Abstract
Rationale: Air pollution by particulate matter (PM) has been associated with cardiovascular deaths, although the mechanism of action is unclear. One proposed pathway is through disturbances of the autonomic control of the heart.
Objectives: We tested the hypothesis that such disturbances are mediated by PM increasing oxidative stress by examining the association between PM and the high-frequency (HF) component of heart rate variability as modified by the presence or absence of the allele for glutathione-S-transferase M1 (GSTM1) and the use of statins, obesity, high neutrophil counts, higher blood pressure, and older age.
Methods: We examined the association between particles less than 2.5 μM in aerodiameter (PM2.5) and HF in 497 participants in the Normative Aging Study, using linear regression controlling for covariates.
Main Results: A 10-μg/m3 increase in PM2.5 during the 48 h before HF measurement was associated with a 34% decrease in HF, 95% confidence interval (−9%, −52%), in subjects without the allele, but had no effect in subjects with GSTM1 present. Among GSTM1-null subjects, the use of statins eliminated the effect of PM2.5. Obesity and high neutrophil counts also worsened the PM effects with or without GSTM1.
Conclusion: The effects of PM2.5 on HF appear to be mediated by reactive oxygen species. This may be a key pathway for the adverse effects of combustion particles.
Keywords: genetic polymorphisms, heart rate variability, oxidative stress, particles
A large body of evidence has demonstrated that particulate air pollution (PM) is associated with short-term changes in the risk of death (1–6). An early study showed the risk of dead-on-arrival deaths associated with particles was three times that for all deaths (7). This suggests a predominant effect on sudden deaths from arrhythmias and myocardial infarctions. Subsequent studies have confirmed that PM is associated with myocardial infarctions (8, 9), hospital admissions for cardiovascular disease (10, 13), discharges of implantable defibrillators (14), and electrocardiographic disturbances (15).
How airborne particles can be producing these responses in still unclear. However, particles have been linked with changes in intermediate markers, such as clotting factors (16, 17) and increased atherosclerosis (18).
Airborne particles have also been associated with changes in heart rate variability (HRV) (15, 19). The parasympathetic and sympathetic stimulation of the heart produces variations in the time intervals between normal heartbeats; analysis of this variability is therefore an estimate of cardiac autonomic regulation. HRV is a noninvasive measure that independently predicts cardiovascular mortality in patients with and without underlying cardiovascular disease (20, 21). Hence, disturbances in HRV may represent one pathway by which particles might be associated with sudden death.
Overall, studies have generally found significant associations with HRV in elderly subjects, but weaker associations in younger subjects (22), suggesting that age-related decreases in toxic defenses play a role in susceptibility. In a recent review (22), we found the only consistent PM association was with the high-frequency (HF) components of HRV, either HF in the frequency domain, or root mean squared differences between adjacent RR intervals (rMSSD) or proportion of adjacent NN intervals differing by more than 50 ms (PNN50) in the time domain. In contrast, low frequency was not associated with particles in four of five studies. This suggests a paramount effect on the parasympathetic nervous system. This may be because the vagus nerve innervates the lung.
Various mechanisms by which particles exert these effects have been proposed (23). Reactive oxygen species (ROS) have been mentioned as a potential pathway for the adverse effects of particles (24, 25). ROS have established importance in the pathogenesis of cardiovascular diseases (26). Exposure to urban particles increased ROS in a dose-dependent manner in the lung and heart of living animals (27). It is unclear what role ROS may play in explaining the effects of particles on autonomic endpoints, such as defibrillator discharge and HRV. This question may be addressed by examining the effects of particles on HRV in populations with different host defenses to an oxidative stress challenge. Genetic polymorphisms have been linked to important differences in such defenses.
Glutathione pathways play a key role in cellular defenses against ROS (28). Glutathione-S-tranferases (GSTs) are a family of enzymes involved in the metabolism of ROS and xenobiotic compounds.
Genetic polymorphisms of the GSTs are common, and have been shown to modify the response to air pollutants (29). The GSTM1 gene is deleted in approximately half of the white population (the polymorphic “null” genotype), and lack of the GSTM1 protein has been associated an enhanced nasal allergic response to diesel exhaust particles (30). Children who are GSTM1-null and are exposed to environmental tobacco smoke had elevated odds of developing asthma (31), and the GSTM1-null genotype interacts with tobacco smoke in increasing the risk of coronary disease (32).
Drugs that modify oxidant defenses may also influence susceptibility to particle-induced ROS. Statins are a widely prescribed class of drugs originally developed for their lipid-lowering properties, but they have been shown to have substantial antiinflammatory and antioxidant activity as well (33). In addition to lowering C-reactive protein concentrations (34), statins have been shown to decrease superoxide production (35), increase release of nitric oxide (NO) (36), which is an antioxidant as well as a vasodilator, and reduce markers of oxidative stress in APOE−1/−1 mice (37).
We examined the association of fine-particulate air pollution of less than 2.5 μM in aerodynamic diameter (PM2.5) on the HF HRV of elderly subjects living in the Boston metropolitan area, and how that association varied by GSTM1 genotype or statin use. In addition, because statins have important effects beyond their antioxidant properties, we examined whether obesity or elevated neutrophil count, which are associated with inflammation and oxidative stress, also modified the association. Finally, we examined two more generic markers of susceptibility, older age or higher blood pressure, as modifiers of the PM effect. This study was reviewed and approved by the institutional review boards of all of the participating institutions.
METHODS
Study Population
The Normative Aging Study is a longitudinal study established by the Veterans Administration in 1961, enrolling 2,280 men from the greater Boston area who were free of known chronic medical conditions (38). Beginning in 2000, during each participant's regularly scheduled evaluation, HRV was measured. Further details have been described previously (22). That study examined a range of air pollutants and measures of HRV, but did not look at genetic or other factors related to oxidative stress. It found the most consistent associations with PM2.5, and with HRV measures indicative of a parasympathetic effect (HF, rMSSD).
HRV Measurement
HRV was measured for 7 min in a sitting position using a two-channel (five-lead) ECG monitor (Trillium 3000; Forest Medical, East Syracuse, NY). Only normal-to-normal (NN) beat intervals were included in the analysis. We used the best 4-consecutive-min intervals for the HRV calculations, and computed the HF (0.15–0.4 Hz) component of HRV using software complying with guidelines (39). Subjects with irregular ECG patterns that interfere with HRV estimation were excluded.
GSTM1 Genotyping.
The assay consists of polymerase chain reaction amplification of exons 4 and 5 of the GSTM1 allele. Because this polymorphism is a gene deletion, polymerase chain reaction product indicates the presence of one or more copies of the gene. Further details are in the online supplement.
Air Pollution and Weather Data
Continuous PM2.5 was measured at a monitoring site 1 km from the exam site, using the Tapered Element Oscillating Microbalance (TEOM, model 1400A; Rupprecht & Pataschnick, Albany, NY), with a season-specific correction to compensate for the loss of semivolatile mass (40). Weather measurements were obtained from the airport weather station.
To control for outdoor weather, we used apparent temperature, defined as a person's perceived air temperature, given the humidity (41). We used the average of PM2.5 concentrations in the 48 h before examination as our exposure index, because that exposure period has been most consistently associated with sudden death (4, 5).
Statistical Methods
HRV was log10-transformed to improve normality and stabilize the variance. The following variables were chosen a priori and included in the linear regression analysis: age, cigarette smoking, body mass index, diastolic blood pressure, fasting blood glucose, alcohol consumption (≥ 2 drinks/d), use of β-blockers, angiotensin-converting enzyme inhibitors, and/or calcium channel blockers, season, room temperature, and average apparent temperature 48 h before the HRV measurement. We used a spline with 3 degrees of freedom to account for potential nonlinearity in the relationship between apparent temperature and HRV. After 14 subjects with missing values of covariates were excluded, 497 subjects were available for the analyses.
Stratified regression models examined subjects with and without the GSTM1 gene, with and without statin use, and by the four possible combinations of genotype and statin use. Stratified analyses were also done, in turn, by the four possible combinations of GSTM1 gene and by whether or not the subjects were in the most adverse quartile of neutrophil count, blood pressure, or age, or whether they had a body mass index above 30.
RESULTS
Table 1 shows the demographic and clinical characteristics and HRV measurements of the subjects, as well as environmental variables. The study participants were all male, and their average age was 72.7 yr (SD, 6.6 yr). The correlation between temperature and particle concentrations was modest (0.35).
TABLE 1.
DESCRIPTIVE STATISTICS OF THE VARIABLES (MEAN [SD] OR NUMBER [%])
| Variable | All Subjects (n = 497) |
|---|---|
| Age, yr | 72.7 (6.6) |
| Body mass index, kg/m2 | 28.3 (4.1) |
| Diastolic blood pressure, mm Hg | 75.7 (9.4) |
| Heart rate, beat/min | 70.7 (6.7) |
| Fasting blood glucose, mg/dl | 108.0 (29.0) |
| Cholesterol, mg/dl | 197.0 (37.6) |
| HDL, mg/dl | 49.7 (13.5) |
| Smoking status, n (%) | |
| Never smoker | 160 (32.2) |
| Former smoker | 311 (62.6) |
| Current smoker | 26 (5.2) |
| Alcohol intake (≥ 2/day), n (%) | 96 (19.3) |
| Hypertension, n (%) | 335 (67.4) |
| Use of β-blocker, n (%) | 163 (32.8) |
| Use of Ca-channel blocker, n (%) | 70 (14.1) |
| Use of ACE inhibitor, n (%) | 100 (20.1) |
| Use of statins, n (%) | 179 (36) |
| Neutrophil count (% of cells) | 62 (8.8) |
| Heart rate variability | |
| Log10 HF, ms2 | 1.9 (0.66) |
| Environmental variables | |
| PM2.5, μg/m3 | 11.4 (8.0) |
| Apparent temperature, °C | 11.4 (9.9) |
| Room temperature, °C | 24.5 (1.4) |
Definition of abbreviations: ACE = angiotensin-converting enzyme; HDL = high-density lipoprotein; HF = high frequency; PM2.5 = particulate matter less than 2.5 μM in aerodiameter.
Values are listed as mean (SD) or numbers (%).
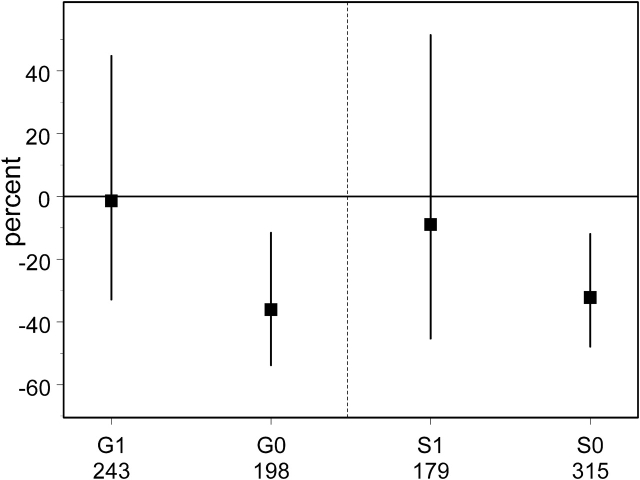
In a model including all subjects, and the covariates listed above, a 10-μg/m3 increase in PM2.5 was associated with a 27% decrease in HF (95% confidence interval, −8%, −42%). Note that the interquartile range for PM2.5 in these data was 7 μg/m3. When stratified by GSTM1 status, no relationship of PM2.5 and HF was seen in persons with the gene, whereas a significant association (34% decrease; 95% confidence interval, −9%, −52%) was seen in subjects with the GSTM1 null deletion (Figure 1). Similarly, when stratified by statin use, only subjects not taking statins evidenced diminished HF in the presence of elevated PM2.5 (Figure 1). When the data were analyzed by strata of both GSTM1 status and statin use, GSTM1-null subjects who were taking statins were protected against the effect of PM2.5, which was only present in subjects with the gene deletion who were not taking statins (Figure 2, Table 2).
Figure 1.
The estimated covariate-adjusted percentage decrease in the high-frequency (HF) component of heart rate variability (and 95% confidence interval) that is associated with a 10-μg/m3 increase in concentrations of particles less than 2.5 μM in aerodiameter (PM2.5) is shown for persons with (G0) and without (G1) the deletion of the GSTM1 gene (left side), and for persons with (S1) and without (S0) statin use (right side). The covariates controlled were age, cigarette smoking, body mass index, diastolic blood pressure, fasting blood glucose, alcohol consumption, use of β-blockers, use of angiotensin-converting enzyme inhibitors, use of calcium channel blockers, season, room temperature, and outdoor temperature. The numbers below the labels are the number of subjects in each analysis.
Figure 2.
The estimated covariate-adjusted percentage decrease in the HF component of heart rate variability (and 95% confidence interval) associated with a 10-μg/m3 increase in PM2.5 concentrations is shown for persons who are (S1) and are not (S0) taking a statin, with (G0) or without (G1) the deletion of GSTM1. The covariates controlled are as in Figure 1. The number of subjects in each category is listed below the category label.
TABLE 2.
EFFECT OF A 10-μg/m3 INCREASE IN PM2.5 ON HIGH FREQUENCY BY STRATA OF GSTM1 AND OTHER POTENTIAL EFFECT MODIFIERS
| Category | Change (%) | 95% Confidence Interval | n |
|---|---|---|---|
| GSTM1 null, no statin | −34.0 | −53.0, −7.20 | 162 |
| GSTM1 null, statin | −6.4 | −66.5, 161.9 | 81 |
| GSTM1 present, no statin | −3.6 | −40.5, 56.2 | 117 |
| GSTM1 present, statin | −3.2 | −50.0, 87.2 | 81 |
| GSTM1 null, high neutrophils* | −55.7 | −88.0, 63.1 | 64 |
| GSTM1 null, normal neutrophils† | −36.1 | −55.2, −8.7 | 179 |
| GSTM1 present, high neutrophils* | −49.6 | −86.4, 86.1 | 51 |
| GSTM1 present, normal neutrophils† | 17.6 | −20.0, 73.0 | 147 |
| GSTM1 null, obese‡ | −57.3 | −88.0, 52.0 | 61 |
| GSTM1 null, not obese§ | −31.0 | −50.6, −3.6 | 182 |
| GSTM1 present, obese‡ | −34.2 | −77.9, 96.5 | 54 |
| GSTM1 present, not obese§ | 7.5 | −29.7, 64.3 | 144 |
| GSTM1 null, older* | −37.0 | −64.9, 13.0 | 63 |
| GSTM1 null, younger† | −33.1 | −55.3, 0.3 | 180 |
| GSTM1 present, older* | −7.6 | −57.1, 98.8 | 49 |
| GSTM1 present, younger† | −0.3 | −41.6, 70.1 | 149 |
| GSTM1 null, higher blood pressure* | −47.3 | −81.0, 45.7 | 59 |
| GSTM1 null, lower blood pressure† | −34.9 | −54.7, −6.5 | 184 |
| GSTM1 present, higher blood pressure* | −21.1 | −76.4, 164.4 | 48 |
| GSTM1 present, lower blood pressure† | −8.7 | −40.0, 38.9 | 150 |
Upper 25th percentile of the distribution in the study population.
Lower 75% of the distribution in the study population.
Obesity: body mass index of 30 kg/m2 or greater.
Body mass index < 30 kg/m2.
The two other potential effect modifiers that we hypothesized were more strongly related to oxidative stress showed similar patterns of effect modification (Table 2). For subjects with obesity or higher neutrophil counts, there was some effect of particles, even with the GSTM1 gene, and an enhancement of the PM2.5 effect for persons both without the gene and with the other oxidative stress–related effect modifier. In contrast, older age did not modify the PM2.5 effect in subjects with or without the gene. Higher blood pressure was intermediate, showing some indication of a PM2.5 effect in subjects with the gene, and a modest enhancement of the effect in subjects without the gene.
DISCUSSION
We found that the association between PM2.5 and reduced HF is only evident in persons missing the allele for GSTM1 or in persons likely to have greater than average baseline systemic inflammation and oxidative stress, such as in obese individuals. Furthermore, among GSTM1-null subjects, statins were protective against the effects of PM2.5. In nonobese subjects, we saw effect modification by GSTM1, but the response was almost doubled in obese subjects who were GSTM1 null. Being in the upper quartile of neutrophil counts also substantially increased the PM2.5 effect in subjects who were GSTM1 null.
These results suggest that the confluence of two factors resulting in increased levels of or impaired defenses against oxidative stress results in even greater response to particles.
Although GSTM1, obesity, increased neutrophils, and statins involve several physiologic pathways, the striking observation that statins counter the susceptibility to PM2.5-associated reductions in HF conferred by the GSTM1 deletion, and that the genotype interacts with obesity and increased neutrophil counts, suggests there exists a common mechanism of action. It seems likely that ROS (a common mechanism of action of these modifiers) plays an important role in this response. Obesity is known to increase systemic inflammation and oxidative stress, and increased neutrophil count is also a marker of systemic inflammation. That subjects with those conditions had a response to PM2.5 even in the presence of GSTM1, but an enhanced response in its absence, also suggests a central role of inflammation and oxidative stress in the autonomic effects of PM2.5.
Particles increase ROS production, perhaps in a catalytic fashion via redox cycling (24, 25, 27). A recent follow-up to the study that showed particles induced ROS in the lung and heart (27) found that administration of N-acetyl cysteine, a glutathione precursor, blunted that effect (42). Those results suggest an important role of the glutathione pathway in the defense against urban particles.
Particles induce proinflammatory mediators such as cytokines in the lungs (24, 43), and increase extracellular calcium influx, possibly through activation of calcium channels in the plasma membrane (44). Recently, particle exposure has been shown to increase circulating levels of asymmetric dimethylarginine, an endogenous inhibitor of NO synthase that is associated with impaired vascular function and increased risk for cardiovascular events (45). This suggests that NO concentrations may be impaired after particle exposure. This fits in well with the observation that statins, which blocked the effects of PM2.5 in this study, enhance NO release. In general, all three PM-associated impairments have been linked with an increase in sympathetic and a reduction in vagal tone (46–48).
Nevertheless, we cannot rule out the importance of other pathways in the modification of the PM2.5 effects. Statins are associated with lower risk of arrhythmic events (49) and increased HF component of HRV (50). The mechanisms of this antiarrhythmic properties are unclear, but may include enhanced NO synthase (51), decreased endothelin-1 (52), or other pathways not yet understood. Similarly, obesity affects many metabolic pathways, and does not merely increase inflammation.
We have also demonstrated that questions of mechanism of action of environmental agents, often considered the domain of toxicology, can also be addressed in humans using gene by environment, gene by drug by environment, and gene by phenotype by environment interactions. Although there are limitations to this approach, the ability to study the species of interest in the exposure range of interest makes it a valuable tool for examining mechanisms of environmental toxins.
There are a number of limitations to this analysis. First, we have used PM2.5 concentrations at a single monitoring site as a surrogate for recent exposure to PM2.5. A recent study comparing personal exposures to monitoring at the same site, in several panels of subjects, reported a high longitudinal correlation between the monitor's readings and personal exposure (53). In addition, PM2.5 concentrations have been shown to be spatially homogeneous over the Boston area, suggesting that this is a reasonable approximation, and the error is likely to be nondifferential (53). Other genes affect responses to ROS, and our findings suggest that these also may play a role in individual response to air pollution–induced morbidity and/or mortality. We believe our current findings provide further evidence that ROS are an important pathway for particle toxicity.
Supplementary Material
Acknowledgments
The authors thank Elaine R. Dibbs and Jordan D. Auerbach for conducting the HRV measurements and other contributions to the VA Normative Aging Study.
Supported by grants EPA R8273535, T32 ES07069-22, and NIEHS ES00002. The VA Normative Aging Study is supported by the Cooperative Studies Program/ERIC of the U.S. Department of Veterans Affairs and is a component of the Massachusetts Veterans Epidemiology Research and Information Center, Boston, Massachusetts. S.K.P. and M.S.O. were supported by National Institutes of Health training grant 2 T32 ES07069-24.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Originally Published in Press as DOI: 10.1164/rccm.200412-1698OC on July 14, 2005
Conflict of Interest Statement: J.S. has no financial relationship with a commercial entity that has an interest in the subject of this manuscript. S.K.P. has no financial relationship with a commercial entity that has an interest in the subject of this manuscript. M.S.O. has no financial relationship with a commercial entity that has an interest in the subject of this manuscript. P.S.V. has no financial relationship with a commercial entity that has an interest in the subject of this manuscript. D.S. has no financial relationship with a commercial entity that has an interest in the subject of this manuscript. S.W. received a grant for $900,065, Asthma Policy Modeling Study, from AstraZeneca from 1997–2003. He has been a coinvestigator on a grant from Boehringer Ingelheim, which began in 2003, to investigate a chronic obstructive pulmonary disease natural history model. He has received no funds for his involvement in this project. He has been an advisor to the TENOR study for Genentech and has received $5,000 for 2003–2004. He received a grant from Glaxo-Wellcome for $500,000 for genomic equipment from 2000–2003. He was a consultant for Roche Pharmaceuticals in 2000 and received no financial renumeration for this consultancy. K.K. has no financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.Schwartz J, Marcus A. Mortality and air pollution in London: a time series analysis. Am J Epidemiol 1990;131:185–194. [DOI] [PubMed] [Google Scholar]
- 2.Schwartz J. Particulate air pollution and daily mortality in Detroit. Environ Res 1991;56:204–213. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz J, Dockery DW. Particulate air pollution and daily mortality in Steubenville, Ohio. Am J Epidemiol 1992;135:12–19. [Discussion: 20–5.] [DOI] [PubMed] [Google Scholar]
- 4.Schwartz J, Dockery DW, Neas LM. Is daily mortality associated specifically with fine particles? J Air Waste Manag Assoc 1996;46:927–939. [PubMed] [Google Scholar]
- 5.Katsouyanni K, Touloumi G, Spix C, Schwartz J, Balducci F, Medina S, Rossi G, Wojtyniak B, Sunyer J, Bacharova L, et al. Short-term effects of ambient sulphur dioxide and particulate matter on mortality in 12 European cities: results from time series data from the APHEA project. Air Pollution and Health: a European Approach. BMJ 1997;314:1658–1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Samet JM, Dominici F, Curriero FC, Coursac I, Zeger SL. Fine particulate air pollution and mortality in 20 US cities, 1987–1994. N Engl J Med 2000;343:1742–1749. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz J. What are people dying of on high air pollution days? Environ Res 1994;64:26–35. [DOI] [PubMed] [Google Scholar]
- 8.Peters A, Dockery DW, Muller JE, Mittleman MA. Increased particulate air pollution and the triggering of myocardial infarction. Circulation 2001;103:2810–2815. [DOI] [PubMed] [Google Scholar]
- 9.Zanobetti A, Schwartz J. The effect of particulate air pollution on emergency admissions for myocardial infarction: a multi-city case-crossover analysis. Environ Health Perspect 2005;113:978–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schwartz J, Morris R. Air pollution and hospital admissions for cardiovascular disease in Detroit, Michigan. Am J Epidemiol 1995;142:23–35. [DOI] [PubMed] [Google Scholar]
- 11.Burnett RT, Smith-Doiron M, Stieb D, Cakmak S, Brook JR. Effects of particulate and gaseous air pollution on cardiorespiratory hospitalizations. Arch Environ Health 1999;54:130–139. [DOI] [PubMed] [Google Scholar]
- 12.Schwartz J. Air pollution and hospital admissions for heart disease in eight US counties. Epidemiology 1999;10:17–22. [PubMed] [Google Scholar]
- 13.LeTertre A, Medina S, Samoli E, Fosberg B, Michelozzi P, Boumghar A, Vonk JM, Bellini A, Atkinson R, Ayres JG, et al. Short-term effects of particulate air pollution on cardiovascular diseases in eight European cities. J Epidemiol Comm Health 2002;56:773–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peters A, Liu E, Verrier RL, Schwartz J, Gold DR, Mittleman M, Baliff J, Oh JA, Allen G, Monahan K, et al. Air pollution and incidence of cardiac arrhythmia. Epidemiology 2000;11:11–17. [DOI] [PubMed] [Google Scholar]
- 15.Pope CA III, Verrier RL, Lovett EG, Larson AC, Raizenne ME, Kanner RE, Schwartz J, Villegas GM, Gold DR, Dockery DW. Heart rate variability associated with particulate air pollution. Am Heart J 1999;138:890–899. [DOI] [PubMed] [Google Scholar]
- 16.Gardner SY, Lehmann JR, Costal DL. Oil fly ash induced elevation of plasma fibrinogen levels in rats. Toxicol Sci 2000;56:175–180. [DOI] [PubMed] [Google Scholar]
- 17.Schwartz J. Air pollution and blood markers of cardiovascular risk. Environ Health Perspect 2001;109:405–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuenzli N, Jerrett M, Mack W, Beckerman B, LaBree L, Gilliland F, Thomas D, Peters J, Hodis H. Ambient air pollution and atherosclerosis in Los Angeles. Environ Health Perspect 2005;113:201–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chan CC, Chuang KJ, Shiao GM, Lin LY. Personal exposure to submicrometer particles and heart rate variability in human subjects. Environ Health Perspect 2004;112:1063–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kleiger R, Miller J, Bigger JJ, Moss A. Decreased heart rate variability and its association with increased mortality after acute myocardial infarction. Am J Cardiol 1987;59:256–262. [DOI] [PubMed] [Google Scholar]
- 21.Tsuji H, Arson M, Venditti FJ, Manders E, Evans J, Feldman C, Levy D. Impact of reduced heart rate variability on risk for cardiac events. The Framingham Heart Study. Circulation 1996;94:2850–2855. [DOI] [PubMed] [Google Scholar]
- 22.Park SK, O'Neill MS, Vokonas PS, Sparrow D, Schwartz J. Effects of air pollution on heart rate variability: the VA Normative Aging Study. Environ Health Perspect 2005;113:304–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brook RD, Franklin B, Cascio W, Hong Y, Howard G, Lipsett M, Luepker R, Mittleman M, Samet J, Smith SC Jr, et al. Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation 2004;109:2655–2671. [DOI] [PubMed] [Google Scholar]
- 24.Donaldson K, Stone V, Seaton A, MacNee W. Ambient particle inhalation and the cardiovascular system: potential mechanisms. Environ Health Perspect 2001;109:523–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brook RD, Brook JR, Rajagopalan S. Air pollution: the “heart” of the problem. Curr Hypertens Rep 2003;5:32–39. [DOI] [PubMed] [Google Scholar]
- 26.Dhalla NS, Temsah RM, Netticadan T. Role of oxidative stress in cardiovascular diseases. J Hypertens 2000;18:655–673. [DOI] [PubMed] [Google Scholar]
- 27.Gurgueira S, Lawrence J, Coull B, Murthy G, Gonzalez-Flecha B. Rapid increases in the steady-state concentration of reactive oxygen species in the lungs and heart after particulate air pollution inhalation. Environ Health Perspect 2002;110:749–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hayes JD, McLellan LI. Glutathione and glutathione dependent enzymes represent a co-ordinately regulated defense against oxidative stress. Free Radic Res 1999;31:273–300. [DOI] [PubMed] [Google Scholar]
- 29.Bergamaschi E, De Palma G, Mozzoni P, Vanni S, Vettori M, Broeckaert F, Bernard A, Mutti A. Polymorphism of quinone-metabolizing enzymes and susceptibility to ozone-induced acute effects. Am J Respir Crit Care Med 2001;163:1426–1431. [DOI] [PubMed] [Google Scholar]
- 30.Gilliland F, Li Y, Saxon A, Diaz-Sanchez D. Effect of glutathione-S-transferase M1 and P1 genotypes on xenobiotic enhancement of allergic responses: randomised, placebo-controlled crossover study. Lancet 2004;363:119–125. [DOI] [PubMed] [Google Scholar]
- 31.Kabesch M, Hoefler C, Carr D, Leupold W, Weiland SK, von Mutius E. Glutathione S transferase deficiency and passive smoking increase childhood asthma. Thorax 2004;59:569–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tamer L, Ercan B, Camsari A, Yildirim H, Cicek D, Sucu N, Ates NA, Atik U. Glutathione S-transferase gene polymorphism as a susceptibility factor in smoking-related coronary artery disease. Basic Res Cardiol 2004;99:223–229. [DOI] [PubMed] [Google Scholar]
- 33.Haendeler J, Hoffmann J, Zeiher AM, Dimmeler S. Antioxidant effects of statins via S-nitrosylation and activation of thioredoxin in endothelial cells: a novel vasculoprotective function of statins. Circulation 2004;110:856–861. [DOI] [PubMed] [Google Scholar]
- 34.Albert MA, Danielson E, Rifai N, Ridker PM. Effect of statin therapy on C-reactive protein levels: the Pravastatin Inflammation/CRP Evaluation (PRINCE): a randomized trial and cohort study. JAMA 2001;286:64–70. [DOI] [PubMed] [Google Scholar]
- 35.Sanguigni V, Pignatelli P, Caccese D. Atorvastatin decreases platelet superoxide anion production in hypercholesterolemic patients. Eur Heart J 2002;4:372. [Google Scholar]
- 36.Kaesemeyer WH, Caldwell RB, Huang J, Caldwell RW. Pravastatin sodium activates endothelial nitric oxide synthase independent of its cholesterol-lowering actions. J Am Coll Cardiol 1999;33:234–241. [DOI] [PubMed] [Google Scholar]
- 37.Li W, Asagami F, McTaggart F, Tasao P. Rosuvastatin inhibits monocyte/endothelial interactions in APOE (-1/-1) mice. Int J Clin Pract 2002;24:5. [Google Scholar]
- 38.Bell B, Rose C, Damon A. The normative aging study: an interdisciplinary and longitudinal study of health and aging. Aging Hum Dev 1972;3:4–17. [Google Scholar]
- 39.Task force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Eur Heart J 1996;17:354–381. [PubMed] [Google Scholar]
- 40.Allen G, Sioutas C, Koutrakis P, Reiss R, Lurmann FW, Roberts PT. Evaluation of the TEOM method for measurement of ambient particulate mass in urban areas. J Air Waste Manag Assoc 1997;47:682–689. [DOI] [PubMed] [Google Scholar]
- 41.Kalkstein L, Valamont K. An evaluation of summer discomfort in the United States using a relative climatological index. Bull Am Meteorol Soc 1986;67:842–848. [Google Scholar]
- 42.Rhoden C, Lawrence J, Godleski J, Gonzalez-Flecha B. N acetylcysteine prevents lung inflammation after short-term inhalation exposure to concentrated ambient particles. Toxicol Sci 2004;79:296–303. [DOI] [PubMed] [Google Scholar]
- 43.van Eeden SF, Tan WC, Suwa T, Mukae H, Terashima T, Fujii T, Qui D, Vincent R, Hogg JC. Cytokines involved in the systemic inflammatory response induced by exposure to particulate matter air pollutants (PM10). Am J Respir Crit Care Med 2001;164:826–830. [DOI] [PubMed] [Google Scholar]
- 44.Stone V, Tuinman M, Vamvakopoulos JE, Shaw J, Brown D, Petterson S, Faux SP, Borm P, MacNee W, Michaelangeli F, et al. Increased calcium influx in a monocytic cell line on exposure to ultrafine carbon black. Eur Respir J 2000;15:297–303. [DOI] [PubMed] [Google Scholar]
- 45.Dvonch JT, Brook RD, Keeler GJ, Rajagopalan S, D'Alecy LG, Marsik FJ, Morishita M, Yip FY, Brook JR, Timm EJ, et al. Effects of concentrated fine ambient particles on rat plasma levels of asymmetric dimethylarginine. Inhal Toxicol 2004;16:473–480. [DOI] [PubMed] [Google Scholar]
- 46.Aronson D, Mittleman MA, Burger AJ. Interleukin-6 levels are inversely correlated with heart rate variability in patients with decompensated heart failure. J Cardiovasc Electrophysiol 2001;12:294–300. [DOI] [PubMed] [Google Scholar]
- 47.Chowdhary S, Ng GA, Nuttall SL, Coote JH, Ross HF, Townend JN. Nitric oxide and cardiac parasympathetic control in human heart failure. Clin Sci (Lond) 2002;102:397–402. [PubMed] [Google Scholar]
- 48.Rodenbaugh DW, Collins HL, Nowacek DG, DiCarlo SE. Increased susceptibility to ventricular arrhythmias is associated with changes in Ca2+ regulatory proteins in paraplegic rats. Am J Physiol Heart Circ Physiol 2003;285:H2605–H2613. [DOI] [PubMed] [Google Scholar]
- 49.Mitchell LB, Powell JL, Gillis AM, Kehl V, Hallstron AP, Investigators AVID. Are lipid-lowering drugs also antiarrhythmic drugs? An analysis of the Antiarrhythmics versus Implantable Defibrillators (AVID) trial. J Am Coll Cardiol 2003;42:81–87. [DOI] [PubMed] [Google Scholar]
- 50.Welzig CM, Shin DG, Park HJ, Kim YJ, Saul JP, Galper JB. Lipid lowering by pravastatin increases parasympathetic modulation of heart rate: Galpha(i2), a possible molecular marker for parasympathetic responsiveness. Circulation 2003;108:2743–2746. [DOI] [PubMed] [Google Scholar]
- 51.Pelat M, Dessy C, Massion P, Desager JP, Feron O, Balligand JL. Rosuvastatin decreases caveolin-1 and improves nitric oxide dependent heart rate and blood pressure variability in apolipoprotein E−/− mice in vivo. Circulation 2003;107:2480–2486. [DOI] [PubMed] [Google Scholar]
- 52.Lee TM, Chou TF, Tsai CH. Effects of pravastatin on cardiomyocyte hypertrophy and ventricular vulnerability in normolipidemic rats after myocardial infarction. J Mol Cell Cardiol 2003;35:1449–1459. [DOI] [PubMed] [Google Scholar]
- 53.Sarnat J, Brown K, Schwartz J, Coull B, Koutrakis P. Relationships among personal exposures and ambient concentrations of particulate and gaseous pollutants and their implications for particle health effects studies. Epidemiology 2005;16:385–395. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.