Abstract
A survey was conducted to determine the extent of intestinal parasite infection in Bat Dambang, Cambodia in March 2004. A total of 623 fecal specimens was collected from kindergarten and schoolchildren and examined using the formalin-ether sedimentation technique. The overall infection rate of intestinal parasites was 25.7% (boys, 26.2%; girls, 25.1%), and the infection rates of intestinal helminthes by species were as follows: Echinostoma sp. 4.8%, hookworm 3.4%, Hymenolepis nana 1.3%, and Rhabditis sp. 1.3%. The infection rates of intestinal protozoa were; Entamoeba coli 4.8%, Giardia lamblia 2.9%, Iodamoeba butschlii 1.4%, Entamoeba polecki 1.1%, and Entamoeba histolytica 0.8%. There were no egg positive cases of Ascaris lumbricoides or Trichuris trichiura. All children infected were treated with albendazole, praziquantel, or metronidazole according to parasite species. The results showed that intestinal parasites are highly endemic in Bat Dambang, Cambodia.
Keywords: Cambodia, intestinal parasites, children
Cambodia is recognized as an endemic area for malaria and schistosomiasis (Meek, 1988; Singhasivanon, 1999; Urbani et al., 2002), but the infection status of intestinal parasites in Cambodia has not been thoroughly investigated. However, several reports show that Cambodian children and refugees are infected with intestinal parasites including nematodes, trematodes, and protozoa (Nwanyanwu et al., 1989; Lurio et al., 1991; Gyorkos et al., 1992; Lee et al., 2002).
With the aid of a local Korean medical service in Cambodia, we collected 623 stool samples from children at Watkor Kindergarten and from schoolchildren in Bat Dambang, Cambodia in March 2004; Bat Dambang is located about 250 km southeast of Phnom Penh, the capital city of Cambodia.
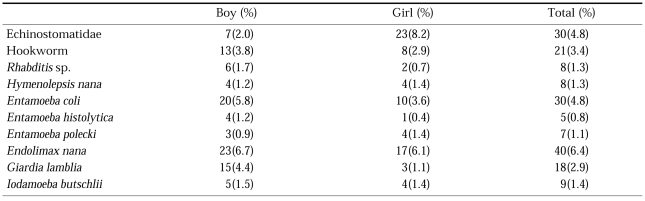
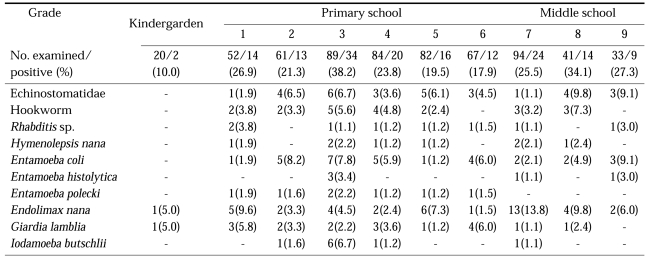
Formalin-ether sedimentation revealed intestinal helminth eggs of Hookworm, Rhabditis sp., Hymenolepis nana, and Echinostoma sp., and protozoan cysts of Entamoeba histolytica, Entamoeba coli, Giardia lamblia, Iodamoeba butschlii, and Entamoeba polecki. Of the 623 stool specimens, 160 (25.7%) were positive. The positive rates for boys and girls were 26.2% (90/344) and 25.1% (70/279), respectively. Data revealed a highest positive rate (4.8%) for Echinostoma sp., followed by 3.4% for Hookworm (Table 1). Multiple parasite infections were found in 9 cases. Infection rates ranged from 10% to 38.2% by school grade; the highest rate was found among third grade of primary schoolchildren. The results of a comparison of trematode infection and eating habits were interesting. In general, children did not consume raw fresh water fish (Story et al., 1989); however, they were believed to have been infected by inadequately cooked fish. Echinostoma species are important trematode parasites and require treatment; anti-helminthics were sent to the Watkor primary school after the stool examination.
Table 1.
Prevalences of intestinal parasite infections in Watkor kindergarten children and schoolchildren in Bat Dambang, Cambodia
The school is located along the Steung Sangkae River, which is connected to Tonle Sab Lake. Although many children swam in this river during the stool examination period, we failed to find Schistosoma eggs. Accordingly, in view of their swimming habits, this area is not considered to be a schistosomiasis endemic area.
The present study showed different patterns of intestinal parasite infection compared to the previous survey at Kampongcham (Lee et al., 2002); this survey showed no cases of Ascaris lumbricoides, Trichuris trichiura or Opisthorchis sp., while egg positive rates of A. lumbricoides, T. trichiura, and Opisthorchis sp. in Kampongcham were 26.3%, 1%, and 10%, respectively. However, children in Bat Dambang were found infected with E. polecki (1.1%) and H. nana (1.3%), whereas no cases of E. polecki or H. nana were recorded in the Kampongcham survey in 2002 (Lee et al., 2002). This study identified regional differences in intestinal parasitic infections between in Bat Dambang and in Kampongcham.
Periodic surveys on intestinal parasitic infections, the treatment of infected cases, and education with respect to eating habits and improved sanitation conditions are highly recommended for parasite control in Cambodia.
Table 2.
Prevalences of intestinal parasite infection by school grade among Watkor kindergarten children and schoolchildren in Bat Dambang, Cambodia
ACKNOWLEDGEMENTS
We thank the medical service team at Wonju Christian Hospital for collection of stool samples, and the Harvest Mission Center in Cambodia for its cooperation during the visit to the survey area.
References
- 1.Gyorkos TW, MacLean JD, Viens P, Chheang C, Kokoskin-Nelson E. Intestinal parasite infection in the Kampuchean refugee population 6 years after resettlement in Canada. J Infect Dis. 1992;166:413–417. doi: 10.1093/infdis/166.2.413. [DOI] [PubMed] [Google Scholar]
- 2.Lee KJ, Bae YT, Kim DH, et al. Status of intestinal parasites infection among primary school children in Kampongcham, Cambodia. Korean J Parasitol. 2002;40:153–155. doi: 10.3347/kjp.2002.40.3.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lurio J, Verson H, Karp S. Intestinal parasites in Cambodians: comparison of diagnostic methods used in screening refugees with implications for treatment of populations with high rates of infestation. J Am Board Fam Pract. 1991;4:71–78. [PubMed] [Google Scholar]
- 4.Meek SR. Epidemiology of malaria in displaced Khmers on the Thai-Kampuchean border. Southeast Asian J Trop Med Public Health. 1988;19:243–252. [PubMed] [Google Scholar]
- 5.Nwanyanwu OC, Moore JS, Adams ED. Parasitic infections in Asian refugees in Fort Worth. Tex Med. 1989;85:42–45. [PubMed] [Google Scholar]
- 6.Singhasivanon P. Mekong malaria. Malaria, multidrug resistance and economic development in the greater Mekong subregion of Southeast Asia. Southeast Asian J Trop Med Public Health 30. 1999;30(Suppl 4):i–iv. 1–101. [PubMed] [Google Scholar]
- 7.Story M, Harris LJ. Food habits and dietary change of Southeast Asian refugee families living in the United States. J Am Diet Assoc. 1989;89:800–803. [PubMed] [Google Scholar]
- 8.Urbani C, Sinoun M, Socheat D, et al. Epidemiology and control of mekongi schistosomiasis. Acta Trop. 2002;82:157–168. doi: 10.1016/s0001-706x(02)00047-5. [DOI] [PubMed] [Google Scholar]