Abstract
Objective
To determine the usefulness of perfusion MR imaging in assessing the histologic grade of cerebral gliomas.
Materials and Methods
In order to determine relative cerebral blood volume (rCBV), 22 patients with pathologically proven gliomas (9 glioblastomas, 9 anaplastic gliomas and 4 low-grade gliomas) underwent dynamic contrast-enhanced T2*-weighted and conventional T1- and T2-weighted imaging. rCBV maps were obtained by fitting a gamma-variate function to the contrast material concentration versus time curve. rCBV ratios between tumor and normal white matter (maximum rCBV of tumor / rCBV of contralateral white matter) were calculated and compared between glioblastomas, anaplastic gliomas and low-grade gliomas.
Results
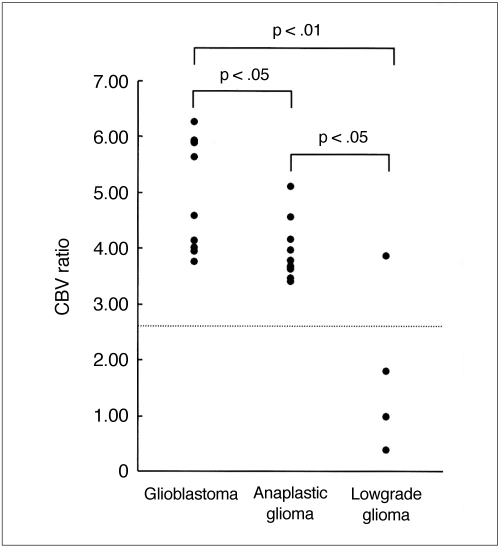
Mean rCBV ratios were 4.90°±1.01 for glioblastomas, 3.97°±0.56 for anaplastic gliomas and 1.75°±1.51 for low-grade gliomas, and were thus significantly different; p < .05 between glioblastomas and anaplastic gliomas, p < .05 between anaplastic gliomas and low-grade gliomas, p < .01 between glioblastomas and low-grade gliomas. The rCBV ratio cutoff value which permitted discrimination between high-grade (glioblastomas and anaplastic gliomas) and low-grade gliomas was 2.60, and the sensitivity and specificity of this value were 100% and 75%, respectively.
Conclusion
Perfusion MR imaging is a useful and reliable technique for estimating the histologic grade of gliomas.
Keywords: Brain neoplasms, MR; Brain, blood flow; Cerebral blood vessels, flow dynamics; Magnetic resonance (MR), contrast enhancement
Gliomas are the most common primary neoplasms of the brain (1), varying histologically from low grade (relatively benign) to high grade (malignant). Even a single tumor mass may be histologically heterogeneous, and at biopsy their grade thus tends to be underestimated. For planning the optimal treatment strategy and assessing prognosis, accurate histologic grading is essential, and for this, vascular proliferation is an important criteria; in determining the histologic grade of a glioma, the evaluation of tumor vascularity is therefore valuable (2-5). Recent developments in perfusion MR imaging techniques have permitted the creation of relative cerebral blood volume (rCBV) maps, leading to the qualitative and quantitative assessment of tumor vascularity (6-14). These maps have helped in the assessment of tumor grade and in targeting the site of biopsy (15, 16). Although a few studies have reported good correlation between rCBV and the histologic grade of gliomas (5, 15, 16), no study-to the best of our knowledge-has assessed the sensitivity and specificity of rCBV measurement for discriminating between high-grade and low-grade tumors.
The purpose of this study was to assess the relationship between rCBV and the histologic grade of gliomas and to determine the rCBV ratio cutoff value which permitted discrimination between high-grade and low-grade gliomas, and the sensitivity and specificity of this value.
MATERIALS AND METHODS
Patients
We retrospectively investigated 24 consecutive patients with gliomas who had undergone both conventional and perfusion MR imaging during a four-year period. Two patients with pilocytic astrocytomas were excluded because these tumors, classified as circumscribed astrocytomas, are more benign than diffuse infiltrating gliomas and do not usually progress to malignancy. Consequently, 22 patients with diffuse infiltrating gliomas were included in this study. Sixteen were male and six were female, and their ages ranged from nine to 71 (mean, 41) years. The presence of gliomas was confirmed by surgical resection (n = 16), or by stereotactic biopsy (n = 6). All tumors were graded according to the World Health Organization grading system (17); there were four grade-2 astrocytomas, nine grade-3 anaplastic gliomas [anaplastic astrocytoma (n = 6), anaplastic oligodendroglioma (n = 2), anaplastic oligoastrocytoma (n = 1)], and nine grade-4 glioblastomas. Tumors were lolocated in the cerebral hemisphere in 14 cases, the basal ganglia in five, and the cerebellum in three.
MR imaging studies
MR examinations were performed on a Siemens 1.5-T 63SP system (Erlangen, Germany) using the following imaging sequences: axial turbo spin-echo T2-weighted, axial spin-echo T1-weighted, dynamic contrast-enhanced T2*-weighted (for perfusion imaging), and axial postcontrast T1-weighted. The imaging parameters were 3500/90 (repetition time msec/echo time msec) for T2-weighted and 550/14 for pre- and postcontrast T1-weighted imaging. The section thickness/gap was 5-6/1.5-1.8 mm and the matrix was 200×256.
For dynamic contrast-enhanced T2*-weighted imaging, a conventional gradient-echo sequence (40/26, 10° flip angle, 64×128 matrix, 5-6 mm slice thickness, 3.8 sec acquisition time) was used. In order to include the largest solid portion of the tumor on the basis of the findings of T1- and T2-weighted imaging, 17-20 serial, single-section dynamic images were obtained. Within 5 seconds of the acquisition of the first three images, a Gd-DTPA (Magnevist, 0.2 mmol/kg; Schering, Germany) or gadodiamide (Omniscan, 0.2 mmol/kg; Nycomed, Norway) bolus was administered manually via a forearm vein, followed by a flush of 30 ml saline. After the initiation of bolus injection, approxinatel, bosecs were required for imaging.
Generation of rCBV maps
All dynamic MR images were transferred to a personal computer via ethernet, and were evaluated with home made software. For the creation of rCBV map, an exponential relationship between relative signal reduction and contrast material concentration was assumed. To fit a gamma-variate function to the contrast material concentration versus time curve on a pixel-by-pixel basis, the non-linear regression method was used (18, 19). The rCBV of each pixel was then calculated by numerical integration of the area under the concentration-time curve (i.e. rCBV = ∫ C(t)dt) (20). Thus, increased signal intensity on the rCBV map indicated increased rCBV, and vice versa.
Data analysis
On an rCBV map, a region-of-interest (ROI), including at least 20 pixels, was placed in the solid portion of a tumor for measurement of rCBV. This was measured at least three times, and for further analysis, its maximum value was chosen. An rCBV obtained by our method is not an absolute quantity, and for this reason, results were normalized by calculating rCBV ratio (i.e. maximum rCBV of a tumor divided by that of white matter). The rCBV of white matter was obtained by placing the ROI, including at least 20 pixels, in contralateral frontal and occipital (or parietal) white matter, and averaging those rCBV values. In three cases of cerebellar tumors, the ROI was placed in contralateral central white matter.
To assess the relationship between rCBV ratio and histologic tumor grade, we compared rCBV ratios between glioblastomas, anaplastic gliomas, and low-grade gliomas using the Kruskal-Wallis and Mann-Whitney U tests. The latter was also used for comparing rCBV ratios between high-grade (glioblastomas and anaplastic gliomas) and low-grade gliomas. To calculate the rCBV ratio cutoff value which permits discrimination between high-grade and low-grade gliomas, and the sensitivity and specificity of this value, univariate discriminant analysis was used. For statistical computation, an SPSS statistical software package (SPSS, Chicago, Ill.) was employed, with the level of significance defined as p < .05.
RESULTS
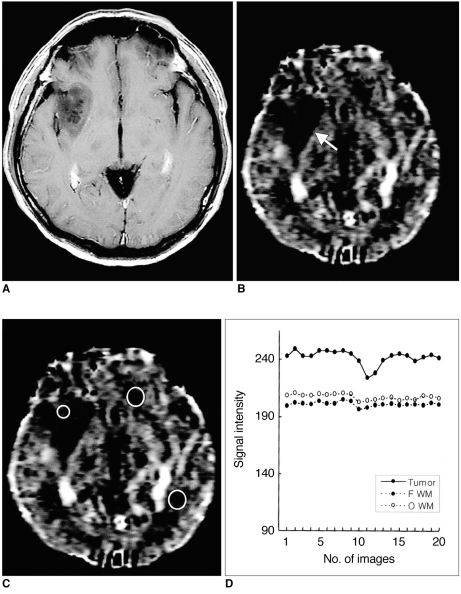
Table 1 summarizes the rCBV ratios of all tumors. These were 3.75-6.26 (mean, 4.90±1.01) in glioblastomas (Fig. 1), 3.40-5.11 (mean, 3.97±0.56) in anaplastic gliomas (Fig. 2), and 0.39-3.85 (mean, 1.75±1.51) in low-grade gliomas (Fig. 3). The overall group difference in rCBV ratios between these three tumor groups was statistically significant (p < .01, using the Kruskal-Wallis test). Individual group differences in rCBV ratios were also significant (p < .05 between glioblastomas and anaplastic gliomas, p < .05 between anaplastic gliomas and low-grade gliomas, and p < .01 between glioblastomas and low-grade gliomas, using the Mann-Whitney U test) (Fig. 4). The rCBV ratios of high-grade gliomas, including glioblastomas and anaplastic gliomas, were 3.40-6.26 (mean, 4.44±0.93), and were statistically significantly higher than those of low-grade gliomas (p < .05, using the Mann-Whitney U test). The rCBV ratio cutoff value which permitted discrimination between high-grade (i.e. glioblastomas and anaplastic gliomas) and low-grade gliomas was 2.60. The sensitivity and specificity of this value were 100% (18/18) and 75% (3/4), respectively.
Table 1.
Relative Cerebral Blood Volume Ratios of 22 Patients with Gliomas
Note.-rCBV = relative cerebral blood volume, L = left, R = right
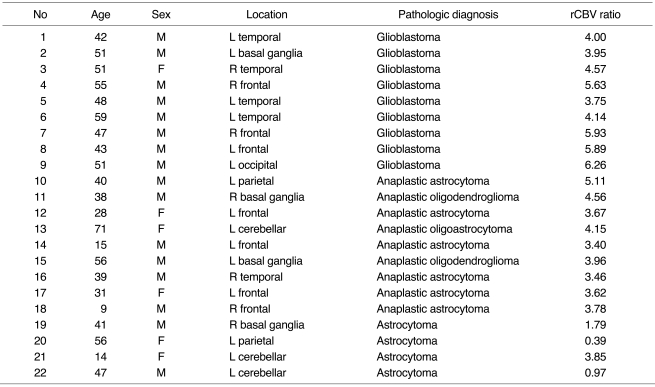
Fig. 1.
Case 7: Glioblastoma in a 47-year-old man.
A. Postcontrast T1-weighted image shows a ring-enhancing necrotic tumor in the right frontal lobe.
B. Relative cerebral blood volume (rCBV) map shows high rCBV in the solid portion of the tumor (arrow). The higher signal on the rCBV map represents a higher rCBV.
C. rCBV map shows the placement of ROIs for measurement of rCBV in the tumor (black circle) and in contralateral frontal and parietal white matter (white circles).
D. Signal intensity-time curves measured at ROIs in C show different patterns of signal reduction between tumor and normal white matter during the transit of contrast material. Remarkable reduction of signal intensity is noted in the tumor compared to normal white matter, suggesting tumor hypervascularity.
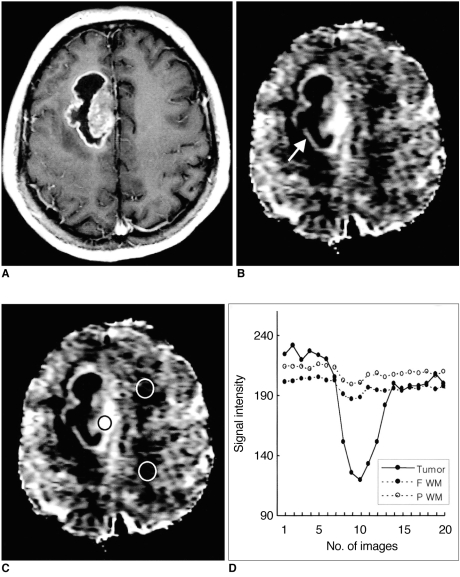
Fig. 2.
Case 15: Anaplastic oligodendroglioma in a 56-year-old man.
A. Postcontrast T1-weighted image shows a strongly enhancing solid tumor in the left basal ganglia.
B. Relative cerebral blood volume (rCBV) map shows heterogeneously increased rCBV in the tumor (arrow).
C. rCBV map shows the placement of ROIs for measurement of rCBV in the tumor (black circle) and in contralateral frontal and occipital white matter (white circles).
D. Signal intensity-time curves measured at ROIs in C show different patterns of signal reduction between tumor and normal white matter, suggesting tumor hypervascularity.
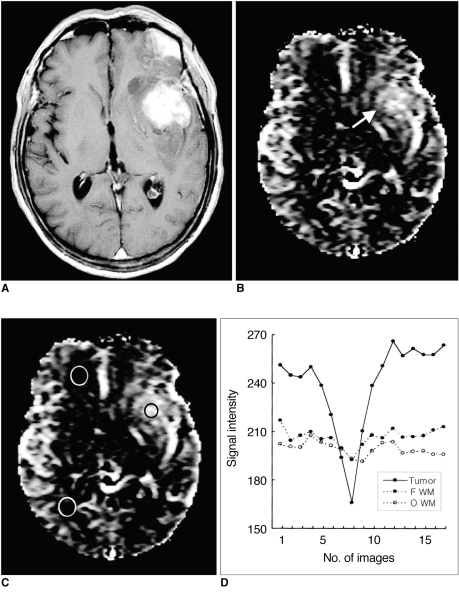
Fig. 3.
Case 19: Low-grade astrocytoma in a 41-year-old man.
A. Postcontrast T1-weighted image shows a non-enhancing low signal intensity tumor in the right basal ganglia.
B. Relative cerebral blood volume (rCBV) map shows low rCBV in the tumor (arrow).
C. rCBV map shows the placement of ROIs for measurement of rCBV in the tumor (small circle) and in contralateral frontal and occipital white matter (large circles).
D. Signal intensity-time curves measured at ROIs in C show less signal reduction in this tumor than in the high-grade gliomas seen in Figs. 1 and 2, suggesting that the vascularity of an astrocytoma is lower.
Fig. 4.
Plot of relative cerebral blood volume (rCBV) ratios in glioblastomas, anaplastic gliomas and low-grade gliomas. The rCBV ratio is highest in glioblastomas and lowest in low-grade gliomas. A comparison of mean rCBV ratios in each tumor group shows statistically significant differences between them. The dotted horizontal line represents the rCBV ratio cutoff value (2.60) which permitted discrimination between high-grade (glioblastomas and anaplastic gliomas) and low-grade gliomas.
DISCUSSION
Gliomas are the most common neoplasm of the brain, and have a heterogeneous histologic spectrum from low-grade astrocytomas to glioblastomas (1). In spite of improvements in the results of surgery, radiation therapy and chemotherapy, the prognosis of patients with gliomas, particularly those with high-grade tumors, remains poor. For planning the optimal treatment strategy, accurate determination of tumor grade is critical, and in most histologic grading systems, vascular proliferation of gliomas is a diagnostic criterion for malignancy (1, 17, 21). Although conventional MR imaging with gadolinium-based contrast enhancement has been useful for grading gliomas, contrast enhancement itself reflects disruption of the blood-brain barrier, not tumor angiogenesis. The area of contrast enhancement observed does not indicate the most malignant portion of the tumor and should not be the only target site for biopsy (16).
Perfusion MR imaging methods include the arterial spintagging and the first-pass contrast techniques. The former does not require the use of contrast material, but is limited by its sensitivity to motion and low contrast-to-noise ratio (22), and for these reasons it has not been widely used in the clinical field. The first-pass technique is based on the reduction of signal intensity due to local field inhomogeneity induced by contrast material within the blood vessels during the period in which contrast material first passes through the brain (23). The reduction is proportional to regional CBV and the concentration of contrast material. Both the spin-echo and gradient-echo techniques can be utilized for first-pass perfusion imaging. The former is more sensitive in detecting tumor vascularity at the capillary level (i.e. microvasculature) than at the large vessel level (5). In contrast, the gradient-echo technique is sensitive to the total volume of blood contained in both capillaries and large vessels (15). Since high-grade gliomas contain both these types of vessel, the gradient-echo technique is more suitable for assessing tumor vascularity. Sugahara et al. (15) reported that the rCBV of gliomas measured by gradient-echo perfusion imaging correlated well with the histopathologic and angiographic findings of tumor vascularity. In our study, the rCBV obtained by gradient-echo perfusion imaging also increased with tumor grade, in accordance with the demonstrated close correspondence between rCBV and tumor grade. Since gradient-echo perfusion imaging findings thus reflect tumor vascularity, the modality can play an important role in the noninvasive determination of which portion of a tumor is most malignant.
The rCBV ratios of gliomas have been described in several previous studies. Aronen et al. (5) reported them to be 0.82-5.40 (mean, 3.64) in high-grade gliomas (glioblastomas and anaplastic astrocytomas), and 1.10-1.21 (mean, 1.11) in low-grade gliomas. Sugahara et al. (15) found that the rCBV ratios of glioblastomas, anaplastic astrocytomas and low-grade gliomas were 4.00-16.20 (mean, 7.32), 0.98-7.93 (mean, 4.61) and 0.64-2.01 (mean, 1.26), respectively; according to Knopp et al. (16), these ratios were 1.73-13.70 (mean, 5.07) in high-grade gliomas and 0.92-2.19 (mean, 1.44) in low-grade. Although these studies showed a wide range of rCBV ratios, and overlapping between tumors of different grades, there were statistically significantly differences between high-grade and low-grade gliomas, as in our study. We found that the rCBV ratio cutoff value which permitted discrimination between high-grade and low-grade gliomas was 2.60, with 100% sensitivity and 75% specificity. All our results suggest that perfusion MR imaging is a valuable technique for assessing the histologic grade of gliomas. In the clinical field, however, it should be borne in mind that rCBV ratios may differ according to the imaging technique employed (i.e. the imaging sequence, amount of contrast material for bolus injection, and duration of contrast injection).
Perfusion MR imaging of gliomas can be used to monitor response to treatment as well as to determine histologic grade. Reductions in rCBV have been reported after radiation therapy (24, 25) and during antiangiogenic therapy (26). rCBV data have also been utilized to distinguish tumor recurrence and non-neoplastic contrast-enhancing tissue after radiation therapy (27), though to ascertain the usefulness of perfusion MR imaging in this field, further investigation is needed.
This study suffers from several technical limitations. First, dynamic contrast-enhanced T2*-weighted imaging technique can evaluate only a single section rather than a complete tumor, and this raises concerns about the reliability of the data thus obtained. The second limitation is the relatively low temporal resolution of the imaging, which provides only a few data points useful for tracking the first pass of contrast material. These shortcomings could, however limitations could be mitigated by using the echo-planar imaging technique, which has become increasingly available in the clinical field.
In conclusion, dynamic contrast-enhanced T2*-weighted perfusion MR imaging performed in these 22 cases provided valuable information about the vascularity of gliomas, and led to the correct assessment of histologic tumor grade. The modality is thus a useful and dependable means of noninvasively assessing the histologic grade of gliomas.
Footnotes
This study was supported by grant number HMP-97-NM-2-0038 from the Good Health R&D Project, Ministry of Health and Welfare, and the Brain Korea 21 Project, Ministry of Education, South Korea.
References
- 1.Russell D, Rubinstein L. Tumours of central neuroepithelial origin. In: Rubinstein LJ, editor. Pathology of tumours of the central nervous system. Baltimore, Md.: Williams & Wilkins; 1989. pp. 83–350. [Google Scholar]
- 2.Van Kirk OC, Cornell SH, Jacoby CG. Posterior fossa intraaxial tumors: a comparision of computed tomography with other imaging methods. J Comput Assist Tomogr. 1979;3:31–39. doi: 10.1016/0149-936x(79)90058-4. [DOI] [PubMed] [Google Scholar]
- 3.Joyce P, Bentson J, Takahashi M, Winter J, Wilson G, Byrd S. The accuracy of predicting histologic grades of supratentorial astrocytomas on the basis of computerized tomography and cerebral angiography. Neuroradiology. 1978;16:346–348. doi: 10.1007/978-3-642-66959-0_114. [DOI] [PubMed] [Google Scholar]
- 4.Seeger JF, Burke DP, Knake JE, Gabrielsen TO. Computed tomographic and angiographic evaluation of hemangioblastoma. Radiology. 1981;138:65–73. doi: 10.1148/radiology.138.1.7192875. [DOI] [PubMed] [Google Scholar]
- 5.Aronen HJ, Gazit IE, Louis DN, et al. Cerebral blood volume maps of gliomas: comparision with tumor grade and histologic findings. Radiology. 1994;191:41–51. doi: 10.1148/radiology.191.1.8134596. [DOI] [PubMed] [Google Scholar]
- 6.Edelman RR, Mattle HP, Atkinson DJ, et al. Cerebral blood flow: assessment with dynamic contrast-enhanced T2*-weighted MR imaging at 1.5T. Radiology. 1990;176:211–220. doi: 10.1148/radiology.176.1.2353094. [DOI] [PubMed] [Google Scholar]
- 7.Rosen BR, Belliveau JW, Aronen HJ, et al. Susceptibility contrast imaging of cerebral blood volume: human experience. Magn Reson Med. 1991;22:293–299. doi: 10.1002/mrm.1910220227. [DOI] [PubMed] [Google Scholar]
- 8.Aronen HJ, Cohen MS, Belliveau JW, Fordham JA, Rosen BR. Ultrafast imaging of brain tumors. Top Magn Reson Imaging. 1993;5:14–24. [PubMed] [Google Scholar]
- 9.Le Bihan D, Douek P, Argyropoulou M, Turner R, Patronas N, Fulham M. Diffusion and perfusion magnetic resonance imaging in brain tumors. Top Magn Reson Imaging. 1993;5:25–31. [PubMed] [Google Scholar]
- 10.Maeda M, Itoh S, Kimura H, et al. Tumor vascularity in the brain: evaluation with dynamic susceptibility-contrast MR imaging. Radiology. 1993;189:233–238. doi: 10.1148/radiology.189.1.8372199. [DOI] [PubMed] [Google Scholar]
- 11.Maeda M, Itoh S, Kimura H, et al. Vascularity of meningioma and neuroma: assessment with dynamic susceptibility-contrast MR imaging. AJR. 1994;163:181–186. doi: 10.2214/ajr.163.1.8010210. [DOI] [PubMed] [Google Scholar]
- 12.Kim JS, Lee GK, Kim JH, et al. Blood volume of intraaxial brain tumor: evaluation with dynamic contrast-enhanced T2*-weighted MR imaging. J Korean Radiol Soc. 1997;37:783–788. [Google Scholar]
- 13.Kim HD, Chang KH, Song IC, et al. Perfusion MR imaging of the brain tumor: preliminary report. J Korean Soc Magn Reson Med. 1997;1:119–124. [Google Scholar]
- 14.Choi JY, Sun JS, Kim SY, et al. Effect of steroid on brain tumors and surround edemas: observation with regional cerebral blood volume (rCBV) maps of perfusion MRI. J Korean Radiol Soc. 2000;42:15–21. [Google Scholar]
- 15.Sugahara T, Korogi Y, Kochi M, et al. Correlation of MR imaging-determined cerebral blood volume maps with histologic and angiographic determination of vascularity of gliomas. AJR. 1998;171:1479–1486. doi: 10.2214/ajr.171.6.9843274. [DOI] [PubMed] [Google Scholar]
- 16.Knopp EA, Cha S, Johnson G, et al. Glial neoplasms: dynamic contrast-enhanced T2*-weighted MR imaging. Radiology. 1999;211:791–798. doi: 10.1148/radiology.211.3.r99jn46791. [DOI] [PubMed] [Google Scholar]
- 17.Kleihues P, Burger PC, Scheithauer BW. Histologic typing of tumours of the central nervous system. 2nd ed. Berlin, Germany: Springer-Verlag; 1993. pp. 11–30. [Google Scholar]
- 18.Thompson HK, Starmer CF, Whalen RE, McIntosh HD. Indicator transit time considered as a gamma variate. Circ Res. 1964;14:502–515. doi: 10.1161/01.res.14.6.502. [DOI] [PubMed] [Google Scholar]
- 19.Benner T, Heiland S, Erb G, Forsting M, Sartor K. Accuracy of gamma-variate fits to concentration-time curves from dynamic susceptibility-contrast MRI: influence of time resolution, maximal signal drop and signal-to-noise. Magn Reson Imaging. 1997;15:307–317. doi: 10.1016/s0730-725x(96)00392-x. [DOI] [PubMed] [Google Scholar]
- 20.Rosen BR, Belliveau JW, Vevea JM, et al. Perfusion MR imaging with NMR contrast agents. Magn Reson Med. 1990;14:249–265. doi: 10.1002/mrm.1910140211. [DOI] [PubMed] [Google Scholar]
- 21.Brem S, Cotran R, Folkman J. Tumor angiogenesis: a quantitative method for histologic grading. J Natl Cancer Inst. 1972;48:347–356. [PubMed] [Google Scholar]
- 22.Edelman RR, Siewert B, Darby DG, et al. Quantitative mapping of cerebral blood flow and functional localization with echo-planar MR imaging and signal targeting with alternating radiofrequency. Radiology. 1994;192:513–520. doi: 10.1148/radiology.192.2.8029425. [DOI] [PubMed] [Google Scholar]
- 23.Belliveau JW, Rosen BR, Kantor HL, et al. Functional cerebral imaging by susceptibility contrast NMR. Magn Reson Med. 1990;14:538–546. doi: 10.1002/mrm.1910140311. [DOI] [PubMed] [Google Scholar]
- 24.Gückel F, Brix G, Rempp K, Deimling M, Rother J, Georgi M. Assessment of cerebral blood volume with dynamic susceptibility contrast enhanced gradient echo imaging. J Comput Assist Tomogr. 1994;18:344–351. doi: 10.1097/00004728-199405000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Wenz F, Rempp K, Hess T, et al. Effect of radiation on blood volume in low-grade astrocytomas and normal brain tissue: quantification with dynamic susceptibility contrast MR imaging. AJR. 1996;166:187–193. doi: 10.2214/ajr.166.1.8571873. [DOI] [PubMed] [Google Scholar]
- 26.Cha S, Knopp EA, Johnson G, et al. Dynamic contrast-enhanced T2*-weighted MR imaging of recurrent malignant gliomas treated with thalidomide and carboplatin. AJNR. 2000;21:881–890. [PMC free article] [PubMed] [Google Scholar]
- 27.Sugahara T, Korogi Y, Tomiguchi S, et al. Posttherapeutic intraaxial brain tumor: the value of perfusion-sensitive contrast-enhanced MR imaging for differentiating tumor recurrence from nonneoplastic contrast-enhancing tissue. AJNR. 2000;21:901–909. [PMC free article] [PubMed] [Google Scholar]