Abstract
OBJECTIVES
To describe functional outcomes in the year following discharge for elders discharged from the hospital after an acute medical illness with a new or additional disability in their basic self-care activities of daily living(ADL)(compared to their preadmission baseline two weeks before admission), compared to elders discharged with baseline ADL function, and identify predictors of failure to recover to baseline function one year after discharge.
DESIGN
Observational Study
SETTING
Tertiary care hospital, Community teaching hospital
PARTICIPANTS
Older(≥70 years) patients non-electively admitted to general medical services(1993-1998).
MEASUREMENTS
Number of ADL disabilities 1,3,6,&12 months after discharge compared to pre-admission baseline. Outcomes were death, sustained decline in ADL function, and recovery to baseline ADL function at each timepoint.
RESULTS
By 12 months after discharge, among those discharged with new or additional ADL disability, 41.3% died, 28.6% were alive but had not recovered to baseline function, and 30.1% were at their baseline function. Among those discharged with baseline function, 17.8% died, 15.2% were alive but with worse than baseline function, and 67% were at their baseline function(p<.001). Among those discharged with new or additional ADL disability, the presence or absence of recovery by one month was associated with long-term outcomes. Age, cardiovascular disease, dementia, cancer, low albumin, and greater number of dependencies in IADL independently predict failure to recover.
CONCLUSION
Among elders discharged with new or additional disability in ADL following hospitalization for medical illness, prognosis for functional recovery is poor. Rehabilitation interventions of longer duration and timing than current reimbursement allows, caregiver support, and palliative care should be evaluated.
Keywords: hospitalization, functional decline, recovery
INTRODUCTION
Hospitalization for acute medical illness frequently precipitates disability in activities of daily living (ADL).1-9 The loss of self-care abilities results in serious short-term consequences for patients and families as patients dependent in ADL can not successfully live at home without the assistance of caregivers. However, the long-term significance of new or additional disabilities in ADL associated with acute medical illness is not known. Recovery from disability among community-dwelling older persons is common, with rates of recovery from episodes of disability as high as 80%.10, 11 In the short term, compared to people whose disability develops more progressively without a hospitalization, rates of recovery for people with a hospitalization may be higher, but hospitalization does not predict persistent recovery, and little is known about functional recovery for more than 1 to 3 months after hospital discharge.4, 9, 12-15 High rates of mortality and nursing home placement after hospitalization suggest that functional outcomes may be poor.13, 16-18
An understanding of the rates, time course, and predictors of functional recovery for older adults hospitalized for medical illness is essential for planning for the care needs of these patients, optimizing preventive and rehabilitative strategies for these patients, and informing health policy. Furthermore, formal rehabilitative services are less commonly provided after hospitalizations for medical illness than for illnesses such as stroke or some surgical procedures, and most of these services are of short duration and low intensity.19-22 The objectives of this study were (1) to describe long-term functional outcomes in the year following discharge for medical hospitalization in elders discharged with a new or additional disability in their self-care ADL compared to their preadmission baseline two weeks before admission, (2) to compare these functional outcomes to the outcomes in elders who were discharged with baseline self-care ADL function, and (3) to identify predictors of failure to recover to baseline function one year after hospital discharge in older people with new or additional disabilities in self-care ADL.
METHODS
Setting and Participants
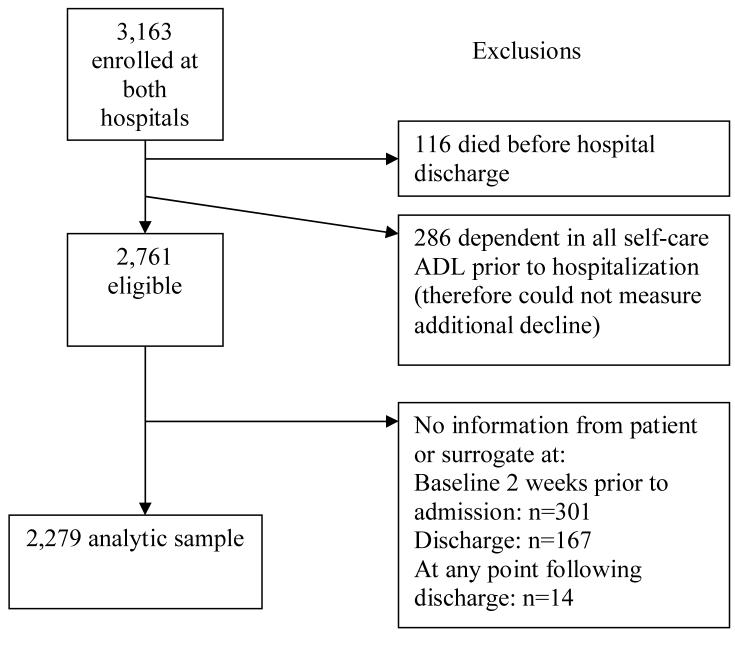
Patients were drawn from two randomized controlled trials of an intervention to improve functional outcomes in older (≥ 70) hospitalized medical patients conducted between 1993 and 1998 at University Hospitals of Cleveland, a tertiary care hospital, and Akron City Hospital, a community teaching hospital in Ohio.23, 24 Both enrolled patients who had non-elective admissions to general medical services. Patients who were admitted electively, who had an expected length of stay of less than 2 days or who were admitted to the intensive care unit were excluded. We combined the intervention and control groups because our analysis focused on post-discharge trajectories and the intervention was hospital-based and did not affect changes in self-care ADL between discharge and one year.23(Figure 1.1)
Figure 1. Derivation of the Analytic Sample and Study Definitions.
1.1) Derivation of the analytic Sample
1.2) Trajectories of Function in Self-care Activities of Daily Living (ADL): Baseline Through Hospital Discharge
Footnote:
Group 1: Discharged with Baseline Self-Care Activities of Daily Living (ADL) Function
Trajectory a: patients who had stable function throughout their course with no decline in self-care ADL function between baseline and admission and no decline between admission and discharge.
Trajectory b: patients who declined in self-care ADL function between baseline and hospital admission, but recovered to baseline self-care ADL function by the time of hospital discharge.
Group 2: Discharged with New or Additional Disability in self-care ADL (decline in self-care ADL function)
Trajectory c: Patients acquiring new or additional disability in self-care ADL between baseline and admission who did not recover to baseline function by the time of hospital discharge
Trajectory d: Patients who did not decline in self-care ADL function between baseline and admission but acquired new or additional disability in self-care ADL between admission and discharge.
Out of 2,279 patients who were eligible for this analysis, 1,480 patients were discharged with similar or better functional status compared to 2 weeks prior to admission while 799 patients were discharged with worse functional status compared to 2 weeks prior to admission, as indicated by a new or additional disability in at least one self-care ADL.(Figure 1.2)
Outcomes and Follow-up
Data were collected in interviews with patients or surrogate respondents at the time of hospital admission and hospital discharge, as well as phone interviews 1,3,6, and 12 months after discharge. Surrogates, identified as the primary caregiver in the nursing admission note, were interviewed when patients were unable to communicate, were too ill, or failed a cognitive screen(defined as ≥5 errors on the Short Portable Mental Status Questionnaire) at the time of hospital admission.25 In general, the same respondent was interviewed at admission, discharge, and after discharge. Twenty-three percent of respondents were surrogates.
To determine whether the subject was independent or dependent in each of 5 self-care ADL (bathing, dressing, eating, transferring from a bed to a chair, and using the toilet), subjects were asked if they needed the help of another person to complete the self-care ADL (e.g. “On the day you were admitted to the hospital, did you need help washing or bathing yourself?”) Each respondent was also asked whether the patient could perform these self-care ADL independently two weeks prior to admission, which defines baseline function in this study. This definition for baseline function was chosen as it generally reflects function prior to the acute illness or exacerbation of chronic illness resulting in hospital admission, but is recent enough that patient and surrogate recall of functional status is reliable. Prior work has demonstrated that these retrospective reports have predictive validity.26 At the time of discharge, and at 1,3,6, and 12 months after discharge, respondents were, again, asked whether the patient could perform each self-care ADL independently at that present time.
At the time of hospital admission, each respondent reported on demographic information on living situation, ethnicity, and education and the patient’s ability to perform seven Instrumental Activities of Daily Living(IADL) without another person’s assistance two weeks prior to admission. Data gathered through medical record review included comorbid diagnosis information for the Charlson Comorbidity index, chart diagnosis of dementia, information for the Acute Physiology Score(APS)27 at the time of admission, and admission serum albumin level.
Definitions: Functional Trajectories Between Baseline and Hospital Discharge
For each time point (baseline, hospital admission, hospital discharge, 1-,3-,6-, and 12-month follow-up) we calculated a global self-care ADL score which was defined as the number of self-care ADL which the patient could perform independently. Patients were classified into one of four functional trajectories based on changes in their functional status between their baseline and the time of hospital discharge (Figure 1.2). The first two trajectories (Group 1) included patients whose self-care ADL function at discharge was at least as good as their baseline function (Discharged with Baseline Function). The first trajectory within this group included those patients who had stable function throughout their course (Group 1, trajectory a: no decline between baseline and admission and no decline between admission and discharge). The second trajectory within this group included patients who declined between baseline and hospital admission, but recovered to baseline self-care ADL function by the time of hospital discharge (Group 1, trajectory b). The next group (Group 2) included patients who declined in self-care ADL function between baseline and discharge (i.e., were dependent in more self-care ADL at the time of hospital discharge than at their pre-illness baseline) (Discharged with New or Additional self-care ADL Disability (Decline in self-care ADL Function)). The first trajectory within this group includes patients who declined in ADL function between baseline and admission who did not recover to baseline function by the time of hospital discharge (Group 2, trajectory c). The second trajectory within this group included patients who did not decline between baseline and admission but declined between admission and discharge (Group 2, trajectory d).
Data Analyses
Description of Functional Outcomes following hospitalization
At 1-,3-,6-, and 12 months following hospitalization, patients in both groups were classified as having died, having worse than baseline self-care ADL function, and having recovered to baseline self-care ADL function at that time point, depending on whether or not they were independent in at least as many self-care ADL as at baseline. Death was determined at each time point by surrogate report or National Death Index. Patients and surrogates who were unable to be contacted were classified as missing at each time point. Average percentage missing at 1-,3-, 6-, and 12-months was 5.8%, 7.9%, 7.8%, and 6.2% respectively. Differences in the proportions who died, who did not recover to baseline self-care ADL function, and who were recovered to baseline self-care ADL function at each point in time were compared using chi-square tests. Then we examined the impact of early functional recovery on patients discharged with worse than baseline functional status(n=799). Outcomes at 3, 6 and 12 months were compared for those with and without functional recovery at 1 month using chi-square tests (excluding those with missing data at one month or who had died by one month resulted in a sample size of n=651). We also determined the timing of recovery for those who were at baseline function at 12 months after hospital discharge.
Predictors of 1-Year Outcome
Additional analyses addressed predictors of failure to recover at 3 and 12 months after discharge among those with new or additional disability in self-care ADL at hospital discharge. First, we used chi-square tests to examine the relationship between predictor variables and failure to recover. Variables were chosen based on review of the literature and a priori hypotheses, and included age, gender, ethnicity, educational level, living alone, number of independent self-care ADL at baseline, number of independent IADL at baseline, the APS, admission from a nursing home, serum albumin, and comorbid conditions included in the Charlson comorbidity index (cardiovascular disease(defined as history of myocardial infarction, coronary artery disease, peripheral vascular disease or stroke), renal disease, diabetes, cancer, chronic obstructive pulmonary disease, dementia, and congestive heart failure). Cutpoints for variables were chosen based on prior work.8 We used logistic regression to identify independent predictors failing to recover by one year. We repeated this analysis to determine independent predictors of failing to recover among 1-year survivors. Only significant variables were retained in the final models. We used established methodology to convert from odds ratios to risk ratios.28
RESULTS
The baseline characteristics of patients who were discharged with baseline function and those who had acquired at least one new disability in self-care ADL as compared to baseline are presented in Table 1.
Table 1.
Characteristics of Patients by Function at Hospital Discharge
| Characteristics of Patients | Discharged with New or Additional Disability in ADL* (n = 799) |
Discharge with Baseline Function (n = 1480) |
P Value |
|---|---|---|---|
| Mean Age (SD†) | 82.0 (7.3) | 78.2 (6.0) | <0.001 |
| Mean length of stay (SD†) | 8.2 (6.6) | 5.3 (3.6) | <0.001 |
| APS‡ (mean, SD†) | 10.2 (3.9) | 9.1 (3.0) | <0.001 |
| Ethnicity White | 76.0 | 76.7 | 0.15 |
| Black | 24.0 | 23.3 | |
| Women, % | 68.3 | 61.0 | <0.001 |
| Lives alone, % | 35.4 | 35.2 | 0.94 |
| Admitted from NH§ % | 7.8 | 3.4 | <0.001 |
| Independent in all ADL* at baseline |
54.7 | 73.4 | <0.001 |
| No. of independent IADL∥ at baseline (of 7), SD† |
4.0 (2.5) | 5.6 (2.1) | <0.001 |
| Education <12 years, % | 42.3 | 39.5 | <0.001 |
| Cardiovascular disease¶ | 42.4 | 35.9 | 0.002 |
| Cancer: solitary | 6.6 | 6.1 | 0.18 |
| Metastatic cancer | 5.2 | 4.0 | |
| Congestive heart failure | 31.0 | 26.9 | 0.04 |
| Dementia | 18.9 | 7.3 | <0.001 |
| COPD# | 18.0 | 23.7 | 0.002 |
| Diabetes | 19.9 | 23.0 | 0.08 |
| Renal disease | 4.8 | 4.0 | 0.47 |
| Albumin <3.5 | 43.3 | 33.4 | <0.001 |
ADL Activities of Daily Living
SD Standard Deviation
APS Acute Physiology Score
NH Nursing Home
IADL Instrumental Activities of Daily Living
Cardiovascular disease is defined as history of stroke, myocardial infarction, peripheral vascular disease or coronary artery disease
COPD Chronic Obstructive Pulmonary Disease
The following variables had some missing data (out of 2279): IADL (n=8); education (n=170); cancer (n=22); CHF (n=22); dementia (n=24); COPD (n=22); diabetes (n=22); APS score (n=7).
Functional Outcomes in the Year After Hospital Discharge
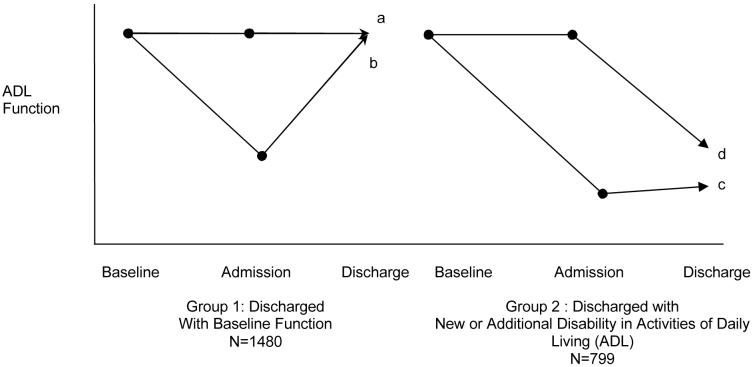
At all time points (1,3,6, and 12 months following discharge), patients discharged with new or additional disability in self-care ADL(n=799) had considerably worse outcomes than patients who were discharged with their baseline function (n=1480)(Figure 2). Most (67%) patients who were discharged at their baseline functional status maintained their baseline level of self-care ADL function in the year after discharge. In contrast, functional outcomes were much poorer in elders who were discharged with new or additional disability in self-care ADL, with high rates of 1-year mortality (41.3%), and less than one third recovering to their baseline level of function. There is also evidence of subsequent decline after recovery.
Figure 2.
Course of self-care Activities of Daily Living (ADL) Outcomes and Survival after Hospitalization
Footnotes:
Discharged at baseline function: N=1480 Discharged with new or additional disability in self-care ADL: N=799
Baseline: at baseline level of self-care ADL function
Decline: with more self-care ADL disabilities compared to baseline level of self-care ADL function
Among patients who were discharged with baseline function(n=1480, Group 1, Figure 1.2), patients who had stable function throughout (trajectory a) had slightly better outcomes than patients who declined between their pre-illness baseline and hospital admission, but then recovered by hospital discharge(trajectory b). At 12 months following discharge, the proportion of patients who were at baseline function was 70% and 60% in these two groups, respectively(p=0.005). Among patients discharged with new or additional disability in self-care ADL (n=799, Group 2, Figure 1.2), rates of recovery by 12 months were similar regardless of whether the patient declined prior to admission, and then failed to recover by discharge(trajectory c), or whether they were admitted with baseline function, but then declined after hospital admission (trajectory d)(30% vs. 31%).
To examine whether better baseline function predicted better functional outcomes, we repeated our analyses in subgroups based on whether or not subjects were independent in all 5 ADL at baseline. The results confirmed that one-year functional outcomes were poor in those with new ADL deficits at discharge regardless of baseline ADL function, though outcomes in those dependent at baseline were worse than in those independent at baseline (20% recovered to baseline ADL function at one year, 28% alive but not recovered, and 51% dead, versus 36%, 27%, and 37%, respectively).
Timing of Functional Recovery
Among those who had a new or additional disability in self-care ADL at hospital discharge, 30% recovered and were at their baseline level of functioning at 1 year. Of these patients, 62% recovered by 1 month with the remainder recovering over the next 11 months. Thus, most recovery, when it happens, occurs in the first month after hospitalization. However, 38% of patients who recovered in the year following discharge do so after the first month after hospitalization. Twenty-two per cent of recovery occurs between 1 and 3 months, with an additional 16% of patients recovering over the next nine months.
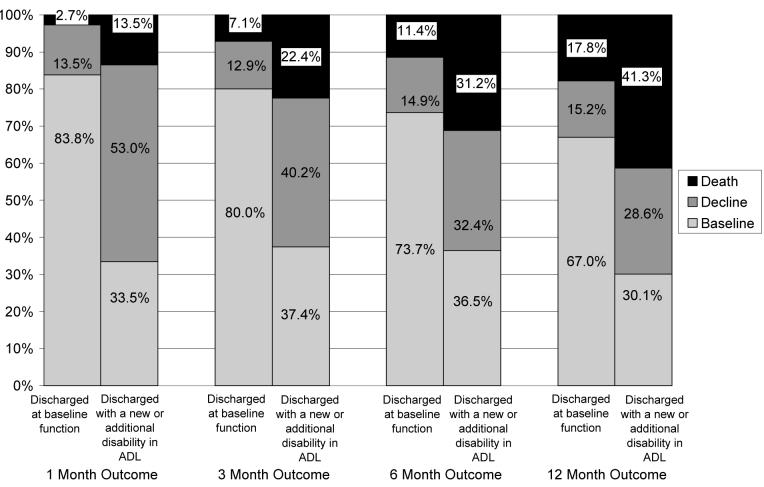
Role of One-Month Outcomes in Predicting Long-term Outcomes
Among patients discharged with a new or additional disability in self-care ADL, the presence or absence of recovery by one month was associated with long-term outcomes. Among those who had recovered by one month after discharge, 56.2% remained at baseline function 1 year after discharge, 20.7% died, and 23.1% declined again in self-care ADL function (Figure 3). In contrast, among those who did not recover by one month after hospital discharge, only 17.1% recovered baseline function at 1 year after discharge, 44.4% died, and 38.4% were alive but not recovered (p<.001).
Figure 3.
Among those discharged with new or additional disability in self-care ADL, recovery to baseline level of self-care Activities of Daily Living by 1 month after discharge (N=651): Association with outcomes over 1 year
Footnotes:
N=651 Of the original sample of those discharged with new or additional disability in self-care ADL (N=799), participants who were alive at discharge but who had died (n=108) or who had missing data at 1 month (n=40) were excluded.
Baseline: recovery to baseline level of self-care Activities of Daily Living (ADL) function
Decline: more self-care ADL disabilities compared to baseline level of self-care ADL function
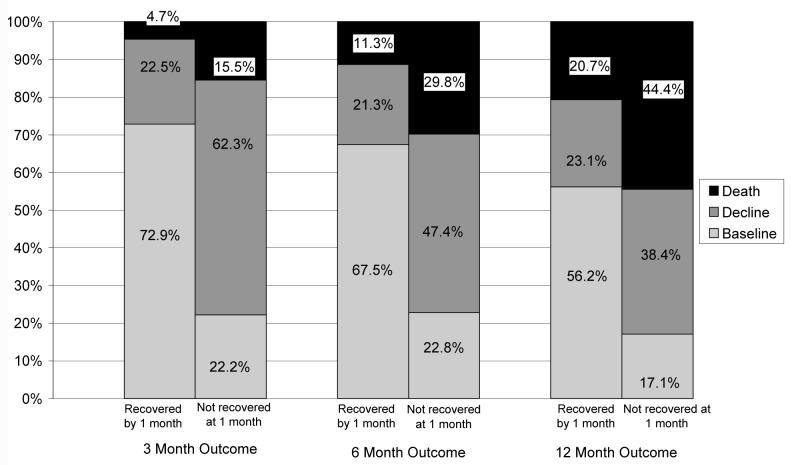
Predictors of Failure to Recover at One Year
Table 2a describes bivariate predictors of failure to recover among those discharged with a new or additional disability in self-care ADL.
Table 2a.
Predictors of Failure to Recover to Baseline Activities of Daily Living Function at 1 year Among Patients Discharged with New or Additional Disability in Activities of Daily Living: Bivariate Analysis (n= 799)
| Characteristic | % Not Recovered to Baseline ADL* function |
P value | |
|---|---|---|---|
| Ethnicity | White Black |
71.1 71.0 |
.97 |
| Gender | Men Women |
73.1 70.1 |
.40 |
| Lives Alone | No Yes |
73.9 65.8 |
.02 |
| Education level, years | 0-8 9-11 12 13-15 16+ |
68 76 72 65 71 |
.83 |
| ADL* at Baseline | Dependent Independent |
79.6 63.6 |
<.001 |
| Number of IADL dependencies at baseline† |
0 1-2 ≥3 |
46.7 69.1 80.4 |
<.001 |
| Cancer | None Solitary Metastatic |
69.0 84.0 87.5 |
.002 |
| Cardiovascular Disease ‡ | No Yes |
66.5 77.2 |
.001 |
| Congestive Heart Failure | No Yes |
68.0 77.6 |
.007 |
| Dementia | No Yes |
67.5 85.6 |
<.001 |
| Chronic Obstructive Pulmonary Disease |
No Yes |
71.7 67.9 |
.37 |
| Diabetes | No Yes |
70.7 72.2 |
.71 |
| Renal | No Yes |
70.6 81.1 |
.17 |
| Admitted from nursing home |
No Yes |
70.4 79.3 |
.15 |
| Age | 70-74 75-79 80-84 85-89 90+ |
65.2 61.7 73.2 71.3 85.9 |
<.001 |
| APS§ | 5-7 8-10 >11 |
67.3 70.2 74.2 |
0.09 |
| Albumin | <3 3-3.4 3.5-3.9 >4 |
74.8 74.0 76.6 61.6 |
0.005 |
In multivariate analysis, the independent predictors of failure to return to baseline function at one year after discharge (either death or worse than baseline functional status) were cancer, cardiovascular disease, dementia, albumin <4, age and number of baseline IADL dependencies (Table 2b), and were similar at 3 months after discharge, with the exception of cardiovascular disease becoming borderline significant. These relative risks are associated with high absolute risks given the high outcome rate in the reference groups. Repeating this analysis excluding subjects who died by one year, the independent predictors of failure to return to baseline function at one year among those who survived (N=469) included age greater than 90 years (RR=1.4, 95% CI 1.0-1.7), cardiovascular disease (RR=1.4, 95% CI 1.2-1.7), dementia (RR=1.4, 95% CI 1.0-1.7), and greater number of baseline IADL dependencies (>2 vs. none, RR=1.9, 95% CI 1.6-2.3), but did not include cancer and albumin.
Table 2b.
Independent predictors of Failure to Return to Baseline Function at 1 year after discharge Among Patients Discharged with New or Additional Disability in Activities of Daily Living (n=799)
| Variable | % not returning to baseline function (low to high risks) |
Unadjusted Risk Ratio (95% CI) |
Adjusted Risk Ratio (95% CI) |
|
|---|---|---|---|---|
| Cancer | None Solitary (7%) Metastatic (5%) |
69% 84% 88% |
Ref 1.22 (1.03-1.33) 1.27 (1.06-1.37) |
Ref 1.25 (1.07-1.36) 1.30 (1.12-1.39) |
| Cardiovascular disease‡ |
No (58%) Yes (42%) |
67% 77% |
Ref 1.16 (1.07-1.23) |
Ref 1.16 (1.06-1.25) |
| Dementia | No (81%) Yes (19%) |
68% 86% |
Ref 1.26 (1.15-1.34) |
Ref 1.21 (1.07-1.30) |
| Albumin | ≥ 4.0 g/dl (30%) <4.0 g/dl (70%) |
62% 75% |
Ref 1.22 (1.11-1.31) |
Ref 1.23 (1.11-1.33) |
| Number of IADL† dependencies at baseline |
0 (22%) 1-2 (17%) > 3 (61%) |
49% 69% 80% |
Ref 1.45 (1.23-1.63) 1.67 (1.54-1.77) |
Ref 1.50 (1.27-1.68) 1.64 (1.49-1.76) |
| Age | <90 (83%) > 90 (17%) |
68% 86% |
Ref 1.26 (1.15-1.34) |
Ref 1.22 (1.08-1.32) |
CI ≥ Confidence Interval
ADL Activities of Daily Living
IADL Instrumental Activities of Daily Living
Cardiovascular disease is defined as history of stroke, myocardial infarction, peripheral vascular disease or coronary artery disease
APS Acute Physiology Score Adjusted for study site and intervention vs. control arm. Neither of these variables were significant.
DISCUSSION
Our results demonstrate that decline in self-care ADL function associated with hospitalization for medical illnesses is often a sentinel and highly-morbid event for elders. The prognosis for elders discharged with new or additional disability in self-care ADL is extremely poor, with only 30% returning to their pre-admission level of self-care ADL functioning by one year. Among those discharged with new or additional disability in self-care ADL, functional recovery by one month is a predictor of one-year outcomes. However, in some cases, time to recovery was prolonged as 38% of those who were at baseline function at one year required more than one month for recovery.
Long-term information on elders’ recovery of function after hospitalization is critically important because large numbers of elders are hospitalized for medical illnesses on an annual basis, and functional decline associated with hospitalization is very common.1-5, 8, 29 Previous reports have documented functional outcomes in hospitalized elders up through 3 months.4, 8, 9, 13, 14 This is one of the first reports to document that the long-term prognosis of hospital-associated new or additional disability in self-care ADL is poor and substantially worse than that observed among community-dwelling elders with disability arising from a broad range of causes.10, 18 Rather, our results suggest that the prognosis for hospital-associated disability in self-care ADL is similar to that reported for other catastrophic conditions such as hip fracture and stroke.30, 31 The processes underlying these long-term outcomes are likely to be complex and highly dynamic.10, 32
Our results have important implications for hospital physicians and providers because they suggest that hospitalized elders may have dramatically higher care needs than before their incident hospitalization. New or additional disabilities in self-care ADL function acquired by the time of hospital discharge have important implications for the patient’s ability to live at home and for their needs for home care services. In addition, the demands on caregivers will markedly increase. As recovery is sometimes prolonged, and some patients who initially recover subsequently decline, our results provide evidence that post-hospitalization functional decline is a chronic, dynamic, long-term process, likely necessitating both acute and chronic services.
The timing, structure, duration and intensity of rehabilitation in acute rehabilitation facilities, long-term care hospitals, skilled nursing facilities, outpatient sites, and home health agencies may not be well suited to the needs of patients with hospital-associated functional decline, whose needs may be long term and chronic. The prospective payment system and diagnosis related groups for acute hospitals and the post-acute sector led to shorter hospital lengths of stay with subsequent increases in post-acute care health utilization and costs during the 1990s.19, 20, 33, 34 While the numbers of patients with medical illnesses receiving post-acute physical, occupational, or speech services has increased in skilled nursing facilities, rehabilitation hospitals, and long-term care hospitals, the amount of rehabilitation received by patients has decreased in some settings and remains of short duration (<1 month).19, 20, 35-37 Little is known about the functional consequences of these utilization changes to older medical patients, or the best way to cost-effectively deliver high quality care that maximizes functional outcomes.
Few elders hospitalized with medical conditions receive acute inpatient rehabilitation.3, 38, 39 The rates of patients with stroke, chronic obstructive pulmonary disease, pneumonia, congestive heart failure, hip fracture receiving inpatient post acute rehabilitation services upon discharge ranged from 0.2%-13% in 1996-1998, with the highest rates observed for stroke and hip fracture.40 Stroke and hip fracture patients have better 1-year functional outcomes if they receive post-acute care, with the best outcomes seen in those discharged to rehabilitation facilities.34 The timing, duration and intensity of therapy are related to functional gains.41, 42 Less is known about patients with functional decline associated with medical illnesses, but therapy intensity is related to gains in mobility, ADL, and executive control among patients with cardiovascular and pulmonary conditions in skilled nursing facilities and increases the likelihood of being discharged to the community.22, 43 Current rehabilitative utilization patterns suggest that many medical patients with functional decline are not receiving the most aggressive short-term intervention available. Possible explanations include inability to meet functional requirements or the requirement that 75% of admissions to inpatient rehabilitation facilities be for specific categorical diagnoses.19, 20, 35-37 It is not known who with medical illness is most likely to benefit from acute rehabilitation, or whether care through home care, skilled nursing facilities, or rehabilitation hospitals would be most likely to improve outcomes.44, 45 Average duration of rehabilitation in all these post-acute sites is relatively short given that 38% of older patients who recover in one year require more than one month to do so. Based on our results, aggressive rehabilitation may be indicated in the first month; but since substantial functional change continues to occur in subsequent months, in many cases it may be important to target longer-term rehabilitation to increase recovery rates and maintain recovery when it occurs.10 Restorative care for older persons receiving home care after acute illness and “prehabilitation” for frail elders, who may have frequent hospitalizations, may be opportunities to maximize functional outcomes.46, 47
Appropriate targeting of older patients for rehabilitation interventions is a critical issue, and current aggressive rehabilitation strategies may be difficult among patients residing in nursing homes or with severe dementia. While our results do not identify which patients are most likely to benefit from interventions, it does suggest that older age, cardiovascular disease, dementia, cancer, lower albumin and prior IADL disability predict failure to recover. It is important that future research also try to distinguish between patients who have the potential for reversibility, and patients for whom this functional decline indicates that the patient is at the end of their life. The high one-year mortality rate among patients with hospital-associated functional decline should prompt consideration of palliative needs. Among patients who are at the end of their life, aggressive palliative interventions focused on symptom management and caregiver support may be more beneficial than interventions aimed at restoring function. Often, it may be appropriate to consider palliative care in tandem with rehabilitative efforts.
LIMITATIONS
While we measured 4 time points over a 12-month period of observation, it is likely that there were additional functional transitions that occurred between observation points.32, 48 It was not our primary goal to describe all the dynamic processes and transitions that occurred over the year following discharge. Second, we were not able to consider all potential predictors of recovery including lack of depressive symptoms, positive affect, and habitual physical activity, and objective measures of strength or physical capabilities.15, 49 Third, we lack data on post-acute utilization of rehabilitative services or recurrent hospitalizations. However; rehabilitation, particularly prolonged, was not widely used for medical patients during the study period, although use of rehabilitation in skilled nursing facilities has increased.38 While data on long-term outcomes of functional decline in the hospital in a large group of older adults presented here were collected beginning in the 1990s, there is no scientific basis to expect that the natural history of functional trajectories have changed. However, it is not known what the effect of shorter length of stays since the study period has had on functional outcomes of older patients. It is possible that now certain additional patients are not at their premorbid level of function prior to discharge. Fourth, we did not have sufficient sample size to look at recovery for specific admission diagnoses or recurrent hospitalizations. Importantly, these older patients were all hospitalized non-electively on general medicine units and, thus, focus on a subset of older adults who experience decline associated with hospitalization for acute illness other than the more commonly studied stroke and hip fracture.
CONCLUSION
Patients discharged with new or additional disability in self-care ADL after medical illness are very high risk for poor outcomes, and should be considered for intensive rehabilitative services during and after discharge from the hospital if this is congruent with the overall goals of care. Since outcomes in the first month seem to predict long-term outcomes, particularly aggressive interventions may be indicated in the first month. However, as a large number of patients may recover after one month, and many who recover by one month decline again, there may also be a need for sustained long-term interventions. Appropriate targeting is likely to be critical in interventions and there is a clear role for palliative and caregiver services, perhaps provided in tandem with rehabilitation focused on maximizing recovery and adapting to new or additional disability. More research is needed to appropriately guide clinical practice and health policy for older adults hospitalized for acute medical illnesses who experience functional decline at hospital discharge.
Supplementary Material
ACKNOWLEDGMENT
Conflict of Interest: Dr. Boyd has been supported by the NIA through the OAIC and received a Pfizer/AGS Junior Faculty Scholars on Health Outcomes Award.
Drs. Landefeld, Covinsky, Palmer, Counsell, Fortinsky, Burant, Kresevic have all received funding from the NIA.
Dr Kresevic has received funding from the VA.
Drs. Landefeld and Boyd have received funding from the John A. Hartford Foundation.
Funding Support: Dr. Boyd was a Pfizer/American Geriatrics Society Junior Faculty Scholar for Research on Health Outcomes during the conduct of this study. Dr. Boyd is a Johns Hopkins Bayview Scholar in the Center for Innovative Medicine. This work was supported by grants from the National Institute on Aging to the Claude Pepper Older Americans Independence Center at Case Western Reserve University and Johns Hopkins University (CMB), National Institute on Aging Grants AG029233, AG00912, and AG10418, The Summa Health System Foundation to Akron City Hospital, and the John A. Hartford Foundation, Inc #2003-0455 to the University of California, San Francisco. This study was approved by Institutional Review Board of Case Western Reserve University. Preliminary results of this work were presented at the Gerontological Society of America Annual Meeting in November, 2004.
Footnotes
Sponsors’ Role: The funding sources had no role in the design and conduct of the study, collection, management, analysis or interpretation of the data, the preparation, review or approval of the manuscript.
REFERENCES
- 1.Ferrucci L, Guralnik JM, Simonsick E, et al. Progressive versus catastrophic disability: A longitudinal view of the disablement process. J Gerontol A Biol Sci Med Sci. 1996;51:M123–130. doi: 10.1093/gerona/51a.3.m123. [DOI] [PubMed] [Google Scholar]
- 2.Gill TM, Williams CS, Tinetti ME. The combined effects of baseline vulnerability and acute hospital events on the development of functional dependence among community-living older persons. J Gerontol A Biol Sci Med Sci. 1999;54:M377–383. doi: 10.1093/gerona/54.7.m377. [DOI] [PubMed] [Google Scholar]
- 3.Ferrucci L, Guralnik JM, Pahor M, et al. Hospital diagnoses, Medicare charges, and nursing home admissions in the year when older persons become severely disabled. JAMA. 1997;277:728–734. [PubMed] [Google Scholar]
- 4.Sager MA, Rudberg MA, Jalaluddin M, et al. Hospital admission risk profile (HARP): identifying older patients at risk for functional decline following acute medical illness and hospitalization. J Am Geriatr Soc. 1996;44:251–257. doi: 10.1111/j.1532-5415.1996.tb00910.x. [DOI] [PubMed] [Google Scholar]
- 5.Boyd CM, Xue QL, Guralnik JM, et al. Hospitalization and development of dependence in dctivities of daily living in a cohort of disabled older women: The Women’s Health and Aging Study I. J Gerontol A Biol Sci Med Sci. 2005;60:888–893. doi: 10.1093/gerona/60.7.888. [DOI] [PubMed] [Google Scholar]
- 6.Boyd CM, Xue QL, Simpson CF, et al. Frailty, hospitalization, and progression of disability in a cohort of disabled older women. Am J Med. 2005;118:1225–1231. doi: 10.1016/j.amjmed.2005.01.062. [DOI] [PubMed] [Google Scholar]
- 7.Gill TM, Allore HG, Holford TR, et al. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292:2115–2124. doi: 10.1001/jama.292.17.2115. [DOI] [PubMed] [Google Scholar]
- 8.Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: Increased vulnerability with age. J Am Geriatr Soc. 2003;51:451–458. doi: 10.1046/j.1532-5415.2003.51152.x. [DOI] [PubMed] [Google Scholar]
- 9.Sager MA, Franke T, Inouye SK, et al. Functional outcomes of acute medical illness and hospitalization in older persons. Arch Intern Med. 1996;156:645–652. [PubMed] [Google Scholar]
- 10.Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004;291:1596–1602. doi: 10.1001/jama.291.13.1596. [DOI] [PubMed] [Google Scholar]
- 11.Gill TM, Robison JT, Tinetti ME. Predictors of recovery in activities of daily living among disabled older persons living in the community. J Gen Intern Med. 1997;12:757–762. doi: 10.1046/j.1525-1497.1997.07161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Magaziner J, Simonsick EM, Kashner TM, et al. Predictors of functional recovery one year following hospital discharge for hip fracture: A prospective study. J Gerontol. 1990;45:M101–107. doi: 10.1093/geronj/45.3.m101. [DOI] [PubMed] [Google Scholar]
- 13.Rudberg MA, Sager MA, Zhang J. Risk factors for nursing home use after hospitalization for medical illness. J Gerontol A Biol Sci Med Sci. 1996;51:M189–194. doi: 10.1093/gerona/51a.5.m189. [DOI] [PubMed] [Google Scholar]
- 14.Mahoney JE, Eisner J, Havighurst T, et al. Problems of older adults living alone after hospitalization. J Gen Intern Med. 2000;15:611–619. doi: 10.1046/j.1525-1497.2000.06139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hardy SE, Gill TM. Factors associated with recovery of independence among newly disabled older persons. Arch Intern Med. 2005;165:106–112. doi: 10.1001/archinte.165.1.106. [DOI] [PubMed] [Google Scholar]
- 16.Walter LC, Brand RJ, Counsell SR, et al. Development and validation of a prognostic index for 1-year mortality in older adults after hospitalization. JAMA. 2001;285:2987–2994. doi: 10.1001/jama.285.23.2987. [DOI] [PubMed] [Google Scholar]
- 17.Inouye SK, Peduzzi PN, Robison JT, et al. Importance of functional measures in predicting mortality among older hospitalized patients. JAMA. 1998;279:1187–1193. doi: 10.1001/jama.279.15.1187. [DOI] [PubMed] [Google Scholar]
- 18.Johnson MF, Kramer AM, Lin MK, et al. Outcomes of older persons receiving rehabilitation for medical and surgical conditions compared with hip fracture and stroke. J Am Geriatr Soc. 2000;48:1389–1397. doi: 10.1111/j.1532-5415.2000.tb02627.x. [DOI] [PubMed] [Google Scholar]
- 19.McCall N, Korb J, Petersons A, et al. Reforming Medicare payment: Early effects of the 1997 Balanced Budget Act on postacute care Milbank Q 200381277–303., 172-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murray PK, Love TE, Dawson NV, et al. Rehabilitation services after the implementation of the nursing home prospective payment system: Differences related to patient and nursing home characteristics. Med Care. 2005;43:1109–1115. doi: 10.1097/01.mlr.0000182490.09539.1e. [DOI] [PubMed] [Google Scholar]
- 21.Shatto A. Comparing Medicare beneficiaries, by type of post-acute care received: 1999. Health Care Financ Rev. 2002;24:137–142. [PMC free article] [PubMed] [Google Scholar]
- 22.Jette DU, Warren RL, Wirtalla C. The relation between therapy intensity and outcomes of rehabilitation in skilled nursing facilities. Arch Phys Med Rehabil. 2005;86:373–379. doi: 10.1016/j.apmr.2004.10.018. [DOI] [PubMed] [Google Scholar]
- 23.Counsell SR, Holder CM, Liebenauer LL, et al. Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older patients: A randomized controlled trial of Acute Care for Elders (ACE) in a community hospital. J Am Geriatr Soc. 2000;48:1572–1581. doi: 10.1111/j.1532-5415.2000.tb03866.x. [DOI] [PubMed] [Google Scholar]
- 24.Covinsky KE, Eng C, Lui LY, et al. The last 2 years of life: Functional trajectories of frail older people. J Am Geriatr Soc. 2003;51:492–498. doi: 10.1046/j.1532-5415.2003.51157.x. [DOI] [PubMed] [Google Scholar]
- 25.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 26.Covinsky KE, Palmer RM, Counsell SR, et al. Functional status before hospitalization in acutely ill older adults: Validity and clinical importance of retrospective reports. J Am Geriatr Soc. 2000;48:164–169. doi: 10.1111/j.1532-5415.2000.tb03907.x. [DOI] [PubMed] [Google Scholar]
- 27.Knaus WA, Draper EA, Wagner DP, et al. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 28.Zhang J, Yu KF. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 29.Kozak LJ, DeFrances CJ, Hall MJ. National hospital discharge survey: 2004 annual summary with detailed diagnosis and procedure data. Vital Health Stat. 2006;162:1–209. [PubMed] [Google Scholar]
- 30.Magaziner J, Fredman L, Hawkes W, et al. Changes in functional status attributable to hip fracture: A comparison of hip fracture patients to community-dwelling aged. Am J Epidemiol 1. 2003;157:1023–1031. doi: 10.1093/aje/kwg081. [DOI] [PubMed] [Google Scholar]
- 31.Tilling K, Sterne JA, Rudd AG, et al. A new method for predicting recovery after stroke. Stroke. 2001;32:2867–2873. doi: 10.1161/hs1201.099413. [DOI] [PubMed] [Google Scholar]
- 32.Hardy SE, Dubin JA, Holford TR, et al. Transitions between states of disability and independence among older persons. Am J Epidemiol. 2005;161:575–584. doi: 10.1093/aje/kwi083. [DOI] [PubMed] [Google Scholar]
- 33.Ottenbacher KJ, Smith PM, Illig SB, et al. Trends in length of stay, living setting, functional outcome, and mortality following medical rehabilitation. JAMA. 2004;292:1687–1695. doi: 10.1001/jama.292.14.1687. [DOI] [PubMed] [Google Scholar]
- 34.Kane RL, Chen Q, Finch M, et al. Functional outcomes of posthospital care for stroke and hip fracture patients under medicare. J Am Geriatr Soc. 1998;46:1525–1533. doi: 10.1111/j.1532-5415.1998.tb01537.x. [DOI] [PubMed] [Google Scholar]
- 35.Yip JY, Wilber KH, Myrtle RC. The impact of the 1997 Balanced Budget Amendment’s prospective payment system on patient case mix and rehabilitation utilization in skilled nursing. Gerontologist. 2002;42:653–660. doi: 10.1093/geront/42.5.653. [DOI] [PubMed] [Google Scholar]
- 36.Wodchis WP, Fries BE, Pollack H. Payer incentives and physical rehabilitation therapy for nonelderly institutional long-term care residents: Evidence from Michigan and Ontario. Arch Phys Med Rehabil. 2004;85:210–217. doi: 10.1016/s0003-9993(03)00616-6. [DOI] [PubMed] [Google Scholar]
- 37.Murtaugh CM, McCall N, Moore S, et al. Trends in Medicare home health care use: 1997-2001. Health Aff (Millwood) 2003;22:146–156. doi: 10.1377/hlthaff.22.5.146. [DOI] [PubMed] [Google Scholar]
- 38.Gage B. Impact of the BBA on post-acute utilization. Health Care Financ Rev. 1999;20:103–126. [PMC free article] [PubMed] [Google Scholar]
- 39.Buechner JS, Donnelly EF. Utilization of inpatient rehabilitation services. Med Health R I. 2001;84:412–413. [PubMed] [Google Scholar]
- 40.Kane RL, Lin WC, Blewett LA. Geographic variation in the use of post-acute care. Health Serv Res. 2002;37:667–682. doi: 10.1111/1475-6773.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen CC, Heinemann AW, Granger CV, et al. Functional gains and therapy intensity during subacute rehabilitation: A study of 20 facilities. Arch Phys Med Rehabil. 2002;83:1514–1523. doi: 10.1053/apmr.2002.35107. [DOI] [PubMed] [Google Scholar]
- 42.Penrod JD, Boockvar KS, Litke A, et al. Physical therapy and mobility 2 and 6 months after hip fracture. J Am Geriatr Soc. 2004;52:1114–1120. doi: 10.1111/j.1532-5415.2004.52309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arling G, Williams AR, Kopp D. Therapy use and discharge outcomes for elderly nursing home residents. Gerontologist. 2000;40:587–595. doi: 10.1093/geront/40.5.587. [DOI] [PubMed] [Google Scholar]
- 44.Intrator O, Berg K. Benefits of home health care after inpatient rehabilitation for hip fracture: Health service use by Medicare beneficiaries, 1987-1992. Arch Phys Med Rehabil. 1998;79:1195–1199. doi: 10.1016/s0003-9993(98)90261-1. [DOI] [PubMed] [Google Scholar]
- 45.Hadley J, Rabin D, Epstein A, et al. Posthospitalization home health care use and changes in functional status in a Medicare population. Med Care. 2000;38:494–507. doi: 10.1097/00005650-200005000-00006. [DOI] [PubMed] [Google Scholar]
- 46.Tinetti ME, Baker D, Gallo WT, et al. Evaluation of restorative care vs usual care for older adults receiving an acute episode of home care. JAMA. 2002;287:2098–2105. doi: 10.1001/jama.287.16.2098. [DOI] [PubMed] [Google Scholar]
- 47.Gill TM, Baker DI, Gottschalk M, et al. A prehabilitation program for physically frail community-living older persons. Arch Phys Med Rehabil. 2003;84:394–404. doi: 10.1053/apmr.2003.50020. [DOI] [PubMed] [Google Scholar]
- 48.Guralnik JM, Ferrucci L. Underestimation of disability occurrence in epidemiological studies of older people: Is research on disability still alive? J Am Geriatr Soc. 2002;50:1599–1601. doi: 10.1046/j.1532-5415.2002.50421.x. [DOI] [PubMed] [Google Scholar]
- 49.Ostir GV, Goodwin JS, Markides KS, et al. Differential effects of premorbid physical and emotional health on recovery from acute events. J Am Geriatr Soc. 2002;50:713–718. doi: 10.1046/j.1532-5415.2002.50167.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.