Abstract
Although surgical resection remains the best option as potentially curative therapy for hepatocellular carcinoma, radiofrequency thermal ablation has begun to receive much attention as an effective minimally invasive technique for the local control of unresectable malignant hepatic tumors. Most recent radiofrequency devices equipped with a powerful generator and larger needle electrode permit larger thermal lesions, up to 5 cm in diameter, with a single ablation. In this article, the author reviews the technical developments and early clinical results obtained with radiofrequency ablation techniques.
Keywords: Liver neoplasms, CT; Liver neoplasms, US; Radiofrequency (RF) ablation
Hepatocellular carcinoma (HCC) is one of the most common malignant neoplasms occurring worldwide (1), and in patients with this condition, surgical excision has evolved as a treatment option. Surgical resection currently provides the best chance of long-term tumor-free survival, but the survival rates following liver resection are low and only a minority of patients are eligible for the surgical procedure (2-4). Liver dysfunction in patients with hepatic cirrhosis makes surgical resection risky, and several minimally invasive techniques for the local control of HCC have therefore been developed. These fall into one of two categories: the direct intratumoral injection of compounds such as absolute ethanol (5) and hot saline (6), and thermal ablation techniques such as interstitial laser photocoagulation (7), microwave ablation (8), and radiofrequency (RF) ablation (9). Among these, the clinical efficacy of percutaneous ethanol injection (PEI) has been established and the procedure is considered an acceptable alternative to surgery for the treatment of HCC (5). Most of the remaining techniques are at the experimental stage, and the experience obtained to date is thus preliminary.
RF thermal ablation is a local ablation technique designed to destroy the tumor by heating. Numerous experimental and clinical studies have concluded that in patients with unresectable liver tumors, the technique is safe and effective (10-20). The concept of using heat to treat tumors is very old, and was used as far back as Greek and Roman times (21), when cautery was used to treat superficial tumors. Heat therapy is based on the observation by Coley (22) that tumor cells are more sensitive to heat than are normal cells. The use of RF to induce controlled thermal injury in living tissue is a well-established technique used by neurosurgeons since the mid-1960s (23), and in the early 1980s LeVeen et al. found that external radiofrequency was effective in treating tumors located deep in the body (24). McGahan et al. (9) pioneered the application of RF ablation to the treatment of malignant hepatic tumors. With the development of high-resolution cross-sectional imaging modalities and interventional techniques, the percutaneous placement of a heating device powered with energy from a microwave (25) or radiofrequency generator has become possible. Unfortunately, the lesions made with initial needle electrodes were no more than 1.6 cm in diameter, but many investigators have subsequently attempted to solve the size limitation using approaches which include the use of multiprobe arrays (10) and saline injection prior to RF ablation (11). These permitted certain advances in the treatment of larger lesions, but were not a satisfactory response to the problem of large hepatic tumors. With the introduction of monopolar needle electrodes with expandable multiple spring wires and a straight tip needle electrode internally cooled with chilled saline (12-14), the induction of consistent and predictable large thermal lesions has become possible. Most recent expandable needle electrodes permit larger thermal lesions, up to 5 cm in diameter, with a single ablation. This review article describes the current status of RF thermal ablation in HCC, with an emphasis on techniques.
Tissue Response to Heat, and the Principle of RF Ablation
Thermal injury to living tissue is known to begin at 42℃. Lethal exposure times at this temperature range from 3 to 50 hours, depending on the tissue involved (26). At temperatures over 43℃, lethal exposure times decrease exponentially; at 46℃, 8 minutes' exposure is enough to cause cell death. At temperatures over 60℃, denaturing of tissue collagen begins and cell death is inevitable (27, 28), and for treatment in cases where injury to normal tissue is not a concern, temperatures of this magnitude are therefore desirable. In clinical practice the tissues around the tip of a needle electrode are heated to 100℃, the temperature required to induce the desirable degree of injury. It is known, however, that rapid heating to too high a temperature (over 100℃) dramatically increases tissue impedance, and the deposition of RF energy, heat diffusion, and further coagulation necrosis are limited (29).
Using either ultrasound or CT guidance, an RF needle electrode is percutaneously introduced directly into a tumor. When the electrode is connected to a generator producing alternating electric current, RF is emitted from its tip, and current within the RF range (460 kHz) passes into surrounding tissue. The current agitates ions of tumor tissue around the needle electrode, and the frictional heat produced by ionic agitation induces cellular death via coagulation necrosis. By changing the intensity and duration of the alternating current, and the size of the electrode, the size of the thermal lesion can be controlled.
Indications and Contraindications
We currently limit the use of RF ablation to patients who are not considered for surgery, or who decline this option. As yet, there is no consensus as to indication, but investigators generally recommend that HCCs smaller than 5 cm in diameter and fewer than four in number are ideal for RF ablation. We are able to treat lesions larger than this by making multiple overlapping ablations with recently developed needle electrodes and powerful generators, but it is known that the larger the tumor, the greater the incidence of incomplete treatment.
Because RF ablation can cause bleeding, uncorrectable coagulopathy due to severe liver dysfunction is an absolute contraindication. The prothrombin time ratio must be greater than 50% and the platelet count greater than 70,000/mm3. Patients with large amounts of ascites, obstructive jaudice, evidence of extrahepatic tumors, or extensive portal venous thrombosis are not suitable candidates for the procedure. A life expectancy of less than 3 months is also a contraindication.
Equipment
At the moment three RF devices, all of which consist of RF generators, needle electrodes and dispersive ground pads, are commercially available. The basic principles of each are similar, but the operational techniques are different. Generator power varies between 50 and 200 watts; some are equipped with functions that display output, tissue impedance, and temperatures in the tissue around the tip of a needle electrode. In each device, the design of these electrodes is different (Fig. 1). The first device to be introduced in Korea, in April 1999, was the RITA '500' model (RITA Medical Systems, Mountain View, Cal., U.S.A.). This consists of a 50-watt electric generator and a 15-gauge needle electrode, insulated except for 0.6-1 cm of its tip. Its hub is a plunger that advances 4 or 7 prongs from the tip, and when fully deployed, these and the needle electrode resemble an open umbrella 3 cm in diameter. All the prongs and uninsulated tip of the needle are active electrodes, and each curved prong contains a thermocouple at its tip that registers the temperature of surrounding tissue. With the use of recently developed software, the temperature around a needle electrode, power, and impedance can be continuously monitored. The more recent 1500 model, manufactured by the same company, is equipped with a more powerful generator (150 watts) and a larger needle electrode, 5 cm in diameter, which can induce thermal lesions of up to this size with a single ablation.
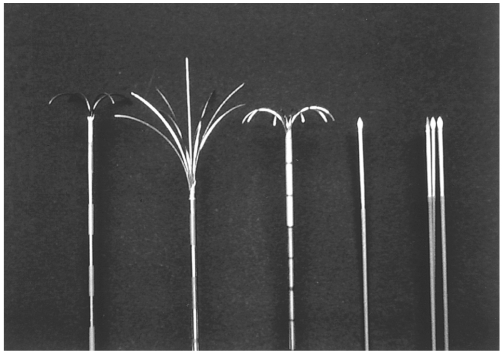
Fig. 1.
Radiofrequency needle electrodes of varying design manufactured by three different companies.
The first three needle electrodes, 15-gauge in external diameter and insulated except for 0.6-1 cm of their tip, have 4, 9, or 10 retractable hook-like prongs which serve as active electrodes during RF ablation. The fourth and fifth have a single 17-gauge straight-tip and triple-cluster electrodes, internally cooled with chilled saline solution during ablation. The needles have active exposed tips 2-4 cm in length
The second device ('RF 2000' system) manufactured by RadioTherapeutics Corporation (Mountain View, Cal.,) incorporates a 100-watt generator, a LeVeen 15-gauge, monopolar array needle electrode, and needle electrodes 2, 3, and 3.5 cm in diameter, the largest of which is able to induce lesions with a diameter of up to 4 cm. The 15-gauge electrode consists of a 12- to 15-cm-long insulated cannula that advances ten individual hook-like arms which are deployed after the needle has been introduced into the tumor.
The third device, manufactured by Radionics Corporation (Burlington, Mass., U.S.A.), includes a needle electrode whose tip is internally cooled with chilled saline, a process thought to increase the size of the thermal lesion. The device is equipped with a 200-watt generator and uses either a single 17-gauge straight electrode or clustered electrodes designed in a triangular shape. With the device, thermal lesions of up to 5 cm in diameter can be induced.
Procedure and Technique
RF ablation can be performed percutaneously, laparoscopically, or during laparotomy, and involves conscious sedation or general anesthesia. For the former, we prefer the intramuscular injection of 50 mg pethidine hydrochloride (Pethidine; Samsung Pharmaceutical, Seoul, Korea) 10-20 minutes before the procedure. Whenever patients report intolerable pain during ablation, an additional 50 mg of the same drug is administered intravenously, with continuous monitoring of the cardiovascular and respiratory systems.
Although lesions can be reliably localized using CT, this part of the procedure has depended mostly on sonography. For grounding, one or two large dispersive pads are attached to the patient's thigh or back, and after skin cleansing using a sterile technique, local anesthetic (Lidocaine; Kwang Myung Pharmaceutical, Seoul, Korea) is injected along the expected needle pathway and a small skin nick is made. The electrode is passed through the nick and advanced into the desired portion of the tumor, using real-time sonographic guidance. Once the needle tip is appropriately positioned in the tumor, the electrode prongs are deployed and ablation is begun. If a RITA device is used, initial ablation involves partial deployment of the curved electrodes, but once the temperature at the tip of these reaches the desired level (usually over 95℃), they are fully deployed. The temperature is then maintained at 95-100℃ for ten minutes until the entire tumor or the desired portion is ablated. After each ablation, the prongs are retracted and the needle is repositioned. At this point, the needle tract is cauterized and the needle withdrawn from the liver. With an RTC device, the power used for initial ablation after deployment of the multiple arrays is 50 watts. At 1, 2, 3, and 4 minutes, 10-watt increments are applied, to a maximum of 90 watts, until the "roll-off" phenomena is observed (i.e., power output falls precipitously as tissue impedance increases markedly). After a 30-second pause, ablation is restarted, at 75% of the maximum power achieved, until "roll-off" again occurs. Each tumor or area of a large tumor is ablated by the application of RF power during these two phases, and at completion the needle is removed with the multiple arrays retracted. With a Radionics device either a single electrode with 2 or 3 cm of exposed metallic tip or a triple- cluster electrode, depending on the size and location of the tumor, can be employed. After the needle electrode is introduced into the tumor, RF is usually applied for 12 minutes. To maintain a temperature of 20°-25℃ in the tissue around the needle tip, a peristaltic pump is used to infuse 0℃ normal saline solution into the lumen of the electrodes. During ablation, generator output, tissue impedance and temperature around the needle tip are continuously monitored.
For RF ablation to be successful and complete, all malignant tissue must be ablated. The ideal goal is to ablate a peripheral margin of 0.5-1 cm of normal hepatic tissue surrounding the tumor, as well as the entire tumor itself: without adequate safety margins, untreated viable tumor may remain, leading to treatment failure and local recurrence. In general, a single ablation, or two, may be adequate for tumors less than 3 cm in diameter when a needle electrode at least 3 cm in diameter is used. For larger tumors, however, multiple overlapping ablations should be performed, according to tumor size. With a needle electrode 3 cm in diameter, a single ablation is applied for tumors < 2 cm in diameter, at least two ablations for those which are 2~3 cm, and multiple overlapping ablations for those > 3 cm. For tumors located in the mid-zone of the liver rather than its periphery or central zone, this treatment strategy may be adopted without difficulty (Fig. 2).
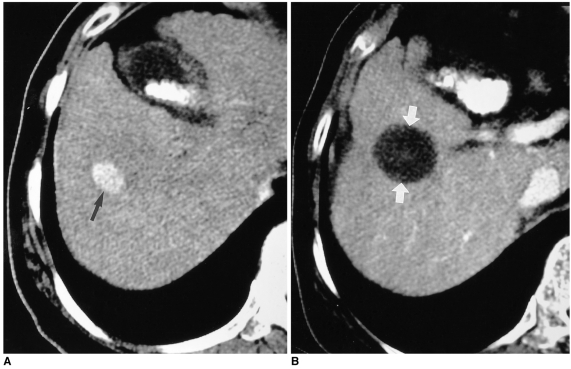
Fig. 2.
HCC located in the mid-zone of the liver surrounded by normal hepatic tissue in a 62-year-old man.
A. Transverse helical CT scan obtained during the hepatic arterial phase prior to RF ablation shows a 2.5-cm HCC (arrow), with homogenous contrast enhancement in liver segment 5.
B. Transverse helical CT scan obtained one month after RF ablation depicts a round ablated area of low attenuation (arrows), representing complete necrosis of the tumor. Note that the ablated area covers the entire tumor and the cuff of surrounding normal hepatic tissue.
In addition to size, tumor location is one of the important factors influencing the likely therapeutic outcome. If the tumor lies in the subcapsular area, no safety margin along the capsule is possible. In subcapsular tumors, a safety margin of normal hepatic tissue is difficult to obtain, but if the liver capsule overlying the tumor appears to be involved by the tumor, the capsule should be ablated. Subcapsular tumors can be effectively treated using either an expandable needle electrode with multiple array or a straight cooled-tip electrode. If a tumor is small and round, the use of an expandable needle electrode is preferred because the lesions it induces tend to be more spherical in shape than those induced by one with a straight tip. For ablating fusiform tumors, a straight-tip needle electrode is better because it frequently makes elliptical lesions. Tumors located between the anterior and posterior liver capsules (e.g. in the inferior angle of the right lobe or the lateral segment of the left) are often difficult to ablate completely, especially when they abut on both capsules, and in this particular situation, the choice of needle electrode is important. When an expandable electrode is used in narrow spaces, multiple overlapping ablations involving partial deployment of the hook-like electrodes are unavoidable even if the tumors are small: the full deployment of hooks can penetrate the liver capsule, and this may cause bleeding or unnecessary thermal injury to adjacent organs. Because its use involves no risk of penetrating either capsule, and the entire length of active electrode can be employed, the situation requires a straight cooled-tip electrode. Additionally, the number of ablations and thus the procedure time are thereby reduced (Fig. 3). If the ultrasound-guided percutaneous approach is used, subcapsular tumors exhibiting exophytic growth can also be difficult to ablate completely. The best way to achieve effective necrosis of an exophytic tumor is to ablate the deepest portion first, thus blocking the blood supply to the exophytic portion, which is subsequently ablated (Fig. 4).
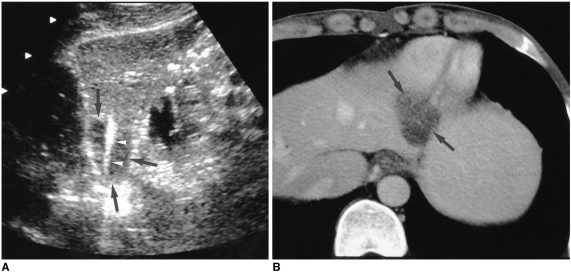
Fig. 3.
HCC in a 45-year-old man.
A. Longitudinal US scan of left hepatic lobe shows a 2.8-cm low echogenic HCC (arrows) which is fusiform in shape. The mass abuts on both liver capsules. Note the 3-cm active tip (arrowheads) of the straight cooled-tip electrode, which conforms to the shape of the mass. A single ablation lasted for 12 minutes.
B. Portal-phase CT scan obtained 30 minutes after RF ablation reveals the presence of an oval low-attenuating lesion (arrows), with absence of contrast enhancement within the ablated area. This indicates complete necrosis.
Fig. 4.
HCC in a 57-year-old man.
A. Hepatic arterial-phase CT scan depicts a 4-cm HCC (arrows) in the subcapsular area of the right hepatic lobe, which shows an outward bulge. Using a 3-cm expandable needle electrode, four ablations were performed. The deep portion of the mass was treated first, and then the exophytic portion.
B. Portal-phase CT scan obtained 13 months after RF ablation shows an ablated lesion (arrows) with no contrast enhancement, indicating complete necrosis.
Another difficult situation arises when tumors are present in the central zone of the liver, near the hepatic hilum. A tumor in this location is almost always surrounded by large vessels, and the resultant tissue cooling may make it difficult to ablate its periphery and the cuff of normal hepatic tissue. In this situation, the extent of coagulation necrosis is less than usual, and follow-up CT reveals the presence of residual perivascular tumor (Fig. 5). On the basis of experimental and clinical studies (30-32), several investigators have found that temporary reduction of vascular flow to the liver during RF ablation by mechanical occlusion of the portal vein and/or arterial vessels, or pharmacologic modulation, increased the extent of coagulation necrosis. When RF ablation is performed percutaneously, the use of a balloon for mechanical occlusion of the portal vein is impractical because it is invasive and time consuming. During intraoperative RF ablation after laparotomy, reduction of vascular inflow by clamping the hepatic artery and portal vein at the level of the porta hepatis (Pringle maneuver) is very helpful in increasing the extent of coagulation necrosis. Pharmacologic modulation of hepatic blood flow has been under investigation and could be the ideal way of creating more extensive coagulation necrosis during percutaneous RF ablation. It is, however, not yet available in clinical practice. We are able to suggest a number of ways in which the use of current RF devices for the ablation of tumors surrounded by large vessels may be efficacious. The space between large vessels is usually small and narrow, and safe ultrasound-guided targeting may thus be difficult. It is important not to penetrate large vessels with a needle electrode, since bleeding or pseudoaneurysm may occur. When RF ablation involves the use of an expandable needle electrode and its hooks within the lumen of the vessel are ineffective, the hooks of the multiple array should not be placed beyond the vascular wall. To induce satisfactory coagulation necrosis in this situation, multiple overlapping ablations with partial deployment of the multiple array are recommended, rather than a single ablation with the needle electrode fully deployed. Even if the tumor is less than 3 cm in diameter, the recommendation applies. To avoid penetration of the vessel wall during deployment of the needle electrode, careful monitoring with real-time ultrasound is essential. If the temperature around any tip of the multiple array fails to rise, this indicates that the tip is inside the blood vessel and should be retracted. For ablation of a tumor surrounded by large vessels, a straight-tip internally cooled needle electrode may have advantages over the expandable needle variety. First, because only the straight part of the active electrode is involved, penetration of the vessel wall is not a matter of concern. Second, the reduced impedance of the tissues nearest the needle electrode, induced by internal cooling with chilled saline, enables heat to diffuse more easily. This, in turn, allows greater RF energy deposition and can lead to more extensive coagulation necrosis than is possible when an expandable needle electrode is used. For ablation of a tumor surrounded by large vessels, it is also useful to increase the duration of RF application, regardless of the type of needle electrode employed; one more ablation with the needle tip placed in the same position may help decrease the amount of residual perivascular tumor. This possible outcome is, however, based on our own experience and is somewhat speculative; firmer conclusions should be based on the findings of further studies.
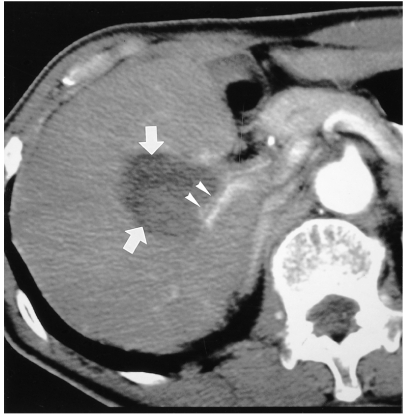
Fig. 5.
Hepatic arterial-phase CT scan obtained 1 month after RF ablation of a 4-cm HCC surrounded by large branches of the hepatic artery and portal vein shows a low attenuating ablated lesion (arrows) near the hepatic hilum. Although the tumor has become mostly necrotic, thin enhancing viable tumor (arrowheads) remains along the posterior branch of the right hepatic artery.
The ablation procedure almost always creates numerous microbubbles in heated tissue, and these increase the echogenicity of the ablated lesion (Fig. 6), a condition which is known to persist for between 15 minutes and 6 hours (33, 34). Hyperechogenicity may be helpful for monitoring the approximate size of an ablated lesion, but makes further placement of the needle electrode difficult. For large tumors, the accurate mapping of multiple overlapping ablations is therefore imperative. One good way of treating a large tumor is to deal with the deepest portion first; in this way increased echogenicity does not obscure its untreated portions.
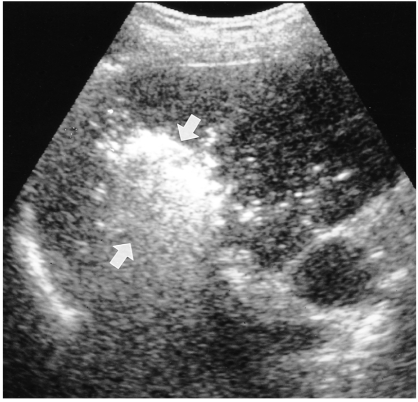
Fig. 6.
Oblique US scan of the liver obtained during RF ablation shows an echogenic ablated lesion (arrows), the result of numerous microbubbles produced by thermal ablation.
Evaluation of Therapeutic Effect
No data concerning the accuracy of CT in depicting residual tumors after RF ablation have been published, and as a standard of reference, the dynamic helical mode suffers certain limitations. Nonetheless, CT has been widely used in the evaluation of therapeutic response after RF ablation. Complete tumor necrosis (successful treatment) is considered to have occurred when follow-up CT reveals no foci of enhancement within the ablated lesion or at its periphery (Figs. 2, 4). Any focal enhancement within the tumor or increase in size of the ablated tumor should be considered indicative of residual or recurrent lesion (Fig. 7). We treat residual or recurrent tumor with additional RF ablation, using three-phase helical CT to evaluate therapeutic outcome; because reactive hyperemia in tissue surrounding the ablated lesion makes accurate assessment difficult, such evaluation does not immediately follow treatment, however (Fig. 8). Whether ablation was successful is usually determined on the basis of CT findings obtained at least one month after the procedure. In our experience, reactive hyperemia has usually resolved by this time. To determine the possible presence of residual or recurrent tumor, follow-up CT is scheduled every three months thereafter.
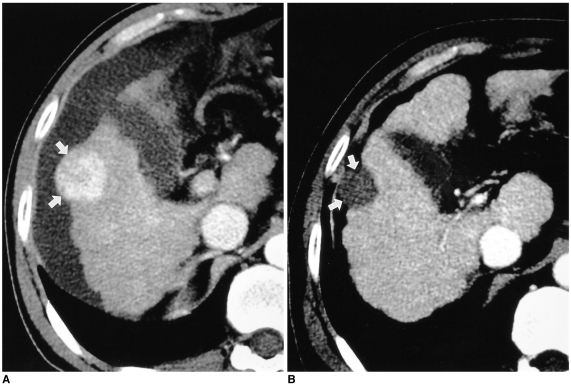
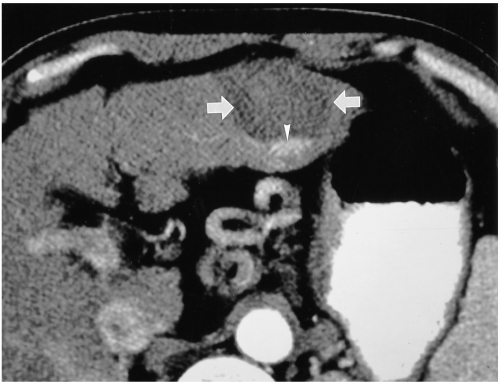
Fig. 7.
Hepatic arterial-phase CT scan obtained one month after RF ablation of a 4-cm HCC in the left hepatic lobe reveals the presence of a round low-attenuating lesion (arrows). Note the focal contrast enhancement (arrowhead) in the posterior aspect of the ablated lesion, indicative of viable untreated tumor. Additional RF ablation was subsequently performed.
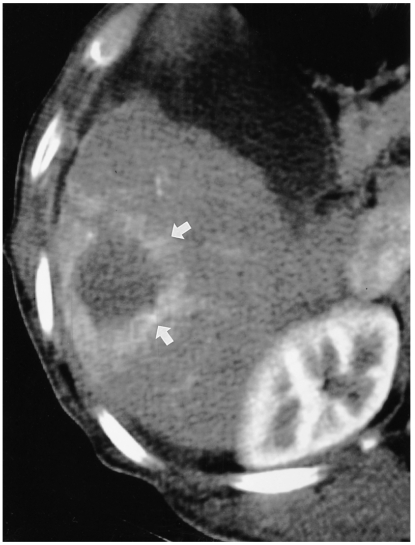
Fig. 8.
Reactive hyperemia revealed by immediate post-treatment CT.
Hepatic arterial-phase CT scan obtained 30 minutes after RF ablation shows uniform rim-like contrast enhancement (arrows) around the ablated lesion, a phenomenon frequently occurring immediately after RF ablation and usually resolving prior to follow-up CT at one month.
Dynamic MRI with Gd-DTPA enhancement is also a good method for evaluating therapeutic response. Areas of the tumor in which treatment was successful do not demonstrate the enhancement seen at contrast-enhanced CT.
Power Doppler ultrasonography (PDUS) using a microbubble contrast agent has recently been reported to be a promising noninvasive technique for assessing the therapeutic response to RF ablation in HCC (34). Nonenhanced PDUS was of little help in depicting residual intratumoral flow signals, though contrast-enhanced PDUS was very sensitive in the detection of residual tumor vascularity within an ablated lesion (Fig. 9).
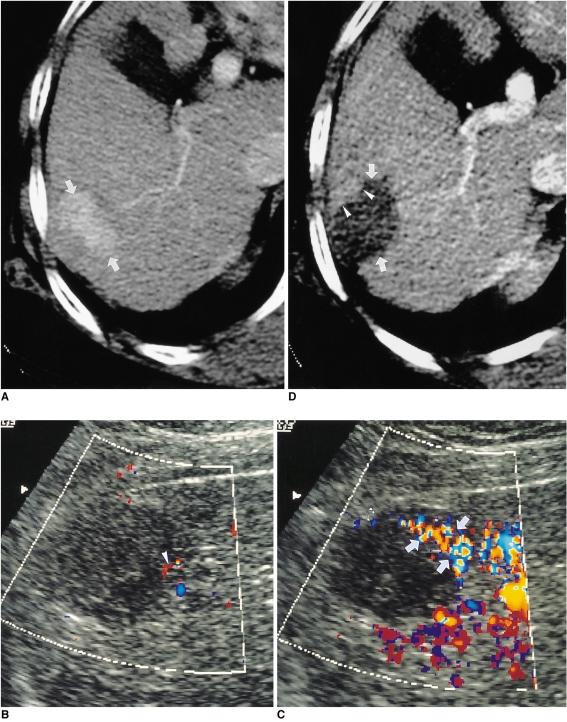
Fig. 9.
HCC in a 67-year-old woman.
A. Hepatic arterial-phase CT scan shows an oval enhancing HCC (arrows), 4 cm in its greatest diameter, at the periphery of the right hepatic lobe.
B. Unenhanced oblique power Doppler US scan obtained 18 hours after RF ablation shows a subtle flow signal (arrowhead) in the antero-superior aspect of the ablated lesion.
C. Contrast-enhanced oblique power Doppler US scan obtained immediately after B, above, shows peripheral flow signals (arrows) within the anterior aspect of the RF-ablated lesion, representing residual tumor. The residual flow signals seen on this contrast-enhanced scan are better appreciated than on nonenhanced power Doppler US scan.
D. Hepatic arterial-phase CT scan obtained 2 hours after RF ablation shows focal nodular contrast enhancement (arrowheads), indicative of residual tumor, in the anterior aspect of the ablated lesion (arrows). The enhanced area corresponds to that in which residual flow signals are present in the image described in C, above.
Results
Several clinical series using different methods of RF application for the treatment of HCC have been reported (12, 13, 15-17, 20). Rossi et al. detailed their seven-year experience with RF ablation in 50 patients with HCC or hepatic metastases (15), reporting very promising survival rates (for HCC patients) of 94%, 86%, 68%, and 40% at 1, 2, 3 and 5 years, respectively. Reported complete necrosis rates after RF ablation have varied according to the size and morphology of the hepatic lesions. Livraghi et al. (16) reported a complete necrosis rate of 90% in 42 patients with 52 small HCCs (< 3 cm in diameter). This rate decreased, however, to 71% for medium HCCs (3.1-5.0 cm) and to 25% for large ones (> 5.0 cm) (17). In an early experience with 51 HCCs (1.0-4.0 cm in diameter) at our institution, the complete necrosis rate was 94% (20). During a recent one-year period, we used RF ablation alone for the treatment of 108 patients with 125 nodular HCCs. Fifty-seven of these 108, with 65 HCCs, underwent follow-up helical CT not less than six months after the procedure. Forty-five tumors were small (0.7-3.0 cm) and 20 were medium (3.1-5.0 cm). Six-month follow-up CT showed complete necrosis of ablated tumor in 43 (96%) of the 45 small lesions and in 18 (90%) of the 20 that were medium-sized. After RF ablation, we found no major but four minor complications (one small pneumothorax and three cases of minor intraperitoneal bleeding) which disappeared spontaneously with no specific treatment (35). Other investigators have also reported low complication rates (12-17).
Summary and Conclusion
On the basis of several clinical studies including ours, we believe that RF ablation is a safe and highly effective technique for the local treatment of HCC, especially for small tumors. RF ablation has several advantages over other existing therapies: it is minimally invasive, and for the treatment of residual or recurrent tumors can be repeated. Compared with PEI, RF ablation leads to a higher complete necrosis rate and requires fewer treatment sessions (16).
The RF ablation of HCC may have its limitations. The procedure is operator dependent, and for successful ablation, accurate placement of the needle electrode is imperative. In order to obtain good results, medical practicioners should therefore be familiar with sonographically-guided interventional techniques. The other limitation is that abundant portal venous flow in normal liver tissue surrounding the tumor may act as a heat sump, making complete ablation of such tissue difficult. To decrease the effect of portal venous flow, several experimental and clinical studies are in progress.
Although long-term follow-up evaluation of clinical outcome is needed, RF ablation is safe and effective, and is thus a highly promising technique for the local destruction of HCC. Further improvements in the devices and techniques employed may further increase its efficacy and safety.
Footnotes
This paper was supported in part by clinical research fund (G1-00-07) of Gastrointestinal Center, Samsung Medical Center.
References
- 1.Colombo M. Hepatocellular carcinoma. J Hepatol. 1992;15:225–236. doi: 10.1016/0168-8278(92)90041-m. [DOI] [PubMed] [Google Scholar]
- 2.Tsuzuki T, Sugioka A, Ueda M. Hepatic resection for hepatocellular carcinoma. Surgery. 1990;107:511–520. [PubMed] [Google Scholar]
- 3.Liver Cancer Study Group of Japan. Primary liver cancer in Japan: clinicopathologic features and results of surgical treatment. Ann Surg. 1990;211:277–284. [PMC free article] [PubMed] [Google Scholar]
- 4.Farmer DG, Rosove MH, Shaked A, Busuttil RW. Current treatment modalities for hepatocellular carcinoma. Ann Surg. 1994;219:236–247. doi: 10.1097/00000658-199403000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Livraghi T, Bolondi L, Lazzaroni S, et al. Percutaneous ethanol injection in the treatment of hepatocellular carcinoma in cirrhosis: a study in 207 patients. Cancer. 1992;69:925–929. doi: 10.1002/1097-0142(19920215)69:4<925::aid-cncr2820690415>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 6.Honda N, Guo Q, Uchida H, Ohishi H, Hiasa Y. Percutaneous hot saline injection therapy for hepatic tumors: an alternative to percutaneous ethanol injection therapy. Radiology. 1994;190:53–57. doi: 10.1148/radiology.190.1.8259428. [DOI] [PubMed] [Google Scholar]
- 7.Amin Z, Donald JJ, Masters A, et al. Hepatic metastases: interstitial laser photocoagulation with real-time sonography monitoring and dynamic CT evaluation of treatment. Radiology. 1993;187:339–347. doi: 10.1148/radiology.187.2.8475270. [DOI] [PubMed] [Google Scholar]
- 8.Murakami R, Yoshimatsu S, Yamashita Y, Matsukawa T, Takahashi M, Sagara K. Treatment of hepatocellular carcinoma: value of percutaneous microwave coagulation. AJR. 1995;164:1159–1164. doi: 10.2214/ajr.164.5.7717224. [DOI] [PubMed] [Google Scholar]
- 9.McGahan JP, Browning PD, Brock JM, Tesluk H. Hepatic ablation using radiofrequency electrocautery. Invest Radiol. 1990;25:264–270. doi: 10.1097/00004424-199003000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg SN, Gazelle GS, Dawson SI, et al. Tissue ablation with radiofrequency using multiprobe arrays. Acad Radiol. 1995;2:670–674. [PubMed] [Google Scholar]
- 11.Livraghi T, Goldberg SN, Monti F, et al. Saline-enhanced radiofrequency tissue ablation in the treatment of liver metastasis. Radiology. 1997;202:205–210. doi: 10.1148/radiology.202.1.8988212. [DOI] [PubMed] [Google Scholar]
- 12.Rossi S, Buscarini E, Garbagnati F, et al. Percutaneous treatment of small hepatic tumors by an expandable RF needle electrode. AJR. 1998;170:1015–1022. doi: 10.2214/ajr.170.4.9530052. [DOI] [PubMed] [Google Scholar]
- 13.Curley SA, Izzo F, Delrio P, et al. Radiofrequency ablation of unresectable primary and metastatic hepatic malignancies: results in 123 patients. Ann Surg. 1999;230:1–8. doi: 10.1097/00000658-199907000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Solbiati L, Goldberg SN, Ierace T, et al. Hepatic metastases: percutaneous radio-frequency ablation with cooled-tip electrodes. Radiology. 1997;205:367–373. doi: 10.1148/radiology.205.2.9356616. [DOI] [PubMed] [Google Scholar]
- 15.Rossi S, Di Stasi M, Buscarini E, et al. Percutaneous RF interstitial thermal ablation in the treatment of hepatic cancer. AJR. 1996;167:759–768. doi: 10.2214/ajr.167.3.8751696. [DOI] [PubMed] [Google Scholar]
- 16.Livraghi T, Goldberg SN, Lazzaroni S, Meloni F, Solbiati L, Gazelle GS. Small hepatocellular carcinoma: treatment with radio-frequency ablation versus ethanol injection. Radiology. 1999;210:655–661. doi: 10.1148/radiology.210.3.r99fe40655. [DOI] [PubMed] [Google Scholar]
- 17.Livraghi T, Goldberg SN, Lazzaroni S, et al. Hepatocellular carcinoma: radio-frequency ablation of medium and large lesions. Radiology. 2000;214:761–768. doi: 10.1148/radiology.214.3.r00mr02761. [DOI] [PubMed] [Google Scholar]
- 18.Goldberg SN, Solbiati L, Hahn PF. Large-volume tissue ablation with radiofrequency by using a clustered, internally cooled electrode: laboratory and clinical experience in liver metastases. Radiology. 1998;209:371–379. doi: 10.1148/radiology.209.2.9807561. [DOI] [PubMed] [Google Scholar]
- 19.Choi D, Lim HK, Park JM, et al. An experimental study on hepatic ablation using an expandable radiofrequency needle electrode. J of Korean Radiol Soc. 1999;41:1127–1132. [Google Scholar]
- 20.Choi D, Lim HK, Kim SH, et al. Radiofrequency ablation of small heaptocellular carcinoma: early experience of efficacy and safety. J of Korean Radiol Soc. 2000;42:743–749. [Google Scholar]
- 21.Hornback NB. Historical aspects of hyperthermia in cancer therapy. Radiol Clin North Am. 1989;27:481–488. [PubMed] [Google Scholar]
- 22.Coley WB. The treatment of malignant tumors by repeated innoculations of erysipelas, with a report of ten original cases. Am J Med Sci. 1893;105:487–492. [PubMed] [Google Scholar]
- 23.Rosomoff Hl, Carroll F, Brown J, Sheptak T. Percutaneous radiofrequency cervical cordotomy technique. J Neurosurgery. 1965;23:639–644. doi: 10.3171/jns.1965.23.6.0639. [DOI] [PubMed] [Google Scholar]
- 24.LeVenn HH, Ahmed N, Piccone VA, Shugaar S, Falk G. Radiofrequency therapy: clinical experience. Ann N Y Acad Sci. 1980;335:362–371. doi: 10.1111/j.1749-6632.1980.tb50761.x. [DOI] [PubMed] [Google Scholar]
- 25.Seki T, Wakabayashi M, Nakagawa T, et al. Ultrasonically guided percutaneous microwave coagulation therapy for small hepatocellular carcinoma. Cancer. 1994;74:817–825. doi: 10.1002/1097-0142(19940801)74:3<817::aid-cncr2820740306>3.0.co;2-8. [DOI] [PubMed] [Google Scholar]
- 26.Dickson JA, Calderwood SK. Temperature range and selective sensitivity of tumors to hyperthermia: a critical review. Ann N Y Acad Sci. 1980;335:180–205. doi: 10.1111/j.1749-6632.1980.tb50749.x. [DOI] [PubMed] [Google Scholar]
- 27.Hill RP, Hunt JW. Hyperthermia. In: Tannock IF, Hill RF, editors. The Basic Science of Oncology. New York: Pergamon Press; 1987. pp. 337–357. [Google Scholar]
- 28.Allain JC, LeLouis M, Bailey AJ, Delaunay A. Isometric tension developed during heating of collagen tissues: relationship with collagen cross-linking. Biochimica et Biophysica Acta. 1978;533:147–155. doi: 10.1016/0005-2795(78)90558-5. [DOI] [PubMed] [Google Scholar]
- 29.Haines DE, Verow AF. Observations on the electrode-tissue interface temperature and effect on electrical impendance during radiofrequency ablation of ventricular myocardium. Circ. 1990;82:1034–1038. doi: 10.1161/01.cir.82.3.1034. [DOI] [PubMed] [Google Scholar]
- 30.Goldberg SN, Hahn PF, Tanabe KK, et al. Percutaneous radiofrequency tissue ablation: does perfusion-mediated tissue cooling limit coagulation necrosis? J Vasc Interv Radiol. 1998;9:101–111. doi: 10.1016/s1051-0443(98)70491-9. [DOI] [PubMed] [Google Scholar]
- 31.Patterson EJ, Scudamore CH, Owen DA, Nagy AG, Buczkowski AK. Radiofrequency ablation of porcine liver in vivo: effects of blood flow and treatement time on lesion size. Annals of Surgery. 1998;227:559–565. doi: 10.1097/00000658-199804000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goldberg SN, Hahn PF, Halpern EF, Fogle RM, Gazelle GS. Radio-frequency tissue ablation: effect of pharmacologic modulation of blood flow on coagulation diameter. Radiology. 1998;209:761–767. doi: 10.1148/radiology.209.3.9844671. [DOI] [PubMed] [Google Scholar]
- 33.Goldberg SN, Gazelle GS, Solbiati L, et al. Ablation of liver tumors using percutaneous RF therapy. AJR. 1998;170:1023–1028. doi: 10.2214/ajr.170.4.9530053. [DOI] [PubMed] [Google Scholar]
- 34.Choi D, Lim HK, Lee WJ, et al. Evaluation of therapeutic response in hepatocellular carcinoma treated with percutaneous radio-frequency ablation: usefulness of power Doppler US with a microbubble contrast agent-preliminary results. Radiology. 2000;217:558–563. doi: 10.1148/radiology.217.2.r00oc07558. [DOI] [PubMed] [Google Scholar]
- 35.Lim HK. Radiofrequency ablation of hepatocellular carcinoma; Proceedings of the 4th Asian Pacific Congress of Cardiovascular and Interventional Radiology; 2000. pp. 120–122. [Google Scholar]