Abstract
Objective
The purpose of this study was to determine, when measuring prostate volume by TRUS, whether height is more accurately determined by transaxial or midsagittal scanning.
Materials and Methods
Sixteen patients who between March 1995 and March 1998 underwent both preoperative TRUS and radical prostatectomy for prostate cancer were included in this study. Using prolate ellipse volume calculation (height × length × width × π/6), TRUS prostate volume was determined, and was compared with the measured volume of the specimen .
Results
Prostate volume measured by TRUS, regardless of whether height was determined transaxially or midsagittally, correlated closely with real specimen volume. When height was measured in one of these planes, a paired t test revealed no significant difference between TRUS prostate volume and real specimen volume (p = .411 and p = .740, respectively), nor were there significant differences between the findings of transaxial and midsagittal scanning (p = .570). A paired sample test, however, indicated that TRUS prostate volumes determined transaxially showed a higher correlation coefficient (0.833) and a lower standard deviation (9.04) than those determined midsagittally (0.714 and 11.48, respectively).
Conclusion
Prostate volume measured by TRUS closely correlates with real prostate volume. Furthermore, we suggest that when measuring prostate volume in this way, height is more accurately determined by transaxial than by midsagittal scanning.
Keywords: Prostate, US; Prostate, hypertrophy; Ultrasound (US), technology
Since prostate volume may influence the operative approach in patients with prostatism, its estimation is of concern to urologists. Prostate volume has been measured by various methods including digital rectal examination, cystourethrography, urethrocystoscopy, and urethral pressure profile, but all of these are inaccurate (1-3). For this reason, ultrasound scanning has gained wide popularity in the past few years (4-10). Three different ultrasound approaches are available: the transrectal, the transurethral, and the transabdominal, though prostate volume measurement using the transrectal approach appears to be most accurate (4, 10).
Three commonly used prostate volume measurement techniques in transrectal ultrasonography (TRUS) are planimetry calculation, prolate ellipse volume calculation, and an ellipsoid volume measurement technique. Prolate ellipse volume calculation is fast and precise, and its universal availability makes it practical for routine clinical application. It is calculated as follows: prolate ellipse volume (centimeters) = (height × length × width) × π/6. Transverse diameter (width) is defined as the maximal transverse diameter at mid-gland level, while longitudinal diameter (length) is defined as the distance from the proximal external sphincter to the urinary bladder (11).
Anteroposterior diameter (height) may be measured in two planes-axial and sagittal. Most authors have employed midsagittal scanning, but some have measured the diameter perpendicular to the transverse diameter seen on transaxial scans (12). By comparing the findings with real specimen volume, we aimed to determine whether height is more accurately determined by transaxial or midsagittal scanning.
MATERIALS AND METHODS
Sixteen patients aged between 51 and 73 (mean, 62) years who underwent preoperative TRUS and radical prostatectomy for prostate cancer were included in this study. Using a HDI 3000 scanner (Advanced Technology Laboratories, Bothell, Wash) with using a 10MHz transverse sector probes, and calculating prolate ellipse volume by means of the (height × length × width × π/6) formula, prostate volume was measured and then compared with real specimen volume (Fig. 1).
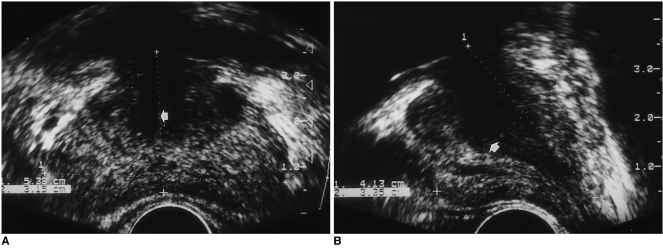
Fig. 1.
Measurement of prostate volume by TRUS
A. Height (arrow) was measured by transaxial scanning (3.15 cm), and prostate volume was calculated as 36.1 cc.
B. Height (arrow) was measured by midsagittal scanning (3.35 cm), and prostate volume was calculated as 35.0 cc. Specimen volume was 45.81 cc.
The volume of gross pathologic specimens (prostate only) was calculated using the formula for prolate ellipse volume calculation, measuring three unequal axes of the prostatectomy specimen within 1hr of excision. Triaxial measurements of the prostate were thus obtained. The transverse diameter was recorded at the point of maximal transverse diameter perpendicular to the anteroposterior plane of the prostate. The anterior-posterior diameter was recorded in the transverse plane at a point perpendicular to the greatest transverse diameter, while the longitudinal diameter was recorded as the distance between the junction of the bladder neck and the prostate, and the prostatic apex at the genitourinary diaphragm. Prior to measurement, all specimens were immersed in normal saline to minimize tissue dessication.
Statistical analysis using a paired t test was used to determine the difference between the volume measured by TRUS and real specimen volume. A paired sample test was used for correlation of these two volume measurements.
RESULTS
Real specimen volume was 16.5-80.6 (average, 31.7±16.1) cc. Prostate volume measured by TRUS using height determined from transaxial scans was 22.0-78.3 (average 29.8±14.8) cc, and using height determined midsagitally was 21.4-72.4 (average 32.7±13.6) cc. Prostate volume measured either transaxially or midsagittally correlated closely with real specimen volume. When height was measured in one of these planes, a paired t test revealed no significant difference between prostate volume according to TRUS and real specimen volume (p = .411 and p = .740, respectively), nor were there significant differences between the findings of transaxial and midsagittal scanning (p = .570). A paired sample test, however, showed that TRUS prostate volumes determined transaxially showed a higher correlation coefficient (0.833) and lower standard deviation (9.04) than those determined midsagittally (0.714 and 11.48, respectively) (Table 1) (Fig. 2).
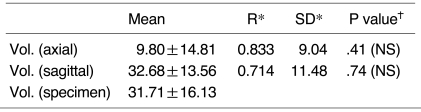
Table 1.
Correlation between Prostate Volume Measured by TRUS and Real Prostate Volume Measured after Radical Prostatectomy
Note.-*Paired sample test, †Paired t test, Vol. (axial): prostate volume calculated by TRUS, with height in axial plane, Vol. (sagittal): prostate volume calculated by TRUS, with height in sagittal plane, Vol. (specimen): specimen volume, R: correla-tion coefficient, SD: standard deviation, NS: no significant difference in statistical analysis (p > .05)
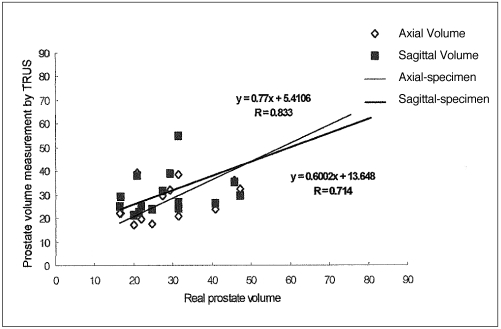
Fig. 2.
Correlation between prostate volume measured by TRUS and real prostate volume measured after radical prostatectomy. When height was determined transaxially rather than midsagitally, prostate volumes measured by TRUS showed higher correlation coefficient (0.833 vs 0.714).
DISCUSSION
Prostate volume was measured by means of the prolate ellipse volume calculation (height × length × width × π/6), a formula used for ellipsoids with three unequal axes. In the early stages of prostate volume measurement by TRUS, maximal height and width measurements were obtained by axial scanning at the mid-gland level which appeared largest. Length was defined as the distance from the proximal external sphincter to the bladder base, as seen on midsagittal scans (11).
To avoid the salami effect, however, height measurement was corrected by sagittal projection in a plane perpendicular to length measurement: salami can be sliced in many different ways; to obtain larger slices, some prefer to cut it obliquely (13). It has been found that height measured transaxially was accurate, and high correlation with real volume was found (11), but as far as we know, no previous study has investigated whether prostate volume measured by TRUS is more accurately calculated using the height measurement obtained by transaxial scanning or by midsaggital. Thus, we determined whether, when measuring prostate volume by TRUS, height is more accurately determined by transaxial or midsagittal scanning, comparing the volume finding thus obtained with real specimen volume.
Using the height measurement obtained in our study by transaxial or by midsaggital scanning, a paired t test demonstrated excellent correlation between TRUS prostate volume and real specimen volume (p = .411 and p = .740, respectively).
Nor were there significant differences between the findings of transaxial and midsagittal scanning (p = .570). A paired sample test, however, showed that TRUS prostate volume determined transaxially showed a higher correlation coefficient (0.833) and lower standard deviation (9.04) than that determined midsagittally (0.714 and 11.48, respectively). We therefore suggest that when determining prostate volume by TRUS, volumes calculated using the height measurement obtained transaxially are more accurate.
Terris et al. (14) have claimed that since the point of juncture between the prostate apex and distal urethra is frequently poorly visualized, prolate ellipse volume calculation may be technically difficult. Likewise, definition between the base of the prostate and the seminal vesicle and bladder neck is often unclear. Accurate height, they believe, is more difficult to determine by midsagittal scanning than by transaxial. Using experimental models, Kim et al. (15) investigated the accuracy of prostate volume calculated by TRUS using height measurements determined transaxially and midsagitally. They concluded that the transaxial mode was more accurate.
Our results are supported by the two studies above. Because we compared the prostate volume obtained by TRUS with real specimen volume, we believe that our study was more physiologic than that of kim et al. (15). In addition, prostate weight or volume of water displaced may provide a more precise measure of prostate size; manipulation of the pathologic specimen (removal of seminal vesicles; dissection of periprostatic fat, connective tissue, and residual bladder neck tissue) prior to sectioning may, however influence the accuracy of the findings. Because we calculated specimen volume using the formula for prolate ellipsoids with three unequal axes (as described for TRUS prostate volume), our result may be more accurate.
During prostate volume measurement by TRUS and processing of the prostate specimen, our study suffered from several limitations. First, since ultrasound is a dynamic modality, operator-dependent factors may contribute to the differences observed between TRUS-derived prostate volume estimates and the volume of the corresponding specimen. Second, after surgical removal of the prostate, varying amounts of residual tissue are left behind, depending on the surgeon and the surgical method; a comparison of the volume of surgically removed tissue with ultrasonically estimated volume may, therefore, be inaccurate. Third, prostate tissue looses between 15 and 42% of its weight after tissue cauterization and due to the effect of irrigating solutions (16, 17).
Henneberry et al. (8), however, who estimated prostate volume pre-and post-operatively in 29 patients (18 of whom had undergone transurethral resection, and 11 open prostectomy), found good correlation in the 11 open prostatectomy cases, but that almost all of the 18 resected specimens weighed less than estimated preoperatively (8). In our study, prostatectomy was performed by open surgery, and we therefore expected less prostate tissue shrinkage.
The value of our study is that we measured prostate volume by TRUS using the height determined by transaxial and midsagittal scanning, and then comparing our finding with a real prostatic specimen. Thus, we investigated which method was most accurate and therefore most useful for clinical evaluation and determination.
In conclusion, prostate volume measured by TRUS closely correlates with real prostate volume. Furthermore, we suggest that when measuring prostate volume in this way, height is more accurately determined by transaxial than by midsagittal scanning.
References
- 1.Jensen KME, Bruskewitz RC, Iversen P, Madsen PO. Significance of prostatic weight in prostatism. Urologia Internationalis. 1983;33:173–178. doi: 10.1159/000280884. [DOI] [PubMed] [Google Scholar]
- 2.Meyhoff HH, Hald T. Are doctors able to assess prostatic size? Scand J Urol Nephrol. 1978;12:219–221. doi: 10.3109/00365597809179720. [DOI] [PubMed] [Google Scholar]
- 3.Meyhoff HH, Ingemann L, Nordling J, Hald T. Accuracy in preoperative estimation of prostatic size. Scand J Urol Nephrol. 1981;15:45–51. doi: 10.3109/00365598109181212. [DOI] [PubMed] [Google Scholar]
- 4.Wadanabe H, Igari D, Tanahashi Y, Harada K, Saitoh M. Measurements of size and weight of prostate by means of transrectal ultrasonotomography. Tohoku J Exp Med. 1974;114:277–285. doi: 10.1620/tjem.114.277. [DOI] [PubMed] [Google Scholar]
- 5.Abu-Yousef MM, Narayana AS. Transabdominal ultrasound in the evaluation of prostate size. JCU. 1982;10:275–278. doi: 10.1002/jcu.1870100606. [DOI] [PubMed] [Google Scholar]
- 6.Walz PH, Wen Deroth U, Jacobi GH. Suprapubic transvesical sonography of the prostate: determination of prostate size. Eur Urol. 1983;9:148–152. doi: 10.1159/000474070. [DOI] [PubMed] [Google Scholar]
- 7.Smith HJ, Haveland H. Preoperative and postoperative volumetry of the prostate by transabdominal ultrasonography. Br J Urol. 1982;54:531–535. doi: 10.1111/j.1464-410x.1982.tb13583.x. [DOI] [PubMed] [Google Scholar]
- 8.Henneberry M, Carter MF, Neiman HI. Estimation of prostatic size by suprapubic ultrasonography. J Urol. 1979;12:615–616. doi: 10.1016/s0022-5347(17)56904-9. [DOI] [PubMed] [Google Scholar]
- 9.Bartsch G, Egender G, Huebscher H, Rohr H. Sonometrics of the prostate. J Urol. 1982;127:1119–1121. doi: 10.1016/s0022-5347(17)54259-7. [DOI] [PubMed] [Google Scholar]
- 10.Hastak SM, Gammelgaard J, Holm HH. Trasrectal ultrasonic volume determination of the prostate-preoperative and postoperative study. J Urol. 1982;127:1115–1118. doi: 10.1016/s0022-5347(17)54258-5. [DOI] [PubMed] [Google Scholar]
- 11.Litttrup PJ, Williams CR, Egglin TK, Kane RA. Determination of prostate volume with transrectal US for cancer screening. II. Accuracy of in vitro and in vivo techniques. Radiology. 1991;179:49–53. doi: 10.1148/radiology.179.1.2006303. [DOI] [PubMed] [Google Scholar]
- 12.Matthews GJ, Motta J, Fracehia JA. The accuracy of transrectal ultrasound prostate volume estimation: clinical correlations. J Clin Ultrasound. 1996;24:501–505. doi: 10.1002/(SICI)1097-0096(199611/12)24:9<501::AID-JCU2>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 13.Dahnert WF. Determination of prostate volume with transrectal US for cancer screening. Radiology. 1992;183:625–627. doi: 10.1148/radiology.183.3.1584907. [DOI] [PubMed] [Google Scholar]
- 14.Terris MK, Stamey TA. Determination of prostate volume by transrectal ultrasound. J Urol. 1991;145:984–987. doi: 10.1016/s0022-5347(17)38508-7. [DOI] [PubMed] [Google Scholar]
- 15.Kim SH, Kim SH, Cho JY, et al. Prostate volume measurement by TRUS: Comparison of reproducibility and accuracy between transaxial and midsagittal scanning by experimental models. J Kor Ultrasound Soc. 1997:93. (abstract book, in Korean) [Google Scholar]
- 16.Einarsson OJ, Lyrdal F, Neidhardt FO. The "shrinkage" of the prostate during transurethral resection. Br J Urol. 1983;55:38–41. doi: 10.1111/j.1464-410x.1983.tb07076.x. [DOI] [PubMed] [Google Scholar]
- 17.Rasmussen F. Weight loss of prostatic tissue during electoresection. Scand J Urol Nephrol. 1975;9:214–215. doi: 10.3109/00365597509134214. [DOI] [PubMed] [Google Scholar]