Abstract
Rationale: Repeated, short-term exposures to ozone (O3) lead to attenuation of the acute lung function and airway inflammatory responses seen after a single exposure in healthy subjects, but it is unclear whether these acute responses also attenuate in subjects with asthma. Objective: To address this question by exposing 14 subjects with asthma to 0.2 ppm O3 for either 4 hours on a single day or 4 hours on 4 consecutive days (multiday [MD]). At least 3 weeks later, subjects underwent the alternate exposure. Methods: Spirometry was performed immediately pre- and postexposure and bronchoalveolar lavage (BAL) was obtained 18 hours after each exposure. Main Results: The decrease in FEV1 was greatest across Day 2 of the MD (MD2) exposure and then gradually declined on successive days of the MD exposure (mean ± SD decrease in FEV1 of 25.4 ± 18.0% across MD2 compared with 4.2 ± 6.5% across MD4). Respiratory symptoms followed a similar pattern to that of FEV1. Although the concentration of neutrophils in BAL after the MD4 exposure was not significantly different from that after the single-day exposure (1.7 ± 1.3 × 104 cells/ml vs. 1.2 ± 0.8 × 104 cells/ml, p = 0.20), the concentration of alveolar macrophages did significantly increase in BAL after the MD exposure (19.9 ± 9.7 × 104 cells/ml after MD4 vs. 12.1 ± 6.4 × 104 cells/ml after the single day). Conclusions: Alveolar macrophages are recruited to the airways of subjects with asthma with repeated short-term exposures to O3, suggesting a possible role for these cells in the chronic response to oxidant-induced injury.
Keywords: airway inflammation, alveolar macrophage, asthma, multiday exposure, ozone
Ozone (O3), a highly reactive oxidizing agent, is a major component of urban air pollution worldwide. Multiple controlled human exposure studies have documented that short-term inhalation of O3 causes dose-dependent decrements in lung function (1–4) as well as injury and inflammation in both proximal airways and distal lung (5–8). Repeated, daily short-term exposures to O3 lead to attenuation of both acute lung function responses and bronchoalveolar lavage (BAL) neutrophilia in healthy persons without asthma (9–12). However, the results of several studies have also suggested that there is a lack of attenuation of airway injury and neutrophilic infiltration of bronchial mucosa with repeated, short-term exposures (11, 12).
Subjects with asthma may be at higher risk of experiencing adverse effects after O3 exposure than healthy subjects without asthma because of underlying airway inflammation and airway hyperresponsiveness (13–15). Given that persons with asthma constitute a large, potentially vulnerable subpopulation, assessing their responses to O3 is highly relevant to our biological understanding of the effects of inhaled oxidants and from a public health policy perspective. The results of several epidemiologic studies indicate that high-ambient O3 concentrations are associated with increased rates of asthma attacks, emergency room visits, and hospital admissions for asthma exacerbation (16–19). In addition, several controlled exposure studies have shown that, although subjects with mild asthma had similar lung function changes after short-term O3 exposure to those of healthy subjects without asthma, they had greater airway inflammatory responses (20–23). Thus, it appears that subjects with asthma constitute a susceptible subgroup at risk for both O3-induced exacerbations and enhanced airway inflammatory responses.
To our knowledge, however, there are no data on whether O3-induced acute inflammatory responses in subjects with asthma persist or attenuate with repeated exposures similar to healthy subjects without asthma. This is a key issue given the potential for chronic lung injury and tissue remodeling from repeated episodes of acute inflammation. Our study was designed to test the hypothesis that repeated daily exposures to O3 cause a progression of airway inflammation in subjects with asthma. Some of the results of this study have been previously reported in the form of an abstract (24).
METHODS
Study Design
This study had a crossover design. Subjects with mild asthma were exposed to 0.2 ppm O3 for either 4 hours on a single day (1-D) or 4 hours on 4 consecutive days (multiday [MD] exposure) followed by bronchoscopy 18 hours later. At least 3 weeks later, to allow recovery from any inflammation or injury caused by the first exposure and bronchoscopy, subjects underwent the alternate exposure (either 1-D or MD exposure to 0.2 ppm O3), again followed by bronchoscopy. The order of exposures within the group was counterbalanced and randomized to the extent possible.
Subjects
Subjects were initially recruited for this study by public advertisements. Inclusion criteria were as follows: self-report of physician-diagnosed asthma, airway hyperresponsiveness to inhaled methacholine (provocative concentration of methacholine resulting in a 20% decrease in FEV1 compared with baseline [PC20] ⩽ 8.0 mg/ml) verified in our laboratory according to a standard protocol (25), and ability to perform moderately strenuous exercise. All subjects were nonsmokers who denied any history of cardiac or pulmonary diseases other than asthma or any respiratory infections within 6 weeks of the onset of each exposure. In addition, all subjects were atopic, although atopy was not an inclusion criterion in our study. They were required to be off oral steroid medications for at least 3 months and inhaled steroids for at least 2 weeks before all sessions. No other medications were withheld. No subject used supplemental vitamin C or E during the study. The subjects were informed of the risks of the experimental protocol and signed a consent form approved by the Committee on Human Research of the University of California, San Francisco. All of the subjects received financial compensation for their participation. Fourteen subjects completed the experimental protocol. Characteristics of individual study participants are listed in Table 1.
TABLE 1.
Subject characteristics
| Subject No. | Sex | Age (yr) |
BMI (kg/m2) |
FEV1† (L) |
FEV1† (% predicted) |
PC20‡ (mg/ml) |
Medications |
|---|---|---|---|---|---|---|---|
| 1 | M | 37 | 28.4 | 3.52 | 108 | 7.48 | B |
| 2 | F | 28 | 22.0 | 3.52 | 110 | 1.92 | B, AH |
| 3 | F | 33 | 31.3 | 2.67 | 97 | 0.13 | B, AH, NS |
| 4 | M | 28 | 25.4 | 5.08 | 109 | 0.49 | B, ICS, AH |
| 5 | M | 18 | 18.7 | 3.64 | 87 | 0.45 | — |
| 6 | F | 45 | 32.6 | 2.64 | 95 | 3.68 | B, ICS |
| 7 | M | 34 | 27.5 | 3.57 | 96 | 3.48 | B |
| 8 | F | 18 | 26.5 | 2.53 | 84 | 2.54 | — |
| 9 | F | 19 | 24.5 | 3.77 | 98 | 0.40 | B, LTI |
| 10 | F | 33 | 28.4 | 3.23 | 114 | 2.95 | B, NS |
| 11 | F | 29 | 19.2 | 2.43 | 80 | 0.04 | B |
| 12 | M | 20 | 32.4 | 3.82 | 89 | 6.25 | B |
| 13 | F | 23 | 18.6 | 3.40 | 105 | 4.42 | ICS |
| 14 | M | 27 | 23.8 | 3.90 | 80 | 0.80 | B |
| Mean* | 28.0 | 25.6 | 3.42 | 96.6 | 2.50 | ||
| SD | 8.0 | 4.8 | 0.70 | 11.4 | 2.36 |
Definition of abbreviations: AH = antihistamines (nonsedating); B = β-agonist metered dose inhalers; BMI = body mass index; F = female; ICS = inhaled corticosteroids; LTI = leukotriene inhibitors; M = male; NS = nasal steroids.
n = 14.
The best effort of the three trials of spirometry performed during the initial subject characterization visit.
Concentration of methacholine required to produce a 20% decrease in FEV1 from baseline calculated by log linear interpolation.
Experimental Protocol
Baseline spirometry, methacholine challenge test, and a 15-minute exercise test designed to determine a workload that generated the target expired minute ventilation (V̇e) of 25 L/minute/m2 body surface area were completed on an initial screening visit. Atopic status was assessed by skin-prick testing to 10 common aeroallergens (Dermatophagoides pteronyssinus, Aspergillus fumigatus, birch mix, Chinese elm, cat, dog, mountain cedar, mugwort sage, olive tree, perennial rye), with histamine as a positive control and saline as a negative control. A positive response was defined by a skin weal larger than 2 mm after 15 minutes.
On exposure days, each subject's spirometry and peak expiratory flow were measured immediately before and after each exposure. Spirometry was performed on a dry rolling-seal spirometer. The best values for FVC and FEV1 were used from three acceptable FVC maneuvers (26) obtained approximately 30 seconds apart. The subjects exercised for the first 30 minutes of each hour and then rested for the remaining 30 minutes of the hour. The exercise consisted of either walking/running on a treadmill or pedaling a cycle ergometer. The exercise intensity was adjusted for each subject to achieve the targeted V̇e. During exercise, V̇e was calculated from Vt and breathing frequency, measured using a pneumotachograph, at the 10- and 20-minute intervals of each 30-minute exercise period. Peak expiratory flow was measured 10 minutes into each 30-minute rest period to monitor for possible bronchoconstriction. Subjects remained inside the chamber for the entire 4-hour exposure period.
Exposure Chamber and Atmospheric Monitoring
All exposures took place in a chamber ventilated with filtered air at 20°C and 50% relative humidity, to which O3 was added. The stainless steel and glass chamber, 2.5 × 2.5 × 2.4 m, was custom-built and designed to maintain chamber temperature and relative humidity within 2.0°C and 4%, respectively, of the set points (5). Relative humidity and temperature were recorded every 30 seconds and averaged over each exposure.
O3 was produced using a corona-discharge O3 generator (Model T408; Polymetrics, Inc., San Jose, CA) and its concentration was monitored every 30 seconds with an ultraviolet light photometer (Model 1004AH; Dasibi, Glendale, CA). The O3 analyzer was calibrated with an O3 transfer standard by the California Air Resources Board.
Respiratory Symptoms
A self-administered symptom questionnaire was completed immediately before and immediately after each exposure. The symptom questionnaire consists of a 5-point rating scale (0 = none and 4 = severe) for 12 symptoms, including lower respiratory (chest discomfort/tightness, chest pain on deep inspiration, shortness of breath, cough, phlegm or sputum production, and wheezing), upper respiratory (throat irritation and nasal irritation), and nonrespiratory (anxiety, eye irritation, headache, and nausea) symptoms.
Bronchoscopy and Lavage Procedures
Bronchoscopies were performed 18 ± 2 hours after the 1-D exposure and after the MD Day 4 (MD4) exposure. The 18 ± 2–hour postexposure time was chosen because previous studies by both our laboratory and other investigators have documented the presence of an O3-induced inflammatory response in many subjects at this time point (5, 6, 27). Our laboratory's procedures of bronchoscopy and BAL have been previously discussed in detail (5, 27). Briefly, intravenous access was established, supplemental O2 was delivered, and the upper airways were anesthetized with topical lidocaine. Sedation with intravenous midazolam and fentanyl was used as needed for subject comfort. The bronchoscope was introduced through the mouth and vocal cords into the airways. The bronchoscope was then directed into the right middle lobe where lavage was performed with two 50-ml aliquots of 0.9% saline warmed to 37°C. The first 15 ml of fluid returned from the first 50-ml aliquot was collected separately and designated bronchial fraction (BFx), whereas the remaining fluid returned was designated BAL. Both lavage samples were immediately put on ice. Multiple endobronchial biopsies were obtained from segmental orifices for potential immunohistochemical analyses of cellular infiltration and protein expression. After bronchoscopy, each subject was observed for an approximate 2-hour recovery period.
Total cells were counted on uncentrifuged aliquots of BFx and BAL using a hemocytometer. Differential cell counts were obtained from slides prepared using a cytocentrifuge, 25 × g for 5 minutes, and stained with Diff-Quik (Dade Behring, Düdingen, Switzerland) as previously described (27). Cells were counted by two independent observers; the average of the two counts was used in data analysis. BFx and BAL fluids were then centrifuged at 180 × g for 15 minutes, and the supernatant was separated and recentrifuged at 1,200 × g for 15 minutes to remove any cellular debris before freezing at −80°C.
Measurement of Biochemical Constituents of BFx and BAL Supernatants
Biochemical assays were performed on BFx and BAL supernatants that had been frozen at −80°C from 13 subjects. Two markers of neutrophilic inflammation, interleukin 8 (IL-8) and myeloperoxidase, and one marker of acute phase reaction, IL-6, were measured with commercially available immunoassays (R&D Systems, Minneapolis, MN). Total protein was measured using the BCA Protein Assay kit (Pierce, Rockford, IL).
Statistical Analysis
All data were entered into a database developed in Microsoft Access 2000 (Microsoft, Redmond, WA). Processed data were then analyzed using Stata 7.0 software (StataCorp, College Station, TX).
For the analysis of spirometric responses to O3 across each exposure, we performed paired Student's t tests using preexposure minus postexposure values. For the analysis of symptoms (a categoric outcome variable) across each exposure, we performed Wilcoxon's signed-rank tests. Correlation of respiratory symptoms and FEV1 was evaluated using the Spearman coefficient. To compare cell counts and biochemical constituents between the lavage fluids obtained after 1-D and MD4, we also used paired Student's t tests. For the analysis of spirometric and respiratory symptom data among different exposure days, we performed a multivariable linear regression that included random subject effects to account for clustering by subject (repeated measures) in the model. A p value of 0.05 was considered statistically significant in all data analyses.
The sample size for this study was calculated on the basis of our laboratory's previous data for O3 exposure in subjects with asthma (21). Single-day O3 exposure results in neutrophilia of 23.6 ± 14.3 and 10.7 ± 8.0% (mean ± SD) in BFx and BAL, respectively. Our null hypothesis was that, similar to healthy subjects without asthma (11), the neutrophilia would attenuate toward levels seen after filtered air exposure (mean ± SD: 6.6 ± 11.9 and 3.3 ± 1.2% in BFx and BAL, respectively) (21). The alternate hypothesis was that MD exposure to O3 would result in continued neutrophilia in BFx and BAL at least at the same level as 1-D exposure. On the basis of these numbers, and for a two-sided type I error of 0.05 and power of 0.8, the sample size would be 8 and 12 subjects for the outcomes of BFx and BAL neutrophilia, respectively. We chose a conservative sample size of 14.
RESULTS
Exposure Data
Mean O3 concentrations were not significantly different from each other on any exposure day (mean ± SD: 0.208 ± 0.005 ppm for 1-D exposure and 0.209 ± 0.005 ppm on the 4 days of MD exposures). The subjects' exercise V̇e was not different between 1-D and MD1 exposures (mean ± SD: 41.3 ± 7.2 vs. 41.3 ± 8.2 L, respectively). V̇e, however, decreased slightly on MD2 exposure (40.6 ± 7.4 L), and then increased slightly on MD3 and MD4 exposures (43.7 ± 7.0 L on MD4). The median time interval between exposure arms (1-D and MD) was 41 days (interquartile range, 31–90 days). The exposure order had no effect on any outcome variable in the multivariable regression models.
Spirometry
The preexposure values for, and the changes across exposure in, FVC, FEV1, maximal midexpiratory flow rate (FEF25–75), and FEF after 75% of expelled volume (FEF75) are shown in Table 2. There were no statistically significant differences in any of these values between the 1-D and MD1 exposures.
TABLE 2.
Spirometric values before and after each ozone exposure
| Spirometry (n = 14) | Preexposure | Postexposure | Change | p Value§ |
|---|---|---|---|---|
| FVC, L* | ||||
| 1-D | 4.2 ± 1.0 | 3.7 ± 0.8 | −0.4 ± 0.4 | 0.001 |
| MD1 | 4.2 ± 1.0 | 3.6 ± 0.7 | −0.6 ± 0.5 | 0.001 |
| MD2 | 4.1 ± 0.8 | 3.2 ± 0.8 | −0.9 ± 0.7‡ | 0.001 |
| MD3 | 4.0 ± 0.8 | 3.5 ± 1.0 | −0.5 ± 0.5 | 0.004 |
| MD4 | 4.0 ± 0.8 | 3.9 ± 0.9 | −0.1 ± 0.2‡ | 0.036 |
| FEV1, L* | ||||
| 1-D | 3.5 ± 0.7 | 3.0 ± 0.6 | −0.5 ± 0.4 | 0.001 |
| MD1 | 3.4 ± 0.8 | 2.8 ± 0.6 | −0.6 ± 0.6 | 0.002 |
| MD2 | 3.3 ± 0.6 | 2.4 ± 0.7 | −0.9 ± 0.7‡ | 0.000 |
| MD3 | 3.2 ± 0.7 | 2.7 ± 0.9 | −0.5 ± 0.5 | 0.004 |
| MD4 | 3.3 ± 0.7 | 3.2 ± 0.7 | −0.1 ± 0.2‡ | 0.017 |
| FEF25–75, L/s† | ||||
| 1-D | 3.6 ± 1.1 | 2.9 ± 0.9 | −0.7 ± 0.9 | 0.012 |
| MD1 | 3.5 ± 1.4 | 2.5 ± 0.8 | −0.9 ± 1.2 | 0.010 |
| MD2 | 3.3 ± 1.0 | 2.2 ± 1.0 | −1.1 ± 0.8 | 0.000 |
| MD3 | 3.3 ± 1.2 | 2.7 ± 1.2 | −0.7 ± 0.8 | 0.011 |
| MD4 | 3.4 ± 1.2 | 3.3 ± 1.2 | −0.1 ± 0.4‡ | 0.271 |
| FEF75, L/s† | ||||
| 1-D | 1.7 ± 0.5 | 1.3 ± 0.4 | −0.4 ± 0.5 | 0.011 |
| MD1 | 1.7 ± 0.7 | 1.2 ± 0.4 | −0.5 ± 0.5 | 0.001 |
| MD2 | 1.5 ± 0.5 | 1.0 ± 0.4 | −0.5 ± 0.5 | 0.001 |
| MD3 | 1.6 ± 0.6 | 1.2 ± 0.5 | −0.3 ± 0.5 | 0.026 |
| MD4 | 1.6 ± 0.6 | 1.6 ± 0.6 | 0.0 ± 0.2‡ | 0.503 |
Definition of abbreviations: 1-D = single-day exposure; FEF25–75 = maximal midexpiratory flow rate; FEF75 = FEF after 75% of expelled volume; MD = multiday exposure.
Values shown are mean ± SD.
p < 0.001 for the association between exposure day and the pre- to postexposure change in spirometric parameters based on multivariable regression analyses.
p < 0.005 for the association between exposure day and the pre- to postexposure change in spirometric parameters based on multivariable regression analyses.
p < 0.05 for comparisons with 1-D in these regression models.
p values for paired Student's t test between pre- and postexposure measurements.
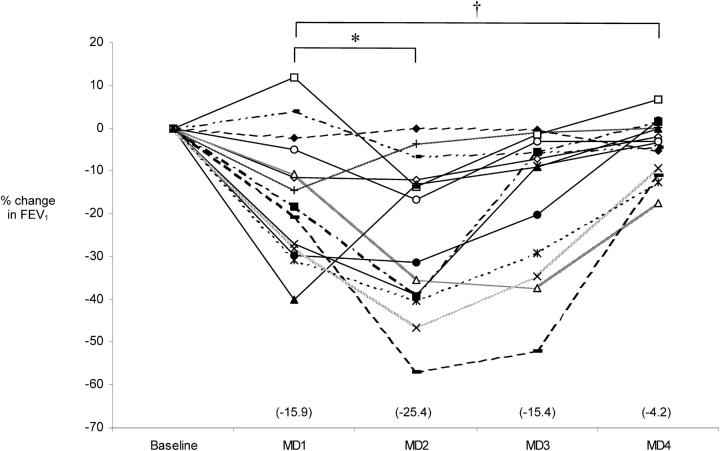
O3 exposure caused a significant decrease in FVC and FEV1 across all exposure days (Table 2). The largest decrease occurred across the MD2 exposure (25.4 ± 18.0% in FEV1). After MD2, the decreases in these values across exposures attenuated, and by MD4, the decreases were small. The FEF25–75 and FEF75 also followed a similar pattern of changes (Table 2). The percentage changes in FEV1 values across each exposure of the MD arm for each subject are shown in Figure 1.
Figure 1.
The percentage of change in FEV1 across consecutive days of ozone exposure. Scatterplot representation of percentage decrease in FEV1 across each exposure of multiday (MD) arm of experiment (MD1–MD4). Mean values are presented in parentheses for each day. *p = 0.016 and †p = 0.003 for comparisons with MD1 based on multivariable regression analysis.
Symptoms
The subjects had a worsening of their lower respiratory tract symptoms (based on the eight symptoms of chest discomfort/tightness, chest pain on deep inspiration, shortness of breath, cough, phlegm or sputum production, and wheezing) after exposure to O3 (Table 3). Symptoms were greatest after 1-D, MD1, and MD2 exposures and decreased gradually with consecutive days of exposure; by MD4, there was no significant difference between the pre- and postexposure symptoms. This pattern of change in lower respiratory symptoms correlated closely with change in FEV1 (Spearman R = 0.80). There were no significant changes in the upper respiratory (throat irritation and nasal irritation) or in nonrespiratory (anxiety, eye irritation, headache, and nausea) symptoms.
TABLE 3.
Respiratory and nonrespiratory symptoms with single-day and multiday ozone exposures
| Symptoms (n = 14) | Preexposure | Postexposure | p Value† |
|---|---|---|---|
| Lower respiratory* | |||
| 1-D | 0.0 (0.0, 0.5) |
0.7 (0.2, 1.5) |
0.012 |
| MD1 | 0.2 (0.0, 0.3) |
0.9 (0.3, 2.3) |
0.001 |
| MD2 | 0.3 (0.0, 0.5) |
1.3 (0.5, 2.2) |
0.001 |
| MD3 | 0.3 (0.0, 1.0) |
0.7 (0.2, 1.3) |
0.229 |
| MD4 | 0.3 (0.2, 0.8) |
0.4 (0.0, 0.7) |
0.950 |
| Upper respiratory | |||
| 1-D | 0.0 (0.0, 1.0) |
0.0 (0.0, 1.0) |
0.377 |
| MD1 | 0.0 (0.0, 1.0) |
0.8 (0.5, 1.0) |
0.112 |
| MD2 | 0.3 (0.0, 0.5) |
0.5 (0.0, 1.5) |
0.072 |
| MD3 | 0.3 (0.0, 1.0) |
0.5 (0.0, 1.0) |
0.760 |
| MD4 | 0.3 (0.0, 0.5) |
0.0 (0.0, 1.0) |
0.502 |
| Nonrespiratory | |||
| 1-D | 0.1 (0.0, 0.5) |
0.0 (0.0, 0.3) |
0.424 |
| MD1 | 0.1 (0.0, 0.3) |
0.1 (0.0, 0.8) |
0.249 |
| MD2 | 0.0 (0.0, 0.5) |
0.1 (0.0, 0.5) |
0.633 |
| MD3 | 0.1 (0.0, 0.5) |
0.1 (0.0, 0.3) |
0.381 |
| MD4 | 0.0 (0.0, 0.5) |
0.1 (0.0, 0.3) |
0.811 |
Definition of abbreviations: 1-D = single-day exposure; MD = multiday exposure.
Values shown are median (interquartile range) scores for each symptom group. The subjects scored their symptoms from a minimum of 0 (no symptoms) to a maximum of 4 before and after each exposure. The upper respiratory and nonrespiratory symptom changes were not significantly associated with exposure day.
p = 0.001 for the association between exposure day and the pre- to postexposure change in lower respiratory symptoms based on multivariable regression analysis.
p values for paired Wilcoxon's signed-rank test between pre- and postexposure measurements.
Lavage Cell Counts
Lavage cell count data are shown in Table 4. The concentration of neutrophils in both BFx and BAL fluid was elevated as expected after 1-D exposure compared with historical filtered-air control data from our laboratory (28). After MD4 exposure, the concentration of neutrophils in BFx and BAL tended to decrease (from [mean ± SD] 4.5 ± 4.5 and 1.7 ± 1.3 × 104 cells/ml after 1-D exposure to 2.9 ± 2.3 and 1.2 ± 0.8 × 104 cells/ml after MD4 exposure in BFx and BAL, respectively). These decreases, however, were not statistically significant. The concentration of total leukocytes in BFx and BAL fluid increased 25 and 49%, respectively, after MD4 exposure compared with 1-D exposure. This increase in concentration of leukocytes was primarily due to the increase in the concentration of alveolar macrophages in the lavage fluid (an increase of 57 and 64% in BFx and BAL, respectively). These alveolar macrophages were large with granular cytoplasm, appearing “foamy” under light microscopy (data not shown), suggestive of intense metabolic activity (29).
TABLE 4.
Leukocyte cell counts in lavage samples after exposures
| Samples (n = 14) | Normal Values* | 1-D | MD4 | p Value |
|---|---|---|---|---|
| BFx (× 104 cells/ml) | ||||
| WBC | 15.3 ± 8.7 | 17.4 ± 9.7 | 21.7 ± 7.6 | 0.073 |
| AM | 13.9 ± 8.8 | 10.8 ± 5.3 | 17.0 ± 6.5 | 0.004 |
| PMN | 1.0 ± 2.2 | 4.5 ± 4.5 | 2.9 ± 2.3 | 0.155 |
| EOS | 0.11 ± 0.20 | 0.18 ± 0.25 | 0.18 ± 0.21 | 0.977 |
| LMP | 0.3 ± 0.3 | 1.9 ± 1.4 | 1.7 ± 1.04 | 0.289 |
| BAL (× 104 cells/ml) | ||||
| WBC | 15.9 ± 10.5 | 15.6 ± 7.3 | 23.2 ± 10.4 | 0.013 |
| AM | 15.0 ± 10.3 | 12.1 ± 6.4 | 19.9 ± 9.7 | 0.005 |
| PMN | 0.50 ± 0.27 | 1.7 ± 1.3 | 1.2 ± 0.8 | 0.204 |
| EOS | 0.15 ± 0.06 | 0.14 ± 0.14 | 0.16 ± 0.15 | 0.743 |
| LMP | 0.3 ± 0.3 | 1.7 ± 0.9 | 1.9 ± 0.7 | 0.471 |
Definition of abbreviations: 1-D = single-day O3 exposure; AM = alveolar macrophage; BAL = bronchoalveolar lavage; BFx = bronchial fraction; EOS = eosinophil; LMP = lymphocyte; MD4 = multiday O3 exposure; PMN = neutrophil; WBC = leukocyte.
The concentration of total and differential leukocytes in BFx (the first 15-ml return of the lavage sample), and BAL (the remainder of the lavage return) after instillation of a total of 100 ml of normal saline into the right middle lobe. Values shown are mean ± SD. p values are for paired Student's t test between 1-D and MD4 measurements.
Values obtained in a previous study of 13 filtered-air–exposed, nonsmoking subjects with asthma in our laboratory (28).
Lavage Biochemical Constituents
Several biochemical markers of inflammation (IL-6, IL-8, and myeloperoxidase) were measured in the lavage fluid. There was no significant difference in the concentration of IL-6, IL-8, or myeloperoxidase in either BFx or BAL after MD4 exposure compared with that after 1-D exposure, although the concentrations of these markers were elevated compared with those of historical control subjects exposed to filtered air in our laboratory (see Table 5). The total protein concentration was elevated (compared with that of historical control subjects exposed to filtered air in our laboratory [30]) after 1-D exposure in both BFx and BAL and remained elevated after MD4 exposure in BAL fluid (mean ± SD: 171.8 ± 74.5 and 123.7 ± 62.2 μg/ml in BFx [p = 0.025] and 195.8 ± 93.4, and 176.5 ± 82.5 μg/ml in BAL [p = 0.205] after 1-D and MD4, respectively; normal values from filtered-air–exposed historical control subjects: 101.0 ± 67.0 and 147.2 ± 33.6 μg/ml in BFx and BAL, respectively).
TABLE 5.
Inflammatory marker concentrations in lavage samples after single-day and multiday ozone exposures
| Samples (n = 13) | Normal Values* | 1-D | MD4 | p Value |
|---|---|---|---|---|
| BFx | ||||
| IL-6, pg/ml | 5.2 ± 4.9 | 6.0 ± 3.7 | 5.5 ± 6.7 | 0.740 |
| IL-8, pg/ml | 24.3 ± 21.4 | 49.1 ± 28.6 | 61.8 ± 58.1 | 0.752 |
| MPO, ng/ml | N/A | 42.9 ± 31.9 | 43.2 ± 24.0 | 0.970 |
| BAL | ||||
| IL-6, pg/ml | 3.8 ± 3.1 | 4.5 ± 4.1 | 3.1 ± 2.0 | 0.083 |
| IL-8, pg/ml | 20.7 ± 32.4 | 23.1 ± 19.1 | 26.9 ± 39.7 | 0.895 |
| MPO, ng/ml | 4.2 ± 1.8 | 18.0 ± 13.5 | 17.3 ± 25.5 | 0.898 |
Definition of abbreviations: 1-D = single-day O3 exposure; BAL = bronchoalveolar lavage; BFx = bronchial fraction; IL = interleukin; MD4 = multiday O3 exposure; MPO = myeloperoxidase; N/A = not available.
The concentration of IL-6, IL-8, and MPO in BFx (the first 15-ml return of the lavage sample) and BAL (the remainder of the lavage return) after instillation of a total of 100 ml of normal saline into the right middle lobe. Values shown are mean ± SD. p values are for paired Student's t test between 1-D and MD4 measurements.
Values obtained in previous studies of filtered-air–exposed, nonsmoking subjects with asthma in our laboratory (28, 46).
DISCUSSION
Contrary to our study hypothesis, we found that short-term O3 exposures on 4 consecutive days did not result in enhancement of the acute neutrophilic response in subjects with asthma seen after a single short-term exposure. In fact, similar to previous reports in subjects without asthma (11, 12), there was some attenuation of lavage neutrophilia in our subjects with asthma after MD exposure; however, this change did not reach statistical significance. The most striking finding, however, was that MD exposure resulted in a marked increase in the number of alveolar macrophages in lavage fluid beyond what is seen after 1-D exposure. In addition, we found that the severity of lower respiratory tract symptoms followed a similar pattern of spirometric values with an initial worsening and then subsequent improvement in our subjects with asthma.
Inhaled O3 at high ambient concentrations can induce recruitment of neutrophils into the airway lumen, resulting in an increase in both the concentration and percentage of neutrophils in the respiratory tract lining fluid (RTLF). Many other irritants as well as viral infections that can cause asthma exacerbation also induce an initial neutrophilia in RTLF (31–33). Our hypothesis was that repeated short-term exposure to oxidative injury by O3 would cause augmentation of this RTLF neutrophilia, which may in turn result in asthma exacerbation. Our previous data from healthy individuals without asthma using an identical MD O3-exposure protocol showed an attenuation of RTLF neutrophilia (11). In this experiment, we expected the subjects with asthma to respond differently because they are an especially susceptible group with preexisting airway inflammation and increased airway oxidative burden (13–15, 34). The response of individuals with asthma to MD O3 exposure may indeed be different from that of individuals without asthma because we observed no significant attenuation of RTLF neutrophilia in our subjects. It is important to note that, although we showed no progression of RTLF neutrophilia with MD O3 exposure, progressive oxidative injury or inflammation might still be occurring in the airways given that we and others have observed persistent elevated concentrations of markers of injury and inflammation in RTLF (11, 12, 35, 36).
Despite the epidemiologic findings of increased rates of asthma exacerbation with episodes of air pollution (16–19), repeated short-term exposures appeared to blunt the effect of O3 on respiratory symptoms in our study. After the initial worsening of respiratory symptoms across MD1 exposure (similar to 1-D exposure), the subjects' symptoms gradually improved starting with MD3 exposure, and by MD4, the subjects had no change in symptoms across the exposure, indicating the development of a sort of “tolerance” toward the O3-induced oxidative injury. The close correlation between respiratory symptoms and the change in FEV1 suggests that the increase in acute asthma exacerbations observed after O3 exposure may be related in part to decreases in spirometric values (37). In our previous study of healthy subjects without asthma, we found a similar pattern of respiratory symptoms and lung function changes (11), suggesting the possibility that increased symptomatic morbidity from acute O3 exposure in individuals with asthma may be related to lower baseline lung function. Thus, the acute O3-induced worsening of respiratory symptoms in individuals with asthma may be unrelated to the underlying eosinophilic airway inflammatory process often considered responsible for asthma exacerbations.
Perhaps the most intriguing finding in our experiment is the increase in the concentration of alveolar macrophages in RTLF with successive days of O3 exposure. As noted above, these macrophages demonstrate features associated with “activation,” including large cytoplasm with foamy, granular microscopic appearance (29). In our previous study of healthy subjects without asthma, we found a similar pattern of increase in the concentration of macrophages in BFx, but not in BAL (35% increase in concentration of alveolar macrophages in BFx [p < 0.05] vs. 7% decrease in BAL from 1-D to MD4 exposure) (11). An increase in RTLF alveolar macrophages with recurrent O3 exposures also has been previously reported in some animal studies (35, 38, 39). Taken together, the data from the current study and from previous animal studies suggest that repeated oxidative injury can result in continued recruitment and activation of macrophages into the airways. In addition, the greater macrophage response in individuals with asthma may be due to their altered airway inflammatory response to oxidative injury (34, 40, 41).
These alveolar macrophages may either produce or prevent further oxidative injury. They may be involved in suppression of the initial O3-induced neutrophilic inflammation and/or may be directly involved in the antioxidant defense of the lungs. Recently, an alternative activation pathway of macrophages has gained attention, suggesting a possible role for alveolar macrophages in Th2 inflammatory responses, including asthma (42). In addition to increasing risk of asthma exacerbation, exposure to O3 has been shown to be a risk factor for new-onset asthma in children (43), and alveolar macrophages may play a role in these responses. In a previous study, we showed that chronic long-term exposure to O3 is associated with lower spirometric values in healthy individuals without asthma (44). The mechanisms of these chronic changes are not known, but likely involve airway remodeling. Alveolar macrophages have been implicated in airway remodeling processes (45) and thus may be involved in the long-term effects of O3-induced oxidative injury. Further research is necessary to elucidate the role of alveolar macrophages in both asthma and oxidative injury.
The major limitation of our study was the relatively small sample size. This is a generic problem in controlled human exposure studies involving bronchoscopy. Despite the small sample size, however, we still had adequate power to detect significant differences in several lavage endpoints between 1-D and MD exposures. Another limitation, again inherent in controlled exposure studies, is that we were only able to study subjects with relatively mild asthma.
In conclusion, alveolar macrophages are recruited to the airways of subjects with asthma with repeated short-term exposures to O3. On the other hand, neutrophil recruitment into the RTLF of these subjects did not increase with repeated exposures. O3-induced oxidative airway injury, however, may continue to occur, and persistence of such injury may lead to airway remodeling. Our results suggest the need for further investigation of the role of alveolar macrophages in oxidant-induced airway remodeling.
Acknowledgments
The authors thank Drs. Peter Bacchetti and David Glidden for their assistance with the statistical analysis and Robert Montanti for his assistance with bronchoscopy.
Supported by the National Institutes of Health (R01 ES08970 and M01RR00083–41), American Lung Association (Research Training Fellowship), and Chest Foundation (Clinical Research Training Grant).
Conflict of Interest Statement: None of the authors have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.Hazucha MJ. Relationship between ozone exposure and pulmonary function changes. J Appl Physiol 1987;62:1671–1680. [DOI] [PubMed] [Google Scholar]
- 2.Horstman DH, Folinsbee LJ, Ives PJ, Abdul-Salaam S, McDonnell WF. Ozone concentration and pulmonary response relationships for 6.6-hour exposures with five hours of moderate exercise to 0.08, 0.10, and 0.12 ppm. Am Rev Respir Dis 1990;142:1158–1163. [DOI] [PubMed] [Google Scholar]
- 3.McDonnell WF, Horstman DH, Hazucha MJ, Seal E Jr, Haak ED, Salaam SA, House DE. Pulmonary effects of ozone exposure during exercise: dose–response characteristics. J Appl Physiol 1983;54:1345–1352. [DOI] [PubMed] [Google Scholar]
- 4.Aris RM, Tager I, Christian D, Kelly T, Balmes JR. Methacholine responsiveness is not associated with O3-induced decreases in FEV1. Chest 1995;107:621–628. [DOI] [PubMed] [Google Scholar]
- 5.Aris R, Christian D, Tager I, Ngo L, Finkbeiner WE, Balmes JR. Effects of nitric acid gas alone or in combination with ozone on healthy volunteers. Am Rev Respir Dis 1993;148:965–973. [DOI] [PubMed] [Google Scholar]
- 6.Koren HS, Devlin RB, Graham DE, Mann R, McGee MP, Horstman DH, Kozumbo WJ, Becker S, House DE, McDonnell WF, et al. Ozone-induced inflammation in the lower airways of human subjects. Am Rev Respir Dis 1989;139:407–415. [DOI] [PubMed] [Google Scholar]
- 7.Schelegle ES, Siefkin AD, McDonald RJ. Time course of ozone-induced neutrophilia in normal humans. Am Rev Respir Dis 1991;143:1353–1358. [DOI] [PubMed] [Google Scholar]
- 8.Seltzer J, Bigby BG, Stulbarg M, Holtzman MJ, Nadel JA, Ueki IF, Leikauf GD, Goetzl EJ, Boushey HA. O3-induced change in bronchial reactivity to methacholine and airway inflammation in humans. J Appl Physiol 1986;60:1321–1326. [DOI] [PubMed] [Google Scholar]
- 9.Hackney JD, Linn WS, Mohler JG, Collier CR. Adaptation to short-term respiratory effects of ozone in men exposed repeatedly. J Appl Physiol 1977;43:82–85. [DOI] [PubMed] [Google Scholar]
- 10.Horvath SM, Gliner JA, Folinsbee LJ. Adaptation to ozone: duration of effect. Am Rev Respir Dis 1981;123:496–499. [DOI] [PubMed] [Google Scholar]
- 11.Christian DL, Chen LL, Scannell CH, Ferrando RE, Welch BS, Balmes JR. Ozone-induced inflammation is attenuated with multiday exposure. Am J Respir Crit Care Med 1998;158:532–537. [DOI] [PubMed] [Google Scholar]
- 12.Jorres RA, Holz O, Zachgo W, Timm P, Koschyk S, Muller B, Grimminger F, Seeger W, Kelly FJ, Dunster C, et al. The effect of repeated ozone exposures on inflammatory markers in bronchoalveolar lavage fluid and mucosal biopsies. Am J Respir Crit Care Med 2000;161:1855–1861. [DOI] [PubMed] [Google Scholar]
- 13.Balmes JR. The role of ozone exposure in the epidemiology of asthma. Environ Health Perspect 1993;101:219–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koenig JQ. Effect of ozone on respiratory responses in subjects with asthma. Environ Health Perspect 1995;103:103–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koren HS, Bromberg PA. Respiratory responses of asthmatics to ozone. Int Arch Allergy Immunol 1995;107:236–238. [DOI] [PubMed] [Google Scholar]
- 16.Bates DV, Sizto R. Air pollution and hospital admissions in southern Ontario: the acid summer haze effect. Environ Res 1987;43:317–331. [DOI] [PubMed] [Google Scholar]
- 17.Whittemore AS, Korn EL. Asthma and air pollution in the Los Angeles area. Am J Public Health 1980;70:687–696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Friedman MS, Powell KE, Hutwagner L, Graham LM, Teague WG. Impact of changes in transportation and commuting behaviors during the 1996 Summer Olympic Games in Atlanta on air quality and childhood asthma. JAMA 2001;285:897–905. [DOI] [PubMed] [Google Scholar]
- 19.Romieu I, Sienra-Monge JJ, Ramirez-Aguilar M, Tellez-Rojo MM, Moreno-Macias H, Reyes-Ruiz NI, del Rio-Navarro BE, Ruiz-Navarro MX, Hatch G, Slade R, et al. Antioxidant supplementation and lung functions among children with asthma exposed to high levels of air pollutants. Am J Respir Crit Care Med 2002;166:703–709. [DOI] [PubMed] [Google Scholar]
- 20.Balmes JR, Chen LL, Scannell C, Tager I, Christian D, Hearne PQ, Kelly T, Aris RM. Ozone-induced decrements in FEV1 and FVC do not correlate with measures of inflammation. Am J Respir Crit Care Med 1996;153:904–909. [DOI] [PubMed] [Google Scholar]
- 21.Scannell C, Chen L, Aris RM, Tager I, Christian D, Ferrando R, Welch B, Kelly T, Balmes JR. Greater ozone-induced inflammatory responses in subjects with asthma. Am J Respir Crit Care Med 1996;154:24–29. [DOI] [PubMed] [Google Scholar]
- 22.Basha MA, Gross KB, Gwizdala CJ, Haidar AH, Popovich J Jr. Bronchoalveolar lavage neutrophilia in asthmatic and healthy volunteers after controlled exposure to ozone and filtered purified air. Chest 1994;106:1757–1765. [DOI] [PubMed] [Google Scholar]
- 23.Bosson J, Stenfors N, Bucht A, Helleday R, Pourazar J, Holgate ST, Kelly FJ, Sandstrom T, Wilson S, Frew AJ, et al. Ozone-induced bronchial epithelial cytokine expression differs between healthy and asthmatic subjects. Clin Exp Allergy 2003;33:777–782. [DOI] [PubMed] [Google Scholar]
- 24.Arjomandi M, Solomon C, Witten A, Girling P, Balmes J. Airway inflammation in asthma after multi-day exposure to ozone. Am J Respir Crit Care Med 2002;165:A703. [Google Scholar]
- 25.Kanner RE, Connett JE, Altose MD, Buist AS, Lee WW, Tashkin DP, Wise RA. Gender difference in airway hyperresponsiveness in smokers with mild COPD: the Lung Health Study. Am J Respir Crit Care Med 1994;150:956–961. [DOI] [PubMed] [Google Scholar]
- 26.American Thoracic Society. Standardization of spirometry, 1994 update. Am J Respir Crit Care Med 1995;152:1107–1136. [DOI] [PubMed] [Google Scholar]
- 27.Aris RM, Christian D, Hearne PQ, Kerr K, Finkbeiner WE, Balmes JR. Ozone-induced airway inflammation in human subjects as determined by airway lavage and biopsy. Am Rev Respir Dis 1993;148:1363–1372. [DOI] [PubMed] [Google Scholar]
- 28.Arjomandi M, Schmidlin I, Girling P, Boylen K, Ferrondo R, Balmes J. Sputum induction and bronchoscopy for assessment of ozone-induced airway inflammation in asthma. Chest (In press) [DOI] [PubMed]
- 29.Huffnagel G, Toews G. Mechanisms of macrophage recruitment into infected lungs. In: Russell S, editor. Lung macrophages and dendritic cells in health and disease, lung biology in health and disease. Vol. 102. New York: Marcel Dekker; 1997. pp. 373–407.
- 30.Solomon C, Balmes J, Power K, Miller L. Mechanisms of particulate toxicity: health effects in susceptible humans. Final Report: California Air Resources Board, Contract Number: 99-314. Sacramento, CA: California Environmental Protection Agency; 2004. Available from: ftp://ftp.arb.ca.gov/carbis/research/apr/past/99-314.pdf.
- 31.Fahy JV, Kim KW, Liu J, Boushey HA. Prominent neutrophilic inflammation in sputum from subjects with asthma exacerbation. J Allergy Clin Immunol 1995;95:843–852. [DOI] [PubMed] [Google Scholar]
- 32.Ordonez CL, Shaughnessy TE, Matthay MA, Fahy JV. Increased neutrophil numbers and IL-8 levels in airway secretions in acute severe asthma: clinical and biologic significance. Am J Respir Crit Care Med 2000;161:1185–1190. [DOI] [PubMed] [Google Scholar]
- 33.Woodruff PG, Khashayar R, Lazarus SC, Janson S, Avila P, Boushey HA, Segal M, Fahy JV. Relationship between airway inflammation, hyperresponsiveness, and obstruction in asthma. J Allergy Clin Immunol 2001;108:753–758. [DOI] [PubMed] [Google Scholar]
- 34.Wood LG, Gibson PG, Garg ML. Biomarkers of lipid peroxidation, airway inflammation and asthma. Eur Respir J 2003;21:177–186. [DOI] [PubMed] [Google Scholar]
- 35.Tepper JS, Costa DL, Lehmann JR, Weber MF, Hatch GE. Unattenuated structural and biochemical alterations in the rat lung during functional adaptation to ozone. Am Rev Respir Dis 1989;140:493–501. [DOI] [PubMed] [Google Scholar]
- 36.Schwartz LW, Dungworth DL, Mustafa MG, Tarkington BK, Tyler WS. Pulmonary responses of rats to ambient levels of ozone: effects of 7-day intermittent or continuous exposure. Lab Invest 1976;34:565–578. [PubMed] [Google Scholar]
- 37.Gong H Jr, McManus MS, Linn WS. Attenuated response to repeated daily ozone exposures in asthmatic subjects. Arch Environ Health 1997;52:34–41. [DOI] [PubMed] [Google Scholar]
- 38.van Bree L, Dormans JA, Koren HS, Devlin RB, Rombout PJ. Attenuation and recovery of pulmonary injury in rats following short-term, repeated daily exposure to ozone. Inhal Toxicol 2002;14:883–900. [DOI] [PubMed] [Google Scholar]
- 39.Dormans JA, Rombout PJ, van Loveren H. Surface morphology and morphometry of rat alveolar macrophages after ozone exposure. J Toxicol Environ Health 1990;31:53–70. [DOI] [PubMed] [Google Scholar]
- 40.Comhair SA, Xu W, Ghosh S, Thunnissen FB, Almasan A, Calhoun WJ, Janocha AJ, Zheng L, Hazen SL, Erzurum SC. Superoxide dismutase inactivation in pathophysiology of asthmatic airway remodeling and reactivity. Am J Pathol 2005;166:663–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bowler RP, Crapo JD. Oxidative stress in allergic respiratory diseases. J Allergy Clin Immunol 2002;110:349–356. [DOI] [PubMed] [Google Scholar]
- 42.Gordon S. Alternative activation of macrophages. Nat Rev Immunol 2003;3:23–35. [DOI] [PubMed] [Google Scholar]
- 43.McConnell R, Berhane K, Gilliland F, London SJ, Islam T, Gauderman WJ, Avol E, Margolis HG, Peters JM. Asthma in exercising children exposed to ozone: a cohort study. Lancet 2002;359:386–391. [DOI] [PubMed] [Google Scholar]
- 44.Kunzli N, Lurmann F, Segal M, Ngo L, Balmes J, Tager IB. Association between lifetime ambient ozone exposure and pulmonary function in college freshmen: results of a pilot study. Environ Res 1997;72:8–23. [DOI] [PubMed] [Google Scholar]
- 45.Mautino G, Henriquet C, Gougat C, Le Cam A, Dayer JM, Bousquet J, Capony F. Increased expression of tissue inhibitor of metalloproteinase-1 and loss of correlation with matrix metalloproteinase-9 by macrophages in asthma. Lab Invest 1999;79:39–47. [PubMed] [Google Scholar]
- 46.Chen LL, Tager IB, Peden DB, Christian DL, Ferrando RE, Welch BS, Balmes JR. Effect of ozone exposure on airway responses to inhaled allergen in asthmatic subjects. Chest 2004;125:2328–2335. [DOI] [PubMed] [Google Scholar]