Abstract
Uterine cervical carcinoma is one of the most common malignant tumors occurring in females. After primary treatment, patients are usually followed up with CT or MRI and the findings of these modalities may be the first sign of recurrent disease. Because earlier additional treatment by chemotherapy or radiation therapy may improve the prognosis, the early detection of recurrent cervical carcinoma is clinically important. In this article, we review the CT and MR imaging findings of recurrent uterine cervical carcinoma, and assign them to one of four groups: a) recurrence at the primary site, involving the intrapelvic organs, b) extension to the pelvic side-wall, c) metastases to pelvic and extrapelvic lymph nodes, or d) metastases to distant organs. A further contribution of CT and MR imaging is the detection of hydronephrosis due to ureteral obstruction. The cases in each group are illustrated and discussed, and since an awareness of the spectrum of imaging findings of recurrent cervical carcinoma is likely to lead to its early detection, radiologists should be familiar with the information presented.
Keywords: Uterine neoplasms, diagnosis; Uterine neoplasms, CT; Uterine neoplasms, MR
Despite the decreased incidence of cervical carcinoma associated with widespread screening using Papanicolaou's smear test, uterine cervical carcinoma is still one of the most common gynecologic malignancies. Even though patients now survive longer due to radiation therapy and more effective chemotherapy, it is also one of the most frequent causes of death in women. In spite of these advances in the methods of treatment, approximately 30% of women with invasive cervical carcinoma die as a result of recurrent or persistent disease (1).
Recurrence is defined as local tumor regrowth or the development of distant metastasis discovered six months or more after complete regression of the treated lesion, and uterine cervical carcinoma often recurs within two years of treatment. The incidence of recurrence depends primarily on tumor bulk and the stage of the disease at presentation (1). About one-half of recurrences appear within the pelvis, but distant metastases may develop in the lung and liver, and in bone and lymph nodes (2).
Conventional radiographic evaluations of these patients include chest radiography, excretory urography, barium enema, and occasionally, lymphangiography. However, improvements in cross-sectional imaging modalities such as CT or MR imaging offer distinct advantages over conventional radiographic techniques, and nowadays, the follow-up of treated cervical carcinoma usually involves the use of these modalities. Because additional chemotherapy or radiation therapy can improve the prognosis, the early detection of recurrent cervical carcinoma is important. In the interests of early detection, radiologists should therefore be familiar with the spectrum of imaging findings presented by this condition.
We retrospectively reviewed the CT and MR imaging findings of patients with recurrent cervical carcinoma, classifying them as one of four types according to the site of recurrence: a) recurrence at the primary site, involving the intrapelvic organs, b) recurrent mass at the pelvic side-wall, c) metastases to pelvic and extrapelvic lymph nodes and d) metastases to a distant organ or organs. In this article, we illustrate and discuss the various CT and MR imaging findings for each group.
RECURRENCE AT THE PRIMARY SITE
Recurrence at the primary site may involve the cervix, uterus, vagina, parametria or ovary, and is the most common manifestation of recurrent cervical carcinoma (3-5). The incidence of recurrence at the primary site varies with the stage at presentation, histologic type, adequacy of therapy used and host response. Kim et al. (5) reported a higher incidence of recurrence among patients treated by radiation therapy than by surgery. Invasion of the urinary bladder and rectum, with or without fistula formation, is a severe complication which can be demonstrated by CT or MR imaging.
RECURRENCE AS A CENTRAL PELVIC MASS
The evaluation of CT and MR imaging findings of recurrence at the primary site requires an understanding of the normal anatomy of the pelvis after hysterectomy. Axial images show that the vaginal vault is located posterior to the bladder and anterior to the rectum at or near the level of the acetabula. It is roughly rectangular or oblong in shape, and should be symmetric and sharply marginated from surrounding fat. The bladder and loops of the small intestine occupy the space just superior to this level (1). The most common CT and MR imaging feature of recurrent tumor of the primary site is an irregular mass averaging 4-7 cm in diameter between the bladder and rectum (3). Central necrosis and irregular enhancement are common findings (Figs. 1, 2), but the lesion may be seen on CT or MR imaging as an area of homogenous soft tissue density. The vaginal vault may be the first site of recurrence.
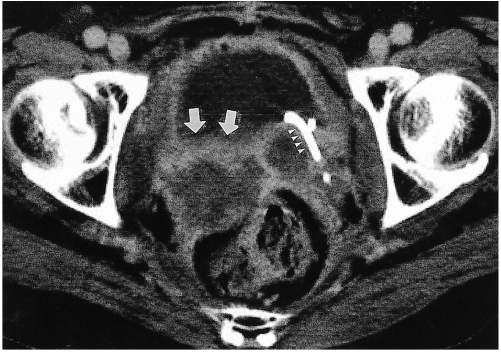
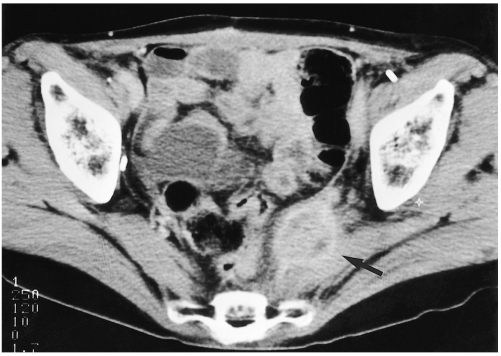
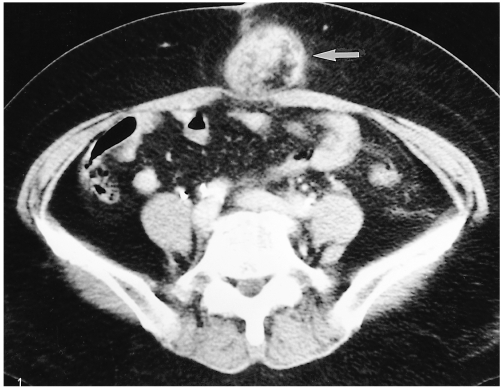
Fig. 1.
Recurrence at the vagina in a 41-year-old woman who underwent hysterectomy and radiation therapy. CT scan reveals an irregular mass (arrows) between the bladder and rectum, and the presence of a centrally located low-attenuated area indicates necrosis and peripheral enhancement. On the left, a double-pigtail ureteral stent (arrowheads) is visible.
Fig. 2.
Recurrence at the uterus following radiation therapy without hysterectomy in a 61-year-old-woman. CT scan shows a central pelvic mass (arrows) replacing the uterus. The central low-attenuated area represents necrosis.
INVASION OF THE BLADDER AND RECTUM
If CT reveals loss of the fat plane between the tumor and the bladder or rectum, invasion of these entities (Figs. 3 and 4) has occurred. MR imaging provides superior soft-tissue contrast, and its use may therefore more accurately detect the occurrence of such invasion. A diagnosis of vesical or rectal invasion by means of T2-weighted MR imaging can involve loss of the normal low signal intensity of the bladder or rectal wall continuous to the mass as well as the loss of normal fat planes (6). Kim and Han (6) reported that in depicting vesical invasion of the urinary bladder in uterine cervical carcinoma, the sensitivity, specificity, and accuracy of MR imaging was 83%, 100%, and 99%, respectively. The MR imaging findings of vesical invasion include nodularity and irregularity of the bladder wall, masses protruding into the bladder lumen, high signal intensity of the anterior aspect of the posterior bladder wall, and abnormal soft-tissue strands in the uterovesical space, implying desmoplastic reaction (6). A fistula sometimes forms, and urine or fecal material may be present in remaining vagina.
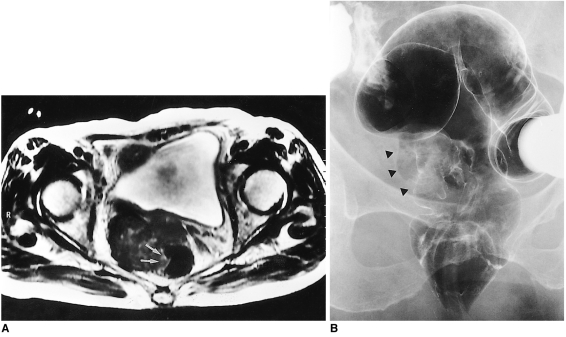
Fig. 3.
Recurrence at the primary site with posterior extension to the rectum in an 80-year-old woman who underwent radical hysterectomy.
A. T2-weighted axial MR image shows an irregular shaped, low signal mass between the bladder and rectum. The mass is continuous with the rectal wall (arrows), and protrudes into the rectal lumen.
B. Barium enema shows luminal irregularity and mucosal destruction of the lateral wall of the rectum, indicating the invasion of rectal mucosa (arrowheads).
Fig. 4.

Recurrence at the primary site, with invasion of the urinary bladder, in a 41-year-old woman. T2-weighted sagittal MR image reveals a large, necrotic mass in the vagina and uterine cervix. A fistula (arrow) between the necrotic cavity of the mass and the urinary bladder is clearly visible.
HYDROMETRA DUE TO CERVICAL MASS
In patients who have not undergone hysterectomy, local tumor recurrence or radiation fibrosis may cause obstruction of the cervical os, leading to hydrometra or pyometra (Fig. 5) (1). The CT appearance is that of a symmetrically enlarged uterus with a low-attenuation, non-enhancing central mass. This central low attenuation and lack of contrast enhancement help differentiate an obstructed uterus from other causes of uterine enlargement (2).
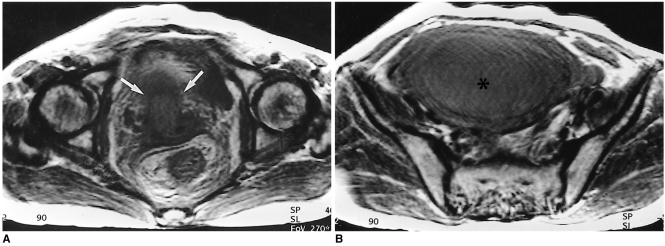
Fig. 5.
Hydrometra due to obstruction of the cervical os in a 57-year-old woman who underwent radiation therapy without hysterectomy.
A. T2-weighted axial MR image shows a low signal mass (arrows) located in the cervical portion of the uterus and anterior to the rectum.
B. In the upper level than in A (also a T2-weighted image), a fluid-filled, dilated uterus is visible. The low signal intensity of fluid in the uterine cavity implies the presence of highly proteineous material.
RECURRENT MASS AT PELVIC SIDE-WALL
Recurrent mass at the pelvic side-wall is another common finding, and since it may or may not be accompanied by a recurrent mass at the primary site (3, 5) (Fig. 6), is separately discussed. It is characterized either by direct continuation of the mass to the pelvic side-wall by means of a linear strand of soft tissue, and involving loss of the fat planes, or by confluence of the solid mass and the muscle of the pelvic wall (1) (Fig. 7). Pelvic bone can be destroyed by tumor invasion (Fig. 8). A recurrent mass at the pelvic side-wall most commonly occurs in the parametria adjacent to the uterine corpus and additional lateral extension might occur at the level of the cervix and vagina (1). Kim et al (5) reported that the there is no significant difference in the incidence of pelvic side-wall extension between patients who undergo surgery and those treated by radiation therapy.
Fig. 6.
Pelvic side-wall extension with invasion of gluteal muscle in a 28-year-old woman. CT scan demonstrates the presence of a necrotic mass (arrows) in the posterolateral aspect of the urinary bladder. The mass extends to the left posterior pelvic side-wall and invades the gluteus muscle.
Fig. 7.
Pelvic side-wall extension with destruction of the pelvic bone in a 60-year-old woman. CT image shows a necrotic mass (arrows) with bulging contour in the posterior pelvic wall, and sacral destruction has occurred.
Fig. 8.
Pelvic side-wall extension without central pelvic mass in a 44-year-old woman who underwent hysterectomy. A round enhancing mass (arrow) is visualized anterior to the left pyriformis muscle. The fat plane between the mass and the pyriformis muscle is obliterated. In this patient, there is no evidence of recurrence at the primary site.
LYMPH NODE METASTASIS
The rich cervical lymphatic network drains into the parametrial, external iliac (including obturator), internal iliac, and lateral sacral lymph nodes, and from there, draining proceeds into the common iliac and para-aortic nodes. The lymphatic spread of uterine cervical carcinoma usually follows the pelvic pathway, the common route for the lymphatic spread of tumors of the pelvic organs, and one which can be divided into the anterior, lateral, hypogastric, and presacral sections. In uterine cervical carcinoma, the lateral route is the most common (7).
In uterine cervical carcinoma, lymphatic involvement has traditionally been separated into primary and secondary nodal groups. The first of these consists of the paracervical, parametrial, internal and external iliac, and obturator nodes, while those comprised by the second include the sacral, common iliac, inguinal and para-aortic (4). When the secondary nodal group is involved, the prognosis worsens. In this article, the system used to classify lymphadenopathy - namely, that this involves either pelvic or extrapelvic lymphnode metastasis - is one suited to the use of cross-sectional imaging techniques.
PELVIC LYMPH NODE METASTASIS
The incidence of pelvic lymph node metastases in uterine cervical carcinoma varies according to the size, extent and histologic type of the primary tumor. A study by Walsh et al (8) showed that in 38% of patients with central pelvic recurrence, pelvic adenopathy was also present. The reported accuracy rate for CT in detecting pelvic node metastasis in patients with uterine cervical carcinoma ranged between 73 and 83%, while the rate for MRI was between 76 and 100% (9). The CT and MR imaging criterion for positive lymph node is a minimal axial diameter of at least 1 cm (10). The CT and MR imaging findings of metastatic nodes vary, ranging from scattered and minimally enlarged to large conglomerated masses (Fig. 9). A finding of central necrosis is not helpful for differentiating metastatic nodes from those that are non-metastatic and hyperplastic (10).
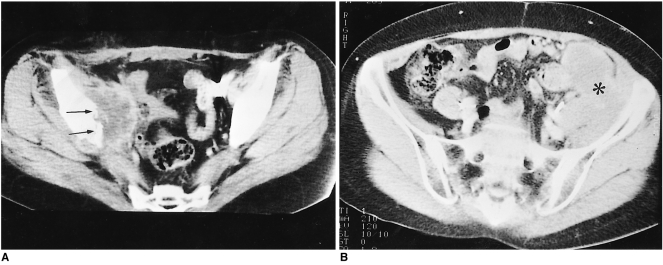
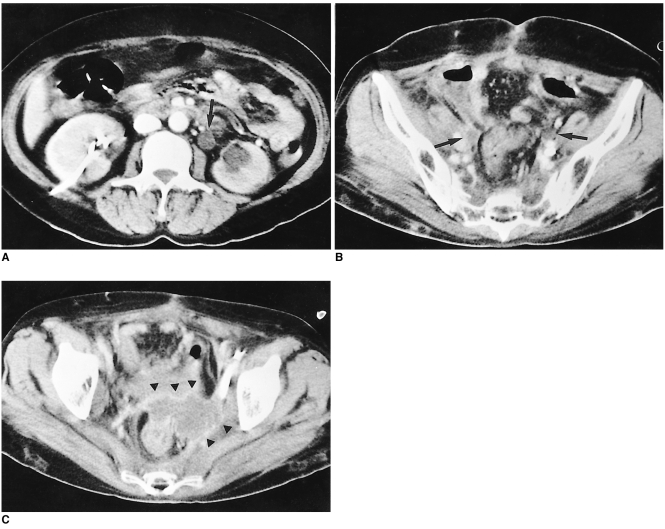
Fig. 9.
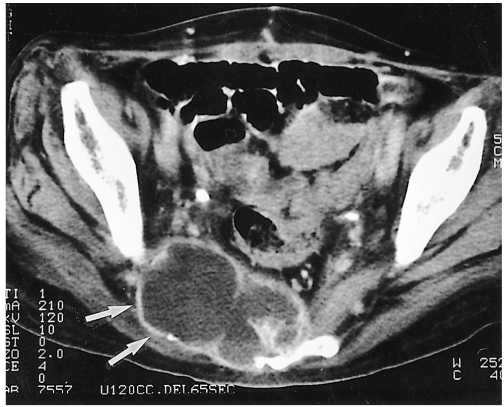
Pelvic lymph node metastases.
A. Obturator node metastasis in a 36-year-old woman who underwent radical hysterectomy and radiation therapy. A peripherally enhancing, low-attenuated mass (arrows) attached to the right iliac bone and anterior to the pyriformis muscle is revealed by CT scanning. Destruction of the pelvic bone is also visible.
B. Iliac node metastasis in a 52-year-old woman. Conglomerated, iso-attenuated masses (asterisk) are seen in the medial aspect of the left iliac wing.
EXTRAPELVIC LYMPH NODE METASTASIS
Extrapelvic lymph nodes - particularly the supraclavicular, para-aortic, and inguinal, in decreasing order of frequency - are common sites of distant metastasis (Fig. 10). In many cases in which confirmed recurrent disease was detected by CT, lymphadenopathy involved only the paraaortic nodes (8). The incidence of recurrence at this site is higher in patients treated by radiation therapy than in those who undergo surgery, and this, as well as the higher incidence of pelvic side-wall extension in such cases, is probably because the tumor stage is generally more advanced and the field of radiation therapy is relatively narrow (5).
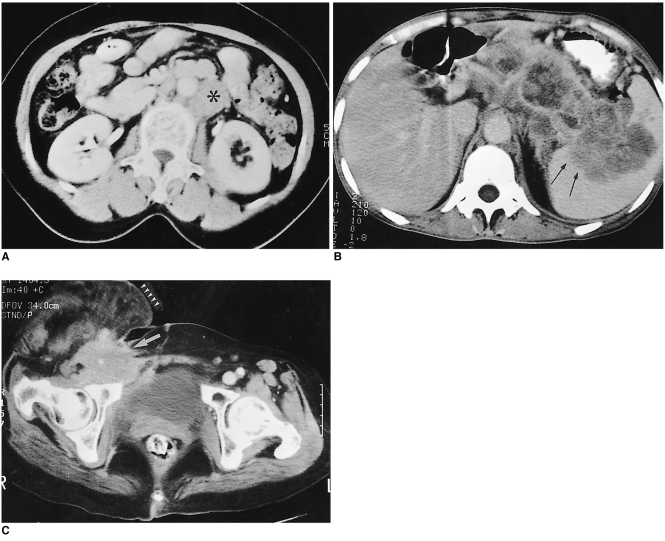
Fig. 10.
Extrapelvic node metastases.
A. Para-aortic node metastasis in a 45-year-old woman. CT scan shows an enlarged para-aortic lymph node (asterisk), which in this patient is the only site involved by recurrent disease.
B. Retroperitoneal lymph node metastasis in a 40-year-old woman. Extensive lymphadenopathy in the para-aortic region and around the celiac trunk is detected by CT. This lesion extends into the splenic hilum (arrows).
C. Inguinal node metastasis. CT scan indicates the presence of an enlarged right inguinal lymph node (arrow). Also note the presence of swelling and soft tissue edema in the right lower extremity (arrowheads) due to lymphatic and venous obstruction by metastatic lymphadenopathy.
DISTANT METASTASIS
The common sites of distant metastasis are the lung, bone, and the abdomen, in decreasing order of frequency, though in cases of recurrent cervical carcinoma, the solid organs of the abdomen are the most frequent sites of involvement. In three separated autopsy series, pulmonary metastasis from recurrent cervical carcinoma, which may exist for a significant period of time before becoming symptomatic and may be either solitary or multiple, occurred in 33-35% of cases (4). Typical patterns of lung involvement are pulmonary nodules (71%), mediastinal and hilar lymphadenopathy (32%), and pleural metastasis (27%). Rare findings include endobronchial obstruction (5%), and lymphangitic carcinomatosis (3%) (Fig. 11).
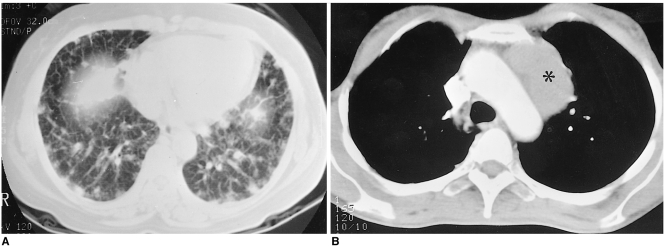
Fig. 11.
Pulmonary metastases.
A. Hematolymphangitic metastasis in a 47-year-old woman. Lung window setting of the lower part of the lung demonstrates multiple nodules and interlobular septal thickening.
B. Pulmonary metastasis manifested as mediastinal lymphadenopathy in a 45-year-old woman who two years earlier underwent hysterectomy. CT scan shows large mediastinal (para-aortic) lymph nodes (asterisk). Percutaneous needle biopsy confirmed that adenocarcinoma had metastasized from the uterine cervix.
The spine, especially the lumbar spine, is the most common site of osseous metastasis. Involvement of the vertebral bodies, the mechanism of which is direct extension of the tumor subsequent to para-aortic lymphadenopathy, is most frequent, followed by that of the pelvis, ribs, and extremities (2).
Abdominal metastasis occurred in the peritoneal cavity (Fig. 12) and solid organs such as the liver (Fig. 13) and adrenal gland (Fig. 14). Peritoneal metastasis, including peritoneal carcinomatosis, is more common than metastasis to the liver. The CT and MR imaging findings of metastases to the peritoneal cavity are ascites, implants scalloping the liver contour, peritoneal thickening with nodularity, and soft tissue mass(4). The CT and MR imaging findings of hepatic and adrenal involvement in recurrent cervical carcinoma are non-specific and indistinguishable from involvement by other primary malignancies. The involvement of another solid abdominal solid organ such as the spleen (Fig. 15), kidney, pancreas or gastrointestinal tract is rare, and in almost all cases, widespread metastasis involving other organs also occurs.
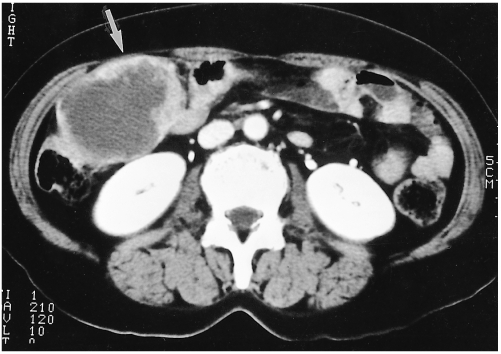
Fig. 12.
Metastasis to the peritoneal cavity in a 48-year-old woman. Abdominal CT scan indicates the presence of a mass (arrow) with extensive central necrosis and lobulated contour in the right upper quadrant.
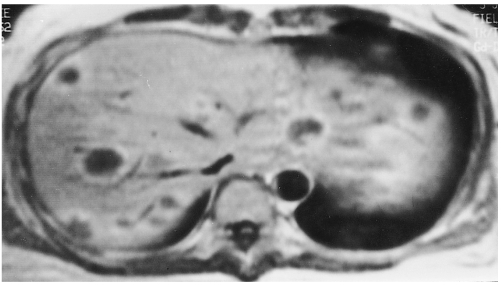
Fig. 13.
Multiple hepatic metastases in a 44-year-old woman. Contrast-enhanced T1-weighted axial MR image shows multiple, target-shaped lesions with peripheral enhancement in the liver.
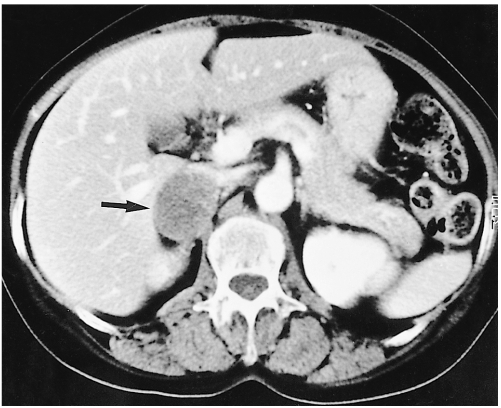
Fig. 14.
Adrenal metastasis in a 61-year-old female. CT scan indicates the presence in the right adrenal gland area of an ovalshaped low-attenuated, 4 cm-sized mass (arrow). Needle biopsy confirmed the occurrence of metastatic carcinoma.
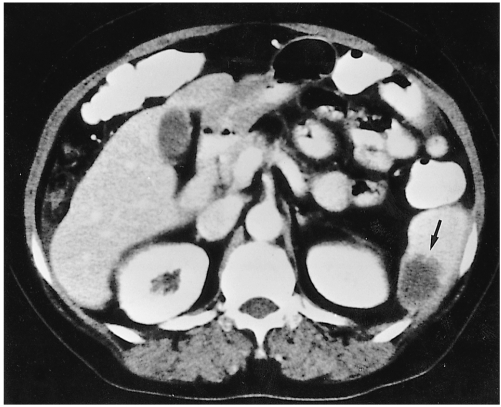
Fig. 15.
Splenic metastasis in a 53-year-old woman who underwent hysterectomy. Enhanced CT scan reveals the presence in the spleen of an ill-defined low-attenuated mass (arrow).
In the detection of abdominal recurrence, the most important problem related to the use of CT and MR imaging is the fact that because the known pattern of spread of the disease is through the iliac and aortic lymph nodes, most such scanning routinely covers the region from the iliac crests to the symphisis pubis. So that other recurrent lesions are not missed, scanning of a cervical neoplasm should, however, include the upper abdomen.
The common primary sites in patients with skin or subcutaneous metastasis are the breast, colon, lung, and ovary; skin metastasis from uterine cervical carcinoma is extremely rare. The most common sites of skin lesions are the abdominal wall and vulva, followed by the anterior chest wall, and in most patients there are multiple lesions. Recurrence at the site of a surgical scar is rare, but is a possible complication of hysterectomy (Fig. 16). It is classified as skin and subcutaneous involvement, and occurs mainly in patients who have not undergone combined radiation therapy or whose radiotherapeutic field did not include the surgical scar.
Fig. 16.
Subcutaneous metastasis to a surgical scar in a 55-year-old woman who underwent radical hysterectomy and radiation therapy. CT scan shows a round heterogenous mass (arrow) in subcutaneous abdominal tissue in the region of the scar.
URETERAL OBSTRUCTION
Another contribution of CT and MR imaging in recurrent uterine cervical carcinoma is the detection of ureteral obstruction, and determination of the etiology and level (3). Such obstruction is due to the encasement or extrinsic compression of a recurrent pelvic mass (Fig. 17) or metastatic lymph nodes (Figs. 18, 19), or tumor infiltration of the bladder wall, which results in obstruction at the ureteral orifice. The site of ureteral obstruction is usually revealed by scanning of the retroperitoneal or pelvic area (3).
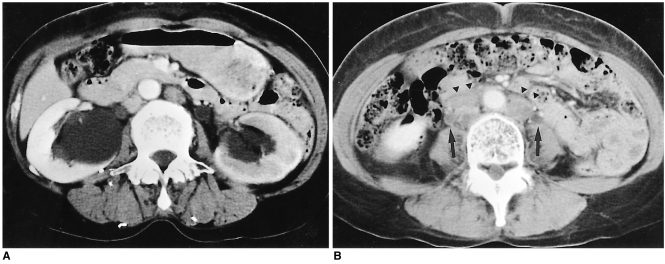
Fig. 17.
Hydronephrosis due to ureteral obstruction caused by recurrence at the primary site in a 41-year-old woman who underwent radical hysterectomy and radiation therapy.
A. CT scan demonstrates hydronephrosis of the left kidney and that the patient had undergone percutaneous nephrostomy of the right kidney. A dilated left ureter (arrow) is depicted.
B. In the lower level than in A, dilated bilateral ureters (arrows) can be traced.
C. Anterior to the rectum, an irregular shaped mass (arrowheads) encased the dilated left ureter. Pelvic side-wall extension is also visualized.
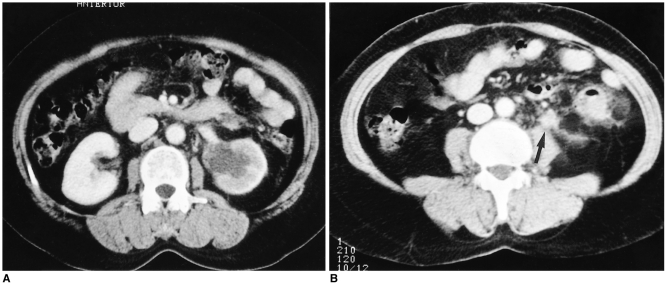
Fig. 18.
Hydronephrosis due to ureteral obstruction by retroperitoneal lymph node metastasis in a 61-year-old woman.
A. Enhanced CT scan shows bilateral hydronephrosis and decreased perfusion of the left kidney.
B. In the lower level than in A, a dilated right ureter (arrow) is visualized, and the presence of retroperitoneal lymphadenopathy is also visu alized (arrowheads).
Fig. 19.
Hydronephrosis due to ureteral obstruction by periureteral lymph node in a 49-year-old woman.
A. CT scan shows hydronephrosis of the left kidney, with decreased renal perfusion.
B. In the lower level than in A, a periureteral lymph node (arrow) obstructing the left ureter is depicted. The ureter can not be traced in this level.
CONCLUSION
The recurrence of uterine cervical carcinoma can involve various organs, with various patterns of imaging findings. CT and MR imaging are the primary imaging modalities used during the follow-up of treated cervical carcinoma. Since the early detection of recurrent cancer makes for a better prognosis, radiologists should be familiar with the spectrum of CT and MR imaging findings of recurrent uterine cervical carcinoma. Recurrence which is extrapelvic or involves the pelvic side-wall is more common in patients who undergo radiation therapy only, a fact probably due to the more advanced stage of the disease in such patients and the limited field within which radiation therapy is possible. More careful examination is, therefore, necessary for the patients treated by radiation therapy only. In the evaluation of pelvic malignancies, including uterine cervical carcinoma, careful examination of the upper abdomen is required in addition to routine pelvic scanning.
References
- 1.Walsh JW. Computed tomography of the pelvis. Churchill Livingstone: New York; 1985. pp. 195–198. [Google Scholar]
- 2.Carlson V, Delclos L, Fletcher GH. Distant metastases in squamous-cell carcinoma of the uterine cervix. Radiology. 1967;88:961–966. doi: 10.1148/88.5.961. [DOI] [PubMed] [Google Scholar]
- 3.Walsh JW, Amendola MA, Hall DJ, Tisnado J, Goplerud DR. Recurrent carcinoma of the pelvis: CT diagnosis. AJR. 1981;136:117–122. doi: 10.2214/ajr.136.1.117. [DOI] [PubMed] [Google Scholar]
- 4.Fulcher AS, O'Sullivan SG, Segreti EM, Kavanagh BD. Recurrent cervical carcinoma: Typical and atypical manifestations. RadioGraphics. 1999;19:s103–s116. doi: 10.1148/radiographics.19.suppl_1.g99oc19s103. [DOI] [PubMed] [Google Scholar]
- 5.Kim JE, Park HA, Kim KH, Lim D, Chin SY. Patterns of recurrent cervical carcinoma on CT. J Korean Radiol Soc. 1988;24:1130–1134. [Google Scholar]
- 6.Kim SH, Han MC. Invasion of the urinary bladder by uterine cervical carcinoma: evaluation with MR imaging. AJR. 1997;168:393–397. doi: 10.2214/ajr.168.2.9016214. [DOI] [PubMed] [Google Scholar]
- 7.Park JM, Charnsangavej C, Yoshimitsu K, Herron DH, Robinson TJ, Wallace S. Pathways of nodal metastasis from pelvic tumors: CT demonstration. RadioGraphics. 1994;14:1309–1321. doi: 10.1148/radiographics.14.6.7855343. [DOI] [PubMed] [Google Scholar]
- 8.Walsh JW, Amendola MA, Konerding KF, Tisnado J, Hazra TA. Computed tomographic detection of pelvc and inguinal lymph-node metastases from primary and recurrent malignant pelvic disease. Radiology. 1980;137:157–166. doi: 10.1148/radiology.137.1.7422839. [DOI] [PubMed] [Google Scholar]
- 9.Kim SH, Choi BI, Lee HP, Kang SB, Choi YM, Han MC, Kim CW. Uterine cervical carcinoma: Comparison of CT and MR findings. Radiology. 1990;175:45–51. doi: 10.1148/radiology.175.1.2315503. [DOI] [PubMed] [Google Scholar]
- 10.Kim SH, Kim SC, Choi BI, Han MC. Uterine cervical carcinoma: Evaluation of pelvic lymph node metastasis with MR imaging. Radiology. 1994;190:807–811. doi: 10.1148/radiology.190.3.8115631. [DOI] [PubMed] [Google Scholar]