Abstract
OBJECTIVE
To review the literature about the health benefits of far-infrared sauna (FIRS) use.
QUALITY OF EVIDENCE
A search of Web of Science, EBSCO, Ovid MEDLINE, Ovid HealthSTAR, and EMBASE using the terms far-infrared and sauna, refined by limiting the search to studies of humans published in English, yielded 9 relevant papers (level I or level II evidence).
MAIN MESSAGE
Far-infrared saunas are approved by the Canadian Standards Association and are sold to the public. The manufacturers claim numerous health benefits; however, the published evidence to substantiate these claims is limited. Four papers support the use of FIRS therapy for those with congestive heart failure and 5 papers support its use for those with coronary risk factors.
CONCLUSION
There is limited moderate evidence supporting FIRS efficacy in normalizing blood pressure and treating congestive heart failure; fair evidence, from a single study, supporting FIRS therapy in chronic pain; weak evidence, from a single study, supporting FIRS therapy in chronic fatigue syndrome; weak evidence, from a single study, supporting FIRS therapy for obesity; and consistent fair evidence to refute claims regarding the role of FIRSs in cholesterol reduction.
Résumé
OBJECTIF
Réviser la littérature sur les avantages pour la santé de l’utilisation des saunas à infrarouge lointain (SIRL).
QUALITÉ DES PREUVES
Une recherche dans Web of Sciences. EBSCO, Ovid MEDLINE, OVID HealthSTAR et EMBASE à l’aide des termes far-infrared et sauna, en se limitant aux études chez l’humain publiées en anglais, a identifié 9 articles pertinents (preuves de niveau I ou II).
PRINCIPAL MESSAGE
Les saunas à infrarouge lointain sont approuvés par l’Association canadienne de normalisation et sont en vente libre. Les manufacturiers leur attribuent plusieurs avantages pour la santé; toutefois, les données de la littérature à l’appui de ces prétentions sont limitées. Quatre articles soutiennent l’utilisation de SIRL dans le traitement de l’insuffisance cardiaque et 5 articles la soutiennent chez les sujets avec facteurs de risque coronarien.
CONCLUSION
Il existe des données limitées d’importance modérée suggérant que les SIRL sont efficaces pour normaliser la tension artérielle et traiter l’insuffisance cardiaque; des données assez bonnes d’une seule étude en faveur du traitement de la douleur chronique par SIRL; des données faibles d’une seule étude pour l’utilisation du SIRL dans le syndrome de fatigue chronique; des données faibles d’une seule étude préconisant l’utilisation du SIRL pour l’obésité; et des preuves assez solides contredisant les prétentions au sujet du rôle des SIRL dans la réduction du cholestérol.
Far-infrared saunas (FIRSs) are approved by the Canadian Standards Association and are sold to the public as recreational saunas. Manufacturers advertise numerous therapeutic effects, including weight loss, improved cardiovascular health, normalized blood pressure (BP), lowered cholesterol, and reduced pain, stress, and fatigue.1 These saunas are also being advertised in publications targeting Canadian physicians.1 The current North American market for FIRSs is valuated at approximately $60 million to $75 million and is growing rapidly, according to Aaron Zack, President and Chief Executive Officer of Sunlight Saunas (written communication, May 2009).
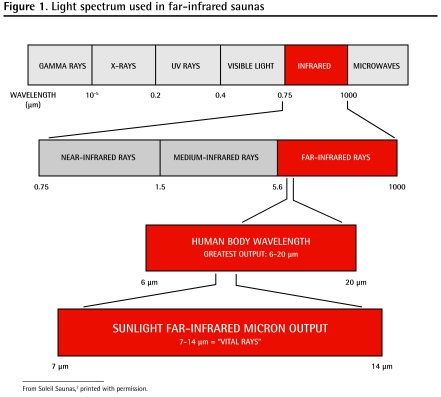
Traditional saunas use either wood stoves or 220-V heaters to heat the air to approximately 85°C, which then heats the occupant, mainly via convection. Some people find this heat uncomfortable. In contrast, FIRSs heat to approximately 60°C, providing a more comfortable and relaxing experience. They utilize 120-V infrared elements, similar to the infrared warmers on neonatal resuscitation beds, to radiate heat with a wavelength of around 10 μm (Figure 12). As infrared heat penetrates more deeply than warmed air, users develop a more vigorous sweat at a lower temperature than they would in traditional saunas. The cardiovascular demand imparted by thermoregulatory homeostasis (sweating, vasodilation, decreased afterload, increased heart rate, increased cardiac output) is similar to that achieved by walking at a moderate pace. As such, FIRS might be of particular benefit to those who are sedentary due to various medical conditions, such as osteoarthritis or cardiovascular or respiratory problems.
Figure 1.
Light spectrum used in far-infrared saunas
This paper seeks to review and summarize the published data on cardiovascular benefits of FIRS use. The implications will be of substantial interest to health care providers, patients, manufacturers, regulatory agencies, and consumers.
Quality of evidence
A search of Web of Science, EBSCO, Ovid MEDLINE, Ovid HealthSTAR, and EMBASE using far-infrared and sauna was refined by limiting the search to human clinical therapeutic studies published in English. Only clinical therapeutic trials of level I (randomized controlled trials [RCTs]) or level II (cohort and non-randomized trials) evidence (Table 13–11) were included in this analysis.
Table 1.
Studies supporting use of FIRSs
| STUDY | N | DURATION | LEVEL OF EVIDENCE | INDICATION | PRIMARY OUTCOMES | COMMENTS |
|---|---|---|---|---|---|---|
| Kihara et al,3 2004 | 30 | 14 d | I | CHF | Fewer PVCs and lowered BNP levels | Infrared sauna treatment improves ventricular arrhythmias in patients with CHF |
| Kihara et al,4 2002 | 30 | 14 d | I | CHF | Clinical symptoms improved and BNP levels decreased; endothelial function improved | Clinical improvement in CHF seen after FIRS therapy might be owing to improved endothelial function |
| Miyamoto et al,5 2005 | 15 | 28 d | II | CHF | CHF symptoms, ejection fraction, and walking distance improved; catecholamine levels decreased | Infrared sauna therapy is a safe and effective treatment of CHF |
| Sugahara et al,6 2003 | 12 | 28 d | II | Pediatric CHF due to VSD | Clinical signs and symptoms of CHF decreased, urine nitrate levels decreased, and 75% of patients avoided surgical repair | Infrared sauna therapy is safe and might be helpful in treating pediatric CHF; VSDs have a high incidence of spontaneous improvement |
| Masuda et al,7 2004 | 28 | 14 d | I | Prevention of atherosclerosis by decreasing oxidative stress | Systolic BP decreased, as did serum PGF2α | Infrared sauna therapy might be cardioprotective |
| Imamura et al,8 2001 | 35 | 14 d | II | Impaired endothelial function in those with coronary risk factors | Endothelium-dependent vasodilatation improved; BP and fasting glucose levels decreased | Infrared sauna therapy is safe and improves vascular endothelial function |
| Biro et al,9 2003 | 10 | 14 d | II | Obesity | Despite weight loss, plasma ghrelin and leptin levels did not change | Infrared sauna therapy might blunt neurohormonal effects of weight loss due to calorie restriction |
| Masuda et al,10 2005 | 46 | 28 d | I | Chronic pain | Increased likelihood of return to work; trend toward decreased pain and anger | Infrared sauna therapy might be promising for the treatment of chronic pain |
| Masuda et al,11 2005 | 2 | 35 d | II* | Chronic fatigue syndrome | Fatigue, pain, sleep, and low- grade fever improved | Infrared sauna treatment might be helpful for chronic fatigue syndrome |
BNP—brain natriuretic peptide, BP—blood pressure, CHF—congestive heart failure, FIRS—far-infrared sauna, PGF2α—prostaglandin F2α, PVC—premature ventricular contraction, VSD— ventricular septal defect.
Although this study represents level II evidence, it is very weak owing to small sample size.
Main Message
Congestive heart failure (CHF)
Four papers support the use of infrared sauna therapy for those with CHF.3–6
In one RCT3 (level I evidence), 30 subjects with New York Heart Association (NYHA) class II or III CHF and more than 200 premature ventricular contractions (PVCs) per 24 hours were randomized into treatment and nontreatment groups. Treatment consisted of 10, 15-minute infrared sauna sessions over a 2-week period. After 2 weeks the sauna group had significantly fewer PVCs (mean [SD] = 848 [415] vs 3097 [1033] per 24 hours, P < .01) and lower brain natriuretic peptide (BNP) levels (mean [SD] = 229 [54] pg/mL vs 419 [110] pg/mL, P < .05) compared with the untreated group. Secondary findings included significant improvements to NYHA CHF class (class II/III = 5/15 before treatment vs 15/5 after treatment, P < .01), weight (mean [SD] = 57 [3] kg before vs 56 [3] kg after, P < .05), cardiothoracic ratio (mean [SD] = 59% [1%] before vs 56% [2%] after, P < .01), and left ventricular ejection fraction (LVEF) (mean [SD] = 29% [2%] before vs 33% [2%] after, P < .05); although BP levels appeared to decrease, results did not reach statistical significance. The authors concluded that repeated FIRS treatment improved ventricular arrhythmias in patients with NYHA class II and III CHF.3 Strengths of this study included a control group that was well matched; although the study was not blinded, the control group relaxed in an environment similar to that of the FIRS (but at 24°C) for the same amount of time. All measurements taken after the intervention were performed on the day after the last treatment and can therefore be considered reliable, as this allowed adequate time for rehydration and fluid compartment redistribution. Patients in this study population, however, had asymptomatic PVCs; as such, we cannot generalize these findings to those with symptomatic PVCs, although the improvement in NYHA class is clinically relevant.
Another RCT4 (level I evidence) studied 30 patients with NYHA class II or III CHF: 10 control subjects matched to 20 intervention subjects. The intervention group had 10, 15-minute FIRS treatments over a 2-week period. There were no adverse events and there were no changes in liver or renal function, electrolyte levels, or hematocrit levels. Clinical symptoms improved in 17 out of 20 patients in the intervention group and were unchanged in the remaining 3 patients. Patients’ NYHA classes improved (NYHA class I/II/III = 0/10/10 before treatment vs 1/14/5 after treatment, P = .01), as did their systolic BP (mean [SD] = 107 [22] mm Hg before vs 97 [17] mm Hg after, P = .02). Diastolic BP, body weight, and LVEF did not improve significantly. Brain natriuretic peptide levels decreased significantly (mean [SD] = 441 [444] pg/mL before vs 293 [302] pg/mL after, P < .005). In contrast, the control group did not improve either clinically or in terms of BNP levels. Endothelial function, as assessed by high-resolution ultrasound to determine endothelium-dependent flow-mediated dilation (FMD), improved with treatment (mean [SD] = 4.4% [2.5%] vs 5.7% [2.5%], P = .0006, n = 20). The authors concluded that FIRS treatment improved cardiac function and clinical symptoms in those with CHF and that this improvement was the result of improved vascular endothelial function.4 Strengths of the study were similar to those in the study by Kihara et al.3 Further, before study entry all subjects were in stable clinical condition for at least 1 month, medications had not been changed for at least 2 weeks, and adverse events were defined (dyspnea, angina pectoris, palpitations, hypotension, or dehydration). Although clinical symptoms were assessed using an unvalidated tool, it is reassuring to note the correlation between FMD improvement and both clinical and BNP improvement.
In a sequential, longitudinal, interrupted time series trial5 (level II evidence), 15 hospitalized patients with NYHA class II or III CHF underwent daily 15-minute FIRS treatment for 4 weeks. Sauna treatment was safely completed without any adverse effects. Symptoms improved in 13 of 15 patients (87%); LVEF increased (mean [SD] = 30% [11%] vs 34% [11%], P < .05); every patient’s 6-minute walking distance increased (mean [SD] = 388 [110] m vs 448 [118] m, P < .05); and plasma epinephrine and norepinephrine concentrations both decreased (mean [SD] = 40 [42] pg/mL vs 21 [23] pg/mL, P < .05, 633 [285] pg/mL vs 443 [292] pg/mL, P < .01, respectively). Further, systolic BP and cardiothoracic ratios improved (mean [SD] = 101 [13] mm Hg vs 98 [14] mm Hg, 59% [7%] vs 58% [7%], respectively; P < .05 for all). Changes in weight and BNP levels did not reach statistical significance, nor did changes in NYHA class (class II/III = 3/12 vs 6/9). The authors concluded that FIRS treatment was a safe and effective adjunct therapy for CHF.5 This is the longest study of FIRS therapy for CHF; it is also the only study to document the effect of FIRS therapy on exercise tolerance. It was, however, not randomized and had a small sample size. Further, adverse events were not defined, clinical symptoms were not evaluated using validated questionnaires, and measurements were taken “immediately after” participants’ last sauna sessions.
Although an additional study supports the use of FIRS therapy for neonates with CHF,6 review of that study is beyond the scope of this paper, as the etiology of neonatal CHF is fundamentally different from that of adult CHF. A brief overview is provided in Table 1.3–11
Coronary risk factors
Three papers support the use of FIRS for individuals with coronary risk factors,7–9 which traditionally include hypercholesterolemia, hypertension, diabetes mellitus, obesity, and smoking.
One RTC7 (level I evidence) divided 28 subjects with at least 1 coronary risk factor into 2 matched groups of 14. Group A had 15-minute daily FIRS sessions for 2 weeks, while group B rested in a room-temperature structure for the equivalent amount of time. Systolic BP was significantly reduced in the sauna group after therapy (mean [SD] = 125 [13] mm Hg vs 110 [15] mm Hg, P < .05) and compared with the nontreatment group (110 [15] mm Hg vs 122 [13] mm Hg, P < .05). Postintervention urinary 8-epi prostaglandin F2α, a marker of oxidation, decreased in the sauna group compared with presauna levels (P < .0001; unfortunately the pretreatment levels were not explicitly stated) and compared with the non-sauna group (mean [SD] = 230 [67] vs 380 [101] pg/mg creatinine, P < .0001). No subjects reported feeling ill during the sauna sessions. There were no reductions in body mass index, heart rate, diastolic BP, or hemato-crit, total cholesterol, high-density lipoprotein cholesterol, triglyceride, or fasting plasma glucose levels. The authors concluded that repeated FIRS therapy might protect against oxidative stress and might be a helpful adjuvant in preventing “lifestyle-related diseases.”7 The authors did not state how much time elapsed between the last sauna session and the posttreatment measurement collection.
In a sequential, longitudinal, interrupted time series cohort trial8 (level II evidence), which included a non-randomized control group, 25 men with at least 1 coronary risk factor underwent 10, 15-minute infrared sauna sessions over a 2-week period. Ten additional men without coronary risk factors served as a baseline control and did not receive any sauna treatment. Systolic BP, diastolic BP, weight, and fasting blood glucose concentrations decreased (128 mm Hg vs 124 mm Hg, P < .01; 77 mm Hg vs 72 mm Hg, P < .05; mean [SD] = 75.2 [9.9] kg vs 74.9 [9.9] kg, P < .05; and 99 mg/dL vs 94 mg/dL, P < .05; respectively). Endothelial function was assessed using high-resolution ultrasound to determine brachial artery diameter at rest, during reactive hyperemia, and after sublingual nitroglycerin. Dilation during reactive hyperemia was used to assess FMD. Dilation in response to nitroglycerin was an additional control used to assess endothelium-independent vasodilation. Baseline FMD was impaired in the group with coronary risk factors (mean [SD] = 4.0% [1.7%] vs 8.2% [2.7%], P < .0001) and improved with treatment (4.0% vs 5.8%, P < .001). Endothelium-independent vasodilatation was similar at baseline between the at-risk and control groups and did not change after 2 weeks of sauna therapy. No change was seen in hematocrit, total cholesterol, triglyceride, high-density lipoprotein, uric acid, creatinine, or liver enzyme levels. The authors concluded that FIRS treatment improved impaired vascular endothelial function and suggested a therapeutic role for FIRS treatment in patients with coronary risk factors.8 Standard deviations and P values were not provided for some data reported in the study. With a standard deviation of 9.9 kg, it is difficult to see why a statistically significant decrease in weight (0.3 kg) was reported. An attempt was made to verify the P value with a statistician, but the paper did not contain sufficient data for verification.
In a sequential, longitudinal, interrupted time series trial9 (level II evidence), 10 obese subjects underwent 15-minute daily FIRS sessions and followed an 1800 calorie per day diet for a 2-week period. Despite weight loss, plasma ghrelin and leptin concentrations did not change. The authors concluded, “We consider that repeated sauna therapy is useful in the treatment of obesity.”9 Could sauna treatment have blunted the response of ghrelin and leptin that one would have expected to see during weight loss? Unfortunately the study was of short duration and did not include diet-only or sauna-only control groups. Data provided in a figure imply that mean weight decreased from 83.8 kg to 82.2 kg, and states P<.05, but the actual mean and standard deviation values are not explicitly given. Concerns regarding the previous paper also apply in this study.
Other indications
Additional studies offer evidence of other possible benefits of FIRS therapy.10–15
Chronic pain
One RCT10 (level I evidence) studied 46 patients with chronic pain. All 46 patients received 4 weeks of multidisciplinary inpatient treatment; 22 of the subjects also had 15-minute daily FIRS sessions during those 4 weeks. After 2 years, those in the sauna group were significantly more likely to have returned to work (77% vs 50%, P < .05) and to have improved sleep scores (mean [SD] = 5.4 [3.0] vs 3.5 [2.4], P < .01), and trended toward greater improvement in pain behaviour scores (mean [SD] = 9.9 [1.8] vs 8.7 [1.9], P = .07) and anger scores (mean [SD] = 2.3 [1.6] vs 1.1 [2.0], P = .05). The authors suggested that FIRS therapy might be promising for the treatment of chronic pain.10 The study used validated tools to measure pain, depression, and anger, and subject groups were well matched. Pain behaviour and sleep quality, however, were measured with unvalidated tools. During the 23 months after sauna therapy and before final follow-up, it is not clear if any further sauna treatment was provided as “maintenance therapy.”
Chronic fatigue syndrome
Another paper11 (level II evidence) supported the use of FIRS therapy for chronic fatigue syndrome. It was essentially a case report with a sample size of 2.11
Reproductive system
Far-infrared sauna use is safe and effective for increasing lactation in breastfeeding mothers,12 and FIRS treatment does not appear to be harmful during pregnancy.13–15 Exposure to heat has been shown to decrease sperm counts in men. The specific effect of FIRS use on male sperm counts has never been studied, although increased scrotal temperatures caused by traditional sauna use cause reversible decreases in sperm movement parameters.16
No adverse effects were found (or reported) in any of the studies reviewed for this article.
Limitations
The absence of blinded placebo-control groups is a limitation of all of the studies reviewed here; however, it is not possible to have blinded control groups in studies of sauna therapy. The best studies have matched control groups that, rather than going into a sauna, went into a similar room at 24°C.
In several studies, the length of time between the last sauna sessions and collection of posttreatment measurements was not stated. If measurements such as BP or weight were collected before the subjects had adequately rehydrated, then they would be artificially low, while hematology measurements, such as catecholamine, glucose, cholesterol, and triglyceride levels, would be artificially elevated. The higher-quality studies allowed 1 day for subjects to rehydrate before taking the posttreatment measurements, and also measured serum hematocrit levels as an additional measure of reassurance. In these studies there was no difference in pre-treatment and posttreatment hematocrit levels, thereby assuring us that 1 day is sufficient time to rehydrate.
All of these studies are limited by small sample sizes, short duration, unvalidated symptom scales, and the fact that they were all conducted by the same core research group. Many of these studies relied on a captive (hospitalized) population and none provides any information about real-life uptake.
Conclusion
This review is of importance to those currently suffering from—or interested in preventing—common symptoms such as pain, stress, and fatigue, as well as common chronic diseases such as hypertension, dyslipidemia, diabetes, and obesity. There is limited level I and level II evidence supporting the therapeutic use of FIRSs. There is preliminary but high-quality support of FIRS therapy for treatment of NYHA class II and III CHF and systolic hypertension, and there is fair preliminary support for its role in reducing chronic pain. There is weak preliminary support for FIRS therapy in treating chronic fatigue syndrome. There are inconsistent data regarding the effects of FIRS on weight loss, diastolic BP, and fasting blood glucose levels: some studies show benefit and others show no statistically significant benefit. There is no evidence to support the claim for cholesterol reduction; the published data have consistently found that sauna therapy does not lower cholesterol or triglyceride levels.
Acknowledgment
This work was supported by the University of British Columbia’s Clinical Investigator R3 program. I also thank Dr S. Douglas, Dr J. Pawlovich, and Dr S. Pawlovich for reviewing this article.
Levels of evidence
Level I: At least one properly conducted randomized controlled trial, systematic review, or meta-analysis
Level II: Other comparison trials, non-randomized, cohort, case-control, or epidemiologic studies, and preferably more than one study
Level III: Expert opinion or consensus statements
EDITOR’S KEY POINTS
Because infrared heat penetrates more deeply than warmed air, users of far-infrared saunas (FIRSs) develop a more vigorous sweat at a lower temperature than users of traditional saunas. The cardiovascular demand imparted by thermoregulatory homeostasis is similar to that achieved by walking at a moderate pace. As such, FIRSs might be of particular benefit to those who are sedentary due to various medical conditions like osteoarthritis or cardiovascular or respiratory problems.
Although the evidence is limited, it does suggest a number of benefits of FIRS use, including effects on systolic hypertension, New York Heart Association class and clinical symptoms of congestive heart failure, premature ventricular contractions, brain natriuretic peptide levels, vascular endothelial function, exercise tolerance, oxidative stress, chronic pain, and possibly weight loss and chronic fatigue. No adverse events were reported in any of the studies.
All of the studies reviewed are limited by small sample sizes, short duration, unvalidated symptom scales, the fact that they were conducted by the same core research group, and the fact that many relied on captive hospitalized populations.
POINTS DE REPÈRE DU RÉDACTEUR
Parce que la chaleur infra-rouge pénètre plus pro-fondément que l’air chauffé, les utilisateurs de saunas à infrarouge lointain (SIRL) transpirent plus abondamment à une température moins élevée que les utilisateurs de saunas traditionnels. La demande cardiovasculaire transmise par la thermorégulation équivaut à celle résultant d’une marche à un pas modéré. Ainsi, les SIRL pourraient être particulièrement bénéfiques pour ceux qui sont sédentaires en raison de conditions médicales comme l’arthrose ou les problèmes cardiovasculaires ou respiratoires.
Quoiqu’en nombre limité, les données probantes suggèrent un certain nombre d’avantages à l’utilisation des SIRL, incluant des effets sur l’hypertension systolique, la classe et les symptômes cliniques de l’insuffisance cardiaque, les extrasystoles ventriculaires, le niveau du peptide natriurétique cérébral, l’activité vasculaire endothéliale, la tolérance à l’exercice, le stress oxydatif, la douleur chronique, et peut-être la perte de poids et la fatigue chronique. Aucune des études n’a signalé d’effet indésirable.
Toutes les études révisées sont limitées par la petite taille des échantillons, des courtes durées, des échelles de symptômes non validées, le fait d’avoir été effectuées par le même groupe de chercheurs et le fait que plusieurs dépendaient de populations hospitalisées captives.
Footnotes
This article has been peer reviewed.
Competing interests
None declared
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.Soleil Saunas [advertisement] Just for Canadian Doctors. 2006 Winter;:2. [Google Scholar]
- 2.Soleil Saunas. Sunlight Saunas micron output/infrared frequency chart [webpage] Peachland, BC: Soleil Saunas; 2006. [Accessed 2009 May 27]. Available from: www.soleil-saunas.com/what_is.htm. [Google Scholar]
- 3.Kihara T, Biro S, Ikeda Y, Fukudone T, Shinsato T, Masuda A, et al. Effects of repeated sauna treatment on ventricular arrhythmias in patents with chronic heart failure. Circ J. 2004;68(12):1146–51. doi: 10.1253/circj.68.1146. [DOI] [PubMed] [Google Scholar]
- 4.Kihara T, Biro S, Imamura M, Yoshifuku S, Takasaki K, Ikeda Y, et al. Repeated sauna treatment improves vascular endothelial and cardiac function in patients with chronic heart failure. J Am Coll Cardiol. 2002;39(5):754–9. doi: 10.1016/s0735-1097(01)01824-1. [DOI] [PubMed] [Google Scholar]
- 5.Miyamoto H, Kai H, Nakaura H, Osada K, Mizuta Y, Matsumoto A, et al. Safety and efficacy of repeated sauna bathing in patients with chronic systolic heart failure: a preliminary report. J Card Fail. 2005;11(6):432–6. doi: 10.1016/j.cardfail.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Sugahara Y, Ishii M, Muta H, Egami K, Akagi T, Matsuishi T. Efficacy and safety of thermal vasodilation therapy by sauna in infants with severe congestive heart failure secondary to ventricular septal defect. Am J Cardiol. 2003;92(1):109–13. doi: 10.1016/s0002-9149(03)00483-1. [DOI] [PubMed] [Google Scholar]
- 7.Masuda A, Miyata M, Kihara T, Minagoe S, Tei C. Repeated sauna therapy reduces urinary 8-epi-prostaglandin F(2alpha) Jpn Heart J. 2004;45(2):297–303. doi: 10.1536/jhj.45.297. [DOI] [PubMed] [Google Scholar]
- 8.Imamura M, Biro S, Kihara T, Yoshifuku S, Takasaki K, Otsuji Y, et al. Repeated thermal therapy improves impaired vascular endothelial function in patients with coronary risk factors. J Am Coll Cardiol. 2001;38(4):1083–8. doi: 10.1016/s0735-1097(01)01467-x. [DOI] [PubMed] [Google Scholar]
- 9.Biro S, Masuda A, Kihara T, Tei C. Clinical implications of thermal therapy in lifestyle-related disease. Exp Biol Med (Maywood) 2003;228(10):1245–9. doi: 10.1177/153537020322801023. [DOI] [PubMed] [Google Scholar]
- 10.Masuda A, Koga Y, Hattanmura M, Minagoe S, Tei C. The effects of repeated thermal therapy for patients with chronic pain. Psychother Psychosom. 2005;74(5):288–94. doi: 10.1159/000086319. [DOI] [PubMed] [Google Scholar]
- 11.Masuda A, Kihara T, Fukudome T, Shinsato T, Minagoe S, Tei C. The effects of repeated thermal therapy for two patients with chronic fatigue syndrome. J Psychosom Res. 2005;58(4):383–7. doi: 10.1016/j.jpsychores.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 12.Ogita S, Imanaka M, Matsuo S, Takebayashi T, Nakai Y, Fukumusa H, et al. Effects of far-infrared radiation on lactation. Ann Physiol Anthropol. 1990;9(2):83–91. doi: 10.2114/ahs1983.9.83. [DOI] [PubMed] [Google Scholar]
- 13.Hannuyksela ML, Ellahham S. Benefits and risks of sauna bathing. Am J Med. 2001;110(2):118–26. doi: 10.1016/s0002-9343(00)00671-9. [DOI] [PubMed] [Google Scholar]
- 14.Judge CM, Chasan-Taber L, Gensburg L, Nasca PC, Marchall EG. Physical exposures during pregnancy and congenital cardiovascular malformations. Paediatr Perinat Epidemiol. 2004;18(5):352–60. doi: 10.1111/j.1365-3016.2004.00586.x. [DOI] [PubMed] [Google Scholar]
- 15.Kauppinen K. Facts and fables about sauna. Ann N Y Acad Sci. 1997;813:654–62. doi: 10.1111/j.1749-6632.1997.tb51764.x. [DOI] [PubMed] [Google Scholar]
- 16.Saikhun J, Kitiyanant Y, Vanadurongwan V, Pavasuthipaisit K. Effects of sauna on sperm movement characteristics of normal men measured by computer-assisted sperm analysis. Int J Androl. 1998;21(6):358–63. doi: 10.1046/j.1365-2605.1998.00138.x. [DOI] [PubMed] [Google Scholar]