Abstract
We investigated the association between occupational exposure to extremely low-frequency magnetic fields (MFs) and the risk of glioma and meningioma. Occupational exposure to MF was assessed for 489 glioma cases, 197 meningioma cases, and 799 controls enrolled in a hospital-based case–control study. Lifetime occupational history questionnaires were administered to all subjects; for 24% of jobs, these were supplemented with job-specific questionnaires, or “job modules,” to obtain information on the use of electrically powered tools or equipment at work. Job-specific quantitative estimates for exposure to MF in milligauss were assigned using a previously published job exposure matrix (JEM) with modification based on the job modules. Jobs were categorized as ≤1.5 mG, >1.5 to <3.0 mG, and ≥3.0 mG. Four exposure metrics were evaluated: (1) maximum exposed job; (2) total years of exposure >1.5 mG; (3) cumulative lifetime exposure; and (4) average lifetime exposure. Odds ratios (ORs) were calculated using unconditional logistic regression with adjustment for the age, gender, and hospital site. The job modules increased the number of jobs with exposure ≥3.0 mG from 4% to 7% relative to the JEM. No statistically significant elevation in ORs or trends in ORs across exposure categories was observed using four different exposure metrics for the three tumor types analyzed. Occupational exposure to MFs assessed using job modules was not associated with an increase in the risk for glioma, glioblastoma, or meningioma among the subjects evaluated in this study.
Keywords: glioma, job modules, magnetic fields, meningioma, occupation
Brain cancer is a rare but often fatal disease. The age-adjusted annual incidence rate for brain and other nervous system cancers (invasive) in the United States from 1998 through 2002 was 6.4 per 100,000, with higher incidence rates among males (7.6 per 100,000) than among females (5.3 per 100,000).1 The only known environmental factor associated with a risk for malignant or benign brain tumors is moderate to high doses of ionizing radiation, such as from radiotherapy to the head, which accounts for only a small fraction of brain tumors.2,3 Other environmental risk factors have been investigated, including occupational exposure to solvents, pesticides, lead, and magnetic fields (MFs), but no conclusive findings have been reported.4–7
The International Agency for Research on Cancer (IARC) has MFs classified at extremely low-frequency electromagnetic fields (ELF) as possibly carcinogenic to humans (i.e., group 2B). The epidemiologic evidence includes associations observed with childhood leukemia and, to a lesser extent, with chronic lymphocytic leukemia in occupationally exposed adults. However, the evidence from animal assays is considered by the IARC to be inadequate for a more definitive classification, and no biologic mechanism has been established.8 A comprehensive review of the health risks associated with exposure to ELF-electric and magnetic fields (EMF) published in 2001 reported a small increase of 10%–20% in the risk of brain cancer for a broad group of electrical occupations but concluded that the available evidence was insufficient to determine whether exposure to MFs increases brain cancer risk.9
A variety of methods have been used in epidemiologic studies to assess exposure to MFs. Some of the first occupational studies to provide suggestive evidence of a possible association between brain cancer and exposure to MFs were based on analyses by job titles, including classification by “electric occupations.”10,11 The development of portable instruments to measure MFs has provided quantitative data that have improved the quality of occupational exposure assessments.12–14 Monitoring studies have revealed substantial temporal and spatial variability in the strength of the MF in occupational environments. MF <1.5 mG (milligauss) are frequently encountered in both occupational and residential environments, while levels >3.0 mG occur primarily in occupational environments near power lines and electrically powered equipment or tools.15,16
The MF measurements in occupational settings have been summarized using job exposure matrices (JEMs) in which the personal MF exposure measurements are averaged by job title.17 JEMs have been applied in several industry-based studies of brain tumor risk among electrical utility workers. A study of electrical utility workers in the United States using a JEM found an elevated risk for brain tumors;18 however, another study of electrical utility workers in the United Kingdom found no association between brain cancer and occupational exposure to MFs.19 JEMs have also been applied in population-based case–control studies that reported possible health effects from occupational exposure to ELF-EMF. A brain cancer study from Sweden reported an elevated risk among men in the highest quartile for duration of exposure >2.0 mG based on measurements based on measurements.20 A nested case–control study of brain tumor risk among U.S. Air Force personnel found a small association with exposure to ELF-EMF based on a JEM with qualitative ratings.21 Using JEMs combined with professional judgment to assign quantitative exposure levels by job title, a study using data from the Canadian National Enhanced Cancer Surveillance System reported a positive association between duration of occupational exposure to MFs >3.0 mG and glioblastoma.22
Some of the inconsistency seen in risk estimates between various studies may be due to challenges related to the assessment of occupational exposures for ELF-EMF. These challenges include the lack of a relevant exposure metric based on a plausible biologic mechanism that can incorporate highly variable exposures from multiple sources of ELF-EMF, contact currents, and shocks in occupational environments.23 It is not known whether the average field strength, the duration of exposure greater than a threshold, the electric current induced by the MF, or some other characteristics of the field (e.g., frequency, waveform, or intermittency) are relevant to human health.23 The JEM itself may contribute to some of the inconsistency among epidemiologic studies by assigning a single average value to all subjects with the same job title when actual exposures can be highly variable, resulting in some misclassification.
To address some of the limitations associated with the use of JEMs, a novel method was developed to generate quantitative estimates for occupational exposure to MF by combining exposure estimates from a JEM with information reported by the study participants or proxies during in-person interviews using job modules.24,25 Job-specific exposure estimates were merged with the work histories to develop four separate exposure metrics: duration of exposure, maximum exposed job, time-averaged exposure, and cumulative lifetime exposure.
Materials and Methods
The subjects in this analysis were enrolled in a hospital-based case–control study conducted at three hospitals specializing in the treatment of brain tumors in Phoenix, Arizona; Boston, Massachusetts; and Pittsburgh, Pennsylvania. Detailed descriptions of this study population have been published previously.24,26 Study subjects were at least 18 years of age and included 489 patients recently diagnosed with glioma (including 241 glioblastoma cases) and 197 patients recently diagnosed with meningioma. An additional 96 cases of acoustic neuroma were also enrolled but are not included in this analysis. A control group of 799 subjects was recruited from patients admitted to the same three hospitals during the same time period as the cases for conditions other than cancer, including trauma and diseases of the circulatory, musculoskeletal, and digestive systems. Controls were frequency-matched to the total case series on age, gender, race/ethnicity, hospital, and distance of residence from the hospital.
Lifetime occupational histories were obtained during in-person interviews with subjects or their proxies conducted by trained nurses using a structured questionnaire to administer computer-assisted in-person interviews (CAPI). The occupational histories included job title, type of industry, years started and stopped, and type of employment (e.g., full-time, part-time, or seasonal) for all jobs held for at least 6 months during their lifetime. The jobs in the work histories were coded using 1980 Standard Occupation Classification (SOC) codes27 and 1987 Standard Industrial Classification codes.28
The CAPI used to administer the occupational histories included job modules for selected jobs with a potential exposure to MFs that were identified based on a literature review and triggered by key words in the occupational titles. The job modules included questions on the tasks performed at work, the type and size of electrically powered tools or equipment used, the average distance from this equipment, and the amount of time spent working with or near electrically powered equipment. The responses to the job modules were reviewed by an industrial hygienist within 2–3 weeks, and follow-up questions were asked when needed to clarify vague or ambiguous responses. The job modules were reviewed and the exposure estimates developed without knowledge of the case–control status.
Exposure to MFs is affected by both the duration of exposure and distance from the source.15,29 To incorporate the job module information into MF exposure estimates, the responses to the job modules were used to calculate time and distance scores for each job based on the amount of time spent working with or near electrically powered equipment and the average distance from the equipment or tools while working. The time factor was calculated by dividing the average hours per week working with or near electrically powered tools or equipment by 40. The distance factor was calculated based on an inverse-square relationship between field strength and distance using questions about proximity to electrical equipment. For subjects who reported use of handheld equipment or who worked within 3 feet of a source, no reduction for distance was applied. For subjects who reported working 3–6 feet from the source, an approximate doubling of the distance, the score was divided by 4. For subjects who reported working more than 6 feet from the source, the score was divided by 9. For subjects who reported working with or near two or more sources, the scores for each source were calculated and combined by summing the squares of the scores and then taking the square root of the sum. A score of 1.0 was assigned to subjects who reported working within 3 feet of one source for 40 hours per week. A subject who worked only 20 hours per week within 3 feet of a source received a score of 0.5. A subject who worked 20 hours per week within 3 feet of two sources was assigned a job score of 0.7. A value of 0.05 was used as the minimum possible score.
A time-weighted average (TWA) exposure to MF was assigned to each job using a previously published population-based JEM compiled from a variety of exposure measurement databases.17 The geometric mean (GM) from the JEM was assigned to each job in the work histories based on the SOC code. The JEM included exposure values for 438 (77%) of the 566 different four-digit SOC codes from the work histories, and 91% of all jobs from the work histories. The jobs from the work histories with no corresponding JEM entry at the four-digit SOC level were assigned the GM value for the corresponding two-digit SOC code.
A scaling factor was calculated for each job module to adjust the JEM values based on the time and distance scores for different subjects with the same job title. The GM value from the JEM was assumed to represent the median exposure level for each SOC code around which the exposures for all subjects with that same SOC code were distributed. Furthermore, the average time and distance score associated with each SOC code was assumed to correspond to the GM value from the JEM. The scaling factor was calculated by dividing the job-specific time and distance scores by the average score for that particular SOC code. The scaling factor was then multiplied by the JEM value to estimate the exposure for each of the jobs for which a module was administered. For jobs without a module, the JEM value without scaling was used as the default exposure estimate.
The job-specific exposure estimates for each job described above were combined with the work histories to generate four quantitative exposure metrics for each subject: (1) the maximum TWA MF magnitude from all the subject’s jobs; (2) duration of employment in jobs with a TWA >1.5 mG; (3) cumulative magnitude over all jobs; and (4) TWA magnitude averaged over all jobs. A 5-year latency period between the exposure and the diagnosis of disease was included by excluding exposures from jobs held within 5 years of the date of interview.
The maximum exposed job was determined based on the highest exposed job over each subject’s working lifetime regardless of the duration of the job. The subjects whose maximum exposed job was <1.5 mG served as the “unexposed” referent group for subsequent analyses. Duration was determined based only on years of employment in jobs with exposure >1.5 mG. A value of 1.5 mG was used as a cutoff point to distinguish between background levels found in residential environments and higher levels more frequently encountered in occupational environments.
Unconditional logistic regression was used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) by exposure category, with adjustment for the matching variables of age, gender, and hospital site. Adjustment for distance from hospital did not affect risk estimates and was not included in the final model. ORs were evaluated separately for all glioma cases combined, for the subset of glioblastoma cases, and for the meningioma cases. All statistical analyses were two sided and conducted using STATA software (version 8.0; StataCorp L.P., College Station, TX, USA).
Results
The number of subjects by gender, age, and hospital site is displayed in Table 1 separately for controls, for all glioma cases combined, and for meningioma cases. The control group was somewhat younger, with a smaller proportion of subjects older than 65 years of age, and included a smaller proportion of males compared with the meningioma cases.
Table 1.
Characteristics of controls, glioma cases, and meningioma cases
| Controls (N = 799)
|
Glioma Cases (N = 489)
|
Meningioma Cases (N = 197)
|
||||
|---|---|---|---|---|---|---|
| Characteristic | n | % | n | % | n | % |
| Gender | ||||||
| Female | 436 | 55% | 212 | 43% | 151 | 80% |
| Male | 363 | 45% | 277 | 57% | 46 | 24% |
| Age (years) | ||||||
| ≤45 | 317 | 40% | 173 | 35% | 47 | 25% |
| 46–65 | 319 | 40% | 188 | 38% | 94 | 50% |
| ≥66 | 163 | 20% | 128 | 26% | 56 | 30% |
| Site | ||||||
| Phoenix | 405 | 51% | 244 | 50% | 99 | 52% |
| Boston | 220 | 28% | 153 | 31% | 79 | 42% |
| Pittsburgh | 174 | 22% | 92 | 19% | 19 | 10% |
Work history information was obtained for 98% of controls and 97% of cases (Table 2). Seven subjects did not provide a work history, and the work histories for four other subjects did not include the start and stop dates. These 11 subjects were excluded from further analyses. There were 119 jobs reported by 68 subjects with one or more missing start or stop dates. These subjects were retained in the analysis, but the jobs with missing dates were excluded from the duration calculation. The controls, glioma cases, and meningioma cases reported a similar number of jobs, with averages of 5.6, 5.2, and 5.9 jobs, respectively, and average duration of employment of 23, 24, and 25 years, respectively.
Table 2.
Work history information
| Controls (N = 799)
|
Glioma Cases (N = 489)
|
Meningioma Cases (N = 197)
|
||||
|---|---|---|---|---|---|---|
| Category | n | % | n | % | n | % |
| Work history | ||||||
| No work history interview | 2 | 5 | 0 | |||
| Missing dates for all jobs | 2 | 2 | 0 | |||
| No work outside of home | 15 | 8 | 5 | |||
| Subjects with work histories | 780 | 98% | 474 | 97% | 192 | 97% |
| Subject | ||||||
| Subject alone | 735 | 94% | 307 | 65% | 152 | 79% |
| Subject and proxy | 23 | 3% | 74 | 16% | 14 | 7% |
| Proxy alone | 17 | 2% | 93 | 20% | 26 | 14% |
| Number of jobs | ||||||
| Number of jobs reported | 4,356 | 2,456 | 1,128 | |||
| Number with job modules | 1,073 | 25% | 503 | 20% | 312 | 28% |
| Average number of jobs | 5.6 | 5.2 | 5.9 | |||
| Average years worked | 22.5 | 24.3 | 24.7 | |||
Use of Job Modules to Modify the JEM Estimates
The work histories for cases and controls combined included a total of 7,940 jobs. Job modules were administered for 24% of these jobs, including 21% of the jobs reported by glioma cases, 28% of the jobs reported by meningioma cases, and 25% of the jobs reported by controls. The time and distance scores from the job modules ranged from 0.05 to 2.6, with a median of 0.25. The median value of 0.25 corresponds to 10 h/week working with an electrically powered handheld tool or within 3 feet of some other source. Scores of ≥1.0 represent subjects who reported working ≥40 h/week within 3 feet of one source and were obtained for 18% of jobs with modules. The minimum score of 0.05 was assigned to subjects who reported working <2 h/week within 3 feet or <8 h/week within 3–6 feet from one source and included 15% of the jobs with modules.
The variation in the subject-specific responses to the job modules resulted in a range of exposures assigned to subjects with the same job title. Table 3 lists occupations with six or more subjects assigned exposure estimates ≥3.0 mG after adjustment using the job modules, sorted from highest to lowest by the unadjusted JEM value, and the number of subjects by occupation exposed to ≥3.0 mG, >1.5 to <3.0 mG, and ≤1.5 mG based on the job module estimates. For example, 58 subjects reported job titles coded as “Garage and service station–related occupations.” The GM from the JEM for this job was 2.1 mG. Among these 58 subjects, 8 reported frequent use of electrically powered tools, resulting in an estimated intensity level for these subjects of ≥3.0 mG. There were 41 subjects assigned an exposure intensity between 1.5 and 3.0 mG, including the 23 subjects who were not administered a job module and were therefore assigned the JEM value of 2.1 mG. At the lower end of the distribution, 9 subjects reported infrequent use of electrically powered tools or equipment, resulting in a reduction of the estimate from the JEM to ≤1.5 mG. After adjustment of the JEM exposure estimate based on the job modules, 8 (14%) of these subjects moved to a higher exposure category and 9 (16%) moved to a lower exposure category.
Table 3.
Number of subjects by occupation and MF exposure level for occupations with six or more subjects exposed to MF fields >3.0 mG based on job module exposure estimate
| MF Exposure Level
|
|||||
|---|---|---|---|---|---|
| Occupational Title | JEM Value (mG) | ≤1.5 mG | >1.5 to <3.0 mG | ≥3.0 mG | %a |
| Welders and cutters | 10.2 | 2 | 28 | 93% | |
| Electrical power installers and repairers | 8.8 | 6 | 100% | ||
| Tailors and dressmakers, hand | 7.8 | 14 | 100% | ||
| Public relations specialists and publicity writers | 6.9 | 11 | 100% | ||
| Textile sewing machine operators and tenders | 6.8 | 1 | 1 | 27 | 93% |
| Electric motor, transformer, and related repairers | 6.0 | 7 | 100% | ||
| Mechanics and repairers, N.E.C. | 5.5 | 11 | 100% | ||
| Laundering and dry cleaning machine operators and tenders | 5.4 | 23 | 100% | ||
| Pressing machine operators | 5.0 | 9 | 100% | ||
| Electronic repairers, commercial and industrial equipment | 4.8 | 2 | 12 | 86% | |
| Construction trades persons | 4.6 | 1 | 7 | 88% | |
| Sales representatives, garments, related products | 4.4 | 7 | 100% | ||
| Sheet metal workers | 3.9 | 1 | 2 | 8 | 73% |
| Railroad conductors and yardmasters | 3.9 | 6 | 100% | ||
| Miscellaneous electrical and electronic equipment repairers | 3.3 | 1 | 6 | 86% | |
| Electricians | 3.1 | 2 | 3 | 16 | 76% |
| Postal clerks, except mail carriers | 3.1 | 8 | 100% | ||
| Duplicating machine operators | 3.1 | 1 | 7 | 88% | |
| Mechanics and repairers | 2.5 | 2 | 15 | 6 | 26% |
| Butchers and meat cutters | 2.3 | 3 | 15 | 7 | 28% |
| Garage and service station–related staff | 2.1 | 9 | 41 | 8 | 14% |
| Electrical and electronic engineers | 2.0 | 6 | 33 | 7 | 15% |
| Aircraft mechanics (except engine specialists) | 2.0 | 5 | 18 | 6 | 21% |
| Machinists | 1.8 | 8 | 14 | 9 | 29% |
| Janitors and cleaners | 1.7 | 14 | 55 | 7 | 9% |
| Officials and administrators, other, N.E.C. | 1.6 | 46 | 189 | 24 | 9% |
| General managers and other top executives | 1.3 | 283 | 25 | 31 | 9% |
| Typists | 1.3 | 31 | 1 | 8 | 20% |
| Teachers, except postsecondary institutions | 1.2 | 142 | 9 | 6 | 4% |
| All others | 3,826 | 2,514 | 228 | 3% | |
| Total | 4,382 | 2,939 | 560 | 7% | |
Percentage of subjects in a job category whose exposure estimates were ≥3.0 mG. Abbreviation: N.E.C., not elsewhere classified.
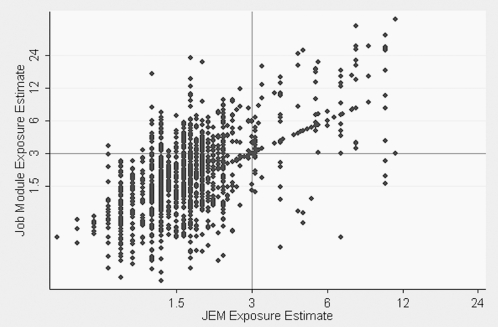
Fig. 1 displays a scatter plot of the job-specific exposure estimates after adjustment using the job modules, compared with the unadjusted estimates from the JEM for each of the jobs for which a job module score was calculated. The distribution in the assigned exposure estimates reflects the variability in the scores among subjects with the same JEM values, with an approximately equal number of jobs assigned exposures greater than and less than the corresponding JEM value. Among the jobs for which modules were administered, the exposure category increased for 27% of jobs, decreased for 15% of jobs, and remained the same for 58% of jobs when compared with the JEM.
Fig. 1.
Job-specific magnetic field exposure estimates adjusted using job modules versus unadjusted estimates from job exposure matrices (JEMs). The percentage of jobs in which subjects were exposed to ≥3.0 mG, when adjusted using job modules, increased from 4% to 7% relative to the JEM value.
When categorized by exposure intensity, the distribution in exposure among cases and controls was similar, with 62% of the jobs among the cases and 61% of the jobs among controls assigned an exposure intensity ≤1.5 mG. Among males, 9% of the jobs reported by both the cases and controls were assigned exposure intensities ≥3.0 mG. Among females, only 4% of the jobs among cases and 6% of jobs among controls were assigned an exposure level ≥3.0 mG.
No significant association with occupational exposure to MF was observed using any of the four different exposure metrics for the three tumor types analyzed (Table 4). None of the ORs calculated by exposure group were significantly elevated, and no trend in ORs was observed across exposure categories. None of the ORs were elevated for subjects ever employed in a job with exposure ≥3.0 mG compared with the referent group for glioma (OR = 0.8; 95% CI, 0.6–1.1), for glioblastoma (OR = 0.8; 95% CI, 0.5–1.2), or for meningioma (OR = 1.0; 95% CI, 0.6–1.8). Categorization by the duration of exposure >1.5 mG, by cumulative exposure, and by average lifetime exposure showed similar results, with no statistically elevated ORs among glioma cases, the subset of glioblastoma cases, or meningioma cases for any of the four exposure metrics. When analyzed by gender, no excesses were found for women (data not shown). A statistically nonsignificant excess of glioblastoma cancer was observed for men whose average exposure level was ≥ 3.0 mG (OR = 1.7; 95% CI, 0.9–3.2).
Table 4.
Number of subjects and odds ratio by ELF-EMF exposure metric for all gliomas, glioblastomas, and meningiomas
| All Glioma Cases
|
Glioblastoma
|
Meningioma Cases
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Exposure Metric | Controls | n | OR (95% CI) | p-Value for Trend | n | OR (95% CI) | p-Value for Trend | n | OR (95% CI) | p-Value for Trend |
| Maximum exposed job (mG) | ||||||||||
| ≤1.5 | 159 | 107 | 46 | 39 | ||||||
| >1.5 to <3.0 | 425 | 246 | 0.8 (0.6–1.1) | 123 | 0.8 (0.5–1.2) | 104 | 1.0 (0.7–1.6) | |||
| ≥3.0 | 196 | 121 | 0.8 (0.6–1.1) | 0.19 | 62 | 0.8 (0.5–1.2) | 0.39 | 49 | 1.0 (0.6–1.8) | 0.79 |
| Duration >1.5 mG (years) | ||||||||||
| 0 | 159 | 107 | 46 | 39 | ||||||
| >0 to 15 | 457 | 250 | 0.8 (0.6–1.0) | 104 | 0.7 (0.5–1.1) | 113 | 1.0 (0.7–1.6) | |||
| >15 | 164 | 115 | 0.8 (0.6–1.2) | 0.32 | 81 | 0.9 (0.6–1.5) | 0.89 | 40 | 1.0 (0.6–1.7) | 0.77 |
| Lifetime average (mG) | ||||||||||
| ≤1.5 | 407 | 240 | 109 | 106 | ||||||
| >1.5 to <3.0 | 302 | 195 | 1.0 (0.8–1.3) | 101 | 1.2 (0.9–1.6) | 73 | 1.1 (0.8–1.5) | |||
| ≥3.0 | 71 | 39 | 0.9 (0.6–1.3) | 0.68 | 21 | 1.0 (0.6–1.7) | 0.60 | 13 | 0.7 (0.4–1.4) | 0.66 |
| Cumulative exposure >1.5 mG (mG-years) | ||||||||||
| 0 | 159 | 107 | 46 | 39 | ||||||
| >0 to 45 | 490 | 276 | 0.8 (0.6–1.1) | 123 | 0.7 (0.5–1.1) | 121 | 1.0 (0.7–1.6) | |||
| >45 | 131 | 91 | 0.8 (0.5–1.2) | 0.23 | 62 | 0.9 (0.6–1.5) | 0.78 | 32 | 1.0 (0.6–1.8) | 0.91 |
Odds ratios calculated using unconditional logistic regression with adjustment for matching factors of gender, age, and site. Trend test conducted using ordinal rankings for exposure categories.
Discussion
Two previous analyses of this study population have been conducted to evaluate the risk of glioma for subjects categorized by job title.30,31 In those analyses, ORs were calculated based on 6 or more months of employment in one of 128 occupational groups. The analyses for gliomas reported positive associations for butchers, electricians, engineers, general farmers, physicians, and physician assistants, several of which were corroborated by previous studies. The analysis conducted for meningioma in that study population did find an elevated risk of meningioma for individuals who had ever worked in the following occupational groups: auto body painters, designers and decorators, military occupations, industrial production supervisors, teachers, and managers. However, those studies did not identify any particular etiologic agent, and the large number of occupational groups analyzed increased the probability of chance findings. The authors did suggest the need for additional follow-up and provided the motivation for an analysis focused specifically on brain tumor risk associated with occupational exposure to ELF-EMF rather than risk by occupational title.
The use of job modules to collect detailed information directly from individual subjects on sources of exposure to MF in their work environments represents an improvement over previous analyses based only on job titles or JEMs. A JEM provides a relatively straightforward method for exposure assessment compared with the more detailed and time-consuming assessment strategy used in this analysis; however, the job modules provided important details that were used to develop subject-specific exposure estimates. An innovative aspect of the exposure estimates used in this analysis was the incorporation of the job module information into the exposure assessment by adjusting the GM values of the measured TWA exposure to MFs from the JEM. The adjustment for duration was based on a TWA calculation, and the adjustment for distance was a simplification of the relationships found with domestic appliances.32 The formula for combining fields from multiple sources is an extension of the “random phase” approximation.33 While the distributions in exposure levels assigned to different subjects within each job title appear plausible, the accuracy of this methodology could not be ascertained from these data, and some misclassification of exposure was still likely to occur. In addition, job modules were available for only 24% of the jobs reported by the study subjects. For the remainder of jobs, exposures were assigned directly from the JEM.
This study uses MF as a surrogate measure and does not directly address the unmeasured components of the electromagnetic field environment that have cast doubts on the previous occupational epidemiology results based only on exposure to MF.34 ELF-EMFs are time-varying vectors whose frequency, polarization, spatial orientation, and intermittency have all been linked to biologic effects. Therefore, the TWA MF magnitude in the ELF band that was measured for the JEM could be misclassifying MF exposures and biasing risk estimates toward the null.
Furthermore, the metrics used in this analysis were based only on occupational exposure to MFs, whereas MFs are also present in residential environments. However, occupational environments typically have much greater variability in exposure levels, with higher average and peak exposures compared with residential environments. In addition, a previously published analysis of self-reported electrical appliance use among this study population found no association with brain tumor risk; thus, environmental and residential exposures are not likely to have confounded these results.35
In conclusion, occupational exposure to ELF-EMF was assessed in this study using a novel exposure assessment method that included adjustment of exposure estimates based on job-specific questionnaires. However, no association with glioma, glioblastoma, or meningioma was observed among the subjects evaluated in this study. Additional studies are needed to evaluate the accuracy of interview-based exposure assessment methods for case–control studies using information from job modules; nonetheless, the extensive efforts made to enhance the exposure assessment increases confidence in the results of epidemiologic analyses.
Acknowledgment
This project has been funded in part through an intramural program from the National Cancer Institute, National Institutes of Health. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. government.
References
- 1.Ries LAG, Melbert D, Krapcho M, et al. Based on November 2006 SEER data submission, posted to the SEER Web site 2007. Bethesda, MD: National Cancer Institute; 2006. [Accessed December 3, 2007]. Surveillance, Epidemiology, and End Result (SEER) Cancer Statistics Review, 1975–2004. Available at http://seer.cancer.gov/csr/1975_2004. [Google Scholar]
- 2.Preston DL, Ron E, Yonehara S, et al. Tumors of the nervous system and pituitary gland associated with atomic bomb radiation exposure. J Natl Cancer Inst. 2002;94:1555–1563. doi: 10.1093/jnci/94.20.1555. [DOI] [PubMed] [Google Scholar]
- 3.Neglia JP, Robison LL, Stovall M, et al. New primary neoplasms of the central nervous system in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Natl Cancer Inst. 2006;98:1528–1537. doi: 10.1093/jnci/djj411. [DOI] [PubMed] [Google Scholar]
- 4.Inskip PD, Linet MS, Heineman EF. Etiology of brain tumors in adults. Epidemiol Rev. 1995;17:382–414. doi: 10.1093/oxfordjournals.epirev.a036200. [DOI] [PubMed] [Google Scholar]
- 5.Navas-Acien A, Pollan M, Gustavsson P, Plato N. Occupation, exposure to chemicals and risk of gliomas and meningiomas in Sweden. Am J Ind Med. 2002;42:214–227. doi: 10.1002/ajim.10107. [DOI] [PubMed] [Google Scholar]
- 6.Samanic C, De Roos AJ, Stewart PA, Rajaraman P, Waters MA, Inskip PD. Occupational exposure to pesticides and risk of adult brain tumors. Am J Epidemiol. 2008 doi: 10.1093/aje/kwm401. [Epub ahead of print, online February 24, 2008] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rajaraman P, Stewart PA, Samet J, et al. Lead, genetic susceptibility, and risk of adult brain tumors. Cancer Epidemiol Biomarkers Prev. 2006;15:2514–2520. doi: 10.1158/1055-9965.EPI-06-0482. [DOI] [PubMed] [Google Scholar]
- 8.IARC. Non-ionizing radiation, part 1: static and extremely low-frequency (ELF) electric and magnetic fields. IARC Monogr Eval Carcinog Risks Hum. 2002;80:1–395. [PMC free article] [PubMed] [Google Scholar]
- 9.Ahlbom IC, Cardis E, Green A, Linet M, Savitz D, Swerdlow A. Review of the epidemiologic literature on EMF and health. Environ Health Perspect. 2001;109(suppl 6):911–933. doi: 10.1289/ehp.109-1240626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas TL, Stolley PD, Stemhagen A, et al. Brain tumor mortality risk among men with electrical and electronics jobs: a case-control study. J Natl Cancer Inst. 1987;79:233–238. [PubMed] [Google Scholar]
- 11.Cocco P, Dosemeci M, Heineman EF. Occupational risk factors for cancer of the central nervous system: a case-control study on death certificates from 24 U.S. states. Am J Ind Med. 1998;33:247–255. doi: 10.1002/(sici)1097-0274(199803)33:3<247::aid-ajim6>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 12.Bracken TD, Kheifets LI, Sussman SS. Exposure assessment for power frequency electric and magnetic fields (EMF) and its application to epidemiologic studies. J Expo Anal Environ Epidemiol. 1993;3:1–22. [PubMed] [Google Scholar]
- 13.Kelsh MA, Kheifets L, Smith R. The impact of work environment, utility, and sampling design on occupational magnetic field exposure summaries. AIHAJ. 2000;61:174–182. doi: 10.1080/15298660008984526. [DOI] [PubMed] [Google Scholar]
- 14.Savitz DA. Overview of occupational exposure to electric and magnetic fields and cancer: advancements in exposure assessment. Environ Health Perspect. 1995;103(suppl 2):69–74. doi: 10.1289/ehp.95103s269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Floderus B, Persson T, Stenlund C. Magnetic-field exposures in the workplace: reference distribution and exposures in occupational groups. Int J Occup Environ Health. 1996;2(3):226–238. doi: 10.1179/oeh.1996.2.3.226. [DOI] [PubMed] [Google Scholar]
- 16.EMF Interagency Committee. EMF RAPID Program, Project #6 Report: Survey of Personal Magnetic Field Exposure, Phase II: 1000-Person Survey. [Accessed May 5, 2007];2006 Available at http://www.niehs.nih.gov/emfrapid/
- 17.Bowman JD, Touchstone JA, Yost MG. A population-based job exposure matrix for power-frequency magnetic fields. J Occup Environ Hyg. 2007;4:715–728. doi: 10.1080/15459620701528001. [DOI] [PubMed] [Google Scholar]
- 18.Savitz DA, Loomis D. P. Magnetic field exposure in relation to leukemia and brain cancer mortality among electric utility workers. Am J Epidemiol. 1995;141:123–134. doi: 10.1093/oxfordjournals.aje.a117400. [DOI] [PubMed] [Google Scholar]
- 19.Harrington JM, McBride DI, Sorahan T, Paddle GM, van Tongeren M. Occupational exposure to magnetic fields in relation to mortality from brain cancer among electricity generation and transmission workers. Occup Environ Med. 1997;54:7–13. doi: 10.1136/oem.54.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Floderus B, Persson T, Stenlund C, Wennberg A, Ost A, Knave B. Occupational exposure to electromagnetic fields in relation to leukemia and brain tumors: a case-control study in Sweden. Cancer Causes Control. 1993;4:465–476. doi: 10.1007/BF00050866. [DOI] [PubMed] [Google Scholar]
- 21.Grayson JK. Radiation exposure, socioeconomic status, and brain tumor risk in the US Air Force: a nested case-control study. Am J Epidemiol. 1996;143:480–486. doi: 10.1093/oxfordjournals.aje.a008768. [DOI] [PubMed] [Google Scholar]
- 22.Villeneuve PJ, Agnew DA, Johnson KC, Mao Y. Brain cancer and occupational exposure to magnetic fields among men: results from a Canadian population-based case-control study. Int J Epidemiol. 2002;31:210–217. doi: 10.1093/ije/31.1.210. [DOI] [PubMed] [Google Scholar]
- 23.Kheifets L, Bowman JD, Checkoway H, et al. Future needs of occupational epidemiology of extremely low frequency electric and magnetic fields: review and recommendations. Occup Environ Med. 2009;66:72–80. doi: 10.1136/oem.2007.037994. [DOI] [PubMed] [Google Scholar]
- 24.Stewart PA, Stewart WF, Heineman EF, Dosemeci M, Linet M, Inskip PD. A novel approach to data collection in a case-control study of cancer and occupational exposures. Int J Epidemiol. 1996;25:744–752. doi: 10.1093/ije/25.4.744. [DOI] [PubMed] [Google Scholar]
- 25.Stewart PA, Stewart WF, Siemiatycki J, Heineman EF, Dosemeci M. Questionnaires for collecting detailed occupational information. AIHAJ. 1998;59:39–44. doi: 10.1080/15428119891010325. [DOI] [PubMed] [Google Scholar]
- 26.Inskip PD, Hatch EE, Stewart PA. Study design for a case-control investigation of cellular telephones and other risk factors for brain tumours in adults. Radiat Prot Dosimetry. 1999;86:45–52. [Google Scholar]
- 27.Office of Management and Budget. Standard Occupational Classification Manual. Washington, DC: Government Printing Office; 1977. [Google Scholar]
- 28.Office of Management and Budget. Standard Industrial Classification Manual. Washington, DC: Government Printing Office; 1972. [Google Scholar]
- 29.National Institute of Environmental Health Sciences. NIEHS Report on Health Effects from Exposure to Power-Line Frequency Electric and Magnetic Fields. [Accessed December 3, 2007];NIH Publication 99-4493. 1999 Available at http://www.niehs.nih.gov./health/topics./agents/emf./docs./niehs.-report.pdf.
- 30.De Roos AJ, Stewart PA, Linet MS, et al. Occupation and the risk of adult glioma in the United States. Cancer Causes Control. 2003;14:139–150. doi: 10.1023/a:1023053916689. [DOI] [PubMed] [Google Scholar]
- 31.Rajaraman P, De Roos AJ, Stewart PA, et al. Occupation and risk of meningioma and acoustic neuroma in the United States. Am J Ind Med. 2004;45:395–407. doi: 10.1002/ajim.10363. [DOI] [PubMed] [Google Scholar]
- 32.Preece AW, Kaune WT, Grainger P, Preece S, Golding J. Magnetic fields from domestic appliances in the UK. Phys Med Biol. 1997;42:67–76. doi: 10.1088/0031-9155/42/1/004. [DOI] [PubMed] [Google Scholar]
- 33.Kaune WT. Estimating the magnitude of the sum of two magnetic fields with uncertain spatial orientations, polarizations and/or relative phase. Bioelectromagnetics. 2002;23:59–67. doi: 10.1002/bem.98. [DOI] [PubMed] [Google Scholar]
- 34.Kheifets LI, Afifi AA, Buffler PA, Zhang ZW. Occupational electric and magnetic field exposure and brain cancer: a meta-analysis. J Occup Environ Med. 1995;37:1327–1341. doi: 10.1097/00043764-199512000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Kleinerman RA, Linet MS, Hatch EE, et al. Self-reported electrical appliance use and risk of adult brain tumors. Am J Epidemiol. 2005;161:136–146. doi: 10.1093/aje/kwi013. [DOI] [PubMed] [Google Scholar]