Abstract
Home visiting programs for at-risk mothers and their infants have proliferated nationally in recent years, yet experimental studies of home visiting have yielded mixed findings. One promising strategy for explicating the effects of early home visiting is to examine moderators of program impacts. This study assessed the roles of maternal depression and attachment insecurity as moderators of the impacts of Healthy Families Alaska home visiting services for at-risk mothers and their infants. At-risk families (N = 325) were randomly assigned to home visiting or community services as usual (n = 162 and 163, respectively). Maternal depression and attachment insecurity (attachment anxiety and discomfort with trust/dependence) were measured at baseline. Maternal psychosocial and parenting outcomes were measured when children were 2 years old via maternal self-report, observation, and review of substantiated reports of child maltreatment. Maternal depression and attachment insecurity interacted in their moderation of program impacts. For several outcomes, home visiting impacts were greatest for non-depressed mothers with moderate to high discomfort with trust/dependence and for depressed mothers with low discomfort with trust/dependence. Implications for practice and policy are discussed.
There is growing appreciation of the challenges of achieving the intended outcomes of home visiting. A 2004 meta-analysis concluded that home visiting positively impacts parenting and child outcomes but that effect sizes were small (Sweet & Applebaum, 2004). Our randomized trial of the Healthy Families America program in Hawaii revealed variations among programs in adhering to the model and modest impacts on maternal psychosocial and parenting outcomes (Duggan, Fuddy, et al., 2004; Duggan, McFarlane et al., 2004). The Nurse-Family Partnership (Olds, 2006) has typically found that positive effects are concentrated in a subset of the participants.
One promising strategy for explicating home visiting is to examine participants' characteristics as moderators of program impacts. There is some evidence that program impacts are greater for inexperienced mothers (DuMont et al., 2006), for mothers with fewer psychological resources (DuMont et al., 2006; Olds, Henderson, Chamberlin, & Tatelbaum, 1986), and for families with partner violence (Eckenrode et al., 2000). Our randomized trial of Hawaii's Healthy Start Program did not find that parity, maternal age, poverty, or overall baseline risk moderated program impacts, but there was some evidence that partner violence moderated program impacts (Duggan, Fuddy, et al., 2004; Duggan, McFarlane, et al., 2004).
Maternal depression may also moderate program impacts. In some of the studies cited above, maternal depression was part of a composite measure of psychological resources (e.g., Olds et al., 1986). It is possible that depression makes it hard for a mother to develop a working relationship with her home visitor and that without separate treatment for depression, home visiting services are insufficient. In these cases, program effectiveness would be reduced for depressed mothers and their children. Alternately, program effectiveness may be enhanced for depressed mothers and their children because there may be greater room for improvement. In the national randomized trial of 17 Early Head Start programs (N = 3001), some of which provided home visiting, program impacts on child-parent interaction were greater when mothers had initially reported more depressive symptoms (Administration for Children and Families, 2002).
Another aspect of maternal functioning that may moderate program impacts is mothers' baseline attachment security, typically measured either via the Adult Attachment Interview (AAI; George, Kaplan, & Main, 1996) or via an adult attachment questionnaire (see Mikulincer & Shaver, 2007, for a review). Both measures are thought to tap aspects of an adult's “internal working models of attachment,” cognitive maps that guide perception and behavior in close relationships (Bowlby, 1973; Bretherton & Munholland, 2008). An adult's internal working models guide her thinking about the extent to which she can and should provide and receive emotional support in close relationships. Thus, maternal attachment security might influence the quality of the relationship that the mother forms with her home visitor, which in turn influences program efficacy. The considerable evidence that attachment, assessed with both the AAI and self-report measures, is linked to the relationships that people form with therapists underscores this possibility (e.g., Dozier, Lomax, Tyrell, & Lee, 2001). On the other hand, mothers with secure working models may well develop supportive, positive relationships with their children without intervention, limiting the effectiveness of home visiting services for them.
Four studies have examined the role of baseline maternal attachment security in mothers receiving home visiting. One study found that within the treatment group, secure mothers (defined by their prenatal AAI) had better parenting and toddler outcomes than insecure mothers (Heinicke et al., 2006). Another study reported that maternal (AAI) attachment did not moderate program impacts for Early Head Start families receiving principally home-based services (Spieker, Nelson, DeKlyen, & Staerkel, 2005). Another study examining two Early Head Start programs revealed the strongest impacts for observed maternal sensitivity (supportiveness) and child involvement of mother in play when mothers reported both depression and a self-reported insecure attachment style (Robinson & Emde, 2004). This study did not distinguish between subtypes of adult attachment insecurity, however.
In the current study, we measure adult attachment style with a questionnaire and separately examine two dimensions of attachment insecurity indicated by the literature as central to the construct. The first dimension pertains to discomfort with interpersonal closeness and with trusting and depending on others. This dimension is most characteristic of adults described as “avoidant” of attachment (Mikulincer & Shaver, 2007). The second dimension pertains to worry that close others are not sufficiently invested in the relationship. This dimension is most characteristic of adults described as having “attachment anxiety” (Mikulincer & Shaver, 2007). Each dimension may moderate home visiting impacts. Mothers who are anxious to be close to others may be particularly open to developing a close relationship with the home visitor, and thereby especially likely to benefit from the intervention. Individuals' discomfort with closeness may also moderate program impacts. For example, two studies have found associations between attachment avoidance and a lack of self-disclosure (Dozier, 1990; Mikulincer & Nachshon, 1991). In the context of home visiting, distancing behavior may make it difficult for the home visitor to understand the mother's needs and to help her. Thus, aspects of attachment avoidance such as discomfort with trust/dependence, may dampen program effects. It is also important to consider that attachment-related moderated program effects may themselves be moderated by concurrent depression (Robinson & Emde, 2004).
The present study draws on data from a recent randomized trial of Healthy Families Alaska (HFAK). Previous findings indicated that programs varied in adherence to the model, that overall impacts were limited, and that impacts were not moderated by maternal demographic characteristics but were attenuated by baseline partner violence (Duggan et al., 2007). In this study, we focused on the outcomes examined in previous reports. Of particular relevance here are previous findings indicating no overall program impacts on maternal substance use, depression, or partner violence, and no program impacts on substantiated child maltreatment. The program significantly decreased the proportion of families with a poor home environment, marginally decreased the proportion of mothers with high parenting stress, and marginally increased maternal sensitivity to infant cues. We first report the baseline prevalence of maternal depression and attachment insecurity. We then examine baseline maternal depression and attachment insecurity as moderators of program impacts on maternal psychosocial outcomes and parenting behaviors assessed two years later.
Method
The Healthy Families Alaska Program
The Healthy Families Alaska (HFAK) program, established in 1995, was administered by the Alaska Department of Health and Social Services (DHHS). It aimed to prevent child maltreatment by promoting healthy family functioning and supportive parenting (Duggan et al., 2007; Healthy Families America, 2001). Following Healthy Families America (HFA) protocol, families in which either parent scored ≥25 on the Kempe Family Stress Checklist were eligible. The HFA model called for voluntary intensive, long-term home visiting, with weekly visits for the first 6-9 months and less frequent visits as family functioning improved (Healthy Families America, 2001).
HFAK staff completed core and wrap-around training by HFA-certified trainers. Core training emphasized building a trusting relationship; developing strategies to encourage positive parenting, build on strengths, address concerns, and promote goal-setting and problem-solving; and using parenting curricula; programs arranged wrap-around training on a range of topics (Healthy Families America, 2001). Home visitors were to promote supportive parent-child interaction and parental empathy through parenting education, role modeling, reinforcement, and referral to community resources. They were to recognize and report child maltreatment, provide support during crises, and screen and refer for developmental delays. Per the management information system, home visitors used parenting curricula in 57% of visits; HFAK did not assess the reliability of reported curriculum use. Home visitors were encouraged to use Individual Family Support Plans to teach problem-solving related to family-initiated goals (Healthy Families America, 2001). Supervisors discussed home visitor observations, actions, and plans in weekly, reflective one-on-one supervision. With supervisor support, home visitors were to encourage parents to seek professional help for partner violence and mental health and substance use problems.
A total of 53 home visitors provided services to HFAK group families during the study; 53% of study families had a single home visitor from enrollment to follow-up, 33% had two home visitors, and 14% had three or more home visitors. Home visitors were 18-51 years old (M = 35.3, SD = 9.1); 30% had a college or graduate degree, 52% had some college training, and 17% had completed high school. They varied in experience as a home visitor; 30% had been a home visitor for less than one year, 26% for one to two years, and 44% for three years or longer.
Setting and Sample
The study occurred in six of seven HFAK program sites, those viewed by the Alaska DHHS as mature enough to achieve program goals. HFAK aimed to reduce the substantiated child maltreatment rate from 15% to 5%. The study was designed to have a power of 80% to detect this difference. Assuming a study follow-up rate of 83%, 316 families were to be recruited and allocated equally to study groups for a final sample of 131 families per group. Mothers eligible for inclusion spoke English, had no previous HFAK services, and agreed to enroll in HFAK if randomized to the program group.
HFAK staff identified 388 eligible families from January 2000 to July 2001, and 364 (94%) mothers consented to participate. Group assignments (HFAK n = 179; control n = 185) were predetermined with randomization site in blocks of six within each program. Program staff obtained randomization assignments by phone after obtaining participant consent, and then informed mothers of group assignment. Program mothers were linked to home visitors; control group mothers were referred to other parenting and family-support services as was usually done for eligible families when HFAK enrollment was full. All communities had public health nursing and a range of infant learning, parenting, and family support programs. Programs for pregnant women and families of newborns were not as comprehensive or intensive as HFAK. According to follow-up interviews, about 50% of control group mothers received public health nursing and about 33% accessed a center- or home-based parenting program.
Research staff completed baseline maternal interviews within one month of enrollment. Overall, 325 (90%) of those randomized were interviewed at baseline (HFAK n = 162; control n = 163), 12 declined and 27 could not be located. Thus, 84% of mothers in the 388 eligible families completed baseline interviews; this is comparable to usual HFAK participation rates.
The treatment and control groups were comparable at baseline in most respects (see Table 1). Over 50% of all mothers lived below the poverty level (1% of mothers reported no household income; 27% reported household income ≥ $25,000). Program mothers were significantly less likely than controls to be depressed at baseline (22% and 33%, respectively).
Table 1.
Baseline Characteristics of HFAK and Control Groups
| Characteristic | HFAK (n = 162) |
Control (n = 163) |
Test of group differencesa |
|
|---|---|---|---|---|
| Maternal age: M (SD) | 23.4 (5.7) | 23.7 (5.7) | t (322) = 0.49 | |
| Mother graduated from high school | 59% | 57% | χ2 (1) = 0.16 | |
| Below poverty level | 57% | 58% | χ2 (1) = 0.07 | |
| Household income: M (SD) | 17,956 (13,917) | 19,162 (14,469) | t (285) = −0.72 | |
| Index child is/will be first birth | 48% | 53% | χ2 (1) = 0.89 | |
| Index child is female | 56% | 48% | χ2 (1)= 1.79 | |
| Mother's primary race/ethnicity | χ2 (3) = 1.99 | |||
| Alaska Native | 23% | 20% | ||
| Caucasian | 54% | 56% | ||
| Multiracial | 10% | 7% | ||
| Other | 13% | 17% | ||
| Parents married or living together | 50% | 56% | χ2 (1) = 1.11 | |
| Maternal depression | 22% | 33% | χ2 (1) = 4.29* | |
| Attachment anxiety: M (SD) | 33.0 (7.8) | 33.8 (8.4) | t (320) = 0.87 | |
| Discomfort with trust/dependence: | 14.8 (3.9) | 15.8 (5.6) | t (321) = 1.31 | |
| M (SD) | ||||
| Partner violence | 32% | 34% | χ2 (1) = 0.10 | |
| Maternal substance use | 55% | 57% | χ2 (1) = 0.08 | |
Note: HFAK = Healthy Families Alaska program group.
N's ranged from 285 to 325.
p < .05
Overall, 86% (n = 278) of families had a follow-up assessment; for 90% of these (n = 249), the biological mother completed the follow-up assessment because she was the primary caregiver. To test moderated program impacts for all outcomes except child maltreatment, the sample was limited to these 249 families (HFAK n = 126; control n = 123). These program and control mothers did not differ significantly on any baseline characteristic except that HFAK mothers were less likely to have been married to or living with the infant's father (52% vs. 64%, p < .01). This factor was controlled in analyses of moderated program impacts.
For analyses of moderated program impacts on substantiated child maltreatment, the sample was limited to families who lived in Alaska at least six months each year (n = 297 of the original 325) because maltreatment data came from Alaska records. These 297 mothers were less likely to be high school graduates (56% vs. 82%, p < .01) and more likely to be positive for substance use (71% vs. 44%, p < .01) than the 28 mothers who were excluded. This subsample comprised 147 (91%) of HFAK families and 150 (92%) of control families; these program and control mothers did not differ significantly on any baseline characteristic.
Procedure
Data were collected by researchers who were blind to families' group status. Baseline data came from intake records and from 90-minute, home-based, maternal interviews. Follow-up data collected when the children were two years old came from (a) Alaska Office of Children's Services (OCS) child welfare reports; (b) 3.5-hour home-based assessments including the follow-up maternal interview, observation of the home environment, and an observational assessment of mother-child interaction.
Measures
Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977)
This 20 item, self-report instrument is the most widely used measure of depressive symptoms in community-based studies. Respondents indicate how often in the past week they have experienced a symptom (e.g., “I was bothered by things that usually don't bother me”) on a 4-point scale (0 = rarely or none of the time; 3 = most or all of the time). Concurrent and construct validity, high internal consistency (α's .85 to .90) and test-retest reliability (r's = .51 to .67 in 2-to 8-week intervals) have been reported (Radloff, 1977). In this sample, internal consistency (α) was .78. A commonly-used cutoff for high depressive symptoms is a score ≥ 16 (McDowell & Newell, 1996; Radloff, 1977). Because higher cut points have been recommended to reduce false positives (McDowell & Newell, 1996), we used a cutoff of ≥ 24 as indicative of clinically significant depression.
Attachment Style Questionnaire (ASQ; Feeney, Noller, & Hanrahan, 1994)
The ASQ consists of 40 items rated on a scale of 1 (totally disagree) to 6 (totally agree). Items include, “I find it hard to trust people” and “I worry a lot about my relationships.” ASQ scores have been linked in theoretically predicted ways to maternal depression, stress, and readiness to end abusive relationships (Feeney, Alexander, Noller, & Hohaus, 2003; Meredith, Strong, & Feeney, 2006; Shurman & Rodriguez, 2006). We selected the ASQ because it was designed to tap general (rather than romantic) attachment security and because its developer had reported good test-retest reliability (r's = .75 to .80) and good internal consistency (Feeney et al., 1994). Also, we had used the ASQ in earlier home visiting research with a large sample of similarly at-risk mothers and infants in Hawaii. In both studies, we used the 34 items from four of the ASQ's original subscales: discomfort with closeness, confidence in self, need for approval, and preoccupation with relationships. We omitted the subscale, relationships as secondary to accomplishments, to reduce respondent burden.
Confirmatory factor analysis revealed that the original ASQ subscale structure was a poor fit for our at-risk samples in Hawaii and Alaska, according to four indices of fit (χ2, RMSEA, CFI, and Tucker-Lewis Index). Because of the compelling evidence of two major dimensions of attachment insecurity, we conducted exploratory factor analysis using a maximum likelihood algorithm and a two-factor solution to identify these factors. All items were included in the first step; those with factor loadings ≥ .40 were retained. The model was rerun, again retaining only items with factor loadings ≥ .40, until the loadings of all remaining items were ≥ .40. Items with equal loadings ≥ .40 on both factors were dropped. Varimax orthogonal rotation and promax (oblique) rotation generated similar factor structures; we report the promax rotation results.
The analysis resulted in two factors containing items that directly tap the two major dimensions of attachment insecurity: attachment anxiety and avoidance. The factor that we labeled “attachment anxiety,” an 11-item factor with loadings of .44 to .75 (α =.80), includes items indicating anxiety about others not being available (e.g., “I worry that others won't care about me as much as I care about them”). The factor that we labeled “discomfort with trust/dependence,” a 5-item factor with loadings of .41 to .87, initially had low internal consistency (α = .55). After dropping one item with a low item-total correlation, the resulting four-item factor had high internal consistency (α = .88). The discomfort with trust/dependence factor includes items indicating discomfort with trust and dependence (e.g., “I find it difficult to depend on others”). Our exploratory factor analysis of ASQ data in the Hawaii study yielded a similar factor structure. In the Hawaii study, the attachment anxiety factor has 16 items, of which 11 are the same as in the current study and three had high loadings on both the anxiety and discomfort with trust/dependence factors in the current study. In the Hawaii study and the current study, the discomfort with trust/dependence factors are identical. Recent analyses of the Hawaii data indicated that maternal attachment anxiety and discomfort with trust/dependence factors were stable over time and that greater maternal attachment anxiety predicted lower rates of program drop-out (McFarlane, Burrell, Derauf, Fuddy, & Duggan, 2008).
The Revised Conflict Tactics Scale (CTS2; Straus, 2007)
The CTS2 is a 39-item self-report measure of the frequency of behaviors in the past year on several subscales: psychological aggression, negotiation, physical assault, injury, and sexual coercion. This widely-used instrument has strong evidence of content and construct validity (Straus, 2007), good internal consistency (subscale α's =.79 - .95; Straus, 1990), and subscale test-retest correlations of .49 to .90 (Straus, 2007). We created a binary partner violence variable, defined as positive if either partner engaged in three or more incidents of violence toward the other in the past year. Mothers without a partner were defined as negative for partner violence.
Parenting Stress Checklist-Short Form (PSI-SF; Abidin, 1990)
Respondents indicate agreement with 36 items on a 5-point scale (1 = strongly agree, 5 = strongly disagree; sample item, “My child rarely does things for me that make me feel good”). The PSI-SF total score is the sum of its three subscales: parental distress, parent-child dysfunctional interaction, and difficult child. The total score's validity, internal consistency (α = .91) and test/retest reliability over 6 months (r = .84) have been reported (Abidin, 1990; Haskett, Ahern, Ward, & Allaire, 2006). In this study, total score internal consistency (α) was .92. Per Abidin (1990), we defined high parenting stress as a total score of at least the 90th percentile.
Infant-Toddler Home Observation for Measurement of the Environment (IT-HOME; Elardo & Bradley, 1981)
This 45-item, semi-structured interview/observational measure reflects the quality of the home environment. The interviewer codes each item on a binary scale (yes/no). Total scores are calculated by summing the number of positive responses. Validity, internal consistency, and test-retest reliability for the total score have been well established (K-R 20 = .89; ICC = .76 for 12 versus 24 months) (Caldwell & Bradley, 1984; Elardo, Bradley & Caldwell, 1975). In the current study, internal consistency was strong (α = .75). In the analyses reported here, a total IT-HOME score ≤ 33 was considered an indicator of a poor home environment and potential neglect. This definition is consistent with previous research on the HOME (e.g., Bradley et al., 1989).
The CAGE (an acronym for “cut down,” “annoyed,” “guilt,” and “eye opener”; Mayfield, McLeod, & Hall, 1974)
The CAGE is a 4-item fixed response (yes/no) measure of lifetime experience of problems associated with alcohol use (e.g., people annoyed you by criticizing your drinking). Internal consistency is good (median α =.74 across 22 samples; Shields & Caruso, 2004), as is test-retest reliability after seven days (.95 in a community sample; Teitelbaum & Carey, 2000). Using two or more positive responses to denote problem alcohol use, the CAGE has reported sensitivities of 43% to 94% and specificities of 70% to 97% (Fiellin, Reid, & O'Connor, 2000). In this study, baseline problem alcohol use was defined as self-reported alcohol use in the year prior to pregnancy and a CAGE score ≥ 2 (Mayfield, McLeod, & Hall, 1974); problem alcohol use at follow-up was defined as self-reported alcohol use in the previous year and a CAGE score ≥ 2.
Addiction Severity Index (ASI; McLellan, et al., 1992)
The ASI is a semi-structured measure of illicit substance use and resulting problems. Concurrent validity has been reported (Alterman, et al., 2000), as has strong internal consistency (α = .69 - .84 on the substance use domains; Leonhard, Mulvey, Gastfriend, & Shwartz, 2000) and test-retest reliability (kappa = .83; McLellan, et al., 1992). We defined illicit drug use at baseline as any such use in the past two years and at follow up as any such use in the past year. A mother was defined as positive for substance use problems if she was positive for problem alcohol use or illicit drug use.
The Nursing Child Assessment Teaching Scale (NCATS; Barnard, 1994)
The NCATS was administered in the home to measure the quality of the mother's behavior while teaching the child a new skill such as putting together a simple puzzle during an interaction of up to six minutes. The scale incorporates 73 binary (yes/no) items in six subscales. Construct and predictive validity have been established as have internal consistency (α = .87 for the total score), and test-retest reliability (.85 for the total parent score and .55 for the total infant score) (Barnard, 1994; Sumner & Spietz, 1995). In this study, the measure was coded live by certified research staff who had been trained to a criterion of 90% (at least 66 of 73 items coded correctly during five consecutive observations). Paralleling other studies of moderated impacts of home visiting services, we focus on one of the subscales, maternal sensitivity to cues (Robinson & Emde, 2004; Spieker et al., 2005). Higher scores indicate greater sensitivity to infant cues.
Substantiated child maltreatment
Data on substantiated child protective services reports were gathered from the Alaska Office of Children's Services (OCS) management information system. We provided subject identifying data to OCS for computer matching using its standard protocol. OCS returned a list of perfect and partial matches with data on report date, type, and whether or not the report was substantiated. Research staff unaware of family group assignment made the final determination on partial matches using additional demographic information.
Statistical Power
Because the study was not originally powered to test for moderation, statistical power to detect moderation for each outcome was estimated through bootstrapping (Walters & Campbell, 2005). This method allowed us to estimate the power of our sample size to detect the moderated effects actually observed. Power to detect moderation for psychosocial outcomes ranged from 46% (high parenting stress) to 48% (substance use) to 60% (partner violence) to 97% (maternal depression). Power to detect moderation for parenting outcomes ranged from 38% (maternal sensitivity to cues) to 63% (poor home environment) to 89% (substantiated child maltreatment). Because study power to detect moderated effects was low for five of the seven outcomes, our analyses, while theoretically- and empirically-based, must also be considered exploratory.
Results
Baseline Maternal Depression, Attachment Anxiety, and Discomfort with Trust/Dependence
Of all mothers, 28% met criteria for depression at baseline. Attachment anxiety and discomfort with trust/dependence scores varied substantially. Of a possible range of 11 to 66 for anxiety, mothers scored from 12 to 59 (M = 33.4, SD = 8.1). Of a possible range of 4 to 24 for discomfort with trust/dependence, mothers scored from 4 to 24 (M = 15.1, SD = 3.7).
Depressed mothers scored higher than non-depressed mothers on attachment anxiety (M = 38.4, SD = 7.9 vs. M = 31.5, SD = 7.3, t (317) = 7.39, p < .001), and discomfort with trust/dependence (M = 17.1, SD = 3.7 vs. M = 14.3, SD = 3.4, t (318) = 6.41, p < .001). Depression was moderately correlated with attachment anxiety (rpb = .38, p < .001) and discomfort with trust/dependence (rpb = .34, p < .001). Attachment anxiety and discomfort with trust/dependence were moderately correlated (r = .36, p < .001).
Baseline depression was less prevalent among teenage mothers and those negative for partner violence, and trended toward being less prevalent among mothers who were Alaskan Native (see Table 2). Baseline attachment anxiety was lower among mothers negative for partner violence. Baseline discomfort with trust/dependence was lower for first time mothers and for mothers negative for partner violence. There were trends toward higher attachment anxiety and discomfort with trust/dependence scores among mothers who lived below the poverty level.
Table 2.
Family Baseline Characteristics by Baseline Maternal Depression, Attachment Anxiety, and Discomfort with Trust/dependence
|
|
Depressed |
Attachment Anxiety |
Discomfort with trust/dependence |
||||
|---|---|---|---|---|---|---|---|
| Characteristic | n | % | M | SD | M | SD | |
| Maternal age | |||||||
| < 20 | 107 | 18** | 32.5 | 7.8 | 14.7 | 3.5 | |
| ≥ 20 | 217 | 32 | 33.9 | 8.2 | 15.4 | 3.8 | |
| Maternal education | |||||||
| Less than 12 years | 136 | 28 | 34.1 | 8.2 | 15.3 | 3.8 | |
| High school graduate | 189 | 27 | 33.0 | 8.0 | 14.9 | 3.5 | |
| Poverty | |||||||
| Above poverty level | 138 | 24 | 32.4 | 8.0† | 14.7 | 3.4† | |
| Below poverty level | 187 | 30 | 34.2 | 8.1 | 15.4 | 3.8 | |
| Index Child Birth Order | |||||||
| Not first birth | 160 | 29 | 34.0 | 8.2 | 15.6 | 3.7* | |
| First birth | 165 | 26 | 32.9 | 8.0 | 14.7 | 3.6 | |
| Mother's primary ethnicity | |||||||
| Alaska Native | 70 | 19† | 33.3 | 8.1 | 14.5 | 3.4 | |
| Caucasian | 180 | 27 | 33.6 | 8.3 | 15.1 | 3.8 | |
| Multiracial | 27 | 46 | 32.4 | 7.8 | 15.3 | 4.1 | |
| Other | 48 | 30 | 33.8 | 7.7 | 15.8 | 3.2 | |
| Parents married or living together |
|||||||
| Yes | 172 | 25 | 33.7 | 8.1 | 15.1 | 3.8 | |
| No | 153 | 31 | 33.2 | 8.7 | 15.2 | 3.6 | |
| Partner violence | |||||||
| No | 156 | 22** | 32.3 | 8.0*** | 14.7 | 3.8** | |
| Yes | 148 | 39 | 35.8 | 7.8 | 15.9 | 3.3 | |
| Maternal substance use | |||||||
| No problem | 137 | 26 | 32.7 | 8.6 | 14.8 | 3.9 | |
| Problem | 175 | 30 | 33.9 | 7.8 | 15.3 | 3.5 | |
Note: Tests of group differences (χ2 for differences by depression and t-tests for differences by attachment anxiety and discomfort with trust/dependence) were performed for each group, with significant differences denoted with superscripts.
p < .10
p < .05
p < .01
p < .001
Prevalence of and Associations among Outcomes
Adverse maternal outcomes were prevalent (see Table 3). Poor HOME scores were significantly less prevalent for home visited families (20% vs. 31%, p < .001). High parenting stress showed a trend toward lower prevalence among home visited mothers (18% vs. 29%, p < .10). Home visited mothers showed a trend toward greater sensitivity to infant cues (M = 94.1, SD = 1.0 vs. M = 9.2, SD = 1.1, p < .10). Correlations among outcomes were low to moderate in both the HFAK and control groups, and in no case was any correlation in one group significantly different from that in the other group (r's = .01 - .43, mean r = .14).
Table 3.
Prevalence of Outcomes Overall and by Group
| Outcome | Overall | HFAK | Control | AOR/B | 95% CI |
|---|---|---|---|---|---|
| Partner Violence | 20% | 19% | 22% | 0.82 | 0.50, 1.34 |
| Substance Use | 30% | 28% | 33% | 0.80 | 0.55, 1.16 |
| High Parenting Stress | 24% | 18% | 29% | 0.62 | 0.35, 1.09† |
| Depressed | 18% | 17% | 22% | 0.66 | 0.37, 1.17 |
| Poor HOME | 24% | 20% | 31% | 0.51 | 0.36, 0.72*** |
| Maternal Sensitivity to Cues | 9.3 ± 1.1 | 9.4 ± 1.0 | 9.2± 1.1 | 0.20 | −0.04, 0.46† |
| Substantiated Child Maltreatment | 16% | 16% | 17% | 0.89 | 0.47, 1.68 |
Note: Results of linear or logistics regressions, controlling for mother's baseline relationship status (married to or living with the infant's father at baseline). HFAK = Healthy Families Alaska program group.
p < .10
p < .001
Moderated Program Impacts on Maternal Psychosocial Outcomes: Partner Violence, Maternal Substance Use, High Parenting Stress, and Depression
To examine moderation, we built regression models incorporating hypothesized moderators (i.e. baseline depression, attachment anxiety, and discomfort with trust/dependence) using conventional group-by-moderator interaction terms. For the continuous attachment anxiety and discomfort with trust/dependence measures, scores were centered at the mean and at one standard deviation above/below the mean (Aiken & West, 1991).
For each binary outcome, we used logistic regression modeling to estimate the adjusted odds ratio (AOR) for home visited versus control families in light of significant interactions of home visiting × maternal depression, attachment anxiety, and/or discomfort with trust/dependence. An AOR of 1 for the home visiting group variable indicates that the odds of the outcome were the same for home visited and control families. Standard logistic regression model diagnostics, including Pearson residuals and observed versus fitted values, confirmed model assumptions (linearity of the log odds) and fit. For the continuous outcome, maternal sensitivity to cues, we used linear regression modeling to estimate the adjusted mean difference (AMD) in scores for home visited versus control mothers. Standard diagnostics, including assessment of residuals and observed versus fitted values and normal probability plots of the residuals, confirmed model assumptions (linearity of means) and fit and conformity with assumptions of normality for linear regression models.
For each outcome, we began by testing a fully specified regression model incorporating all three-way interaction terms that included the intervention (i.e., home visiting × depression × attachment anxiety, home visiting × depression × discomfort with trust/dependence, and home visiting × attachment anxiety × discomfort with trust/dependence) and all two-way interactions and main effects. We used a step-down approach (Aiken & West, 1991) to identify the most parsimonious model of moderation of program impacts on each outcome. We first dropped non-significant (p > .05) three-way interactions, then dropped non-significant two-way interactions that were not a component of significant three-way interactions. Parents' baseline relationship was included as a covariate. We used robust variance estimates to account for any correlation of outcomes within program site. The robust variance estimates adjust the models' standard errors to account for the possibility that, although observations are independent across program sites, they might not be independent within program site (Liang & Zeger, 1986). For partner violence and substance use, we had both baseline and follow-up measures. Model tests for these outcomes with and without these baseline measures were the same; we report the results for the latter.
We used a 10% statistical significance criterion for a series of correlated tests examining an intervention effect, and we did not use statistical corrections to correct for chance. We justified this approach by noting that (a) the analyses were exploratory and (b) we did not examine a large number of outcomes beyond those reported here.
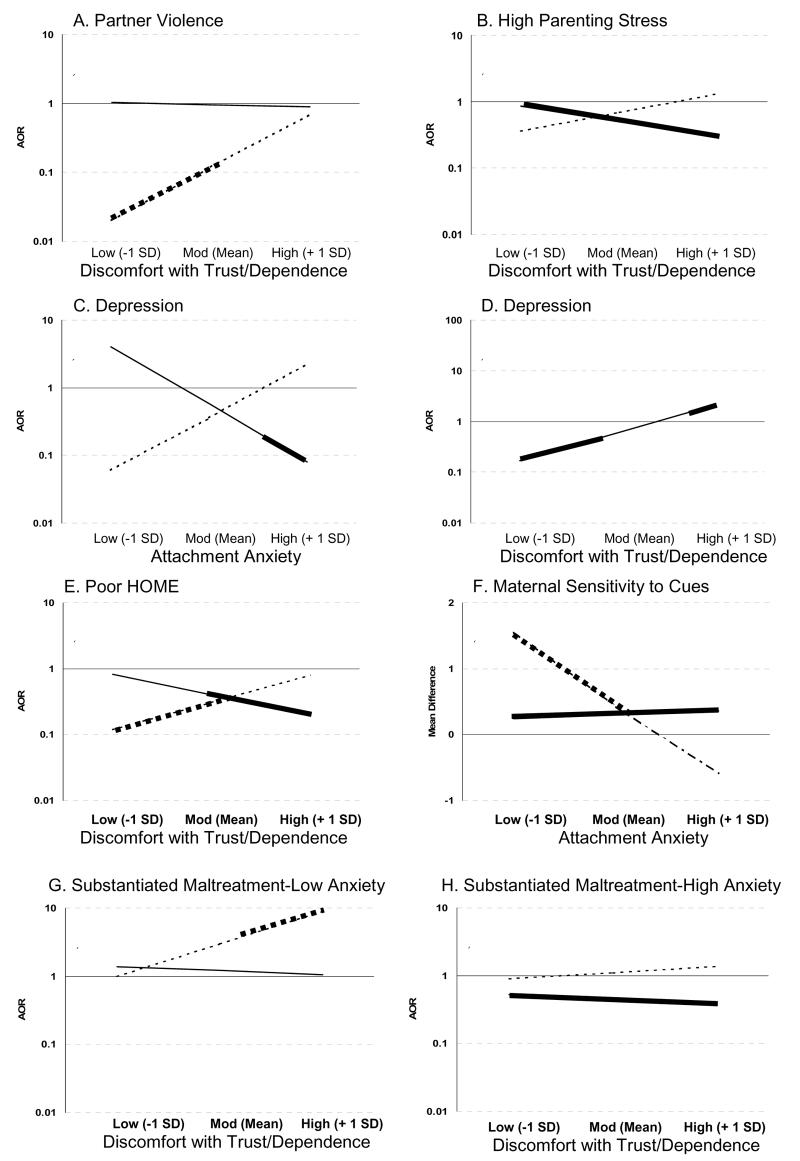
Significant three-way interactions of home visiting × baseline depression × attachment anxiety or discomfort with trust/dependence emerged for all four maternal psychosocial outcomes. First, for partner violence, there was a significant three-way interaction of home visiting × baseline depression × discomfort with trust/dependence (AOR = 1.56, p < .01; see Figure 1, Panel A). For mothers who were depressed at baseline, as discomfort with trust/dependence increased, the impact of home visiting on reducing partner violence was attenuated (AOR = 1.53, p < .05). Among these depressed mothers, home visiting reduced partner violence for those who reported low to moderate levels of discomfort with trust/dependence at baseline (AOR ≤ 0.12 for mothers with discomfort with trust/dependence scores of 15 or lower; this region of significance is indicated by the bold portion of the dotted line in Figure 1, Panel A). In contrast, among mothers who were not depressed at baseline, the impact of home visiting did not vary by discomfort with trust/dependence (AOR = 0.98, p = .92), and for none of these non-depressed mothers was there a program impact on partner violence (AOR = 1.00, p = .99).
Figure 1.
Moderated program impacts on maternal psychosocial outcomes and parenting behaviors. Dotted lines represent AORs for mothers depressed at baseline. Solid line represents AORs for mothers not depressed at baseline. Bold portions of lines indicate regions of significance for home visited vs. control group mothers (p < .10).
Panel A: Program impacts on partner violence as moderated by baseline maternal depression and discomfort with trust/dependence.
Panel B: Program impacts on high parenting stress as moderated by baseline maternal depression and discomfort with trust/dependence.
Panel C: Program impacts on maternal depression as moderated by baseline maternal depression and attachment anxiety.
Panel D: Program impacts on maternal depression as moderated by maternal discomfort with trust/dependence.
Panel E: Program impacts on poor HOME scores as moderated by baseline maternal depression and discomfort with trust/dependence.
Panel F: Program impacts on maternal sensitivity to cues as moderated by baseline maternal depression and attachment anxiety.
Panel G: Program impacts on substantiated child maltreatment as moderated by baseline maternal depression and discomfort with trust/dependence for mothers with low attachment anxiety (1 SD below the mean).
Panel H: Program impacts on substantiated child maltreatment as moderated by baseline maternal depression and discomfort with trust/dependence for mothers with high attachment anxiety (1 SD above the mean).
Second, for maternal substance use, there was a significant three-way interaction of home visiting × baseline depression × discomfort with trust/dependence (AOR = 1.38, p < .05). However, two-way interactions of home visiting × discomfort with trust/dependence were not significant for mothers who were depressed nor for those not depressed at baseline. Further, for neither depressed nor non-depressed mothers overall was there a statistically significant impact of home visiting on substance use.
Third, for high parenting stress, there was a significant three-way interaction of home visiting × baseline depression × discomfort with trust/dependence (AOR = 1.34, p < .01; see Figure 1, Panel B). Among mothers who were depressed at baseline, home visiting impact did not vary by discomfort with trust/dependence (AOR = 1.15, p = .15), nor was there an impact of home visiting on parenting stress for these mothers (AOR = 1.88, p = .52). Among mothers who were not depressed at baseline, home visiting impact did not vary by discomfort with trust/dependence (AOR = 0.88, p = .12). There was, however, a significant intervention impact such that home visiting reduced high parenting stress for all nondepressed mothers (AOR = 0.48, p < .05; see bold, solid line in Figure 1, Panel B).
Fourth, for depression at follow-up, two significant interactions emerged. First, there was a significant three-way interaction of home visiting × depression × attachment anxiety (AOR = 1.60, p < .05; see Figure 1, Panel C). For mothers who were depressed at baseline, the impact of home visiting did not vary by attachment anxiety (AOR = 1.26, p = .17) nor did home visiting reduce the likelihood of depression at follow-up (AOR = 0.95, p = .95). In contrast, among mothers who were not depressed at baseline, as attachment anxiety increased, so did the impact of home visiting in preventing depression at follow-up (AOR = 0.78, p < .05). Among non-depressed mothers with relatively high attachment anxiety scores, home visiting significantly reduced the likelihood that they would be depressed two years later (AOR ≤ 0.22 for mothers with anxiety scores of 37 or higher, as indicated by the bold portion of the solid line in Figure 1, Panel C).
A two-way interaction of home visiting × discomfort with trust/dependence also emerged. For all mothers, discomfort with trust/dependence moderated the impact of home visiting on depression at follow-up (AOR = 1.37, p < .001; see Figure 1, Panel D). For mothers with low to moderate discomfort with trust/dependence (scores of 14 or lower), the program significantly reduced depression at follow-up (AOR ≤ 0.44). For mothers with moderate discomfort with trust/dependence (scores of 15 to 17), home visiting did not have an impact on depression at follow-up. For mothers with high discomfort with trust/dependence (scores of 18 or higher), the program actually increased depression at follow-up (AOR ≥ 1.55).
In sum, discomfort with trust/dependence moderated home visiting impacts on all four psychosocial outcomes. For three outcomes – partner violence, substance use, and high parenting stress – its moderating effects were conditioned on maternal baseline depression. For the fourth outcome – depression at follow-up – discomfort with trust/dependence moderated program impacts for all mothers. For this outcome, attachment anxiety also moderated home visiting impacts, conditioned on maternal depression at baseline. Among mothers not depressed at baseline, attachment anxiety enhanced home visiting impacts in preventing depression two years later.
Moderated Program Impacts on Parenting Behaviors: Poor HOME scores, Maternal Sensitivity to Cues, and Substantiated Child Maltreatment
First, for poor HOME scores, there was a significant three-way interaction of home visiting × baseline depression × discomfort with trust/dependence (AOR = 1.52, p < .01; see Figure 1, Panel E). Among mothers who were depressed at baseline, as discomfort with trust/dependence increased, there was a trend for home visiting impacts to be attenuated (AOR = 1.27, p< .10); for mothers with low to moderate discomfort with trust/dependence (scores of 16 or lower), home visiting reduced poor HOME scores (AOR ≤ 0.39). In contrast, among mothers who were not depressed at baseline, home visiting impact in reducing poor HOME scores increased as discomfort with trust/dependence increased (AOR = 0.83, p < .001); for mothers with moderate to high discomfort with trust/dependence (scores of 14 or higher), home visiting reduced poor HOME scores (AOR ≤ 0.47).
Second, for the continuous outcome of maternal sensitivity to infant cues, there was a significant three-way interaction of home visiting × depression × attachment anxiety (B = −0.08, p < .05; see Figure 1, Panel F). Among mothers who were depressed at baseline, home visiting impact was attenuated as attachment anxiety increased (B = −0.08, p < .05); home visiting increased maternal sensitivity to cues (minimum change in mean score = 0.42) among those depressed mothers with low attachment anxiety (scores of 33 or lower) only. In contrast, among mothers who were not depressed at baseline, the impact of home visiting on maternal sensitivity to cues did not vary by attachment anxiety (B = 0.01, p = .65); home visiting increased maternal sensitivity for these mothers overall (B = 0.24, p < .05).
Third, for substantiated child maltreatment, two three-way interactions achieved the level of at least a trend. First, there was a marginally significant interaction of home visiting × depression × discomfort with trust/dependence AOR = 1.22, p < .10). Second, there was a significant interaction of home visiting × attachment anxiety × discomfort with trust/dependence (AOR = 0.99, p < .05). Figure 1, Panels G and H, illustrate the combined effects of these interactions for depressed and non-depressed mothers with low and with high attachment anxiety.
Among mothers with low attachment anxiety, for those depressed at baseline, home visiting impact varied significantly by discomfort with trust/dependence (AOR = 1.31, p < .05; see Figure 1, Panel G). For the subset of depressed mothers with high discomfort with trust/dependence (scores of 16 or higher), home visiting increased substantiated child maltreatment (AOR ≥ 3.94). In contrast, for mothers with low attachment anxiety who were not depressed at baseline, the impact of home visiting did not vary by discomfort with trust/dependence (AOR = 1.08, p = .34) and home visiting did not have an impact on substantiated maltreatment (AOR = 1.53, p = .31).
Among mothers with high attachment anxiety, for those depressed at baseline, home visiting impact did not vary by discomfort with trust/dependence (AOR = 1.05, p = .74), and home visiting did not have an impact on substantiated maltreatment (AOR = 1.23, p = .78; see Figure 1, Panel H). Among mothers with high attachment anxiety who were not depressed at baseline, home visiting impact did not vary by discomfort with trust/dependence (AOR = 0.86, p = .22), but there was a trend for home visiting to reduce substantiated maltreatment (overall AOR = 0.35, p < .10).
The finding of a higher incidence of substantiated maltreatment for a subset of home visited versus control families was not due to greater reporting by home visitors. In the home visited group, 23 families had a total of 40 substantiated reports. Home visitors made the referral for only 3 of these substantiated reports. None of these three reports were for families in the subgroup with a higher incidence of maltreatment for home visited versus control families.
In sum, the moderated effects of home visiting by maternal depression, attachment anxiety, and discomfort with trust/dependence varied across parenting outcomes. For poor HOME scores, discomfort with trust/dependence attenuated home visiting impacts among depressed mothers but enhanced impacts among non-depressed mothers. For the second observational measure – maternal sensitivity to cues – attachment anxiety attenuated home visiting impacts among depressed mothers but did not moderate program impacts among non-depressed mothers. Interactive effects were most complex for home visiting impacts on substantiated child maltreatment. Discomfort with trust/dependence moderated program impacts only among depressed mothers with low attachment anxiety. Specifically, among depressed mothers with low attachment anxiety, the likelihood of substantiated child maltreatment was higher for home visited than control mothers when discomfort with trust/dependence was also high. Attachment anxiety increased program impacts among non-depressed mothers; among non-depressed mothers with moderate to high attachment anxiety, home visiting decreased substantiated child maltreatment.
Robustness of Moderated Program Effects with Poverty Controlled
Because attachment anxiety and discomfort with trust/dependence were marginally associated with poverty, we tested the robustness of our models controlling for poverty. For all outcomes, the moderated program impacts were robust.
Discussion
At enrollment, mothers varied widely in attachment insecurity and over a quarter had CES-D scores suggestive of clinically significant depression. These findings demonstrate participant heterogeneity on factors that might influence program engagement and outcomes. Although our previous analyses of the full sample identified program impacts on only three of the outcomes examined here, the present study found program effects moderated by both maternal depression and attachment insecurity for six of the seven outcomes studied.
Among non-depressed mothers, home visiting reduced high parenting stress and increased maternal sensitivity to their infant's cues. Other benefits were limited to non-depressed mothers with moderate to high attachment anxiety or discomfort with trust/dependence. Among non-depressed mothers with moderate to high attachment anxiety, home visiting reduced depression at follow-up and decreased substantiated child maltreatment. Among those with moderate to high discomfort with trust/dependence, home visiting reduced poor HOME scores.
Among depressed mothers, home visiting benefits were more apparent in those with low to moderate attachment insecurity. Home visiting improved maternal sensitivity to cues among depressed mothers with low to moderate attachment anxiety; it decreased depression, partner violence, and poor HOME scores in those with relatively low discomfort with trust/dependence.
Two subgroups appeared to experience adverse effects. Among mothers with high discomfort with trust/dependence, home visiting increased the likelihood of depression at follow-up. In depressed mothers with both low attachment anxiety and high discomfort with trust/dependence, home visiting increased the likelihood of substantiated child maltreatment.
The patterns of moderation we identified differed from those of two previous studies. Robinson and Emde (2004) found that Early Head Start was most effective in promoting maternal sensitivity in mothers who were depressed and held insecure attachment attitudes. We found that home visiting did not enhance maternal sensitivity to cues for mothers with both depression and moderate to high attachment anxiety; rather, it enhanced maternal sensitivity in mothers with neither or only one of these attributes. This difference in findings may relate to methods. The current study used a higher threshold for depression than did Robinson and Emde, and it distinguished between attachment anxiety and attachment avoidance or discomfort with trust/dependence.
Our findings differed from those of Spieker et al. (2005), who found that depression, but not attachment insecurity, enhanced program impacts on maternal sensitivity. The current study found that the moderating effect of each was conditioned by the other. This difference in findings may be attributable to differences in methods. The current study used self-reports of attachment style, whereas Spieker et al. used AAI classifications.
The present study's findings of a moderate correlation between attachment anxiety and discomfort with trust/dependence was higher than that reported for attachment anxiety and avoidance measured with a focus on romantic relationships (Brennan, Clark, & Shaver, 1998). This suggests that attachment anxiety and discomfort with trust/dependence (or avoidance) might relate to each other differently when considering general rather than romantic relationships. It also suggests that there is a group of mothers who are both anxious and uncomfortable with trust/dependence for whom intervention impacts might be different than for mothers who are anxious or uncomfortable with trust/dependence only. We tested for this, but found only one significant three-way interaction of home visiting by attachment anxiety by discomfort with trust/dependence. A new questionnaire measuring a “profoundly distrustful” adult attachment style may better illuminate program effects for such mothers (Holmes & Lyons-Ruth, 2006).
Methodological Considerations
The sample was limited to high risk families where the mother was willing to take part in home visiting. Although 94% of mothers in eligible families agreed to participate, we do not know the generalizability of findings to families unwilling to do so. It was not possible to collect child welfare services data from other states; analysis for this outcome was limited to families who lived in Alaska for most of the follow-up period. Even so, the sample was identified through routine HFAK population-based screening and assessment and thus might be generalizable to at-risk families typically served by programs similar to HFAK.
Although close monitoring revealed no deviations from the family group assignment protocol, the percent of mothers with CES-D scores ≥ 24 was higher in the control versus the HFAK group at baseline. Random assignment is never perfect; it is possible that this group difference was due to chance. Alternately, because assignment preceded the baseline interview, it might have increased depressive symptoms among control group mothers.
A single source – maternal report – was used to measure hypothesized moderators and several outcomes. Use of a single source could have given rise to correlated measurement error, which might have influenced how program effects appear to have been moderated. However, the study also used observational parenting measures and official records of child maltreatment. The validity of study findings is enhanced by the coherence of the findings across data sources.
Follow-up was limited to outcomes when children were two years old. Long-term follow-up is needed to assess the stability of outcomes and to determine if other effects emerge later.
Study power may be a concern. Bootstrapping showed that power to detect interactive effects was low for several outcomes. It may be that some nonsignificant interactions involving these variables would have proven significant with a larger sample. Thus, our analyses must be considered exploratory and conclusions should be drawn accordingly.
Implications for Practice and Policy
Targeted mothers were heterogeneous in terms of depression and attachment insecurity and these attributes influenced how families benefited. Our findings, like those of Robinson and Emde (2004) and Spieker et al. (2005) indicate that these factors should be considered when tailoring preventive intervention services. Given the complex nature of the findings, and that they differ from and converge with previous research, replication is essential.
Home visiting is complex and costly. Screening for maternal depression and attachment insecurity might be useful for identifying subsets of currently targeted families for whom less intensive approaches are adequate. Non-depressed mothers with low attachment anxiety and avoidance did not seem to benefit from home visiting services. It is possible that, even with the other parenting risks identified in screening and assessment, these mothers do not need home visiting, perhaps because they are able to access other support services.
Another subset of families – those in which the mother was depressed and had high levels of discomfort with trust/dependence – appeared to suffer some adverse consequences. This also suggests the importance of baseline screening for depression and attachment insecurity. For these families, home visiting alternatives and enhancements should be tested. This finding points to the need for research to ascertain not only whether preventive interventions achieve intended outcomes, but also whether they do harm. It also supports the perspective that home visiting should be targeted to families for whom evidence shows a favorable risk/benefit ratio, or tailored to family needs (Berlin, Brooks-Gunn, & McCarton; 1998; Guterman, 1999).
Programs such as HFA screen and assess families for parenting risks such as history of abuse as a child using instruments such as the Family Stress Checklist that do not explicitly assess parental attachment security. Research is needed to test instruments that assess attachment insecurity. This could begin by testing the feasibility and utility of existing instruments such as the ASQ and the Relationship Questionnaire-Clinical Version (Holmes & Lyons-Ruth, 2006).
Home visiting programs aim to improve a range of outcomes. Evaluative research should test moderation of impacts on the full range of intended outcomes to determine if achievement of some outcomes is coupled with adverse consequences for others. Research is needed to elucidate how maternal depression and attachment insecurity moderate impact. Research is needed to elucidate the influence of depression and attachment insecurity on home visit content and quality, the home visitor's relationship with the mother, and the mother's engagement in services.
Acknowledgments
This research was supported by the Alaska Mental Health Trust Authority and the Alaska State Department of Health and Social Services. Manuscript preparation was also supported by NIMH K01MH70378 to Lisa J. Berlin, and by sabbatical support from the University of Maryland to Jude Cassidy.
References
- Abidin RR. Parenting Stress Index Short Form Test Manual. Pediatric Psychology Press; Charlottesville, VA: 1990. [Google Scholar]
- Administration for Children and Families . Making a difference in the lives of children and families: The impacts of Early Head Start Programs on young children and their families. US Department of Health and Human Services; Washington, DC: 2002. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Sage; Newbury Park, CA: 1991. [Google Scholar]
- Alterman AI, McDermott PA, Cook TG, Cacciola JS, McKay JR, McLellan AT, et al. Generaliziability of the clinical dimensions of the Addiction Severity Index to nonopioid-dependent patients. Psychology of Addictive Behaviors. 2000;14:287–294. doi: 10.1037//0893-164x.14.3.287. [DOI] [PubMed] [Google Scholar]
- Barnard K. The Nursing Child Assessment Satellite Training (NCAST) Teaching Scale. University of Washington, School of Nursing; Seattle, WA: 1994. [Google Scholar]
- Berlin LJ, Brooks-Gunn J, McCarton C. The effectiveness of early intervention: Examining risk factors and pathways to enhanced development. Preventive Medicine. 1998;27:238–245. doi: 10.1006/pmed.1998.0282. [DOI] [PubMed] [Google Scholar]
- Bowlby J. Attachment and loss: Vol. 2. Separation. Basic Books; New York: 1973. [Google Scholar]
- Bradley RH, Caldwell BM, Rock SL, Ramey CT, Barnard KE, Gray A, et al. Home environment and cognitive development in the first three years of life: A collaborative study involving six sites and three ethnic groups in North America. Developmental Psychology. 1989;25:217–235. [Google Scholar]
- Brennan KA, Clark CL, Shaver PR. Self-report measurement of adult attachment: An integrative overview. In: Simpson JA, Rholes WS, editors. Attachment theory and close relationships. Guilford; New York: 1998. pp. 46–76. [Google Scholar]
- Bretherton I, Munholland K. Internal working models in attachment relationships: Elaborating a central construct in attachment theory. In: Cassidy J, Shaver PR, editors. Handbook of attachment: Theory, research, and clinical applications. 2nd ed. Guilford; New York: 2008. pp. 102–127. [Google Scholar]
- Caldwell BM, Bradley RH. Home observation for measurement of the environment. University of Arkansas; Little Rock: 1984. [Google Scholar]
- Dozier M. Attachment organization and treatment use for adults with serious psychopathological disorders. Development and Psychopathology. 1990;2:47–60. [Google Scholar]
- Dozier M, Lomax L, Tyrrell CL, Lee SW. The challenge of treatment for clients with dismissing states of mind. Attachment and Human Development. 2001;3:62–76. doi: 10.1080/14616730122704. [DOI] [PubMed] [Google Scholar]
- Duggan AK, Caldera D, Rodriguez K, Burrell L, Rohde C, Crowne SS. Impact of a statewide home visiting program to prevent child abuse. Child Abuse and Neglect. 2007;31:829–852. doi: 10.1016/j.chiabu.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Duggan AK, Fuddy L, Burrell L, Higman SM, McFarlane E, Windham A, et al. Randomized trial of a statewide home visiting program to prevent child abuse: Impact in reducing parental risk factors. Child Abuse and Neglect. 2004;28:623–643. doi: 10.1016/j.chiabu.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Duggan AK, McFarlane E, Fuddy L, Burrell L, Higman SM, Windham A, et al. Randomized trial of a statewide home visiting program to prevent child abuse: Impact in preventing child abuse and neglect. Child Abuse and Neglect. 2004;28:597–622. doi: 10.1016/j.chiabu.2003.08.007. [DOI] [PubMed] [Google Scholar]
- DuMont K, Mitchell-Herzfeld S, Greene R, Lee E, Lowenfels A, Rodriguez M. Healthy Families New York (HFNY) randomized trial: Impacts on parenting after the first two years. State Office of Children and Family Services; New York: 2006. [Google Scholar]
- Eckenrode JJ, Ganzel B, Henderson CR, Jr., Smith E, Olds DL, Powers J, et al. Preventing child abuse and neglect with a program of nurse home visitation: The limiting effects of domestic violence. Journal of the American Medical Association. 2000;284:1385–1391. doi: 10.1001/jama.284.11.1385. [DOI] [PubMed] [Google Scholar]
- Elardo R, Bradley RH. The Home Observation for Measurement of the Environment (HOME) Scale: A review of the research. Developmental Review. 1981;1:113–145. [Google Scholar]
- Elardo R, Bradley R, Caldwell BM. The relation of infants' home environments to mental test performance from six to thirty-six months: A longitudinal analysis. Child Development. 1975;46:71–76. [Google Scholar]
- Feeney JA, Alexander R, Noller P, Hohaus L. Attachment insecurity, depression, and the transition to parenthood. Personal Relationships. 2003;10:475–493. [Google Scholar]
- Feeney JA, Noller P, Hanrahan M. Assessing adult attachment. In: Sperling MB, Berman WH, editors. Attachment in adults: Clinical and developmental perspectives. Guilford; New York: 1994. pp. 128–152. [Google Scholar]
- Fiellin DA, Reid MC, O'Connor PG. Screening for alcohol problems in primary care: A systematic review. Archives of Internal Medicine. 2000;160:1977–1989. doi: 10.1001/archinte.160.13.1977. [DOI] [PubMed] [Google Scholar]
- George C, Kaplan N, Main M. Adult Attachment Interview protocol. 3rd ed. University of California; Berkeley: 1996. Unpublished manuscript. [Google Scholar]
- Guterman NB. Enrollment strategies in early home visitation to prevent physical child abuse and neglect and the “universal versus targeted” debate: A meta-analysis of population-based and screening-based programs. Child Abuse and Neglect. 1999;23:863–890. doi: 10.1016/s0145-2134(99)00062-9. [DOI] [PubMed] [Google Scholar]
- Haskett ME, Ahern LS, Ward CS, Allaire JC. Factor structure and validity of the Parenting Stress Index – Short Form. Journal of Clinical Child and Adolescent Psychology. 2006;35:302–312. doi: 10.1207/s15374424jccp3502_14. [DOI] [PubMed] [Google Scholar]
- Healthy Families America . Healthy Families America training participant's manual-program manager, supervisor, family support worker and assessment worker. Prevent Child Abuse America; Chicago, IL: 2001. [Google Scholar]
- Heinicke CM, Goorsky M, Levine M, Ponce V, Ruth G, Silverman M, et al. Pre- and postnatal antecedents of a home-visiting intervention and family developmental outcome. Infant Mental Health Journal. 2006;27:91–119. doi: 10.1002/imhj.20082. [DOI] [PubMed] [Google Scholar]
- Holmes B, Lyons-Ruth K. The Relationship Questionnaire-Clinical Version (RQCV): Introducing a profoundly-distrustful attachment style. Infant Mental Health Journal. 2006;27:310–325. doi: 10.1002/imhj.20094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonhard C, Mulvey K, Gastfriend DR, Shwartz M. Addiction Severity Index: A field study of internal consistency and validity. Journal of Substance Abuse Treatment. 2000;18:129–135. doi: 10.1016/s0740-5472(99)00025-2. [DOI] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- Mayfield D, McLeod G, Hall P. The CAGE Questionnaire: Validation of a new alcoholism screening instrument. American Journal of Psychiatry. 1974;131:1121–1123. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- McDowell I, Newell C. Depression. In: McDowell I, Newell C, editors. Measuring health: A guide to rating scales and questionnaires. 2nd ed. Oxford University Press; New York: 1996. pp. 238–286. [Google Scholar]
- McFarlane E, Burrell, Derauf DC, Fuddy L, Duggan A. Home visiting for at-risk families of newborns: Home visitor and maternal attachment security as factors for engagement; Poster session presented at the annual meetings of the Society for Prevention Research; San Francisco, CA. May, 2008. [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Meredith PJ, Strong J, Feeney JA. The relationship of adult attachment to emotion, catastrophizing, control, threshold, and tolerance in experimentally-induced pain. Pain. 2006;120:44–52. doi: 10.1016/j.pain.2005.10.008. [DOI] [PubMed] [Google Scholar]
- Mikulincer M, Nachshon O. Attachment styles and patterns of self-disclosure. Journal of Personality and Social Psychology. 1991;61:321–332. [Google Scholar]
- Mikulincer M, Shaver PR. Attachment in adulthood: Structure, dynamics, and change. Guilford; New York: 2007. [Google Scholar]
- Olds DL. The Nurse-Family Partnership: An evidence-based preventive intervention. Infant Mental Health Journal. 2006;27:5–25. doi: 10.1002/imhj.20077. [DOI] [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: A randomized trial of nurse home visitation. Pediatrics. 1986;78:65–78. [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Robinson J, Emde RN. Mental health moderators of Early Head Start on parenting and child development: Maternal depression and relationship attitudes. Parenting: Science and Practice. 2004;4:73–97. [Google Scholar]
- Shields AL, Caruso JC. A reliability induction and reliability generalization study of the CAGE questionnaire. Educational and Psychological Measurement. 2004;64:254–270. [Google Scholar]
- Shurman LA, Rodriguez CM. Cognitive-affective predictors of women's readiness to end domestic violence relationships. Journal of Interpersonal Violence. 2006;21:1417–1439. doi: 10.1177/0886260506292993. [DOI] [PubMed] [Google Scholar]
- Spieker S, Nelson D, DeKlyen M, Staerkel F. Enhancing early attachments in the context of Early Head Start: Can programs emphasizing family support improve rates of secure infant-mother attachments in low-income families? In: Berlin LJ, Ziv Y, Amaya-Jackson L, Greenberg MT, editors. Enhancing early attachments: Theory, research, intervention and policy. Guilford; New York: 2005. pp. 250–275. [Google Scholar]
- Straus MA. The conflict tactics scales and its critics: An evaluation and new data on validity and reliability. In: Straus MA, Gelles RJ, editors. Physical violence in American families: Risk factors and adaptations to violence in 8,145 families. Transaction; New Brunswick, NJ: 1990. pp. 49–73. [Google Scholar]
- Straus MA. Conflict Tactics Scales. In: Jackson NA, editor. Encyclopedia of Domestic Violence. Routledge; New York: 2007. pp. 190–197. [Google Scholar]
- Sumner G, Spietz AL. NCAST Caregiver/Parent-Child Interaction Teaching Manual. 2nd Edition NCAST Publications, University of Washington; Seattle, WA: 1995. [Google Scholar]
- Sweet MA, Applebaum MI. Is home visiting an effective strategy? A meta-analytic review of home visiting programs for families with young children. Child Development. 2004;75:1435–56. doi: 10.1111/j.1467-8624.2004.00750.x. [DOI] [PubMed] [Google Scholar]
- Teitelbaum LM, Carey KB. Temporal stability of alcohol screening measures in a psychiatric setting. Psychology of Addictive Behaviors. 2000;14:401–404. doi: 10.1037//0893-164x.14.4.401. [DOI] [PubMed] [Google Scholar]
- Walters SJ, Campbell MJ. The use of bootstrap methods for estimating sample size and analyzing health-related quality of life outcomes. Statistics in Medicine. 2005;24:1075–102. doi: 10.1002/sim.1984. [DOI] [PubMed] [Google Scholar]