Abstract
The present study was undertaken to investigate the infection status of Cryptosporidium parvum in the villagers and the reservoir hosts in several rural areas in Korea. A total 5,262 fecal samples were collected from the inhabitants residing at Gangwon-do, Chungcheongbuk-do, Jeollanam-do, and Gyeongsangnam-do between the dates of September, 2001 to June, 2002. In addition, 1,453 fecal samples were collected from livestock reared in Gokseong-gun, Jeollanam-do and Chungju-si, Chungcheongbuk-do. All the fecal smears were prepared by formalin-ether sedimentation, and examined by light microscopy after modified acid-fast staining. The overall positive rate of human cryptosporidiosis was 3.3%. Gokseong-gun, Jeollanam-do showed a 8.2% positive rate and appeared as the highest endemic area among the surveyed areas. Haman-gun, Gyeongsangnam-do showed a 0.4% positive rate and was the lowest endemic area. The positive rate of livestock infection in Gokseong-gun, Jeollanam-do was 94%, which was more than ten times higher than that of Chungju-si, Chungcheongbuk-do (9.3%). From these results, it was revealed that cryptosporidiosis was an endemic disease in some rural areas of Korea, and the livestock could be an important source of human infection.
Keywords: Cryptosporidium parvum, prevalence
INTRODUCTION
Cryptosporidium parvum is a common protozoan pathogen with a worldwide distribution and it can cause severe and life-threatening diarrhea in an immunocompromised host. This protozoan was first recognized in the stomachs of autopsied mice (Tyzzer, 1907) and first reported in an immunocompetent child and an immunosuppressed adult with diarrhea in 1976 (Nime et al., 1976; Meisel et al., 1976). Since then, cryptosporidiosis has become recognized as a highly prevalent opportunistic pathogen for immunocompromised humans. However, the huge waterborne outbreak affecting over 400,000 residents of South Milwaukee in 1993 (MacKenzie et al., 1994) provoked a remarkable interest on cryptosporidiosis in immunocopetant people as well.
In a review of over 130,000 presumably immunocompetent patients with diarrhea, Adal et al. (1995) noted that 6.1% in developing areas and 2.1% in developed areas with diarrhea had Cryptosporidium infections. Among HIV-positive patients with diarrhea, the percentages with Cryptosporidium infections rose to 24% and 14% (Adal et al., 1995). In Korea, Cho et al. (1993) reported 22% fecal oocyst positive rate out of 230 out-patients of private hospital and Chai et al. (1996) reported 7.9% from 3,146 inhabitants. Recently, Seo et al.(2001) reported 1.9% among 461 inhabitants.
Transmission of C. parvum occurs mainly by the ingestion of oocysts either from fecal to oral contact or through contaminated food or drinking water. It has been known that cattle can be a source of Cryptosporidium infection. Rhee et al. (1991) detected 111 (22.2%) cryptosporidiosis calves out of 500 dairy cattle and Wee et al. (1996) found 29 (14.4%) oocyst positive calves among the 201 that he examined. Chai et al. (1996) reported that 13 (93.3%) out of 15 cattle reared in endemic village were positive for C. parvum oocysts. In addition, C. parvum oocysts were detected in almost all of the environmental waters tested (Smith and Rose, 1998). The present study was performed to investigate the infection status of cryptosporidiosis in normal inhabitants of some rural areas in Korea and reservoir hosts as their sources of infection.
MATERIALS AND METHODS
Samples from the inhabitants
Fecal samples were collected from the inhabitants residing in Chuncheon-si, Gangwon-do, Chungju-si, Chungcheongbuk-do, Gokseong-gun, Jeollanam-do, Haman-gun, Gyeongsangnam-do, and Uiryeong-gun, Gyeongsangnam-do between September in 2001 to June in 2002. Among 5,262 samples collected, 691 were from Chuncheon-si, Gangwon-do, 1,945 from Chungju-si, Chungcheongbuk-do, 1,962 from Gokseong-gun, Jeollanam-do, 485 from Haman-gun, Gyeongsangnam-do and 179 from Uiryeong-gun, Gyeongsangnam-do. Fecal collection was repeated three times at Gokseong-gun, Jeollanam-do, but not from the same person, to observe seasonal variation of Cryptosporidium infection.
Fecal smears were prepared from each sample by the formalin-ether concentration technique, stained by modified acid-fast procedure, and then examined for oocysts of C. parvum. Oocysts of 4-5 µm in diameter, red in color and containing sporozoites were considered positive for C. parvum.
Samples from the livestock
In searching for the source of human infection, fecal samples of livestocks reared in the village were collected. Gokseong-gun, Jeollanam-do, and Chungju-si, Chungcheongbuk-do were selected for the presence of cryptosporidiosis in livestocks. Among the 1,453 samples collected, 863 were beef cattle, 84 dairy cattle, 493 were pigs, and 13 were deer. Cryptosporidium oocysts were examined after formalin-ether sedimentation and modified acid fast staining.
RESULTS
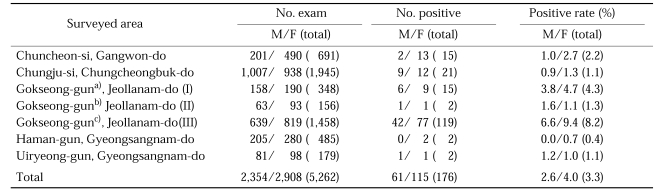
The overall positive rate of cryptosporidiosis among the 5,262 inhabitants examined was 3.3% with 176 positive people excreting oocysts of Cryptosporidium parvum in their feces (Table 1). The area shown the highest positive rate was Gokseong-gun, Jeollanam-do (8.2%) when the survey was undertaken on June 2002. The positive rate of this area was changed according to the time of the survey, from 4.3% on September 2001 to 1.3% on January 2002 and to 8.2% on June 2002. And the area showing the lowest positive rate was Haman-gun, Gyeongsangnam-do (0.4%) (Table 1). The positive rates of inhabitants of Chuncheon-si, Gangwon-do and Chungju-si, Chungcheongbuk-do were 2.2 and 1.1% respectively, which were lower than the average infection rates of this study.
Table 1.
The oocyst positive rates of C. parvum in inhabitants of surveyed areas in Korea
a)Fecal samples were collected in September 2001.
b)Fecal samples were collected in January 2002.
c)Fecal samples were collected in June 2002.
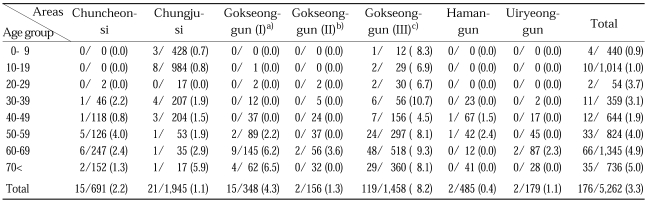
The positive rate of males was 2.6% and that of females was 4.8% in the examined people (Table 1). The positive rates were higher in female group over the surveyed areas, but this was not statistically significant (P > 0.05). The age distribution showed that the positive rates of the older population (> 50) were higher, 4.0 to 5.0%, than those of the younger people, 0.9 to 3.7% (Table 2). A peak positive rate was noted in the age group over 70 (5.0%), followed by the sixties (4.9%) (Table 2).
Table 2.
Age prevalence of C. parvum infeciton among the surveyed population, indicated by no. of positive/no. of exam (%)
a)Fecal samples were collected in September 2001.
b)Fecal samples were collected in January 2002.
c)Fecal samples were collected in June 2002.
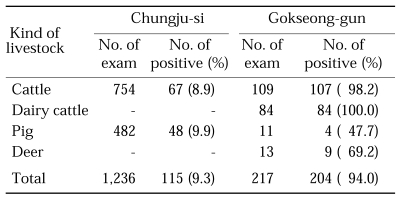
Among the 217 livestock in Gokseong-gun Jeollanam-do, the positive rate of cryptosporidiosis was 94%, higher than that of Chungju-si, Chungcheongbuk-do, 9.3% (Table 3). It was noticed that 100% of the examined dairy cattle from Gokseong-gun were infected with C. parvum and infection rates in beef cattle were 98.2% (Table 3). Although the sample size was small, the infection rates of the pigs and deer were 47.7% and 69.2% respectively. In Chungju-si, the prevalence of infection amoung cattle and pigs were 8.9% and 9.9% respectively.
Table 3.
Infection rates of C. parvum in livestock raised in Chungju-si, Chungcheongbuk-do, and Gokseong-gun, Jeollanam-do
DISCUSSION
Chai et al. (1996) reported 7.9% positive rates of cryptosporidiosis among the 3,146 people examined. The study showed a remarkable difference in positive rates between rural area and urban area, from 10.6% to 0.5%. In the present study, we examined inhabitants in five rural areas belong to four provinces, i.e., Gangwon-do, Chuncheongbuk-do, Jeollanam-do, and Gyeongsangnam-do. The average positive rate in this study was 3.3% and this figure is much lower than the previous report by Chai et al. (1996). Wee found however, that Jeollanam-do had the highest endemic of cryptosporidosis among four provinces examined. In the report by Chai et al. (1996), there was no available data about other provinces other than Jeollanam-do. The prevalence rates of the other three provinces except Jeollanam-do were similar with each other and in the range of 0.4 to 2.2%; this was also similar with the prevalence rates of Chorwon-gun, Gangwon-do (1.9%) reported by Seo et al. (2001) previously.
Seasonal trends of Cryptosporidium infection have been reported by a number of authors suggesting that the incidence of cryptosporidiosis is highest in the warm or wet seasons. Griffiths (1998) reported that the incidence in children under 2 years old was greatest in the rainy season in Gabon, and in Aragon, Spain, Clavel et al. (1996) detected more cryptosporidiosis during the autumn-winter period than in spring and summer. Chai et al. (2001) reported that seasonal peaks of cryptosporidiosis appeared twice a year, in spring (March-May) and in autumn (October-November). In this study the positive rate in Gokseong-gun, Jeollanam-do was the highest in June 2002, with as much as 8.2% versus to 4.2% in September 2001, and 1.3% in January 2002. Although we did not study prevalence rates every month, the present study suggested that the rainy season could have the effect of increasing infection rates of C. parvum because June is usually the rainy season in Korea. Heavy rainfall could help the transmission of C. parvum by inducing a wider spread of the animal feces onto fields or water. Infection rates in January showed the lowest value (as was expected) because the outside temperature was cold and dry enough to negatively affect the viability of C. parvum oocysts. The cold temperature can also reduce the outdoor activity of people and have the effect of making infection rates lower by decreasing the chance to contact to the oocysts.
According to Casemore (1990), the peak incidence of cryptosporidiosis is in children aged 1-5 years. In Korea, the opposite has been noted as the peak positive rates were recorded in older age groups. Chai et al. reported that the age groups in their fifties and sixties showed higher positive rates, 13.2% and 15.9% respectively in 1996, and 80.0% and 69% respectively in 2001 (Chai et al., 1996; 2001). In the present study, the senile inhabitants aged over fifty showed a higher prevalence rate (4.0-5.0%) than younger people as already mentioned by Chai et al. (1996; 2001). The results of the age distribution in this study possibly reflected a bias due to the deviated population structure toward aged people in rural communities of our country. In other words, the number of people examined in the young generation was not enough in all the surveyed areas (except Chungju-si) to make a representative data sample on infection rates. The persons excreting oocysts of C. parvum through their feces were not complaining of any specific clinical symptomes such as diarrhea. Therefore most of the people that were positive for C. parvum oocysts seemed to be in the carrier status of cryptosporidiosis and played a role of an infection source to their community.
Direct contact with infected animals is suggested to be an important mode of transmission of. C. parvum. C. parvum is probably present in every domestic cattle herd in the world with asymptomatic infections and prolonged oocyst excretion by adult cattle recognized as a major and continuous source of environmental contamination (Tzipori and Ward, 2002). Wee et al. (1996) found 29 (14.4%) oocyst positive calves among 201 examined. Chai et al. (1996) also found 93.3% of cattle were positive for C. parvum oocysts. But their study sample was small; they only examined 15 herds. In this study, we found that 94% (204) of livestock of the 217 examined in Gokseong-gun, Jeollanam-do were infected with C. parvum. Most of the beef cattle (98.2%) were positive and all the dairy cattle examined were positive for oocysts of C. parvum. On the other hand, infection rates of cattle in Chungju-si, Chungcheongbuk-do were less than 10%. The results suggested that the infection rates of C. parvum in cattle seemed to be different according to regional difference. It is also suggested that where the human cryptosporidiosis is highly endemic the area also has a high incidence of cryptosporidiosis in cattle as well.
At least six Cryptosporidium species are currently recognized; this is based on genotyping and a limited number of transmission experiments (Tzipori and Ward, 2002). Among these species, C. parvum is the main cause of human disease. C. parvum has recently been known to have several different genotypes such as genotype I, found exclusively in humans and a few other primates, and genotype 2, found in most mammals, including humans (Tzipori and Ward, 2002). We did not evaluate the genotype of C. parvum in humans and animals in this study. Especially in cattle, we found that most animals had a mixed infection of C. parvum and other species. This was because the sizes of the oocysts in feces were not even and there were larger oocysts than the size of C. parvum oocysts (4-5 µm). Future study will soon be necessary to verify the mixed infection status of the cattle in Korea. The pigs and deer also showed positive rates of C. parvum oocysts (as much as 47.7 to 69.2%), so these findings suggested that these animals could be a source of human infection although the exact species of Cryptosporidium will have to be studied further. In addition, the high infection rate of livestock in rural communities strongly suggests the possibility of heavy environmental contamination with C. parvum oocysts. Because C. parvum is one of major waterborne protozoa, water contamination should be investigated in the near future to protect the public health from the risk of this pathogen.
Footnotes
This work was supported by grant No. R04-2001-000-00203-0 from the Korea Science & Engineering Foundation.
References
- 1.Adal KA, Sterling CR, Guerrant RL. Cryptosporidium and related species. In: Blaser MJ, Smith PD, Ravdin JI, Greenberg HB, Guerrant RL, editors. Infections of the Gastrointestinal Tract. New York: Raven Press; 1995. pp. 1107–1128. [Google Scholar]
- 2.Casemore DP. Epidemiological aspects of human cryptosporidiosis. Epidemiol Infect. 1990;104:1–28. doi: 10.1017/s0950268800054480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chai JY, Lee SH, Guk SM, Lee SH. An epidemiological survey of Cryptosporidium parvum infection in randomly selected inhabitants of Seoul and Jeollanam-do. Korean J Parasitol. 1996;34:113–119. doi: 10.3347/kjp.1996.34.2.113. [DOI] [PubMed] [Google Scholar]
- 4.Chai JY, Kim NY, Guk SM, et al. High prevalence and seasonality of cryptosporidiosis in a small rural village occupied predominantly by aged people in the Republic of Korea. Am J Trop Med Hyg. 2001;65:518–522. doi: 10.4269/ajtmh.2001.65.518. [DOI] [PubMed] [Google Scholar]
- 5.Cho MH, Kim AK, Im K. Detection of Cryptosporidium oocysts from out-patients of the Severance hospital. Korean J Parasitol. 1993;31:193–199. doi: 10.3347/kjp.1993.31.3.193. [DOI] [PubMed] [Google Scholar]
- 6.Clavel A, Olivares JL, Flea J, et al. Seasonality of cryptosporidiosis in children. Eur J Clin Microbiol Infect Dis. 1996;15:77–79. doi: 10.1007/BF01586190. [DOI] [PubMed] [Google Scholar]
- 7.Griffiths JK. Human cryptosporidiosis: epidemiology, transmission, clinical disease, treatment, and diagnosis. Adv Parasitol. 1998;40:37–85. doi: 10.1016/s0065-308x(08)60117-7. [DOI] [PubMed] [Google Scholar]
- 8.MacKenzie WR, Hoxie NJ, Proctor ME, et al. A massive outbreak in Milwaukee of Cryptosporidium infection transmitted through the public water supply. N Engl J Med. 1994;331:161–167. doi: 10.1056/NEJM199407213310304. [DOI] [PubMed] [Google Scholar]
- 9.Meisel JL, Perera DR, Meligro C, Rubin CE. Overwhelming watery diarrhea associated with Cryptosporidium in an immunocompromised patient. Gastroenterology. 1976;70:1156–1160. [PubMed] [Google Scholar]
- 10.Nime FA, Burek JD, Page DL, Holsher MA, Yardley JH. Acute enterocolitis in a human being infected with the protozoan Cryptosporidium. Gastroenterology. 1976;70:592–598. [PubMed] [Google Scholar]
- 11.O'Donoghue PJ. Cryptosporidium and cryptosporidiosis in man and animals. Int J Parasitol. 1995;25:139–195. doi: 10.1016/0020-7519(94)e0059-v. [DOI] [PubMed] [Google Scholar]
- 12.Rhee JK, Seu YS, Park BK. Isolation and identification of Cryptosporidium from various animals in Korea. I. Prevalence of Cryptosporidium in various animals. Korean J Parasitol. 1991;29:139–148. doi: 10.3347/kjp.1991.29.2.139. [DOI] [PubMed] [Google Scholar]
- 13.Seo M, Huh S, Chai JY, Yu JR. An epidemiological survey on Cryptosporidium parvum infection of inhabitants in Chorwon-gun, Kangwon-do. Korean J Parasitol. 2001;39:201–203. doi: 10.3347/kjp.2001.39.2.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith HV, Rose JB. Waterborne cryptosporidiosis: current status. Parasitol Today. 1998;14:14–22. doi: 10.1016/s0169-4758(97)01150-2. [DOI] [PubMed] [Google Scholar]
- 15.Tyzzer EE. A sporozoan found in the peptic glands of the common mouse. Proc Soc Exp Biol Med. 1907;5:12–13. [Google Scholar]
- 16.Tzipori S, Ward H. Cryptosporidiosis: biology, pathogenesis and disease. Microbes Infect. 2002;4:1047–1058. doi: 10.1016/s1286-4579(02)01629-5. [DOI] [PubMed] [Google Scholar]
- 17.Wee SH, Joo HD, Kang YB. Evaluation for detection of Cryptosporidium oocysts in diarrheal feces of calves. Korean J Parasitol. 1996;34:121–126. doi: 10.3347/kjp.1996.34.2.121. [DOI] [PubMed] [Google Scholar]