Abstract
We established the nationwide, population-based incidence of oligodendroglioma in Denmark during 59 years of monitoring and compared the overall survival of patients with oligodendroglial tumors during the periods 1943–1977 and 1978–2002. On the basis of reports in the Danish Cancer Registry, 1,304 cases of oligodendroglioma were included in the study. We calculated sex- and age-specific incidence rates in 5-year age intervals and for 5-year calendar periods. Overall survival was estimated by the Kaplan-Meier method. In the period 1943–2002, the incidence rate of oligodendroglioma was less than 1 case per 100,000 person-years, but varied somewhat when viewed across isolated periods. Comparison of the incidence rate before and after the introduction of CT scanning did not reveal a significant difference in the incidence rate. The median survival increased from 1.4 years (95% confidence interval [CI], 1.0–1.6) to 3.4 years (95% CI, 2.6–4.2) during the period of study. The overall incidence of oligodendroglioma showed a relatively stable pattern over nearly 60 years of monitoring. Overall survival improved significantly during the study period, which could partly be due to improved diagnostic methods and treatment options.
Keywords: Denmark, epidemiology, oligodendroglioma
Primary brain tumors are a heterogeneous group of relatively uncommon but particularly lethal cancers. Gliomas are the most common major subgroup of primary brain tumors. Oligodendrogliomas are a rare type of glial tumor but are interesting because they are considered to have a better prognosis than other tumors of this type and are particularly sensitive to chemotherapy.1–11 Furthermore, recent research on oligodendrogliomas and other glial tumors has shown that how these tumors respond to chemotherapy is influenced by the presence of certain tumor genetic anomalies such as loss of 1p and 19q.1–6,11,12
Oligodendrogliomas progress slowly and usually arise in the white matter of the brain with involvement of the frontal lobe in more than half of the cases. They are characterized by diffusely infiltrative growth, resulting in a high incidence of seizures during the course of illness.2,3,13–16 They are usually diagnosed in adults aged 40–60 years and slightly more frequently in men than in women.2,4,15–17
No risk factors for oligodendroglioma have been established. Cases have been documented in patients previously irradiated for other reasons, but these account for only a small fraction of all oligodendrogliomas.17
The incidence rates of oligodendroglioma range in different studies from 4% to 33% of all gliomas.3,17–21 This range of rates might be explained by improvements in diagnostic procedures and access to more scanners over time or to increased awareness of oligodendrogliomas because of better treatment results and improved prognosis. Another explanation might be associated with problems in the diagnosis, classification, changes in the criteria for diagnosis of oligodendroglioma versus astrocytoma, period of study, and grading of oligodendrogliomas.18,22,23
The most frequent genetic alterations in oligodendrogliomas are loss of heterozygosity on chromosomes 1p and 19q. The proportions of tumors with these changes were 40%–92% and 50%–80%, respectively.17 Most oligodendrogliomas show loss of heterozygosity at both sites.14,17 The tumor suppressor genes expected to map within these regions have not yet been identified.26 Several studies have shown that loss of heterozygosity at 1p with or without that at 19q is strongly associated with chemosensitivity and longer recurrence-free survival after chemotherapy.5,11,24–26
The results of this large population-based study on the incidence of oligodendrogliomas cover the period 1943–2002 and include data on survival in the period 1943–1999, representing nearly 60 years of nationwide cancer registration in Denmark. Complete information on 1,304 oligodendroglioma patients has been collected.
Materials and Methods
We included all persons from birth to more than 90 years old with oligodendroglioma in Denmark who were reported to the Danish Cancer Registry between 1943 and 2002. The group included both low-grade and anaplastic oligodendrogliomas. Since 1943, this Registry on a nationwide and population-based platform has maintained records of all patients with malignant and benign neoplasms in Denmark, and reporting of cases to the Registry has been mandatory since 1987. Cases reported manually are supplemented with unrecorded cases identified by computerized linkage to the Cause of Death Registry and the National Registry of Patients. Comprehensive validation has shown that the Danish Cancer Registry is 95%–99% complete and valid.27–31 Between 1943 and 2002, tumors were coded and classified according to a modified Danish version of the International Classification of Diseases, version 7 (ICD-7) (code 0935). Tumors identified between 1978 and 2002 were also coded and classified according to the International Classification of Diseases–Oncology (ICD-O).
The information retrieved from the Danish Cancer Registry included all cases of oligodendroglioma (ICD-O morphology codes 9450.3–9460.3 and topography codes 191.0–9) reported between 1943 and 2002. For each patient, we obtained the date of diagnosis, sex, age, degree of histological verification, tumor characteristics (topographical and morphological features), treatment (within 4 months of date of diagnosis), and mode of diagnosis. Information on vital status was retrieved from the Central Population Registry. The Central Population Registry was established in Denmark on April 1, 1968, when all residents were assigned a 10-digit personal identification number, which includes six digits for date of birth. We identified the vital statistics of all patients during the period of study by matching the study population to this Registry.
We calculated age-specific incidences for both sexes in 5-year age intervals and for 5-year calendar periods between 1943 and 2002. The incidences during 1998–2002 were divided into two calendar periods, 1998–1999 and 2000–2002, because the data from the Danish Cancer Registry on oligodendrogliomas in 2000–2002 has not yet been cross-checked against other registries. The incidences were age-standardized to the World Standard Population.32
The overall survival of patients with oligodendroglioma in Denmark 1943–1999 was estimated by the Kaplan–Meier method. Survival was measured from the date of diagnosis until date of emigration, date of death, or December 31, 1999, whichever came first. Tests of equality of the survival curves were performed with the log-rank method. Patients were separated into two groups—those in whom oligodendroglioma was diagnosed between 1943 and 1977 and those in whom it was diagnosed between 1978 and 1999 on the basis of the time of introduction of CT scanners in Denmark and the introduction of the ICD-O.
Results
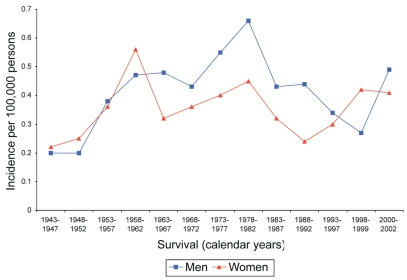
In the period 1943–2002, 1,304 patients with oligodendroglioma were reported to the Danish Cancer Registry, 695 (53%) of which were men and 609 (47%) women, for a male:female ratio of 1.1:1 (data not shown). During the period of the study, the incidence of oligodendroglioma showed some variation, ranging from 0.21 cases/100,000 persons per year in 1943–1947 to the highest incidence of 0.56 cases/100,000 persons per year in 1978–1982 (Fig. 1 and Table 1). Analysis of data in Table 1 produced an average total incidence rate of 0.37 cases/100,000 person-years before 1978, and an incidence rate of 0.40 cases/100,000 person-years subsequent to 1978 (even with the inclusion of the particularly high incidence rate of 0.56 in the years 1978–1982). The steepest increase in the incidence took place from the beginning of the study period (1943) to around 1960. From the period 1958–1962 the incidence rates have varied somewhat when viewed across isolated periods and have been relatively unchanged throughout the time of the study. The incidence rates for men and women separately showed a similar pattern. Overall, the incidence of oligodendroglioma was higher in men than in women. The percentage of oligodendroglial tumors verified by histological confirmation rose from 94% in 1943 to an almost complete confirmation from the beginning of the 1980s (Table 1). Since 1983, almost 100% of histological tissue specimens have been derived from the primary tumor (data not shown).
Fig. 1.
Incidence of oligodendroglioma per 100,000 persons, 1943–2002.
Table 1.
Incidence of oligodendroglioma, adjusted to the World Standard Population, in a study in Denmark, 1943–2002
| Women
|
Men
|
All
|
|||||
|---|---|---|---|---|---|---|---|
| Period of Diagnosis | No. of Cases | Cases/ 100,000 Person-Years | No. of Cases | Cases/ 100,000 Person-Years | No. of Cases | Cases/ 100,000 Person-Years | Histological Confirmation (%) |
| 1943–1947 | 25 | 0.22 | 23 | 0.20 | 48 | 0.21 | 94 |
| 1948–1952 | 30 | 0.25 | 22 | 0.20 | 52 | 0.23 | 94 |
| 1953–1957 | 46 | 0.36 | 46 | 0.38 | 92 | 0.37 | 92 |
| 1958–1962 | 75 | 0.56 | 59 | 0.47 | 134 | 0.51 | 96 |
| 1963–1967 | 46 | 0.32 | 62 | 0.48 | 108 | 0.40 | 98 |
| 1968–1972 | 52 | 0.36 | 59 | 0.43 | 111 | 0.39 | 95 |
| 1973–1977 | 61 | 0.40 | 76 | 0.55 | 137 | 0.47 | 96 |
| 1978–1982 | 72 | 0.45 | 94 | 0.66 | 166 | 0.56 | 100 |
| 1983–1987 | 47 | 0.32 | 63 | 0.42 | 110 | 0.37 | 99 |
| 1988–1992 | 37 | 0.24 | 66 | 0.44 | 103 | 0.34 | 99 |
| 1993–1997 | 48 | 0.30 | 51 | 0.33 | 99 | 0.32 | 97 |
| 1998–1999 | 28 | 0.42 | 18 | 0.27 | 46 | 0.35 | 100 |
| 2000–2002 | 41 | 0.41 | 53 | 0.49 | 94 | 0.45 | 97 |
Table 2 shows that the number of patients with oligodendroglioma receiving surgery versus surgery and radiation in Denmark between 1943 and 2002 has been fairly consistent.
Table 2.
Treatment of patients with oligodendroglioma, from birth to 90+ years, in a study in Denmark, 1943–2002
| Period of Diagnosis | Surgery
|
Surgery and Radiotherapy
|
Surgery and Chemotherapy
|
No information and Other Methods
|
||||
|---|---|---|---|---|---|---|---|---|
| No. of Cases | % | No. of Cases | % | No. of Cases | % | No. of Cases | % | |
| 1943–1947 | 22 | 46 | 11 | 23 | – | – | 15 | 31 |
| 1948–1952 | 20 | 39 | 15 | 29 | – | – | 17 | 33 |
| 1953–1957 | 31 | 34 | 23 | 25 | – | – | 38 | 41 |
| 1958–1962 | 62 | 46 | 40 | 30 | – | – | 32 | 24 |
| 1963–1967 | 51 | 47 | 41 | 38 | – | – | 16 | 15 |
| 1968–1972 | 59 | 53 | 11 | 10 | – | – | 41 | 37 |
| 1973–1977 | 82 | 60 | 13 | 10 | – | – | 42 | 31 |
| 1978–1982 | 90 | 54 | 19 | 11 | 15 | 9 | 42 | 25 |
| 1983–1987 | 43 | 39 | 27 | 24 | 8 | 7 | 33 | 30 |
| 1988–1992 | 54 | 51 | 26 | 25 | 2 | 2 | 23 | 22 |
| 1993–1997 | 39 | 39 | 35 | 35 | 2 | 2 | 24 | 24 |
| 1998–1999 | 23 | 50 | 12 | 26 | 2 | 4 | 9 | 20 |
| 2000–2002 | 46 | 49 | 26 | 28 | 7 | 7 | 15 | 16 |
| Total | 622 | 48 | 299 | 23 | 36 | 3 | 347 | 27 |
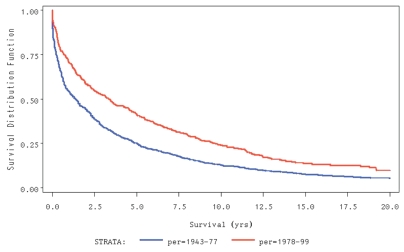
Fig. 2 shows that the median survival of patients with oligodendroglioma improved significantly from 1.4 years (95% CI, 1.0–1.6) in patients whose tumors were diagnosed between 1943 and 1977 to 3.4 years (95% CI, 2.6–4.2) in patients whose tumors were diagnosed between 1978 and 1999.
Fig. 2.
Kaplan-Meier analysis revealed that of median survival among patients with oligodendroglioma improved significantly from 1.4 years between 1943 and 1977 to 3.4 years between 1978 and 1999.
Discussion
In this nationwide, population-based study of 1,304 cases of oligodendrogliomas in Denmark, incidence of this rare tumor varied somewhat when viewed across isolated periods between 1943 and 2002; however, the incidence has been relatively unchanged throughout the period of the study and did not increase significantly from the period 1943–1977 to the period 1978–2002. In addition, we observed a significant long-term improvement in overall survival for patients with oligodendrogliomas diagnosed between 1978 and 1999 as compared with those diagnosed between 1943 and 1977.
It is important to investigate whether the pattern of observed incidence rates of gliomas is real or whether it can be attributed to the introduction of improved diagnostic methods, such as CT and MRI, or to changes in diagnostic criteria. Lönn et al. described an increase in the incidence of glioma mostly confined to the oldest age groups in the population in the Nordic countries including Denmark in the late 1970s and early 1980s, after which the incidence remained fairly stable.33 We also found that the incidence of oligodendroglioma increased more in older age groups (data not shown) and, in general, that our main findings are in line with those reported in most other studies of the incidence of oligodendroglioma (Table 3). The results of the various studies are, however, difficult to compare owing to a lack of consensus about use of the World Standard Population as the reference population.
Table 3.
Average annual crude incidence of oligodendroglioma in descriptive epidemiological studies
| Incidence per 100,000 Person-Years
|
||||||
|---|---|---|---|---|---|---|
| Geographical Area (Reference No.) | Year of Publication | Period of Notification | No. of Cases | Overall | Male | Female |
| Ferrara, Italy40 | 1994 | 1976–1991 | 13 | 0.45 | 0.36 | 0.52 |
| Norway6 | 1989 | 1955–1984 | 382 | 0.30 | – | – |
| Victoria State, Australia41 | 1993 | 1982–1990 | 43 | – | 0.13 | 0.09 |
| Scandinavia33 | 2004 | 1993–1998 | – | – | 0–1 | 0–1 |
| Denmark (current study) | 1943–2002 | 1,304 | 0.38 | 0.40 | 0.35 | |
The first CT scanner was installed in Denmark in 1978. In a recent report on CT scanner capacity in Denmark, 55 scanners were found to be operating in 1998.31 It is evident that this increased capacity, in general, could have resulted in the diagnosis of more brain tumors. In line with this argument, Helseth showed a close relationship between CT use and an increased incidence of primary brain tumors.34 Also the introduction of MRI in Denmark is important for the diagnosis of oligodendrogliomas, in particular for the diagnosis of low-grade oligodendrogliomas, which do not always show on CT. Although the role of MRI on oligodendroglioma incidence for now is not evident, it could become more important in the future. Certain studies have shown MRI to be able to distinguish between low-grade oligodendrogliomas and astrocytomas, and also between oligodendroglioma cases with loss of heterozygosity on chromosomes 1p and 19q and oligodendroglioma cases without these characteristics. However, we did not observe a clear increase in the incidence of the rare oligodendroglioma tumor during the study period concurrent with increasing access to CT or MRI scanning facilities.
A rise in the incidence of oligodendroglioma in Denmark was observed in 1978–1982 (Fig. 1). In 1978, a new classification system, ICD-O, was introduced in Denmark for coding and classifying tumors, in addition to the ICD-7. The introduction of a new classification system can create greater awareness of tumors, and this often results in increased incidence rates immediately after the change. We cannot exclude the possibility that a changed pattern of seeking medical services influenced the incidence, assuming that some patients in the first part of the study period died before diagnosis and further were not diagnosed by autopsy. This number of undiagnosed cases might be reduced in the later period of the study owing to earlier contact with the public health system. However, this possible change in behavior is impossible to evaluate with the use of the information in the Danish Cancer Registry. In addition this factor is speculative and cannot explain major changes in the incidence rates.
Several studies have shown that men are at higher risk for developing oligodendroglioma than women.3–4,14,17 Furthermore, Fleury et al. reported that the peak incidence occurred at a slightly higher age in women than in men.4 We had a similar finding and speculate that this difference indicates an effect of female sex hormones on the risk of developing oligodendroglioma, with higher levels offering more protection. The fact that oligodendrogliomas are frequently diagnosed later in life in women than in men supports this theory; however, no studies have been published indicating an association.
In this study we found that the survival of patients with oligodendroglial tumors in Denmark has improved, although the improvement is smaller than that seen in other studies (Table 4). Several factors influence survival, including an early, correct diagnosis, the immediate treatment given, subsequent care, and age. Early, correct diagnoses can be obtained by use of CT and MRI and also by ensuring histological verification of the tumors. The introduction of CT and MRI into clinical practice in Denmark might therefore account for some of the observed increase in survival. Johannesen et al. found that the median duration of the pre-diagnosis period decreased from 12.4 months before the introduction of scanning as a routine diagnostic instrument to 6.1–6.3 months after.35 A shorter pre-diagnostic period probably allows for earlier treatment and smaller tumor size at the time of diagnosis.
Table 4.
Median duration of survival in studies of oligodendroglioma
| Geographical Area (Reference No.) | Year of Publication | Median Years of Follow-up (Range) | Period of Notification | No. of Cases | Median Survival
|
|
|---|---|---|---|---|---|---|
| Years | 95% CI | |||||
| Norway35 | 2003 | (0–32) | 1970–1981 | 135 | 4.6 | 3.6–5.7 |
| Norway35 | 2003 | (0–32) | 1982–1993 | 108 | 8.1 | 6.0–10.2 |
| Japan5 | 2003 | 3.1 (1–7) | 1976–2001 | 20 | 6.0 | – |
| Rochester, Minnesota, USA42 | 2001 | 7.5 (1.9–11.5) | 1960–1990 | 122 | 8.8 | – |
| Minnesota, USA23 | 1992 | 8.5 (3–22.3) | 1960–1982 | 82 | 7.1 | – |
| Germany36 | 1998 | (0–14) | 1977–1990 | 89 | 2.8 | – |
| Denmark (current study) | (0–34) | 1943–1977 | 682 | 1.4 | 1.0–1.6 | |
| Denmark (current study) | (0–21) | 1978–1999 | 524 | 3.4 | 2.6–4.2 | |
The immediate treatment given to patients with oligodendroglioma is usually surgery, and the extent of surgical resection can affect survival, as shown in three studies. Johannesen et al. reported a survival time of 7.6 years after total resection and 6.4 years after biopsy; however, this study also included other types of astrocytomas in the survival analyses.35 Likewise, Paleologos and Cairncross described a median survival time of 12.6 years after gross total resection and 4.9 years after subtotal resection.15 Dehgani et al. reported a difference of only 2.1 years in median survival time after total resection compared with subtotal resection.36 Brain surgery has undoubtedly improved in Denmark since 1943, and this improvement could be one of the main reasons for increased survival; however, diagnostic capabilities could also partly explain this increase in survival, as more tumors can be diagnosed at a level where total resection is possible.
About 10% of patients with oligodendroglioma in Denmark received chemotherapy in 1978–1982, after which use of this modality decreased. Treatment with chemotherapy is, therefore, unlikely to be responsible for the observed improved survival of patients with oligodendrogliomas diagnosed between 1978 and 1999. However, for a large number of patients (15%–41%) per time period, we have no treatment information (Table 2). It is possible some of these have received unreported chemotherapy and thereby contribute to the observed improved survival. A trend to increasing use in 1998 indicates that it would be important to reevaluate the survival of patients with oligodendroglial tumors in Denmark in 5 years’ time, although information about treatment is incomplete in the Danish Cancer Registry.
The increased survival after the introduction of chemotherapy has been clearly established. But whether chemotherapy is given at first diagnosis or at recurrence seems irrelevant with respect to overall survival.37 Cairn-cross and Macdonald reported that chemotherapy is not curative for oligodendrogliomas, but the high response and long response durations are very encouraging. Despite a few patients diagnosed with low-grade oligodendrogliomas who responded well to chemotherapy, it is not the immediate appropriate treatment for these patient groups.38
Age-dependent variations in prognosis have been observed in several studies, with patients whose tumors were diagnosed at younger ages surviving longer than those who received their diagnosis at older ages.19,35,39 In our study, patients aged 0–44 years made up 42.5% of the study population in the period 1943–1977 and 43.0% in the period 1978–1999; however, no difference in age-specific results for median survival was seen between the two periods (data not shown).
The information on treatment in the Danish Cancer Registry indicated no major change in treatment methods in Denmark during the years under study, indicating that the observed improvement in survival cannot be explained by a change in treatment. Thus, improved diagnostic capacity appears to be the major factor in the increase in median survival time. Although the median survival time appears to be shorter in Denmark than in the United States (Table 4), the wide confidence intervals in the U.S. study31,40 include the risk estimate found in our study, indicating that the small number of cases in the U.S. study can explain the overall results. One could argue that the size of our study and the rigorous data collection method including complete follow-up give these survival data more weight than data from other studies. Nevertheless, we cannot totally exclude the possibility that differences in diagnostic criteria, including a combination of grade 2 and 3 oligodendroglioma tumors, or misclassification of oligodendroglial tumors can explain the differences in the results published so far.
Surprisingly, the median survival in Norway is also found to be longer than that in Denmark (Table 4). The difference might be explained by the number of cases included in the studies and by differences in criteria for patient selection. The Norwegian study included only patients aged 15 to 69 years, whereas our study included patients aged 0 to more than 90 years. The age-dependent variation in survival can explain part of the difference in results.
Our study has a number of advantages. With 1,304 cases of oligodendroglioma, this study is the largest study conducted so far. It is based on data from a nationwide, population-based cancer registry and not on surgical series of brain cancer patients from various hospitals. In addition, the data were cross-checked against data in other administrative registries by a unique personal identifier. The entire quality control process is supervised by medical doctors. The data in the Danish Cancer Registry are of high quality, and the source population is homogeneous and has free access to medical care, thereby reducing the likelihood of selection or information bias. As this study is based on data from registries, it is not vulnerable to the potential bias seen in studies based on self-reported data.
The limitations of our study include the possibility of coding errors. Furthermore, use of registry data does not allow evaluation of the effect of changes in histopathological criteria. The diagnosis of this tumor is difficult, and a centralized pathological review would reduce misclassification. Although possible misclassification of oligodendroglioma could create bias, the extensive histological verification in our study was mainly conducted at large university-based neuropathological departments, which to some extent could have eliminated this potential bias. New evidence suggests that gene arrays contribute to a better classification of cases of oligoden-drogliomas.37
Lead-time bias can also influence survival analysis; thus, the improved survival after 1978 versus before is partly due to an earlier diagnosis.
Between 1943 and 2002 the incidence of oligodendroglioma in Denmark, although somewhat variable when viewed across isolated periods, has been relatively unchanged. A comparison of the two study periods before and after 1978 did not reveal a significant increase in the incidence rate. A 2-year increase in the median survival of patients with oligodendroglial tumors occurred between 1943–1977 and 1978–1999. This study underscores the importance of an early diagnosis of cases of oligodendrogliomas, thereby ensuring the appropriate treatment and outcome for patients.
References
- 1.Allison RR, Schulsinger A, Vongtama V, Barry T, Shin KH. Radiation and chemotherapy improve outcome in oligodendroglioma. Int J Radiat Oncol Biol Phys. 1997;37:399–403. doi: 10.1016/s0360-3016(96)00452-x. [DOI] [PubMed] [Google Scholar]
- 2.Ellis TL, Stieber VW, Austin RC. Oligodendroglioma. Curr Treat Options Oncol. 2003;4:479–490. doi: 10.1007/s11864-003-0048-1. [DOI] [PubMed] [Google Scholar]
- 3.Engelhard HH, Stelea A, Mundt A. Oligodendroglioma and anaplasticoligodendroglioma: clinical features, treatment and prognosis. Surg Neurol. 2003;60:443–456. doi: 10.1016/s0090-3019(03)00167-8. [DOI] [PubMed] [Google Scholar]
- 4.Fleury A, Menegoz F, Grosclaude P, et al. Descriptive epidemiology of cerebral gliomas in France. Cancer. 1997;79:1195–1202. doi: 10.1002/(sici)1097-0142(19970315)79:6<1195::aid-cncr19>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 5.Hashimoto N, Murakami M, Takahashi Y, Fujimoto M, Inazawa J, Mineura K. Correlation between genetic alteration and long-term clinical outcome of patients with oligodendroglial tumors, with identification of a consistent region of deletion on chromosome arm 1p. Cancer. 2003;97:2254–2261. doi: 10.1002/cncr.11322. [DOI] [PubMed] [Google Scholar]
- 6.Helseth A, Mork SJ. Neoplasms of the central nervous system in Norway. III. Epidemiological characteristics of intracranial gliomas according to histology. APMIS. 1989;97:547–555. [PubMed] [Google Scholar]
- 7.Jacob R, Jyothirmayi R, Dalal Y, Nambiar U, Rajan B, Nair MK. Oligodendroglioma: clinical profile and treatment results. Neurol India. 2002;50:462–466. [PubMed] [Google Scholar]
- 8.Karim AB, Maat B, Hatlevoll R, et al. A randomized trial on dose-response in radiation therapy of low-grade cerebral glioma: European Organization for Research and Treatment of Cancer (EORTC) Study 22844. Int J Radiat Oncol Biol Phys. 1996;36:549–556. doi: 10.1016/s0360-3016(96)00352-5. [DOI] [PubMed] [Google Scholar]
- 9.Karim AB, Afra D, Cornu P, et al. Randomized trial on the efficacy of radiotherapy for cerebral low-grade glioma in the adult: European Organization for Research and Treatment of Cancer Study 22845 with the Medical Research Council Study BRO4: an interim analysis. Int J Radiat Oncol Biol Phys. 2002;52:316–324. doi: 10.1016/s0360-3016(01)02692-x. [DOI] [PubMed] [Google Scholar]
- 10.Van den Bent MJ, Taphoorn MJ, Brandes AA, et al. Phase II study of first-line chemotherapy with temozolomide in recurrent oligodendroglial tumors: the European organization for research and treatment of cancer brain tumor group study 26971. J Clin Oncol. 2003;21:2525–2528. doi: 10.1200/JCO.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 11.Van den Bent MJ. Advances in the biology and treatment of oligodendrogliomas. Curr Opin Neurol. 2004;17:675–680. doi: 10.1097/00019052-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Nutt CL, Mani DR, Betensky RA, et al. Gene expression-based classification of alignantgliomas correlates better with survival than histological classification. Cancer Res. 2003;63:1602–1607. [PubMed] [Google Scholar]
- 13.Daumas-Duport C, Varlet P, Tucker ML, Beuvon F, Cervera P, Chodkiewicz JP. Oligodendrogliomas. Part I: Patterns of growth, histological diagnosis, clinical and imaging correlations: a study of 153 cases. J Neurooncol. 1997;34:37–59. doi: 10.1023/a:1005707203596. [DOI] [PubMed] [Google Scholar]
- 14.Engelhard HH, Stelea A, Cochran EJ. Oligodendroglioma: pathology and molecular biology. Surg Neurol. 2002;58:111–117. doi: 10.1016/s0090-3019(02)00751-6. [DOI] [PubMed] [Google Scholar]
- 15.Paleologos NA, Cairncross JG. Treatment of oligodendroglioma: an update. Neuro-Oncology. 1999;1:61–68. [PMC free article] [PubMed] [Google Scholar]
- 16.Peterson K, Cairncross JG. Oligodendrogliomas. Neurol Clin. 1995;13:861–873. [PubMed] [Google Scholar]
- 17.World Health Organization. Pathology and genetics, tumours of the nervous system. Lyon, France: World Health Organization; 2000. [Google Scholar]
- 18.Chinot O. Chemotherapy for the treatment of oligodendroglial tumors. Semin Oncol. 2001;28:13–18. doi: 10.1016/s0093-7754(01)90066-1. [DOI] [PubMed] [Google Scholar]
- 19.Feigenberg SJ, Amdur RJ, Morris CG, Mendenhall WM, Marcus RB, Jr, Friedman WA. Oligodendroglioma: does deferring treatment compromise outcome? Am J Clin Oncol. 2003;26:e60–e66. doi: 10.1097/01.COC.0000072507.25834.D6. [DOI] [PubMed] [Google Scholar]
- 20.Fortin D, Cairncross JG, Hammond RR. Oligodendroglioma: an appraisal of recent data pertaining to diagnosis and treatment. Neurosurgery. 1999;45:1279–1291. doi: 10.1097/00006123-199912000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Sunyach MP, Pommier P, Martel L, et al. Conformal irradiation for pure and mixed oligodendroglioma: the experience of Centre Leon Berard Lyon. Int J Radiat Oncol Biol Phys. 2003;56:296–303. doi: 10.1016/s0360-3016(03)00089-0. [DOI] [PubMed] [Google Scholar]
- 22.Coons SW, Johnson PC, Scheithauer BW, Yates AJ, Pearl DK. Improving diagnostic accuracy and interobserver concordance in the classification and grading of primary gliomas. Cancer. 1997;79:1381–1393. doi: 10.1002/(sici)1097-0142(19970401)79:7<1381::aid-cncr16>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 23.Shaw EG, Scheithauer BW, O’Fallon JR, Tazelaar HD, Davis DH. Oligodendrogliomas: the Mayo Clinic experience. J Neurosurg. 1992;76:428–434. doi: 10.3171/jns.1992.76.3.0428. [DOI] [PubMed] [Google Scholar]
- 24.Hoang-Xuan K, Capelle L, Kujas M, et al. Temozolomide as initial treatment for adults with low-grade oligodendrogliomas or oligoastrocytomas and correlation with chromosome 1p deletions. J Clin Oncol. 2004;22:3133–3138. doi: 10.1200/JCO.2004.10.169. [DOI] [PubMed] [Google Scholar]
- 25.Perry JR, Louis DN, Cairncross JG. Current treatment of oligodendrogliomas. Arch Neurol. 1999;56:434–436. doi: 10.1001/archneur.56.4.434. [DOI] [PubMed] [Google Scholar]
- 26.Reifenberger G, Louis DN. Oligodendroglioma: toward molecular definitions in diagnostic neurooncology. J Neuropathol Exp Neurol. 2003;62:111–126. doi: 10.1093/jnen/62.2.111. [DOI] [PubMed] [Google Scholar]
- 27.Jensen AR, Storm HH, Moller S, Overgaard J. Validity and representativity in the Danish breast cancer cooperative group—a study on protocol allocation and data validity from one country to a multicentre database. Acta Oncol. 2003;42:179–185. doi: 10.1080/02841860310000737. [DOI] [PubMed] [Google Scholar]
- 28.Storm HH. Completeness of cancer registration in Denmark 1943–1966 and efficacy of record linkage procedures. Int J Epidemiol. 1988;17:44–49. doi: 10.1093/ije/17.1.44. [DOI] [PubMed] [Google Scholar]
- 29.Storm HH. The Danish Cancer Registry, a self-reporting national cancer registration system with elements of active data collection. IARC Sci Publ. 1991:220–236. [PubMed] [Google Scholar]
- 30.Storm HH, Michelsen EV, Clemmesen IH, Pihl J. The Danish Cancer Registry—history, content, quality and use. Dan Med Bull. 1997;44:535–539. [PubMed] [Google Scholar]
- 31.The National Board of Health. CT and MR-scanner report. Copenhagen, Denmark: The National Board of Health; 2000. [Google Scholar]
- 32.Boyle P, Parkin DM. Cancer registration: principles and methods Statistical methods for registries. IARC Sci Publ. 1991;(95):126–158. [PubMed] [Google Scholar]
- 33.Lönn S, Klaeboe L, Hall P, et al. Incidence trends of adult primary intra-cerebral tumors in four Nordic countries. Int J Cancer. 2004;108:450–455. doi: 10.1002/ijc.11578. [DOI] [PubMed] [Google Scholar]
- 34.Helseth A. The incidence of primary central nervous system neoplasms before and after computerized tomography availability. J Neurosurg. 1995;83:999–1003. doi: 10.3171/jns.1995.83.6.0999. [DOI] [PubMed] [Google Scholar]
- 35.Johannesen TB, Langmark F, Lote K. Progress in long-term survival in adult patients with supratentorial low-grade gliomas: a population-based study of 993 patients in whom tumors were diagnosed between 1970 and 1993. J Neurosurg. 2003;99:854–862. doi: 10.3171/jns.2003.99.5.0854. [DOI] [PubMed] [Google Scholar]
- 36.Dehghani F, Schachenmayr W, Laun A, Korf HW. Prognostic implication of histopathological, immunohistochemical and clinical features of oligodendrogliomas: a study of 89 cases. Acta Neuropathol. 1998;95:493–504. doi: 10.1007/s004010050830. [DOI] [PubMed] [Google Scholar]
- 37.Van den Bent MJ. Advances in the biology and treatment of oligodendrogliomas. Curr Opin Neurol. 2004;17:675–680. doi: 10.1097/00019052-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Cairncross JG, Macdonald DR. Successful chemotherapy for recurrent malignant oligodendroglioma. Ann Neurol. 1988;23:360–364. doi: 10.1002/ana.410230408. [DOI] [PubMed] [Google Scholar]
- 39.Bauman G, Lote K, Larson D, et al. Pretreatment factors predict overall survival for patients with low-grade glioma: a recursive partitioning analysis. Int J Radiat Oncol Biol Phys. 1999;45:923–929. doi: 10.1016/s0360-3016(99)00284-9. [DOI] [PubMed] [Google Scholar]
- 40.Tola MR, Casetta I, Granieri E, et al. Intracranial gliomas in Ferrara, Italy, 1976 to 1991. Acta Neurol Scand. 1994;90:312–317. doi: 10.1111/j.1600-0404.1994.tb02730.x. [DOI] [PubMed] [Google Scholar]
- 41.Preston-Martin S, Staples M, Farrugia H, Giles G. Primary tumors of the brain, cranial nerves and cranial meninges in Victoria, Australia, 1982–1990: patterns of incidence and survival. Neuroepidemiology. 1993;12:270–279. doi: 10.1159/000110328. [DOI] [PubMed] [Google Scholar]
- 42.Giannini C, Scheithauer BW, Weaver AL, et al. Oligodendrogliomas: reproducibility and prognostic value of histological diagnosis and grading. J Neuropathol Exp Neurol. 2001;60:248–262. doi: 10.1093/jnen/60.3.248. [DOI] [PubMed] [Google Scholar]