Abstract
Rationale: Factors predicting the development of wheeze may differ between sexes and between childhood and adolescence. Methods: A New Zealand birth cohort of 1,037 children was followed to age 26. For this analysis, those reporting recurrent wheezing at two or more assessments were classified as “wheezers.” We examined risk factors for development of wheeze before age 10 (childhood) and subsequently (adolescent-onset) for males and for females separately using Cox regression modeling. Results: Males more often developed childhood wheeze (p = 0.002) and females adolescent-onset wheeze (p < 0.001). Maternal atopy (asthma or hay fever) was a risk factor for childhood wheeze in both sexes (hazard ratio [HR], 1.48, p < 0.05 for males; HR, 2.37, p < 0.001 for females). Paternal atopy also influenced childhood wheeze, significantly for males (HR, 1.72; p = 0.01), and similarly but not significantly for females (HR, 1.70; p = 0.08). For adolescent-onset wheeze, neither maternal (HR, 1.41; p = 0.19) nor paternal history (HR, 0.73; p = 0.42) was a risk factor in males, but maternal history (HR, 2.08; p < 0.01) was a significant risk factor for females. When both age ranges were combined, providing greater power for analysis, paternal history was a stronger risk factor for wheeze in females (HR, 1.62; p = 0.02) than in males (HR, 1.35; p = 0.12). Conclusion: The influence of parental atopy on the development for wheeze differs between males and females and between childhood- and adolescent-onset wheeze.
Keywords: age of onset, asthma, parental history, risk factors, sex
Studies of the epidemiology and natural history of childhood asthma demonstrate changing sex prevalence with age. Until age 12 to 13 years, the incidence of asthma is greater in males than in females (1–3). During adolescence, the incidence of asthma increases in females such that, by age 20, the dominance of males with asthma is reversed (1, 4–6). A higher prevalence of asthma in females persists throughout adult life.
Risk factors for the development of asthma in childhood include the following: atopy, a family history of asthma or hay fever, and airway hyperresponsiveness. Studies of the natural history of asthma consistently find that female sex, atopy, and airway hyperresponsiveness are associated with the persistence of asthma from childhood to adulthood (2, 7–21). However, studies are conflicting regarding risk factors for predicting new asthma or wheeze during adolescence. One recent German study reported that atopy was not a risk factor for incidence of asthma in females during puberty (22), whereas an Australian longitudinal cohort study showed that, in addition to family history of asthma, atopy was a risk factor for the development of adolescent wheeze (23).
Population-based studies of asthma may include subgroups with different risk factors for asthma. If these different subgroups are not separated, the strength of a risk factor for asthma will be averaged across the different groups in both univariate and multiple variable analyses. Only those risk factors that are strong in one or a few subpopulations or moderate in most or all subpopulations will be identified. Examples of subpopulations in asthma include males and females, and those with and without a family history of asthma or atopic disease. By examining these subpopulations, the underlying mechanisms of disease may be better understood.
We have analyzed data from a longitudinal study of a New Zealand population-based birth cohort study followed to adulthood to examine factors associated with development of asthma or wheeze during childhood and during adolescence in male and female subpopulations. We have previously reported that, although there were no significant sex differences in the prevalence of recurrent wheeze by age 13, males were more likely to have been diagnosed with asthma than females (24). This finding is confirmed by several other studies (25–27). To eliminate gender bias in the diagnosis of asthma, we have used either recurrent wheeze or asthma as the outcome variable.
METHODS
Participants in the Dunedin Multidisciplinary Health and Development Research Study (7, 21, 24, 28–34) were born April 1972 through March 1973. A population-representative birth cohort of 1,037 children was assessed at age 3. Follow-up assessments occurred at ages 5, 7, 9, 11, 13, 15, 18, 21, and 26 years. The Otago Hospital Research Ethics Committee approved each assessment. Written, informed consent was obtained at each visit from the guardian or participant.
Comprehensive respiratory questionnaires were completed at all visits from age 9 (7, 29). Parental asthma or hay fever was recorded at the age 7 (30) and 18 visit. Breastfeeding was recorded at age 3 and validated from prospective records (31, 35, 36). Ownership of cats and dogs was recorded at each age (29), and smoking history from age 15 onward (7).
Spirometry was performed at each assessment from 9 to 26 years (7, 32). Methacholine challenge was performed by all consenting study members at ages 9, 11, 13, 15, and 21 using a validated abbreviated protocol (32). Allergen skin testing was performed at age 13 and 21 (33). Detailed methods are described in previous publications (7, 21, 28–34, 36) and in the online supplement.
We included all study members seen at least once between ages 7 and 26 and whose age of first wheezing (if wheezing occurred) could be determined (n = 1,022).
Statistical Analysis
For this analysis, children with recurrent wheezing reported at two or more assessments were classified as “wheezers.” The youngest age at which wheezing was reported was used as the age of onset. The oldest age at which nonwheezers were seen was when data were censored. Males and females were analyzed separately. Analyses were repeated defining wheezers as those with recurrent wheezing at three or more assessments, and those who had persistent or relapsing symptoms, as previously described (7).
Kaplan-Meier analysis log-rank test was used with univariate analysis. For continuous variables, and to calculate univariate hazard ratios, Cox regression modeling was used; the proportional hazard assumption was tested using log minus log plots and by modeling a “time × factor” interaction term.
We examined factors associated with onset of wheeze during childhood (to age 10) and adolescence (after age 10). To examine risk factors for adolescent-onset wheeze, individuals who developed wheeze before age 10 were excluded from the analysis. Age-dependent risk was noted if hazard ratios for childhood- and adolescent-onset wheeze differed significantly. To isolate the independent influence of maternal and paternal history on the development of wheeze, individuals with only a maternal or only a paternal history were identified and compared with study members where neither parent had a history of asthma or hay fever. Multiple variable analyses by Cox regression used a backward likelihood ratio (p ⩽ 0.05 in, p> 0.1 out). All multiple regression analyses for adolescent-onset wheeze were corrected for smoking at age 15. A secondary analysis identified factors associated with the development of wheeze at any age to last follow-up at age 26. Statistical analysis was completed using SPSS, version 12 (SPSS, Inc., Chicago, IL).
RESULTS
Sample Characteristics
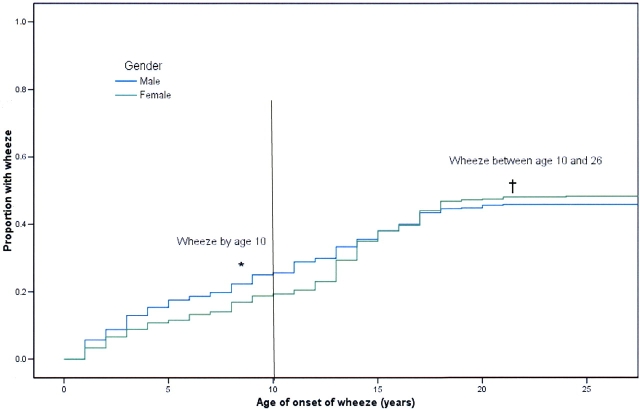
Of the 1,022 study members included in this analysis, 474 were classified as wheezers (reported at two or more assessments) by age 26, of which 50.1% were males. Of the 220 study members with onset of wheeze between ages 10 and 26, 210 (95.5%) developed symptoms between 10 and 18 years. Among males who developed wheeze by age 26, 63% did so before age 10 (p = 0.002 compared with females), whereas females were more likely to develop wheeze between ages 10 and 26 (p < 0.001; Figure 1).
Figure 1.
Proportion of males and females who develop wheeze by age 26, by age of onset. *Males, compared with females, are more likely to develop wheeze before age 10, p = 0.002; †females, compared with males, are more likely to develop wheeze after age 10, p < 0.001.
Compared with nonwheezers, both males and females who developed wheeze by age 26 had a lower FEV1/FVC ratio at all ages tested, were more likely to be atopic at age 13 and 21, to have a positive methacholine challenge at age 9, to have a maternal history of atopy, to be ever diagnosed with asthma, and to smoke at age 15 (Table 1). Differences between wheezers and nonwheezers for breastfeeding, having pets before age 9, being first-born, and smoke exposure as a child were not significant in this analysis (Table 1).
TABLE 1.
Sample characteristics of male and female study members reporting recurrent wheezing at two or more assessments by age 26
| Males
|
Females
|
|||
|---|---|---|---|---|
| Wheezers by Age 26* (n = 238) |
Nonwheezer by Age 26 (n = 297) |
Wheezers by Age 26* (n = 236) |
Nonwheezer by Age 26 (n = 266) |
|
| Age of onset of wheeze by age 10 | 151 (63%) | N/A | 102 (43%) | N/A |
| FEV1/FVC at age 26, % | 79.2† | 81.7 | 82.7† | 85.4 |
| SD, 8.1 | SD, 5.9 | SD, 6.5 | SD, 5.4 | |
| BMI at age 26, kg/m2 | 25.5 | 24.8 | 25.7† | 24.3 |
| SD, 3.9 | SD, 3.8 | SD, 5.7 | SD, 4.0 | |
| Atopic at 13 | 123/187† | 68/182 | 78/170† | 50/175 |
| 65.8% | 37.4% | 45.9% | 28.6% | |
| Positive methacholine at 9 years (PC20 ⩽ 8 mg/ml) | 49/185† | 13/216 | 46/182† | 3/185 |
| 26.5% | 6.0% | 25.3% | 1.6% | |
| Any maternal history of atopy (asthma or hay fever) | 80/227† | 67/266 | 92/221† | 47/235 |
| 35.2% | 25.2% | 41.6% | 20.0% | |
| Any paternal history of atopy (asthma or hay fever) | 57/224 | 53/259 | 60/218† | 41/232 |
| 25.5% | 20.5% | 27.5% | 17.7% | |
| Diagnosis of asthma ever | 126/237† | 19/288 | 121/236† | 20/261 |
| 53.2% | 6.6% | 51.3% | 7.7% | |
| Smoker at 15 yr | 40/232† | 23/260 | 61/229† | 36/241 |
| 17.2% | 8.9% | 26.6% | 14.9% | |
| Breastfed ⩾ 4 wk | 122/237 | 129/288 | 118/236 | 129/261 |
| 51.5% | 44.8% | 50.0% | 49.4% | |
| Tobacco smoke exposure as a child | 146/215 | 141/234 | 137/215 | 126/204 |
| 67.9% | 60.3% | 63.7% | 61.8% | |
| Dog ownership before age 9 | 109/206 | 109/221 | 80/194† | 108/193 |
| 52.9% | 49.3% | 41.2% | 56.0% | |
| Cat ownership before age 9 | 160/206 | 176/221 | 154/194 | 149/193 |
| 77.7% | 79.6% | 79.4% | 77.2% | |
| First-born | 76/215 | 86/234 | 74/215 | 86/204 |
| 35.4% | 36.8% | 34.4% | 42.2% | |
Definition of abbreviation: BMI = body mass index; NA = not applicable.
Except where otherwise indicated, figures are number with characteristic/number assessed.
Defined as recurrent wheezing reported at two or more surveys.
p < 0.05 comparing wheezers to nonwheezers.
Females who developed wheeze at any age to 26 had a higher body mass index from age 9 onward and were more likely to have a paternal history of atopy, but were less likely to have owned a dog before age 9.
Univariate Analysis
Results using wheezing defined by reported symptoms at two or more assessments or three or more assessments, or adolescent-onset wheeze defined only between ages 10 and 18, or those with persistent or relapsing systems were consistent. Results using wheeze defined by symptoms at two or more assessments are presented. Unadjusted hazard ratios (HR) for childhood-onset wheeze (Table 2), adolescent-onset wheeze (Table 3), and wheeze at any age to 26 (Table 4) are presented. None of the variables violated the proportional hazards assumption. Several variables demonstrated an age-dependent risk.
TABLE 2.
Univariate analyses for factors associated with development of childhood-onset wheeze (recurrent wheeze, onset before age 10, reported at two or more assessments)
| Males
|
Females
|
|||||
|---|---|---|---|---|---|---|
| Risk Factor | p Value | HR | 95% CI | p Value | HR | 95% CI |
| Any family history | 0.003 | 1.61 | 1.17–2.23 | < 0.001 | 2.22 | 1.48–3.33 |
| Maternal history only | 0.055 | 1.48 | 0.99–2.22 | < 0.001 | 2.37 | 1.48–3.81 |
| Paternal history only | 0.014 | 1.72 | 1.11–2.68 | 0.08 | 1.70 | 0.92–3.14 |
| Breastfed ⩾ 4 wk | 0.07 | 1.34 | 0.97–1.85 | 0.021 | 1.58 | 1.06–2.35 |
| Owned a dog before age 9 | 0.99 | 1.00 | 0.72–1.39 | 0.15 | 0.74 | 0.48–1.12 |
| Owned a cat before age 9 | 0.79 | 0.95 | 0.64–1.41 | 0.96 | 0.99 | 0.60–1.63 |
| Had childhood tobacco smoke exposure | 0.55 | 1.11 | 0.78–1.58 | 0.92 | 1.02 | 0.67–1.56 |
| FEV1/FVC at 9 yr (HR is per 1 unit FEV1/FVC) | < 0.001 | 0.93 | 0.91–0.95 | < 0.001 | 0.91 | 0.88–0.93 |
| Positive methacholine at age 9 | < 0.001 | 4.20 | 2.88–6.12 | < 0.001 | 6.48 | 4.14–10.14 |
| BMI at age 9 (HR is per unit BMI) | 0.150 | 1.08 | 0.97–1.19 | 0.50 | 1.04 | 0.93–1.16 |
| Atopy at 13 yr | < 0.0001 | 2.89 | 1.97–4.25 | < 0.001 | 2.62 | 1.68–4.09 |
Definition of abbreviations: BMI = body mass index; CI = confidence interval; HR = hazard ratio.
TABLE 3.
Univariate analyses for factors associated with adolescent-onset wheeze (recurrent wheeze, onset after age 10, on two or more assessments)
| Males
|
Females
|
|||||
|---|---|---|---|---|---|---|
| Risk Factor | p Value | HR | 95% CI | p Value | HR | 95% CI |
| Any family history | 0.46 | 1.18 | 0.76–1.83 | < 0.001 | 2.00 | 1.41–2.83 |
| Maternal history only | 0.19 | 1.41 | 0.83–2.40 | < 0.001 | 2.08 | 1.34–3.22 |
| Paternal history only | 0.42 | 0.73 | 0.33–1.61 | 0.10 | 1.57 | 0.92–2.66 |
| Breastfed ⩾ 4 wk | 0.73 | 1.08 | 0.71–1.65 | 0.20 | 0.81 | 0.57–1.13 |
| Owned a dog before age 9 | 0.24 | 1.34 | 0.82–2.20 | 0.021 | 0.64 | 0.44–0.95 |
| Owned a cat before age 9 | 0.79 | 0.92 | 0.51–1.67 | 0.43 | 1.22 | 0.75–1.98 |
| Had childhood tobacco smoke exposure | 0.07 | 1.55 | 0.95–2.55 | 0.63 | 1.09 | 0.75–1.58 |
| FEV1/FVC at 9 yr (HR is per 1 unit FEV1/FVC) | 0.19 | 0.97 | 0.93–1.02 | 0.053 | 0.97 | 0.93–1.00 |
| Positive methacholine at age 9 | 0.12 | 1.82 | 0.83–3.98 | < 0.001 | 4.07 | 2.21–7.48 |
| Change in BMI between age 9 and 11 (HR is per unit change in BMI) | 0.24 | 1.20 | 0.88–1.64 | 0.07 | 1.18 | 0.99–1.42 |
| Atopy at 13 yr | 0.041 | 1.69 | 1.01–2.82 | 0.31 | 1.24 | 0.80–1.92 |
| Smoked at 15 yr | < 0.001 | 2.57 | 1.56–4.22 | 0.005 | 1.71 | 1.16–2.53 |
For definition of abbreviations, see Table 2.
TABLE 4.
Univariate analyses for factors associated with development of wheeze at any age to 26 (wheeze on two or more assessments)
| Males
|
Females
|
|||||
|---|---|---|---|---|---|---|
| Risk Factor | p Value | HR | 95% CI | p Value | HR | 95% CI |
| Any family history | 0.005 | 1.44 | 1.11–1.87 | < 0.001 | 2.09 | 1.60–2.72 |
| Maternal history only | 0.019 | 1.46 | 1.06–2.01 | < 0.001 | 2.21 | 1.60–3.04 |
| Paternal history only | 0.12 | 1.35 | 0.92–1.97 | 0.016 | 1.62 | 1.09–2.42 |
| Breastfed ⩾ 4 wk | 0.10 | 1.24 | 0.96–1.60 | 0.57 | 1.08 | 0.83–1.39 |
| Owned a dog before age 9 | 0.51 | 1.10 | 0.83–1.44 | 0.008 | 0.69 | 0.51–0.91 |
| Owned a cat before age 9 | 0.71 | 0.94 | 0.68–1.31 | 0.58 | 1.10 | 0.78–1.56 |
| Had childhood tobacco smoke exposure | 0.12 | 1.25 | 0.94–1.67 | 0.67 | 1.06 | 0.80–1.40 |
| FEV1/FVC at 9 yr (HR is per 1 unit FEV1/FVC) | < 0.001 | 0.94 | 0.92–0.96 | < 0.001 | 0.93 | 0.91–0.95 |
| Positive methacholine at age 9 | < 0.001 | 3.45 | 2.48–4.81 | < 0.001 | 5.44 | 3.83–7.72 |
| BMI at age 26 (HR is per unit BMI) | 0.056 | 1.03 | 1.00–1.06 | 0.003 | 1.04 | 1.01–1.06 |
| Atopy at 13 yr | < 0.001 | 2.40 | 1.77–3.25 | < 0.001 | 1.78 | 1.32–2.41 |
| Smoked at 15 yr | 0.021 | 1.48 | 1.05–2.08 | < 0.001 | 1.64 | 1.22–2.19 |
For definition of abbreviations, see Table 2.
Development of childhood-onset wheeze (by age 10).
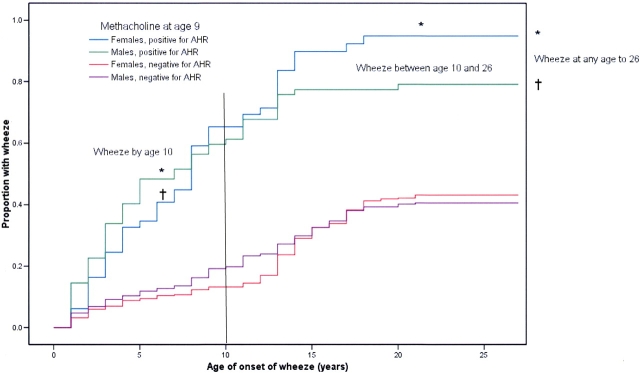
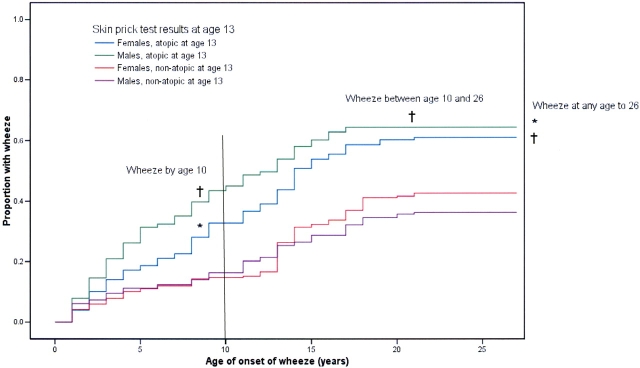
Both males and females who developed childhood-onset wheeze were more likely to have a positive methacholine challenge at age 9 (HR, 4.20 [2.88–6.12] for males; HR, 6.48 [4.14–10.14] for females; Figure 2), to be atopic at age 13 (HR, 2.89 [1.97–4.25] for males; HR, 2.62 [1.68–4.09] for females; Figure 3), and have a parental history of atopy (HR, 1.61 [1.17–2.23] for males; HR, 2.22 [1.48–3.33] for females). Males and females with childhood-onset wheeze had a lower FEV1/FVC ratio at all ages tested between 9 and 26 years compared with nonwheezers (p < 0.001; Table 2).
Figure 2.
Proportion of individuals with and without a positive methacholine challenge (PC20 ⩽ 8 mg/ml) at age 9 who develop wheeze by age 26, by age of onset. *Females positive for airway hyperresponsiveness (AHR) at age 9 are more likely to develop wheeze by age 10, between ages 10 and 26, and at any age to 26 versus those females without AHR, p < 0.001 for all analyses; †males positive for AHR at age 9 are more likely to develop wheeze by 10, and at any age to 26 versus those males without AHR, p < 0.001 for both analyses.
Figure 3.
Proportion of individuals with and without any positive skin-prick test (⩾ 2-mm wheal) at age 13 and the development of wheeze by age 26, by age of onset. *Females positive for any atopy at age 13 are more likely to develop wheeze by age 10, and at any age to 26 versus nonatopic females, p < 0.001; †males positive for any atopy at age 13 are more likely to develop wheeze by 10, between ages 10 and 26, and at any age to 26 versus nonatopic males, p < 0.001.
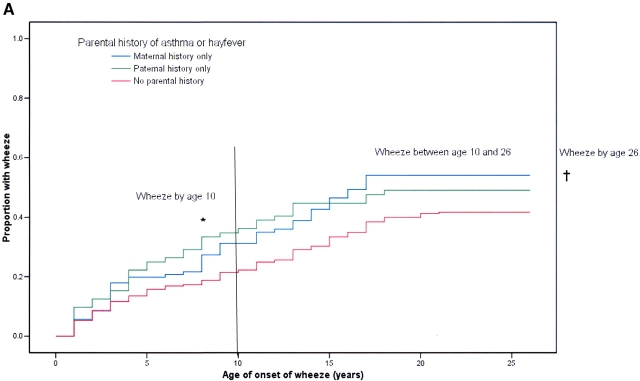
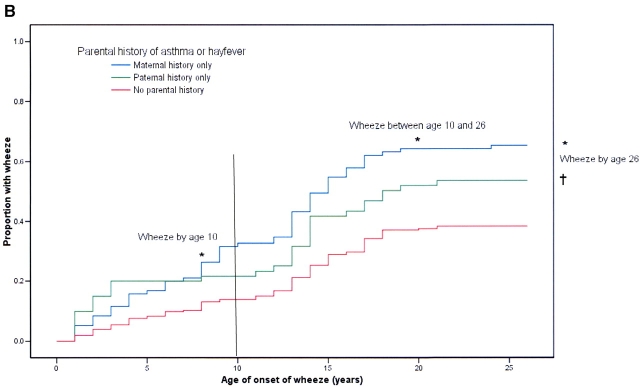
Males with only a paternal history were more likely to develop childhood wheeze (by age 10) than those with no parental history of atopy (HR, 1.72 [1.11–2.69]; Figure 4A). Because fewer females develop childhood wheeze, the same hazard ratio (HR, 1.70 [0.92–4.14]) for paternal history was not significant for females (p = 0.085; Figure 4B). However, although females with a maternal history were more likely to develop childhood wheeze (by age 10) than those with no parental history (HR, 2.37 [1.48–3.81]), the influence of maternal history for males was only borderline significant (HR, 1.48 [0.99–2.22]).
Figure 4.
(A) Proportion of males with parental history of asthma or hay fever who develop wheeze by age 26, by age of onset. *Males with only a paternal history of atopy are more likely to develop wheeze by 10 versus males with no parental history of atopy: p = 0.005; †males with only a maternal history of atopy are more likely to develop wheeze at any age to 26 versus males with no parental history of atopy, p = 0.005. (B) Proportion of females with parental history of asthma or hay fever who develop wheeze by age 26, by age of onset. *Females with only a maternal history of atopy are more likely to develop wheeze by age 10, between age 10 and 26, at any age to 26 versus females with no parental history of atopy, p < 0.0001; †females with only a paternal history of atopy are more likely to develop wheeze a any age to 26 versus females with no parental history of atopy, p = 0.015.
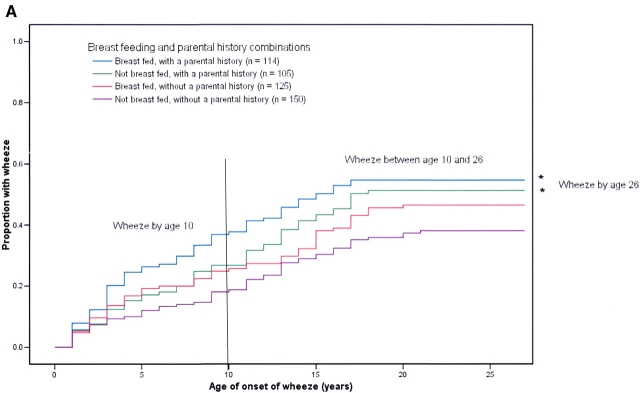
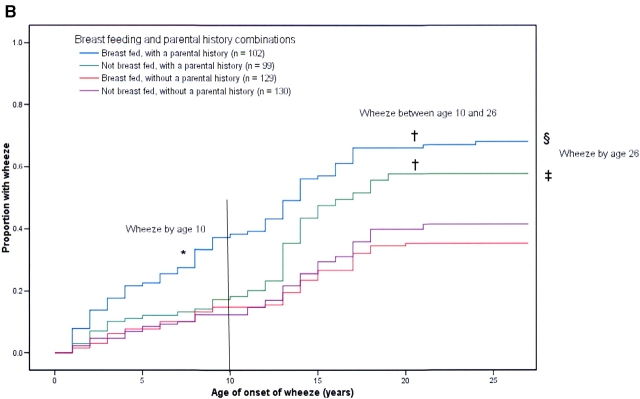
Females who were breastfed were more likely to develop childhood-onset wheeze, with a less strong trend seen in males (HR, 1.34 [0.97–1.85] for males; HR, 1.58 [1.06– 2.38] for females). When stratified by any parental history, the influence of breastfeeding was most strongly seen for childhood-onset wheeze in breastfed females with a parental history of atopy (HR, 1.44 [1.02–2.05]) versus breastfed females without a parental history (HR, 0.83 [0.56–1.24]). A similar trend was seen in males (Figure 5A, males; Figure 5B, females).
Figure 5.
(A) Proportion of males, with and without a family history of asthma or hay fever, stratified by breastfeeding status, who develop wheeze by age 26, by age of onset. *Males with a family history of atopy, regardless of breastfeeding status, are more likely to develop wheeze at any age to 26 versus males with no family history of atopy and who were not breastfed, p = 0.036. (B) Proportion of females, with and without a family history of asthma or hay fever, stratified by breastfeeding status, who develop wheeze by age 26, by age of onset. *Females with a family history of atopy, who were breastfed, are more likely to develop wheeze by age 10 versus females with no family history of atopy and who were not breastfed, p = 0.067; †females with a family history of atopy, regardless of breastfeeding status, were more likely to develop wheeze between ages 10 and 26 compared with females without a family history of atopy, p = 0.022; ‡females with a family history of atopy, who were not breastfed, were more likely to develop wheeze at any age to 26 versus females with no family history of atopy and who were not breastfed, p = 0.015; §females with a family history of atopy, who were breastfed, were more likely to develop wheeze at any age to 26 than all other groups, including females with a family history of atopy only, p = 0.042.
Development of adolescent-onset wheeze (after age 10 to age 26).
Smoking at age 15 was a risk factor for adolescent-onset wheeze for both males and females (HR, 2.57 [1.56–4.22] for males; HR, 1.71 [1.16–2.53] for females). All other risk factors for adolescent-onset wheeze were different between the sexes (Table 3).
In males, any atopy at age 13 (HR, 1.69 [1.01–2.28]) and maternal smoking during the third trimester of pregnancy were associated with adolescent-onset wheeze (HR, 1.79 [1.02–3.14]).
In females, maternal history (HR, 2.08 [1.34–3.22]) was a significant risk factor and paternal history was again borderline significant (HR, 1.57 [0.92–2.66]). A positive methacholine challenge at age 9 (HR, 4.07 [2.21–7.48]) was also a risk factor for adolescent-onset wheeze. Females with adolescent-onset wheeze also had a lower FEV1/FVC at age 9 (p = 0.053). Atopy was not a risk factor for adolescent-onset wheeze in females. Females whose families owned a dog before age 9 were less likely to develop wheeze at any age to 26, with the effect being most pronounced on the development of adolescent-onset wheeze (HR, 0.64 [0.44–0.95]). Change in body mass index between age 9 and 11 was a borderline significant risk factor for adolescent-onset wheeze in females (HR, 1.18 [0.99–1.42).
Development of wheeze at any age to 26.
To address the issue of reduced power resulting from subdivision of the sample into two age ranges, the relation of paternal history to wheeze at any age to 26 was examined (Table 4). Compared with study members with no family history of atopy, having only a paternal history was a risk factor for wheeze at any age to 26 for females (HR, 1.62 [1.09–2.42]) but was not a significant risk factor for males (HR, 1.35 [0.92–1.97]) across this broader age range, whereas maternal history was a predictor in both sexes.
Multiple Variable Analyses
Development of childhood-onset wheeze.
To identify the strongest factors associated with wheeze by age 10, factors entered into the Cox regression included the following: any parental history of atopy, any atopy at age 13, PC20 FEV1 less than or equal to 8 mg/ml at age 9, owning either a cat or dog before age 9, FEV1/FVC at age 9, maternal smoking during the third trimester, breastfeeding, birth order, maternal and paternal smoking during the childhood of the study member, and body mass index at all ages. If any parental history was found to be a factor associated with wheeze, to maintain the same reference population, both maternal-only and paternal-only history were substituted into the model. Model 1 included all variables listed. Because atopy, lung function, and airway hyperresponsiveness were measured near or after the end of the period, it is less certain whether these factors are a result of wheeze or a risk factor for wheeze. Model 2 therefore excluded these variables from the regression.
For males, any atopy at age 13 and airway hyperresponsiveness at age 9 were associated with childhood-onset wheeze (Table 5). When airway hyperresponsiveness was excluded from the regression, lung function at age 9, in addition to atopy, was associated with development of wheeze by age 10. For Model 2, only parental history was found to be a risk factor for childhood wheeze in males. When any parental history was replaced by maternal-only and paternal-only history, paternal history was the strongest predictor of childhood wheeze in males.
TABLE 5.
Multiple variable analysis examining factors associated with development of childhood-onset wheeze (between birth and age 10) in males
| 95% CI for the HR
|
||||
|---|---|---|---|---|
| Factor | Significance | HR | Lower | Upper |
| Model 1: all variables included | ||||
| Atopy at age 13 | 0.001 | 2.20 | 1.45 | 3.34 |
| Positive methacholine at 9 yr | 0.000 | 3.49 | 2.32 | 5.21 |
| Excluding airway hyperresponsiveness | ||||
| FEV1/FVC at 9 yr | < 0.001 | 0.94 | 0.91 | 0.96 |
| Atopy at age 13 | < 0.001 | 2.64 | 1.79 | 3.89 |
| Model 2: excluding airway hyperresponsiveness, atopy, and lung function | ||||
| Any family history of asthma or hay fever | 0.004 | 1.61 | 1.17 | 2.23 |
| Replacing family history with maternal and paternal history of atopy* | ||||
| Maternal history of asthma or hay fever | 0.05 | 1.49 | 0.99 | 2.22 |
| Paternal history of asthma or hay fever | 0.016 | 1.73 | 1.11 | 2.69 |
Definition of abbreviations: CI = confidence interval; HR = hazard ratio.
Maternal only and paternal only, compared with reference group with no family history.
For females, any atopy at age 13, airway hyperresponsiveness at age 9, and lung function at age 9 were also found to be associated with childhood-onset wheeze (Table 6). When airway responsiveness was excluded, atopy and lung function remained significant risk factors. For Model 2, the interaction of any parental history of asthma or hay fever with breastfeeding was a risk factor for childhood wheeze. When any parental history was replaced by maternal-only and paternal-only history, only the interaction of breastfeeding by maternal history was a risk factor for childhood wheeze.
TABLE 6.
Multiple variable analysis examining factors associated with development of childhood-onset wheeze (between birth and age 10) in females
| 95% CI for the HR
|
||||
|---|---|---|---|---|
| Factor | Significance | HR | Lower | Upper |
| Model 1: all variables included | ||||
| FEV1/FVC at 9 yr | 0.002 | 0.93 | 0.89 | 0.97 |
| Atopy at age 13 | 0.027 | 1.88 | 1.14 | 3.10 |
| Positive methacholine at 9 yr | 0.001 | 3.14 | 1.81 | 5.44 |
| Excluding airway hyperresponsiveness | ||||
| FEV1/FVC at 9 yr | < 0.001 | 0.92 | 0.89 | 0.95 |
| Atopy at 13 yr | 0.003 | 2.18 | 1.38 | 3.46 |
| Model 2: excluding airway hyperresponsiveness, atopy, and lung function | ||||
| Any parental history of asthma or hay fever | 0.27 | 1.42 | 0.76 | 2.66 |
| Breastfed ⩾ 4 wk | 0.98 | 1.01 | 0.53 | 1.91 |
| Breastfed × parental history interaction | 0.07 | 2.18 | 0.95 | 5.00 |
| Replacing family history with maternal and paternal history of atopy | ||||
| Maternal history of asthma or hay fever | 0.74 | 1.15 | 0.50 | 2.63 |
| Paternal history of asthma or hay fever | 0.96 | 0.97 | 0.33 | 2.87 |
| Breastfed ⩾ 4 wk | 1.00 | 1.00 | 0.53 | 1.89 |
| Breastfed × maternal history interaction | 0.025 | 3.22 | 1.16 | 8.99 |
| Breastfed × paternal history interaction | 0.18 | 2.49 | 0.66 | 9.36 |
For definition of abbreviations, see Table 5.
Development of adolescent-onset wheeze.
To identify risk factors associated with new wheeze after age 10, factors entered into the Cox regression included the following: any parental history of atopy, any atopy at age 13, PC20 FEV1 less than or equal to 8 mg/ml at age 9, owning a cat or dog before age 9, FEV1/FVC at age 9, maternal smoking during the third trimester, breastfeeding, birth order, maternal and paternal smoking during the childhood of the study member, and body mass index at age 9 and 11 for both males and females. If any parental history was found to be a factor associated with wheeze, to maintain the same reference population, both maternal-only and paternal-only history were substituted into the model. All multiple variable analyses are corrected for smoking at age 15.
For males, atopy at age 13 and maternal smoking in the third trimester of pregnancy were associated with adolescent-onset wheeze (Table 7). No difference was found when either variable was excluded from the regression. For females, airway hyperresponsiveness at age 9 was the strongest risk factor for adolescent-onset wheeze (Table 8). When airway hyperresponsiveness was excluded from the multiple variable regression, lung function at age 9 and any parental history of asthma or hay fever were then found to be risk factors for adolescent-onset wheeze. When any parental history was replaced by maternal-only and paternal-only history, both maternal history and lung function were associated with adolescent-onset wheeze in females.
TABLE 7.
Results for the multiple variable analysis examining factors associated with development of adolescent-onset wheeze (onset after age 10) in males
| 95% CI for the HR
|
||||
|---|---|---|---|---|
| Factor (all variables included) | Significance | HR | Lower | Upper |
| Maternal smoking during the third trimester |
0.006 | 2.26 | 1.27 | 4.02 |
| Atopy at 13 yr | 0.016 | 2.03 | 1.14 | 3.60 |
For definition of abbreviations, see Table 5.
TABLE 8.
Results for the multiple variable analysis examining factors associated with development of adolescent-onset wheeze (onset after age 10) in females
| 95% CI for the HR
|
||||
|---|---|---|---|---|
| Factor | Significance | HR | Lower | Upper |
| All variables included | ||||
| Positive methacholine at 9 yr | < 0.001 | 3.69 | 2.00 | 6.81 |
| Excluding airway hyperresponsiveness | ||||
| FEV1/FVC at 9 yr | 0.025 | 0.96 | 0.93 | 1.00 |
| Any parental history of asthma or hay fever |
0.006 | 1.75 | 1.18 | 2.50 |
| Replacing family history with maternal and paternal history of atopy |
||||
| Maternal history of asthma or hay fever |
0.009 | 1.89 | 1.17 | 3.06 |
| Paternal history of asthma or hay fever |
0.41 | 1.28 | 0.71 | 2.30 |
| FEV1/FVC at 9 yr | 0.022 | 0.96 | 0.92 | 0.99 |
For definition of abbreviations, see Table 5.
DISCUSSION
This analysis of data from a population-based birth cohort has identified significant differences between males and females for factors associated with childhood- and adolescent-onset wheeze. Atopy and airway hyperresponsiveness were associated with childhood wheeze in both sexes. However, although atopy continues to be a risk factor for developing wheeze through adolescence in males, atopy was not a risk factor for adolescent-onset wheeze in females.
The results from this study may clarify contradictory results from previous studies on the influence of atopy on the development of adolescent asthma. An Australian study has previously reported that atopy, defined by skin testing at age 8 through 10, was a risk factor for the development of wheeze in puberty (23). In contrast, a German study found that atopy at age 10 was not a risk factor for the development of adolescent asthma (22). Although the proportion of females included in the analysis is similar for both studies (55% females in the Australian study, 48.5% females in the German study; p> 0.05), the prevalence of atopy at baseline was significantly lower in the Australian study than in the German cohort and our cohort (22.3% in the Australian cohort, 45.6% in the German cohort, 44.7% in our cohort; p < 0.001). The lower prevalence of atopy in the Australian study may explain why atopy was a risk factor for adolescent-onset wheeze. Neither the Australian or German studies stratified their analysis to evaluate if atopy was a sex-specific risk for adolescent-onset wheeze. Our analysis found that atopy was a risk factor for adolescent-onset wheeze in males but not in females.
One of the limitations of our study is that several factors associated with childhood-onset wheeze, including atopy and airway responsiveness, were measured near or after age 10. As a result, this study cannot establish whether these factors are causally related. Further studies with more detailed and prospective measurements of childhood atopy and airway responsiveness are needed to understand the relationship between these variables and asthma. The first comprehensive history of childhood wheezing was obtained when the children were age 9 (29). Those study members with childhood-onset wheeze likely represent children with either persistent or relapsing symptoms, symptoms significant enough to be reported by the mother. Early-childhood wheezing not recalled by the mother had probably been mild and had remitted; otherwise, one would expect these symptoms to be remembered. Therefore, the risk factors for childhood wheeze identified in this study are more likely to apply to children with persistent wheeze, and less to children with transient wheeze.
Paternal and maternal history of asthma and hay fever was obtained from the guardian (usually mother) at age 7 and the study member at 18. Both mother and study member may underreport or confuse symptoms for other family members (e.g., reporting hay fever rather than a diagnosis of asthma). Therefore, we chose to combine asthma and hay fever into a single variable. Despite the potential for recall bias for maternal and paternal atopy by mother and study member, a maternal history of atopy was a risk factor for wheeze for both males and females, consistent with other studies (37, 38). A paternal history of atopy was a significant predictor of wheeze in females but did not show an age-dependent effect. Previous studies have found that maternal history was a strong risk factor for asthma under age 5, with paternal history being a weak risk factor for early-childhood wheeze and a stronger risk factor for wheeze after age 5 (39, 40). Both of these studies were analyzed cross-sectionally, without stratification by sex. If we analyze our study in a similar manner, paternal history is a risk factor for adolescent-onset wheeze. When analyzed longitudinally with stratification by sex, maternal and paternal history affects males and females differently.
Although dividing a sample into subgroups decreases the power of the study, subgroup analysis may still be sufficiently powered to see larger effects in at-risk subgroups within a study population (e.g., wheeze in females with a family history of atopy who are breastfed). One danger in stratification is if the subgroups are selected after a preliminary analysis has been completed. Such post hoc stratification may lead to biased results because the authors have prior knowledge of differences within the sample. In this report, all stratification decisions were made before undertaking the analyses.
We have considered several potential explanations for the finding of maternal history as a strong risk factor for wheeze in males and females, and paternal history as a strong risk factor for wheeze in females but a weak risk factor in males. Several of these (maternal–fetal interactions, genomic imprinting) only provide an incomplete explanation. We suggest that asthma might possibly be partly explained as an X-linked recessive disorder in the context of a complex genetic disorder. In short, if asthma is an X-linked recessive disorder, males should have a higher incidence of disease because they only have one copy of the X chromosome, whereas females need an abnormal X chromosome from both parents to manifest disease. However, because of X inactivation, heterozygous females may still develop a milder form of disease. Maternal history would be a strong risk factor because it would affect both sons and daughters. Paternal history would be a risk factor for asthma in females, who receive an X chromosome from their father, but not for males, who do not.
This X-linked recessive disorder hypothesis alone cannot explain the increased incidence of wheeze among adolescent females. However, several studies have suggested that female sex hormones influence asthma (41). Atopy, measured by skin-prick test, changes during the menstrual cycle (42). When estrogen levels are high, wheal and flare responses increase (42–44). The proliferation of peripheral blood monocytes to pokeweed mitogen is increased in the presence of estrogen, whereas testosterone inhibits this response (45, 46).
This analysis of our longitudinal birth cohort study suggests different mechanisms for the development of asthma at different times between males and females. The possibility that asthma may in part be an X-linked recessive disorder, explaining the different effects of maternal and paternal history of atopy, and that the gene products on the X chromosome that cause asthma are subsequently influenced by changes in sex hormones, needs to be further tested in genetic, epidemiologic, and clinical studies (47).
Supplementary Material
Acknowledgments
The authors thank the study members and their parents for their continued support. They also thank Air New Zealand, Dr. Phil A. Silva, the study founder, and Dr. Richie Poulton, current director.
The Dunedin Multidisciplinary Health and Development Research Unit is funded by the Health Research Council of New Zealand. The respiratory section of the study was funded by the Health Research Council, the Otago Medical Research Foundation, the New Zealand Lottery Grants Board, and the Asthma Foundation of New Zealand. Collection of data used in this report was also funded by the National Heart Foundation (New Zealand) and the U.S. National Institute of Mental Health grant MH45070. P.J.M. is a CIHR Strategic Training Fellow in the Canadian Child Health Clinician Scientist Program and holds a training award from the CHEST foundation (United States). M.R.S. holds the AstraZeneca Chair in Respiratory Epidemiology, McMaster University.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Conflict of Interest Statement: P.J.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; J.M.G. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; J.O.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript; D.R.T. has no commercial interests that represent a conflict of interest regarding this study. He received airfare and accommodation expenses for speaking at a symposium sponsored by AstraZeneca in 2005. His department received an educational grant from GlaxoSmithKline annually until 2004, valued at N.Z. $45,000 per annum; M.R.S. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.Dodge RR, Burrows B. The prevalence and incidence of asthma and asthma-like symptoms in a general population sample. Am Rev Respir Dis 1980;122:567–575. [DOI] [PubMed] [Google Scholar]
- 2.Becklake MR, Kauffmann F. Gender differences in airway behaviour over the human life span. Thorax 1999;54:1119–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nicolai T, Illi S, Tenborg J, Kiess W, v Mutius E. Puberty and prognosis of asthma and bronchial hyper-reactivity. Pediatr Allergy Immunol 2001;12:142–148. [DOI] [PubMed] [Google Scholar]
- 4.de Marco R, Locatelli F, Sunyer J, Burney P. Differences in incidence of reported asthma related to age in men and women: a retrospective analysis of the data of the European Respiratory Health Survey. Am J Respir Crit Care Med 2000;162:68–74. [DOI] [PubMed] [Google Scholar]
- 5.Crawford WA, Beedham CG. The changing demographic pattern in asthma related to sex and age: a study of 13,651 patients on sodium cromoglycate (Intal). Med J Aust 1976;1:430–434. [PubMed] [Google Scholar]
- 6.Bjornson CL, Mitchell I. Gender differences in asthma in childhood and adolescence. J Gend Specif Med 2000;3:57–61. [PubMed] [Google Scholar]
- 7.Sears MR, Greene JM, Willan AR, Wiecek EM, Taylor DR, Flannery EM, Cowan JO, Herbison GP, Silva PA, Poulton R. A longitudinal, population-based, cohort study of childhood asthma followed to adulthood. N Engl J Med 2003;349:1414–1422. [DOI] [PubMed] [Google Scholar]
- 8.Grol MH, Gerritsen J, Postma DS. Asthma: From childhood to adulthood. Allergy 1996;51:855–869. [DOI] [PubMed] [Google Scholar]
- 9.European Community Respiratory Health Survey. Variations in the prevalence of respiratory symptoms, self-reported asthma attacks, and use of asthma medication in the European Community Respiratory Health Survey (ECRHS). Eur Respir J 1996;9:687–695. [DOI] [PubMed] [Google Scholar]
- 10.Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, Mitchell EA, Pearce N, Sibbald B, Stewart AW, et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J 1995;8:483–491. [DOI] [PubMed] [Google Scholar]
- 11.Mao Y, Semenciw R, Morrison H, MacWilliam L, Davies J, Wigle D. Increased rates of illness and death from asthma in Canada. Can Med Assoc J 1987;137:620–624. [PMC free article] [PubMed] [Google Scholar]
- 12.Vollmer WM, Osborne ML, Buist AS. 20-year trends in the prevalence of asthma and chronic airflow obstruction in an HMO. Am J Respir Crit Care Med 1998;157:1079–1084. [DOI] [PubMed] [Google Scholar]
- 13.Mannino DM, Homa DM, Pertowski CA, Ashizawa A, Nixon LL, Johnson CA, Ball LB, Jack E, Kang DS. Surveillance for asthma: United States, 1960–1995. MMWR CDC Surveill Summ 1998;47:1–27. [PubMed] [Google Scholar]
- 14.International Study of Asthma and Allergies in Childhood. Worldwide variations in the prevalence of asthma symptoms: the International Study of Asthma and Allergies in Childhood (ISAAC). Eur Respir J 1998;12:315–335. [DOI] [PubMed] [Google Scholar]
- 15.Italian Studies on Respiratory Disorders in Childhood and the Environment. Asthma and respiratory symptoms in 6–7 yr old Italian children: gender, latitude, urbanization and socioeconomic factors. SIDRIA (Italian Studies on Respiratory Disorders in Childhood and the Environment). Eur Respir J 1997;10:1780–1786. [DOI] [PubMed] [Google Scholar]
- 16.Sunyer J, Anto JM, Kogevinas M, Barcelo MA, Soriano JB, Tobias A, Muniozguren N, Martinez-Moratalla J, Payo F, Maldonado JA. Risk factors for asthma in young adults. Spanish Group of the European Community Respiratory Health Survey. Eur Respir J 1997;10:2490–2494. [DOI] [PubMed] [Google Scholar]
- 17.Jarvholm B, Brisman J, Toren K. The association between epidemiological measures of the occurrence of asthma. Int J Tuberc Lung Dis 1998;2:1029–1036. [PubMed] [Google Scholar]
- 18.De Marco R, Locatelli F, Cerveri I, Bugiani M, Marinoni A, Giammanco G. Incidence and remission of asthma: a retrospective study on the natural history of asthma in Italy. J Allergy Clin Immunol 2002;110:228–235. [DOI] [PubMed] [Google Scholar]
- 19.Bronnimann S, Burrows B. A prospective study of the natural history of asthma: remission and relapse rates. Chest 1986;90:480–484. [DOI] [PubMed] [Google Scholar]
- 20.Martin AJ, McLennan LA, Landau LI, Phelan PD. The natural history of childhood asthma to adult life. BMJ 1980;280:1397–1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sears MR. Consequences of long-term inflammation: the natural history of asthma. Clin Chest Med 2000;21:315–329. [DOI] [PubMed] [Google Scholar]
- 22.Nicolai T, Pereszlenyiova-Bliznakova L, Illi S, Reinhardt D, von Mutius E. Longitudinal follow-up of the changing gender ratio in asthma from childhood to adulthood: role of delayed manifestation in girls. Pediatr Allergy Immunol 2003;14:280–283. [DOI] [PubMed] [Google Scholar]
- 23.Xuan W, Marks GB, Toelle BG, Belousova E, Peat JK, Berry G, Woolcock AJ. Risk factors for onset and remission of atopy, wheeze, and airway hyperresponsiveness. Thorax 2002;57:104–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sears MR, Burrows B, Flannery EM, Herbison GP, Holdaway MD. Atopy in childhood: I. Gender and allergen related risks for development of hay fever and asthma. Clin Exp Allergy 1993;23:941–948. [DOI] [PubMed] [Google Scholar]
- 25.Yeatts K, Davis KJ, Sotir M, Herget C, Shy C. Who gets diagnosed with asthma? Frequent wheeze among adolescents with and without a diagnosis of asthma. Pediatrics 2003;111:1046–1054. [DOI] [PubMed] [Google Scholar]
- 26.Henriksen AH, Holmen TL, Bjermer L. Gender differences in asthma prevalence may depend on how asthma is defined. Respir Med 2003;97:491–497. [DOI] [PubMed] [Google Scholar]
- 27.Siersted HC, Boldsen J, Hansen HS, Mostgaard G, Hyldebrandt N. Population based study of risk factors for underdiagnosis of asthma in adolescence: Odense schoolchild study. BMJ 1998;316:651–655 [discussion 655–656]. [PMC free article] [PubMed] [Google Scholar]
- 28.Silva PA, Stanton WR. From child to adult: the Dunedin multidisciplinary health and development study. Auckland, New Zealand: Oxford University Press; 1996.
- 29.Jones DT, Sears MR, Holdaway MD, Hewitt CJ, Flannery EM, Herbison GP, Silva PA. Childhood asthma in New Zealand. Br J Dis Chest 1987;81:332–340. [DOI] [PubMed] [Google Scholar]
- 30.Sears MR, Jones DT, Silva PA, Simpson A, Williams SM. Asthma in seven year old children: a report from the Dunedin Multidisciplinary Child Development Study. N Z Med J 1982;95:533–536. [PubMed] [Google Scholar]
- 31.Sears MR, Greene JM, Willan AR, Taylor DR, Flannery EM, Cowan JO, Herbison GP, Poulton R. Long-term relation between breastfeeding and development of atopy and asthma in children and young adults: a longitudinal study. Lancet 2002;360:901–907. [DOI] [PubMed] [Google Scholar]
- 32.Sears MR, Jones DT, Holdaway MD, Hewitt CJ, Flannery EM, Herbison GP, Silva PA. Prevalence of bronchial reactivity to inhaled methacholine in New Zealand children. Thorax 1986;41:283–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sears MR, Herbison GP, Holdaway MD, Hewitt CJ, Flannery EM, Silva PA. The relative risks of sensitivity to grass pollen, house dust mite and cat dander in the development of childhood asthma. Clin Exp Allergy 1989;19:419–424. [DOI] [PubMed] [Google Scholar]
- 34.Hancox RJ, Milne BJ, Poulton R, Taylor DR, Greene JM, McLachlan CR, Cowan JO, Flannery EM, Herbison GP, Sears MR. Sex differences in the relation between body mass index and asthma and atopy in a birth cohort. Am J Respir Crit Care Med 2005;171:440–445. [DOI] [PubMed] [Google Scholar]
- 35.Sears MR, Taylor DR, Poulton R. Breastfeeding and asthma: appraising the controversy: a rebuttal. Pediatr Pulmonol 2003;36:366–368. [DOI] [PubMed] [Google Scholar]
- 36.Sears MR, Taylor DR, Greene JM, Poulton R, Herbison GP. Breastfeeding, atopy, and asthma: authors reply. Lancet 2003;361:175–176. [Google Scholar]
- 37.Sulit LG, Storfer-Isser A, Rosen CL, Kirchner HL, Redline S. Associations of obesity, sleep-disordered breathing, and wheezing in children. Am J Respir Crit Care Med 2005;171:659–664. [DOI] [PubMed] [Google Scholar]
- 38.Frey U, Kuehni C, Roiha H, Cernelc M, Reinmann B, Wildhaber JH, Hall GL. Maternal atopic disease modifies effects of prenatal risk factors on exhaled nitric oxide in infants. Am J Respir Crit Care Med 2004;170:260–265. [DOI] [PubMed] [Google Scholar]
- 39.Litonjua AA, Carey VJ, Burge HA, Weiss ST, Gold DR. Parental history and the risk for childhood asthma: does mother confer more risk than father? Am J Respir Crit Care Med 1998;158:176–181. [DOI] [PubMed] [Google Scholar]
- 40.Dold S, Wjst M, von Mutius E, Reitmeir P, Stiepel E. Genetic risk for asthma, allergic rhinitis, and atopic dermatitis. Arch Dis Child 1992;67:1018–1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Varraso R, Siroux V, Maccario J, Pin I, Kauffmann F. Asthma severity is associated with body mass index and early menarche in women. Am J Respir Crit Care Med 2005;171:334–339. [DOI] [PubMed] [Google Scholar]
- 42.Kalogeromitros D, Katsarou A, Armenaka M, Rigopoulos D, Zapanti M, Stratigos I. Influence of the menstrual cycle on skin-prick test reactions to histamine, morphine and allergen. Clin Exp Allergy 1995;25:461–466. [DOI] [PubMed] [Google Scholar]
- 43.Barbee RA, Kaltenborn W, Lebowitz MD, Burrows B. Longitudinal changes in allergen skin test reactivity in a community population sample. J Allergy Clin Immunol 1987;79:16–24. [DOI] [PubMed] [Google Scholar]
- 44.Cline MG, Burrows B. Distribution of allergy in a population sample residing in Tucson, Arizona. Thorax 1989;44:425–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sthoeger ZM, Chiorazzi N, Lahita RG. Regulation of the immune response by sex hormones: I. In vitro effects of estradiol and testosterone on pokeweed mitogen-induced human B cell differentiation. J Immunol 1988;141:91–98. [PubMed] [Google Scholar]
- 46.Paavonen T, Andersson LC, Adlercreutz H. Sex hormone regulation of in vitro immune response. Estradiol enhances human B cell maturation via inhibition of suppressor T cells in pokeweed mitogen-stimulated cultures. J Exp Med 1981;154:1935–1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Blumenthal MN. New thoughts regarding the genetics of atopy. Am J Respir Crit Care Med 2004;169:555–556. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.