Abstract
Rationale: Although inadequate health literacy has been associated with lower asthma medication knowledge and worse metered-dose inhaler (MDI) technique, the relationship between health literacy and the capacity to learn asthma self-management skills is unknown.
Objectives: In this prospective cohort study of adults hospitalized for severe asthma exacerbations at two inner-city hospitals, we examined the relationship between inadequate health literacy and difficulties learning and retaining instructions about discharge medications and appropriate MDI technique.
Methods: At hospital discharge, participants received one-on-one, 30-min, guideline-based, written and oral instruction about their asthma discharge regimen as well as appropriate MDI technique.
Measurements and Main Results: Seventy-three patients were enrolled. Inadequate health literacy was identified in 16 (22%) participants. Before instruction, inadequate health literacy was associated with lower asthma medication knowledge (5.2/10 vs. 7.2/10, p < 0.001) and worse MDI technique (3.2/6 vs. 3.9/6, p =0.03). However, inadequate health literacy was not associated with difficulty learning (p =0.33) or retaining (p =0.35) instructions about the discharge regimen. Similarly, inadequate health literacy was not associated with difficulty learning (p =0.26) or retaining (p =0.97) appropriate MDI technique. Results were similar in multivariable models adjusted for demographic characteristics and asthma severity indicators.
Conclusions: These findings suggest that inadequate health literacy is a surmountable barrier to learning and remembering key asthma self-management skills.
Keywords: asthma, education, functional health literacy
Health literacy is “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” (1–4) and is most often measured by reading comprehension of health-related information (5, 6). Multiple studies indicate that inadequate health literacy is associated with worse health status and higher rates of hospitalization across a number of patient populations (4, 7, 8), including patients with diabetes mellitus, patients with HIV infection, and the elderly (9–12). However, there are relatively few data about the effects of inadequate health literacy in patients with asthma, a common chronic respiratory disorder affecting 5 to 10% of the U.S. population (13). In cross-sectional studies, inadequate health literacy has been linked to lower asthma-related knowledge (14, 15) and improper use of metered dose inhalers (MDIs) (14). Although national asthma guidelines recommend patient education to improve patient–physician partnerships for care (16), no studies have evaluated the extent to which inadequate health literacy serves as a barrier for patients to learn and retain asthma self-management skills (17).
The objective of this study was to examine the relationship between inadequate health literacy and difficulties learning and retaining instructions about discharge medications and appropriate MDI technique. We recruited an inner-city predominately African-American patient population hospitalized for asthma exacerbations, a group at high risk for low health literacy and a two- to threefold risk of death from asthma exacerbations (18–20). We hypothesized that inadequate health literacy is associated with lower knowledge of asthma medications, improper use of MDI technique, as well as difficulty learning and retaining instructions about discharge medications and proper MDI technique. These hypotheses represent secondary goals of a study also intended to examine adherence to corticosteroid therapy after hospital discharge (21). Some results of the current study have been previously reported in the form of an abstract (22).
METHODS
Study Design
This was a prospective cohort study conducted from April 2001 through October 2002. Adults (age, ⩾ 18 yr) admitted with a physician diagnosis of asthma exacerbation to two inner-city academic medical centers were screened for eligibility. Patients with other chronic lung diseases, those with a contraindication to corticosteroids, patients (or physicians) who declined consent, and investigators' patients were excluded. The study was approved by the Johns Hopkins Institutional Review Board.
Study Procedures
At hospital discharge (discharge study visit), eligible subjects were approached about participating in this study. Patients who provided written, informed consent were enrolled. Participants completed an interviewer-administered survey about sociodemographics (age, sex, ethnicity, education, income), smoking history (never, ever, current), and asthma-related health care use (emergency department or hospitalization) in the past year. On the basis of a review of medical records and interview responses, subjects were classified as having a history of near-fatal asthma exacerbation if they had ever been intubated due to asthma (yes vs. no).
Health literacy was measured with the Short Test of Functional Health Literacy in Adults and classified as having inadequate health literacy (yes [score ⩽ 16/36] vs. no [score > 16/36]), based on published recommendations (23, 24). The Short Test of Functional Health Literacy in Adults is a test of reading comprehension that takes 5 to 7 min to administer. The test has a set of sentences from medical scenarios with key words missing. Subjects select words to complete the sentences from a list provided. There are 36 items and each correct response is awarded 1 point (range of possible scores, 0–36). The test has high internal consistency (Cronbach's α =0.97) and is well correlated with the Rapid Estimate of Adult Literacy in Medicine (Spearman correlation, 0.81) and the full Test of Functional Health Literacy in Adults (Spearman correlation, 0.91) (25).
In addition, we also assessed patients' understanding of asthma medications. There were no previously validated measures to assess patients' understanding of asthma medications (inhaled corticosteroids, oral corticosteroids, and short-acting bronchodilators). Therefore, we developed 10 items based on existing asthma knowledge scales, professional opinion, and the desire for each item to be directly related to medication use. Participants were given 1 point for each correctly answered item. Based on a total possible score of 10, we calculated a mean asthma medication knowledge score (total score/10). Internal consistency reliability was adequate (Cronbach α =0.62) and comparable to another published asthma knowledge scale (26).
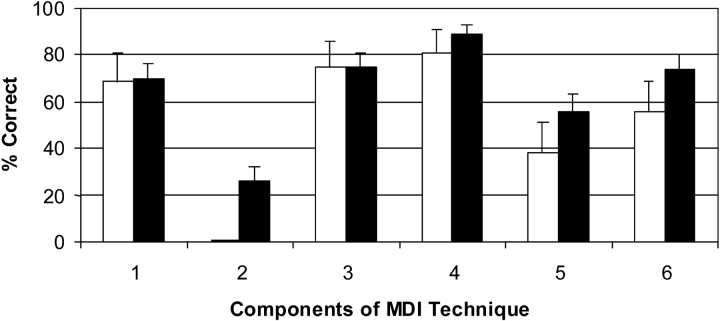
Participants were asked to demonstrate use of an MDI. Participants' MDI technique was assessed on the basis of the following six criteria (16, 27–30): (1) shaking the MDI, (2) exhaling before actuation, (3) closing lips tightly around the mouthpiece, (4) pressing down once on the canister, (5) taking a full/deep breath without triggering the auditory “whistle” indicator of the spacer, and (6) holding breath for at least 5 s. One point was given for each step for a total possible score of 6 as follows: 0 (unable to perform any step) to 6 (perfect technique; Figure 1). The asthma discharge regimen was standardized to include both oral corticosteroids (prednisone: 20 mg/tablet, 2 tablets each morning for 7 d), inhaled corticosteroids (fluticasone MDI: 220 μg/puff, 2 puffs twice/d), and a short-acting bronchodilator (albuterol MDI: 2 puffs every 4 h as needed). These medications and a spacer for use with MDIs were provided for free to study participants. Participants took part in a one-on-one, 30-min-long, guideline-based, written and oral asthma-education session about this discharge regimen. This session included education about appropriate MDI technique; the research assistant provided both verbal instructions and demonstrated proper technique to study participants. After the education intervention and before discharge, participants were asked to state the following: (1) the name of each medication, (2) the number of tablets or actuations to be taken each time, (3) the number of times per day the medication should be taken, and (4) the prescribed duration of medication use. Teaching was repeated until participants could successfully demonstrate mastery of the asthma discharge regimen (defined as correctly describing items 1–4 for all three of the medicines) and MDI technique (30). The number of rounds of teaching necessary to achieve mastery of the asthma discharge regimen and MDI technique was recorded.
Figure 1.
Proportion (%) of patients correctly performing each component of metered-dose inhaler (MDI) technique according to literacy level. Inadequate health literacy: white bars =yes; black bars =no. 1: shaking the inhaler (p =0.91); 2: exhaling before actuation (p =0.02); 3: closing lips around mouthpiece (p =0.97); 4: pressing down once (p =0.38); 5: taking a full/deep breath without triggering “whistle” (p =0.19); 6: holding breath > 5 s (p =0.18).
Participants returned for a 2-wk follow-up visit. At the follow-up visit, participant's MDI technique and knowledge of the asthma discharge regimen were reevaluated. In addition, at follow-up, asthma symptom control was assessed using the six symptom items in the Asthma Control Questionnaire (31). The total possible asthma symptom control was (0, well controlled, to 6, extremely poorly controlled).
In a subset of participants (n =46) enrolled in the current study, we also electronically measured patients' use of inhaled and oral corticosteroids after hospital discharge. Adherence to inhaled corticosteroids was assessed using the Doser CT (Meditrac, Inc., Hudson, MA), which records the number of actuations of the fluticasone MDI each day (32, 33). Adherence to oral corticosteroids was assessed using the MEMS TrackCap (AARDEX Ltd., Union City, CA), which records the number of prednisone bottle openings each day (34–36). Adherence was defined as percentage of prescribed use after hospital discharge (use/prescribed use × 100%) and was calculated for both inhaled and oral corticosteroids. Poor adherence to corticosteroid therapy was defined a priori as electronically measured adherence to inhaled corticosteroids of less than 50% during the 2-wk period after hospital discharge or electronically measured adherence to oral corticosteroid therapy of less than 50% from hospital discharge through Day 7 (oral corticosteroids were prescribed for the first 7 d after discharge).
The data collection and educational intervention were conducted by a trained research assistant using standardized text and questionnaires. To minimize interviewer bias, the health literacy status of participants was not available to the interviewer at the follow-up visit. Also, electronic adherence data were collected after the interviewer-administered survey. Participants were informed that medication use was assessed, but were not told about precise monitoring abilities (i.e., that daily medication use was electronically measured).
Thus, at the discharge study visit, data regarding sociodemographics, asthma care, smoking history, morbidity, health literacy, asthma medication knowledge, and MDI technique were collected before any educational intervention. After the first and subsequent rounds of education, knowledge of the asthma discharge regimen and MDI technique were assessed. The education was repeated until participants could demonstrate mastery of the asthma discharge regimen and MDI technique. At the follow-up visit, knowledge of the asthma discharge regimen and MDI technique were tested again, adherence data for corticosteroid therapy were collected, and asthma symptom control was assessed.
Statistical Analyses
Descriptive statistics used means, medians, and proportions. Wilcoxon rank sum, matched pairs signed rank, or χ2 tests were used in bivariate analyses. Logistic regression models were used to determine if inadequate health literacy was an independent predictor of the following outcomes: better asthma medication knowledge (yes [⩾ mean score] vs. no), better MDI technique (yes [⩾ mean score] vs. no), mastery of the discharge regimen after one round (yes vs. no), poor adherence to corticosteroid therapy (adherence < 50%: yes vs. no) (21), and better asthma symptom control (yes [⩾ mean score] vs. no). To determine if knowledge about medications mediated the relationship between inadequate health literacy and inferior self-management practices, we constructed additional models in which we included “better asthma medication knowledge” as a covariate in models to predict “better MDI technique” and “poor adherence to corticosteroid therapy.”
Each regression model included the identical set of demographic and asthma severity indicators as independent variables: inadequate health literacy (yes vs. no; primary predictor of interest), age (quartiles), sex, ethnicity (African American vs. white), education level (high school graduate or equivalent degree; yes vs. no), income (annual combined household income ⩽ $19,999: yes [⩽ mean score] vs. no), history of near-fatal asthma (yes vs. no), asthma hospitalization in the prior 12 mo (yes vs. no), having a physician for asthma care (yes vs. no), and prior emergency department visits for asthma in the past 12 mo (yes vs. no). Results were similar when we analyzed outcomes as continuous or as binary variables; we presented the latter results to facilitate interpretation. To avoid overfitting the regression models, we elected to use a backward stepwise procedure in the multivariable logistic regression models to identify the most influential predictors for each of the outcomes (p < 0.2 for removal) (37). A two-tailed p value of less than 0.05 defined statistical significance. Computations were performed using STATA, version 7.0. (StataCorp, College Station, TX). Additional details regarding the methods are available in the online supplement.
RESULTS
Of 136 patients screened for eligibility, 36 met the following exclusion criteria: history of another chronic lung disease (n =20), discharged to location other than home (n =8), clinic patient of an investigator (n =2), and contraindication to corticosteroids (n =6). Of 100 eligible patients, 8 patients were excluded because the physician declined consent and 19 were excluded because the patient declined consent.
Seventy-three patients (73% of eligible) were enrolled. Participants' mean age was 41 yr and they were mostly African American, female, unmarried, and employed. There was substantial evidence of previous asthma morbidity among participants, with more than three-quarters reporting at least one other emergency department visit for an asthma exacerbation in the previous 12 mo and nearly half with a history of near-fatal asthma. Fifty-six participants (77% of enrolled) returned for the 2-wk follow-up visit. Those not returning for the 2-wk visit were younger, had lower asthma medication knowledge scores, and tended to be African American. However, health literacy was similar, whether or not patients returned for the follow-up visit (Table 1).
TABLE 1.
Patient characteristics for subjects with and without 2-WK data
| All (n =73) | With 2-wk Data (n =56) | Without 2-wk Data (n =17) | p Value‡ | |
|---|---|---|---|---|
| Sociodemographics | ||||
| Age, mean yr (SD, range) | 40.9 (10.9) | 43.0 (11.1) | 33.9 (7.1) | < 0.01 |
| Female | 48 (66) | 35 (63) | 13 (76) | 0.29 |
| Race | 0.09 | |||
| African American | 58 (79) | 42 (75) | 16 (94) | |
| White | 15 (21) | 14 (25) | 1 (6) | |
| High school graduate or GED | 44 (60) | 32 (57) | 12 (71) | 0.32 |
| Income ⩾ $19,999* | 36 (65) | 27 (63) | 9 (75) | 0.43 |
| Asthma-related health care use | ||||
| Hospitalization past 12 mo† | 42 (58) | 35 (63) | 7 (44) | 0.18 |
| ED visit past 12 mo† | 55 (77) | 43 (78) | 12 (75) | 0.79 |
| Near-fatal asthma | 31 (42) | 23 (41) | 8 (47) | 0.66 |
| Inadequate health literacy | 16 (22) | 12 (21) | 4 (24) | 0.85 |
| Cigarette smoking history | 0.43 | |||
| Never smoker | 32 (44) | 26 (46) | 6 (35) | |
| Past smoker | 20 (27) | 16 (29) | 4 (24) | |
| Current smoker | 21 (29) | 14 (25) | 7 (41) | |
| Physician for asthma care | 37 (51) | 30 (54) | 7 (41) | 0.37 |
| Asthma knowledge score (SD) | 6.9 (2.0) | 7.2 (1.9) | 6.2 (2.2) | 0.07 |
Definition of abbreviations: ED =emergency department; GED =general equivalency diploma.
Values are given as numbers with percentages in parentheses unless otherwise noted.
Limited data due to nonresponse (n =55).
Excludes current hospitalization/ED visit.
Wilcoxon rank sum test or χ2 test.
Health Literacy
At the discharge study visit, 16 (22%) participants had inadequate health literacy. Sociodemographic characteristics (including age) were similar in patients with and without inadequate health literacy (Table 2). However, participants with inadequate health literacy were significantly more likely to have been hospitalized for asthma in the past 12 mo (81 vs. 52%, p =0.04) and there was a trend toward a higher rate of near-fatal asthma in patients with inadequate health literacy (63 vs. 37%, p =0.07).
TABLE 2.
Patient characteristics by level of health literacy
| Inadequate Health Literacy
|
|||
|---|---|---|---|
| Yes (n =16) | No (n =57) | p Value‡ | |
| Sociodemographics | |||
| Age, mean yr (SD, range) | 41.1 (12.9) | 40.8 (10.5) | 0.92 |
| Female | 9 (56) | 39 (68) | 0.37 |
| Race | |||
| African American | 15 (94) | 43 (75) | |
| White | 1 (6) | 14 (25) | 0.11 |
| High school graduate or GED | 9 (56) | 35 (61) | 0.71 |
| Income ⩽ $19,999* | 8 (57) | 28 (68) | 0.45 |
| Asthma-related health care use | |||
| Hospitalization past 12 mo† | 13 (81) | 29 (52) | 0.04 |
| ED visit past 12 mo† | 14 (88) | 41 (75) | 0.28 |
| Near-fatal asthma | 10 (63) | 21 (37) | 0.07 |
| Cigarette smoking history | 0.31 | ||
| Never smoker | 6 (38) | 26 (46) | |
| Past smoker | 3 (19) | 17 (30) | |
| Current smoker | 7 (44) | 14 (25) | |
| Physician for asthma care | 7 (44) | 30 (53) | 0.53 |
For definition of abbreviations, see Table 1.
Values are given as numbers with percentages in parentheses unless otherwise noted.
Limited data due to nonresponse (n =55).
Excludes current hospitalization/ED visit.
Wilcoxon rank sum test or χ2 test.
Asthma Medication Knowledge Questionnaire
At the discharge study visit, the mean asthma medication knowledge score was 6.8 (of 10, SD =2.1; Table 3). Participants with inadequate literacy had lower Asthma Medication Knowledge scores (odds ratio [OR] for better asthma medication knowledge score, 0.11; 95% confidence interval [CI], 0.03–0.42; p =0.001; Table 4). Participants with inadequate health literacy were less likely to correctly answer every question, with significant differences noted for 5 of 10 items. In a multivariate logistic model, inadequate health literacy was the only significant independent predictor of asthma medication knowledge (OR for better asthma medication knowledge score, 0.08; 95% CI, 0.02–0.38; p =0.002).
TABLE 3.
Asthma medication knowledge according to literacy level
| Inadequate Health Literacy
|
|||
|---|---|---|---|
| Question (correct answer) | Yes, % correct (n =16) | No, % correct (n =57) | p Value‡ |
| Even if I have no symptoms from my asthma, I should take (say β2-agonist they are on)*every day so that I can stop asthma attacks from starting (False) |
10 | 60 | < 0.01 |
| If I am told to take two puffs, twice a day, then I should press down on the inhaler two times before I start to take a breath (False) |
40 | 87 | < 0.01 |
| The longer I wait to treat an asthma attack after it begins, the easier it is to stop the attack (False) | 75 | 96 | < 0.01 |
| When I am prescribed steroid tapers like prednisone for an asthma attack, I can stop taking them as soon as I start feeling well even if I have not finished the taper (False) |
65 | 87 | 0.02 |
| (Say inhaled steroid they are on)† should be taken only when I have asthma symptoms (False) | 40 | 69 | 0.02 |
| After I press down on the inhaler, I should take a normal, regular-sized breath (False) | 25 | 49 | 0.06 |
| (Say β2-agonist they are on)*should be taken only when I have asthma symptoms (True) | 60 | 74 | 0.21 |
| (Say β2-agonist they are on)*works within minutes to help you breathe better (True) | 85 | 90 | 0.55 |
| (Say inhaled steroid they are on)† takes days or weeks before it starts to help you breathe better (True) | 50 | 55 | 0.68 |
| Even if I have no symptoms from my asthma, I should take (say inhaled steroid they are on)† every day so that I can stop asthma attacks from starting (True) |
70 | 73 | 0.78 |
| Total test score, mean (95% CI) | 5.2 (4.3–6.2) | 7.2 (6.8–7.6) | < 0.01 |
Definition of abbreviation: CI =confidence interval.
Each question has a true, false, do not know format.
If participant did not list a short-acting β2-agonist as a medication on hospital admission medication, then the phrase “medicines such as Ventolin, Proventil, Maxair, Alupent, or Albuterol” was used.
If the participant did not list an inhaled steroid as a medication on hospital admission, then the phrase “medicines like Flovent, Pulmicort, Azmacort, Vanceril, or Advair” was used.
χ2 test and Wilcoxon rank sum test.
TABLE 4.
Predictors of better asthma medication knowledge at discharge study visit, better metered-dose inhaler technique at discharge study visit, and mastery of the discharge regimen after initial round of instruction (bivariate analyses)
| Better Asthma Medication Knowledge
|
Better MDI Technique
|
Mastery of Medication Discharge Regimen |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P Value | OR | 95% CI | p Value | OR | 95% CI | P Value | |
| Inadequate health literacy | 0.1 | 0.0–0.4 | < 0.01 | 0.3 | 0.1–0.9 | 0.03 | 0.7 | 0.2–2.6 | 0.64 |
| Sociodemographics | |||||||||
| Age, quartiles | 1.1 | 0.7–1.6 | 0.77 | 1.1 | 0.7–1.7 | 0.58 | 1.2 | 0.7–2.2 | 0.49 |
| Female | 1.1 | 0.4–2.9 | 0.85 | 1.7 | 0.6–4.4 | 0.32 | 1.0 | 0.3–2.9 | 1.00 |
| White (Black is reference) | 0.3 | 0.1–1.0 | 0.06 | 0.4 | 0.1–1.4 | 0.14 | 0.4 | 0.1–1.8 | 0.22 |
| High school Graduate or GED | 0.9 | 0.4–2.4 | 0.88 | 1.4 | 0.5–3.5 | 0.54 | 0.7 | 0.3–2.1 | 0.56 |
| Asthma-related health care use | |||||||||
| Hospitalization past 12 mo* | 1.3 | 0.5–3.3 | 0.60 | 0.6 | 0.2–1.8 | 0.36 | 0.7 | 0.3–2.1 | 0.58 |
| ED visit past 12 mo* | 2.1 | 0.7–6.4 | 0.20 | 1.0 | 0.9–1.0 | 0.23 | 0.8 | 0.2–2.8 | 0.71 |
| Near-fatal asthma, ever | 0.8 | 0.3–2.1 | 0.69 | 0.2 | 0.1–0.7 | < 0.01 | 0.7 | 0.2–1.8 | 0.41 |
| Cigarettes, smoked in past | 0.6 | 0.2–1.8 | 0.37 | 0.8 | 0.3–2.5 | 0.68 | 0.6 | 0.2–2.0 | 0.42 |
| Cigarettes, currently smoking | 0.1 | 0.0–0.4 | < 0.01 | 0.3 | 0.1–1.0 | 0.05 | 0.6 | 0.2–1.9 | 0.35 |
| Asthma physician | 2.5 | 1.1–5.7 | 0.03 | 1.6 | 0.6–4.2 | 0.30 | 1.0 | 0.4–2.8 | 0.97 |
Definition of abbreviations: CI =confidence interval; ED =emergency department; GED =graduate equivalency diploma; MDI =metered-dose inhaler; OR =odds ratio.
Asthma medication knowledge was dichotomized such that a score of ⩾ 7/10 was considered better knowledge; MDI technique at the discharge study visit was dichotomized such that a score of ⩾ 4/6 was considered better technique; mastery of the discharge regimen was dichotomized such that a score of 4/4 after initial instruction was considered mastery.
Excludes current hospitalization/ED visit.
MDI Technique
The mean MDI technique score at the discharge study visit was 3.8 (of 6, SD=1.4). Failure to exhale before actuation of the MDI was the most frequently missed step. Pressing once on the canister at the time of actuation was the step that was most frequently done correctly. At the discharge study visit, subjects with inadequate health literacy were less likely to have superior MDI technique (OR for better MDI technique, 0.27; 95% CI, 0.08–0.87; p =0.03). Having a history of near-fatal asthma was also associated with worse MDI technique at discharge study visit (OR for better MDI technique, 0.20; 95% CI, 0.1–0.7; p < 0.01; Table 4). In a multivariate model, inadequate health literacy was the only significant independent predictor of MDI technique (OR for better MDI technique, 0.29; 95% CI, 0.08–1.00; p =0.05). When asthma medication knowledge was included as a covariate, inadequate health literacy was no longer a significant predictor of MDI technique (OR for better MDI technique, 0.53; 95% CI, 0.14–2.01), and asthma medication knowledge became the sole independent predictor of MDI technique (OR for better MDI technique, 1.48; 95% CI, 1.08–2.03).
After a single round of education, 59% (10/16) of subjects with inadequate health literacy and 73% (41/57) of subjects with higher health literacy exhibited mastery of MDI technique (p =0.26). Overall, 21% (15) of subjects required one additional round of education, 10% (7) required two additional rounds of education, and no subject needed more than two additional rounds of education to exhibit mastery of MDI technique. Inadequate health literacy was not associated with the number of rounds of education needed to exhibit master of MDI technique (p =0.79).
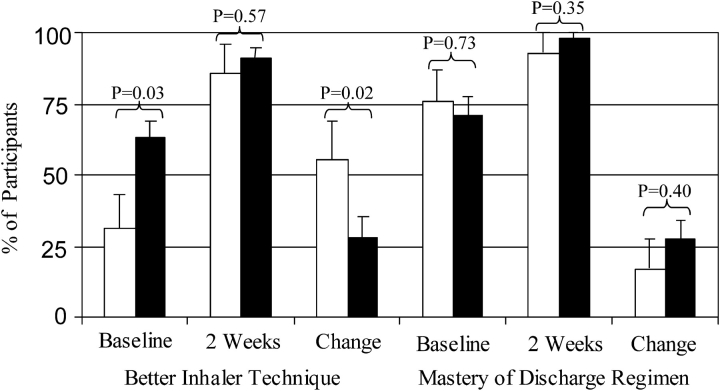
At the follow-up visit, the overall mean MDI technique score was 4.8 (SE =0.14), which was significantly improved from the discharge study visit measurement (change =1.1 [SE =0.21], p < 0.001). There was a greater increase in the proportion of subjects achieving better MDI technique in patients with inadequate health literacy (p =0.02; Figure 2), suggesting that this subgroup benefited most from the tailored education. At 2 wk, the proportion of participants with better MDI technique was no longer associated with health literacy (p =0.57).
Figure 2.
Better MDI technique score (% with ⩾ 4/6 correctly done) and mastery of discharge medication regimen (% exhibiting 4/4 questions correctly answered for all three medications in the standardized regimen) by literacy category at discharge study visit and at 2 wk. Inadequate health literacy: white bars =yes; black bars =no.
Understanding of Discharge Regimen
After a single round of education, 69% (11/16) of subjects with inadequate health literacy and 68% (39/57) of subjects with higher health literacy were able to exhibit mastery of the discharge regimen. The need for supplemental education to exhibit mastery of the discharge regimen at the discharge study visit was not associated with health literacy in bivariate and multivariable analyses (p =0.73 and p =0.33, respectively). Overall, 17 (25%) subjects required one additional round of education, one subject required two additional rounds of education, one subject required three additional rounds of education, and no subject required more than three additional rounds of education to exhibit mastery of the discharge regimen. At the follow-up visit, the proportion of patients having mastery of the discharge regimen was also similar between groups based on health literacy (p =0.35; Figure 2).
Adherence
Data on adherence to corticosteroid therapy and asthma symptom control were available in a substudy of 46 participants (63% of participants for the current study). About half (22/46, 48%) of the patients had poor adherence to corticosteroid therapy. Inadequate health literacy was not associated with poor adherence to corticosteroid therapy (OR, 0.89; 95% CI, 0.2–3.3; p =0.86). In multivariable analyses, health literacy was not associated with adherence to corticosteroid therapy, whether (p =0.45) or not (p =0.45) the model included asthma medication knowledge.
Asthma Symptom Control
At the follow-up visit, asthma symptom control was similar in patients with and without inadequate health literacy (mean [95% CI]: 1.6 [0.95–2.31] vs. 1.5 [1.22–1.75]; p =0.69). In multivariable analyses, inadequate health literacy was not associated with asthma symptom control at the follow-up visit (p =0.84).
DISCUSSION
Deficiencies in asthma medication knowledge, MDI technique, and mastery of the discharge regimen were common in inner-city adults hospitalized for asthma exacerbations. Observed deficiencies in asthma self-management skills could not be explained by sociodemographic characteristics (age, sex, ethnicity, and education) or past asthma-related health care use but were independently associated with inadequate health literacy. Inadequate health literacy was associated with a greater likelihood of hospitalization for asthma exacerbations in the past 12 mo and significantly less knowledge of asthma medication and improper MDI technique. Patients with inadequate health literacy also were more likely to have lower asthma medication knowledge scores and improper MDI technique before the educational intervention. Surprisingly, inadequate health literacy was not associated with difficulty learning or retaining instructions about discharge regimen and proper MDI technique.
The link between inadequate health literacy and less knowledge of asthma medication and improper MDI technique reported here is consistent with prior reports (14, 15). A few studies in other disease models present evidence related to the role of health literacy in learning and retaining self-management skills in patients with other chronic diseases. For example, simplified materials have been shown to improve knowledge (38–44), health care use (45), and health behaviors (46, 47) for patients with diabetes mellitus, rheumatoid arthritis, obesity, and hypertension, irrespective of health literacy. In addition, subjects with low health literacy have been able to learn and retain self-management skills in small studies of heart failure, obesity, and osteoarthritis (48–50).
Results of our study, however, are the first to provide data in asthma and indicate that interventions using tailored education can successfully overcome barriers related to inadequate health literacy and improve asthma self-management skills. These observations are reasons for patients, clinicians, and policymakers to be optimistic about the benefits of providing tailored education to vulnerable patient populations. Additional studies, however, are needed to determine whether these short-term gains in self-management are retained at subsequent points in time or whether “refresher” courses are necessary. Sustained success with asthma self-management may, for example, be related to specific health beliefs, which may be related to health literacy (51, 52). Also, future research should include interventions focused on other guideline-recommended self-management skills (e.g., allergen avoidance and other triggers), which are critical to maintaining effective asthma control.
We provided intensive asthma medication education at hospital discharge, which included both oral and written instructions during a one-on-one training session until mastery was achieved (“teach to goal” strategy). Although this study cannot clarify which aspects of the education were critical to ensure learning and retention (combined use of oral and written instruction, one-on-one personalized training, teach-to-goal until mastery was achieved, exhibiting appropriate MDI technique), we speculate that the physical exhibition of MDI technique by study personnel and structured assessment of participants' understanding served to reinforce what was learned and overcome the barrier of inadequate health literacy (30). Because resources needed for this type of intensive inpatient education may not be routinely available, additional research is needed to identify key components of our multimodality intervention.
It is important to underscore the high prevalence of poor MDI technique and poor understanding of the discharge regimen we observed. Despite our intensive program to improve patients' self-management skills provided in this study, fully 28% did not understand the discharge regimen and 30% had not mastered the MDI technique after one full round of education. These observations suggest that dramatic gains from the use of effective therapies in asthma are not reaching this high-risk population and highlight the need for evaluating patients' comprehension when providing discharge instructions and the development of systematic approaches to tailored inpatient asthma education.
Asthma self-management skills and use of acute medical services for asthma have been linked to various sociodemographic factors (18, 19, 53–56). In particular, fewer years of education completed has been implicated as an important risk factor in patients with asthma for cigarette smoking, worse MDI technique, and higher rates of emergency room visits, hospitalization, and mortality (19, 53–58). In this study, patients' level of education was not an independent predictor of asthma medication knowledge, MDI technique, or understanding of the discharge regimen. Instead, we found that health literacy was predictive of asthma medication knowledge and MDI technique. Moreover, our findings indicate that asthma medication knowledge plays a role in the causal pathway linking inadequate health literacy to poor MDI technique.
The prospective study design, uniform medication regimen after hospital discharge, and standardized education before discharge provided the unique opportunity to determine whether inadequate literacy served as a barrier to learning and retaining asthma self-management skills. Nonetheless, several potential limitations should be kept in mind. Although rates of follow-up were high (77%), bias may have been introduced due to incomplete follow-up, because not returning to the 2-wk follow-up visit was associated with age, race, and asthma medication knowledge. Also, without a control group, we cannot definitively conclude that our educational intervention was responsible for all the gains in asthma self-management that were noted. For example, it is possible but not certain that the lack of association we report between literacy and adherence was due to our educational intervention. Our data do, however, provide estimates of effect sizes that can be used to develop more definitive studies in this area (e.g., randomized clinical trial with an attention control group). Although interviewer bias is unlikely due to several safeguards put in place in our protocol, it is difficult to exclude completely the possibility that knowledge of health literacy status of participants influenced the teaching or assessment of self-management. Also, although we deliberately targeted an inner-city predominantly African-American population, a group at highest risk of complications resulting from asthma exacerbations, further research is needed to determine whether our findings are generalizable to other vulnerable patient populations (e.g., elderly with asthma).
Prior hospitalization strongly predicts risks of reexacerbations and death in the subsequent 12 mo (59–60). These poor outcomes are particularly common among African-American and inner-city patients for whom both hospitalizations and deaths related to asthma exacerbations are two to three times more likely than in other patient populations (64–66). These observations have led to a variety of inpatient programs to improve patients' self-management after hospital discharge (67, 68). The current study demonstrates that inpatient programs that embrace an intensive education program similar to ours are likely to overcome disparities in asthma self-management skills associated with inadequate health literacy.
In conclusion, this study presents evidence that inadequate asthma self-management skills are common and that inadequate health literacy is associated with worse asthma medication knowledge and MDI technique. However, inadequate health literacy was not associated with difficulty learning or retaining instructions about discharge regimen and proper MDI technique. Our results suggest the need for a systematic assessment of patient comprehension of discharge instructions and medications at hospital discharge. In patients with deficiencies in asthma self-management, we recommended a tailored, teach-to-goal, asthma education program.
Supplementary Material
Supported by the Parker B. Francis Fellowship Award and the National Institutes of Health (HL67850, HL063333).
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Conflict of Interest Statement: None of the authors have a financial relationship with a commercial entity that has an interest in the subject matter of this manuscript.
References
- 1.Adams K, Corrigan JM. Institute of Medicine. Priority areas for national action: transforming health care quality. Committee on Identifying Priority Areas for Quality Improvement. Washington, DC: National Academies Press; 2003. [PubMed]
- 2.Carmona RH. Surgeon General of the United States: health literacy in America: the role of health care professionals. Prepared remarks given at the American Medical Association House of Delegates Meeting, June 14th, 2003. Available from: http://www.surgeongeneral.gov/news/speeches/ama061403.htm (accessed February 19, 2004).
- 3.Ratzan SC, Parker RM. Introduction. In: Selden CR, Zorn M, Ratzan SC, Parker RM, editors. National Library of Medicine current bibliographies in medicine: health literacy. Vol. NLM. Bethesda, MD: National Institutes of Health, U.S. Department of Health and Human Services; 2000. Publication No. CBM 2000-1. Available from: http://www.nlm.nih.gov/pubs/cbm/hliteracy.html (accessed January 15, 2004).
- 4.Nielsen-Bohlman LT, Panzer AM, Hamlin B, Kindig DA. Institute of Medicine. Health literacy: a prescription to end confusion. Committee on Health Literacy, Board on Neuroscience and Behavioral Health. Washington, DC: National Academies Press; 2004. [PubMed]
- 5.DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med 2004;19:1228–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med 2005;20:175–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weiss BD, Blanchard JS, McGee DL, Hart G, Warren B, Burgoon M, Smith KJ. Illiteracy among Medicaid recipients and its relationship to health care costs. J Health Care Poor Underserved 1994;5:99–111. [DOI] [PubMed] [Google Scholar]
- 8.Rudd RE, Moeykens BA, Colton TC. Health and literacy: a review of medical and public health literature. In: Comings J, Garners B, Smith C, editors. Health and literacy, 1st ed. Available from: http://www.hsph.harvard.edu/healthliteracy/litreview_final.pdf (accessed September 9, 2005).
- 9.Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, Ren J, Peel J. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. Am J Public Health 2002;92:1278–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gazmararian JA, Baker DW, Williams MV, Parker RM, Scott TL, Green DC, Fehrenbach SN, Ren J, Koplan JP. Health literacy among Medicare enrollees in a managed care organization. JAMA 1999;281:545–551. [DOI] [PubMed] [Google Scholar]
- 11.Kalichman SC, Rompa D. Functional health literacy is associated with health status and health-related knowledge in people living with HIV-AIDS. J Acquir Immune Defic Syndr 2000;25:337–344. [DOI] [PubMed] [Google Scholar]
- 12.Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB. Association of health literacy with diabetes outcomes. JAMA 2002;288:475–482. [DOI] [PubMed] [Google Scholar]
- 13.Mannino DM, Homa DM, Akinbami LJ, Moorman JE, Gwynn C, Redd SC. Surveillance for asthma: United States, 1980–1999. MMWR Surveill Summ 2002;51:1–13. [PubMed] [Google Scholar]
- 14.Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest 1998;114:1008–1015. [DOI] [PubMed] [Google Scholar]
- 15.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns 2003;51:267–275. [DOI] [PubMed] [Google Scholar]
- 16.Williams SG, Schmidt DK, Redd SC, Storms W. Key clinical activities for quality asthma care. Recommendations of the National Asthma Education and Prevention Program. MMWR Recomm Rep 2003;52:1–8. [PubMed] [Google Scholar]
- 17.Berkman ND, DeWalt DA, Pignone MP, Sheridan SL, Lohr KN, Lux L, Sutton SF, Swinson T, Bonito AJ. Literacy and health outcomes. Evidence Report/Technology Assessment No. 87 (prepared by RTI International–University of North Carolina Evidence-based Practice Center under Contract No. 290-02-0016). January. Rockville, MD: Agency for Healthcare Research and Quality; 2004. AHRQ Publication No. 04-E007-2.
- 18.Boudreaux ED, Emond SD, Clark S, Camargo CA Jr. Acute asthma among adults presenting to the emergency department: the role of race/ethnicity and socioeconomic status. Chest 2003;124:803–812. [DOI] [PubMed] [Google Scholar]
- 19.Grant EN, Lyttle CS, Weiss KB. The relation of socioeconomic factors and racial/ethnic differences in US asthma mortality. Am J Public Health 2000;90:1923–1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirsch I, Jungeblut A, Jenkins L, Kolstad A. Adult literacy in America: a first look at the findings of the national adult literacy survey. Washington, DC: National Center for Education Statistics, U.S. Department of Education; 1993.
- 21.Krishnan JA, Riekert KA, McCoy JV, Stewart DY, Schmidt S, Chanmugam A, Hill P, Rand CS. Corticosteroid use after hospital discharge among high-risk adults with asthma. Am J Respir Crit Care Med 2004;170:1281–1285. [DOI] [PubMed] [Google Scholar]
- 22.Paasche-Orlow MK, Brancati FL, Rand CS, Krishnan JA. Education of patients with asthma and low literacy. J Gen Intern Med 2003;18(Suppl):S227. [Google Scholar]
- 23.Nurss JR, Parker RM, Williams MV, Baker DW. Test of functional literacy in adults, 2nd ed. Snow Camp, NC: Peppercorn Books and Press; 2001.
- 24.Nurss JR, Parker RM, Williams MV, Baker DW. Test of functional literacy in adults. Greensboro, NC: Peppercorn Books and Press; 1995. Available from: http://www.peppercornbooks.com/test_of_functional_health_literacy_in_adults.asp (accessed February 24, 2004).
- 25.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns 1999;38:33–42. [DOI] [PubMed] [Google Scholar]
- 26.Ho J, Bender BG, Gavin LA, O'Connor SL, Wamboldt MZ, Wamboldt FS. Relations among asthma knowledge, treatment adherence, and outcome. J Allergy Clin Immunol 2003;111:498–502. [DOI] [PubMed] [Google Scholar]
- 27.Barry PW, O'Callaghan C. Inhalational drug delivery from seven different spacer devices. Thorax 1996;51:835–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee H, Evans HE. Evaluation of inhalation aids of metered dose inhalers in asthmatic children. Chest 1987;91:366–369. [DOI] [PubMed] [Google Scholar]
- 29.Interiano B, Guntupalli KK. Metered-dose inhalers: do health care providers know what to teach? Arch Intern Med 1993;153:81–85. [DOI] [PubMed] [Google Scholar]
- 30.Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, Leong-Grotz K, Castro C, Bindman AB. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med 2003;163:83–90. [DOI] [PubMed] [Google Scholar]
- 31.Juniper EF, O'Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. Eur Respir J 1999;14:902–907. [DOI] [PubMed] [Google Scholar]
- 32.Julius SM, Sherman JM, Hendeles L. Accuracy of three electronic monitors for metered-dose inhalers. Chest 2002;121:871–876. [DOI] [PubMed] [Google Scholar]
- 33.Simmons MS, Nides MA, Kleerup EC, Chapman KR, Milgrom H, Rand CS, Spector SL, Tashkin DP. Validation of the Doser, a new device for monitoring metered-dose inhaler use. J Allergy Clin Immunol 1998;102:409–413. [DOI] [PubMed] [Google Scholar]
- 34.George CF, Peveler RC, Heiliger S, Thompson C. Compliance with tricyclic antidepressants: the value of four different methods of assessment. Br J Clin Pharmacol 2000;50:166–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu H, Golin CE, Miller LG, Hays RD, Beck CK, Sanandaji S, Christian J, Maldonado T, Duran D, Kaplan AH, et al. A comparison study of multiple measures of adherence to HIV protease inhibitors. Ann Intern Med 2001;134:968–977. [DOI] [PubMed] [Google Scholar]
- 36.Cramer JA, Mattson RH, Prevey ML, Scheyer RD, Ouellette VL. How often is medication taken as prescribed? A novel assessment technique. JAMA 1989;261:3273–3277. [PubMed] [Google Scholar]
- 37.Harrell FE Jr, Lee KL, Matchar DB, Reichert TA. Regression models for prognostic prediction: advantages, problems, and suggested solutions. Cancer Treat Rep 1985;69:1071–1077. [PubMed] [Google Scholar]
- 38.Eaton ML, Holloway RL. Patient comprehension of written drug information. Am J Hosp Pharm 1980;37:240–243. [PubMed] [Google Scholar]
- 39.Meade CD, Byrd JC, Lee M. Improving patient comprehension of literature on smoking. Am J Public Health 1989;79:1411–1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Meade CD, McKinney WP, Barnas GP. Educating patients with limited literacy skills: the effectiveness of printed and videotaped materials about colon cancer. Am J Public Health 1994;84:119–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Michielutte R, Bahnson J, Dignan MB, Schroeder EM. The use of illustrations and narrative text style to improve readability of a health education brochure. J Cancer Educ 1992;7:251–260. [DOI] [PubMed] [Google Scholar]
- 42.Murphy PW, Chesson AL, Walker L, Arnold CL, Chesson LM. Comparing the effectiveness of video and written material for improving knowledge among sleep disorders clinic patients with limited literacy skills. South Med J 2000;93:297–304. [PubMed] [Google Scholar]
- 43.Wydra EW. The effectiveness of a self-care management interactive multimedia module. Oncol Nurs Forum 2001;28:1399–1407. [PubMed] [Google Scholar]
- 44.Hayes KS. Randomized trial of geragogy-based medication instruction in the emergency department. Nurs Res 1998;47:211–218. [DOI] [PubMed] [Google Scholar]
- 45.Davis TC, Berkel HJ, Arnold CL, Nandy I, Jackson RH, Murphy PW. Intervention to increase mammography utilization in a public hospital. J Gen Intern Med 1998;13:230–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Howard-Pitney B, Winkleby MA, Albright CL, Bruce B, Fortmann SP. The Stanford Nutrition Action Program: a dietary fat intervention for low-literacy adults. Am J Public Health 1997;87:1971–1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hartman TJ, McCarthy PR, Park RJ, Schuster E, Kushi LH. Results of a community-based low-literacy nutrition education program. J Community Health 1997;22:325–341. [DOI] [PubMed] [Google Scholar]
- 48.DeWalt DA, Pignone M, Malone RM, Bryant B, Felix K, Corr K, Kosnar MC, Rawls C, Rogers N, Rothman R, et al. Randomized controlled trial of a primary care-based heart failure disease management program for patients with low literacy. J Gen Intern Med 2004;19(Suppl):S203. [Google Scholar]
- 49.Gans KM, Lovell HJ, Fortunet R, Lasater TM. Low-literacy audio intervention for lowering fat intake. J Nutr Educ 1998;30:410B–410B1. [Google Scholar]
- 50.Bill-Harvey D, Rippey R, Abeles M, Donald MJ, Downing D, Ingenito F, Pfeiffer CA. Outcome of an osteoarthritis education program for low-literacy patients taught by indigenous instructors. Patient Educ Couns 1989;13:133–142. [DOI] [PubMed] [Google Scholar]
- 51.Bhat BR, Friedman S, Adimoolam S, Schneider AT, Chiaramonte LT. Study of social, educational, environmental and cultural aspects of childhood asthma in clinic and private patients in the city of New York. Ann Allergy 1978;41:89–92. [PubMed] [Google Scholar]
- 52.George M, Freedman TG, Norfleet AL, Feldman HI, Apter AJ. Qualitative research-enhanced understanding of patients' beliefs: results of focus groups with low-income, urban, African American adults with asthma. J Allergy Clin Immunol 2003;111:967–973. [DOI] [PubMed] [Google Scholar]
- 53.Huovinen E, Kaprio J, Laitinen LA, Koskenvuo M. Social predictors of adult asthma: a co-twin case-control study. Thorax 2001;56:234–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Adams RJ, Smith BJ, Ruffin RE. Factors associated with hospital admissions and repeat emergency department visits for adults with asthma. Thorax 2000;55:566–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Radeos MS, Leak LV, Lugo BP, Hanrahan JP, Clark S, Camargo CA Jr. Risk factors for lack of asthma self-management knowledge among ED patients not on inhaled steroids. Am J Emerg Med 2001;19:253–259. [DOI] [PubMed] [Google Scholar]
- 56.Diette GB, Krishnan JA, Dominici F, Haponik E, Skinner EA, Steinwachs D, Wu AW. Asthma in older patients: factors associated with hospitalization. Arch Intern Med 2002;162:1123–1132. [DOI] [PubMed] [Google Scholar]
- 57.Silverman RA, Boudreaux ED, Woodruff PG, Clark S, Camargo CA Jr. Cigarette smoking among asthmatic adults presenting to 64 emergency departments. Chest 2003;123:1472–1479. [DOI] [PubMed] [Google Scholar]
- 58.Eisner MD, Yelin EH, Katz PP, Shiboski SC, Henke J, Blanc PD. Predictors of cigarette smoking and smoking cessation among adults with asthma. Am J Public Health 2000;90:1307–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Weiss KB, Sullivan SD, Lyttle CS. Trends in the cost of illness for asthma in the United States, 1985–1994. J Allergy Clin Immunol 2000;106:493–499. [DOI] [PubMed] [Google Scholar]
- 60.Flora GS, Sharma AM, Sharma OP. Asthma mortality in a metropolitan county hospital, a 38-year study. Allergy Proc 1991;12:169–179. [DOI] [PubMed] [Google Scholar]
- 61.Miller TP, Greenberger PA, Patterson R. The diagnosis of potentially fatal asthma in hospitalized adults: patient characteristics and increased severity of asthma. Chest 1992;102:515–518. [DOI] [PubMed] [Google Scholar]
- 62.Crane J, Pearce N, Burgess C, Woodman K, Robson B, Beasley R. Markers of risk of asthma death or readmission in the 12 months following a hospital admission for asthma. Int J Epidemiol 1992;21:737–744. [DOI] [PubMed] [Google Scholar]
- 63.McCarren M, McDermott MF, Zalenski RJ, Jovanovic B, Marder D, Murphy DG, Kampe LM, Misiewicz VM, Rydman RJ. Prediction of relapse within eight weeks after an acute asthma exacerbation in adults. J Clin Epidemiol 1998;51:107–118. [DOI] [PubMed] [Google Scholar]
- 64.Thomas SD, Whitman S. Asthma hospitalizations and mortality in Chicago: an epidemiologic overview. Chest 1999;116:135S–141S. [DOI] [PubMed] [Google Scholar]
- 65.Ray NF, Thamer M, Fadillioglu B, Gergen PJ. Race, income, urbanicity, and asthma hospitalization in California: a small area analysis. Chest 1998;113:1277–1284. [DOI] [PubMed] [Google Scholar]
- 66.De Palo VA, Mayo PH, Friedman P, Rosen MJ. Demographic influences on asthma hospital admission rates in New York City. Chest 1994;106:447–451. [DOI] [PubMed] [Google Scholar]
- 67.Evans R III, LeBailly S, Gordon KK, Sawyer A, Christoffel KK, Pearce B. Restructuring asthma care in a hospital setting to improve outcomes. Chest 1999;116:210S–216S. [DOI] [PubMed] [Google Scholar]
- 68.George MR, O'Dowd LC, Martin I, Lindell KO, Whitney F, Jones M, Ramondo T, Walsh L, Grissinger J, Hansen-Flaschen J, et al. A comprehensive educational program improves clinical outcome measures in inner-city patients with asthma. Arch Intern Med 1999;159:1710–1716. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.