Abstract
Survival rates of pediatric brain tumor patients have significantly improved over the years due to developments in diagnostic techniques, neurosurgery, chemotherapy, radiotherapy, and supportive care. However, brain tumors are still an important cause of cancer-related deaths in children. Prognosis is still highly dependent on clinical characteristics, such as the age of the patient, tumor type, stage, and localization, but increased knowledge about the genetic and biological features of these tumors is being obtained and might be useful to further improve outcome for these patients. It has become clear that the deregulation of signaling pathways essential in brain development, for example, sonic hedgehog (SHH), Wnt, and Notch pathways, plays an important role in pathogenesis and biological behavior, especially for medulloblastomas. More recently, data have become available about the cells of origin of brain tumors and the possible existence of brain tumor stem cells. Newly developed array-based techniques for studying gene expression, protein expression, copy number aberrations, and epigenetic events have led to the identification of other potentially important biological abnormalities in pediatric medulloblastomas and ependymomas.
Keywords: biological characteristics, ependymoma, epigenetic events, gene expression, medulloblastoma, protein expression, signaling pathways
The causes of pediatric brain tumors are largely unknown. Environmental factors, such as smoking, diet, and other exposures, do not predispose the brain to develop tumors.1 Only a very small proportion of brain tumors are caused by hereditary gene defects (Table 1), irradiation, or immune suppression. Additional knowledge about the biological characteristics of pediatric brain tumors may provide new information about pathogenesis, facilitate diagnosis, contribute to better risk-group stratification for therapy, or be used to develop new therapeutic targets. To identify these biological factors, many techniques have been developed over the years. In this article, we review newly identified aberrantly expressed genes and proteins, chromosomal changes, DNA copy number abnormalities, and other genetic changes that may be important in the pathogenesis and biological behavior of two frequent pediatric brain tumor subtypes, medulloblastomas and ependymomas.
Table 1.
Hereditary syndromes predisposing to the development of a brain tumor
| Disease | Gene (Chromosomal Location) | CNS Tumor Associated with Disease | Involvement in Sporadic CNS Tumor |
|---|---|---|---|
| Li-Fraumeni syndrome | p53 (17p13.1) | Astrocytoma | Astrocytoma |
| Medulloblastoma | Choroid plexus tumor | ||
| Neurofibromatosis type I | NF1 (17q11.2) | Astrocytoma | ? |
| Neurofibromatosis type II | NF2 (22q12.2) | Vestibular and spinal schwannoma | Meningioma |
| Ependymoma | Schwannoma | ||
| Meningioma | |||
| Nevoid basal cell carcinoma syndrome (Gorlin’s syndrome) | PTCH (9q22.3) | Medulloblastoma | Medulloblastoma |
| Tuberous sclerosis | TSC1 (9q34) | Subependymal giant-cell tumor | ? |
| TSC2 (16p13) | |||
| Turcot’s syndrome A | APC (5q21–q22) | Medulloblastoma | Medulloblastoma |
| Turcot’s syndrome B | MLH1 (3p21.3) | Glioblastoma | (Astrocytic tumor) |
| MSH2 (2p22–p21) | Ependymoma | ||
| MLH3 (14q24) | |||
| PMS1 (2q31–q33) | |||
| PMS2 (7p22) | |||
| Von Hippel Lindau disease | VHL (3p25) | Hemangioblastoma | ? |
| Cowden disease | PTEN (10q22–q23) | Astrocytoma | Glioblastoma |
| Melanoma-astrocytoma syndrome | CDKN2A (9p21) | Astrocytoma | Astrocytoma |
| Rubenstein-Taybi syndrome | CBP (16p13.3) | Medulloblastoma | ? |
| Meningioma | |||
| Oligodendroglioma | |||
| MEN1 syndrome | MEN1 (11q13) | Ependymoma | Ependymoma |
| Pituitary tumor |
Medulloblastoma
Clinical Aspects
Medulloblastoma is the most common embryonal CNS tumor of childhood and is likely composed of biologically different subsets of tumors arising from stem and/or progenitor cells of the cerebellum. The World Health Organization recognizes at least five different histological types of medulloblastoma, and there is increasing evidence that prognosis and possibly response to therapy depend on the tumor’s cell of origin and the cellular pathways active in tumor development and growth.
Medulloblastomas, which by definition arise in the posterior fossa, are conventionally stratified on the basis of clinical parameters, such as extent of tumor at the time of diagnosis and completeness of surgical resection, into average-risk and high-risk (poor-prognosis) disease.2 For children older than 3 years with nondisseminated disease and for partially resected “high-risk” disease, standard therapy includes both treatment with radiotherapy and adjuvant chemotherapy.3 Five-year disease-free survival rates of 80% or more are now being reported by multiple groups for patients with average-risk medulloblastoma, and a major focus of new treatment approaches is the development of innovative ways to reduce long-term toxicity of therapy.3 Approaches that have been used and are under study include reduction of the total dose of craniospinal radiation therapy, reduction of the volume of local boost radiotherapy, and use of less neurotoxic chemotherapeutic agents.3 Even in patients with high-risk disease, with current means of treatment, 5-year survival rates of 60% or more are now being reported.4 Most therapeutic approaches for “high-risk” patients have continued to use relatively high doses of craniospinal radiation therapy and aggressive chemotherapeutic approaches.4
The treatment for infants with medulloblastoma remains highly problematic. The volumes and doses of radiotherapy required for disease control cause significant brain injury in patients of all ages and predominantly manifest as long-term neurocognitive sequelae, but they are especially damaging in the very young child.5 For this reason, most therapeutic approaches have focused on either delaying or eliminating radiotherapy by the use of increasingly aggressive chemotherapeutic approaches that have incorporated potentially neurotoxic drugs, such as methotrexate, or high-dose chemotherapy supported by autologous peripheral stem cell rescue.6 There is some suggestion that such approaches are more effective, but some of these apparent improvements in survival may also be related to separation of more aggressive tumors, such as atypical teratoid/rhabdoid tumors, from the cohort of patients treated or the inclusion of lower-risk patients, such as those with desmoplastic tumors, in treatment protocols.7 A major hope for the future is that the incorporation of biological agents targeting specific signaling pathways will not only make treatment more effective, but also allow a reduction in neurotoxic therapy.
Genetic and Biological Aspects
Developmental Signaling Pathways
Several hereditary syndromes predispose to the development of a brain tumor (Table 1), and the underlying gene defects are thought to provide information about the critical genes in the pathogenesis of brain tumors. The genes mutated in syndromes predisposing to medulloblastoma development are frequently involved in cellular signaling pathways (Table 2), which are important regulators of brain development, such as sonic hedgehog (SHH), Wnt, and Notch (Fig. 1).
Table 2.
Differentially expressed genetic and proteomic markers identified in medulloblastomas and ependymomas
| Gene | Change | Percentage of Tumors Expressing Gene | Reference | Correlating with |
|---|---|---|---|---|
| MEDULLOBLASTOMA | ||||
| SHH signaling | ||||
| PTCH1 | Mutation | 4.8%–13.5% | 105–109 | Desmoplastic subtype |
| PTCH2 | Overexpression | Unknown | 16 | — |
| SUFU | Mutation | 0%–9% | 110, 111 | Desmoplastic subtype |
| Smo | Mutation | 0%–10% | 112, 113 | Desmoplastic subtype |
| Gli | Overexpression | ~30% | 16, 24, 28 | Desmoplastic subtype |
| BMI1 | Overexpression | ~67% | 10 | — |
| RENKCTD11 | Deletion | ~39% | 114 | — |
| Wnt signaling | ||||
| Axin 1 | Mutation | 1.2%–5.6% | 17, 115, 116 | — |
| Deletion | 12%–41.7% | 17, 115 | — | |
| Axin 2 | Mutation | ~3% | 117 | — |
| APC | Mutation | 1.3%–4.3% | 118, 119 | — |
| β-catenin | Mutation | 0.5%–63.8% | 15, 116, 118–121 | Favorable outcome |
| Survivin | Overexpression | 0.5%–50% | 18, 19, 122, 123 | Unfavorable outcome |
| SOX4 | Overexpression | Unknown | 21, 22, 124 | — |
| SOX11 | Overexpression | Unknown | 21, 22 | — |
| Cyclin D1 | Overexpression | Unknown | 23, 24 | — |
| Cyclin D2 | Overexpression | Unknown | 24, 124 | — |
| Lef1 | Overexpression | Unknown | 16, 24, 125 | — |
| Notch signaling | ||||
| HES1 | Overexpression | Up to 46% | 24, 25, 28 | Unfavorable outcome |
| HES5 | Overexpression | Up to 71% | 24, 28 | — |
| JAG1 | Overexpression | Unknown | 24 | — |
| Notch1 | Overexpression | ~75% | 27 | — |
| Notch2 | Overexpression | 12.5%–15% | 24, 25, 28 | — |
| Notch3 | Overexpression | Unknown | 24 | — |
| FOXG1 | Overexpression | >90% | 126 | — |
| Mushashi | Overexpression | Unknown | 124 | — |
| ErbB signaling | ||||
| ErbB4 | Overexpression | ~66% | 29, 31, 32, 126 | Unfavorable outcome |
| ErbB2 | Overexpression | 70%–86% | 126, 127 | Unfavorable outcome |
| CIC | Overexpression | Unknown | 128 | — |
| NRG-1β | Overexpression | ~87% | 29 | — |
| c-myc | Amplification | 5%–10% | 40, 129–133 | Anaplasia and |
| Overexpression | ~42% | unfavorable outcome | ||
| MnT | Underexpression | ~43% | 134, 135 | — |
| n-myc | Amplification | ~5% |
24, 39, 40, 130, 136 137, 138 |
Unfavorable outcome |
| JPO2 | Overexpression | Unknown | 139 | Metastases |
| BCAT1 | Overexpression | Unknown | 22 | Metastases |
| IGF signaling | ||||
| IGF-1R | Expression/phosphorylation | ~80% | 140 | — |
| IRS-1 | Overexpression | Unknown | 140 | — |
| IGF-2 | Overexpression | Unknown | 38, 45 | Desmoplastic subtype |
| AKT/PKB | Phosphorylation | Unknown | 140 | — |
| Erk-1 | Phosphorylation | Unknown | 140 | — |
| Erk-2 | Phosphorylation | Unknown | 140 | — |
| IGFBP-2 | Overexpression | Unknown | 48 | — |
| IGFBP-3 | Overexpression | Unknown | 48 | — |
| Other | ||||
| CXCR4 | Overexpression | ~51% | 16, 141 | Desmoplastic and extensive nodularity subtype |
| PDGFRB | Overexpression | Unknown | 142 | Metastatic medulloblastoma |
| OTX2 | Overexpression | >70% | 53, 54, 124, 143, 144 | Classic subtype and anaplastic features |
| Amplification | ~33% | — | ||
| ATOH1 | Expression | Unknown | 16 | Desmoplastic subtype |
| p75NTR | Expression | Unknown | 49, 145 | Desmoplastic subtype and unfavorable outcome? |
| TrkA | Overexpression | ~67% | 146 | Apoptotic index |
| TrkC | Overexpression | 29%–73% | 40, 146–150 | Favorable outcome |
| Heparanase | Expression | 62%–88% | 150, 151 | — |
| NEUROG1 | Expression | ~55% | 152, 153 | Nondesmoplastic metastatic medulloblastoma and unfavorable outcome |
| Calbindin | Expression | ~41% | 154 | Nondesmoplastic medulloblastoma and tumor recurrence |
| p53 | Mutation | 0%–11% | 155–157 | Unfavorable outcome |
| PAX5 | Overexpression | ~70% | 159 | — |
| MDM2 | Overexpression | 0%–20% | 155, 160 | Unfavorable outcome in adults |
| CDK6 | Overexpression | ~30% | 63 | Unfavorable outcome |
| HIC1 | Hypermethylation | ~70% | 161, 162 | Unfavorable outcome |
| EEF1D | Overexpression | Unknown | 163 | Unfavorable outcome |
| RPL30 | Overexpression | Unknown | 163 | Unfavorable outcome |
| RPS20 | Overexpression | Unknown | 163 | Unfavorable outcome |
| STMN1 | Overexpression | Unknown | 23, 164 | Unfavorable outcome |
| hTERT | Overexpression | ~42% | 165, 166 | Tumor progression |
| SGNE1/7B2 | Hypermethylation | ~70% | 38, 167 | Classic medulloblastoma |
| RASSF1A | Hypermethylation | 80%–90% | 72, 161 | — |
| CASP8 | Hypermethylation | ~90% | 74, 161, 168–171 | Classic and anaplastic subtype and unfavorable outcome |
| ZIC2 | Hypermethylation | Unknown | 75 | — |
| p14ARF | Hypermethylation | 4%–50% | 161 | — |
| p16INK4A | Hypermethylation | 2%–14% | 161, 168, 172, 173 | — |
| TIMP3 | Hypermethylation | 0%–11% | 161, 168, 172 | — |
| CDH1 | Hypermethylation | ~8% | 168 | — |
| p18INK4C | Hypermethylation | ~20% | 174 | — |
| S100A6 | Hypermethylation | ~12% | 175 | Large-cell anaplastic subtype |
| S100A10 | Hypermethylation | ~12% | 175 | — |
| S100A4 | Hypomethylation | ~17% | 175 | Metastatic medulloblastoma |
| MCJ | Hypermethylation | ~33% | 176 | |
| RB1 | Hypermethylation | ~18% | 177 | |
| DKK1 | Histone acetylation | Unknown | 178 | |
| EPENDyMOMA | ||||
| SHH signaling | ||||
| Gli1 | Overexpression | Unknown | 88 | — |
| Gli2 | Overexpression | Unknown | 88 | — |
| Cyclin D1 | Overexpression | Unknown | 83, 88 | Supratentorial ependymoma |
| Wnt signaling | ||||
| EB1 | Underexpression | Unknown | 87 | — |
| Notch signaling | ||||
| HES1 | Overexpression | Unknown | 88 | — |
| JAG1 | Overexpression | Unknown | 83 | Supratentorial ependymoma |
| JAG2 | Overexpression | Unknown | 83 | Supratentorial ependymoma |
| Notch1 | Overexpression | Unknown | 88 | — |
| Notch2 | Overexpression | Unknown | 88 | — |
| FZD1 | Overexpression | Unknown | 88 | — |
| HEY2 | Overexpression | Unknown | 88 | — |
| EPHB-EPHRIN signaling | ||||
| EPHRIN A3 | Overexpression | Unknown | 83 | Supratentorial ependymoma |
| EPHB3 | Overexpression | Unknown | 83 | Supratentorial ependymoma |
| EPHB2 | Overexpression | Unknown | 83 | Supratentorial ependymoma |
| ErbB signaling | ||||
| ErbB4 | Overexpression | >75% | 179 | Proliferation activity and unfavorable outcome |
| ErbB2 | Overexpression | >75% | 179 | Proliferation activity and unfavorable outcome |
| IGF signaling | ||||
| IGF-1R | Expression | 29%–80% | 180 | Anaplastic ependymoma? |
| IGF-2 | Overexpression | Unknown | 48, 181 | — |
| IGFBP-2 | Overexpression | Unknown | 48 | — |
| IGFBP-3 | Overexpression | Unknown | 48 | — |
| IGFBP-5 | Overexpression | Unknown | 48 | — |
| Other | ||||
| NF2 | Mutation | 10%–71% | 182–184 | Spinal ependymoma |
| Hypermethylation | 0%–7% | 185, 186 | — | |
| SCHIP1 | Underexpression | Unknown | 87 | — |
| MEN1 | Mutation | ~2% | 82, 187 | Recurrent ependymoma |
| SULT4A1 | Underexpression | Unknown | 88 | — |
| SOX9 | Overexpression | Unknown | 164 | Favorable outcome |
| Calcyphosine | Expression | ~59% | 164 | Epithelial differentiation |
| hTERT | Amplification | ~24% | 98, 188 | Proliferation activity and unfavorable outcome |
| CBX7 | Underexpression | ~55% | 87 | — |
| p53 | Mutation | 0%–6% | 185, 189–192 | — |
| MDM2 | Amplification | 4%–35% | 189, 193 | — |
| p73 | Overexpression | Unknown | 194, 195 | Grade II ependymoma |
| Hypermethylation | 5%–33% | 186, 196, 197 | — | |
| p14ARF | Deletion | 1%–7% | 83, 98 | Supratentorial ependymoma |
| Hypermethylation | 0%–28% | 196–198 | Adults | |
| p15INK4B | Hypermethylation | 0%–21% | 196, 198 | Adults |
| p16INK4A | Deletion | 1%–7% | 83, 98 | Supratentorial ependymoma |
| Hypermethylation | 0%–32% | 88, 186, 196, 197 | Adults | |
| RASSF1A | Hypermethylation | 56%–86% | 185, 198 | — |
| CASP8 | Hypermethylation | 4%–50% | 185, 186, 196 | Myxopapillary ependymoma |
| DAPK | Hypermethylation | 0%–57% | 88, 185, 186, 197 | — |
| MGMT | Hypermethylation | 0%–20% | 88, 185, 186, 196, 198 | — |
| FHIT | Hypermethylation | 22% | 185 | — |
| TFRSF10C | Hypermethylation | 9%–50% | 185 | — |
| TFRSF10D | Hypermethylation | 36% | 185 | — |
| BLU | Hypermethylation | 14% | 185 | — |
| RARB | Hypermethylation | 0%–15% | 88, 185 | — |
| THBS1 | Hypermethylation | 0%–30% | 186, 196 | — |
| TIMP3 | Hypermethylation | 0%–40% | 186, 196, 197 | — |
| RB1 | Hypermethylation | 0%–14% | 177, 185, 197 | — |
| MCJ | Hypermethylation | 10% | 175 | — |
| GSTP1 | Hypermethylation | 28% | 197 | — |
| HIC1 | Hypermethylation | 83% | 88, 199 | — |
Fig. 1.
Signaling pathways involved in the development of the brain and pathogenesis of medulloblastoma and ependymoma. Deregulation of these pathways is important in the pathogenesis of medulloblastoma and ependymoma. Interactions among these pathways are multiple and complex.
Sonic Hedgehog Signaling. Gorlin’s syndrome is an autosomal dominant disorder that is characterized by multiple developmental defects and a predisposition for basal cell carcinoma, rhabdomyosarcoma, and medulloblastoma.8 The tumor suppressor gene Patched 1 (PTCH1) on chromosome 9q22.3, encoding a trans-membrane surface receptor for hedgehog proteins, is mutated in this syndrome. The hedgehog–Patched signaling pathway controls normal development of the external granular layer of the cerebellum.9 SHH, produced by Purkinje cells, binds to the PTCH1 receptor and induces proliferation of cerebellar granule cell precursors by relieving the inhibition of Smo and inducing activation of the Gli family of transcription factors.9 Mutations in various components of the SHH pathway, such as PTCH1 and Smo, occur in approximately 30% of sporadic medulloblastomas, predominantly desmoplastic medulloblastomas (Table 2). These tumors show up-regulation of important SHH target genes, such as Gli1 and BMI1, indicating active SHH signaling. BMI1 is overexpressed in medulloblastomas, which might result in the abnormal regulation of both the Rb and p53 pathways.10 The importance of the SHH pathway in medulloblastoma is underlined by the observed growth inhibition after treatment with inhibitors of the SHH pathway.11 Because only a small subset of PTCH1 +/− mice develop medulloblastoma, other genetic events are thought to influence the susceptibility of developing medulloblastoma. For example, concomitant loss of p53 or Ink4C has been shown to facilitate the development of medulloblastoma.12
Wnt Signaling. The Wnt signaling pathway may also be involved in regulating the embryonal development of the brain. One of the genes involved in this pathway, adenomatous polyposis coli (APC), is mutated in patients with Turcot’s syndrome, who have a predisposition to develop colon cancers, glioblastomas, and medulloblastomas (Table 2). APC forms a protein complex together with β-catenin, glycogen synthase kinase 3-β (GSK3-β), and axin.13 Activation of the Wnt pathway results in decreased β-catenin degradation followed by the interaction with TCF/LEF transcription factors and activation of Wnt targets, such as c-Myc, cyclin D1, and AXIN2.14 Activating mutations in the Wnt path-way occur in a substantial number of medulloblastomas (Table 2).15,16 Most mutations have been found in the β-catenin gene, but mutations in the APC and AXIN2 genes and deletions of the AXIN1 gene have also been described (Table 2). However, deletions of AXIN1 were also identified in normal brain tissue, suggesting that at least some of the AXIN1 deletions found in medulloblastoma represent polymorphisms or PCR artifacts.17 Another marker associated with activation of the Wnt signaling pathway is increased expression of survivin, an apoptosis inhibitor (Table 2). Survivin expression is related to an unfavorable outcome, independent of clinical staging or tumor histology.18,19 SOX gene family members can also regulate the Wnt signaling pathway.20 Interestingly, SOX4 and SOX11 are overexpressed in predominantly classic medulloblastoma.21–23
The SHH and Wnt signaling pathways interact with each other, but also with other signaling pathways, including Notch, ErbB, and insulin-like growth factor (IGF) (Fig. 1). For example, cyclin D1, an important mediator of the proliferation of cerebellar granule cell precursors, is an important downstream target of SHH, Wnt, and Notch signaling. Moreover, medulloblastomas of PTCH1 +/− mice show increased expression of genes involved in activation of both SHH and Wnt signaling.24
Notch Signaling. In the cerebellum, Notch2 is predominantly expressed in proliferating cerebellar granule cell precursors, whereas Notch1 is found in differentiated internal granule layer neurons.25 Notch2 is over-expressed in a subset of medulloblastomas, whereas Notch1 expression is scarce. Activation of the Notch signaling pathway results in the transcriptional activation of helix-loop-helix transcription factors HES1 and HES5.26 HES1 expression is associated with decreased survival rates of medulloblastoma patients (Table 2). It has been recently hypothesized that HES1 forms transcriptional repressor complexes with FOXG1 to negatively regulate the differentiation of neural progenitor cells.27 Interestingly, the function of the FOXG1 gene is deregulated in most medulloblastomas (Table 2). Treatment of medulloblastoma xenografts with inhibitors of the Notch signaling pathway results in decreased proliferation and increased apoptosis.28
ErbB Signaling. ErbB belongs to the receptor tyrosine kinase family I, which consists of four receptor tyrosine kinases (ErbB1–ErbB4) and a variety of ligands, including several neuregulins that are important in regulating the development of neuronal tissue.29 ErbB4, especially the CYT1 isoform, is overexpressed in tumors with low Gli1 levels, which suggests that ErbB signaling is regulated by SHH signaling.30 CYT1 is the only isoform of ErbB4 that is able to activate antiapoptotic phosphatidyl inositol 3-kinase (PI3K)/protein kinase B (PKB)/AKT signaling,31 which is important in medulloblastoma development. Overexpression of the CYT1 ErbB4 isoform correlates with the anaplastic medulloblastoma subtype and ErbB2 expression levels. Because the ErbB2 gene is located on chromosome 17q11.2–q12, a region that is frequently gained in medulloblastomas, ErbB2 is regarded as a potential medulloblastoma oncogene. ErbB2 expression, especially in combination with high ErbB4 expression, has poor prognostic impact in medulloblastoma and is associated with the presence of metastases and a high mitotic index.29,32 Overexpression of ErbB2 increases the migration of medulloblastoma cells in vitro, and prometastatic genes involved in, for example, cell adhesion and invasion are up-regulated by ErbB2.33 Approximately one-third of the medulloblastomas coexpressing ErbB2 and ErbB4 also express the ErbB ligand NRG1-β, suggesting an autocrine loop resulting in disease progression. Interestingly, one of the targets of NRG1-β is c-myc.34
c-myc Signaling. c-Myc belongs to the myc transcription factor family, which is important in cell cycle regulation, proliferation, and differentiation and is involved in many human malignancies.35 c-Myc over-expression in medulloblastoma is associated with the large-cell/anaplastic subtype and poor survival (Table 2). c-myc activation can be caused by activation of the SHH and Wnt pathways,36 translocations, activating mutations, viral insertion, and genomic amplification. In mouse models, c-Myc alone is not sufficient to induce medulloblastomas, but it is suggested that c-Myc cooperates with SHH in the pathogenesis of medulloblastoma.37 The c-Myc binding protein JPO2 can potentiate c-Myc transforming activity and is associated with metastatic medulloblastoma (Table 2). We observed up-regulation of mRNA levels of BCAT1, a myc target, in metastatic medulloblastoma and also detected the BCAT1 protein in the cerebrospinal fluid of medulloblastoma patients.22 Another member of the myc family, n-myc, is amplified in approximately 5% of medulloblastomas and is an important and direct target of the SHH signaling pathway promoting cell cycle progression in the developing cerebellum (Table 2). In concordance, n-myc up-regulation is observed in medulloblastoma associated with activated SHH signaling.38,39 n-myc amplification correlates with unfavorable survival, but this correlation is less clear than for c-myc.40 Prevention of n-Myc degradation by PI3K41 may provide an explanation for the enhancing effect of IGF/PI3K signaling pathway on the SHH-related development of medulloblastoma.39
IGF/PI3K Signaling. The IGF system also plays an important role in neuronal development and is involved in the development of brain tumors.42 Most medulloblastomas overexpress the IGF-1 receptor (IGF-1R) protein, and more than half of medulloblastomas express the activated phosphorylated form of IGF-1R (Table 2). Moreover, activated forms of downstream signaling molecules of IGF-1R, such as insulin receptor substrate-1 (IRS-1), PI3K, AKT/PKB, Erk-1, and Erk-2, are detected in most medulloblastomas. Inhibition of IGF-1R signaling reduces medulloblastoma tumor growth.43 This inhibition is augmented by constitutive GSK3-β phosphorylation,44 suggesting that the combined inhibition of the IGF-1R and dephosphorylation of GSK3-β might be an effective treatment for medulloblastoma. The IGF-1R ligands IGF-1 and IGF-2 are important mitogens in cerebellar granule precursors and medulloblastoma.45,46 Patti et al.46 showed the presence of an autocrine loop causing IGF-1R activation and leading to proliferation in a medulloblastoma cell line. IGF-2 is a downstream target of SHH signaling,47 and in concordance, IGF-2 overexpression is predominantly observed in desmoplastic medulloblastomas. The IGF-binding proteins (IGFBPs) modulate IGF action and are differentially expressed in brain tumors. We have observed increased IGFBP-2 and IGFBP-3 mRNA expression levels in medulloblastoma, which is accompanied by increased IGFBP-3 levels and IGFBP-3 proteolysis in the cerebrospinal fluid of brain tumor patients.48 The IGF-1R signaling pathway may result in activation of AKT and PI3K, and also ras/MAPK (mitogen-activated protein kinase) signaling. Downstream targets of the ras/MAPK pathway and platelet-derived growth factor receptor B (PDGFRB) are up-regulated in metastatic medulloblastoma (Table 2).
Cells of Origin
Lateral Cerebellar Hemispheres
Activation of different signaling pathways in different medulloblastoma subtypes suggests that medulloblastomas have different origins. Potential cells of origin are the stem and/or progenitor cells in the external granular layer that have persisted after the first years of life and the pluripotent stem cells of the ventricular subependymal matrix, which are capable of differentiating into neuronal or glial cells. Several findings support this hypothesis of double origin. Desmoplastic medulloblastomas are usually found in the cerebellar hemispheres and are thought to arise from neural precursor cells in the external granule layer.49 In concordance, they are characterized by activated SHH signaling and IGF-2 overexpression, which affects the proliferation of cerebellar granule precursors. CXCR4, ATOH1, and the p75 neurotrophin receptor (p75NTR) are markers of the stem and/or progenitor cells in the external granular layer and are predominantly found in desmoplastic medulloblastomas (Table 2). CXCR4 is important for migration and cell cycle control of granular precursors and is a target of SHH. Aberrant activation of the CXCR4 receptor might contribute to an increased malignant potential, but mutations in CXCR4 are only rarely observed in medulloblastoma. ATOH1 is a basic helix-loop-helix transcription factor that influences the development of granular cerebellar precursors via the Notch pathway.50 p75NTR belongs to the family of neurotrophins and neurotrophin receptors, which are important in the normal development of the cerebellum.51 Expression of p75NTR is suggested to be a marker of tumor progression (Table 2). Another neurotrophin receptor, TrkC, is one of the first biological markers in medulloblastoma and is a strong predictor of favorable outcome (Table 2), probably because binding of the TrkC ligand to the receptor induces apoptosis.51
Cerebellar Vermis. In contrast to desmoplastic medulloblastomas arising in the lateral cerebellar hemispheres, medulloblastoma subtypes arising in the cerebellar vermis are suggested to originate from cells in the ventricular matrix and Purkinje neurons. Calbindin and NeuroG1 expression are specific for stem and/or progenitor cells in the cerebellar ventricular zone. Calbindin is expressed in most classic medulloblastomas, and its expression may be a marker for recurrence in medulloblastoma (Table 2). NeuroG1 (NeuroD3) belongs to the NeuroD family of basic helix-loop-helix transcription factors, regulating the transcription of genes involved in neuronal differentiation.52 NeuroG1 expression is correlated with the overexpression of myc and is indicative of a poor prognosis in medulloblastoma (Table 2).
OTX2 (head development gene) overexpression, observed in more than two-thirds of medulloblastomas, is also characteristic for the classic medulloblastomas arising in the cerebellar vermis (Table 2). However, because cells of the fetal external granular cerebellar layer are also shown to express OTX2, a subset of classic medulloblastomas negative for calbindin may also arise from the external granular layer.53 OTX2 expression is correlated to the presence of proliferating, poorly differentiated cells with anaplastic features, but no correlation with outcome has been observed. Amplification of OTX2 occurs in up to one-third of primary medulloblastomas, but mutations have not been identified. OTX2 knockdown, either by small interfering RNAs or by treatment with all-trans-retinoic acid, induced apoptosis in vitro, which suggests that OTX2 might be an interesting therapeutic target.54
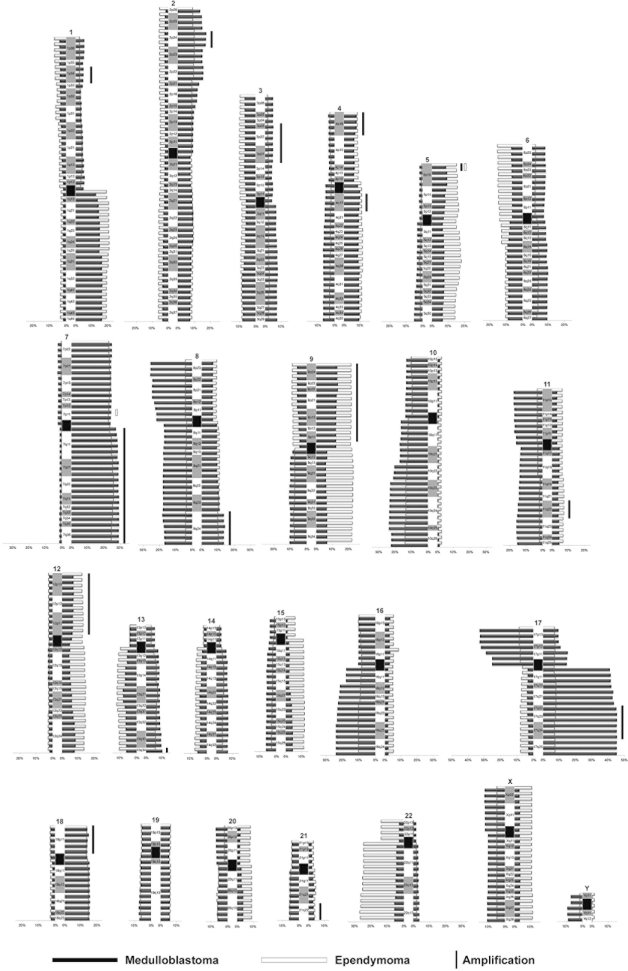
Cytogenetics
Much knowledge about cytogenetic abnormalities of brain tumors has been obtained by conventional cytogenetic, loss of heterozygosity (LOH), and molecular genetic analyses, for example, comparative genomic hybridization (CGH). Karyotyping reveals that balanced translocations are relatively infrequent in medulloblastomas (Table 3) compared with chromosomal gains and losses. No recurrent translocations have thus far been identified in medulloblastoma. Fig. 2 summarizes the chromosomal gains and losses in medulloblastomas identified by CGH. Conventional CGH can detect regions of copy number change, and the recent development of array-based CGH has resulted in higher-resolution analyses allowing more precise definition of which regions are involved. In addition, correlation of these data with gene expression levels may identify genes that are potentially important driver genes in these copy abnormalities.
Table 3.
Balanced chromosomal translocations identified in medulloblastomas and ependymomas.
| Medulloblastoma | Reference | Ependymoma | Reference |
|---|---|---|---|
| t(1;3)(p13;p13) | 200 | t(1;2)(p33;q21) | 201 |
| t(1;3)(q32;q27) | 202 | t(1;2)(q21;q35) | 203 |
| t(1;4)(q31;q35) | 204 | t(1;3)(p34;q21) | 203 |
| t(1;6)(p21;q11–13) | 205 | t(1;7)(q25;q35) | 206 |
| t(1;8)(q1?;q2?) | 207 | t(1;8) | 201 |
| t(1;8)(q25;q22) | 208 | t(1;9)(p36;q13) | 209 |
| t(1;11)(q32;p15) | 210 | t(1;14)(q?;p?) | 210 |
| t(1;14)(p22;q31) | 211 | t(1;20)(q21;q13) | 201 |
| t(1;15)(p36;q11) | 210 | t(1;22)(q11;q13) | 212 |
| t(2;12)(q21;q23) | 210 | t(2;4)(q34;q35) | 213 |
| t(2;15)(q37;q15) | 214 | t(2;10)(p25;q12) | 213 |
| t(3;6)(p21;q12) | 214 | t(2;17)(p11;p11) | 201 |
| t(3;9)(q27;q22) | 210 | t(2;22)(p12;q13) | 211 |
| t(3;12)(p21;q13) | 210 | t(2;22)(p13;q13) | 215 |
| t(3;17)(p13;p13) | 210 | ?t(3;3)(q29;q25) | 216 |
| t(5;6)(q13;q21) | 214 | t(3;4)(q?;q?) | 210 |
| t(5;8;10)(q34;q24;q24) | 210 | t(3;6)(q11;q11) | 215 |
| t(6;13)(q25;q14) | 202 | t(3;11)(q29;q25) | 217 |
| t(6;14)(q27;q11) | 202 | t(3;15)(q?;q?) | 210 |
| t(6;19)(q21;q13) | 204 | t(4;22)(p16;p13) | 217 |
| t(7;13)(q11;q34) | 208 | t(6;11)(p?;q?) | 210 |
| t(7;19)(p11;p11) | 210 | t(6;11)(q27;q25) | 217 |
| t(9;11)(q34;q13) | 200 | t(6;16) | 219 |
| t(9;19)(q22;q13) | 201 | t(9;11)(q34;q25) | 217 |
| t(10;16) | 207 | t(9;16)(q?;q?? | 210 |
| t(11;13)(p13;q14) | 202 | t(9;17)(q34;q25) | 217 |
| t(11;13)(q15;q11) | 204 | t(10;11;15)(p12;q13;p12) | 220 |
| t(12;13)(p13;p11) | 201 | t(11;12)(q13;q24) | 187 |
| t(12;21) | 218 | t(11;17)(q13;q21) | 218 |
| t(13;14)(q11;p11) | 201 | t(11;17)(q25;q25) | 217 |
| t(13;15)(q32;q22) | 210 | t(11;18)(q13;q21) | 201 |
| t(?15;16)(q13;p13) | 138 | t(11;19)(q25;q13) | 217 |
| t(16;17)(q?;q?) | 221 | t(12;18)(p11;q11) | 201 |
| t(16;20)(q13–22;q13) | 55 | ||
| t(17;17)(p?;p?) | 218 | ||
| t(17;18)(p11;q11) | 202 | ||
| t(18;22)(q23;q11) | 202 | ||
| t(18;20)(q23;p13) | 222 | ||
| t(X;15)(p22;q25) | 210 | ||
| t(X;18)(p11;q11) | 201 | ||
| t(X;22)(p22;q11) | 223 |
Source: Mitelman Database of Chromosome Aberrations in Cancer (http://cgap.nci.nih.gov/Chromosomes/Mitelman).
Fig. 2.
Copy number aberrations and amplifications in medulloblastomas (n = 455)56,65,67,68,70,136,163,165,202,224–236 and ependymomas (n = 354)97,99,100,113,237–245 by CGH. Some studies provided only a summary of data62–64,88,98 or did not distinguish between medulloblastomas and primitive neuroectodermal tumors,246 and we excluded those results here. The numbers at the tops of the graphs indicated chromosome number.
Chromosome 17. The most commonly reported cytogenetic change in medulloblastoma is loss of 17p in up to approximately 50% of medulloblastomas, often associated with a gain of 17q leading to the formation of an isochromosome 17q [i(17q)].55 Because i(17q) can be found as a single structural abnormality, it may be a primary event in medulloblastoma development. In some studies, loss of 17p was associated with a poor prognosis, while others failed to find this association.56,57 The incidence of i(17q) is low in desmoplastic medulloblastoma compared with classic and large-cell anaplastic medulloblastoma. Despite the identification of several common chromosomal breakpoint regions at 17p11.2, 17p11.2–17q11.2, and 17q21.31 and various commonly deleted regions on 17p, for example, 17p13.1 and 17p13.3,58,59 the affected tumor suppressor gene involved in the pathogenesis of medulloblastoma has not been identified thus far.
p53, one of the most important tumor suppressor genes, was initially suggested to be of importance in medulloblastoma, because it is localized on chromosome 17p13. However, despite the facts that (1) patients with germline p53 mutations have a predisposition to develop medulloblastomas (Table 1), (2) loss of p53 facilitates medulloblastoma development in mouse models,12 and (3) up to 40% of medulloblastomas show p53 protein expression indicating a dysfunctional p53 protein, we and others have shown that the incidence of p53 mutations in sporadic medulloblastoma is low (Table 2). Overexpression of the p53 binding protein MDM2, known to cause inactivation of p53, is also very rare in medulloblastomas (Table 2). p53 inhibition by PAX5 (early development gene) is suggested to play a role in medulloblastomas as the expression of PAX5 is deregulated in approximately 70% of cases (Table 2).
Besides p53, several other candidate tumor suppressor genes on 17p have been suggested. Interestingly, 17p carries several genes suggested to be involved in the regulation of SHH signaling. HIC1, located on 17p13.3, is aberrantly methylated in medulloblastoma, and the subsequent transcriptional silencing is associated with poor outcome (Table 2). Recently, loss of HIC1 together with loss of PTCH1 was found to result in a higher incidence of medulloblastomas.60 This is probably related to the cooperation of HIC1 and PTCH1 in the silencing of ATOH1 expression, which is required for medulloblastoma growth. RENKCTD11, a putative tumor suppressor gene located on chromosome 17p13.2, is deleted in 39% of medulloblastomas (Table 2). RENKCTD11 inhibits medulloblastoma cell proliferation by antagonizing the activation of SHH target genes. Deletion of this gene might thus result in enhanced SHH signaling and increased proliferation of granule cell precursors. The myc inhibitor MnT, mapped to 17p13.3, is also deleted or underexpressed in medulloblastoma. Because c-myc and n-myc are both targets of SHH signaling, loss of the Mnt gene on 17p might again link this chromosomal abnormality to SHH signaling.
Gain of 17q can also occur in the absence of a 17p deletion, suggesting that duplication of genes on 17q influence medulloblastoma development. An amplicon on 17q23.2 contains the APPBP2 and PPM1D genes.59 PPM1D overexpression can, for example, inhibit p53 tumor suppressor activity.61 Because the regions of loss of 17p and gain of 17q are large, the gene dosage effect of genes on 17p and 17q, rather than one tumor suppressor gene, may be tumorigenic in medulloblastoma.59
Chromosome 7. A cytogenetic abnormality that is often seen in combination with a gain of 17q is gain of chromosome 7. As for chromosome 17, the gene of interest is not yet identified. Hui et al.62 found an amplification core at 7q34–q35 containing several oncogenes. A novel amplicon at 7q21.2 contained only the CDK6 gene. Cyclin-dependent kinase 6 (CDK6) can phosphorylate retinoblastoma 1 (RB1), which is an important regulator of proliferation and differentiation. CDK6 is overexpressed and indicates poor prognosis in medulloblastomas (Table 2).
Other Copy Number Abnormalities
Other recurrent abnormalities in medulloblastomas are losses on 6q, 8p, 9q, 10q, 11, 16q, 20, X, and Y and gains on 1q, 2p, 4q, 6q, 9p, 13q, 14q, and 18 (Fig. 2). Several regions with consistent copy number gain have been identified on 1q, for example, 1q21.3–23.1,62 1q32.1,62,63 and 1q32.3–qter.63,64 HLX1 is suggested to be involved in the gain on 1q, because its expression was markedly increased in medulloblastomas.65 Concerning losses on 6q, a small region of deletion is identified at 6q23.1.62 The commonly deleted region on 8p is localized between 8p21.3 and 8p23.2, adjacent to the tumor suppressor gene DLC1.64,66 The minimal region of overlap of losses on chromosome 16q is at the distal end of 16q, at 16q22.2–qter.67 Regarding losses of chromosome 10, several minimal regions of overlap are observed, one involving the 10q23 region containing the PTEN gene, another involving a hemizygous deletion in 10q25.1, and a third involving the 10q26.3 region.67–69 The SUFU gene, described as being mutated in a small subset of medulloblastomas, maps to 10q24.3 and is therefore suggested to have a role as tumor suppressor gene (Table 2). Loss of 11p is identified in 10%–20% of medulloblastomas (Fig. 2). However, LOH analyses show allelic loss of 11p in >50% of tumors.69 Minimal overlapping regions of loss on chromosome 11 are 11pter–11p11.2 and 11q13.2–11qter. The region of gain on 14q is mapped to 14q12 and contains the FOXG1 gene, which is aberrantly expressed in most medulloblastomas (described above; see “Notch Signaling”). Loss of chromosome 20 frequently involves the whole chromosome. However, recently the commonly deleted region on chromosome 20 is identified at 20q13.2–q13.3,62,64 but no target genes have been identified yet.
Amplifications
Gene amplifications are relatively rare in medulloblastomas. The identified amplification sites are displayed in Fig. 2. Several potential oncogenes are involved in these amplifications. MYCL1 is an important candidate gene in the amplification region on chromosome 1p34.64 The c-myc and n-myc genes on chromosomes 8q24 and 2p24, respectively, are amplified in a small proportion of tumors, mainly large-cell anaplastic medulloblastoma (Table 2). However, gain of 8q, including the three ribosomal genes EEF1D, RPL30, and RPS20, is also predictive of poor outcome independent of myc (Table 2). The amplicon on 5p15 involves the hTERT gene, known to be amplified and overexpressed in medulloblastoma (Table 2). hTERT is able to compensate for progressive telomere shortening, leading to immortalization. Amplification of hTERT is associated with tumor progression in medulloblastoma. Further analysis of the 9p amplification suggested the importance of the 9p23–p24 region, including the JMJD2C gene. The 11q22.3 region maps the cyclin D1 locus, which is amplified in a variety of tumors. A possible candidate gene for the 13q34 amplification is IRS-2,70 which is amplified and overexpressed in a small subset of glioblastomas.
Epigenetics
Recently, epigenetic changes have also been shown to be important in tumorigenesis. Both histone modifications (acetylation, methylation, and phosphorylation) and hypermethylation of CpG motifs in promoter regions may induce transcriptional silencing of tumor suppressor genes.71 Several putative tumor suppressor genes are aberrantly methylated in subgroups of medulloblastoma (Table 2). RASSF1A (RAS association domain gene) regulates cyclin D1 expression, which is important in controlling the cell cycle. In contrast to other malignancies, hypermethylation of RASSF1A in medulloblastoma is not accompanied by allelic loss of 3p21.3 or mutation, indicating that biallelic loss is the primary mechanism of inactivation of RASSF1A.72 CASP8 is a cysteine protease involved in death-receptor-mediated apoptosis.73 We and others have shown that promoter hypermethylation of CASP8 leading to loss of CASP8 mRNA expression induces resistance to apoptosis induced by tumor necrosis factor–related apoptosis-inducing ligand (TRAIL) in embryonal tumors of childhood, such as medulloblastoma and neuroblastoma.74 In primary tumors, aberrant promoter methylation of CASP8 was seen most frequently in classic and anaplastic medulloblastoma and is an independent unfavorable prognostic factor. Transcriptional silencing of SGNE1/7B2, a gene located on 15q11–15, occurs predominantly in classic medulloblastoma. SGNE1 is a calcium-dependent serine protease that inhibits tumor cell proliferation. ZIC2 is a zinc-finger transcription factor essential for the developing CNS, and its expression is down-regulated in medulloblastomas.75 p18INK4C is a CDK inhibitor, and loss of expression of this gene can induce medulloblastoma in mouse models in collaboration with loss of PTCH1 or p53.76 Three members of the S100 gene family are found to be aberrantly methylated in 10%–20% of medulloblastomas (Table 2). Hypermethylation and silencing of S100A6 is associated with the large-cell anaplastic subtype of medulloblastoma. In contrast, S100A4 is hypomethylated, which results in increased expression. The prometastatic gene S100A4 is a direct target of ErbB2 signaling, associated with a poor prognosis in medulloblastoma. MCJ, a member of the DNAJ protein family that influences chemotherapy resistance, can be inactivated by biallelic hypermethylation, but hypermethylation of one allele also occurs in combination with genetic loss of the second allele (Table 2). Dickkopf-1 (DKK1) is epigenetically silenced in medulloblastoma by histone acetylation in the promoter region (Table 2). DKK1, a Wnt signaling antagonist, is an important suppressor of cell growth and inducer of apoptosis.
Proteomics
Despite enormous progress in applications and sensitivity, proteomic techniques are not frequently used to screen for aberrantly expressed proteins in brain tumors. The proteome of two representative medulloblastoma cell lines, DAOY and D283MED, has been studied by two-dimensional gel electrophoresis with subsequent matrix-assisted laser desorption/ionization identification.77 Several proteins described previously in other malignancies, such as SIP or HSP27 and other new candidate tumor-related proteins, were identified. We studied protein expression profiles of primary medulloblastomas using two-dimensional difference gel electrophoresis followed by mass spectrometry and found STMN1 to be overexpressed in medulloblastoma (Table 2).
Ependymoma
Clinical Aspects
Ependymomas, predominantly occurring in the posterior fossa in childhood, may also arise supratentorially and account for approximately 10% of all intracranial tumors in childhood and a higher proportion, up to 30% in some series, in children younger than 3 years.78 A variety of different subtypes of ependymomas have been identified, and the anaplastic variant seems to carry a worse prognosis.78,79 Surgery remains a major component of the management of ependymomas, and patients with posterior fossa ependymomas who have tumors amenable to gross total resections and are subsequently treated with radiotherapy have a 70% or greater likelihood of long-term disease control and possible cure.
Recent studies have focused on the utility of chemotherapy followed by second-look surgery prior to radio-therapy in those patients whose tumors are not totally, or near-totally, resected.80 Increasing evidence suggests that ependymomas are chemosensitive, but in older children chemotherapy has been primarily reserved for those patients with subtotally resected tumors or with anaplastic lesions. Conformal radiation therapy techniques are primarily used in children with ependymomas, and radiotherapy has now been used in cooperative group studies in children as young as 1 year. In very young children, especially those younger than 1 year, treatment with chemotherapy is often used in attempts to delay and, in select cases, obviate the need for radiotherapy, but high-dose chemotherapeutic regimens supported by autologous peripheral stem cell rescue have not been effective.80 The incidence of leptomeningeal dissemination at the time of diagnosis has varied significantly among series, but in general, less than 10% of children will have disseminated disease at the time of diagnosis, and craniospinal radiotherapy is reserved for those with documented disseminated disease. Increasing evidence suggests that supratentorial ependymomas differ biologically from those arising in the posterior fossa. Although standard treatment of partially resected supratentorial ependymomas is the same as for partially resected posterior fossa tumors, studies are evaluating the efficacy of surgery alone for totally resected supratentorial tumors.
Genetic and Biological Aspects
Developmental Signaling Pathways
Unfortunately, biological characteristics of ependymomas are largely unknown. This is mainly because ependymoma is a heterogeneous disease and can be subdivided into a wide range of subgroups based on histology and localization, which results in relatively small series of patients.
NF2. As in medulloblastomas, genetic syndromes associated with a predisposition to develop ependymomas, such as neurofibromatosis type 2 (NF2) (Table 1), were initially thought to provide clues about the genetic abnormalities involved in the pathogenesis of ependymomas. The NF2 gene is located on 22q12, and because allelic loss of chromosome 22 is frequently observed in ependymomas, NF2 was suggested to be a tumor suppressor gene involved in the development of ependymomas. However, mutations of the NF2 gene are rarely observed in sporadic ependymomas, except for the spinal ependymomas (Table 2). Inactivation of NF2 by hypermethylation is also rare (Table 2). Interestingly, although NF2 does not play an important role in sporadic nonspinal ependymomas, the expression of SCHIP-1, an NF2-interacting gene, is significantly down-regulated in pediatric ependymomas (Table 2).
MEN1. Other hereditary forms of ependymoma are uncommon. Ependymomas have been described in patients with MEN1 syndrome, which is characterized by the development of multiple endocrine tumors.81 The MEN1 gene is located on chromosome 11q13, a region that is involved in allelic losses and rearrangements in ependymomas.82 However, mutations in the MEN1 gene are described in only a small number of recurrent ependymomas (Table 2).
An important recent finding is that gene expression signatures of ependymomas from different locations of the CNS correlate with those of the corresponding region of the normal developing CNS.83 The differentially expressed genes are predominantly involved in the regulation of neural precursor cell proliferation and differentiation. In addition, ependymomas contain rare populations of cancer stem cells resembling radial glial cells, which are sufficient to give rise to tumor development in mice.83 Therefore, these radial glial cells in different parts of the CNS may be predisposed to acquire distinct genetic abnormalities that transform them into cancer stem cells of supratentorial, infratentorial, and spinal ependymomas. These data imply that signaling pathways involved in the development of the brain and neural stem cells, such as Notch, Wnt, SHH, and p53, are important in the pathogenesis of ependymomas (Fig. 1).
EPHB-EPHRIN and Notch Signaling. Active EPHB-EPHRIN (intercellular tyrosine kinase signalling) and Notch signaling is indeed observed in ependymomas, especially in those located in the supratentorial region (Table 2). Both signaling pathways are important for the maintenance of neural stem cells in the cerebral subventricular zone.84,85 The overexpression of the Notch target ErbB2 in most ependymomas and its correlation with proliferation and poor outcome also point to the importance of Notch signaling in ependymomas.
Wnt Signaling. Ependymomas have been described in patients with APC mutations associated with Turcot’s syndrome.86 However, in contrast to medulloblastomas, mutations in APC and β-catenin are not found in sporadic ependymomas (Table 2). Despite the absence of these mutations, gene expression profiling identifies aberrantly expressed genes involved in the Wnt signaling pathway, suggesting alternative mechanisms for disruption of this pathway.87
SHH Signaling. Involvement of SHH signaling in ependymomas is suggested by the overexpression GLI2, GLI-Kruppel family member (Gli), and serine threonine kinase 36 (STK36) and underexpression of PRKAR1B.88 In addition, overexpression of the SHH target IGF-2 is frequently observed in these tumors (Table 2). Besides the overexpression of IGF-2, we have found overexpression of IGFBP-2, -3, and -5 in ependymomas, also suggesting the involvement of the IGF system in the pathogenesis of ependymomas.48
p53 Signaling. Only one patient with a germline p53 mutation has been reported with an ependymoma.89 Despite the fact that p53 immunostaining is suggested to be associated with an unfavorable prognosis,90 p53 mutations are extremely rare in sporadic ependymomas (Table 2). Other methods of p53 inactivation have been observed in subgroups of ependymomas but are also relatively uncommon. Some report a high incidence of mdm2 expression and amplification in ependymomas, whereas others conclude that mdm2 plays a role in only a very small number of patients (Table 2). p73, a gene that shares structural and functional homologies with p53 and is able to induce mdm2, is overexpressed in grade II ependymoma (Table 2). Inhibition of p53 expression by PAX5 is not of importance in ependymomas. The negative regulation of p53 by p14ARF is recently suggested to be of importance in subgroups of ependymomas. p14ARF is located on chromosome 9p21 together with two other tumor suppressor genes, p15INK4B and p16INK4A, which are all cell cycle regulators.91 Expression of these genes is decreased by homozygous deletion, promoter hypermethylation, or point mutations in several malignancies. In ependymomas, decreased levels of p14ARF protein correlate with increased tumor grade and p53 protein accumulation.92 Deletion of the p16INK4A/p14ARF locus has recently been associated with supratentorial ependymomas (Table 2). The observed frequency of inactivation by hypermethylation of the three tumor suppressor genes in ependymomas is variable (Table 2) and is observed more frequently in adults than in children.
Gene Expression and Clinical Characteristics
Although recent gene expression profiling studies from our and other laboratories have correlated sets of genes to patient characteristics, tumor location, and tumor grade, the significance of these genes in the pathogenesis of ependymomas still needs to be determined. Genes that are overexpressed in ependymomas compared with normal control tissue include GLU, RAF1, SOX9, calcyphosine, annexin A1, and YAP1. We have shown that SOX9 expression was associated with a favorable outcome in pediatric ependymomas (Table 2). Several genes are characteristic for tumor location. Intracranial ependymomas are characterized by the overexpression of EMX2, MSI2, ABCG1, FLT1, TOP2A, CRIM1, CAMK2D, TFPI2, EBI2, ACTR3, NRCAM, PAX3, NET1, and MSX1, in which the first three were specifically up-regulated in supratentorial ependymomas and the last three in infratentorial ependymomas. ADAM9, TFAM, EDN1, and GAS2L1 were down-regulated in intracranial ependymomas. HOX genes might play a role in the maintenance of the cancer stem-cell phenotype in spinal ependymomas, because HOX family members, such as HOXB5 and HOXA9, are predominantly overexpressed in spinal ependymomas.83
Underexpression of proapoptotic nuclear factor-κβ2 (NF-κβ2) and pleckstrin and the overexpression of a PTEN homologue are associated with tumor recurrence.93 Several genes, such as NRCAM, COL4A2, CDK4, and survivin, are overexpressed in ependymomas with high proliferation indices.94,95 Tumor proliferation, reflected by Ki-67 positivity, is an important factor in the discrimination between low- and high-grade ependymoma and is a more reliable unfavorable prognostic factor than is histological grading.96
Cytogenetics
As is described for medulloblastomas, advanced cytogenetic techniques now allow more precise determination of chromosomal breakpoint regions and the identification of the genes involved. Table 2 and Fig. 2 provide the identified balanced translocations and a summary of observed copy number aberrations in ependymomas, respectively.
Recurrent Copy Number Abnormalities
Frequently observed copy number abnormalities in ependymomas are losses of 6, 9p, 10, 11, 13, 17, and 22 and gains of 1q, 5, 7, 9, and 12. Gain of 1q, for example, occurs more frequently in children than in adults, correlating with an intracranial tumor localization and grade III ependymomas.97,98 More specified regions on chromosomes 1q, 1q21.1–32.1, and 1q25 are associated with unfavorable outcome.98,99 As in medulloblastoma, the 5p15.3 region, containing the hTERT gene, is frequently gained in ependymomas, and high hTERT expression is associated with proliferation and unfavorable outcome (Table 2). Loss of 6q is associated with intracranial, predominantly infratentorial, tumors.100 Gain of chromosome 7 is predominantly found in spinal cord tumors,97,100 and gain or high-level amplification of epidermal growth factor receptor (EGFR) at 7p11.2 also predicts prognosis in intracranial tumors.98 Another region of gain on 7p21 contains the candidate proto-oncogenes TWIST1 and HDAC9,88 and a small region on 7q34 contains the ARHGEF5 gene.98 Gain of chromosome 12q and loss of chromosome 13 are predominantly observed in intracranial ependymomas.97,98 HOXC4 and CDK4 on 12q13 are mentioned as genes important in the 12q gain.98,100 Loss of 17p13.3 is associated with intracranial infratentorial ependymomas.88 HIC1 on 17p13.3 is suggested as the potentially involved oncogene. In addition to chromosomal loss, HIC1 hypermethylation and consequent transcriptional repression are observed in a substantial percentage of ependymomas (Table 2), suggesting an important role in ependymoma development.
Chromosome 22
Monosomy 22 is found more frequently in adults than in children, which results from the higher incidence of spinal tumors in adults than in children. The existence of ependymomas with loss of 22q lacking NF2 mutations suggests that other tumor suppressor genes are located on this chromosome. Multiple regions have been suggested, such as 22pter–22q11.2101,102 distal to the hSNF5/INI1 locus or 22q13.3, including the SULT4A1 gene (Table 2). Mutations in hSNF5/INI1 are rare or absent in ependymomas.103 Gene expression profiling of ependymomas has revealed several under-expressed genes on 22q12.3–q13.3, for example, FBX, c22orf2, CBX7, and SBF1.87 Interestingly, CBX7 is involved in gene silencing of, for example, the p16INK4A/p14ARF locus (Table 2).
Epigenetics
Epigenetic studies have also identified genes potentially important in ependymoma pathogenesis (Table 2). Independent of clinical and histological subtype, RASSF1A is transcriptionally silenced by methylation in most ependymomas, suggesting a function as a tumor suppressor gene. The fact that methylation is almost 100% at every CpG site suggests that RASSF1A inactivation is an early event in tumorigenesis. CASP8, TFRSF10C, and TFRSF10D are genes involved in the TRAIL apoptosis pathway, and methylation of CASP8 is suggested to be characteristic of low-grade myxopapillary ependymomas. MGMT is involved in DNA repair, and silencing of the gene is associated with increased sensitivity to alkylating agents in gliomas.104
Conclusion and Future Directions
Much progress has been made in the identification of biological factors involved in the pathogenesis of pediatric medulloblastomas and ependymomas in the past years, but much has yet to be discovered. Deregulation of signaling pathways involved in brain development seems to play a more important role in the pathogenesis of these tumors than do abnormalities in well-known tumor oncogenes and tumor suppressors, such as p53 or EGFR. Large collaborative studies are needed to provide insights into the importance of the genes discovered so far, in order to evaluate their possible use for improved risk stratification of patients and their use as therapeutic targets. In addition, data from newly developed techniques such as microRNA profiling and the use of single nucleotide polymorphisms or exon arrays may provide new insights into the regulation of posttranscriptional gene expression and alternative splicing.
References
- 1.Wrensch M, Minn Y, Chew T, et al. Epidemiology of primary brain tumors: current concepts and review of the literature. Neuro-Oncology. 2002;4(4):278–299. doi: 10.1093/neuonc/4.4.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ray A, Ho M, Ma J, et al. A clinicobiological model predicting survival in medulloblastoma. Clin Cancer Res. 2004;10(22):7613–7620. doi: 10.1158/1078-0432.CCR-04-0499. [DOI] [PubMed] [Google Scholar]
- 3.Packer RJ, Gajjar A, Vezina G, et al. Phase III study of craniospinal radiation therapy followed by adjuvant chemotherapy for newly diagnosed average-risk medulloblastoma. J Clin Oncol. 2006;24(25):4202–4208. doi: 10.1200/JCO.2006.06.4980. [DOI] [PubMed] [Google Scholar]
- 4.Taylor RE, Bailey CC, Robinson K, et al. Results of a randomized study of preradiation chemotherapy versus radiotherapy alone for nonmetastatic medulloblastoma: the International Society of Paediatric Oncology/United Kingdom Children’s Cancer Study Group PNET-3 Study. J Clin Oncol. 2003;21(8):1581–1591. doi: 10.1200/JCO.2003.05.116. [DOI] [PubMed] [Google Scholar]
- 5.Ris MD, Packer R, Goldwein J, et al. Intellectual outcome after reduced-dose radiation therapy plus adjuvant chemotherapy for medulloblastoma: a Children’s Cancer Group study. J Clin Oncol. 2001;19(15):3470–3476. doi: 10.1200/JCO.2001.19.15.3470. [DOI] [PubMed] [Google Scholar]
- 6.Rutkowski S, Bode U, Deinlein F, et al. Treatment of early childhood medulloblastoma by postoperative chemotherapy alone. N Engl J Med. 2005;352(10):978–986. doi: 10.1056/NEJMoa042176. [DOI] [PubMed] [Google Scholar]
- 7.Packer RJ, Biegel JA, Blaney S, et al. Atypical teratoid/rhabdoid tumor of the central nervous system: report on workshop. J Pediatr Hematol Oncol. 2002;24(5):337–342. doi: 10.1097/00043426-200206000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Cowan R, Hoban P, Kelsey A, et al. The gene for the naevoid basal cell carcinoma syndrome acts as a tumour-suppressor gene in medulloblastoma. Br J Cancer. 1997;76(2):141–145. doi: 10.1038/bjc.1997.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wechsler-Reya RJ, Scott MP. Control of neuronal precursor proliferation in the cerebellum by sonic hedgehog. Neuron. 1999;22(1):103–114. doi: 10.1016/s0896-6273(00)80682-0. [DOI] [PubMed] [Google Scholar]
- 10.Leung C, Lingbeek M, Shakhova O, et al. Bmi1 is essential for cerebellar development and is overexpressed in human medulloblastomas. Nature. 2004;428(6980):337–341. doi: 10.1038/nature02385. [DOI] [PubMed] [Google Scholar]
- 11.Romer JT, Kimura H, Magdaleno S, et al. Suppression of the Shh pathway using a small molecule inhibitor eliminates medulloblastoma in Ptc1(+/−)p53(−/−) mice. Cancer Cell. 2004;6(3):229–240. doi: 10.1016/j.ccr.2004.08.019. [DOI] [PubMed] [Google Scholar]
- 12.Wetmore C, Eberhart DE, Curran T. Loss of p53 but not ARF accelerates medulloblastoma in mice heterozygous for patched. Cancer Res. 2001;61(2):513–516. [PubMed] [Google Scholar]
- 13.Polakis P. Wnt signaling and cancer. Genes Dev. 2000;14(15):1837–1851. [PubMed] [Google Scholar]
- 14.Novak A, Dedhar S. Signaling through beta-catenin and Lef/Tcf. Cell Mol Life Sci. 1999;56(5–6):523–537. doi: 10.1007/s000180050449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Clifford SC, Lusher ME, Lindsey JC, et al. Wnt/Wingless pathway activation and chromosome 6 loss characterize a distinct molecular subgroup of medulloblastomas associated with a favorable prognosis. Cell Cycle. 2006;5(22):2666–2670. doi: 10.4161/cc.5.22.3446. [DOI] [PubMed] [Google Scholar]
- 16.Thompson MC, Fuller C, Hogg TL, et al. Genomics identifies medulloblastoma subgroups that are enriched for specific genetic alterations. J Clin Oncol. 2006;24(12):1924–1931. doi: 10.1200/JCO.2005.04.4974. [DOI] [PubMed] [Google Scholar]
- 17.Baeza N, Masuoka J, Kleihues P, et al. AXIN1 mutations but not deletions in cerebellar medulloblastomas. Oncogene. 2003;22(4):632–636. doi: 10.1038/sj.onc.1206156. [DOI] [PubMed] [Google Scholar]
- 18.Pizem J, Cort A, Zadravec-Zaletel L, et al. Survivin is a negative prognostic marker in medulloblastoma. Neuropathol Appl Neurobiol. 2005;31(4):422–428. doi: 10.1111/j.1365-2990.2005.00664.x. [DOI] [PubMed] [Google Scholar]
- 19.Fangusaro JR, Jiang Y, Holloway MP, et al. Survivin, Survivin-2B, and Survivin-deltaEx3 expression in medulloblastoma: biologic markers of tumour morphology and clinical outcome. Br J Cancer. 2005;92(2):359–365. doi: 10.1038/sj.bjc.6602317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zorn AM, Barish GD, Williams BO, et al. Regulation of Wnt signaling by Sox proteins: XSox17 alpha/beta and XSox3 physically interact with beta-catenin. Mol Cell. 1999;4(4):487–498. doi: 10.1016/s1097-2765(00)80200-2. [DOI] [PubMed] [Google Scholar]
- 21.Lee CJ, Appleby VJ, Orme AT, et al. Differential expression of SOX4 and SOX11 in medulloblastoma. J Neurooncol. 2002;57(3):201–214. doi: 10.1023/a:1015773818302. [DOI] [PubMed] [Google Scholar]
- 22.de Bont JM, Kros JM, Passier MMCJ, et al. Differential expression and prognostic significance of SOX genes in pediatric medulloblastoma and ependymoma identified by microarray analysis Neuro-oncology 2008June24[epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Neben K, Korshunov A, Benner A, et al. Microarray-based screening for molecular markers in medulloblastoma revealed STK15 as independent predictor for survival. Cancer Res. 2004;64(9):3103–3111. doi: 10.1158/0008-5472.can-03-3968. [DOI] [PubMed] [Google Scholar]
- 24.Dakubo GD, Mazerolle CJ, Wallace VA. Expression of Notch and Wnt pathway components and activation of Notch signaling in medulloblastomas from heterozygous patched mice. J Neurooncol. 2006;79(3):221–227. doi: 10.1007/s11060-006-9132-2. [DOI] [PubMed] [Google Scholar]
- 25.Fan X, Mikolaenko I, Elhassan I, et al. Notch1 and Notch2 have opposite effects on embryonal brain tumor growth. Cancer Res. 2004;64(21):7787–7793. doi: 10.1158/0008-5472.CAN-04-1446. [DOI] [PubMed] [Google Scholar]
- 26.Baron M. An overview of the Notch signalling pathway. Semin Cell Dev Biol. 2003;14(2):113–119. doi: 10.1016/s1084-9521(02)00179-9. [DOI] [PubMed] [Google Scholar]
- 27.Adesina AM, Nguyen Y, Mehta V, et al. FOXG1 dysregulation is a frequent event in medulloblastoma. J Neurooncol. 2007;85(2):111–122. doi: 10.1007/s11060-007-9394-3. [DOI] [PubMed] [Google Scholar]
- 28.Hallahan AR, Pritchard JI, Hansen S, et al. The SmoA1 mouse model reveals that notch signaling is critical for the growth and survival of sonic hedgehog-induced medulloblastomas. Cancer Res. 2004;64(21):7794–7800. doi: 10.1158/0008-5472.CAN-04-1813. [DOI] [PubMed] [Google Scholar]
- 29.Gilbertson RJ, Clifford SC, MacMeekin W, et al. Expression of the ErbB-neuregulin signaling network during human cerebellar development: implications for the biology of medulloblastoma. Cancer Res. 1998;58(17):3932–3941. [PubMed] [Google Scholar]
- 30.Ferretti E, Di Marcotullio L, Gessi M, et al. Alternative splicing of the ErbB-4 cytoplasmic domain and its regulation by hedgehog signaling identify distinct medulloblastoma subsets. Oncogene. 2006;25(55):7267–7273. doi: 10.1038/sj.onc.1209716. [DOI] [PubMed] [Google Scholar]
- 31.Elenius K, Choi CJ, Paul S, et al. Characterization of a naturally occurring ErbB4 isoform that does not bind or activate phosphatidyl inositol 3-kinase. Oncogene. 1999;18(16):2607–2615. doi: 10.1038/sj.onc.1202612. [DOI] [PubMed] [Google Scholar]
- 32.Bal MM, Das Radotra B, Srinivasan R, et al. Expression of c-erbB-4 in medulloblastoma and its correlation with prognosis. Histopathology. 2006;49(1):92–93. doi: 10.1111/j.1365-2559.2006.02337.x. [DOI] [PubMed] [Google Scholar]
- 33.Hernan R, Fasheh R, Calabrese C, et al. ERBB2 up-regulates S100A4 and several other prometastatic genes in medulloblastoma. Cancer Res. 2003;63(1):140–148. [PubMed] [Google Scholar]
- 34.Amin DN, Tuck D, Stern DF. Neuregulin-regulated gene expression in mammary carcinoma cells. Exp Cell Res. 2005;309(1):12–23. doi: 10.1016/j.yexcr.2005.04.034. [DOI] [PubMed] [Google Scholar]
- 35.Henriksson M, Luscher B. Proteins of the Myc network: essential regulators of cell growth and differentiation. Adv Cancer Res. 1996;68:109–182. doi: 10.1016/s0065-230x(08)60353-x. [DOI] [PubMed] [Google Scholar]
- 36.He TC, Sparks AB, Rago C, et al. Identification of c-MYC as a target of the APC pathway. Science. 1998;281(5382):1509–1512. doi: 10.1126/science.281.5382.1509. [DOI] [PubMed] [Google Scholar]
- 37.Rao G, Pedone CA, Coffin CM, et al. c-Myc enhances sonic hedgehog-induced medulloblastoma formation from nestin-expressing neural progenitors in mice. Neoplasia. 2003;5(3):198–204. doi: 10.1016/S1476-5586(03)80052-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pomeroy SL, Tamayo P, Gaasenbeek M, et al. Prediction of central nervous system embryonal tumour outcome based on gene expression. Nature. 2002;415(6870):436–442. doi: 10.1038/415436a. [DOI] [PubMed] [Google Scholar]
- 39.Browd SR, Kenney AM, Gottfried ON, et al. N-myc can substitute for insulin-like growth factor signaling in a mouse model of sonic hedgehog-induced medulloblastoma. Cancer Res. 2006;66(5):2666–2672. doi: 10.1158/0008-5472.CAN-05-2198. [DOI] [PubMed] [Google Scholar]
- 40.Eberhart CG, Kratz J, Wang Y, et al. Histopathological and molecular prognostic markers in medulloblastoma: c-Myc, n-Myc, TrkC, and anaplasia. J Neuropathol Exp Neurol. 2004;63(5):441–449. doi: 10.1093/jnen/63.5.441. [DOI] [PubMed] [Google Scholar]
- 41.Kenney AM, Widlund HR, Rowitch DH. Hedgehog and PI-3 kinase signaling converge on Nmyc1 to promote cell cycle progression in cerebellar neuronal precursors. Development. 2004;131(1):217–228. doi: 10.1242/dev.00891. [DOI] [PubMed] [Google Scholar]
- 42.Zumkeller W, Westphal M. The IGF/IGFBP system in CNS malignancy. Mol Pathol. 2001;54(4):227–229. doi: 10.1136/mp.54.4.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang JY, Del Valle L, Gordon J, et al. Activation of the IGF-IR system contributes to malignant growth of human and mouse medulloblastomas. Oncogene. 2001;20(29):3857–3868. doi: 10.1038/sj.onc.1204532. [DOI] [PubMed] [Google Scholar]
- 44.Urbanska K, Trojanek J, Del Valle L, et al. Inhibition of IGF-1 receptor in anchorage-independence attenuates GSK-3beta constitutive phosphorylation and compromises growth and survival of medulloblastoma cell lines. Oncogene. 2007;26(16):2308–2317. doi: 10.1038/sj.onc.1210018. [DOI] [PubMed] [Google Scholar]
- 45.Hartmann W, Koch A, Brune H, et al. Insulin-like growth factor II is involved in the proliferation control of medulloblastoma and its cerebellar precursor cells. Am J Pathol. 2005;166(4):1153–1162. doi: 10.1016/S0002-9440(10)62335-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Patti R, Reddy CD, Geoerger B, et al. Autocrine secreted insulin-like growth factor-I stimulates MAP kinase-dependent mitogenic effects in human primitive neuroectodermal tumor/medulloblastoma. Int J Oncol. 2000;16(3):577–584. doi: 10.3892/ijo.16.3.577. [DOI] [PubMed] [Google Scholar]
- 47.Hahn H, Wojnowski L, Specht K, et al. Patched target Igf2 is indispensable for the formation of medulloblastoma and rhabdomyosarcoma. J Biol Chem. 2000;275(37):28341–28344. doi: 10.1074/jbc.C000352200. [DOI] [PubMed] [Google Scholar]
- 48.De Bont JM, van Doorn J, Reddingius RE, et al. Various components of the insulin-like growth factor system in tumor tissue, cerebrospinal fluid and peripheral blood of pediatric medulloblastoma and ependymoma patients. Int J Cancer. 2008;123(3):594–600. doi: 10.1002/ijc.23558. [DOI] [PubMed] [Google Scholar]
- 49.Buhren J, Christoph AH, Buslei R, et al. Expression of the neurotrophin receptor p75NTR in medulloblastomas is correlated with distinct histological and clinical features: evidence for a medulloblastoma subtype derived from the external granule cell layer. J Neuropathol Exp Neurol. 2000;59(3):229–240. doi: 10.1093/jnen/59.3.229. [DOI] [PubMed] [Google Scholar]
- 50.Gazit R, Krizhanovsky V, Ben-Arie N. Math1 controls cerebellar granule cell differentiation by regulating multiple components of the Notch signaling pathway. Development. 2004;131(4):903–913. doi: 10.1242/dev.00982. [DOI] [PubMed] [Google Scholar]
- 51.Kruttgen A, Schneider I, Weis J. The dark side of the NGF family: neurotrophins in neoplasias. Brain Pathol. 2006;16(4):304–310. doi: 10.1111/j.1750-3639.2006.00037.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lee JE. NeuroD and neurogenesis. Dev Neurosci. 1997;19(1):27–32. doi: 10.1159/000111182. [DOI] [PubMed] [Google Scholar]
- 53.de Haas T, Oussoren E, Grajkowska W, et al. OTX1 and OTX2 expression correlates with the clinicopathologic classification of medulloblastomas. J Neuropathol Exp Neurol. 2006;65(2):176–186. doi: 10.1097/01.jnen.0000199576.70923.8a. [DOI] [PubMed] [Google Scholar]
- 54.Di C, Liao S, Adamson DC, et al. Identification of OTX2 as a medulloblastoma oncogene whose product can be targeted by all-trans retinoic acid. Cancer Res. 2005;65(3):919–924. [PubMed] [Google Scholar]
- 55.Biegel JA, Rorke LB, Packer RJ, et al. Isochromosome 17q in primitive neuroectodermal tumors of the central nervous system. Genes Chromosomes Cancer. 1989;1(2):139–147. doi: 10.1002/gcc.2870010206. [DOI] [PubMed] [Google Scholar]
- 56.Pan E, Pellarin M, Holmes E, et al. Isochromosome 17q is a negative prognostic factor in poor-risk childhood medulloblastoma patients. Clin Cancer Res. 2005;11(13):4733–4740. doi: 10.1158/1078-0432.CCR-04-0465. [DOI] [PubMed] [Google Scholar]
- 57.Biegel JA, Janss AJ, Raffel C, et al. Prognostic significance of chromosome 17p deletions in childhood primitive neuroectodermal tumors (medulloblastomas) of the central nervous system. Clin Cancer Res. 1997;3(3):473–478. [PubMed] [Google Scholar]
- 58.Burnett ME, White EC, Sih S, et al. Chromosome arm 17p deletion analysis reveals molecular genetic heterogeneity in supratentorial and infratentorial primitive neuroectodermal tumors of the central nervous system. Cancer Genet Cytogenet. 1997;97(1):25–31. doi: 10.1016/s0165-4608(96)00319-6. [DOI] [PubMed] [Google Scholar]
- 59.Mendrzyk F, Korshunov A, Toedt G, et al. Isochromosome breakpoints on 17p in medulloblastoma are flanked by different classes of DNA sequence repeats. Genes Chromosomes Cancer. 2006;45(4):401–410. doi: 10.1002/gcc.20304. [DOI] [PubMed] [Google Scholar]
- 60.Briggs KJ, Corcoran-Schwartz IM, Zhang W, et al. Cooperation between the Hic1 and Ptch1 tumor suppressors in medulloblastoma. Genes Dev. 2008;22(6):770–785. doi: 10.1101/gad.1640908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bulavin DV, Demidov ON, Saito S, et al. Amplification of PPM1D in human tumors abrogates p53 tumor-suppressor activity. Nat Genet. 2002;31(2):210–215. doi: 10.1038/ng894. [DOI] [PubMed] [Google Scholar]
- 62.Hui AB, Takano H, Lo KW, et al. Identification of a novel homozygous deletion region at 6q23.1 in medulloblastomas using high-resolution array comparative genomic hybridization analysis. Clin Cancer Res. 2005;11(13):4707–4716. doi: 10.1158/1078-0432.CCR-05-0128. [DOI] [PubMed] [Google Scholar]
- 63.Mendrzyk F, Radlwimmer B, Joos S, et al. Genomic and protein expression profiling identifies CDK6 as novel independent prognostic marker in medulloblastoma. J Clin Oncol. 2005;23(34):8853–8862. doi: 10.1200/JCO.2005.02.8589. [DOI] [PubMed] [Google Scholar]
- 64.McCabe MG, Ichimura K, Liu L, et al. High-resolution array-based comparative genomic hybridization of medulloblastomas and supratentorial primitive neuroectodermal tumors. J Neuropathol Exp Neurol. 2006;65(6):549–561. doi: 10.1097/00005072-200606000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lo KC, Rossi MR, Burkhardt T, et al. Overlay analysis of the oligonucleotide array gene expression profiles and copy number abnormalities as determined by array comparative genomic hybridization in medulloblastomas. Genes Chromosomes Cancer. 2007;46(1):53–66. doi: 10.1002/gcc.20388. [DOI] [PubMed] [Google Scholar]
- 66.Yin XL, Pang JC, Ng HK. Identification of a region of homozygous deletion on 8p22–23.1 in medulloblastoma. Oncogene. 2002;21(9):1461–1468. doi: 10.1038/sj.onc.1205204. [DOI] [PubMed] [Google Scholar]
- 67.Lo KC, Rossi MR, Eberhart CG, et al. Genome wide copy number abnormalities in pediatric medulloblastomas as assessed by array comparative genome hybridization. Brain Pathol. 2007;17(3):282–296. doi: 10.1111/j.1750-3639.2007.00072.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rossi MR, Conroy J, McQuaid D, et al. Array CGH analysis of pediatric medulloblastomas. Genes Chromosomes Cancer. 2006;45(3):290–303. doi: 10.1002/gcc.20292. [DOI] [PubMed] [Google Scholar]
- 69.Yin XL, Pang JC, Liu YH, et al. Analysis of loss of heterozygosity on chromosomes 10q, 11, and 16 in medulloblastomas. J Neurosurg. 2001;94(5):799–805. doi: 10.3171/jns.2001.94.5.0799. [DOI] [PubMed] [Google Scholar]
- 70.Ehrbrecht A, Muller U, Wolter M, et al. Comprehensive genomic analysis of desmoplastic medulloblastomas: identification of novel amplified genes and separate evaluation of the different histological components. J Pathol. 2006;208(4):554–563. doi: 10.1002/path.1925. [DOI] [PubMed] [Google Scholar]
- 71.Jones PA, Baylin SB. The fundamental role of epigenetic events in cancer. Nat Rev Genet. 2002;3(6):415–428. doi: 10.1038/nrg816. [DOI] [PubMed] [Google Scholar]
- 72.Lusher ME, Lindsey JC, Latif F, et al. Biallelic epigenetic inactivation of the RASSF1A tumor suppressor gene in medulloblastoma development. Cancer Res. 2002;62(20):5906–5911. [PubMed] [Google Scholar]
- 73.Debatin KM, Krammer PH. Death receptors in chemotherapy and cancer. Oncogene. 2004;23(16):2950–2966. doi: 10.1038/sj.onc.1207558. [DOI] [PubMed] [Google Scholar]
- 74.Grotzer MA, Eggert A, Zuzak TJ, et al. Resistance to TRAIL-induced apoptosis in primitive neuroectodermal brain tumor cells correlates with a loss of caspase-8 expression. Oncogene. 2000;19(40):4604–4610. doi: 10.1038/sj.onc.1203816. [DOI] [PubMed] [Google Scholar]
- 75.Pfister S, Schlaeger C, Mendrzyk F, et al. Array-based profiling of reference-independent methylation status (aPRIMES) identifies frequent promoter methylation and consecutive downregulation of ZIC2 in pediatric medulloblastoma. Nucleic Acids Res. 2007;35(7):e51. doi: 10.1093/nar/gkm094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Uziel T, Zindy F, Xie S, et al. The tumor suppressors Ink4c and p53 collaborate independently with Patched to suppress medulloblastoma formation. Genes Dev. 2005;19(22):2656–2667. doi: 10.1101/gad.1368605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Peyrl A, Krapfenbauer K, Slavc I, et al. Protein profiles of medulloblastoma cell lines DAOY and D283: identification of tumor-related proteins and principles. Proteomics. 2003;3(9):1781–1800. doi: 10.1002/pmic.200300460. [DOI] [PubMed] [Google Scholar]
- 78.Horn B, Heideman R, Geyer R, et al. A multi-institutional retrospective study of intracranial ependymoma in children: identification of risk factors. J Pediatr Hematol Oncol. 1999;21(3):203–211. doi: 10.1097/00043426-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 79.Merchant TE, Jenkins JJ, Burger PC, et al. Influence of tumor grade on time to progression after irradiation for localized ependymoma in children. Int J Radiat Oncol Biol Phys. 2002;53(1):52–57. doi: 10.1016/s0360-3016(01)02801-2. [DOI] [PubMed] [Google Scholar]
- 80.Grundy RG, Wilne SA, Weston CL, et al. Primary postoperative chemotherapy without radiotherapy for intracranial ependymoma in children: the UKCCSG/SIOP prospective study. Lancet Oncol. 2007;8(8):696–705. doi: 10.1016/S1470-2045(07)70208-5. [DOI] [PubMed] [Google Scholar]
- 81.Kato H, Uchimura I, Morohoshi M, et al. Multiple endocrine neoplasia type 1 associated with spinal ependymoma. Intern Med. 1996;35(4):285–289. doi: 10.2169/internalmedicine.35.285. [DOI] [PubMed] [Google Scholar]
- 82.Lamszus K, Lachenmayer L, Heinemann U, et al. Molecular genetic alterations on chromosomes 11 and 22 in ependymomas. Int J Cancer. 2001;91(6):803–808. doi: 10.1002/1097-0215(200002)9999:9999<::aid-ijc1134>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 83.Taylor MD, Poppleton H, Fuller C, et al. Radial glia cells are candidate stem cells of ependymoma. Cancer Cell. 2005;8(4):323–335. doi: 10.1016/j.ccr.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 84.Conover JC, Doetsch F, Garcia-Verdugo JM, et al. Disruption of Eph/ephrin signaling affects migration and proliferation in the adult sub-ventricular zone. Nat Neurosci. 2000;3(11):1091–1097. doi: 10.1038/80606. [DOI] [PubMed] [Google Scholar]
- 85.Hitoshi S, Alexson T, Tropepe V, et al. Notch pathway molecules are essential for the maintenance, but not the generation, of mammalian neural stem cells. Genes Dev. 2002;16(7):846–858. doi: 10.1101/gad.975202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mullins KJ, Rubio A, Myers SP, et al. Malignant ependymomas in a patient with Turcot’s syndrome: case report and management guidelines. Surg Neurol. 1998;49(3):290–294. doi: 10.1016/s0090-3019(97)00299-1. [DOI] [PubMed] [Google Scholar]
- 87.Suarez-Merino B, Hubank M, Revesz T, et al. Microarray analysis of pediatric ependymoma identifies a cluster of 112 candidate genes including four transcripts at 22q12.1-q13.3. Neuro-Oncology. 2005;7(1):20–31. doi: 10.1215/S1152851704000596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Modena P, Lualdi E, Facchinetti F, et al. Identification of tumor-specific molecular signatures in intracranial ependymoma and association with clinical characteristics. J Clin Oncol. 2006;24(33):5223–5233. doi: 10.1200/JCO.2006.06.3701. [DOI] [PubMed] [Google Scholar]
- 89.Metzger AK, Sheffield VC, Duyk G, et al. Identification of a germ-line mutation in the p53 gene in a patient with an intracranial ependymoma. Proc Natl Acad Sci U S A. 1991;88(17):7825–7829. doi: 10.1073/pnas.88.17.7825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zamecnik J, Snuderl M, Eckschlager T, et al. Pediatric intracranial ependymomas: prognostic relevance of histological, immunohistochemical, and flow cytometric factors. Mod Pathol. 2003;16(10):980–991. doi: 10.1097/01.MP.0000087420.34166.B6. [DOI] [PubMed] [Google Scholar]
- 91.Michalides RJ. Cell cycle regulators: mechanisms and their role in aetiology, prognosis, and treatment of cancer. J Clin Pathol. 1999;52(8):555–568. doi: 10.1136/jcp.52.8.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Korshunov A, Golanov A, Timirgaz V. p14ARF protein (FL-132) immunoreactivity in intracranial ependymomas and its prognostic significance: an analysis of 103 cases. Acta Neuropathol (Berl) 2001;102(3):271–277. doi: 10.1007/s004010100379. [DOI] [PubMed] [Google Scholar]
- 93.Sowar K, Straessle J, Donson AM, et al. Predicting which children are at risk for ependymoma relapse. J Neurooncol. 2006;78(1):41–46. doi: 10.1007/s11060-005-9072-2. [DOI] [PubMed] [Google Scholar]
- 94.Lukashova-v Zangen I, Kneitz S, Monoranu CM, et al. Ependymoma gene expression profiles associated with histological subtype, proliferation, and patient survival. Acta Neuropathol. 2007;113(3):325–337. doi: 10.1007/s00401-006-0190-5. [DOI] [PubMed] [Google Scholar]
- 95.Preusser M, Wolfsberger S, Czech T, et al. Survivin expression in intracranial ependymomas and its correlation with tumor cell proliferation and patient outcome. Am J Clin Pathol. 2005;124(4):543–549. doi: 10.1309/PP2G5GAAFKV82DTG. [DOI] [PubMed] [Google Scholar]
- 96.Wolfsberger S, Fischer I, Hoftberger R, et al. Ki-67 immunolabeling index is an accurate predictor of outcome in patients with intracranial ependymoma. Am J Surg Pathol. 2004;28(7):914–920. doi: 10.1097/00000478-200407000-00011. [DOI] [PubMed] [Google Scholar]
- 97.Hirose Y, Aldape K, Bollen A, et al. Chromosomal abnormalities subdivide ependymal tumors into clinically relevant groups. Am J Pathol. 2001;158(3):1137–1143. doi: 10.1016/S0002-9440(10)64061-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mendrzyk F, Korshunov A, Benner A, et al. Identification of gains on 1q and epidermal growth factor receptor overexpression as independent prognostic markers in intracranial ependymoma Clin Cancer Res 200612(7 pt 1)2070–2079. [DOI] [PubMed] [Google Scholar]
- 99.Dyer S, Prebble E, Davison V, et al. Genomic imbalances in pediatric intracranial ependymomas define clinically relevant groups. Am J Pathol. 2002;161(6):2133–2141. doi: 10.1016/S0002-9440(10)64491-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jeuken JW, Sprenger SH, Gilhuis J, et al. Correlation between localization, age, and chromosomal imbalances in ependymal tumours as detected by CGH. J Pathol. 2002;197(2):238–244. doi: 10.1002/path.1086. [DOI] [PubMed] [Google Scholar]
- 101.Hulsebos TJ, Oskam NT, Bijleveld EH, et al. Evidence for an ependymoma tumour suppressor gene in chromosome region 22pter-22q11.2. Br J Cancer. 1999;81(7):1150–1154. doi: 10.1038/sj.bjc.6690822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Rousseau-Merck M, Versteege I, Zattara-Cannoni H, et al. Fluorescence in situ hybridization determination of 22q12-q13 deletion in two intracerebral ependymomas. Cancer Genet Cytogenet. 2000;121(2):223–227. doi: 10.1016/s0165-4608(00)00262-4. [DOI] [PubMed] [Google Scholar]
- 103.Sevenet N, Sheridan E, Amram D, et al. Constitutional mutations of the hSNF5/INI1 gene predispose to a variety of cancers. Am J Hum Genet. 1999;65(5):1342–1348. doi: 10.1086/302639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Esteller M, Garcia-Foncillas J, Andion E, et al. Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med. 2000;343(19):1350–1354. doi: 10.1056/NEJM200011093431901. [DOI] [PubMed] [Google Scholar]
- 105.Vorechovsky I, Tingby O, Hartman M, et al. Somatic mutations in the human homologue of Drosophila patched in primitive neuroectodermal tumours. Oncogene. 1997;15(3):361–366. doi: 10.1038/sj.onc.1201340. [DOI] [PubMed] [Google Scholar]
- 106.Wolter M, Reifenberger J, Sommer C, et al. Mutations in the human homologue of the Drosophila segment polarity gene patched (PTCH) in sporadic basal cell carcinomas of the skin and primitive neuroectodermal tumors of the central nervous system. Cancer Res. 1997;57(13):2581–2585. [PubMed] [Google Scholar]
- 107.Pietsch T, Waha A, Koch A, et al. Medulloblastomas of the desmoplastic variant carry mutations of the human homologue of Drosophila patched. Cancer Res. 1997;57(11):2085–2088. [PubMed] [Google Scholar]
- 108.Raffel C, Jenkins RB, Frederick L, et al. Sporadic medulloblastomas contain PTCH mutations. Cancer Res. 1997;57(5):842–845. [PubMed] [Google Scholar]
- 109.Zurawel RH, Allen C, Wechsler-Reya R, et al. Evidence that haploinsufficiency of Ptch leads to medulloblastoma in mice. Genes Chromosomes Cancer. 2000;28(1):77–81. [PubMed] [Google Scholar]
- 110.Taylor MD, Liu L, Raffel C, et al. Mutations in SUFU predispose to medulloblastoma. Nat Genet. 2002;31(3):306–310. doi: 10.1038/ng916. [DOI] [PubMed] [Google Scholar]
- 111.Koch A, Waha A, Hartmann W, et al. No evidence for mutations or altered expression of the Suppressor of Fused gene (SUFU) in primitive neuroectodermal tumours. Neuropathol Appl Neurobiol. 2004;30(5):532–539. doi: 10.1111/j.1365-2990.2004.00560.x. [DOI] [PubMed] [Google Scholar]
- 112.Reifenberger J, Wolter M, Weber RG, et al. Missense mutations in SMOH in sporadic basal cell carcinomas of the skin and primitive neuroectodermal tumors of the central nervous system. Cancer Res. 1998;58(9):1798–1803. [PubMed] [Google Scholar]
- 113.Zurawel RH, Allen C, Chiappa S, et al. Analysis of PTCH/SMO/SHH pathway genes in medulloblastoma. Genes Chromosomes Cancer. 2000;27(1):44–51. doi: 10.1002/(sici)1098-2264(200001)27:1<44::aid-gcc6>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 114.Di Marcotullio L, Ferretti E, De Smaele E, et al. REN(KCTD11) is a suppressor of Hedgehog signaling and is deleted in human medulloblastoma. Proc Natl Acad Sci U S A. 2004;101(29):10833–10838. doi: 10.1073/pnas.0400690101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Dahmen RP, Koch A, Denkhaus D, et al. Deletions of AXIN1, a component of the WNT/wingless pathway, in sporadic medulloblastomas. Cancer Res. 2001;61(19):7039–7043. [PubMed] [Google Scholar]
- 116.Yokota N, Nishizawa S, Ohta S, et al. Role of Wnt pathway in medulloblastoma oncogenesis. Int J Cancer. 2002;101(2):198–201. doi: 10.1002/ijc.10559. [DOI] [PubMed] [Google Scholar]
- 117.Koch A, Hrychyk A, Hartmann W, et al. Mutations of the Wnt antagonist AXIN2 (conductin) result in TCF-dependent transcription in medulloblastomas. Int J Cancer. 2007;121(2):284–291. doi: 10.1002/ijc.22675. [DOI] [PubMed] [Google Scholar]
- 118.Koch A, Waha A, Tonn JC, et al. Somatic mutations of WNT/wingless signaling pathway components in primitive neuroectodermal tumors. Int J Cancer. 2001;93(3):445–449. doi: 10.1002/ijc.1342. [DOI] [PubMed] [Google Scholar]
- 119.Huang H, Mahler-Araujo BM, Sankila A, et al. APC mutations in sporadic medulloblastomas. Am J Pathol. 2000;156(2):433–437. doi: 10.1016/S0002-9440(10)64747-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zurawel RH, Chiappa SA, Allen C, et al. Sporadic medulloblastomas contain oncogenic beta-catenin mutations. Cancer Res. 1998;58(5):896–899. [PubMed] [Google Scholar]
- 121.Ellison DW, Onilude OE, Lindsey JC, et al. beta-Catenin status predicts a favorable outcome in childhood medulloblastoma: the United Kingdom Children’s Cancer Study Group Brain Tumour Committee. J Clin Oncol. 2005;23(31):7951–7957. doi: 10.1200/JCO.2005.01.5479. [DOI] [PubMed] [Google Scholar]
- 122.Bodey B, Bodey V, Siegel SE, et al. Survivin expression in childhood medulloblastomas: a possible diagnostic and prognostic marker. In Vivo. 2004;18(6):713–718. [PubMed] [Google Scholar]
- 123.Haberler C, Slavc I, Czech T, et al. Histopathological prognostic factors in medulloblastoma: high expression of survivin is related to unfavourable outcome. Eur J Cancer. 2006;42(17):2996–3003. doi: 10.1016/j.ejca.2006.05.038. [DOI] [PubMed] [Google Scholar]
- 124.Yokota N, Mainprize TG, Taylor MD, et al. Identification of differentially expressed and developmentally regulated genes in medulloblastoma using suppression subtraction hybridization. Oncogene. 2004;23(19):3444–3453. doi: 10.1038/sj.onc.1207475. [DOI] [PubMed] [Google Scholar]
- 125.Thomson SA, Kennerly E, Olby N, et al. Microarray analysis of differentially expressed genes of primary tumors in the canine central nervous system. Vet Pathol. 2005;42(5):550–558. doi: 10.1354/vp.42-5-550. [DOI] [PubMed] [Google Scholar]
- 126.Gilbertson RJ, Perry RH, Kelly PJ, et al. Prognostic significance of HER2 and HER4 coexpression in childhood medulloblastoma. Cancer Res. 1997;57(15):3272–3280. [PubMed] [Google Scholar]
- 127.Bal MM, Das Radotra B, Srinivasan R, et al. Does c-erbB-2 expression have a role in medulloblastoma prognosis? Indian J Pathol Microbiol. 2006;49(4):535–539. [PubMed] [Google Scholar]
- 128.Lee CJ, Chan WI, Scotting PJ. CIC, a gene involved in cerebellar development and ErbB signaling, is significantly expressed in medulloblastomas. J Neurooncol. 2005;73(2):101–108. doi: 10.1007/s11060-004-4598-2. [DOI] [PubMed] [Google Scholar]
- 129.Stearns D, Chaudhry A, Abel TW, et al. c-Myc overexpression causes anaplasia in medulloblastoma. Cancer Res. 2006;66(2):673–681. doi: 10.1158/0008-5472.CAN-05-1580. [DOI] [PubMed] [Google Scholar]
- 130.Aldosari N, Bigner SH, Burger PC, et al. MYCC and MYCN oncogene amplification in medulloblastoma. A fluorescence in situ hybridization study on paraffin sections from the Children’s Oncology Group. Arch Pathol Lab Med. 2002;126(5):540–544. doi: 10.5858/2002-126-0540-MAMOAI. [DOI] [PubMed] [Google Scholar]
- 131.Bruggers CS, Tai KF, Murdock T, et al. Expression of the c-Myc protein in childhood medulloblastoma. J Pediatr Hematol Oncol. 1998;20(1):18–25. doi: 10.1097/00043426-199801000-00003. [DOI] [PubMed] [Google Scholar]
- 132.Grotzer MA, Hogarty MD, Janss AJ, et al. MYC messenger RNA expression predicts survival outcome in childhood primitive neuroectodermal tumor/medulloblastoma. Clin Cancer Res. 2001;7(8):2425–2433. [PubMed] [Google Scholar]
- 133.Herms J, Neidt I, Luscher B, et al. C-MYC expression in medulloblastoma and its prognostic value. Int J Cancer. 2000;89(5):395–402. [PubMed] [Google Scholar]
- 134.Sommer A, Waha A, Tonn J, et al. Analysis of the Max-binding protein MNT in human medulloblastomas. Int J Cancer. 1999;82(6):810–816. doi: 10.1002/(sici)1097-0215(19990909)82:6<810::aid-ijc7>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 135.Cvekl A, Jr, Zavadil J, Birshtein BK, et al. Analysis of transcripts from 17p13.3 in medulloblastoma suggests ROX/MNT as a potential tumour suppressor gene. Eur J Cancer. 2004;40(16):2525–2532. doi: 10.1016/j.ejca.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 136.Fruhwald MC, O’Dorisio MS, Rush LJ, et al. Gene amplification in PNETs/medulloblastomas: mapping of a novel amplified gene within the MYCN amplicon. J Med Genet. 2000;37(7):501–509. doi: 10.1136/jmg.37.7.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Pession A, Tonelli R. The MYCN oncogene as a specific and selective drug target for peripheral and central nervous system tumors. Curr Cancer Drug Targets. 2005;5(4):273–283. doi: 10.2174/1568009054064606. [DOI] [PubMed] [Google Scholar]
- 138.Tomlinson FH, Jenkins RB, Scheithauer BW, et al. Aggressive medulloblastoma with high-level N-myc amplification. Mayo Clin Proc. 1994;69(4):359–365. doi: 10.1016/s0025-6196(12)62221-6. [DOI] [PubMed] [Google Scholar]
- 139.Huang A, Ho CS, Ponzielli R, et al. Identification of a novel c-Myc protein interactor, JPO2, with transforming activity in medulloblastoma cells. Cancer Res. 2005;65(13):5607–5619. doi: 10.1158/0008-5472.CAN-05-0500. [DOI] [PubMed] [Google Scholar]
- 140.Del Valle L, Enam S, Lassak A, et al. Insulin-like growth factor I receptor activity in human medulloblastomas. Clin Cancer Res. 2002;8(6):1822–1830. [PubMed] [Google Scholar]
- 141.Schuller U, Koch A, Hartmann W, et al. Subtype-specific expression and genetic alterations of the chemokinereceptor gene CXCR4 in medulloblastomas. Int J Cancer. 2005;117(1):82–89. doi: 10.1002/ijc.21116. [DOI] [PubMed] [Google Scholar]
- 142.Gilbertson RJ, Clifford SC. PDGFRB is overexpressed in metastatic medulloblastoma. Nat Genet. 2003;35(3):197–198. doi: 10.1038/ng1103-197. [DOI] [PubMed] [Google Scholar]
- 143.Boon K, Eberhart CG, Riggins GJ. Genomic amplification of orthodenticle homologue 2 in medulloblastomas. Cancer Res. 2005;65(3):703–707. [PubMed] [Google Scholar]
- 144.Michiels EM, Oussoren E, Van Groenigen M, et al. Genes differentially expressed in medulloblastoma and fetal brain. Physiol Genomics. 1999;1(2):83–91. doi: 10.1152/physiolgenomics.1999.1.2.83. [DOI] [PubMed] [Google Scholar]
- 145.Salsano E, Pollo B, Eoli M, et al. Expression of MATH1, a marker of cerebellar granule cell progenitors, identifies different medulloblastoma sub-types. Neurosci Lett. 2004;370(2–3):180–185. doi: 10.1016/j.neulet.2004.08.053. [DOI] [PubMed] [Google Scholar]
- 146.Ohta T, Watanabe T, Katayama Y, et al. TrkA expression is associated with an elevated level of apoptosis in classic medulloblastomas. Neuropathology. 2006;26(3):170–177. doi: 10.1111/j.1440-1789.2006.00678.x. [DOI] [PubMed] [Google Scholar]
- 147.Grotzer MA, Janss AJ, Fung K, et al. TrkC expression predicts good clinical outcome in primitive neuroectodermal brain tumors. J Clin Oncol. 2000;18(5):1027–1035. doi: 10.1200/JCO.2000.18.5.1027. [DOI] [PubMed] [Google Scholar]
- 148.Segal RA, Goumnerova LC, Kwon YK, et al. Expression of the neurotrophin receptor TrkC is linked to a favorable outcome in medulloblastoma. Proc Natl Acad Sci U S A. 1994;91(26):12867–12871. doi: 10.1073/pnas.91.26.12867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Korshunov A, Golanov A, Timirgaz V. Immunohistochemical markers for prognosis of ependymal neoplasms. J Neurooncol. 2002;58(3):255–270. doi: 10.1023/a:1016222202230. [DOI] [PubMed] [Google Scholar]
- 150.Sinnappah-Kang ND, Mrak RE, Paulsen DB, et al. Heparanase expression and TrkC/p75NTR ratios in human medulloblastoma. Clin Exp Metastasis. 2006;23(1):55–63. doi: 10.1007/s10585-006-9017-y. [DOI] [PubMed] [Google Scholar]
- 151.Sinnappah-Kang ND, Kaiser AJ, Blust BE, et al. Heparanase, TrkC and p75NTR: their functional involvement in human medulloblastoma cell invasion. Int J Oncol. 2005;27(3):617–626. [PubMed] [Google Scholar]
- 152.Salsano E, Croci L, Maderna E, et al. Expression of the neurogenic basic helix-loop-helix transcription factor NEUROG1 identifies a subgroup of medulloblastomas not expressing ATOH1. Neuro-Oncology. 2007;9(3):298–307. doi: 10.1215/15228517-2007-014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Rostomily RC, Bermingham-McDonogh O, Berger MS, et al. Expression of neurogenic basic helix-loop-helix genes in primitive neuroectodermal tumors. Cancer Res. 1997;57(16):3526–3531. [PubMed] [Google Scholar]
- 154.Katsetos CD, Herman MM, Krishna L, et al. Calbindin-D28k in subsets of medulloblastomas and in the human medulloblastoma cell line D283 Med. Arch Pathol Lab Med. 1995;119(8):734–743. [PubMed] [Google Scholar]
- 155.Adesina AM, Nalbantoglu J, Cavenee WK. p53 gene mutation and mdm2 gene amplification are uncommon in medulloblastoma. Cancer Res. 1994;54(21):5649–5651. [PubMed] [Google Scholar]
- 156.Saylors RL, 3rd, Sidransky D, Friedman HS, et al. Infrequent p53 gene mutations in medulloblastomas. Cancer Res. 1991;51(17):4721–4723. [PubMed] [Google Scholar]
- 157.Raffel C, Thomas GA, Tishler DM, et al. Absence of p53 mutations in childhood central nervous system primitive neuroectodermal tumors. Neurosurgery. 1993;33(2):301–306. doi: 10.1227/00006123-199308000-00018. [DOI] [PubMed] [Google Scholar]
- 158.Nozaki M, Tada M, Matsumoto R, et al. Rare occurrence of inactivating p53 gene mutations in primary non-astrocytic tumors of the central nervous system: reappraisal by yeast functional assay. Acta Neuropathol. 1998;95(3):291–296. doi: 10.1007/s004010050800. [DOI] [PubMed] [Google Scholar]
- 159.Kozmik Z, Sure U, Ruedi D, et al. Deregulated expression of PAX5 in medulloblastoma. Proc Natl Acad Sci U S A. 1995;92(12):5709–5713. doi: 10.1073/pnas.92.12.5709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Giordana MT, Duo D, Gasverde S, et al. MDM2 overexpression is associated with short survival in adults with medulloblastoma. Neuro-Oncology. 2002;4(2):115–122. doi: 10.1093/neuonc/4.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Lindsey JC, Lusher ME, Anderton JA, et al. Identification of tumour-specific epigenetic events in medulloblastoma development by hypermethylation profiling. Carcinogenesis. 2004;25(5):661–668. doi: 10.1093/carcin/bgh055. [DOI] [PubMed] [Google Scholar]
- 162.Rood BR, Zhang H, Weitman DM, et al. Hypermethylation of HIC-1 and 17p allelic loss in medulloblastoma. Cancer Res. 2002;62(13):3794–3797. [PubMed] [Google Scholar]
- 163.De Bortoli M, Castellino RC, Lu XY, et al. Medulloblastoma outcome is adversely associated with overexpression of EEF1D, RPL30, and RPS20 on the long arm of chromosome 8. BMC Cancer. 2006;6:223. doi: 10.1186/1471-2407-6-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.de Bont JM, den Boer ML, Kros JM, et al. Identification of novel biomarkers in pediatric primitive neuroectodermal tumors and ependymomas by proteome-wide analysis. J Neuropathol Exp Neurol. 2007;66(6):505–516. doi: 10.1097/01.jnen.0000240475.35414.c3. [DOI] [PubMed] [Google Scholar]
- 165.Yoshimoto M, Bayani J, Nuin PA, et al. Metaphase and array comparative genomic hybridization: unique copy number changes and gene amplification of medulloblastomas in South America. Cancer Genet Cytogenet. 2006;170(1):40–47. doi: 10.1016/j.cancergencyto.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 166.Fan X, Wang Y, Kratz J, et al. hTERT gene amplification and increased mRNA expression in central nervous system embryonal tumors. Am J Pathol. 2003;162(6):1763–1769. doi: 10.1016/S0002-9440(10)64311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Waha A, Koch A, Hartmann W, et al. SGNE1/7B2 is epigenetically altered and transcriptionally downregulated in human medulloblastomas. Oncogene. 2007;26(38):5662–5668. doi: 10.1038/sj.onc.1210338. [DOI] [PubMed] [Google Scholar]
- 168.Ebinger M, Senf L, Wachowski O, et al. Promoter methylation pattern of caspase-8, P16INK4A, MGMT, TIMP-3, and E-cadherin in medulloblastoma. Pathol Oncol Res. 2004;10(1):17–21. doi: 10.1007/BF02893403. [DOI] [PubMed] [Google Scholar]
- 169.Zuzak TJ, Steinhoff DF, Sutton LN, et al. Loss of caspase-8 mRNA expression is common in childhood primitive neuroectodermal brain tumour/medulloblastoma. Eur J Cancer. 2002;38(1):83–91. doi: 10.1016/s0959-8049(01)00355-0. [DOI] [PubMed] [Google Scholar]
- 170.Pingoud-Meier C, Lang D, Janss AJ, et al. Loss of caspase-8 protein expression correlates with unfavorable survival outcome in childhood medulloblastoma. Clin Cancer Res. 2003;9(17):6401–6409. [PubMed] [Google Scholar]
- 171.Gonzalez-Gomez P, Bello MJ, Inda MM, et al. Deletion and aberrant CpG island methylation of caspase 8 gene in medulloblastoma. Oncol Rep. 2004;12(3):663–666. [PubMed] [Google Scholar]
- 172.Muhlisch J, Bajanowski T, Rickert CH, et al. Frequent but borderline methylation of p16 (INK4a) and TIMP3 in medulloblastoma and sPNET revealed by quantitative analyses. J Neurooncol. 2007 doi: 10.1007/s11060-006-9309-8. [DOI] [PubMed] [Google Scholar]
- 173.Fruhwald MC, O’Dorisio MS, Dai Z, et al. Aberrant promoter methylation of previously unidentified target genes is a common abnormality in medulloblastomas—implications for tumor biology and potential clinical utility. Oncogene. 2001;20(36):5033–5042. doi: 10.1038/sj.onc.1204613. [DOI] [PubMed] [Google Scholar]
- 174.Uziel T, Zindy F, Sherr CJ, et al. The CDK inhibitor p18Ink4c is a tumor suppressor in medulloblastoma. Cell Cycle. 2006;5(4):363–365. doi: 10.4161/cc.5.4.2475. [DOI] [PubMed] [Google Scholar]
- 175.Lindsey JC, Lusher ME, Anderton JA, et al. Epigenetic deregulation of multiple S100 gene family members by differential hypomethylation and hypermethylation events in medulloblastoma. Br J Cancer. 2007;97(2):267–274. doi: 10.1038/sj.bjc.6603852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Lindsey JC, Lusher ME, Strathdee G, et al. Epigenetic inactivation of MCJ (DNAJD1) in malignant paediatric brain tumours. Int J Cancer. 2006;118(2):346–352. doi: 10.1002/ijc.21353. [DOI] [PubMed] [Google Scholar]
- 177.Gonzalez-Gomez P, Bello MJ, Alonso ME, et al. CpG island methylation status and mutation analysis of the RB1 gene essential promoter region and protein-binding pocket domain in nervous system tumours. Br J Cancer. 2003;88(1):109–114. doi: 10.1038/sj.bjc.6600737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Vibhakar R, Foltz G, Yoon JG, et al. Dickkopf-1 is an epigenetically silenced candidate tumor suppressor gene in medulloblastoma. Neuro-Oncology. 2007;9(2):135–144. doi: 10.1215/15228517-2006-038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Gilbertson RJ, Bentley L, Hernan R, et al. ERBB receptor signaling promotes ependymoma cell proliferation and represents a potential novel therapeutic target for this disease. Clin Cancer Res. 2002;8(10):3054–3064. [PubMed] [Google Scholar]
- 180.Ogino S, Kubo S, Abdul-Karim FW, et al. Comparative immunohistochemical study of insulin-like growth factor II and insulin-like growth factor receptor type 1 in pediatric brain tumors. Pediatr Dev Pathol. 2001;4(1):23–31. doi: 10.1007/s100240010112. [DOI] [PubMed] [Google Scholar]
- 181.Korshunov A, Neben K, Wrobel G, et al. Gene expression patterns in ependymomas correlate with tumor location, grade, and patient age. Am J Pathol. 2003;163(5):1721–1727. doi: 10.1016/S0002-9440(10)63530-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Rubio MP, Correa KM, Ramesh V, et al. Analysis of the neurofibromatosis 2 gene in human ependymomas and astrocytomas. Cancer Res. 1994;54(1):45–47. [PubMed] [Google Scholar]
- 183.Birch BD, Johnson JP, Parsa A, et al. Frequent type 2 neurofibromatosis gene transcript mutations in sporadic intramedullary spinal cord ependymomas. Neurosurgery. 1996;39(1):135–140. doi: 10.1097/00006123-199607000-00026. [DOI] [PubMed] [Google Scholar]
- 184.Ebert C, von Haken M, Meyer-Puttlitz B, et al. Molecular genetic analysis of ependymal tumors. NF2 mutations and chromosome 22q loss occur preferentially in intramedullary spinal ependymomas. Am J Pathol. 1999;155(2):627–632. doi: 10.1016/S0002-9440(10)65158-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Michalowski MB, de Fraipont F, Michelland S, et al. Methylation of RASSF1A and TRAIL pathway-related genes is frequent in childhood intracranial ependymomas and benign choroid plexus papilloma. Cancer Genet Cytogenet. 2006;166(1):74–81. doi: 10.1016/j.cancergencyto.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 186.Alonso ME, Bello MJ, Gonzalez-Gomez P, et al. Aberrant CpG island methylation of multiple genes in ependymal tumors. J Neurooncol. 2004;67(1–2):159–165. doi: 10.1023/b:neon.0000021862.41799.f7. [DOI] [PubMed] [Google Scholar]
- 187.Urioste M, Martinez-Ramirez A, Cigudosa JC, et al. Complex cytogenetic abnormalities including telomeric associations and MEN1 mutation in a pediatric ependymoma. Cancer Genet Cytogenet. 2002;138(2):107–110. doi: 10.1016/s0165-4608(01)00532-5. [DOI] [PubMed] [Google Scholar]
- 188.Rushing EJ, Yashima K, Brown DF, et al. Expression of telomerase RNA component correlates with the MIB-1 proliferation index in ependymomas. J Neuropathol Exp Neurol. 1997;56(10):1142–1146. doi: 10.1097/00005072-199710000-00008. [DOI] [PubMed] [Google Scholar]
- 189.Tong CY, Ng HK, Pang JC, et al. Molecular genetic analysis of non-astrocytic gliomas. Histopathology. 1999;34(4):331–341. doi: 10.1046/j.1365-2559.1999.00603.x. [DOI] [PubMed] [Google Scholar]
- 190.Gaspar N, Grill J, Geoerger B, et al. p53 Pathway dysfunction in primary childhood ependymomas. Pediatr Blood Cancer. 2006;46(5):604–613. doi: 10.1002/pbc.20532. [DOI] [PubMed] [Google Scholar]
- 191.von Haken MS, White EC, Daneshvar-Shyesther L, et al. Molecular genetic analysis of chromosome arm 17p and chromosome arm 22q DNA sequences in sporadic pediatric ependymomas. Genes Chromosomes Cancer. 1996;17(1):37–44. doi: 10.1002/(SICI)1098-2264(199609)17:1<37::AID-GCC6>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 192.Fink KL, Rushing EJ, Schold SC, Jr, et al. Infrequency of p53 gene mutations in ependymomas. J Neurooncol. 1996;27(2):111–115. doi: 10.1007/BF00177473. [DOI] [PubMed] [Google Scholar]
- 193.Suzuki SO, Iwaki T. Amplification and overexpression of mdm2 gene in ependymomas. Mod Pathol. 2000;13(5):548–553. doi: 10.1038/modpathol.3880095. [DOI] [PubMed] [Google Scholar]
- 194.Loiseau H, Arsaut J, Demotes-Mainard J. p73 gene transcripts in human brain tumors: overexpression and altered splicing in ependymomas. Neurosci Lett. 1999;263(2–3):173–176. doi: 10.1016/s0304-3940(99)00130-5. [DOI] [PubMed] [Google Scholar]
- 195.Kamiya M, Nakazato Y. The expression of p73, p21 and MDM2 proteins in gliomas. J Neurooncol. 2002;59(2):143–149. doi: 10.1023/a:1019633910603. [DOI] [PubMed] [Google Scholar]
- 196.Hamilton DW, Lusher ME, Lindsey JC, et al. Epigenetic inactivation of the RASSF1A tumour suppressor gene in ependymoma. Cancer Lett. 2005;227(1):75–81. doi: 10.1016/j.canlet.2004.11.044. [DOI] [PubMed] [Google Scholar]
- 197.Alonso ME, Bello MJ, Gonzalez-Gomez P, et al. Aberrant promoter methylation of multiple genes in oligodendrogliomas and ependymomas. Cancer Genet Cytogenet. 2003;144(2):134–142. doi: 10.1016/s0165-4608(02)00928-7. [DOI] [PubMed] [Google Scholar]
- 198.Rousseau E, Ruchoux MM, Scaravilli F, et al. CDKN2A, CDKN2B and p14ARF are frequently and differentially methylated in ependymal tumours. Neuropathol Appl Neurobiol. 2003;29(6):574–583. doi: 10.1046/j.0305-1846.2003.00505.x. [DOI] [PubMed] [Google Scholar]
- 199.Waha A, Koch A, Hartmann W, et al. Analysis of HIC-1 methylation and transcription in human ependymomas. Int J Cancer. 2004;110(4):542–549. doi: 10.1002/ijc.20165. [DOI] [PubMed] [Google Scholar]
- 200.Bhattacharjee MB, Armstrong DD, Vogel H, et al. Cytogenetic analysis of 120 primary pediatric brain tumors and literature review. Cancer Genet Cytogenet. 1997;97(1):39–53. doi: 10.1016/s0165-4608(96)00330-5. [DOI] [PubMed] [Google Scholar]
- 201.Neumann E, Kalousek DK, Norman MG, et al. Cytogenetic analysis of 109 pediatric central nervous system tumors. Cancer Genet Cytogenet. 1993;71(1):40–49. doi: 10.1016/0165-4608(93)90200-6. [DOI] [PubMed] [Google Scholar]
- 202.Bayani J, Zielenska M, Marrano P, et al. Molecular cytogenetic analysis of medulloblastomas and supratentorial primitive neuroectodermal tumors by using conventional banding, comparative genomic hybridization, and spectral karyotyping. J Neurosurg. 2000;93(3):437–448. doi: 10.3171/jns.2000.93.3.0437. [DOI] [PubMed] [Google Scholar]
- 203.Stratton MR, Darling J, Lantos PL, et al. Cytogenetic abnormalities in human ependymomas. Int J Cancer. 1989;44(4):579–581. doi: 10.1002/ijc.2910440403. [DOI] [PubMed] [Google Scholar]
- 204.Bigner SH, McLendon RE, Fuchs H, et al. Chromosomal characteristics of childhood brain tumors. Cancer Genet Cytogenet. 1997;97(2):125–134. doi: 10.1016/s0165-4608(96)00404-9. [DOI] [PubMed] [Google Scholar]
- 205.Biegel JA, Rorke LB, Janss AJ, et al. Isochromosome 17q demonstrated by interphase fluorescence in situ hybridization in primitive neuroectodermal tumors of the central nervous system. Genes Chromosomes Cancer. 1995;14(2):85–96. doi: 10.1002/gcc.2870140202. [DOI] [PubMed] [Google Scholar]
- 206.Vagner-Capodano AM, Zattara-Cannoni H, Gambarelli D, et al. Cytogenetic study of 33 ependymomas. Cancer Genet Cytogenet. 1999;115(2):96–99. doi: 10.1016/s0165-4608(99)00080-1. [DOI] [PubMed] [Google Scholar]
- 207.Cohen N, Betts DR, Tavori U, et al. Karyotypic evolution pathways in medulloblastoma/primitive neuroectodermal tumor determined with a combination of spectral karyotyping, G-banding, and fluorescence in situ hybridization. Cancer Genet Cytogenet. 2004;149(1):44–52. doi: 10.1016/S0165-4608(03)00285-1. [DOI] [PubMed] [Google Scholar]
- 208.Vagner-Capodano AM, Zattara-Cannoni H, Gambarelli D, et al. Detection of i(17q) chromosome by fluorescent in situ hybridization (FISH) with interphase nuclei in medulloblastoma. Cancer Genet Cytogenet. 1994;78(1):1–6. doi: 10.1016/0165-4608(94)90037-x. [DOI] [PubMed] [Google Scholar]
- 209.Ransom DT, Ritland SR, Kimmel DW, et al. Cytogenetic and loss of heterozygosity studies in ependymomas, pilocytic astrocytomas, and oligodendrogliomas. Genes Chromosomes Cancer. 1992;5(4):348–356. doi: 10.1002/gcc.2870050411. [DOI] [PubMed] [Google Scholar]
- 210.Chadduck WM, Boop FA, Sawyer JR. Cytogenetic studies of pediatric brain and spinal cord tumors. Pediatr Neurosurg. 1991;17(2):57–65. doi: 10.1159/000120569. [DOI] [PubMed] [Google Scholar]
- 211.Vagner-Capodano AM, Gentet JC, Gambarelli D, et al. Cytogenetic studies in 45 pediatric brain tumors. Pediatr Hematol Oncol. 1992;9(3):223–235. doi: 10.3109/08880019209016590. [DOI] [PubMed] [Google Scholar]
- 212.Weremowicz S, Kupsky WJ, Morton CC, et al. Cytogenetic evidence for a chromosome 22 tumor suppressor gene in ependymoma. Cancer Genet Cytogenet. 1992;61(2):193–196. doi: 10.1016/0165-4608(92)90085-m. [DOI] [PubMed] [Google Scholar]
- 213.Rogatto SR, Casartelli C, Rainho CA, et al. Chromosomes in the genesis and progression of ependymomas. Cancer Genet Cytogenet. 1993;69(2):146–152. doi: 10.1016/0165-4608(93)90093-2. [DOI] [PubMed] [Google Scholar]
- 214.Agamanolis DP, Malone JM. Chromosomal abnormalities in 47 pediatric brain tumors. Cancer Genet Cytogenet. 1995;81(2):125–134. doi: 10.1016/0165-4608(94)00123-s. [DOI] [PubMed] [Google Scholar]
- 215.Yamada K, Kasama M, Kondo T, et al. Chromosome studies in 70 brain tumors with special attention to sex chromosome loss and single autosomal trisomy. Cancer Genet Cytogenet. 1994;73(1):46–52. doi: 10.1016/0165-4608(94)90180-5. [DOI] [PubMed] [Google Scholar]
- 216.Mazewski C, Soukup S, Ballard E, et al. Karyotype studies in 18 ependymomas with literature review of 107 cases. Cancer Genet Cytogenet. 1999;113(1):1–8. doi: 10.1016/s0165-4608(99)00046-1. [DOI] [PubMed] [Google Scholar]
- 217.Sawyer JR, Miller JP, Ellison DA. Clonal telomeric fusions and chromosome instability in a subcutaneous sacrococcygeal myxopapillary ependymoma. Cancer Genet Cytogenet. 1998;100(2):169–175. doi: 10.1016/s0165-4608(97)00055-1. [DOI] [PubMed] [Google Scholar]
- 218.Sainati L, Bolcato S, Montaldi A, et al. Cytogenetics of pediatric central nervous system tumors. Cancer Genet Cytogenet. 1996;91(1):13–27. doi: 10.1016/s0165-4608(96)00036-2. [DOI] [PubMed] [Google Scholar]
- 219.Pearson AD, Reid MM, Davison EV, et al. Cytogenetic investigations of solid tumours of children. Arch Dis Child. 1988;63(9):1012–1015. doi: 10.1136/adc.63.9.1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Dal Cin P, Sandberg AA. Cytogenetic findings in a supratentorial ependymoma. Cancer Genet Cytogenet. 1988;30(2):289–293. doi: 10.1016/0165-4608(88)90197-5. [DOI] [PubMed] [Google Scholar]
- 221.Karnes PS, Tran TN, Cui MY, et al. Cytogenetic analysis of 39 pediatric central nervous system tumors. Cancer Genet Cytogenet. 1992;59(1):12–19. doi: 10.1016/0165-4608(92)90150-7. [DOI] [PubMed] [Google Scholar]
- 222.Thiel G, Losanowa T, Kintzel D, et al. Karyotypes in 90 human gliomas. Cancer Genet Cytogenet. 1992;58(2):109–120. doi: 10.1016/0165-4608(92)90095-p. [DOI] [PubMed] [Google Scholar]
- 223.Roberts P, Chumas PD, Picton S, et al. A review of the cytogenetics of 58 pediatric brain tumors. Cancer Genet Cytogenet. 2001;131(1):1–12. doi: 10.1016/s0165-4608(01)00483-6. [DOI] [PubMed] [Google Scholar]
- 224.Avet-Loiseau H, Venuat AM, Terrier-Lacombe MJ, et al. Comparative genomic hybridization detects many recurrent imbalances in central nervous system primitive neuroectodermal tumours in children. Br J Cancer. 1999;79(11–12):1843–1847. doi: 10.1038/sj.bjc.6690293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Eberhart CG, Kratz JE, Schuster A, et al. Comparative genomic hybridization detects an increased number of chromosomal alterations in large cell/anaplastic medulloblastomas. Brain Pathol. 2002;12(1):36–44. doi: 10.1111/j.1750-3639.2002.tb00420.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Nishizaki T, Harada K, Kubota H, et al. Genetic alterations in pediatric medulloblastomas detected by comparative genomic hybridization. Pediatr Neurosurg. 1999;31(1):27–32. doi: 10.1159/000028827. [DOI] [PubMed] [Google Scholar]
- 227.Gilhuis HJ, Anderl KL, Boerman RH, et al. Comparative genomic hybridization of medulloblastomas and clinical relevance: eleven new cases and a review of the literature. Clin Neurol Neurosurg. 2000;102(4):203–209. doi: 10.1016/s0303-8467(00)00112-8. [DOI] [PubMed] [Google Scholar]
- 228.Inda MM, Perot C, Guillaud-Bataille M, et al. Genetic heterogeneity in supratentorial and infratentorial primitive neuroectodermal tumours of the central nervous system. Histopathology. 2005;47(6):631–637. doi: 10.1111/j.1365-2559.2005.02304.x. [DOI] [PubMed] [Google Scholar]
- 229.Reardon DA, Michalkiewicz E, Boyett JM, et al. Extensive genomic abnormalities in childhood medulloblastoma by comparative genomic hybridization. Cancer Res. 1997;57(18):4042–4047. [PubMed] [Google Scholar]
- 230.Shlomit R, Ayala AG, Michal D, et al. Gains and losses of DNA sequences in childhood brain tumors analyzed by comparative genomic hybridization. Cancer Genet Cytogenet. 2000;121(1):67–72. doi: 10.1016/s0165-4608(00)00218-1. [DOI] [PubMed] [Google Scholar]
- 231.Michiels EM, Weiss MM, Hoovers JM, et al. Genetic alterations in childhood medulloblastoma analyzed by comparative genomic hybridization. J Pediatr Hematol Oncol. 2002;24(3):205–210. doi: 10.1097/00043426-200203000-00009. [DOI] [PubMed] [Google Scholar]
- 232.Russo C, Pellarin M, Tingby O, et al. Comparative genomic hybridization in patients with supratentorial and infratentorial primitive neuroectodermal tumors. Cancer. 1999;86(2):331–339. doi: 10.1002/(sici)1097-0142(19990715)86:2<331::aid-cncr18>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 233.Brown HG, Kepner JL, Perlman EJ, et al. “Large cell/anaplastic” medulloblastomas: a Pediatric Oncology Group study. J Neuropathol Exp Neurol. 2000;59(10):857–865. doi: 10.1093/jnen/59.10.857. [DOI] [PubMed] [Google Scholar]
- 234.Jay V, Squire J, Bayani J, et al. Oncogene amplification in medulloblastoma: analysis of a case by comparative genomic hybridization and fluorescence in situ hybridization. Pathology. 1999;31(4):337–344. doi: 10.1080/003130299104693. [DOI] [PubMed] [Google Scholar]
- 235.Tong CY, Hui AB, Yin XL, et al. Detection of oncogene amplifications in medulloblastomas by comparative genomic hybridization and array-based comparative genomic hybridization. J Neurosurg. 2004;100(2 suppl Pediatrics):187–193. doi: 10.3171/ped.2004.100.2.0187. [DOI] [PubMed] [Google Scholar]
- 236.Nicholson J, Wickramasinghe C, Ross F, et al. Imbalances of chromosome 17 in medulloblastomas determined by comparative genomic hybridisation and fluorescence in situ hybridisation. Mol Pathol. 2000;53(6):313–319. doi: 10.1136/mp.53.6.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Gilhuis HJ, van der Laak J, Wesseling P, et al. Inverse correlation between genetic aberrations and malignancy grade in ependymal tumors: a paradox? J Neurooncol. 2004;66(1–2):111–116. doi: 10.1023/b:neon.0000013493.31107.20. [DOI] [PubMed] [Google Scholar]
- 238.Reardon DA, Entrekin RE, Sublett J, et al. Chromosome arm 6q loss is the most common recurrent autosomal alteration detected in primary pediatric ependymoma. Genes Chromosomes Cancer. 1999;24(3):230–237. doi: 10.1002/(sici)1098-2264(199903)24:3<230::aid-gcc8>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 239.Ward S, Harding B, Wilkins P, et al. Gain of 1q and loss of 22 are the most common changes detected by comparative genomic hybridisation in paediatric ependymoma. Genes Chromosomes Cancer. 2001;32(1):59–66. doi: 10.1002/gcc.1167. [DOI] [PubMed] [Google Scholar]
- 240.Grill J, Avet-Loiseau H, Lellouch-Tubiana A, et al. Comparative genomic hybridization detects specific cytogenetic abnormalities in pediatric ependymomas and choroid plexus papillomas. Cancer Genet Cytogenet. 2002;136(2):121–125. doi: 10.1016/s0165-4608(02)00516-2. [DOI] [PubMed] [Google Scholar]
- 241.Carter M, Nicholson J, Ross F, et al. Genetic abnormalities detected in ependymomas by comparative genomic hybridisation. Br J Cancer. 2002;86(6):929–939. doi: 10.1038/sj.bjc.6600180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Scheil S, Bruderlein S, Eicker M, et al. Low frequency of chromosomal imbalances in anaplastic ependymomas as detected by comparative genomic hybridization. Brain Pathol. 2001;11(2):133–143. doi: 10.1111/j.1750-3639.2001.tb00386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Zheng PP, Pang JC, Hui AB, et al. Comparative genomic hybridization detects losses of chromosomes 22 and 16 as the most common recurrent genetic alterations in primary ependymomas. Cancer Genet Cytogenet. 2000;122(1):18–25. doi: 10.1016/s0165-4608(00)00265-x. [DOI] [PubMed] [Google Scholar]
- 244.Rickert CH, Korshunov A, Paulus W. Chromosomal imbalances in clear cell ependymomas. Mod Pathol. 2006;19(7):958–962. doi: 10.1038/modpathol.3800614. [DOI] [PubMed] [Google Scholar]
- 245.Granzow M, Popp S, Weber S, et al. Isochromosome 1q as an early genetic event in a child with intracranial ependymoma characterized by molecular cytogenetics. Cancer Genet Cytogenet. 2001;130(1):79–83. doi: 10.1016/s0165-4608(01)00465-4. [DOI] [PubMed] [Google Scholar]
- 246.Schutz BR, Scheurlen W, Krauss J, et al. Mapping of chromosomal gains and losses in primitive neuroectodermal tumors by comparative genomic hybridization. Genes Chromosomes Cancer. 1996;16(3):196–203. doi: 10.1002/(SICI)1098-2264(199607)16:3<196::AID-GCC7>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]