Abstract
Objective
To explore the underlying structure of symptom presentation in older adults with major depression by identifying homogeneous clusters of individuals based on symptom profiles.
Design
Secondary data analysis using latent class cluster analysis.
Setting
Clinical Research Center for the Study of Depression in Later Life conducted at Duke University.
Participants
366 patients age 60+ who met DSM-IV criteria for major depression and were enrolled in a longitudinal naturalistic treatment study.
Measurements
Responses to the ten items of the Montgomery-Asberg Depression Rating Scale (MADRS) at the time of study enrollment.
Results
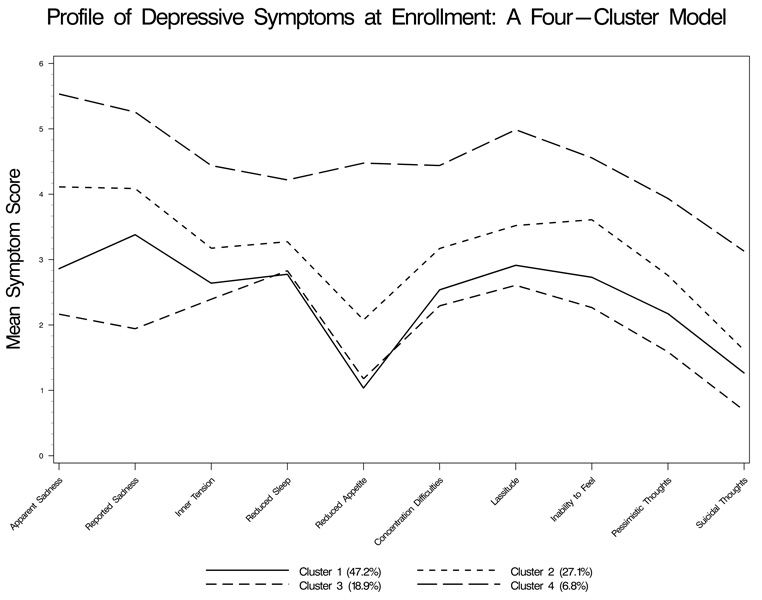
We identified four latent clusters of older adults with major depression. Patients in Cluster 1 (47.2%) had mean scores of average severity for reported and apparent sadness and lassitude and low mean scores for reduced appetite. Patients in Cluster 2 (27.1%) had higher mean scores compared to Cluster 1 for all items, and particularly for apparent sadness. Patients in Cluster 3 (18.9%) had the lowest mean scores for both apparent and reported sadness, but a similar profile compared to Cluster 1 for inner tension, reduced sleep, reduced appetite, and concentration difficulties. Cluster 4 (6.8%) had the highest mean scores for each item. Both apparent and reported sadness accounted for a large amount of variance among the four clusters. Patients in Cluster 4 were more likely to have 12 or less years of education and/or one or more functional limitations.
Conclusion
The heterogeneity in symptom presentation among older adults diagnosed with major depression can potentially inform the development of DSM-V.
Keywords: depression, latent class analysis
The prevalence of major depression among older adults in community samples can be as high as 5% (1–3), and in primary care settings, home health care populations, and institutional samples can range from 4–14% (4–7). In longitudinal studies, depression has been shown to often have a chronic course, and to be associated with adverse outcomes such as disability, cognitive decline, and mortality (8). The current nomenclature may not adequately reflect depression as observed in older adults, suggesting the true prevalence of clinically significant depressive symptoms may be even higher.
Across psychiatry in general, there have been recent discussions about the validity of psychiatric diagnoses as the field moves toward a revised nomenclature. For example, Krishnan suggested a dual classification system – one reflecting clinical manifestations and the other reflecting etiology, a suggestion particularly applicable to geriatric psychiatry where patients with late onset disorders may differ from those with an earlier onset (9). Others support the importance of moving beyond categorical diagnoses while noting establishing causality in the midst of comorbid conditions as often observed among older adults may present additional challenges to geriatric psychiatry (10). There has also been discussion about the necessity and advantages of focusing on or adding a dimensional approach to complement the existing categorical criteria (11, 12). Kraemer recently reviewed the history and context of this potential enhancement to the nomenclature, pointing out within a categorical diagnosis there can be variation in etiology, clinical characteristics, symptomatology and adverse consequences, and the necessity of identifying important sources of heterogeneity among those patients with a categorical diagnosis (12).
Recent work has utilized latent class cluster analysis to examine the structure of various psychiatric syndromes, including posttraumatic stress disorder (13), hypochondriasis (14), Alzheimer’s disease (15), chronic fatigue and fibromyalgia (16), borderline personality disorder (17), psychosis (18), and eating disorders (19, 20).
In cluster analysis, individuals are grouped into clusters based on their personal data such that individuals in one group share similar characteristics and differ from those in other groups. This technique differs from other classification techniques such as factor analysis, where the multivariate relationship among variables is of interest. For example, a factor analysis of depressive symptoms in a scale would show how different symptoms covary due to their dependence on underlying latent constructs (factors) that suggest a subdimension of depression (e.g., negative affect). In a cluster analysis, the study participants are placed into groups or clusters based on their characteristics such as depressive symptoms. Cluster analysis characterizes individuals into subtypes (i.e., individuals are assigned to groups based on their symptom profiles). Latent class cluster analysis has potential advantages over more traditional clustering techniques in that latent class cluster analysis utilizes a model-based approach and assigns individuals to clusters based on their posterior membership probabilities (21, 22). As in traditional clustering methods, the number of groups is unknown a priori and is specified as k. The dependent variable for these cluster models, therefore, is a k-category latent variable where k represents the number of clusters derived from the data. In latent class cluster analysis, each individual is assigned a probability of class membership for each of the identified clusters based on both measured and unmeasured characteristics. These types of models therefore have much to offer the field of psychiatry in their ability to identify sources of heterogeneity within samples of individuals.
The structure of depressive symptoms has been studied in community samples across all age groups using latent class analysis. Eaton et al. fit a three-class model to the Baltimore and Duke ECA data and found one class resembled DSM-III major depression. A second class was an intermediate disorder and the last group was a group of ‘normals’ (23). Sullivan et al. using latent class analysis identified six classes of depressive symptoms among participants in the National Comorbidity Survey who reported a lifetime history of depressive symptoms. The classes were severe typical, mild typical, severe atypical, mild atypical, intermediate, and minimal symptoms (24). Older adults, however, were not included in this sample. Similar work was done using the Virginia Twin Registry in which seven classes of depression were identified, again with the classes generally on a gradient (25). Using data from the National Survey of American Life, Lincoln et al. recently examined profiles of depressive symptoms among African Americans and Caribbean Blacks, and identified a high symptom and low symptom class (26). Two decades ago, using data from the Duke Epidemiologic Catchment Area (ECA) Survey and grade-of-membership analyses, Blazer et al. identified five subtypes of depression among those 18 or older with depressive symptoms (27). One profile closely resembled major depression, while other subtypes included a premenstrual syndrome among younger women, a mixed anxiety/depression group, a mildly dysphoric group, and a group with cognitive difficulties.
Little is known about the structure of depressive symptoms specific to older adults. With the number of older adults expected to increase over the coming decades, the public health impact of depressive symptoms in this population may be substantial, and a greater understanding of the structure underlying symptom presentation as a potential source of heterogeneity is critical. The structure of depressive symptoms in older adults may differ from that observed in younger adults since depression in older adults like other psychiatric syndromes can be more heterogeneous and affected by variables such as age of onset, number of lifetime episodes, and particularly, comorbidity, which can contribute to, be associated with, or result from psychopathology. Work is needed to identify symptom profiles in both community and clinical populations of older adults.
As noted, studies of depressive symptoms in community samples, like those for other psychiatric syndromes, typically identify one or two classes that resemble DSM disorders. Whether or not there is heterogeneity within groups of individuals with a categorical diagnosis is not known, but relevant to the field of psychiatry. The purpose of this analysis was to identify latent clusters or discrete groups of individuals within a sample of older adults diagnosed with major depression based on symptom scores at the time of study enrollment. These clusters or subtypes are therefore derived from the actual symptoms older adults reported to clinicians, and can lead to other studies focusing on etiologic and treatment variables associated with these subtypes as well as outcomes and course of depression over time. We hypothesized that we would find more than one cluster of patients within this group with a categorical diagnosis, that is, that symptomatology would be an important source of heterogeneity. A secondary objective was to examine if demographic, clinical and social variables known to be associated with late life depression were differentially associated with the clusters identified.
Methods
Sample Design
Participants were 366 inpatients and outpatients 60 years of age or older who met DSM-IV (28) criteria for major depression and were enrolled in the NIMH Mental Health Clinical Research Center (MHCRC) for the Study of Depression in Later Life conducted at Duke University. The purpose of the MHCRC is to examine neurocognitive outcomes of late life depression among patients without dementia or suspected dementia at enrollment (29). Patients were also excluded if they had any comorbid major psychiatric illness such as schizophrenia, any primary neurologic illness, active alcohol or drug abuse or dependence, or metal in the body which precluded magnetic resonance imaging of the brain. A total of 24 patients with symptoms of cognitive impairment who were enrolled and then later determined to be ineligible for the MHCRC because their decreased cognitive function did not improve with treatment were excluded from this analysis. Patients were recruited through clinician referrals from both psychiatry and primary care clinics at Duke. Both new (incident) and recurrent (prevalent) cases were included. The study is a naturalistic treatment study and patients have been followed up to 12 years. All patients provided written informed consent to participate and the research protocol is reviewed and approved annually.
Measures
At study enrollment, patients were administered the Duke Depression Evaluation Schedule (DDES) (30), a composite diagnostic instrument that included sections of the Diagnostic Interview Schedule (DIS) (31) modified for DSM-IV, the Montgomery-Asberg Depression Rating Scale (MADRS) (32), the Mini-Mental State Examination (MMSE) (33), and selected questions concerning demographics, limitations in basic and instrumental activities of daily living (ADLs), perceived stress and subjective social support. The primary variables of interest in this analysis were the responses to each of the ten items on the MADRS at the time of study enrollment. Each item is clinician scored from 0–6, with lower scores indicating less severity for that symptom.
A number of variables at their baseline level were examined as correlates of cluster membership. Demographic variables included sex, age as a continuous variable, race (White vs. Black/other), marital status (married vs. not married), and years of education (high school or less vs. more than high school). Clinical variables included MMSE score (<28 vs. 28+), age of onset of first spell of depression as a continuous variable, and number of lifetime depressive spells lasting two weeks or more (<4 vs. 4+). Social variables included perceived stress asking ‘On a scale of 1–10 how would you rate your average stress during the preceding 6 months?’ with 10 indicating high stress. We also included a measure of subjective social support (34), dichotomized as impaired/not impaired. We identified any difficulties or limitations with activities of daily living (ADLs) or mobility/instrumental ADLs as no limitations vs. one or more.
Statistical Analysis
The dependent variable for the latent class cluster analyses was a k-category latent variable where each k category represents an unobservable or latent subgroup or cluster. The predictor or indicator variables were the ten items of the MADRS. Each cluster represents a homogeneous group of patients who share similar responses to the model parameters (the MADRS symptoms). Individuals are assigned to clusters based on their posterior membership probabilities – and assigned to the cluster for which their probability is the highest (21, 35). The latent class cluster analyses were run using Latent Gold (36) analysis software.
We first explored models comparing a score of 0 (symptom not present) vs. 1 or more (symptom present) and found a one-cluster model fit the data well based on symptom endorsement. A one-cluster model suggests a similar profile for all the individuals with random variation around the mean for each symptom. Because this was a sample of patients with current major depression, most of the patients endorsed the majority of the ten items at some degree. For these analyses, we therefore looked at models that would incorporate symptom severity, and used each item score as an ordinal variable with a range of 0–6.
We assessed the fit of five consecutive models with 1–5 clusters each and used fit statistics to identify the model with the best fit to these data. The L2 likelihood-ratio statistic indicates the amount of the observed relationship between the ten MADRS items that remains unexplained by the model (36). The significance of the L2 is a measure of the fit of the model, with significance levels p>.05 desired. Because we were modeling a number of variables each with a number of values and the data in individual response categories could be sparse, we estimated the significance by bootstrapping (n=500 iterations). The resulting p-value for each model is the proportion of the re-estimated models with a higher L2 than in the comparison model (35, 36). We also used the Bayesian Information Criteria (BIC) which takes the number of parameters into account to compare the models. A smaller BIC indicates a better fit. Because these were nested models, we also used a conditional bootstrap option (n=500 iterations) computing the difference in the log-likelihood statistics between the two models (-2LL Diff) to see if adding another cluster significantly improved the model fit. In our final model, we examined the bivariate residuals assessing how well the model explained the correlation between each of the variables.
To identify covariates associated with cluster membership, we ran bivariate descriptive analyses using SAS (37) analysis software. For categorical variables, we used chi-square analyses, and for continuous variables we compared means across the clusters using F tests. Because we conducted multiple tests between covariates and cluster membership, we set our significance level at α < .01 to decrease the probability of a Type I error. All statistical tests were two-tailed.
Results
There were a total of 382 eligible patients enrolled in the study. Four patients had missing baseline (enrollment) MADRS data and 12 patients had missing MMSE data. These patients were excluded, resulting in an analysis sample of 366 patients. Patients were predominantly white (85.5%) and female (66.1%), and had a mean age of 69.1 years. Approximately 56% of the patients were taking an antidepressant at the time of study enrollment, while 33% had no history of antidepressant use.
The distribution of symptom scores for each of the ten items of the MADRS is shown in Table 1. Over 98% of the patients had apparent sadness, reported sadness, lassitude and inability to feel at some degree, which would be consistent with a diagnosis of major depression. Suicidal thoughts (not present in 30%), and reduced appetite (not present in 45%), were the least prevalent symptoms. Most symptoms, if present, were more likely to be moderate or severe rather than mild with two exceptions. Pessimistic or suicidal thoughts were more likely to be scored 1 or 2 compared to 3 or greater.
Table 1.
MADRS Symptom Endorsement at Study Enrollment (n=366)
| MADRS Symptom | Mean | Standard Deviation | Range |
|---|---|---|---|
| Item 1: Apparent sadness | 3.25 | 1.14 | 0–6 |
| Item 2: Reported sadness | 3.43 | 1.04 | 0–6 |
| Item 3: Inner tension | 2.86 | 1.18 | 0–6 |
| Item 4: Reduced sleep | 3.02 | 1.38 | 0–6 |
| Item 5: Reduced appetite | 1.58 | 1.69 | 0–6 |
| Item 6: Concentration difficulties | 2.79 | 1.19 | 0–6 |
| Item 7: Lassitude | 3.16 | 1.13 | 0–6 |
| Item 8: Inability to feel | 3.01 | 1.11 | 0–6 |
| Item 9: Pessimistic thoughts | 2.34 | 1.28 | 0–6 |
| Item 10: Suicidal thoughts | 1.38 | 1.23 | 0–6 |
| Total MADRS Score | 26.82 | 7.37 | 14–54 |
In Table 2, we present the results of the model selection process. All of our models fit the data based on the L2. Using the BIC, we determined a four-cluster model adequately fit the data. The addition of a cluster was significant through four clusters, while adding a fifth cluster was not significant at p<.01. We then refined our four-cluster model. There were seven bivariate residuals that were significant at the p<.05 level. As suggested by the developers of the software, we included each bivariate residual as a direct effect in the model therefore introducing local dependencies (21, 35, 36). This was done individually beginning with the largest residual, and the model was then re-estimated. In our final model, there were five bivariate residuals included as direct effects for the following pairs: items 3 and 9, items 4 and 7, items 6 and 7, items 7 and 8, and items 9 and 10. Two other residuals were significant at p<.05, but with the addition of the fourth and fifth bivariate residuals, the model fit was not improved, so these two other residuals were not included. Because cluster assignment is based on probability across ten items, the model is open to classification error once more than one cluster is included. The proportion of cases estimated by the model to be misclassified was low (8%), indicating a good separation of clusters.
Table 2.
Analysis of model selection
| Model | BIC | Number of Parameters | L2 | df | Bootstrap p-value | Classification Error | -2LL Diff | df | Bootstrap p-Value |
|---|---|---|---|---|---|---|---|---|---|
| 1-Cluster | 11424.732 | 60 | 6752.619 | 306 | 0.2180 | .0000 | |||
| 2-Cluster | 10861.248 | 71 | 6124.206 | 295 | 0.3420 | .0245 | 628.4132 | 11 | <0.0001 |
| 3-Cluster | 10711.784 | 82 | 5909.813 | 284 | 0.3100 | .0468 | 214.3924 | 11 | <0.0001 |
| 4-Cluster | 10706.476 | 93 | 5839.576 | 273 | 0.2200 | .1209 | 70.2374 | 11 | <0.0001 |
| 5-Cluster | 10739.356 | 104 | 5807.528 | 262 | 0.1900 | .1373 | 32.0484 | 11 | 0.0160 |
| Final Model* | |||||||||
| 4-Cluster | 10681.126 | 98 | 5784.713 | 268 | 0.1680 | .0802 |
BIC=Bayesian information criteria; L2=likelihood-ratio statistic; df=degrees of freedom; -2LLDiff=log likelihood ratio chi-square comparing nested models; se=standard error;
Final model includes five bivariate residuals included as direct effects;
A total of 47.2% of the patients were assigned to Cluster 1, 27.1% to Cluster 2, 18.9% to Cluster 3, and 6.8% to Cluster 4. Cluster numbers were assigned based on size. Figure 1 shows the symptom profile for each cluster, with mean scores plotted for each item by cluster. Across all clusters, we note that some symptoms have higher mean scores than others, indicating more severity. The four clusters seem to generally differentiate by severity – that is, the profiles are roughly parallel for inner tension, concentration difficulties, lassitude, inability to feel, pessimistic thoughts, and suicidal thoughts. But there are several other patterns noted. Reduced appetite is more severe for patients in Cluster 4 and of similar severity to other classic depressive symptoms within this cluster. Reduced appetite is noticeably less severe for the other three clusters, and similar for Clusters 1 and 3. Clusters 1 and 3 also have similar mean scores for reduced sleep and concentration difficulties. The clusters may differentiate by apparent and reported sadness, with patients in Cluster 3 having more mild sadness compared to the other three clusters. For patients in Cluster 1 (almost half of the sample), reported sadness was more prevalent than apparent sadness, but this pattern was not observed within the other three clusters.
Figure 1.
Profiles of depressive symptoms at enrollment by cluster
In analysis not shown, all ten MADRS items were positively associated with Cluster 4 and negatively associated with Clusters 1 and 3. Each of the ten symptoms significantly discriminated between the clusters, and the degree of sadness, in particular, accounted for much of the variance between clusters.
In Table 3, we show the characteristics for the sample as a whole and across the four clusters to identify covariates associated with cluster membership. Cluster 4 has a higher proportion of individuals with high school or less years of education compared to the other clusters. The proportion of patients with ADL and IADL limitations is also considerably higher in Cluster 4. Other demographic, clinical, and social variables do not appear to be associated with cluster membership. We also looked at history of antidepressant use at the time of study enrollment by cluster using our STAGED variable (38), and found significant differences (χ2[12]=71.98, p<.0001). The proportion of patients without a history of antidepressant use was 43.8% in Cluster 1, 23.3% in Cluster 2, 43.9% in Cluster 3, and 4.2% in Cluster 4. The proportion of patients taking an antidepressant at the time of enrollment was 40.6% in Cluster 1, 68.5% in Cluster 2, 48.8% in Cluster 3, and 95.8% in Cluster 4. A total of 36% of the patients in the analysis sample had missing data on this variable, so these findings must be interpreted with caution and as a suggestion for future research. We also examined if there were differences among the clusters with regard to receiving ECT treatment during the course of the study and found significant differences. Overall, 20.5% of these patients later received ECT– 8.2% in Cluster 1, 26.1% in Cluster 2, 6.4% in Cluster 3, and 83.3% in Cluster 4 (χ2 [3]=75.99, p<0.0001). A total of 27% of the patients had missing ECT data, so these results must also be interpreted with caution.
Table 3.
Sample characteristics by cluster
| Total Sample (n=366) | Cluster 1 (n=173) | Cluster 2 (n=101) | Cluster 3 (n=67) | Cluster 4 (n=25) | ||
|---|---|---|---|---|---|---|
| Mean age in years (sd) | 69.1 (6.8) | 68.2 (6.6) | 69.4 (6.8) | 69.7 (6.8) | 72.0 (8.1) | F (3,362)=2.77; p=0.0417 |
| No. White (%) | 313 (85.5%) | 152 (87.9%) | 86 (85.2%) | 53 (79.1%) | 22 (88.0%) | χ2 (3)=3.13; p=0.3723 |
| No. Female (%) | 242 (66.1%) | 106 (61.3%) | 73 (72.3%) | 45 (67.2%) | 18 (72.0%) | χ2 (3)=3.94; p=0.2677 |
| No. with 12 or less years of education (%) | 134 (36.7%) | 46 (26.7%) | 41 (40.6%) | 26 (38.8%) | 21 (84.0%) | χ2 (3)=32.20; p<0.0001 |
| Mean age of onset (sd) | 43.8 (20.6) | 42.3 (21.1) | 44.4 (20.0) | 45.3 (19.7) | 49.0 (20.5) | F (3,340)=0.94; p=0.4199 |
| No. with 4+ lifetime spells of depression (%) | 185 (52.3%) | 85 (50.0%) | 52 (53.1%) | 34 (54.8%) | 14 (58.3%) | χ2 (3)=0.89; p=0.8270 |
| No. with MMSE score <28 (%) | 104 (28.4%) | 42 (24.3%) | 28 (27.7%) | 22 (32.8%) | 12 (48.0%) | χ2 (3)=6.84; p=0.0773 |
| No. unmarried (%) | 163 (44.5%) | 75 (43.4%) | 47 (46.5%) | 30 (44.8%) | 11 (44.0%) | χ2 (3)=0.27; p=0.9663 |
| Mean average stress (sd) | 6.5 (2.1) | 6.4 (2.0) | 7.0 (2.1) | 6.3 (2.2) | 6.6 (2.4) | F (3,356)=1.98; p=0.1170 |
| No. with impaired subjective social support (%) | 198 (56.9%) | 94 (57.3%) | 58 (59.8%) | 31 (48.4%) | 15 (65.2%) | χ2 (3)=2.86; p=0.4136 |
| No. with 1+ basic ADL limitations (%) | 67 (18.5%) | 24 (14.0%) | 21 (21.0%) | 7 (10.5%) | 15 (62.5%) | χ2 (3)=36.54; p<0.0001 |
| No. with 1+ IADL limitations (%) | 232 (65.0%) | 98 (58.0%) | 75 (75.8%) | 38 (57.6%) | 21 (91.3%) | χ2 (3)=17.28; p=0.0006 |
Numbers derived by percentages may not sum to 366 if missing data
Discussion
To the best of our knowledge, these findings are the first to explore the latent structure of depressive symptoms within a clinical sample of older adults diagnosed with major depression. Our major finding was that a multi-cluster model fit the data better than a one-cluster model, suggesting heterogeneity among these older patients in our clinical sample based on their profile of depressive symptoms at the index episode. In other words, these findings provide evidence to what is clinically known, that there is considerable variability in symptom presentation among older adults who are diagnosed with a single categorical diagnosis, major depression. However, we also recognize that a pattern across the four clusters emerged, such that sadness was frequent and suicidal thoughts were less frequent, suggesting also some homogeneity in presentation.
We found a four-cluster model provided a good fit to these data. Almost half of the patients were assigned to Cluster 1, which exhibited a symptom profile consistent with DSM-IV major depression – moderate apparent and reported sadness, lassitude and inability to feel. Approximately a quarter of the patients had the highest probability of being assigned to Cluster 2, which followed a similar profile to Cluster 1 but each symptom tended to be more severe. The remaining quarter of the patients were divided between a cluster that had a milder profile of symptoms (Cluster 3), and particularly were less likely to report sadness, and a cluster with more severe symptoms (Cluster 4). While a small proportion of patients were assigned to Cluster 4, this cluster seemed to exhibit the most severity and greater likelihood of having all symptoms and was significantly associated with functional limitations. This association provides evidence to support what is known in geriatric psychiatry, that functional impairment and depression are commonly associated in late life (39), especially among the more severely depressed. Overall, these findings support our hypothesis that within a group of patients diagnosed with major depression there exist discrete homogeneous clusters of patients who share similar symptom profiles.
Explanations for the association between fewer years of education and membership in Cluster 4 or reduced likelihood of membership in the other three clusters are not immediately apparent. It is possible patients with more years of education seek treatment before the symptoms become as severe as those seen in Cluster 4. Other studies have shown a lower attained educational level may be one of a number of factors that put older adults at risk for chronic or recurrent depression (40). Consistent with this hypothesis, we also noted that Cluster 4 had the highest proportion of patients already taking an antidepressant at the time of the index episode. This cluster may represent patients with a severe depression with more biologic symptoms which may be refractory to medication. The higher probability of reduced appetite may be due to the side effects of antidepressant use, but is more likely consistent with more severe depression. We did not find cluster membership to be significantly associated with other clinical variables such as age of onset and number of lifetime spells of depression or social variables such as perceived stress and social support, suggesting these variables are similarly associated across all four subtypes of late life depression. It is not likely that the clusters reflect treatment response since Cluster 4, which had the highest levels of symptom endorsement, also had the highest proportion of patients taking an antidepressant at the time of study enrollment, and, a higher proportion of patients in Cluster 2 were taking antidepressants at baseline when compared to Cluster 3.
It appears from these data that the degree of sadness may play a significant role in differentiating the clusters. Of particular interest are the mean levels of the two sadness variables for Clusters 1 and 3. Particularly for Cluster 3, sadness (a key component of DSM-IV major depression) is not the most severe symptom in the symptom profile. While sadness in some degree was present across all clusters, the data support the concept of 'depression without sadness' (41) seen in older adults.
These analyses provide support for a multi-cluster model, and we can conclude as suggested by Kraemer (12), that we have identified a source of heterogeneity within a sample of patients with a categorical diagnosis of major depression. The symptom profiles suggest the patient groups may differ in terms of symptom severity providing support for an adjunct dimensional component as the nomenclature goes forward. But we also found different covariates were associated with cluster membership, suggesting the patients may potentially differ in ways other than severity. We noted in Cluster 4, for example, that a higher proportion of patients later received ECT. Latent class cluster analysis allows us only to conclude there appear to be discrete patient groups within a sample of older adults diagnosed with major depression who may differ because of measured variables (e.g., symptom severity) or unmeasured factors (e.g., etiologic factors). At this point, it is not clear how we could label these clusters, and it is preferable to allow the data to speak for themselves. Whether the clusters differ in ways other than severity will be the subject of additional work. A simple sum of the items would suggest the relationship with future behavior is linear. Latent cluster analysis assumes the relationship is not linear – that each symptom may not have the same effect. Future research will determine if these clusters differ in their longitudinal course or are differentially associated with adverse outcomes.
In summary, these profiles provide new information concerning the heterogeneity of late life depression by identifying naturally occurring symptom profiles within discrete clusters of patients. Across all age groups, considerable effort has been expended to identify a genetic component of major depression (42). Analyses such as these, which separate patients into unobserved or latent clusters, can add much to this discussion by helping identify phenotypes that have a greater genetic component, while others may be more linked to environmental or situational variables such as functional impairment. Future work will also explore symptom profiles within a sample of community dwelling older adults, which can help with an overall goal of identifying homogeneous groups of older adults based on their endorsement of depressive symptoms.
There are several limitations to these findings. Our sample of older adults with major depression was predominantly White, the majority had education past high school, and the sample was drawn from a clinical population and may not be representative of all older adults diagnosed with major depression. Our patients were also predominantly healthy and able to come into the clinic for follow-up visits and may not reflect those patients in poorer health. Because this was a naturalistic treatment study, our patients approximate those seen in clinical practice seeking treatment, and may overlap with patients typically seen in primary care. Our clusters were based on the responses to the ten items of the MADRS. In future work, we plan to look for consistency across other assessments of depression in this sample. Our structure was based on the use of each MADRS item as an ordinal variable, and as we indicated earlier, had we used only symptom endorsement we would have found a one-cluster model fit the data best because most patients endorsed each of the symptoms at some degree.
Assignment to each cluster is based on probability across symptoms, which may introduce misclassification error. Specifically, if a patient has a profile that is very similar to the profile of two or more clusters and has similar probability of being in each cluster, the patient will be assigned to the cluster with the highest probability when in fact another cluster may have a similar profile as well. Using the items as ordinal variables also resulted in a complex model with data spread across various levels for each item and some slightly significant local dependencies present. We relaxed the local independence assumption for these pairs of MADRS symptoms by including their bivariate residuals into the model as direct effects which was not hypothesized a priori but generally provides a better fit than adding another cluster to the model. While the additional of these bivariate residuals as direct effects improved the fit of the model, the overall findings did not change.
Overall, these types of analyses are critical in beginning to disentangle the structure of late life depressive symptoms through the use of latent classes. This work is exploratory, but these clusters within samples of older adults diagnosed with major depression can later be linked to biologic and genetic variables and provide important information in understanding etiology and treatment response. Finally, we plan to explore whether the clusters differentiate not only the course of depression but adverse outcomes.
Acknowledgements
This research was supported by NIMH grants K01 MH066380, R01 MH080311, K24 MH70027, R01 MH54846 and P50 MH 60451. The authors report no competing interests. The authors would like to acknowledge the helpful comments provided by the anonymous reviewers.
Contributor Information
Celia F. Hybels, Department of Psychiatry and Behavioral Sciences, Center for the Study of Aging and Human Development, Box 3003, Duke University Medical Center, Phone: (919) 660-7546, FAX: (919) 668-0453, E-mail: cfh@geri.duke.edu.
Dan G. Blazer, Department of Psychiatry and Behavioral Sciences, Center for the Study of Aging and Human Development, Duke University Medical Center.
Carl F. Pieper, Department of Biostatistics and Bioinformatics, Center for the Study of Aging and Human Development, Duke University Medical Center.
Lawrence R. Landerman, School of Nursing, Center for the Study of Aging and Human Development, Duke University Medical Center.
David C. Steffens, Department of Psychiatry and Behavioral Sciences, Center for the Study of Aging and Human Development, Duke University Medical Center.
References
- 1.Regier DA, Boyd JH, Burke JD, et al. One-month prevalence of mental disorders in the United States. Arch Gen Psychiatry. 1988;45:977–986. doi: 10.1001/archpsyc.1988.01800350011002. [DOI] [PubMed] [Google Scholar]
- 2.Beekman ATF, Deeg DJH, van Tilberg T, et al. Major and minor depression in later life: a study of prevalence and risk factors. J Affect Disord. 1995;36:65–75. doi: 10.1016/0165-0327(95)00061-5. [DOI] [PubMed] [Google Scholar]
- 3.Steffens DC, Skoog I, Norton M, et al. Prevalence of depression and its treatment in an elderly population: The Cache County Study. Arch Gen Psychiatry. 2000;57:601–607. doi: 10.1001/archpsyc.57.6.601. [DOI] [PubMed] [Google Scholar]
- 4.Bruce ML, McAvay GJ, Raue PJ, et al. Major depression in elderly home health care patients. Am J Psychiatry. 2002;159:1367–1374. doi: 10.1176/appi.ajp.159.8.1367. [DOI] [PubMed] [Google Scholar]
- 5.Lyness JM, King DA, Cox C, et al. The importance of subsyndromal depression in older primary care patients: Prevalence and associated functional disability. J Am Geriatr Soc. 1999;47:647–652. doi: 10.1111/j.1532-5415.1999.tb01584.x. [DOI] [PubMed] [Google Scholar]
- 6.Parmelee PA, Katz IR, Lawton MP. Depression among institutionalized aged: Assessment and prevalence estimation. J Gerontol A Biol Sci Med Sci. 1989;44:M22–M29. doi: 10.1093/geronj/44.1.m22. [DOI] [PubMed] [Google Scholar]
- 7.Teresi J, Abrams R, Holmes D, et al. Prevalence of depression and depression recognition in nursing homes. Soc Psychiatry Psychiatr Epidemiol. 2001;36:613–620. doi: 10.1007/s127-001-8202-7. [DOI] [PubMed] [Google Scholar]
- 8.Blazer DG. Depression in late life: Review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58A:249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 9.Krishnan KRR. Concept of disease in geriatric psychiatry. Am J Geriatr Psychiatry. 2007;15:1–11. doi: 10.1097/01.JGP.0000224600.37387.4b. [DOI] [PubMed] [Google Scholar]
- 10.Caine ED. Etiologies, environments, and genes - Challenges for psychiatric diagnosis during an era of scientific transition. Am J Geriatr Psychiatry. 2007;15:12–16. doi: 10.1097/01.JGP.0000249762.75403.2e. [DOI] [PubMed] [Google Scholar]
- 11.Helzer JE, Kraemer HC, Krueger RF. The feasibility and need for dimensional psychiatric diagnoses. Psychol Med. 2006;36:1671–1680. doi: 10.1017/S003329170600821X. [DOI] [PubMed] [Google Scholar]
- 12.Kraemer HC. DSM categories and dimensions in clinical and research contexts. Int J Methods Psychiatr Res. 2007;16(S1):S8–S15. doi: 10.1002/mpr.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Breslau N, Reboussin BA, Anthony JC, et al. The structure of posttraumatic stress disorder. Arch Gen Psychiatry. 2005;62:1343–1351. doi: 10.1001/archpsyc.62.12.1343. [DOI] [PubMed] [Google Scholar]
- 14.Fink P, Ornbol E, Toft T, et al. A new, empricially established hypochondriasis diagnosis. Am J Psychiatry. 2004;161:1680–1691. doi: 10.1176/appi.ajp.161.9.1680. [DOI] [PubMed] [Google Scholar]
- 15.Lyketsos CG, Sheppard JE, Steinberg M, et al. Neuropsychiatric disturbance in Alzheimer's disease clusters into three groups: the Cache County study. Int J Geriatr Psychiatry. 2001;16:1043–1053. doi: 10.1002/gps.448. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan PF, Smith W, Buchwald D. Latent class analysis of symptoms associated with chronic fatigue syndrome and fibromyalgia. Psychol Med. 2002;32:881–888. doi: 10.1017/s0033291702005834. [DOI] [PubMed] [Google Scholar]
- 17.Shevlin M, Dorahy M, Adamson G, et al. Subtypes of borderline personality disorder, associated clinical disorders and stressful life-events: A latent class analysis based on the British psychiatric Morbidity Survey. Br J Clin Psychol. 2007;46:273–281. doi: 10.1348/014466506x150291. [DOI] [PubMed] [Google Scholar]
- 18.Shevlin M, Murphy J, Dorahy MJ, et al. The distribution of positive psychosis-like symptoms in the population: A latent class analysis of the National Comorbidity Survey. Schizophr Res. 2007;89:101–109. doi: 10.1016/j.schres.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 19.Wade TD, Crosby RD, Martin NG. Use of latent profile analysis to identify eating disorder phenotypes in an adult Australian twin cohort. Arch Gen Psychiatry. 2006;63:1377–1384. doi: 10.1001/archpsyc.63.12.1377. [DOI] [PubMed] [Google Scholar]
- 20.Duncan AE, Bucholz KK, Neumar RJ, et al. Clustering of eating disorder symptoms in a general population female twin sample: a latent class analysis. Psychol Med. 2007;37:1097–1107. doi: 10.1017/S0033291707000505. [DOI] [PubMed] [Google Scholar]
- 21.Vermunt J, Magidson J. Latent class cluster analysis. In: Hagenuars J, McCutcheon A, editors. Applied Latent Class Analysis. Cambridge: Cambridge University Press; 2002. pp. 89–106. [Google Scholar]
- 22.Magidson J, Vermunt JK. Latent class models for clustering: A comparison with K-means. Canadian Journal of Marketing Research. 2002;20:37–44. [Google Scholar]
- 23.Eaton WW, Dryman A, Sorenson A, et al. DSM-III major depressive disorder in the community: A latent class analysis of data from the NIMH Epidemiologic Catchment Area Programme. Br J Psychiatry. 1989;155:48–54. doi: 10.1192/bjp.155.1.48. [DOI] [PubMed] [Google Scholar]
- 24.Sullivan PF, Kessler RC, Kendler KS. Latent class analysis of lifetime depressive symptoms in the National Comorbidity Survey. Am J Psychiatry. 1998;155:1398–1406. doi: 10.1176/ajp.155.10.1398. [DOI] [PubMed] [Google Scholar]
- 25.Sullivan PF, Prescott CA, Kendler KS. The subtypes of major depression in a twin registry. J Affect Disord. 2002;68:273–284. doi: 10.1016/s0165-0327(00)00364-5. [DOI] [PubMed] [Google Scholar]
- 26.Lincoln KD, Chatters LM, Taylor RJ, et al. Profiles of depressive symptoms among African Americans and Caribbean Blacks. Soc Sci Med. 2007;65:200–213. doi: 10.1016/j.socscimed.2007.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Blazer D, Swartz M, Woodbury M, et al. Depressive symptoms and depressive diagnoses in a community population. Arch Gen Psychiatry. 1988;45:1078–1084. doi: 10.1001/archpsyc.1988.01800360026004. [DOI] [PubMed] [Google Scholar]
- 28.American Psychiatric Association. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. Washington D.C: American Psychiatric Association; 1994. [Google Scholar]
- 29.Steffens DC, Potter GG, McQuoid DR, et al. Longitudinal magnetic resonance imaging vascular changes, apolipoprotein E genotype, and development of dementia in the Neurocognitive Outcomes of Depression in the Elderly Study. Am J Geriatr Psychiatry. 2007;15:839–849. doi: 10.1097/JGP.0b013e318048a1a0. [DOI] [PubMed] [Google Scholar]
- 30.Blazer D, Hughes DC, George LK. Age and impaired subjective support: Predictors of depressive symptoms at one-year follow-up. J Nerv Ment Dis. 1992;180:172–178. [PubMed] [Google Scholar]
- 31.Robins LN, Helzer JE, Croughan J, et al. National Institute of Mental Health Diagnostic Interview Schedule: Its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 32.Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 33.Folstein MF, Folstein SE, McHugh P. Mini-mental state: A practical method for grading the cognitive state of patients for clinicians. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 34.Landerman R, George LK, Campbell RT, et al. Alternative models of the stress buffering hypothesis. Am J Community Psychol. 1989;17:625–641. doi: 10.1007/BF00922639. [DOI] [PubMed] [Google Scholar]
- 35.Vermunt JK, Magidson J. Technical Guide for Latent GOLD 4.0: Basic and Advanced. Belmont Massachusetts: Statistical Innovations, Inc; 2005. [Google Scholar]
- 36.Vermunt J, Magidson J. Latent GOLD 4.0 User's Guide. Belmont, Massachusetts: Statistical Innovations, Inc; 2005. [Google Scholar]
- 37.SAS Institute. Statistical Analysis System, Version 9. Cary NC: SAS Institute; 2004. [Google Scholar]
- 38.Steffens DC, McQuoid DR, Krishnan KR. The Duke Somatic Treatment Algorithm for Geriatric Depression (STAGED) approach. Psychopharmacol Bull. 2002;36:58–68. [PubMed] [Google Scholar]
- 39.Bruce ML. Depression and disability in late life: Directions for future research. Am J Geriatr Psychiatry. 2001;9:102–112. [PubMed] [Google Scholar]
- 40.Smit F, Smits N, Schoevers R, et al. An epidemiological approach to depression prevention in old age. Am J Geriatr Psychiatry. 2008;16:444–453. doi: 10.1097/JGP.0b013e3181662ab6. [DOI] [PubMed] [Google Scholar]
- 41.Gallo JJ, Rabins PV, Lyketsos CG, et al. Depression without sadness: Functional outcomes of nondysphoric depression in later life. J Am Geriatr Soc. 1997;45:570–578. doi: 10.1111/j.1532-5415.1997.tb03089.x. [DOI] [PubMed] [Google Scholar]
- 42.Hasler G, Drevets WC, Manji HK, et al. Discovering endophenotypes for major depression. Neuropsychopharmacology. 2004;29:1765–1781. doi: 10.1038/sj.npp.1300506. [DOI] [PubMed] [Google Scholar]