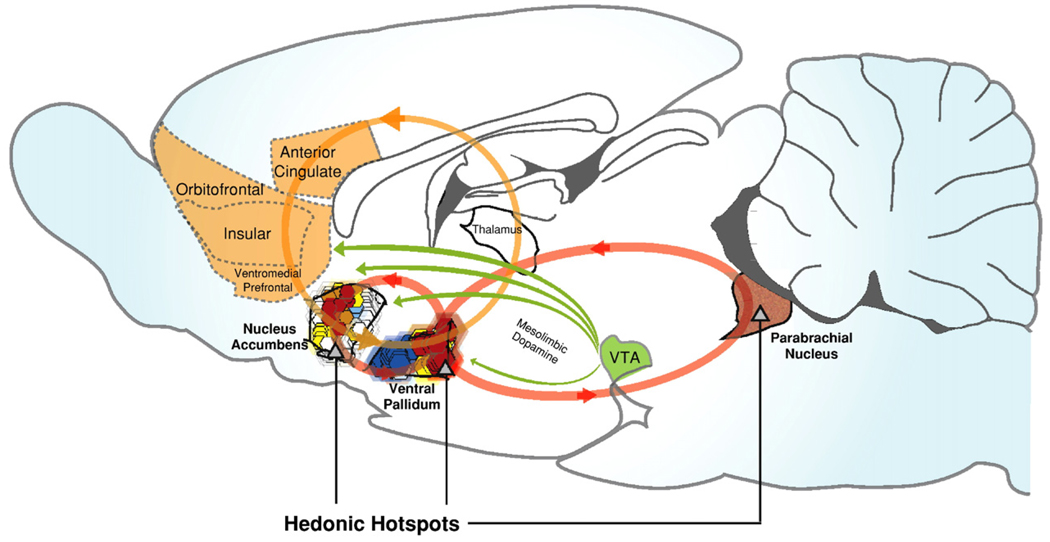
Fig. 2.
Hedonic hotspots and hedonic circuits. Hedonic hotspots are shown in nucleus accumbens, ventral pallidum, and brainstem parabrachial nucleus where opioid or other signals cause amplification of core ‘liking’ reactions to sweetness. Reprinted by permission from [55], based on [38,76,80].
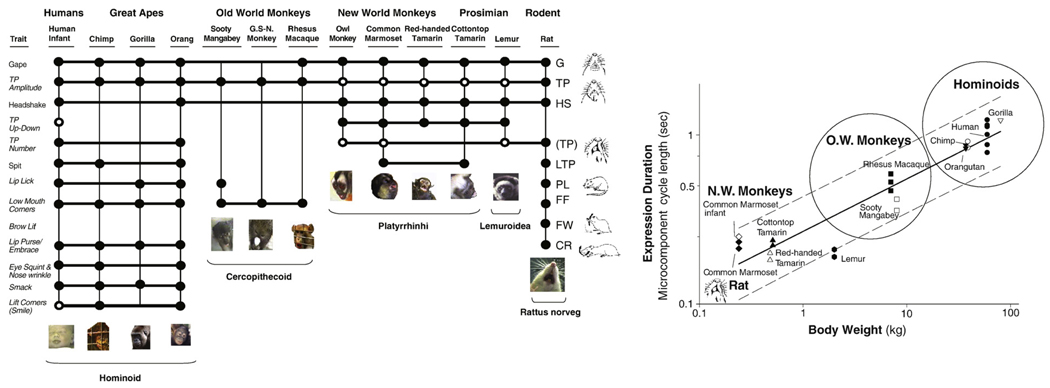
Most brain manipulations cannot be performed ethically except in animals, yet one must also be able to identify pleasure ‘liking’ when it occurs, and that requires reliable indices of ‘liking’ reaction even in animals. A useful ‘liking’ reaction to measure taste pleasure in our studies has been the affective facial expressions elicited by the hedonic impact of sweet tastes. These were described originally in human infants by Jacob Steiner and in rats by Harvey Grill and Ralph Norgren, allied with Carl Pfaffmann [39–42]. Sweet tastes elicit positive facial ‘liking’ expressions (tongue protrusions, etc.), whereas bitter tastes instead elicit facial ‘disliking’ expressions (gapes, etc.) (Fig. 3 and Fig.4). Fortunately for studies of pleasure causation, these ‘liking–disliking’ facial reactions are homologous in humans and animals, in that they have developed from the same evolutionary source in humans, orangutans, chimpanzees, monkeys, and even rats and mice, and therefore share underlying brain circuits [42,43] (Fig. 3). The most similar ‘liking’ reactions are shown by species that are closest in phylogenetic relationship, and a number of the reactions share the same underlying deep structural features across humans, other primates and rodents. The deep features include conformity to identical allometric timing laws scaled to the particular size of the species (Fig. 4). For example, human or gorilla tongue protrusions to sweetness or gapes to bitterness may appear relaxed and slow, whereas the same reactions by rats or mice seem startlingly fast, yet, they are actually the ‘same’ durations in what is called an allometric sense; that is, each species is timed proportionally to their evolved sizes. That timing is programmed deep in their brains, which is evident in that even young infants obey the timing rule of their species. Such universal rules applying to different species further underlines the common brain origins of these ‘liking’ and ‘disliking’ reactions in rats and humans, and indicates that what is learned about brain mechanisms in animals is likely to apply to humans too.
Fig. 3.
Taste ‘liking’ reactions and contrast map of nucleus accumbens hotspots. Positive ‘liking’ reactions to pleasant sweet tastes shared by human newborn, young orangutan, and adult rat (tongue protrusion; left top), and aversive ‘disliking’ reactions to unpleasant bitter tastes (gape; left bottom). Opioid hotspots and coldspots in the nucleus accumbens (medial shell region shown in sagittal view; right). Green; the entire medial shell mediates opioid-stimulated increases in ‘wanting’ for food reward. Red; only a cubic-millimeter sized hedonic hotspot generates increases in ‘liking’ for the same opioid stimulation. Blue; opioid stimulation of a small hedonic ‘coldspot’ suppresses ‘liking’ reactions to sucrose, whereas a larger purple zone suppresses ‘disliking’ reactions to quinine, all while stimulating food intake. Reprinted by permission from [55], based on data from [53].
Fig. 4.
Homology in affective facial expressions of taste ‘liking’: Left: Taxonomic tree based on shared details of affective facial expressions to taste. Behavioral expression taxonomy mirrors phylogenetic relationships among humans, 11 other primate species and rats. Species that are closely related share the most components (indicated by connecting horizontal lines). All species share some universal components, such as gapes to bitter. Right: Allometric deep structure in the timed duration of a single tongue protrusion. Although cycle durations of rodents are short whereas cycles of apes and humans are long, they all follow the identical timing rule that generates speed proportionally to body size. Modified from [42,43].
2.4. Brain systems for food pleasure
This sets the stage for animal affective neuroscience studies to use these affective expressions to identify brain mechanisms that generate hedonic impact. Recent years have seen progress in identifying brain systems responsible for generating the pleasure gloss that makes palatable foods ‘liked’ [1,2,27,28,32,44–50]. What has emerged most recently is a connected network of hotspots in the limbic forebrain that use opioid neurotransmission to causally increase taste ‘liking’ and ‘wanting’ together to enhance food reward. The hotspots form a distributed network of brain islands like an archipelago that connects the limbic forebrain and brainstem [48,51–54]. There are hedonic hotspots identified so far in the nucleus accumbens and ventral pallidum, and indicated to exist in deep brainstem regions such as the parabrachial nucleus in the pons; possibly others yet unconfirmed could exist in amygdala or in cortical regions such as orbitofrontal cortex [1,55]. These distributed ‘liking’ sites are all connected together so that they interact as a single integrated ‘liking’ system, which operates by largely hierarchical control rules across the major levels of the brain (Fig. 2).
2.5. Building affect from the brainstem up
Affect, in a sense, begins in the brainstem. Basic brainstem circuits participate in ‘liking’ reactions as well as in pain, and are partially autonomous, able to function as reflexes in an isolated brainstem. For example, basic positive or negative facial expressions are still found in human anencephalic infants born with a midbrain and hindbrain, but no cortex, amygdala, or classic limbic system, due to a congenital defect that prevents prenatal development of their forebrain. Yet, sweet tastes still elicit normal positive affective facial expressions from anencephalic human infants, whereas bitter or sour tastes elicit negative expressions [41]. Similarly, a decerebrate rat has an isolated brainstem, because of a surgical transaction at the top of its midbrain that separates the brainstem from the forebrain, but that decerebrate brainstem remains able to generate normal positive expressions to sweet tastes and negative expressions to bitter tastes when those are placed in the rat's mouth [56,57].
Some people find it disconcerting that decerebrates have the capacity to generate core affective reactions, or even grounds for rejecting facial expressions as a measure of affect. The rejection is rooted in traditional notions that a brainstem has only reflexes. It may seem hard to accept that facial hedonic expressions to sweetness can be any measure of ‘liking’ when decerebrate rats or infants display similar expressions. It is difficult for this view to accept that a decerebrate ‘likes’ the stimulus in any sense. There are really two points here: 1) whether the brainstem participates in mediating affect, and 2) whether in a normal individual with a whole brain, the same behavioral reaction expresses affect processes that are generated in the forebrain (rather than being just a brainstem reflex).
First, is the brainstem at all affective? It is important to recognize that affect generation is not localized to just one place in the brain. We live in localizationist age, powered in part by the accomplishments of neuroimaging (and consistent with discoveries of forebrain hedonic hotspots). But the idea that pleasure and motivation arises in the forebrain can be carried too far: identifying a function in one brain site does not rule out that the same function is also mediated by another site elsewhere. Affect circuits are distributed across the brain, even down into the brainstem.
Certainly a decerebrate rat or infant cannot like a sweet taste in the same sense that a normal individual does. But I think it we should consider the possibility that it still has a residual core component of ‘liking’. Not necessarily a conscious pleasure, of course, but an affective subcomponent of the subcomponent of the ‘liking’ process nevertheless. After all, almost every feeling of physical pleasure or pain felt by your forebrain has climbed its way there through the brain stem. Ascending signals don't just pass through the brainstem; much processing happens to them on the way up. There is compelling reason to believe that affect begins in the brainstem for both pleasure and pain. In a normal brain, brainstem sites make important contributions to affective experiences that mostly are generated by forebrain circuits above them. For example, ‘liking’ and food ‘wanting’ are amplified by benzodiazepines microinjections in the parabrachial nucleus of the pons [58–60], where neurons code the palatability shift by changes in firing rate [61], and even decerebrates show enhanced ‘liking’ reactions to sucrose taste after benzodiazepine administration [62]. Even a decerebrate brain may contain the kernel of a ‘liking’ reaction that the word reflex does not adequately capture, just as the brainstem also contains substantial circuitry for pain and analgesia. This may reflect the adaptive functions of affective reactions throughout brain evolution [63], and may also be relevant to how unconscious ‘liking’ reactions occur in people even today [18].
Second, in a normal brain the brainstem participates more fully in ‘liking’ and ‘wanting’, when it is connected to the forebrain and becomes a hierarchical intermediary stage in larger affect circuits. As the pioneering neurologist John Hughlings Jackson described the brain's hierarchical organization a century ago, “They (forebrain structures) represent over again in more complex, etc., combinations, the parts which all middle centres have re-represented, and thus they represent the whole organism; they are re-re-representative” [64], (p. 42). This reiterative structure implies that the forebrain re-re-represents pleasures that the brainstem has already represented in simpler fashion. In turn, forebrain systems normally control the brainstem circuits, so that normal ‘liking’ reactions are not merely brainstem reflexes in a whole-brained individual. A good parallel to facial expression is vocalization: anencephalic infants also cry and vocalize and even a decerebrate rat squeaks and emits distress-type cries if its tail is pinched. But vocalizations such as the cries of normal babies or of normal rats are certainly not brainstem reflexes. Rather in a normal brain the brainstem systems are always under hierarchical control by forebrain systems: the brainstem systems are often activated at forebrain command. Likewise, as described below, forebrain hedonic hotspots control the ‘liking’ activation of brainstem-generated facial expressions. Obviously neither vocalizations or affective expressions are merely brainstem reflexes when generated by an entire brain that connects all levels via hierarchical control.
Hierarchical control can be empirically demonstrated by the ability of a forebrain manipulation to activate affective reaction, such as when a drug microinjection in a limbic hedonic hotspot selectively doubles the number of ‘liking’ facial reactions elicited by a sweet taste. When brainstem is connected to the forebrain, the entire affective system operates in a hierarchical, flexible and complex fashion, and the final behavioral of affective expression redlects forebrain ‘liking’ processes.
2.6. Forebrain ‘liking’ generation: hedonic hotspot in nucleus accumbens
Affect generated by forebrain circuits does indeed control ‘liking’ expressions to sweetness. As an illustration, we have recently endeavored to pinpoint affect-generating circuits in the forebrain, and have identified a hedonic hotspot in the nucleus accumbens that uses opioid and endocannabinoid signals to amplify ‘liking’ for sweetness. The nucleus accumbens is recognized to contain major subdivisions called core and shell, and the hotspot lies in the shell subdivision: specifically, a cubic-millimeter volume of tissue in the rostrodorsal quadrant of the medial shell. The medial shell is a brick-shaped entity that lies on its long edge and runs lengthwise front to back. The hedonic hotspot in the medial shell amplifies ‘liking’ by using opioid and endocannabinoid neurochemical signals released within it. Opioid neurotransmitters, such as enkephalin and endorphin are mimicked by opiate drugs made from the opium poppy (e.g., heroin). Endocannabinoid neurotransmitters such as anandamide are mimicked by drugs such as marijuana.
A number of investigators have suggested over the years that endogenous opioid or cannabinoid receptor activation stimulates appetite in part by enhancing ‘liking’ for the perceived palatability of food [46,48,65–74]. Our results have confirmed the hypothesis that these agents amplify food ‘liking’. In the hedonic hotspot of the nucleus accumbens, activating the mu subtype of opioid receptor in particular causes increase in food reward ‘liking’ (and ‘wanting’ too). Studies led by Susana Peciña in our laboratory found that within the cubic-millimeter hotspot site in the medial shell, microinjections of a drug (DAMGO) which activate the mu type of opioid receptor appear sufficient to enhance the pleasure gloss painted by the brain on sweetness sensation [53,55,75,76]. More than double the usual number of positive ‘liking’ reactions were emitted to sucrose taste by rats with DAMGO microinjections in their hotspots. ‘Disliking’ reactions to quinine were never enhanced, but rather were suppressed by DAMGO in and around the hotspot (Fig. 2).
Similarly for endocannabinoids, a study by Stephen Mahler and Kyle Smith found that an anatomically-overlapping hotspot appears to exist in medial shell for anandamide, which likely acts by stimulating the CB1 type of cannabinoid receptor [55,77]. Inside the accumbens hotspot, anandamide microinjection potently doubled the number of positive ‘liking’ facial reactions that sucrose taste elicits from rats, just as opioid stimulation had, whereas again aversive reactions to bitter were not similarly enhanced. It is possible that opioid and endocannabinoid signals in the overlapping hotspots interact or cooperate together to amplify sensory pleasures. Anandamide has been suggested to be a reverse neurotransmitter, which would be released by a target neuron in the shell to float back to nearby presynaptic axon terminals and stimulate CB1 receptors especially. Future studies may be able to explore if endocannabinoid signals enhance ‘liking’ by recruiting presynaptic opioid release, perhaps in a cooperative positive feedback mechanism.
To aid in pinpointing the ‘liking’ mechanisms we developed a ‘Fos plume’ tool that maps the boundaries of hedonic hotspots. A Fos plume contains neurons clustered around a microinjection site which are stimulated by the drug to begin transcription and translation of the c-fos gene into Fos protein inside their nuclei, as a step to activating other genes and changing the molecular biology of the neurons that in turn changes the neurons' functions. When a drug microinjection causes an increase in ‘liking’, neurons directly stimulated by the drug and most likely responsible for starting the psychological enhancement can be visualized as a plume-shaped fluorescent green group surrounding the microinjection site (when the brain tissue is processed soon after). This plume allows assignment of causation to the appropriate brain sites, and hotspot boundaries emerge by comparing the plume maps for microinjection sites that successfully enhanced ‘liking’ to surrounding sites that failed (Fig. 3).
2.7. Larger opioid sea of ‘wanting’ in nucleus accumbens
The same hotspot microinjections of DAMGO or anandamide also stimulate ‘wanting’ or eating of food. But ‘wanting’ mechanisms extend far beyond hedonic hotspots. For example, the opioid hedonic hotspot comprises a mere 10% of the entire nucleus accumbens, and even only 30% of its medial shell. Yet DAMGO microinjections throughout the entire 100% of medial shell potently increased ‘wanting’, more than doubling the amount of food intake. Peciña found that DAMGO enhanced ‘wanting’ as effectively even at a more posterior ‘coldspot’ where the same microinjections suppressed ‘liking’ for sweetness. Widely spread opioid mechanisms for ‘wanting’ in the nucleus accumbens is consistent with previous findings that opioids stimulate food ‘wanting’ throughout the entire nucleus accumbens and even in outside structures that include amygdala or neostriatum [48,50,52,78,79]. Thus the appetite-increasing zone is much larger than the pleasure hotspot: it is as though a large sea of ‘wanting’ opioid systems fill the shell of nucleus accumbens, and contains a smaller opioid island that can simultaneously enhance ‘liking’ for the same reward [53].
The anatomical dissociation of ‘liking’ (only in the hotspot) from ‘wanting’ (entire nucleus accumbens) means that the brain's pleasure network does not extend to the entire opioid limbic system that stretches throughout much of the forebrain. That happy possibility would give every brain a really large opioid hedonic causation system for generating pleasure. Instead, opioid activation enhances taste pleasure at only some of the limbic sites where it stimulates the motivation to consume palatable foods. The parallel situation for endocannabinoids is still less clear, as the only mapping study of the anandamide hedonic hotspot in shell so far found marked co-extension of ‘liking’ and ‘wanting’ anatomically, and so more remains to be done.
2.8. Ventral pallidum: ‘liking’ and ‘wanting’ pivot point for limbic food reward circuits
The ventral pallidum is relatively new on the affective neuroscience scene, but there is reason to believe this chief target of nucleus accumbens is crucial for both normal reward ‘liking’ and for enhanced ‘liking’ caused under some neurochemical conditions. Studies by Kyle Smith have identified a second opioid hedonic hotspot within the ventral pallidum [54,55,76,80]. Knowledge about the anatomy of the brain region that contains ventral pallidum has grown in recent years [52,55,81–85]. Until about 10 years ago the ventral pallidum was known sometimes as part of the substantia innominata, or brain substance without a name, and earlier than 20 years ago it was often mistaken for part of the lateral hypothalamus. Today it has a name, actually several names that correspond to different divisions of this intriguing part of the ventral forebrain. The chief names today include ‘ventral pallidum’ containing the part known to cause ‘liking’ for sensory pleasure, ‘basal nucleus’ for an acetylcholine-rich anterior zone involved in attention, and ‘sublenticular extended amygdala’ for a bit behind that lies between ventral pallidum and lateral hypothalamus (the extended amygdala also contains the bed nucleus of the stria terminalis stretching back toward the central amygdala).
As limbic signals leave the nucleus accumbens, the two heaviest projections may be posteriorly to two nearby neighbors, the ventral pallidum and lateral hypothalamus. Of these two structures, the lateral hypothalamus has long been the most famous for roles in food intake and food reward. But my colleagues and I believe the ventral pallidum may be even more important, at least for ‘liking’ food rewards [54,55,76,80,86].
What seems to me to be an astounding fact is that the ventral pallidum and its environs contains the only brain region known so far where the death of neurons abolishes all ‘liking’ and replaces with ‘disliking’ even for sweetness (at least for several weeks) [87]. This assertion may surprise readers who remember learning that the lateral hypothalamus is a site where lesions cause aversion (or who remember that decerebrates show ‘liking’ reactions), so some explanation is in order.
Lesions of the lateral hypothalamus have long been known to disrupt eating and drinking behaviors, sending food and water intakes to zero [88,89]. After electrolytic lesions to lateral hypothalamus, rats starve to death unless given intensive nursing care and artificial intra-gastric feeding. Decades ago, lateral hypothalamic lesions were thought not only to abolish food ‘wanting’, but also to abolish food ‘liking’ too. Even sweet tastes were reported to elicit bitter-type disliking reactions [88,90,91]. However, it appears that lateral hypothalamus may have been blamed through a case of mistaken identity for the effects of lesions that actually stretched beyond it in lateral and anterior directions. Those large lesions of the 1960s and 1970s typically damaged the ventral pallidum too.
An early lesion mapping study of aversion by Schallert and Whishaw attempted to identify the precise location for lesion-induced aversion, before the ventral pallidum was recognized to exist as a distinct limbic structure, and reported that sucrose ‘liking’ was replaced by sucrose ‘disliking’ only if the lesion was in the anterior zone of lateral hypothalamus — and not if the lesion was in the posterior part of lateral hypothalamus, where it would produce loss of eating and drinking, but leave ‘liking’ reactions essentially normal [90]. A subsequent lesion mapping study by Howard Cromwell in our laboratory used a more precise neuron-counting method to quantify excitotoxin lesions and recognized the existence of ventral pallidum, and therefore aimed to identify more carefully the boundaries of where neuron death actually caused aversion, by explicitly comparing ventral pallidum to lateral hypothalamus. Cromwell found that the ‘disliking’ lesions actually had to be so far anterior and lateral that they escaped the boundaries of the lateral hypothalamus itself — and lay in the structure further anterior or lateral, namely the ventral pallidum [87]. Essentially these lesions seem to disinhibit other aversion-generating systems of the forebrain, so what remains is ‘disliking’ for everything.
Ventral pallidum can also generate enhancement of natural pleasure when it is intact, by opioid stimulation of its own hedonic hotspot [54,80]. The ventral pallidum hotspot is roughly a cubic-millimeter in volume and is located in the posterior end of the structure. The ventral pallidum is somewhat cigar shaped. If you hold out your hands as if grasping a small steering wheel in front of your waist, your two forearms are in approximately in the same orientations relative to your upright body as your left ventral pallidum and right ventral pallidum are in your brain. An elongated structure pointing forward slightly down and inward, the opioid hedonic hotspot is the posterior one-third corresponding to the two or 3 inches of your forearm nearest the elbow. The elbow zone is the posterior ventral pallidum that contains the hedonic hotspot.
Studies by Kyle Smith in our lab identified the ventral pallidum hotspot and showed that in it microinjections of the opioid agonist DAMGO caused sucrose taste to elicit over twice as many ‘liking’ reactions as it normally did [54]. Opioid activation in the posterior ventral pallidum increased the hedonic impact of the natural taste reward, and also caused rats to eat over twice as much food. If the same opioid microinjections were moved anteriorly outside the hotspot toward the front of the ventral pallidum, it actually suppressed hedonic ‘liking’ reactions to sucrose and suppressed food intake too [54]. These effects seem consistent with the findings of several other laboratories on the importance of ventral pallidum in food and drug and other rewards [92–98].
A final reason to suppose that ventral pallidum mediates hedonic impact of ‘liked’ sensations is that the activity of neurons in the posterior hedonic hotspot appears to code ‘liking’ for sweet, salty and other food rewards [19,44,92,93,99–101]. In rats, recording electrodes can be permanently implanted in the ventral pallidum, and neurons there fire faster when rats eat a sweet taste. The firing of sucrose-triggered neurons appears to reflect hedonic ‘liking’ for the taste. For example, the same neurons will not fire to an intensely salty solution that is unpleasant (three-times saltier than seawater). However, the neurons suddenly begin to fire to the triple-seawater taste if a physiological state of ‘salt appetite’ is induced in the rats, by administering hormones that cause the body to need more salt, and which increase the perceived ‘liking’ for intensely salty taste [101]. Thus neurons in the ventral pallidum code taste pleasure in away that is sensitive to the physiological need of the moment. When a taste becomes more pleasant during a particular physiological hunger, in a hedonic shift called ‘alliesthesia’, the ventral pallidum neurons code the increase in salty pleasure. The observation that those hedonic neurons are in the same hedonic hotspot where opioid activation causes increased ‘liking’ reactions to taste suggests that their firing rate might actually be part of the causal mechanism that paints the pleasure gloss onto taste sensation. Conversely, in humans, the sight of disgustingly rotten food has been reported to especially activate the anterior portion of ventral pallidum where in rats microinjections of DAMGO would actually suppress ‘liking’ reactions and reduce eating behavior, more than the posterior hotspot [93].
3. ‘Wanting’ without ‘liking’
Quite different from hotspots for ‘liking’ generation has been the revelation that some previously-thought hedonic brain mechanisms actually fail to live up to that role, and turn out instead to mediate only the motivational ‘wanting’ to eat, without mediating hedonic ‘liking’ for the same food at all. One example was already described: the opioid sea of pure wanting in nucleus accumbens outside the hedonic hotspot. There are now many other examples as well. The phenomenon of ‘wanting’ without ‘liking’ opens up fascinating possibilities for what might be called irrational desires that could underlie some pathologies of appetite [21].
In my opinion, perhaps the most famous is dopamine, which was once thought to be a pleasure neurotransmitter. The mesolimbic dopamine projection arises from neurons in the midbrain ventral tegmental area that project up to the nucleus accumbens in the forebrain [102]. Dopamine release is triggered by pleasant foods and many other pleasant rewards, and dopamine neurons themselves fire more to pleasant food (especially when the reward is suddenly and unexpectedly received) and their predictive cues [33,103–110].
Beyond correlative activations by rewards, the causal importance of dopamine in some aspect of reward is seen in the well-known observation that drugs that are rewarding or addictive typically cause dopamine activation — either directly or by acting on other neurochemical systems that in turn cause dopamine activation [8,111]. Conversely, dopamine suppression reduces the degree to which animals and people seem to want rewarding foods, or rewards of other types [7,49,112].
Everyone therefore agrees that dopamine causes some aspect of reward, but argument persists on which aspect it mediates [113–116]. I will focus below on hypotheses that dopamine causes ‘liking’ or ‘wanting’ for food rewards, and only note in passing that a third popular hypothesis is that dopamine causes reward learning [33,117,118]. That hypothesis is of interest for the neuroscience of reward prediction, but has not been applied much to explaining food appetite or eating disorders. The learning hypothesis for dopamine therefore will not be discussed here, though I and others have recently discussed it elsewhere [33,104,113,114,116,119,120].
The suppression of reward ‘wanting’ by dopamine blockade or loss gave rise decades ago to the idea that dopamine must also mediate reward ‘liking’ [121]. The view of most neuroscientists has shifted subsequently, although some correlative evidence collected in recent years can still be viewed as consistent with the original dopamine pleasure hypothesis of reward. For example, PET neuroimaging studies have suggested that obese people may have lower levels of dopamine D2 receptor-binding in their brains' striatum than others [122,123]. At first take, if one supposes that dopamine causes pleasure, then reduced dopamine receptors in obese individuals can be viewed as reducing the pleasure they get from food. By that view, reduced pleasure has been suggested to cause those individuals to eat more food in a quest to regain normal amounts of pleasure. A difficulty may arise for this account in that it also seems to require that the less people like a food the more they will eat it. Instead, humans and rats all tend to eat less of food that is unpalatable, and to eat more of palatable treats. Otherwise people might consume oatmeal and broccoli much more avidly than ice cream, if people compensated for hedonic dilution by wanting to eat more of what gave them less pleasure. In general, much evidence from psychology and neuroscience evidence indicates that reducing how much a food is ‘liked’ usually reduces how much it is ‘wanted’, rather than increasing its pursuit and consumption [48,78,124–126].
Still, one might perhaps rescue this dopamine anhedonia account of D2 signalling decrement by supposing that all other life pleasures are reduced even more by dopamine receptor suppression than food pleasure, so that food remains the only pleasure available. However, we can see that actually getting an increase in food consumption from reduced pleasure via any known neuro-psychological system of food reward may prove trickier than first appears. So alternatives are worth entertaining too. A reverse interpretation of reduced dopamine D2 binding in obese people is that the reduction is a consequence of overeating and obesity, rather than its cause. As a parallel example, over-consumption of drug rewards that provide increased stimulation to dopamine receptors eventually causes the receptors to reduce in number, even if dopamine receptors were normal to begin with — this is a down-regulation mechanism of drug tolerance and withdrawal [111]. That makes it conceivable that similar sustained over-activation of dopamine systems by over-eating food rewards in obese individuals perhaps could cause a similar eventual down-regulation of their dopamine receptors. In a related vein, other physiological aspects of pre-existing obesity states might also send excessive signals to brain systems sensitive to body weight, which indirectly cause reduction of D2 receptor as a negative feedback consequence or a sort of long-term satiety signal that down-regulates incentive systems. These speculative alternatives are enough to illustrate that possibilities exist by which reduced dopamine receptor binding could be a consequence, rather than the cause, of sustained obesity. Finally, one last complication is that D2 receptors can switch between high and low modes of signalling [127]. Current D2 binding drugs attach to both high and low modes, but only receptors in the high mode may actually contribute to the transmission of dopamine signals. Further, sometimes high and low populations change in opposite directions. That raises the possibility some individuals so far reported to have reduced D2 signalling related to total population suppression (mostly in low mode) might actually turn out to have a higher proportion of receptors in high mode, and therefore possess an elevation in functional high-mediated dopamine signalling despite overall reduction in receptors (perhaps the former might even contribute to the latter) [127,128]. Future research will be needed to resolve these fascinating issues regarding D2 receptors and dopamine signalling.
If we turn to animal studies in which dopamine's causal roles have been manipulated, then dopamine does not appear to be important for ‘liking’ the hedonic impact of food rewards after all. For example, mutant mice that lack any dopamine in their brains have been argued to still register the hedonic impact of sucrose or food rewards, in that their preference or learning about a palatable reward remains [129,130]. Similarly, taste reactivity studies have shown that dopamine suppression or complete lesion in normal rats does not suppress taste ‘liking’ facial expressions elicited by the taste of sucrose [7,131]. Instead, the hedonic impact of sweetness remains robust even in a nearly dopamine-free forebrain (also, still robust is the ability to learn some new reward values for a sweet taste, which indicates that forebrain ‘liking’ systems remain in control of ‘liking’ expressions after loss of 99% of accumbensstriatal dopamine) [7].
Conversely, too much dopamine in the brain, either in mutant mice whose gene mutation causes extra dopamine to remain in synapses or in ordinary rats given amphetamine in nucleus accumbens that causes dopamine release (or that have drug-sensitized dopamine systems), show elevated ‘wanting’ for sweet food rewards, but no elevation in ‘liking’ expressions to the taste of sweet rewards [19,20,132]. All of these brain manipulations make animals ‘want’ to eat food more, though they fail to make the animals ‘like’ food more (and sometimes even make them ‘like’ it less).
It may be important to note that a dopamine role in ‘wanting’ for food does not mean that dopamine-related systems must be constantly active in a hungry individual [133]. Continuous hyperactivity is different from hyper-reactivity. It only suggests that food cues may elicit higher reactions in dopamine-related brain circuits. Simultaneous presence of cues and hunger states (or drug states) can be needed to reveal amplification of incentive salience in neural and behavioral experiments [20,134], and may be important to reveal dopamine increases and related limbic activations [35,135,136]. This reflects the nature of incentive salience as a cue-triggered incentive process, rather than a constant drive [137–139].
Important confirmation that dopamine mediates ‘wanting’ but not ‘liking’ may now be coming from neuroimaging studies of humans, especially those that manipulate dopamine signalling with drugs, which report that dopamine release triggered when people encounter a food or drug reward may better correlate to their subjective ratings of wanting the reward than to their pleasure ratings of liking the same reward [36,140]. Similarly, in humans, drugs that block dopamine receptors may completely fail to reduce the subjective pleasure ratings that people give to a reward stimulus such as amphetamine [141–144].
Thus, the idea that dopamine is a pleasure neurotransmitter has faded considerably in the neuroscience literature, with only a few hedonia pockets remaining (though dopamine seems important to ‘wanting’ rewards, even if not to ‘liking’ rewards). Separating true ‘liking’ substrates from false ones is a useful step in identifying the real affective neural circuits for hedonic processes in the brain.
Why did brains evolve separate ‘wanting’ and ‘liking’ mechanisms for the same reward? One speculative possibility is that, originally, ‘wanting’ might have evolved first as an elementary form of goal directedness to pursue particular innate incentives even in advance of experience of their hedonic effects. Later, as hedonic and associative mechanisms evolved, ‘wanting’ became harnessed to work with them in extending ‘wanting’ to learned stimuli associated with ‘liked’ rewards [16,33,124,139]. Another evolutionary pressure that may have promoted a distinct mechanism for ‘wanting’ is the need for a common neural currency of incentive salience shared by all rewards, which could compare and help decide choices for competing rewards of food, sex, and other incommensurate types of pleasure that might each involve partly distinct neural ‘liking’ circuits [1,145]. The important point is that ‘liking’ and ‘wanting’ normally go together, but they can be split apart under certain circumstances, especially by certain brain manipulations.
3.1. Connecting brain reward, stress and regulatory systems
A related fascinating topic, though beyond my present scope, is the interaction between brain systems of ‘liking’ and ‘wanting’ reward, on the one hand, with hypothalamic-focused hunger and body weight regulation mechanisms on the other In the phenomenon of alliesthesia, hedonic ‘liking’ for food reward, as well as motivational ‘wanting’ to eat, can be enhanced by hunger and diminished by satiety [38,101,110,146–150]. Another important topic is how stress systems interact with brain reward systems [151–155]. Though also beyond current reach, it is interesting to note that CRF stimulation in nucleus accumbens magnifies cue-triggered ‘wanting’ similarly to dopamine stimulation, making sugar cues trigger much higher bursts of ‘wanting’ expressed as more lever pressing in rats [154]. Stress-induced amplification of incentive salience mechanisms could contribute to binge eating when stress and food cues combine together [152].
How do reward and regulatory brain systems connect and influence each other? Great progress has been made in recent years toward understanding these neural interactions. Control signals go back and forth between mesocorticolimbic reward systems and hypothalamic regulation systems [45,126,133,147,156–164]. For example, hypothalamic orexin–hypocretin neurons send projections to modulate the nucleus accumbens in ways that might allow hunger states to enhance food reward [165], and even interact with other rewards such as drugs [160]. In return, nucleus accumbens influences hypothalamic circuits. For example, manipulations of nucleus accumbens that cause increased food intake and that modulate reward, such as GABA microinjections into the medial shell, send descending signals that activate orexin neurons in the hypothalamus [166–168].
Neuroscientists have only begun to understand the nature and role of interactions between mesolimbic reward systems and hypothalamic hunger systems, but recent developments show that such interactions exist and are of great importance. They undoubtedly play major roles in alliesthesia modulation of the pleasure and incentive value of food rewards during normal hunger versus satiety states, possibly also in connecting reward modulation to longer-term body weight elevation and dieting states, and finally perhaps even in allowing food reward cues to influence the activation of hunger deficit systems. These interactions also provide avenues, at least in principle, by which eating disorders cause distortion in the function of reward systems, so that they become either exaggerated or suppressed in function. Such interactions will be important to try to understand better in the future.
4. Potential roles of brain reward systems in eating disorders
So how do ‘wanting’ and ‘liking’ relate to human eating disorders? At least in principle, we can sketch several alternative possibilities in principle for how brain reward systems might function in any particular eating disorder. Comparison of these alternatives may help to frame the issue.
The idea of food addiction will not be adequately discussed here (and will only briefly touch upon potential brain mechanisms). Researchers who deal with eating disorders are best positioned to judge whether there are in fact food addictions, and what are the criteria that allow the use of this term. It is an important question whether food addiction exists as comparable to drug addiction or instead is simply a shorthand for eating patterns pushed to an extreme [169–171]. The debate largely focuses on whether particular addiction processes, such as withdrawal or sensitization, actually occur in eating disorders. It might also be relevant to think about whether eating disorders share addictive features of behavior that can help distinguish a compulsion, such as persistence in the face of adverse costs or escalation of intensity in binge/purge patterns (though constraints such as stomach size place stricter limits on food intake, by comparison to drug intake that is relatively free to escalate).
Further, it is also important to acknowledge that other psychological and cultural factors are involved in eating disorders, beyond reward-related or regulatory processes. Concepts such as a focus on thinness and associations with OCD have explanatory power for certain anorexia and other eating disorders. Mesolimbic mechanisms involved in food reward, including dopamine, might contribute to generating obsessive dreads as well as obsessive desires (perhaps such as a focus on avoiding weight gain and remaining thin), and mesolimbic desires and dreads can even co-exist or feed off one another [155,172,173]. Still, eating disorders also likely involve much more elaborate cognitive, psychodynamic, and cultural processes that are simply beyond the present scope.
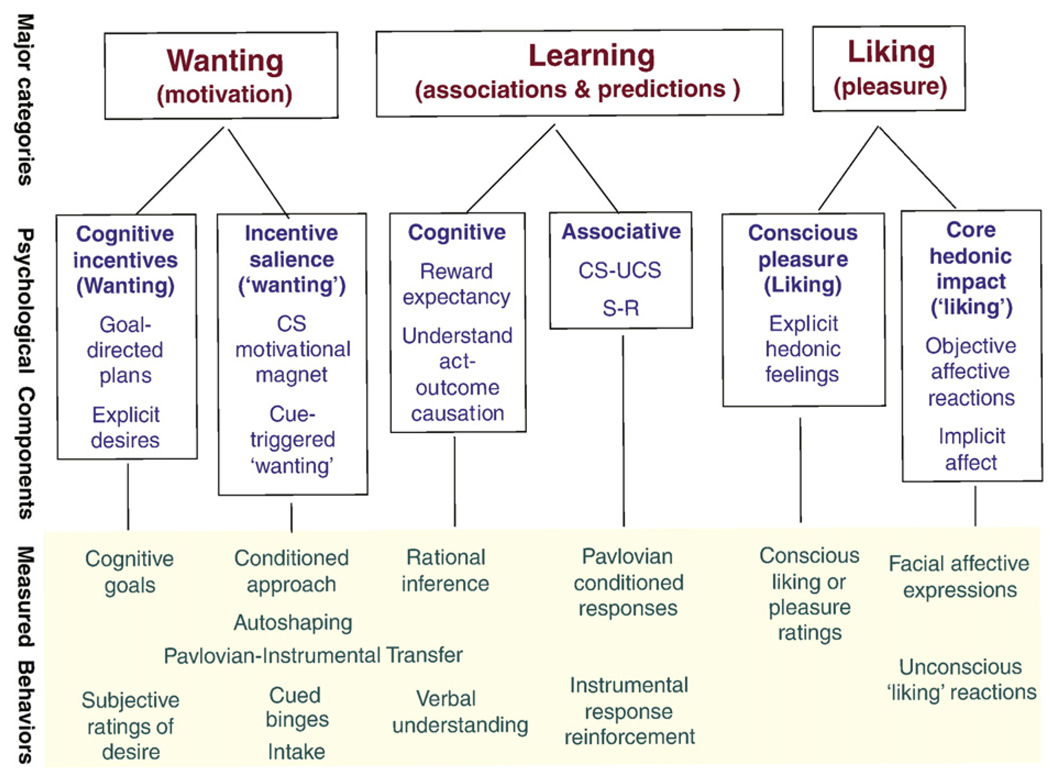
Yet brain reward mechanisms still remain of interest in under-standing eating disorders (Fig. 5). It may be useful to sketch out several alternatives for how they might relate to a particular disorder.
Fig. 5.
Components of liking, wanting, and learning inside reward. This table represents the various components of reward discussed, and how each has been measured in experiments. The reward components occur together simultaneously, but have separable neural substrates and different psychological features. For example, ‘liking’ or core hedonic impact is generated by hedonic hotspot circuits in accumbens-pallidal-brainstem; ‘wanting’ or incentive salience depends heavily on mesolimbic dopamine projections to accumbens-striatum and related corticolimbic circuits, cognitive goal values of tasty rewards may involve orbitofrontal cortex, etc. Most reward components have both explicit (conscious) and implicit (unconscious) forms, which also can be measured in different ways and which may differ in neural substrates (e.g., cortical versus subcortical circuit weighting). Modified from [199].
4.1. Reward dysfunction as cause
First, it is possible that some aspects of brain reward function may go wrong and actually cause an eating disorder. Foods might become hedonically ‘liked’ too much or too little via reward dysfunction. For example, pathological over-activation of the opioid or endocannabinoid hedonic hotspots in nucleus accumbens and ventral pallidum might cause enhanced ‘liking’ reaction to taste pleasure in some individuals. An endogenously produced increase in opioid tone there could in principle magnify the hedonic impact of foods, making an individual ‘like’ food more than other people, and ‘want’ to eat more. Conversely, a suppressive form of hotspot dysfunction might reduce ‘liking’ or even create ‘disliking’ for a normally palatable food.
Or incentive salience ‘wanting’ to eat might detach from normal close association with hedonic ‘liking’, leading to changes in motivated food consumption that are no longer hedonically driven. Activation of mesolimbic dopamine mechanisms of incentive salience, or even opioid ‘wanting’ circuits outside the hedonic hotspots, could cause ‘wanting’ without ‘liking’ similar to the animal studies described above. If eating disorders involve a pathology specifically in incentive salience ‘wanting’, such an individual could ‘want’ to eat food that they cognitively do not want to eat at all, and without enhancement of ‘liking’. In such cases, the sight, smell, or vivid imagination of food could trigger a compulsive urge to eat, even though the person would not expect it to be very pleasurable, nor find the actual experience very pleasurable in the end. Neural sensitization of incentive salience systems, if it truly happens in any eating disorder, might be one way by which excessive ‘wanting’ to eat could generate excessive food intake. Or yet again, suppression of positive hedonic reward systems or activation of dysphoric stress systems might prompt persistent attempts to self-medicate by eating palatable food. All of these possibilities have been suggested at one time or another. Each of them deserves consideration because different answers might apply to different disorders.
4.2. Passively distorted reward function as consequence
As a second category of possibilities, brain reward systems might remain intrinsically normal and have no essential pathology in eating disorders, but still become distorted in function as a passive secondary consequence of disordered intake. In that case, brain systems of ‘liking’ and ‘wanting’ might well attempt to function normally. The abnormal feedback from physiological signals that are altered by binges of eating or by periods of anorexia might induce reward dysfunction as a consequence of the behavioral disorder that arose from other causes. This would provide a potential red herring to researchers for causes of the eating disorder, because brain abnormalities might appear as neural markers for a particular disorder, but be mistaken as causes when they were actually consequences. However, it might still provide a window of opportunity for pharmacological treatments that aimed to correct eating behavior in part by modulating reward function back to a normal range.
4.3. Normal resilience in brain reward
Third, it is possible that most aspects of brain reward systems will function even more normally than suggested by the passively distorted consequence model above. Many compensatory changes can take place in response to physiological alterations, to oppose them via homeostatic or negative feedback corrections. The final consequence of those compensations might restore normality to brain reward functions. In such cases, the causes of eating disorder might then be found to lie completely outside brain reward functions. Indeed, brain reward functions will persist largely normally, and may even serve as aids to eventually help spontaneously normalize eating behavior even without treatment.
The answer to which of these alternative possibilities is best may well vary from case to case. Different eating disorders may require different answers. Perhaps even different individuals with the ‘same’ disorder will involve different answers, at least if there are distinct subtypes within the major types of eating disorder.
4.4. Practical consequences of theoretical possibilities
It is important to strive toward discovering which answers are most correct for particular disorders or subtypes, because those answers carry implications for what treatment strategy might be best. For example, should one try to restore normal eating by reversing brain reward dysfunction via medications to correct the underlying problem? That would be appropriate if reward dysfunction is the underlying cause.
Or should one use drugs instead only as compensating medications, not cures? Such a medication might aim to boost aspects of brain reward function and so correct eating, even though it may not address the original underlying cause? For example, just as aspirin often helps treat pain, even though the original cause of pain was never a deficit in endogenous aspirin, so a medication that altered reward systems might still help to oppose whatever original underlying factors are altering eating, even though it will not reverse those causal factors.
Or instead should treatment be focused entirely on separate brain or peripheral targets that are unrelated to food reward? That might be the best choice if brain reward systems simply remain normal in all cases of eating disorders, and thus perhaps essentially irrelevant to the expression of pathological eating behavior.
Placing these alternatives side by side helps illustrate that there are therapeutic implications that would follow from a better understanding of brain reward systems. Only if we know how food reward is processed normally in the brain will we be able to recognize pathology in brain reward function. And only if we can recognize reward pathology when it occurs will we be able to judge which of the possibilities above best applies to a particular eating disorder.
4.5. Addictions and incentive sensitization
Perhaps a bit more should be said about the possibility of excessive ‘wanting’ without commensurate ‘liking’. Could over-activation of ‘wanting’ mechanisms in certain individuals lead to actual addiction to food and over-eating similar to the compulsive pursuit of drugs in drug addiction? For some human drug addicts, real-life ‘wanting’ without ‘liking’ may occur due to long-lasting sensitization of their brain mesolimbic systems induced by repeated binging on heroin, cocaine or related drugs. Addicts sometimes take drugs compulsively even when they do not derive much pleasure from them [8,128]. For example, nicotine fails to produce great sensory pleasure in many people, but still can be quite addictive even in those cases.
In early 1990s, Terry Robinson and I proposed the incentive-sensitization theory of addiction to explain such compulsive ‘wanting’ by combining incentive salience and neural sensitization concepts [9,22]. The theory does not deny that drug pleasure, withdrawal, or habits are all reasons people sometimes take drugs, but suggests that something else, sensitized ‘wanting’, may be needed in order to understand why addiction becomes so motivationally compulsive and long-lasting.
Many addictive drugs cause neural sensitization in the brain mesocorticolimbic systems (e.g., cocaine, heroin, amphetamine, alcohol, nicotine). Sensitization means that the brain system can be triggered into abnormally high levels of activation by drugs or related stimuli. Sensitization is nearly the opposite of drug tolerance. Different processes within the same brain systems can simultaneously instantiate both sensitization (e.g., via increase in dopamine release) and tolerance (e.g., via decrease in dopamine receptors) [9,22,111,174]. However, tolerance mechanisms usually recover within days to weeks once drugs are given up, whereas neural sensitization can last for years. If the incentive-sensitization theory is true for drug addiction, it helps explain why addicts may sometimes even ‘want’ to take drugs that they do not particularly ‘like’. The long-lasting nature of neural sensitization may also help explain why recovered addicts, who have been drug-free and out of withdrawal for months or years, are still sometimes liable to relapse back into addiction even if not expecting to gain much pleasure from their relapse.
Sensitization of incentive salience does not mean that addicts ‘want’ all rewards more in a general fashion. ‘Wanting’ increases instead are highly specific to particular rewards and particular moments, often linked to encounters with cues for the ‘wanted’ reward [19,175]. This directional specificity may relate to why a drug addict particularly ‘wants’ drug, whereas someone with an eating disorder might particularly ‘want’ food, especially upon encounters with cues for the person's most ‘wanted’ reward.
4.6. Is there a neural sensitization role in food addictions?
Could incentive-sensitization apply to food addictions too? Several investigators have suggested that sensitization-like changes in brain systems are indeed produced by exposure to certain regimens of food and restriction that model oscillations between dieting and binging on palatable foods [176–183]. Their evidence is that when rats are given a number of brief chances to consume sucrose (sucrose binges) a number of accumulating sensitization-like changes are sometimes seen, especially when binges are separated by periods of food restriction: increasing propensity to over-consume when allowed, an enduring enhanced neural response to the presentation of food reward and cues, and an over-response to the psychostimulant effects of drugs such as amphetamine (a typical behavioral marker of drug-induced neural sensitization, which suggests a common underlying mechanism). Conversely, drug-induced sensitization of brain mesolimbic systems creates over-responsiveness to cues for sugar rewards in behavioral ‘wanting’ (cue-triggered peaks in lever pressing for sugar) and neural signals carrying incentive salience [19,184], and mesolimbic sensitization can produce increases in food intake [175,185].
If brain mesolimbic sensitization caused by binge eating truly exists, it gives a bit more reality to the possibility of food addictions. However, some caution may be in order before concluding that food binging creates limbic sensitization of ‘wanting’ similar to drug addiction. There are several alternative explanations for some of the evidence, which could interact with sensitization or perhaps even masquerade as limbic sensitization under some conditions. For example, repeated binging on a palatable food is likely to induce strong Pavlovian conditioning, creating strong conditioned incentive stimuli. Hunger itself also promotes mesolimbic activation in response to reward under some conditions [103,186–190].During normal hunger, sucrose tastes more pleasant than when one is full (alliesthesia) [191] and foods of all sorts become more motivating as incentives. Individuals who binge when hungry should establish even more intense ‘wanting’ cues, even without any sensitization. Finally, evolutionary psychologists might suggest that brains would be well adapted to naturally increase the propensity to overeat when-ever possible if faced with an environment of scarce resources, a situation mimicked by intermittent deprivation. These factors could snowball together to increase intake, and the resulting picture might look a bit like sensitization, without actually being it.
This is not to discount the possibility that real sensitization might still occur induced by diet-binge cycles or similar exposure regimens, nor to deny that the studies mentioned above might be examples of food incentive-sensitization. Sensitization-like states do indeed seem to be implicated by certain types of physiological deprivation regimens [192,193]. It only means that caution may be needed going forward. Otherwise we could be fooled into thinking sensitization has occurred when it has not, and be led to posit ‘food addiction’ when not really necessary.
4.7. What happens in actual human eating disorders
Whether actual obesity or human eating disorders such as or anorexia nervosa or binge eating in bulimia involve abnormal ‘liking’ or ‘wanting’ is an empirical question to be answered by studies of people with those conditions. The question has begun to receive thoughtful attention from a number of investigators [157,161,163,194]. At present, the data is still not entirely clear, and sometimes even a bit contradictory. Most fundamentally, there is still debate about whether food addictions really exist [169–171].
Still, distortions of reward could conceivably contribute to some eating disorders. In principle, ‘liking’ might be altered in some individuals. In human obesity, some individuals who are obese have some-times been reported to give higher pleasantness ratings to palatable foods than other individuals [195,196]. However, when people merely tasted and spit the foods in a recent ‘sham feeding’ study, no difference was found in wanting or liking ratings between obese and other individuals [197].
Alternatively, ‘wanting’ might dissociate via separate alteration. Food ‘liking’ and ‘wanting’ can dissociate somewhat even in normal situations, which eating disorders might exaggerate. For example, humans who eat repeated bits of chocolate to satiation report stronger declines in ratings of wanting the final bit of chocolate than in ratings of liking it [35] (and higher malleability of wanting than liking also seems consistent with animal studies of alliesthesia) [198].
5. Conclusion
For most people, eating patterns and body weights remain within normally prescribed bounds. Perhaps it is the prevalence of normal body weights, rather than obesity, that should be most surprising in affluent modern societies where tasty foods abound. As is often pointed out, brain mechanisms for food reward and appetite evolved under pressures to protect us from scarcity. As a result, overeating in the face of present abundance could be an understandable overshoot inherited from our evolutionary past. Indeed, facing modern temptations, it is impressive how many people remain in normal weight range today.
When eating patterns and body weight do diverge from the norm, questions arise concerning the involvement of food reward systems in the brain. All eating patterns are controlled intimately by brain mechanisms of food reward, whether those mechanisms operate in normal mode or abnormal modes. A primary signpost to help guide future thinking is to know whether any pathological patterns of eating are caused by identifiable pathologies in brain reward function. Can distorted patterns of eating be corrected by medications that alter brain reward mechanisms? Or are the causes of eating disorders essentially independent of brain reward systems? These remain questions to guide future research on how brain substrates of food reward relate to eating disorders.
Supplementary Material
Acknowledgements
I thank Eric Jackson and anonymous reviewers for helpful comments on an earlier version of the manuscript. This paper is based on a Mars Lecture given to the Society for the Study of Ingestive Behavior Conference in Paris in July 2008 and some parts have been adapted from a previous chapter. I am grateful to the SSIB organizers and the editors of this issue for the invitation to contribute. Research from my laboratory described here was supported by grants from the NIH (DA015188 and MH63649).
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.physbeh.2009.02.044.
References
- 1.Berridge KC, Kringelbach ML. Affective neuroscience of pleasure: reward in humans and animals. Psychopharmacology (Berl) 2008;199:457–480. doi: 10.1007/s00213-008-1099-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.James W. What is an emotion. Mind. 1884;9:188–205. [Google Scholar]
- 3.Kringelbach ML, Berridge KC, editors. Pleasures of the brain. Oxford: Oxford University Press; in press. [Google Scholar]
- 4.Garcia J, Lasiter PS, Bermudez-Rattoni F, Deems DA. A general theory of aversion learning. Ann N Y Acad Sci. 1985;443:8–21. doi: 10.1111/j.1749-6632.1985.tb27060.x. [DOI] [PubMed] [Google Scholar]
- 5.Reilly S, Schachtman TR, editors. Conditioned taste aversion: behavioral and neural processes. New York: Oxford University Press; 2009. [Google Scholar]
- 6.Rozin P. Disgust. In: Lewis M, Haviland-Jones JM, editors. Handbook of emotions. New York: Guilford; 2000. pp. 637–653. [Google Scholar]
- 7.Berridge KC, Robinson TE. What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res Rev. 1998;28:309–369. doi: 10.1016/s0165-0173(98)00019-8. [DOI] [PubMed] [Google Scholar]
- 8.Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005;8:1481–1489. doi: 10.1038/nn1579. [DOI] [PubMed] [Google Scholar]
- 9.Robinson TE, Berridge KC. Addiction. Annu Rev Psychol. 2003;54:25–53. doi: 10.1146/annurev.psych.54.101601.145237. [DOI] [PubMed] [Google Scholar]
- 10.Salamone JD, Correa M. Motivational views of reinforcement: implications for understanding the behavioral functions of nucleus accumbens dopamine. Behav Brain Res. 2002;137:3–25. doi: 10.1016/s0166-4328(02)00282-6. [DOI] [PubMed] [Google Scholar]
- 11.Pelchat ML, Johnson A, Chan R, Valdez J, Ragland JD. Images of desire: food-craving activation during fMRI. Neuroimage. 2004;23:1486–1493. doi: 10.1016/j.neuroimage.2004.08.023. [DOI] [PubMed] [Google Scholar]
- 12.Flagel SB, Akil H, Robinson TE. Individual differences in the attribution of incentive salience to reward-related cues: implications for addiction. Neuropharmacology. 2008 doi: 10.1016/j.neuropharm.2008.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jenkins HM, Moore BR. The form of the auto-shaped response with food or water reinforcers. J Exp Anal Behav. 1973;20:163–181. doi: 10.1901/jeab.1973.20-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahler SV, Berridge KC. Which cue to ‘want?’ Central amygdala opioid activation enhances and focuses incentive salience on a prepotent reward cue. Soc Neurosci Abstr. 2008 doi: 10.1523/JNEUROSCI.3875-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tomie A. Locating reward cue at response manipulandum(CAM) induces symptoms of drug abuse. Neurosci Biobehav Rev. 1996;20:31. doi: 10.1016/0149-7634(95)00023-2. [DOI] [PubMed] [Google Scholar]
- 16.Berridge KC. Reward learning: reinforcement, incentives, and expectations. In: Medin DL, editor. The psychology of learning and motivation. N.Y: Academic Press; 2001. pp. 223–278. [Google Scholar]
- 17.Berridge KC, Winkielman P. What is an unconscious emotion? (The case for unconscious “liking”) Cogn Emot. 2003;17:181–211. doi: 10.1080/02699930302289. [DOI] [PubMed] [Google Scholar]
- 18.Winkielman P, Berridge KC, Wilbarger JL. Unconscious affective reactions to masked happy versus angry faces influence consumption behavior and judgments of value. Pers Soc Psychol Bull. 2005;31:121–135. doi: 10.1177/0146167204271309. [DOI] [PubMed] [Google Scholar]
- 19.Tindell AJ, Berridge KC, Zhang J, Peciña S, Aldridge JW. Ventral pallidal neurons code incentive motivation: amplification by mesolimbic sensitization and amphetamine. Eur J Neurosci. 2005;22:2617–2634. doi: 10.1111/j.1460-9568.2005.04411.x. [DOI] [PubMed] [Google Scholar]
- 20.Wyvell CL, Berridge KC. Intra-accumbens amphetamine increases the conditioned incentive salience of sucrose reward: enhancement of reward “wanting” without enhanced “liking” or response reinforcement. J Neurosci. 2000;20:8122–8130. doi: 10.1523/JNEUROSCI.20-21-08122.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berridge KC, Aldridge JW. Decision utility, the brain and pursuit of hedonic goals. Soc Cogn. 2008;26:621–646. doi: 10.1521/soco.2008.26.5.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robinson TE, Berridge KC. The neural basis of drug craving: an incentive-sensitization theory of addiction. Brain Res Rev. 1993;18:247–291. doi: 10.1016/0165-0173(93)90013-p. [DOI] [PubMed] [Google Scholar]
- 23.Dickinson A, Balleine B. Hedonics: The cognitive-motivational interface. In: Kringelbach ML, Berridge KC, editors. Pleasures of the brain. Oxford, U.K: Oxford University Press; in press. [Google Scholar]
- 24.Berns GS, McClure SM, Pagnoni G, Montague PR. Predictability modulates human brain response to reward. J Neurosci. 2001;21:2793–2798. doi: 10.1523/JNEUROSCI.21-08-02793.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cardinal RN, Parkinson JA, Hall J, Everitt BJ. Emotion and motivation: the role of the amygdala, ventral striatum, and prefrontal cortex. Neurosci Biobehav Rev. 2002;26:321–352. doi: 10.1016/s0149-7634(02)00007-6. [DOI] [PubMed] [Google Scholar]
- 26.Craig AD. How do you feel? Interoception: the sense of the physiological condition of the body. Nat Rev Neurosci. 2002;3:655–666. doi: 10.1038/nrn894. [DOI] [PubMed] [Google Scholar]
- 27.Kringelbach ML. Food for thought: hedonic experience beyond homeostasis in the human brain. Neuroscience. 2004;126:807–819. doi: 10.1016/j.neuroscience.2004.04.035. [DOI] [PubMed] [Google Scholar]
- 28.Kringelbach ML. The hedonic brain: a functional neuroanatomy of human pleasure. In: Kringelbach ML, Berridge KC, editors. Pleasures of the brain. Oxford, U.K: Oxford University Press; in press. [Google Scholar]
- 29.Kringelbach ML, de Araujo IE, Rolls ET. Taste-related activity in the human dorsolateral prefrontal cortex. Neuroimage. 2004;21:781–788. doi: 10.1016/j.neuroimage.2003.09.063. [DOI] [PubMed] [Google Scholar]
- 30.Levine AS, Kotz CM, Gosnell BA. Sugars: hedonic aspects, neuroregulation, and energy balance. Am J Clin Nutr. 2003;78:834S–842S. doi: 10.1093/ajcn/78.4.834S. [DOI] [PubMed] [Google Scholar]
- 31.O Doherty JP, Deichmann R, Critchley HD, Dolan RJ. Neural responses during anticipation of a primary taste reward. Neuron. 2002;33:815–826. doi: 10.1016/s0896-6273(02)00603-7. [DOI] [PubMed] [Google Scholar]
- 32.Rolls ET. Emotion explained. Oxford, New York: Oxford University Press; 2005. [Google Scholar]
- 33.Schultz W. Behavioral theories and the neurophysiology of reward. Annu Rev Psychol. 2006 doi: 10.1146/annurev.psych.56.091103.070229. [DOI] [PubMed] [Google Scholar]
- 34.Small D, Veldhuizen M. Human crossmodal studies of taste and smell. In: Kringelbach ML, Berridge KC, editors. Pleasures of the brain. Oxford, U.K: Oxford University Press; in press. [Google Scholar]
- 35.Small DM, Zatorre RJ, Dagher A, Evans AC, Jones-Gotman M. Changes in brain activity related to eating chocolate — from pleasure to aversion. Brain. 2001;124:1720–1733. doi: 10.1093/brain/124.9.1720. [DOI] [PubMed] [Google Scholar]
- 36.Volkow ND, Wang GJ, Fowler JS, Logan J, Jayne M, Franceschi D, et al. “Nonhedonic” food motivation in humans involves dopamine in the dorsal striatum and methylphenidate amplifies this effect. Synapse. 2002;44:175–180. doi: 10.1002/syn.10075. [DOI] [PubMed] [Google Scholar]
- 37.Wang GJ, Volkow ND, Telang F, Jayne M, Ma J, Rao M, et al. Exposure to appetitive food stimuli markedly activates the human brain. Neuroimage. 2004;21:1790–1797. doi: 10.1016/j.neuroimage.2003.11.026. [DOI] [PubMed] [Google Scholar]
- 38.Kringelbach ML. The human orbitofrontal cortex: linking reward to hedonic experience. Nat Rev Neurosci. 2005;6:691–702. doi: 10.1038/nrn1747. [DOI] [PubMed] [Google Scholar]
- 39.Grill HJ, Norgren R. The taste reactivity test. I. Mimetic responses to gustatory stimuli in neurologically normal rats. Brain Res. 1978;143:263–279. doi: 10.1016/0006-8993(78)90568-1. [DOI] [PubMed] [Google Scholar]
- 40.Pfaffmann C, Norgren R, Grill HJ. Sensory affect and motivation. Ann N Y Acad Sci. 1977;290:18–34. doi: 10.1111/j.1749-6632.1977.tb39713.x. [DOI] [PubMed] [Google Scholar]
- 41.Steiner JE. The gustofacial response: observation on normal and anencephalic newborn infants. Symp Oral Sens Percept. 1973;4:254–278. [PubMed] [Google Scholar]
- 42.Steiner JE, Glaser D, Hawilo ME, Berridge KC. Comparative expression of hedonic impact: affective reactions to taste by human infants and other primates. Neurosci Biobehav Rev. 2001;25:53–74. doi: 10.1016/s0149-7634(00)00051-8. [DOI] [PubMed] [Google Scholar]
- 43.Berridge KC. Measuring hedonic impact in animals and infants: microstructure of affective taste reactivity patterns. Neurosci Biobehav Rev. 2000;24:173–198. doi: 10.1016/s0149-7634(99)00072-x. [DOI] [PubMed] [Google Scholar]
- 44.Aldridge JW, Berridge KC. Neural coding of pleasure: “rose-tinted glasses” of the ventral pallidum. In: Kringelbach ML, Berridge KC, editors. Pleasures of the brain. Oxford: Oxford University Press; in press. [Google Scholar]
- 45.Baldo BA, Kelley AE. Discrete neurochemical coding of distinguishable motivational processes: insights from nucleus accumbens control of feeding. Psychopharmacology (Berl) 2007;191:439–459. doi: 10.1007/s00213-007-0741-z. [DOI] [PubMed] [Google Scholar]
- 46.Higgs S, Williams CM, Kirkham TC. Cannabinoid influences on palatability: micro-structural analysis of sucrose drinking after delta(9)-tetrahydrocannabinol, anandamide, 2-arachidonoyl glycerol and SR141716. Psychopharmacology (Berl) 2003;165:370–377. doi: 10.1007/s00213-002-1263-3. [DOI] [PubMed] [Google Scholar]
- 47.Leknes S, Tracey I. Pleasure and pain: masters of mankind. In: Kringelbach ML, Berridge KC, editors. Pleasures of the brain. Oxford, U.K: Oxford University Press; in press. [Google Scholar]
- 48.Levine AS, Billington CJ. Opioids as agents of reward-related feeding: a consideration of the evidence. Physiol Behav. 2004;82:57–61. doi: 10.1016/j.physbeh.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 49.Wise RA. Drive, incentive, and reinforcement: the antecedents and consequences of motivation. Nebr Symp Motiv. 2004;50:159–195. [PubMed] [Google Scholar]
- 50.Yeomans MR, Gray RW. Opioid peptides and the control of human ingestive behaviour. Neurosci Biobehav Rev. 2002;26:713–728. doi: 10.1016/s0149-7634(02)00041-6. [DOI] [PubMed] [Google Scholar]
- 51.Berridge KC. Pleasures of the brain. Brain Cogn. 2003;52:106–128. doi: 10.1016/s0278-2626(03)00014-9. [DOI] [PubMed] [Google Scholar]
- 52.Kelley AE, Baldo BA, Pratt WE. A proposed hypothalamic–thalamic–striatal axis for the integration of energy balance, arousal, and food reward. J Comp Neurol. 2005;493:72–85. doi: 10.1002/cne.20769. [DOI] [PubMed] [Google Scholar]
- 53.Peciña S, Berridge KC. Hedonic hot spot in nucleus accumbens shell: where do mu-opioids cause increased hedonic impact of sweetness? J Neurosci. 2005;25:11777–11786. doi: 10.1523/JNEUROSCI.2329-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Smith KS, Berridge KC. The ventral pallidum and hedonic reward: neurochemical maps of sucrose “liking” and food intake. J Neurosci. 2005;25:8637–8649. doi: 10.1523/JNEUROSCI.1902-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Smith KS, Tindell AJ, Aldridge JW, Berridge KC. Ventral pallidum roles in reward and motivation. Behav Brain Res. 2009;196:155–167. doi: 10.1016/j.bbr.2008.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Grill HJ, Kaplan JM. The neuroanatomical axis for control of energy balance. Front Neuroendocrinol. 2002;23:2–40. doi: 10.1006/frne.2001.0224. [DOI] [PubMed] [Google Scholar]
- 57.Grill HJ, Norgren R. The taste reactivity test. II. Mimetic responses to gustatory stimuli in chronic thalamic and chronic decerebrate rats. Brain Res. 1978;143:281–297. doi: 10.1016/0006-8993(78)90569-3. [DOI] [PubMed] [Google Scholar]
- 58.Higgs S, Cooper SJ. Microinjection of the benzodiazepine agonist midazolam into the parabrachial nucleus of the rat results in a hyperphagia. Appetite. 1994;23:307–308. [Google Scholar]
- 59.Pecina S, Berridge KC. Brainstem mediates diazepam enhancement of palatability and feeding: microinjections into fourth ventricle versus lateral ventricle. Brain Res. 1996;727:22–30. doi: 10.1016/0006-8993(96)00325-3. [DOI] [PubMed] [Google Scholar]
- 60.Soderpalm AH, Berridge KC. The hedonic impact and intake of food are increased by midazolam microinjection in the parabrachial nucleus. Brain Res. 2000;877:288–297. doi: 10.1016/s0006-8993(00)02691-3. [DOI] [PubMed] [Google Scholar]
- 61.Baird JP, Chung YN. Benzodiazepine modulation of gustatory coding in the parabrachial nucleus. Appetite. 2008;51:352. [Google Scholar]
- 62.Berridge KC. Brainstem systems mediate the enhancement of palatability by chlordiazepoxide. Brain Res. 1988;447:262–268. doi: 10.1016/0006-8993(88)91128-6. [DOI] [PubMed] [Google Scholar]
- 63.Cabanac M, Cabanac AJ, Parent A. The emergence of consciousness in phylogeny. Behav Brain Res. 2009;198:267–272. doi: 10.1016/j.bbr.2008.11.028. [DOI] [PubMed] [Google Scholar]
- 64.Hughlings Jackson J, editor. Selected writings of John Hughlings Jackson. London: Staples Press; 1958. [Google Scholar]
- 65.Barbano MF, Cador M. Opioids for hedonic experience and dopamine to get ready for it. Psychopharmacology (Berl) 2007;191:497–506. doi: 10.1007/s00213-006-0521-1. [DOI] [PubMed] [Google Scholar]
- 66.Cooper SJ. Endocannabinoids and food consumption: comparisons with benzodiazepine and opioid palatability-dependent appetite. Eur J Pharmacol. 2004;500:37–49. doi: 10.1016/j.ejphar.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 67.Dallman MF. Fast glucocorticoid feedback favors ‘the munchies’. Trends Endocrinol Metab. 2003;14:394–396. doi: 10.1016/j.tem.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 68.Jarrett MM, Limebeer CL, Parker LA. Effect of Delta9-tetrahydrocannabinol on sucrose palatability as measured by the taste reactivity test. Physiol Behav. 2005;86:475–479. doi: 10.1016/j.physbeh.2005.08.033. [DOI] [PubMed] [Google Scholar]
- 69.Kelley AE, Bakshi VP, Haber SN, Steininger TL, Will MJ, Zhang M. Opioid modulation of taste hedonics within the ventral striatum. Physiol Behav. 2002;76:365–377. doi: 10.1016/s0031-9384(02)00751-5. [DOI] [PubMed] [Google Scholar]
- 70.Kirkham TC. Endocannabinoids in the regulation of appetite and body weight. Behav Pharmacol. 2005;16:297–313. doi: 10.1097/00008877-200509000-00004. [DOI] [PubMed] [Google Scholar]
- 71.Kirkham TC, Williams CM. Endogenous cannabinoids and appetite. Nutr Res Rev. 2001;14:65–86. doi: 10.1079/NRR200118. [DOI] [PubMed] [Google Scholar]
- 72.Le Magnen J, Marfaing-Jallat P, Miceli D, Devos M. Pain modulating and reward systems: a single brain mechanism? Pharmacol Biochem Behav. 1980;12:729–733. doi: 10.1016/0091-3057(80)90157-4. [DOI] [PubMed] [Google Scholar]
- 73.Panksepp J. The neurochemistry of behavior. Annu Rev Psychol. 1986;37:77–107. doi: 10.1146/annurev.ps.37.020186.000453. [DOI] [PubMed] [Google Scholar]
- 74.Sharkey KA, Pittman QJ. Central and peripheral signaling mechanisms involved in endocannabinoid regulation of feeding: a perspective on the munchies. Sci STKE 2005. 2005:pe15. doi: 10.1126/stke.2772005pe15. [DOI] [PubMed] [Google Scholar]
- 75.Pecina S. Opioid reward ‘liking’ and ‘wanting’ in the nucleus accumbens. Physiol Behav. 2008;94:675–680. doi: 10.1016/j.physbeh.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 76.Peciña S, Smith KS, Berridge KC. Hedonic hot spots in the brain. Neuroscientist. 2006;12:500–511. doi: 10.1177/1073858406293154. [DOI] [PubMed] [Google Scholar]
- 77.Mahler SV, Smith KS, Berridge KC. Endocannabinoid hedonic hotspot for sensory pleasure: anandamide in nucleus accumbens shell enhances ‘liking’ of a sweet reward. Neuropsychopharmacology. 2007;32:2267–2278. doi: 10.1038/sj.npp.1301376. [DOI] [PubMed] [Google Scholar]
- 78.Cooper SJ, Higgs S. Neuropharmacology of appetite and taste preferences. In: Legg CR, Booth DA, editors. Appetite: neural and behavioural bases. New York: Oxford University Press; 1994. pp. 212–242. [Google Scholar]
- 79.Kelley AE. Ventral striatal control of appetitive motivation: role in ingestive behavior and reward-related learning. Neurosci Biobehav Rev. 2004;27:765–776. doi: 10.1016/j.neubiorev.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 80.Smith KS, Berridge KC. Opioid limbic circuit for reward: interaction between hedonic hotspots of nucleus accumbens and ventral pallidum. J Neurosci. 2007;27:1594–1605. doi: 10.1523/JNEUROSCI.4205-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Heimer L, Van Hoesen GW. The limbic lobe and its output channels: implications for emotional functions and adaptive behavior. Neurosci Biobehav Rev. 2006;30:126–147. doi: 10.1016/j.neubiorev.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 82.Morgane PJ, Mokler DJ. The limbic brain: continuing resolution. Neurosci Biobehav Rev. 2006;30:119–125. doi: 10.1016/j.neubiorev.2005.04.020. [DOI] [PubMed] [Google Scholar]
- 83.Sarter M, Parikh V. Choline transporters, cholinergic transmission and cognition. Nat Rev Neurosci. 2005;6:48–56. doi: 10.1038/nrn1588. [DOI] [PubMed] [Google Scholar]
- 84.Swanson LW. Anatomy of the soul as reflected in the cerebral hemispheres: neural circuits underlying voluntary control of basic motivated behaviors. J Comp Neurol. 2005;493:122–131. doi: 10.1002/cne.20733. [DOI] [PubMed] [Google Scholar]
- 85.Zahm DS. The evolving theory of basal forebrain functional–anatomical ‘macrosystems’. Neurosci Biobehav Rev. 2006;30:148–172. doi: 10.1016/j.neubiorev.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 86.Smith KS, Mahler SV, Pecina S, Berridge KC. Hedonic hotspots: generating sensory pleasure in the brain. In: Kringelbach M, Berridge KC, editors. Pleasures of the brain. Oxford, U.K: Oxford University Press; in press. [Google Scholar]
- 87.Cromwell HC, Berridge KC. Where does damage lead to enhanced food aversion: the ventral pallidum/substantia innominata or lateral hypothalamus? Brain Res. 1993;624:1–10. doi: 10.1016/0006-8993(93)90053-p. [DOI] [PubMed] [Google Scholar]
- 88.Teitelbaum P, Epstein AN. The lateral hypothalamic syndrome: recovery of feeding and drinking after lateral hypothalamic lesions. Psychol Rev. 1962;69:74–90. doi: 10.1037/h0039285. [DOI] [PubMed] [Google Scholar]
- 89.Winn P. The lateral hypothalamus and motivated behavior: an old syndrome reassessed and a new perspective gained. Curr Dir Psychol. 1995;4:182–187. [Google Scholar]
- 90.Schallert T, Whishaw IQ. Two types of aphagia and two types of sensorimotor impairment after lateral hypothalamic lesions: observations in normal weight, dieted, and fattened rats. J Comp Physiol Psychol. 1978;92:720–741. doi: 10.1037/h0077504. [DOI] [PubMed] [Google Scholar]
- 91.Stellar JR, Brooks FH, Mills LE. Approach and withdrawal analysis of the effects of hypothalamic stimulation and lesions in rats. J Comp Physiol Psychol. 1979;93:446–466. doi: 10.1037/h0077590. [DOI] [PubMed] [Google Scholar]
- 92.Beaver JD, Lawrence AD, van Ditzhuijzen J, Davis MH, Woods A, Calder AJ. Individual differences in reward drive predict neural responses to images of food. J Neurosci. 2006;26:5160–5166. doi: 10.1523/JNEUROSCI.0350-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Calder AJ, Beaver JD, Davis MH, van Ditzhuijzen J, Keane J, Lawrence AD. Disgust sensitivity predicts the insula and pallidal response to pictures of disgusting foods. Eur J Neurosci. 2007;25:3422–3428. doi: 10.1111/j.1460-9568.2007.05604.x. [DOI] [PubMed] [Google Scholar]
- 94.Johnson PI, Stellar JR, Paul AD. Regional reward differences within the ventral pallidum are revealed by microinjections of a mu opiate receptor agonist. Neuropharmacology. 1993;32:1305–1314. doi: 10.1016/0028-3908(93)90025-x. [DOI] [PubMed] [Google Scholar]
- 95.Johnson PI, Parente MA, Stellar JR. NMDA-induced lesions of the nucleus accumbens or the ventral pallidum increase the rewarding efficacy of food to deprived rats. Brain Res. 1996;722:109–117. doi: 10.1016/0006-8993(96)00202-8. [DOI] [PubMed] [Google Scholar]
- 96.McFarland K, Davidge SB, Lapish CC, Kalivas PW. Limbic and motor circuitry underlying footshock-induced reinstatement of cocaine-seeking behavior. J Neurosci. 2004;24:1551–1560. doi: 10.1523/JNEUROSCI.4177-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Shimura T, Imaoka H, Yamamoto T. Neurochemical modulation of ingestive behavior in the ventral pallidum. Eur J Neurosci. 2006;23:1596–1604. doi: 10.1111/j.1460-9568.2006.04689.x. [DOI] [PubMed] [Google Scholar]
- 98.Zubieta JK, Ketter TA, Bueller JA, Xu YJ, Kilbourn MR, Young EA, et al. Regulation of human affective responses by anterior cingulate and limbic mu-opioid neurotransmission. Arch Gen Psychiatry. 2003;60:1145–1153. doi: 10.1001/archpsyc.60.11.1145. [DOI] [PubMed] [Google Scholar]
- 99.Aldridge JW, Berridge KC, Herman M, Zimmer L. Neuronal coding of serial order: syntax of grooming in the neostriatum. Psychol Sci. 1993;4:391–395. [Google Scholar]
- 100.Tindell AJ, Berridge KC, Aldridge JW. Ventral pallidal representation of Pavlovian cues and reward: population and rate codes. J Neurosci. 2004;24:1058–1069. doi: 10.1523/JNEUROSCI.1437-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Tindell AJ, Smith KS, Pecina S, Berridge KC, Aldridge JW. Ventral pallidum firing codes hedonic reward: when a bad taste turns good. J Neurophysiol. 2006;96:2399–2409. doi: 10.1152/jn.00576.2006. [DOI] [PubMed] [Google Scholar]
- 102.Ikemoto S. Dopamine reward circuitry: two projection systems from the ventral midbrain to the nucleus accumbens-olfactory tubercle complex. Brain Res Rev. 2007;56:27–78. doi: 10.1016/j.brainresrev.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ahn S, Phillips AG. Dopaminergic correlates of sensory-specific satiety in the medial prefrontal cortex and nucleus accumbens of the rat. J Neurosci. 1999;19:B1–B6. doi: 10.1523/JNEUROSCI.19-19-j0003.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Di Chiara G. Nucleus accumbens shell and core dopamine: differential role in behavior and addiction. Behav Brain Res. 2002;137:75–114. doi: 10.1016/s0166-4328(02)00286-3. [DOI] [PubMed] [Google Scholar]
- 105.Hajnal A, Norgren R. Taste pathways that mediate accumbens dopamine release by sapid sucrose. Physiol Behav. 2005;84:363–369. doi: 10.1016/j.physbeh.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 106.Montague PR, Hyman SE, Cohen JD. Computational roles for dopamine in behavioural control. Nature. 2004;431:760–767. doi: 10.1038/nature03015. [DOI] [PubMed] [Google Scholar]
- 107.Norgren R, Hajnal A, Mungarndee SS. Gustatory reward and the nucleus accumbens. Physiol Behav. 2006;89:531–535. doi: 10.1016/j.physbeh.2006.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Roitman MF, Stuber GD, Phillips PEM, Wightman RM, Carelli RM. Dopamine operates as a subsecond modulator of food seeking. J Neurosci. 2004;24:1265–1271. doi: 10.1523/JNEUROSCI.3823-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Roitman MF, Wheeler RA, Wightman RM, Carelli RM. Real-time chemical responses in the nucleus accumbens differentiate rewarding and aversive stimuli. Nat Neurosci. 2008;11:1376–1377. doi: 10.1038/nn.2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Small DM, Jones-Gotman M, Dagher A. Feeding-induced dopamine release in dorsal striatum correlates with meal pleasantness ratings in healthy human volunteers. Neuroimage. 2003;19:1709–1715. doi: 10.1016/s1053-8119(03)00253-2. [DOI] [PubMed] [Google Scholar]
- 111.Koob GF, Le Moal M. Neurobiology of addiction. New York: Academic Press; 2006. [Google Scholar]
- 112.Dickinson A, Smith J, Mirenowicz J. Dissociation of Pavlovian and instrumental incentive learning under dopamine antagonists. Behav Neurosci. 2000;114:468–483. doi: 10.1037//0735-7044.114.3.468. [DOI] [PubMed] [Google Scholar]
- 113.Berridge KC. The debate over dopamine's role in reward: the case for incentive salience. Psychopharmacology (Berl) 2007;191:391–431. doi: 10.1007/s00213-006-0578-x. [DOI] [PubMed] [Google Scholar]
- 114.Niv Y, Daw ND, Joel D, Dayan P. Tonic dopamine: opportunity costs and the control of response vigor. Psychopharmacology (Berl) 2007;191:507–520. doi: 10.1007/s00213-006-0502-4. [DOI] [PubMed] [Google Scholar]
- 115.Robbins TW, Everitt BJ. A role for mesencephalic dopamine in activation: commentary on Berridge (2006) Psychopharmacology (Berl) 2007;191:433–437. doi: 10.1007/s00213-006-0528-7. [DOI] [PubMed] [Google Scholar]
- 116.Salamone JD. Functions of mesolimbic dopamine: changing concepts and shifting paradigms. Psychopharmacology (Berl) 2007;191:389. doi: 10.1007/s00213-006-0623-9. [DOI] [PubMed] [Google Scholar]
- 117.Daw ND, Niv Y, Dayan P. Uncertainty-based competition between prefrontal and dorsolateral striatal systems for behavioral control. Nat Neurosci. 2005;8:1704–1711. doi: 10.1038/nn1560. [DOI] [PubMed] [Google Scholar]
- 118.Niv Y, Joel D, Dayan P. A normative perspective on motivation. Trends Cogn Sci. 2006;10:375–381. doi: 10.1016/j.tics.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 119.Everitt BJ, Belin D, Economidou D, Pelloux Y, Dalley JW, Robbins TW. Review. Neural mechanisms underlying the vulnerability to develop compulsive drug-seeking habits and addiction. Philos Trans R Soc Lond B Biol Sci. 2008;363:3125–3135. doi: 10.1098/rstb.2008.0089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wise RA. Role of brain dopamine in food reward and reinforcement. Philos Trans R Soc Lond B Biol Sci. 2006;361:1149–1158. doi: 10.1098/rstb.2006.1854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wise RA. The anhedonia hypothesis: Mark III. Behav Brain Sci. 1985;8:178–186. [Google Scholar]
- 122.Wang GJ, Volkow ND, Logan J, Pappas NR, Wong CT, Zhu W, et al. Brain dopamine and obesity. Lancet. 2001;357:354–357. doi: 10.1016/s0140-6736(00)03643-6. [DOI] [PubMed] [Google Scholar]
- 123.Wang GJ, Volkow ND, Thanos PK, Fowler JS. Similarity between obesity and drug addiction as assessed by neurofunctional imaging: a concept review. J Addict Dis. 2004;23:39–53. doi: 10.1300/J069v23n03_04. [DOI] [PubMed] [Google Scholar]
- 124.Dickinson A, Balleine B. The role of learning in the operation of motivational systems. In: Gallistel CR, editor. Stevens' handbook of experimental psychology: learning, motivation, and emotion. New York: Wiley and Sons; 2002. pp. 497–534. [Google Scholar]
- 125.Grigson PS. Like drugs for chocolate: separate rewards modulated by common mechanisms? Physiol Behav. 2002;76:389–395. doi: 10.1016/s0031-9384(02)00758-8. [DOI] [PubMed] [Google Scholar]
- 126.Kelley AE, Baldo BA, Pratt WE, Will MJ. Corticostriatal-hypothalamic circuitry and food motivation: integration of energy, action and reward. Physiol Behav. 2005;86:773–795. doi: 10.1016/j.physbeh.2005.08.066. [DOI] [PubMed] [Google Scholar]
- 127.Seeman P, Weinshenker D, Quirion R, Srivastava LK, Bhardwaj SK, Grandy DK, et al. Dopamine supersensitivity correlates with D2High states, implying many paths to psychosis. Proc Natl Acad Sci U S A. 2005;102:3513–3518. doi: 10.1073/pnas.0409766102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Robinson TE, Berridge KC. Review. The incentive sensitization theory of addiction: some current issues. Philos Trans R Soc Lond B Biol Sci. 2008;363:3137–3146. doi: 10.1098/rstb.2008.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Cannon CM, Palmiter RD. Reward without dopamine. J Neurosci. 2003;23:10827–10831. doi: 10.1523/JNEUROSCI.23-34-10827.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Robinson S, Sandstrom SM, Denenberg VH, Palmiter RD. Distinguishing whether dopamine regulates liking, wanting, and/or learning about rewards. Behav Neurosci. 2005;119:5–15. doi: 10.1037/0735-7044.119.1.5. [DOI] [PubMed] [Google Scholar]
- 131.Peciña S, Berridge KC, Parker LA. Pimozide does not shift palatability: separation of anhedonia from sensorimotor suppression by taste reactivity. Pharmacol Biochem Behav. 1997;58:801–811. doi: 10.1016/s0091-3057(97)00044-0. [DOI] [PubMed] [Google Scholar]
- 132.Peciña S, Cagniard B, Berridge KC, Aldridge JW, Zhuang X. Hyperdopaminergic mutant mice have higher “wanting” but not “liking” for sweet rewards. J Neurosci. 2003;23:9395–9402. doi: 10.1523/JNEUROSCI.23-28-09395.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Palmiter RD. Is dopamine a physiologically relevant mediator of feeding behavior? Trends Neurosci. 2007;30:375–381. doi: 10.1016/j.tins.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 134.Tindell AJ, Smith KS, Berridge KC, Aldridge JW. Ventral pallidal neurons integrate learning and physiological signals to code incentive salience of conditioned cues. Society for Neuroscience Conference; Washington, D.C. 2005. [Google Scholar]
- 135.Ahn S, Phillips AG. Modulation by central and basolateral amygdalar nuclei of dopaminergic correlates of feeding to satiety in the rat nucleus accumbens and medial prefrontal cortex. J Neurosci. 2002;22:10958–10965. doi: 10.1523/JNEUROSCI.22-24-10958.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Wilson C, Nomikos GG, Collu M, Fibiger HC. Dopaminergic correlates of motivated behavior: importance of drive. J Neurosci. 1995;15:5169–5178. doi: 10.1523/JNEUROSCI.15-07-05169.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Berridge KC. Motivation concepts in behavioral neuroscience. Physiol Behav. 2004;81:179–209. doi: 10.1016/j.physbeh.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 138.Bindra D. How adaptive behavior is produced: a perceptual-motivation alternative to response reinforcement. Behav Brain Sci. 1978;1:41–91. [Google Scholar]
- 139.Toates F. Motivational systems. Cambridge: Cambridge University Press; 1986. [Google Scholar]
- 140.Leyton M, Boileau I, Benkelfat C, Diksic M, Baker G, Dagher A. Amphetamine-induced increases in extracellular dopamine, drug wanting, and novelty seeking: a PET/[11C] raclopride study in healthy men. Neuropsychopharmacology. 2002;27:1027–1035. doi: 10.1016/S0893-133X(02)00366-4. [DOI] [PubMed] [Google Scholar]
- 141.Brauer LH, De Wit H. High dose pimozide does not block amphetamine-induced euphoria in normal volunteers. Pharmacol Biochem Behav. 1997;56:265–272. doi: 10.1016/s0091-3057(96)00240-7. [DOI] [PubMed] [Google Scholar]
- 142.Brauer LH, Goudie AJ, de Wit H. Dopamine ligands and the stimulus effects of amphetamine: animal models versus human laboratory data. Psychopharmacology(Berl) 1997;130:2–13. doi: 10.1007/s002130050207. [DOI] [PubMed] [Google Scholar]
- 143.Wachtel SR, Ortengren A, de Wit H. The effects of acute haloperidol or risperidone on subjective responses to methamphetamine in healthy volunteers. Drug Alcohol Depend. 2002;68:23–33. doi: 10.1016/s0376-8716(02)00104-7. [DOI] [PubMed] [Google Scholar]
- 144.Leyton M. The neurobiology of desire: dopamine and the regulation of mood and motivational states in humans. In: Kringelbach ML, Berridge KC, editors. Pleasures of the brain. Oxford, U.K: Oxford University Press; in press. [Google Scholar]
- 145.Shizgal P. Neural basis of utility estimation. Curr Opin Neurobiol. 1997;7:198–208. doi: 10.1016/s0959-4388(97)80008-6. [DOI] [PubMed] [Google Scholar]
- 146.Berridge KC, Schulkin J. Palatability shift of a salt-associated incentive during sodium depletion. Quarterly J Exp Psychol [b] 1989;41:121–138. [PubMed] [Google Scholar]
- 147.Berthoud HR, Morrison C. The brain, appetite, and obesity. Annu Rev Psychol. 2008;59:55–92. doi: 10.1146/annurev.psych.59.103006.093551. [DOI] [PubMed] [Google Scholar]
- 148.Cabanac M. The dialectics of pleasure. In: Kringelbach ML, Berridge KC, editors. Pleasures of the brain. Oxford, U.K: Oxford University Press; in press. [Google Scholar]
- 149.Cabanac M. Pleasure: the common currency. J Theor Biol. 1992;155:173–200. doi: 10.1016/s0022-5193(05)80594-6. [DOI] [PubMed] [Google Scholar]
- 150.Rozin P. Preadaptation and the puzzles and properties of pleasure. In: Kahneman D, Diener E, Schwarz N, editors. Well-being: the foundations of hedonic psychology. New York: Russell Sage Foundation; 1999. pp. 109–133. [Google Scholar]
- 151.Dallman MF, Pecoraro N, Akana SF, La Fleur SE, Gomez F, Houshyar H, et al. Chronic stress and obesity: a new view of “comfort food”. Proc Natl Acad Sci U S A. 2003;100:11696–11701. doi: 10.1073/pnas.1934666100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Dallman MF, Pecoraro NC, La Fleur SE, Warne JP, Ginsberg AB, Akana SF, et al. Glucocorticoids, chronic stress, and obesity. Prog Brain Res. 2006;153:75–105. doi: 10.1016/S0079-6123(06)53004-3. [DOI] [PubMed] [Google Scholar]
- 153.Koob G, Kreek MJ. Stress, dysregulation of drug reward pathways, and the transition to drug dependence. Am J Psychiatry. 2007;164:1149–1159. doi: 10.1176/appi.ajp.2007.05030503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Pecina S, Schulkin J, Berridge KC. Nucleus accumbens corticotropin-releasing factor increases cue-triggered motivation for sucrose reward: paradoxical positive incentive effects in stress? BMC Biol. 2006;4:8. doi: 10.1186/1741-7007-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Reynolds SM, Berridge KC. Emotional environments retune the valence of appetitive versus fearful functions in nucleus accumbens. Nat Neurosci. 2008;11:423–425. doi: 10.1038/nn2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Carr KD. Chronic food restriction: enhancing effects on drug reward and striatal cell signaling. Physiol Behav. 2007;91:459–472. doi: 10.1016/j.physbeh.2006.09.021. [DOI] [PubMed] [Google Scholar]
- 157.Finlayson G, King N, Blundell JE. Liking vs. wanting food: importance for human appetite control and weight regulation. Neurosci Biobehav Rev. 2007;31:987–1002. doi: 10.1016/j.neubiorev.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 158.Fulton S, Pissios P, Manchon R, Stiles L, Frank L, Pothos EN, et al. Leptin regulation of the mesoaccumbens dopamine pathway. Neuron. 2006;51:811–822. doi: 10.1016/j.neuron.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 159.Harris GC, Aston-Jones G. Arousal and reward: a dichotomy in orexin function. Trends Neurosci. 2006;29:571–577. doi: 10.1016/j.tins.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 160.Harris GC, Wimmer M, Aston-Jones G. A role for lateral hypothalamic orexin neurons in reward seeking. Nature. 2005;437:556–559. doi: 10.1038/nature04071. [DOI] [PubMed] [Google Scholar]
- 161.Mela DJ. Eating for pleasure or just wanting to eat? Reconsidering sensory hedonic responses as a driver of obesity. Appetite. 2006;47:10–17. doi: 10.1016/j.appet.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 162.Myers MG., Jr Metabolic sensing and regulation by the hypothalamus. Am J Physiol Endocrinol Metab. 2008;294:E809. doi: 10.1152/ajpendo.90282.2008. [DOI] [PubMed] [Google Scholar]
- 163.Robertson SA, Leinninger GM, Myers MG., Jr Molecular and neural mediators of leptin action. Physiol Behav. 2008;94:637–642. doi: 10.1016/j.physbeh.2008.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Zheng H, Berthoud HR. Eating for pleasure or calories. Curr Opin Pharmacol. 2007;7:607–612. doi: 10.1016/j.coph.2007.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Scammell TE, Saper CB. Orexin, drugs and motivated behaviors. Nat Neurosci. 2005;8:1286–1288. doi: 10.1038/nn1005-1286. [DOI] [PubMed] [Google Scholar]
- 166.Baldo BA, Gual-Bonilla L, Sijapati K, Daniel RA, Landry CF, Kelley AE. Activation of a subpopulation of orexin/hypocretin-containing hypothalamic neurons by GABAA receptor-mediated inhibition of the nucleus accumbens shell, but not by exposure to a novel environment. Eur J Neurosci. 2004;19:376–386. doi: 10.1111/j.1460-9568.2004.03093.x. [DOI] [PubMed] [Google Scholar]
- 167.Zheng HY, Corkern M, Stoyanova I, Patterson LM, Tian R, Berthoud HR. Peptides that regulate food intake — appetite-inducing accumbens manipulation activates hypothalamic orexin neurons and inhibits POMC neurons. Am J Physiol — Reg Int and Comp Physiol. 2003;284:R1436–R1444. doi: 10.1152/ajpregu.00781.2002. [DOI] [PubMed] [Google Scholar]
- 168.Zheng H, Patterson LM, Berthoud HR. Orexin signaling in the ventral tegmental area is required for high-fat appetite induced by opioid stimulation of the nucleus accumbens. J Neurosci. 2007;27:11075–11082. doi: 10.1523/JNEUROSCI.3542-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Ifland JR, Preuss HG, Marcus MT, Rourke KM, Taylor WC, Burau K, et al. Refined food addiction: a classic substance use disorder. Med Hypotheses. 2009;72(5):518–526. doi: 10.1016/j.mehy.2008.11.035. [DOI] [PubMed] [Google Scholar]
- 170.Pelchat ML. Food addiction in humans. J Nutr. 2009;139:620–622. doi: 10.3945/jn.108.097816. [DOI] [PubMed] [Google Scholar]
- 171.Rogers PJ, Smit HJ. Food craving and food “addiction”: a critical review of the evidence from a bio psychosocial perspective. Pharmacol Biochem Behav. 2000;66:3–14. doi: 10.1016/s0091-3057(00)00197-0. [DOI] [PubMed] [Google Scholar]
- 172.Faure A, Reynolds SM, Richard JM, Berridge KC. Mesolimbic dopamine in desire and dread: enabling motivation to be generated by localized glutamate disruptions in nucleus accumbens. J Neurosci. 2008;28:7184–7192. doi: 10.1523/JNEUROSCI.4961-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kapur S. Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. Am J Psychiatry. 2003;160:13–23. doi: 10.1176/appi.ajp.160.1.13. [DOI] [PubMed] [Google Scholar]
- 174.Vezina P. Sensitization of midbrain dopamine neuron reactivity and the self-administration of psychomotor stimulant drugs. Neurosci Biobehav Rev. 2004;27:827–839. doi: 10.1016/j.neubiorev.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 175.Nocjar C, Panksepp J. Chronic intermittent amphetamine pretreatment enhances future appetitive behavior for drug- and natural-reward: interaction with environmental variables. Behav Brain Res. 2002;128:189–203. doi: 10.1016/s0166-4328(01)00321-7. [DOI] [PubMed] [Google Scholar]
- 176.Avena NA, Hoebel BG. Amphetamine-sensitized rats show sugar-induced hyper-activity (cross-sensitization) and sugar hyperphagia. Pharmacol Biochem Behav. 2003;74:635–639. doi: 10.1016/s0091-3057(02)01050-x. [DOI] [PubMed] [Google Scholar]
- 177.Avena NM, Hoebel BG. A diet promoting sugar dependency causes behavioral cross-sensitization to a low dose of amphetamine. Neuroscience. 2003;122:17–20. doi: 10.1016/s0306-4522(03)00502-5. [DOI] [PubMed] [Google Scholar]
- 178.Bell SM, Stewart RB, Thompson SC, Meisch RA. Food-deprivation increases cocaine-induced conditioned place preference and locomotor activity in rats. Psychopharmacology (Berl) 1997;131:1–8. doi: 10.1007/s002130050258. [DOI] [PubMed] [Google Scholar]
- 179.Bello NT, Sweigart KL, Lakoski JM, Norgren R, Hajnal A. Restricted feeding with scheduled sucrose access results in an upregulation of the rat dopamine transporter. Am J Physiol Regul Integr Comp Physiol. 2003;284:R1260–R1268. doi: 10.1152/ajpregu.00716.2002. [DOI] [PubMed] [Google Scholar]
- 180.Carr KD. Augmentation of drug reward by chronic food restriction: behavioral evidence and underlying mechanisms. Physiol Behav. 2002;76:353–364. doi: 10.1016/s0031-9384(02)00759-x. [DOI] [PubMed] [Google Scholar]
- 181.Colantuoni C, Schwenker J, McCarthy J, Rada P, Ladenheim B, Cadet JL, et al. Excessive sugar intake alters binding to dopamine and mu-opioid receptors in the brain. Neuroreport. 2001;12:3549–3552. doi: 10.1097/00001756-200111160-00035. [DOI] [PubMed] [Google Scholar]
- 182.de Vaca SC, Carr KD. Food restriction enhances the central rewarding effect of abused drugs. J Neurosci. 1998;18:7502–7510. doi: 10.1523/JNEUROSCI.18-18-07502.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Gosnell BA. Sucrose intake enhances behavioral sensitization produced by cocaine. Brain Res. 2005;1031:194–201. doi: 10.1016/j.brainres.2004.10.037. [DOI] [PubMed] [Google Scholar]
- 184.Wyvell CL, Berridge KC. Incentive-sensitization by previous amphetamine exposure: Increased cue-triggered ‘wanting’ for sucrose reward. J Neurosci. 2001;21:7831–7840. doi: 10.1523/JNEUROSCI.21-19-07831.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Bakshi VP, Kelley AE. Sensitization and conditioning of feeding following multiple morphine microinjections into the nucleus accumbens. Brain Res. 1994;648:342–346. doi: 10.1016/0006-8993(94)91139-8. [DOI] [PubMed] [Google Scholar]
- 186.Carr KD, Cabeza de Vaca S, Sun Y, Chau LS. Reward-potentiating effects of D-1 dopamine receptor agonist and AMPAR GluR1 antagonist in nucleus accumbens shell and their modulation by food restriction. Psychopharmacology (Berl) 2008 doi: 10.1007/s00213-008-1355-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Hommel JD, Trinko R, Sears RM, Georgescu D, Liu ZW, Gao XB, et al. Leptin receptor signaling in midbrain dopamine neurons regulates feeding. Neuron. 2006;51:801–810. doi: 10.1016/j.neuron.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 188.Marinelli M, Rudick CN, Hu XT, White FJ. Excitability of dopamine neurons: modulation and physiological consequences. CNS Neurol Disord Drug Targets. 2006;5:79–97. doi: 10.2174/187152706784111542. [DOI] [PubMed] [Google Scholar]
- 189.Nader K, Bechara A, van der Kooy D. Neurobiological constraints on behavioral models of motivation. Annu Rev Psychol. 1997;48:85–114. doi: 10.1146/annurev.psych.48.1.85. [DOI] [PubMed] [Google Scholar]
- 190.Wilson C, Nomikos GG, Collu M, Fibiger HC. Dopaminergic correlates of motivated behavior: importance of drive. J Neurosci. 1995;15:5169–5178. doi: 10.1523/JNEUROSCI.15-07-05169.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Cabanac M. Physiological role of pleasure. Science. 1971;173:1103–1107. doi: 10.1126/science.173.4002.1103. [DOI] [PubMed] [Google Scholar]
- 192.Dietz DM, Curtis KS, Contreras RJ. Taste, salience, and increased NaCl ingestion after repeated sodium depletions. Chem Senses. 2005 doi: 10.1093/chemse/bjj003. [DOI] [PubMed] [Google Scholar]
- 193.Roitman MF, Na E, Anderson G, Jones TA, Bernstein IL. Induction of a salt appetite alters dendritic morphology in nucleus accumbens and sensitizes rats to amphetamine. J Neurosci. 2002 doi: 10.1523/JNEUROSCI.22-11-j0001.2002. 20026416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Finlayson G, King N, Blundell JE. Is it possible to dissociate ‘liking’ and ‘wanting’ for foods in humans? A novel experimental procedure. Physiol Behav. 2007;90:36–42. doi: 10.1016/j.physbeh.2006.08.020. [DOI] [PubMed] [Google Scholar]
- 195.Drewnowski A, Schwartz M. Invisible fats: sensory assessment of sugar/fat mixtures. Appetite. 1990;14:203–217. doi: 10.1016/0195-6663(90)90088-p. [DOI] [PubMed] [Google Scholar]
- 196.Salbe AD, DelParigi A, Pratley RE, Drewnowski A, Tataranni PA. Taste preferences and body weight changes in an obesity-prone population. Am J Clin Nutr. 2004;79:372–378. doi: 10.1093/ajcn/79.3.372. [DOI] [PubMed] [Google Scholar]
- 197.Klein DA, Schebendach JE, Brown AJ, Smith GP, Walsh BT. Modified sham feeding of sweet solutions in women with and without bulimia nervosa. Physiol Behav. 2009;96(1):44–50. doi: 10.1016/j.physbeh.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Berridge KC. Modulation of taste affect by hunger, caloric satiety, and sensory-specific satiety in the rat. Appetite. 1991;16:103–120. doi: 10.1016/0195-6663(91)90036-r. [DOI] [PubMed] [Google Scholar]
- 199.Berridge KC, Robinson TE. Parsing reward. Trends Neurosci. 2003;26:507–513. doi: 10.1016/S0166-2236(03)00233-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.