Abstract
A small scale survey was performed to know the infection status of intestinal parasite in children of the residential institutions and street communities in Metro Manila, Philippines. A total of 284 stool samples from 11 institutions and 3 street communities was examined by the formalin-ether concentration method. The scotch tape anal swab was adapted to 121 children to investigate the infection status of Enterovius vermicularis. It was found out that 62.0% of the children examined were positive for one or more intestinal parasites. Multiple infections were observed in 34.2% of the children. Among 172 children who gave detail information, the prevalence for Ascaris lumbricoides, Trichuris trichiura, and hookworm was 36.0%, 44.8%, and 7.0% respectively. Of the children examined, 47.7% were found to be harboring parasitic protozoans such as Entamoeba histolytica, Giardia lamblia, and Blastocystis hominis. The most prevalent of these protozoans was B. hominis with an infection rate of 40.7%. The prevalence of these infections among children living in institutions was relatively high. More efforts should be made to implement anthelminthic programs including bi-annual follow-up treatments.
Keywords: child, residential institution, intestinal parasitism, prevalence, Philippines
"Street children" are children ages 7 to 18 who live or work in the streets in the Philippines. In 1997, the number of street children nationwide is estimated at 1.5 million, approximately 100,000 of which are in Metro Manila (Caparas, 1998). In the Philippines, there is an estimated 300 agencies working with street children. Most of these agencies (about 70%) are nongovernment organizations (NGOs) and approximately 50% of these NGOs are within Metro Manila where a third of them offer center-based programs including a residential shelter or institution (PhilDHRRA, 1988). Soil-transmitted helminthiasis (STH) is a persistent problem in the Philippines but it does not yet have a definitive control plan (David et al., 1999). Recently, several surveys have been done to figure out the prevalence of intestinal parasitic infection among children in the Philippines (Auer, 1990; Lee, 2000; Belizario et al., 2002). However, little is known about the infection status of intestinal parasites among street children. This study aimed to survey the prevalence of intestinal parasites among street children housed in shelters managed by the government and NGOs.
On December 2002, stool samples were collected from street children housed in different NGO and government managed shelters in Metro Manila. Stool samples were also collected from children who were living in street communities (i.e. communities adjacent to a road, highway, or street) and who were staying in their own homes or places of residence. Children from the institutions were also examined for Enterobius vermicularis infection by the scotch tape swab. The stool samples were examined by the formalin-ether concentration technique.
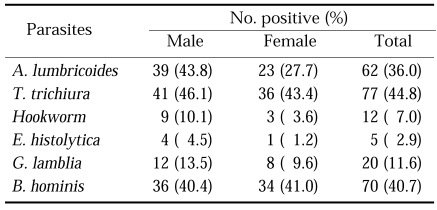
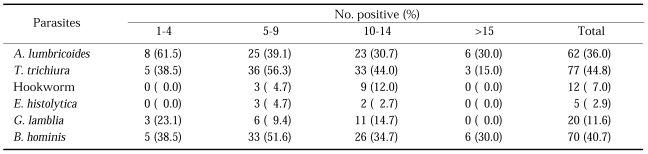
A total of 204 children from 11 institutions was examined for this study. For comparison, 80 children from 3 street communities were also examined. Prevalence of helminth infection among children living in institutions was 59.8% and those living in street communities had a prevalence of 52.5%. Prevalence of infection with parasitic protozoa is also similar, 44.1% of the children in institutions and 48.8% of the children from the street communities were positive for at least one parasitic protozoan. A total of 155 (76.0%) children from the institutions and 57 (71.3%) from the communities was found to be infected with any of helminth or protozoa. Almost 33% of the children from the institutions and 37.5% from the communities harbored more than two kinds of intestinal parasites. Among 204 children from the institutions, 172 children gave detail information on their sex, age, and length of stay, etc. Table 1 and 2 shows the infection status of intestinal parasites of those 172 children. Examination for the presence of E. vermicularis in 121 children living in institutions revealed 40 positive cases or a prevalence of 33.1%.
Table 1.
Prevalence of intestinal parasite infection according to the sex of 172 children living in residential institutions in Metro Manila, the Philippines
Table 2.
Prevalence of intestinal parasite infection according to the age of 172 children living in residential institutions in Metro Manila, the Philippines
The results obtained did not show a significant difference of prevalence between the two groups, children from the institutions and the communities, in terms of overall prevalence. Infection rates for intestinal parasites were higher in male than female. Tricuris trichiura and Ascaris lumbricoides remain to be the most prevalent helminths. The infection rates of these helminths were around 40%, which is similar to results obtained by a recent survey in a Philippine community (Kim et al., 2003). Hookworm infection, although common, has a prevalence lesser than 10%. Hookworm prevalence for the Philippines, primarily an agricultural country, is surprisingly low compared to other STH endemic countries (de Silva et al., 2003). The hand to mouth infection route for A. lumbricoides and T. trichiura can readily explain their high prevalence. Hookworm infection by the cutaneous route may be impeded by many factors including the susceptibility of the infective larvae to harsh environmental conditions (Rukmono, 1976; Neva and Brown, 1994). Tilled or shaded sandy soil is less common in the already urbanized Metro Manila. Although the temperature of the Philippines is favorable for the viability of hookworm larvae, particularly Necator americanus, which is the more common hookworm species (Cabrerra, 1981), the weather pattern of the Philippines may contribute to making the environment unfavorable for hookworm larvae. The Philippines experiences a cyclic wet and dry season characterized by six months of much rainfall and the other half of the year usually dry, hot and humid. Furthermore, the children involved in the study are required to wear shoes and slippers when already inside the institution and when going to school, thus lessening exposure to the hookworm infective stage. For parasitic protozoan infections, the most prevalent parasitic protozoans observed in the children was B. hominis and G. lamblia with respective prevalence of 40.7% and 11.6% (Table 1 & 2). B. hominis infection had a significant prevalence that was not shown even in the more recent studies (Lee et al., 2000; Kim et al., 2003). B. hominis is commonly found in the intestinal tract but it is only lately that it is recognized to cause disease (Neva and Brown, 1994; de Leon, 1998) and thus previous researchers may not have given much attention to it. However, the high occurrence of B. hominis may also be indicative of poor water quality and sanitation in the shelters.
The prevalence of intestinal parasites among children housed in institutions managed by the government and NGOs remains high. More than half of the children were shown to harbor at least one intestinal helminth and almost half of them had parasitic protozoan infections. In 1988, a cross sectional stool sample survey performed among children living in a garbage dump site in Metro Manila revealed a prevalence rate of 96% for intestinal parasitism (Auer, 1990). In another Philippine community, children had a prevalence of 78.1% (Lee et al., 2002). Belizario et al. (2002) mentioned that the cumulative prevalence of intestinal helminth infection in pupils of a public elementary school to be included in a treatment program was 94%. The high prevalence of parasitism shown in this study, although lower than that of other examinations reported from children in communities and schools (Auer, 1990; Lee 2000; Belizario et al., 2002) suggests that there is still much room for the improvement of health delivery and health program implementation. Sanitation practices and water quality should be improved, as these are the major contributory factors for the spread of helminth and protozoan infections. The administrators of the institutions included in this study mentioned that deworming activities were conducted in the shelters at certain times of the year. However, the results show that reinfection could have happened because the prevalence remained high. Examination for intestinal parasitism was also not routine procedure when children were admitted. In essence, health education, improved sanitation practices, and consistent implementation of an examination and treatment program for intestinal parasitism with a follow-up of at least every six months should be done to protect and treat children in institutions from the harmful effects of intestinal parasitism.
ACKNOWLEDGMENTS
The authors would like to thank the children, staff, volunteers, and administrators of the organizations that have been part of the study and to the National Institutes of Health, University of the Philippines, Manila for providing the laboratory facilities and equipment during diagnosis.
References
- 1.Auer C. Health status of children living in a squatter area of Manila, Philippines, with a particular emphasis on intestinal parasites. Southeast Asian J Trop Med Public Health. 1990;21:289–300. [PubMed] [Google Scholar]
- 2.Belizario VY, Amarillo ME, de Leon WU, de los Reyes AE, Bugayong MG, Macatangay BJ. A comparison of the efficacy of single doses of albendazole, ivermectin, and diethylcarbamazine alone or in combinations against Ascaris and Trichuris spp. Bull World Health Organ. 2003;81:35–42. [PMC free article] [PubMed] [Google Scholar]
- 3.Cabrerra BD . Collected Papers on the Control of Soil-transmitted Helminthiases. Vol II. Japan: APCO Research Group; 1981. Species determination of human hookworm using the polyethylene-tube culture technique in selected areas in the Philppines; pp. 11–18. Asian Parasite Control Organization. [Google Scholar]
- 4.Caparas MV. The Bahay Tuluyan and its Junior Educator's Program : strengthening the streetchildren's resilience. Philippine Soc Sci Rev. 1998;55:1–4. [Google Scholar]
- 5.David LC, Lumampao YCF, Hipolito JH, Ortega DB. Reference manual on soil - transmitted helminthiasis produced for the National Program to Control Soil - Transmitted Helminthiasis. Center for Infectious Disease, Department of Health, Philippines; 1999. available from http://www.doh.gov.ph/sth/index3.htm. [Google Scholar]
- 6.De Leon WU. Other intestinal protozoans. In: Belizario VY, Solon JAA, editors. Philippine textbook of medical parasitology. Philippines: University of the Philippines Manila; 1998. pp. 55–56. [Google Scholar]
- 7.de Silva NR, Brooker S, Hotez PJ, Montresor A, Engels D, Savioli L. Soil-transmitted helminth infections: updating the global picture. Trends Parasitol. 2003;19:547–551. doi: 10.1016/j.pt.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 8.Kim BJ, Ock MS, Chung DI, Yong TS, Lee KJ. The intestinal parasite infection status of inhabitants in theRoxas City, the Philippines. Korean J Parasitol. 2003;41:113–115. doi: 10.3347/kjp.2003.41.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee KJ, Ahn YK, Yong TS. A small scale survey of intestinal parasite infections among children and adolescents in Legaspi City, the Philippines. Korean J Parasitol. 2000;38:183–185. doi: 10.3347/kjp.2000.38.3.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Neva FA, Brown HW. Basic Clinical Parasitology. 6th ed. Connecticut, USA: Appleton and Lange; 1994. pp. 128–133. [Google Scholar]
- 11.Philippine Partnership for the Development of Human Resources in Rural Areas (PhilDHRRA) Directory of Philippine NGOs. 3rd ed. Manila, Philippines: PhilDHRRA; 1988. [Google Scholar]
- 12.Rukmono B. Collected Papers on the Control of Soil-transmitted Helminthiases. Vol I. Japan: APCO Research Group; 1976. Infection route of roundworm and hookworm (with reference to the development and viability in the soil of the infective stages) pp. 125–128. Asian Parasite Control Organization. [Google Scholar]