Abstract
Background
The time to skill deterioration between primary training/retraining and further retraining in Cardiopulmonary resuscitation (CPR) and automated external defibrillation (AED) for lay-persons is unclear. The Public Access Defibrillation (PAD) Trial was a multi-center randomized controlled trial evaluating survival after CPR-only vs. CPR+AED delivered by onsite non-medical volunteer responders in out-of-hospital cardiac arrest.
Aims
This sub-study evaluated the relationship of time between primary training/retraining and further retraining on volunteer performance during pretest AED and CPR skill evaluation.
Methods
Volunteers at 1260 facilities in 24 North American regions underwent training/retraining according to facility randomization, which included an initial session and a refresher session at approximately 6 months. Before the next retraining, a CPR and AED skill test was completed for 2729 volunteers. Primary outcome for the study was assessment of global competence of CPR or AED performance (adequate vs not adequate) using Chi-square tests for trends by time interval (3, 6, 9, and 12 months). Confirmatory (GEE) logistic regression analysis, adjusted for site and potential confounders.
Results
The proportion of volunteers judged to be competent did not diminish by interval (3,6,9,12 months) for either CPR or AED skills. After adjusting for site and potential confounders, longer intervals before to further retraining was associated with a slightly lower likelihood of performing adequate CPR but not with AED scores.
Conclusions
After primary training/retraining, the CPR skills of targeted lay responders deteriorate nominally but 80% remain competent up to one year. AED skills do not significantly deteriorate and 90% of volunteers remain competent up to one year.
Keywords: automated external defibrillator (AED), bystander CPR, cardiac arrest, cardiopulmonary resuscitation (CPR), skill retention, training, public access defibrillation
1. Introduction
The incidence of cardiac arrest is estimated to be 55 EMS-treated events per 100,000 population1 or roughly 220,000 cases per year in North America. Early defibrillation when applied effectively by laypersons is effective2 and bystander cardiopulmonary resuscitation (CPR) is one of the most powerful predictors of increased survival.3 Organized and efficient training of lay people in the use of automated external defibrillators (AEDs) and CPR is essential if we are to maximize the benefit of these actions at the time of sudden cardiac death.
The skills required in basic cardiopulmonary resuscitation (CPR) have been characterized as difficult to teach 4, 5 and once taught, difficult to retain.4, 6–15 The component skills needed to use an automated external defibrillator (AED) have been less well studied but may be easier to learn.16–21 The American Heart Association currently recommends that CPR and AED retraining in PAD programs “should occur at least once every 2 years. More frequent training is recommended and may be dictated by local policies and regulations”.22 However, objective information on learning and retention is lacking, especially in public settings with organized emergency response by motivated volunteers. The Public Access Defibrillation (PAD) trial2, 23 measured retention of CPR and AED skills prospectively at each training and retraining session. The purpose of this PAD sub-study was to describe the degradation in performance of CPR and AED skills between primary training and maintenance retraining according to time interval.
2. Methods
Summary of PAD Methods
The PAD Trial was a multi-center, prospective, randomized, controlled clinical trial evaluating the effect of volunteer, non-medical responder AED use on survival from out-of-hospital cardiac arrest. The study involved 24 clinical centers in North America and was coordinated by the Clinical Trials Center at the University of Washington in Seattle. Institutional review boards at University of Washington and at each local center reviewed and approved the study.
The methods and primary results have been previously published.23 Briefly, a total of 1260 facilities such as office complexes, shopping centers, hotels, golf courses, etc. were recruited to participate. Volunteers without a duty to respond to health emergencies and without an advanced medical degree were recruited to respond to medical emergencies. Informed consent was obtained before training. All volunteers were instructed in assessment of cardiac arrest, accessing 911 and providing CPR until EMS arrival. Half the facilities were randomized to receive additional training in AED use.
CPR and AED training
Training was structured and standardized. Primary training included an initial training course using guidelines closely following those of the American Heart Association HeartSaver AED course (with or without the AED) and a refresher training session. Any approved course was acceptable if the following guidelines were followed: class length 3–4 hours depending on course content, student/instructor ratio of not more that 6:1 and preferably 4:1, no more than 12 students per class, scenario-based training, individual skills practice of approximately 30 minutes, lecture/demonstration (preferably using a skills video) of not more than 45 minutes, and a minimum instructor qualification of BLS instructor certification. PAD training guidelines did not require proficiency in a pulse check or any written evaluation. Primary training included refresher training planned 3–6 months after the initial training course and included evaluation and training to correct any deficiencies. The primary refresher training actually occurred approximately 6 months after the primary initial training. Facilities were randomized to deliver maintenance retraining 3, 6, 9 or 12 months after primary initial and refresher training were completed. Volunteers who received maintenance retraining from 1.5 to 13.5 months later are the subject of this report.
Maintenance retraining sessions commenced with an individual skills test prior to any retraining information allowing the volunteer to demonstrate CPR (and/or AED) skills without any prompts while the instructor evaluated the skills and completed a checklist. After the test, the instructor provided remediation focusing on identified deficits in performance.
Proficiency was evaluated in five core CPR skills and five core AED skills. These skills were scored using a CPR and AED performance skills checklist which included criteria for passing each skill.(Table 1). In addition, each volunteer was given a global assessment of competence of the effectiveness of CPR and AED performance. Specifically, instructors determined if the CPR performed “would have been adequate to produce perfusion”. Improper sequence was not considered incompetence as long as compressions were adequate to provide perfusion. In AED testing, trainers evaluated global assessment of competence as delivery of a successful shock regardless of minor mistakes in other components not critical to that specific outcome.
Table 1.
Component criteria for evaluation of skill performance
| CPR skill components | |
| assess responsiveness | |
| access 911 | |
| adequate ventilation/chest rise | |
| proper hand placement | |
| adequate compression depth | |
| AED skill components | |
| bare chest for pad placement | |
| place pads correctly | |
| clears self | |
| verbally clears area | |
| shock patient within 90 sec of AED arrival |
Volunteer Inclusion and Exclusion Criteria
For this analysis we included only volunteers who completed primary training (including initial and refresher sessions) and one maintenance retraining session. We excluded volunteers whose maintenance retraining occurred earlier than 1.5 months or later than 13.5 months after primary training, volunteers who were trained in one intervention but tested in the other and volunteers for whom the testing protocol was not followed (e.g. volunteers tested in groups rather than individually). In addition, interim data quality control checks identified a small number of sites with artificially high scores (i.e., 100% proficiency in all volunteers on all skills because e.g., “volunteers were allowed to start over again if a mistake was made”). Remedial measures were taken with these sites and volunteers retrained prior to remediation were excluded.
Outcomes
The primary outcome of this study was the assessment of overall competence of CPR or AED skill retention as determined by the instructor prior to maintenance retraining. Secondary endpoints included successful demonstration of individual skill components (Table 1), a simple composite score of a maximum of 5 (1 point for each individual skill) and time required to retrain to proficiency.
Statistical Analysis
Volunteer facilities were initially randomized to receive maintenance retraining, at 3, 6, 9 or 12 months following primary training; however, due to the larger than expected training/retraining burden in the study, centers were unable to adhere closely to assigned groups. Thus, outcomes were evaluated with respect to the actual time interval since initial training (1.5–4.5, 4.5–7.5, 7.5–10.5, and 10.5–13.5 months), rather than the assigned interval. Volunteers excluded from analysis were grouped according to study participation status (i.e., active, moved, dropped/unknown). Means (± SD) and percents summarizing measured characteristics were computed for volunteers within each interval. Proportions, means (± SD), and error bar plots were generated to describe patterns of skill retention by maintenance retraining group for the specified outcome measures. Volunteer-level tests were performed for both primary and secondary outcome measures: Chi-square tests for trend were computed for the overall assessment and individual component measures, the non-parametric Kruskal-Wallis test was computed for the composite scores and ANOVA F-tests for linearity were computed for total testing/retraining time. Confirmatory analyses using logistic Generalized Estimating Equations (GEE) models were performed for the AED and CPR global assessment measures. An exchangeable correlation structure was used to model correlation within a given community unit. Models were adjusted for site, however this required excluding a small number of sites which had too few volunteers to obtain stable estimates. Potential confounders and important covariates/interactions were included in the model via backward stepwise regression, using p=.05 as the entry criterion. No adjustment was made for multiple comparisons. To illustrate an age-by-retraining-interval interaction, volunteers were grouped into four age quartiles and an error bar plot generated to display mean predicted probabilities from the logistic model with 95% confidence intervals in each of the four retraining intervals. All analyses were performed using SPSS (SPSS, Inc, Chicago, IL), Stata (Stata Corporation, College Station, TX), or S-Plus (S-Plus 2000, Mathsoft, Inc., Cambridge, MA).
3. Results
This analysis was performed on data collected from August, 2000 through April, 2003. Of a volunteer cohort of 8,788 in the CPR-only group and 11,758 in the CPR+AED group, 977 and 1,752 volunteers respectively had primary training and maintenance retraining and met additional inclusion criteria. Table 2 shows the numbers of volunteers excluded for each criterion by participation status. Approximately 80% of volunteers did not receive both primary training and maintenance retraining. Of the 6065 volunteers without any maintenance retraining, 71% appeared to be actively participating in the study, 24% had moved from the facility in which they had volunteered and 5% had dropped out of the study for other reasons.
Table 2.
Volunteers excluded from analyses
| Total | |
|---|---|
| Volunteers with Primary Initial Course | 20546 |
| No Primary Refresher training | 10209 |
| No Maintenance retraining | 6065 |
| Protocol Violation | 826 |
| Crossover | 174 |
| Outside 1.5–13.5 mo. training window | 543 |
| Volunteers included | 2729 |
Volunteer characteristics by participation status are shown in Table 3. There were no differences in baseline characteristics of the four groups compared by time interval to maintenance retraining (Table 4). The primary and secondary outcome measures for CPR and AED skills for each maintenance retraining interval are detailed in Table 5. There were no clinically significant trends across intervals. Overall, 81% of volunteers analyzed were able to perform acceptable CPR (i.e., were likely to provide perfusion in the instructor’s judgment). For AED skills, approximately 90% of volunteers were judged likely to be able to deliver an effective shock at each interval and this figure did not diminish over time.
Table 3.
Characteristics of Volunteers by Exclusion status
| Analyzed1 | Active2 | Moved3 | Other Drop/Unknown4 | |
|---|---|---|---|---|
| N | 2729 | 4313 | 1480 | 271 |
| Mean (± SD) age | 41.1 (13.8) | 41.8 (13.8) | 35.3(14.1) | 36.5 (17.3) |
| % male | 53% | 53% | 58% | 51% |
| % white | 83% | 79% | 79% | 85% |
| % randomized to CPR only | 36% | 43% | 44% | 40% |
| % Previous CPR, First Aid or advanced training | 66% | 55% | 64% | 60% |
| % aided in emergency or seizure | 60% | 53% | 59% | 49% |
| % with friend or family with OOHCA | 51% | 48% | 46% | 45% |
| % with English as native language | 94% | 95% | 95% | 92% |
| % attended college or higher | 73% | 73% | 72% | 54% |
| % operate a computer | 89% | 86% | 87% | 84% |
| % with back problems | 8% | 9% | 9% | 9% |
| % with arthritis | 5% | 6% | 5% | 7% |
| % security guard | 17% | 13% | 22% | 19% |
| % lifeguard/aqua instructor | 5% | 2% | 4% | 19% |
volunteers included in analyses
active volunteers excluded from analysis, largely due to missing primary refresher and/or maintenance retraining
volunteers who moved from the unit
volunteers who discontinued participation for other reasons or were lost to follow-up.
Table 4.
Baseline characteristics (covariates) of analyzed groups by time strata (n = 2729)
| 1.5 – 4.5 | 4.5 – 7.5 | 7.5 – 10.5 | 10.5 – 13.5 | |
|---|---|---|---|---|
| N | 457 | 769 | 873 | 630 |
| Months from primary initial to primary refresher training: Mean (±SD) | 6.4 (±4.1) | 6.3 (±3.7) | 6.7 (± 3.5) | 6.5 (± 3.3) |
| Months from completion of primary training to maintenance retraining: Mean (±SD) | 3.5 (±0.6) | 6.1 (±0.8) | 8.9 (±0.8) | 12.1 (±0.8) |
| % Previous CPR, FA or advanced training | 62 | 66 | 68 | 64 |
| % male | 52 | 50 | 53 | 56 |
| % white | 76 | 85 | 83 | 84 |
| Age, Mean (± SD) | 41 (±14) | 41 (±15) | 41 (±13) | 41 (± 14) |
| % using computer/video aids (2nd retraining) | 1 | 3 | 0 | 2 |
| % with previous mock or real arrest (1st retrain) | 6 | 9 | 11 | 9 |
| % previous mock or real cardiac arrest (2nd retrain | 9 | 16 | 16 | 15 |
| % randomized to CPR only | 39 | 37 | 33 | 35 |
| % aided in emergency or seizure | 60 | 57 | 61 | 60 |
| % with friend or family with OOHCA | 49 | 50 | 51 | 51 |
| English as native language | 91 | 95 | 95 | 93 |
| % attended college or higher | 73 | 73 | 74 | 73 |
| % operate a computer | 89 | 88 | 90 | 88 |
| % with back problems | 11 | 8 | 7 | 7 |
| % with arthritis | 5 | 6 | 5 | 3 |
| % trained to proficiency (first retrain) | 99 | 98 | 99 | 100 |
| % security guard | 27 | 14 | 15 | 14 |
| % lifeguard/aqua instructor | 5 | 8 | 5 | 2 |
Table 5.
| Table 5a. Primary and secondary outcome measures by maintenance retraining interval for CPR skills | ||||||
|---|---|---|---|---|---|---|
| Total | 1.5 – 4.5 | 4.5 – 7.5 | 7.5 – 10.5 | 10.5 – 13.5 | p-value | |
| N | 2729 | 457 | 769 | 873 | 630 | |
| % Competent by global assessment (likely to provide perfusing CPR) | 81% | 82% | 81% | 82% | 80% | .5021 |
| % assessing responsiveness | 87% | 89% | 85% | 89% | 84% | .2611 |
| % accessing 911 | 71% | 72% | 71% | 71% | 68% | .1581 |
| % providing adequate ventilation | 81% | 83% | 81% | 81% | 78% | .0471 |
| % placing hands properly | 82% | 86% | 84% | 79% | 80% | .0041 |
| % demonstrating adequate compression depth | 88% | 91% | 88% | 87% | 87% | .0591 |
| Mean Composite CPR score | 4.1 (1.1) | 4.2 (1.1) | 4.1 (1.2) | 4.1 (1.1) | 4.0 (1.2) | .0122 |
| Time (min.) to test & train, CPR (N=801) | 4.9 (2.7) | 4.6 (2.3) | 4.7 (2.5) | 5.2 (3.1) | 5.2 (2.9) | .0383 |
| Table 5b. Primary and secondary outcome measures by maintenance retraining interval for AED skills | ||||||
|---|---|---|---|---|---|---|
| All | 1.5–4.5 mo | 4.5–7.5 mo | 7.5–10.5 mo | 10.5–13.5 mo | p-value | |
| N | 1752 | 278 | 482 | 581 | 411 | |
| % competent by global assessment (likely to provide effective shock) | 91% | 89% | 92% | 90% | 91% | .8931 |
| % baring chest for pad placement | 96% | 97% | 95% | 94% | 98% | .8371 |
| % placing pads correctly | 84% | 82% | 84% | 83% | 86% | .2081 |
| % clearing self | 84% | 86% | 86% | 83% | 84% | .2221 |
| % verbally clearing area | 75% | 73% | 76% | 74% | 78% | .2711 |
| % able to shock within 90 sec. | 80% | 82% | 80% | 80% | 78% | .2621 |
| Mean Composite AED score | 4.2 (1.1) | 4.2 (1.1) | 4.2 (1.1) | 4.1 (1.2) | 4.2 (1.1) | .4452 |
| Time to test & train, AED (min.) (N=1342) | 7.2 (3.4) | 6.6 (3.5) | 7.1 (3.4) | 7.1 (3.2) | 8.2 (3.5) | <.0013 |
Chi-square test for linearity
Kruskal-Wallis test
ANOVA F-test for linearity
Figure 1 shows the overall proportion of volunteers judged to be competent overall by the instructor for each maintenance retraining interval. When the continuous maintenance retraining interval measure (time in months) was analyzed using the logistic model and adjusting for potential confounders, a statistically and clinically significant association was seen between time to maintenance retraining and overall CPR performance. This interaction was dependent on the age of the volunteer (i.e. there was an interaction between retraining interval and age). Results of the model estimation are reported in Table 6a. Not surprisingly, volunteers achieving proficiency during the primary refresher training were three times more likely to perform adequate CPR compared to those who didn’t (p=.006) and lifeguards were roughly 2.5 times more likely to perform adequately relative to others (p=.005). Better CPR performance was also associated with male sex (p=.044), white race (p=.034) and previous experience responding to an emergency or seizure (p<.001). The age-by-time interaction is illustrated in Figure 2 using predicted probabilities from the model. In general, CPR performance appeared to be lower in the longest interval. Among volunteers in the highest age category, this decrease was smaller; however, the estimated probability of performing adequate CPR in this group is lower than that of the other groups over all periods – markedly so in the first three. Longer intervals to maintenance retraining were not associated with the probability of performing adequate AED skills (Table 6b); however, age was associated with a small but significantly lower probability of performing these skills (about 2.5% per additional year of age, p=.001). Volunteers speaking English as a primary language were over three times more likely to perform adequate AED skills (p=.001) relative to those with another primary language, and volunteers reporting the ability to operate a computer were almost twice likely to perform well compared to those who did not (p=.045).
Figure 1.
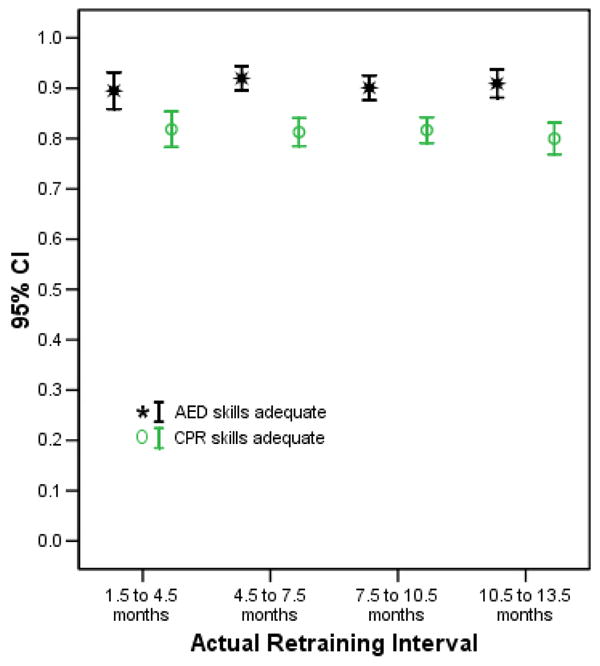
Proportion of Volunteers with adequate CPR and AED skills by time interval
Table 6.
| Table 6a. Independent predictors of CPR skill competence by regression modeling | ||
|---|---|---|
| Independent Predictors of Adequate CPR1 | Exp{B}, (robust SE) | P-value |
| Maintenance retraining interval (mr6onths) | 0.842 (0.050) | .004 |
| Age (years) | 0.937 (0.012) | <.001 |
| Age by Maintenance retraining interval interaction | 1.003 (0.001) | .013 |
| Gender | 1.276 (0.154) | .044 |
| White race | 1.509 (0.293) | .034 |
| Previously responded to seizure/emergency situation | 1.600 (0.204) | <.001 |
| Achieved proficiency at primary refresher training | 3.049 (1.245) | .006 |
| Lifeguard | 2.676 (0.933) | .005 |
| Table 6b. Independent predictors of AED skill competence by regression modeling | ||
|---|---|---|
| Independent Predictors of Delivery of AED Shock1 | Exp(B) (robust SE) | P-value |
| Maintenance retraining interval (months) | 0.956 (0.039) | .267 |
| Age | 0.975 (0.007) | 0.001 |
| English primary language | 3.125 (1.073) | 0.001 |
| Able to operate a computer | 1.891 (0.601) | 0.045 |
Model also adjusted for site
Figure 2.
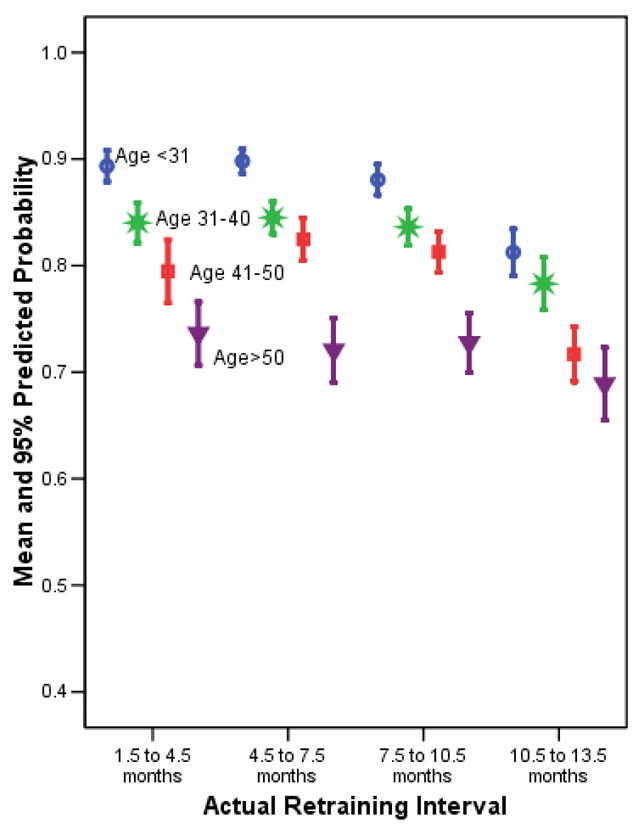
Mean predicted probabilities and 95% CIs for performing adequate CPR by age category and maintenance retraining interval group
4. Discussion
Results of this study strongly suggest that committed volunteers acting within a structured emergency response plan retain core CPR and AED skills up to 12 months after primary initial and refresher training. CPR skills do degrade minimally over the next 12 months but more than 80% of volunteers in all CPR groups and more than 90% in AED groups remained competent overall at 12 months. These findings provide valuable information for those recommending training schedules in public access emergency response settings.
Effective CPR training has been an elusive goal since the inception of the “chain of survival” concept. CPR is a complex cognitive and psychomotor task and past evidence suggests that fewer than half of traditional CPR trainees are able to perform immediately following training.4, 5 The retention of CPR skills also has been documented to be poor.6–11 Nyman & Sihvonen12 describe CPR skill retention in 298 nurses and nursing students. They found no degradation in overall performance between those who had received training within 6 months and those who had not, but the results were uniformly dismal, identifying overall that 36% first assessed the patient’s response, 67% opened the airway, 21% performed chest compressions correctly for at least half of the test, and 33% ventilated correctly at least half of the time. They conclude that skills of the participants in that study could not be considered adequate. Many studies document the difficulty in learning and remembering the correct sequence of steps in CPR.24–28
Attempts to identify improved methods for delivering CPR training have included simplification of CPR protocols, most recently by removing mouth-to-mouth resuscitation.10, 29 Alternatives to the classroom approach have been investigated most notably by Braslow30 who demonstrated improved skill mastery and retention among laypersons who completed video self-instruction in CPR compared to laypersons who attended traditional CPR training. Subsequent work has found similar results5, 31 but while different educational modalities have shown improvements on initial learning, the overall proportion of trainees who retain CPR skills are typically less than 50% at 6 months.
Formal evaluation of AED skill acquisition and retention is less frequent but the small number of studies reported suggest that AED skills may be easier to learn and maintain than CPR.17–21 One of the prime reasons may be the benefit of voice and visual prompts provided on modern AEDs.
Our experience is in contrast to many previous skill-retention studies, presumably because of a different design and a different study population. The most common testing model involves performing a set of distinct skills in sequence on artificial manikins according to objective measures in a classroom situation. The combination of skills measured is complex and the evaluation process is stressful. It is unknown whether passing or failing scores in this type of environment reflect the ability to perform core skills that improve survival at a real cardiac arrest event. The most common mistake in CPR testing was failure to activate 911 but no instances of failure to do so were recorded in 3413 actual events. Due to the large number of volunteers requiring CPR training, we chose to measure competence in an overall manner focusing on compressions, the key act that would most likely save a life. Bystander CPR does not have to be perfect to be associated with increased survival from cardiac arrest.32, 33 Although most agree that optimizing CPR is important, even CPR by professional advanced trained responders is not always ideal.34. Our global evaluation of AED skills, which focused on the delivery of an acceptable shock, and our reinforced primary training strategy may also explain the high rates of competence in this study. The most common mistake in AED testing was failure to clear the patient verbally prior to defibrillation attempt, but no cases of electrical shock to volunteers of bystanders were recorded during the PAD trial. We are convinced that our overall assessment of both CPR and AED skills is a practical and relevant method of evaluation. There was no formal attempt to measure the inter-observer reliability of the overall score applied by a large number of instructors.
We sought to optimize skill retention by providing all volunteers with primary training that included the initial course combined with testing and focused refresher training if necessary, 3 to 6 months later. The method of maintenance retraining in this study was one-to-one and individualized. The pre-test allowed the instructor to focus on deficiencies thus providing efficient testing often within the work environment. In our model, testing for competence, identification of weaknesses and retraining to CPR proficiency took an average of 4.9 (± 2.7) minutes per volunteer. The average time for AED plus CPR testing and maintenance retraining was 7.2 (± 3.4) minutes demonstrating that 2 or 4 hour retraining sessions are not necessary in most cases. Information about the frequency of retraining volunteer emergency responders is important to agencies delivering training programs and facilities incorporating CPR or AED response plans. This study suggests that after primary training, yearly maintenance retraining will result in modest reduction in mean CPR composite skill scores but without reduction in the proportion of volunteers able to perform adequate chest compressions and no significant reduction in the proportion of volunteers able to deliver a shock with an AED. There is no consensus on an appropriate and achievable goal for the absolute proportion of volunteers who should be able to respond appropriately. Although 100% is optimal, it is unrealistic. It is unknown whether more frequent training would increase the proportion of volunteers who perform proficiently and this study cannot predict performance beyond 12 months after primary initial and refresher training. Of importance, volunteers with poor performance on previous training sessions likely require more intense remediation than these group results would suggest. Other characteristics associated with CPR successful performance include younger age, male sex, white race, previous response to a health emergency and prior lifeguard training. Characteristics associated with AED success include young age, English as a primary language and ability to operate a computer. These predictors of success can be used to identify volunteers who are likely to succeed and conversely those who may require more intense training. They are consistent with a previous analysis of PAD volunteer performance at the primary refresher training session.35
It must be emphasized that the volunteer cohort in this trial was motivated, had responsibility for responding during specific hours and worked in an environment of relative high risk; conditions that likely increased learning and retention. Some also had experience responding to emergencies (first aid attendants, security guards, lifeguards) and are not directly comparable to lay groups in many previous studies.
The results of this study should be considered with an understanding of the limitations. The overall assessment model may reflect more accurately whether the trainee is able to remember and perform the fundamentals of CPR or AED use that are important to successful resuscitation but it can be challenged on its lack of standardization and unknown inter-observer reliability. It was however, defined and collected on identical scoring sheets for consistency. Overall scores were consistent with simple composite scores providing some evidence of internal validity and some confidence in the global score as a reasonable measure. Subjects analyzed included only 20% of those who were primarily trained and 40% of those who had initial refresher retraining. This circumstance was largely due to a retraining burden that was too great for sites to complete on allocated resources and the completion of this study prior to scheduled retraining. An additional group of volunteers could not be retrained because they left the facility (e.g., changed jobs) thus, it is possible that the analyzed sample is biased. For example, difficult facilities or volunteers may have been a lower priority for retraining resources, or volunteers performing poorly previously may have refused to attend a subsequent retraining. Despite our attempts to control for potential bias using measured volunteer characteristics there may have been an imbalance in important unmeasured characteristics. Any program that trains volunteer responders in similar settings must expect significant turnover and plan training of new volunteers accordingly. The intended analysis according to randomization of training by time interval was impossible due to the large variability in actual retraining timing intervals. Adherence to the planned training schedule encountered practical difficulties in the coordination of simultaneous training in multiple facilities. Significant logistic scheduling problems are likely to also occur in many real-world settings.
Despite limitations outlined above, this trial is the largest published trial of volunteers who were actually involved in CPR or AED response plans in their respective environments. This volunteer group was committed to the PAD trial and training and therefore more closely represents real-world training and skill retention than other studies of subjects with no immediate responsibilities to respond.
5. Conclusion
After receiving primary training, CPR skills of targeted lay responders deteriorate nominally as time between retraining increases but 80% remain competent up to one year. AED skills do not significantly deteriorate and 90% remain competent up to one year. Consensus of realistic targets for maintaining skill retention can be developed and these data used to plan training programs.
Supplementary Material
Acknowledgments
Support: National Heart, Lung, and Blood Institute, Bethesda, MD, under contract #N01-HC-95177; American Heart Association, Dallas, TX; Medtronic/Physio-Control Corporation, Redmond, WA; Cardiac Science/Survivalink, Inc., Minneapolis, MN; Philips Corporation/Heartstream Operation, Seattle, WA; Guidant Corporation, Minneapolis, MN; and Laerdal Corporation, Minneapolis, MN.
This study was supported by contract #N01-HC-95177 from the National Heart, Lung, and BloodInstitute (Bethesda, Md), with additional support from the American Heart Association (Dallas, Tex); Guidant Corporation (Indianapolis, Ind); Medtronic, Inc (Minneapolis, Minn); Cardiac Science/Survivalink, Inc (Minneapolis, Minn); Medtronic Physio-Control (Redmond, Wash); Philips Medical Systems, Heartstream Operation (Seattle, Wash); and Laerdal Medical Corporation (WappingersFalls, NY).
We are indebted to the thousands of volunteers who participated in the PAD trial.
Appendix
The investigators and coordinators participating in the PAD Trial were as follows: Arizona Heart Institute, Phoenix: K. Vijayaraghavan, T. Mattioni, and C. Williams. Calgary Emergency Medical Services, Calgary, Alta., Canada: A.R. Anton, C.D. Jones, S. Yahn, and D. Rabel. Christiana Health Care Services, Newark, Del.: R.E. O’Connor, P. McGraw, M. Bollinger, and R.E. Megargel. East Coast Clinical Research, Virginia Beach, Va.: R.A. Craven, L.A. Bosken, M.P. Burke, J. Paulsen, and G. Newton. Hennepin County Medical Center, Minneapolis: B.D. Mahoney, R. Knudson-Ballard, and G. Vasquez. Indiana University, Indianapolis: W.J. Groh, D. Cordes, and S.J. Bondurant. Intermountain Injury Control Research Center, Department of Pediatrics, University of Utah School of Medicine, Salt Lake City: N.C. Mann, B. Shaum, K. Brown, and K. Jacobsen. Medical College of Wisconsin, Milwaukee: T.P. Aufderheide, R.G. Pirrallo, C.J. Conrad, D.J. Kitscha, C.W. Sparks, C. von Briesen, K.A. Deja, M.M. LeStarge, R.W. Janisch, S.S. Schmidt, L. Parmenter, and L. Grabowski. Mission Hospital, Mission Viejo, Calif., and Orange County Emergency Medical Services, Orange County, Calif.: S. Ehrlich, B. Haynes, L. Asbury, and M. Amaya. Mount Sinai School of Medicine, New York: L.D. Richardson, F. Ehlert, C. Freyberg, N. Richmond, C. Shields, I. Wilets, and J. Holohan. Oregon Health and Science University, Portland: M. Daya, M.D. Gunnels, J.R. Hedges, J. Jui, T. Schmidt, L. Wittwer, H. Brooks, C. Burke, and D. Griffiths. Riverside County Emergency Medical Services, Riverside, Calif.: M. Osur, B. MacGavin, and B. Myrin. Institute of Critical Care Medicine, Palm Springs, Calif.: M.H. Weil. Loma Linda University Medical Center, Loma Linda, Calif.: R. Sehra. University of Washington, Seattle: R.O. Cummins, A. Doherty, S. Thompson, and S. Wood. St. Paul’s Hospital, Vancouver, B.C., Canada: J. Christenson, S. Pennington, A. Holmes, H. Payne, R. Webb, N. Douglas, and P. Lawson. Stony Brook University, Stony Brook, N.Y.: M.C. Henry, S. Johnson, H. Thode, and E.R. Stapleton. SUNY Upstate Medical University Hospital, Syracuse, N.Y.: D.B. Reed, L.H. Brown, and L.M. Evans. George Washington University Medical Center, Washington, D.C.: P.J. Varghese and R. Lucas. University of Alabama at Birmingham, Birmingham: T.E. Terndrup, S. Stephens, S. Nafziger, and J. Sanford. University of Alberta–City of Edmonton Emergency Response Department, Edmonton, Alta., Canada: A. Travers, A. Panylyk, K. Irwin, and B. Heisz. University of Chicago Hospitals, Chicago: L.B. Becker, A. Barry, and E. Demertsidis. University of Cincinnati, Cincinnati: J. Van Zile, C. Grimmelsman, and L. Nolting. University of Pittsburgh School of Medicine, Pittsburgh: V.N. Mosesso, Jr., B.K. Slater, V.J. Campbell, and D. Hostler. Virginia Commonwealth University Health System, Richmond: J.P. Ornato (Steering Committee chair), M.A. Peberdy, J. Overton, and K. Schaffer. Wayne State University, Detroit: R. Zalenski, S. Compton, R. Dunne, R. Swor, R. Welch, L.M. Mango, and K. Bilicki. Johns Hopkins University School of Medicine, Baltimore: M. Weisfeldt. Ohio State University, Columbus: M.R. Sayre. School of Nursing, University of Pennsylvania, Philadelphia: B. Riegel. National Heart, Lung, and Blood Institute, Bethesda, Md.: E.B. Schron, J. Fleg, M.J. Domanski, M. Proschan, Y. Rosenberg, L. O’Neill, and the following former project officers: D. Simons-Morton and M.E. Salive. Economic Center, University of Ottawa, Ottawa, Ont., Canada: G. Nichol, G. Wells, E. Huszti, J. Rokosh, and D. Morris. Harvard University, Boston: K. Kuntz. University of Alberta, Edmonton, Alta., Canada: D. Feeny. Clinical Trial Center, University of Washington, Seattle: A.P. Hallstrom, H.L. Greene, M.A. McBurnie, J. Powell, L. Van Ottingham, A. Birnbaum, R.B. Ledingham, R. Moore, M. Morris, M. Scholz, and A. Kerr.
Footnotes
6. Conflict of Interest
None of the authors have conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rea TD, Eisenberg MS, Sinibaldi G, White RD. Incidence of EMS-treated out-of-hospital cardiac arrest in the United States. Resuscitation. 2004;63:17–24. doi: 10.1016/j.resuscitation.2004.03.025. [DOI] [PubMed] [Google Scholar]
- 2.The Public Access Defibrillation Trial Investigators. Public-Access Defibrillation and Survival after Out-of-Hospital Cardaic Arrest. N Engl J Med. 2004;351:637–46. doi: 10.1056/NEJMoa040566. [DOI] [PubMed] [Google Scholar]
- 3.Stiell IG, Wells GA, Field B, et al. Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med. 2004;351:647–56. doi: 10.1056/NEJMoa040325. [DOI] [PubMed] [Google Scholar]
- 4.Brennan RT, Braslow A. Skill mastery in public CPR classes. Am J Emerg Med. 1998;16:653–7. doi: 10.1016/s0735-6757(98)90167-x. [DOI] [PubMed] [Google Scholar]
- 5.Batcheller AM, Brennan RT, Braslow A, Urrutia A, Kaye W. Cardiopulmonary resuscitation performance of subjects over forty is better following half-hour video self-instruction compared to traditional four-hour classroom training. Resuscitation. 2000;43:101–10. doi: 10.1016/s0300-9572(99)00132-x. [DOI] [PubMed] [Google Scholar]
- 6.Wilson E, Brooks B, Tweed WA. CPR skills retention of lay basic rescuers. Ann Emerg Med. 1983;12:482–4. doi: 10.1016/s0196-0644(83)80643-x. [DOI] [PubMed] [Google Scholar]
- 7.Berden HJ, Bierens JJ, Willems FF, Hendrick JM, Pijls NH, Knape JT. Resuscitation skills of lay public after recent training. Ann Emerg Med. 1994;23:1003–8. doi: 10.1016/s0196-0644(94)70094-x. [DOI] [PubMed] [Google Scholar]
- 8.Morgan CL, Donnelly PD, Lester CA, Assar DH. Effectiveness of the BBC’s 999 training roadshows on cardiopulmonary resuscitation: video performance of cohort of unforewarned participants at home six months afterwards. Bmj. 1996;313:912–6. doi: 10.1136/bmj.313.7062.912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flesche CW, Noetges P, Schlack W, Zucker TP, Tarnow J. Quality of lay public cardiopulmonary resuscitation after standard first aid training courses (abstract) Resuscitation. 1994;28:S25. [Google Scholar]
- 10.Swor R, Compton S, Vining F, et al. A randomized controlled trial of chest compression only CPR for older adults-a pilot study. Resuscitation. 2003;58:177–85. doi: 10.1016/s0300-9572(03)00123-0. [DOI] [PubMed] [Google Scholar]
- 11.Wenzel V, Lehmkuhl P, Kubilis PS, Idris AH, Pichlmayr I. Poor correlation of mouth-to-mouth ventilation skills after basic life support training and 6 months later. Resuscitation. 1997;35:129–34. doi: 10.1016/s0300-9572(97)00044-0. [DOI] [PubMed] [Google Scholar]
- 12.Nyman J, Sihvonen M. Cardiopulmonary resuscitation skills in nurses and nursing students. Resuscitation. 2000;47:179–84. doi: 10.1016/s0300-9572(00)00226-4. [DOI] [PubMed] [Google Scholar]
- 13.Moser DK, Dracup K, Guzy PM, Taylor SE, Breu C. Cardiopulmonary resuscitation skills retention in family members of cardiac patients. Am J Emerg Med. 1990;8:498–503. doi: 10.1016/0735-6757(90)90150-x. [DOI] [PubMed] [Google Scholar]
- 14.Chamberlain D, Smith A, Woollard M, et al. Trials of teaching methods in basic life support (3): comparison of simulated CPR performance after first training and at 6 months, with a note on the value of re-training. Resuscitation. 2002;53:179–87. doi: 10.1016/s0300-9572(02)00025-4. [DOI] [PubMed] [Google Scholar]
- 15.Gombeski WR, Jr, Effron DM, Ramirez AG, Moore TJ. Impact on retention: comparison of two CPR training programs. Am J Public Health. 1982;72:849–52. doi: 10.2105/ajph.72.8.849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gundry JW, Comess KA, DeRook FA, Jorgenson D, Bardy GH. Comparison of naive sixth-grade children with trained professionals in the use of an automated external defibrillator. Circulation. 1999;100:1703–7. doi: 10.1161/01.cir.100.16.1703. [DOI] [PubMed] [Google Scholar]
- 17.Woollard M, Whitfeild R, Smith A, et al. Skill acquisition and retention in automated external defibrillator (AED) use and CPR by lay responders: a prospective study. Resuscitation. 2004;60:17–28. doi: 10.1016/j.resuscitation.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 18.Usatch BR, Cone DC. Automated external defibrillator training and skill retention at a ski patrol. Prehosp Emerg Care. 2002;6:325–9. doi: 10.1080/10903120290938409. [DOI] [PubMed] [Google Scholar]
- 19.Amith G. Revising educational requirements: challenging four hours for both basic life support and automated external defibrillators. New Horiz. 1997;5:167–72. [PubMed] [Google Scholar]
- 20.Kaye W, Mancini ME, Giuliano KK, et al. Strengthening the in-hospital chain of survival with rapid defibrillation by first responders using automated external defibrillators: training and retention issues. Ann Emerg Med. 1995;25:163–8. doi: 10.1016/s0196-0644(95)70318-7. [DOI] [PubMed] [Google Scholar]
- 21.Walters G, Glucksman E, Evans TR. Training St John Ambulance volunteers to use an automated external defibrillator. Resuscitation. 1994;27:39–45. doi: 10.1016/0300-9572(94)90020-5. [DOI] [PubMed] [Google Scholar]
- 22.American Heart Association: AED. Public acccess to Defibrillation. 2004 www.americanheart.org.
- 23.The PAD Trial Investigators. The Public Access Defibrillation (PAD) Trial Study design and rationale. Resuscitation. 2003;56:135–47. doi: 10.1016/s0300-9572(02)00442-2. [DOI] [PubMed] [Google Scholar]
- 24.Rosafio T, Cichella C, Vetrugno L, Ballone E, Orlandi P, Scesi M. Chain of survival: differences in early access and early CPR between policemen and high-school students. Resuscitation. 2001;49:25–31. doi: 10.1016/s0300-9572(00)00341-5. [DOI] [PubMed] [Google Scholar]
- 25.Handley JA, Handley AJ. Four-step CPR--improving skill retention. Resuscitation. 1998;36:3–8. doi: 10.1016/s0300-9572(97)00095-6. [DOI] [PubMed] [Google Scholar]
- 26.van Kalmthout PM, Speth PA, Rutten JR, Vonk JT. Evaluation of lay skills in cardiopulmonary resuscitation. Br Heart J. 1985;53:562–6. doi: 10.1136/hrt.53.5.562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nelson M, Brown CG. CPR instruction: modular versus lecture course. Ann Emerg Med. 1984;13:118–21. doi: 10.1016/s0196-0644(84)80574-0. [DOI] [PubMed] [Google Scholar]
- 28.Weaver FJ, Ramirez AG, Dorfman SB, Raizner AE. Trainees’ retention of cardiopulmonary resuscitation. How quickly they forget. Jama. 1979;241:901–3. [PubMed] [Google Scholar]
- 29.Cohen TJ, Goldner BG, Maccaro PC, et al. A comparison of active compression-decompression cardiopulmonary resuscitation with standard cardiopulmonary resuscitation for cardiac arrests occurring in the hospital. N Engl J Med. 1993;329:1918–21. doi: 10.1056/NEJM199312233292603. [DOI] [PubMed] [Google Scholar]
- 30.Braslow A, Brennan RT, Newman MM, Bircher NG, Batcheller AM, Kaye W. CPR training without an instructor: development and evaluation of a video self-instructional system for effective performance of cardiopulmonary resuscitation. Resuscitation. 1997;34:207–20. doi: 10.1016/s0300-9572(97)01096-4. [DOI] [PubMed] [Google Scholar]
- 31.Todd KH, Heron SL, Thompson M, Dennis R, O’Connor J, Kellermann AL. Simple CPR: A randomized, controlled trial of video self-instructional cardiopulmonary resuscitation training in an African American church congregation. Ann Emerg Med. 1999;34:730–7. doi: 10.1016/s0196-0644(99)70098-3. [DOI] [PubMed] [Google Scholar]
- 32.Van Hoeyweghen RJ, Bossaert LL, Mullie A, et al. Quality and efficiency of bystander CPR. Belgian Cerebral Resuscitation Study Group Resuscitation. 1993;26:47–52. doi: 10.1016/0300-9572(93)90162-j. [DOI] [PubMed] [Google Scholar]
- 33.Cobb LA, Hallstrom AP. Community-based cardiopulmonary resuscitation: what have we learned? Ann N Y Acad Sci. 1982;382:330–42. doi: 10.1111/j.1749-6632.1982.tb55228.x. [DOI] [PubMed] [Google Scholar]
- 34.Aufderheide TP, Sigurdsson G, Pirrallo RG, et al. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109:1960–5. doi: 10.1161/01.CIR.0000126594.79136.61. [DOI] [PubMed] [Google Scholar]
- 35.Riegel B, Birnbaum A, Aufderheide TP, et al. Predictors of Cardiopulmonary Resuscitation and Automated External Defibrillator Skill Retention. American Heart Journal. 2005 doi: 10.1016/j.ahj.2005.01.042. in press. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


