This report describes a type of ɛγγδβ-thalassemia due to a rare private deletion, detected early and successfully treated with intrauterine blood transfusions.
Keywords: intrauterine anemia, thalassemia, Norwegian family
Abstract
Severe intrauterine anemia of unknown cause presents a diagnostic challenge. We describe a Norwegian case, managed successfully by intrauterine transfusions, that further investigations demonstrated to be due to a rare type of thalassemia. A deletion of the 5’ end of the β globin gene cluster was characterized, the breakpoints sequenced and a new type of ɛγγδβ thalassemia identified. This case highlights the need to consider diagnoses of rare conditions not normally associated with a particular population.
Introduction
Early detection, prevention and treatment of rhesus hemolytic disease has removed a major cause of severe intrauterine anemia, but the diagnosis in cases of uncertain etiology is frequently a challenge. Identifying the underlying cause and pinpointing the disorder responsible may be extremely difficult. Here we describe a Norwegian family with severe neonatal anemia across two generations due to a rare form of β thalassemia, a disease that is extremely uncommon (<0.1%) in this population.
Design and Methods
Hematologic data, hemoglobin electrophoresis and other investigations followed standard procedures. Lympho-blastoid cell lines were prepared from the peripheral blood of the parents and, after birth, from the proband by EBV transformation.
Multiplex ligation-dependent probe amplification (MPLA)1 was carried out with probe sets obtained from MRC-Holland b.v., Amsterdam (P102 SALSA probemix) and ServiceXS, Leiden (β-globinXS-MPLA probemix) according to the manufacturer’s instructions.
Southern blotting followed standard procedures using probes for the β globin gene and a probe (probe 45) made by PCR of sequences between the closest intact and deleted MPLA probes (fwd primer TGGGTAATGGAGGTGATGCCTG, rev primer CACAAGGAGAAGCAGAGAGAGAGG). The junction fragment across the deletion was amplified using primers (fwd TTTTTGTTGTGTCTCTGCCCG and rev GGGACATCTAACTGTTTCTGCCTG) and sequenced on an ABI 3100 DNA sequencer.
Case report
A 24-year old primigravida, with a family history of juvenile polycystic kidney disease, was examined by ultrasound at 29+1 weeks’ gestation. The fetus was hydropic with extensive ascites and pericardial fluid, an enlarged heart and a hyperkinetic circulation. Maximum velocity in the middle cerebral artery was 76 cm/s. The etiology of these findings consistent with fetal anemia, was unknown. The pretransfusion blood sample showed a Hb of 5.8 g/dL, Hct 0.19, MCV 91 fL, MCH 28 pg, reticulocytes 30.8% (0.6×1012/L) and a platelet count of 247×109/L. The blood film showed marked anisopoikilocytosis with target cells and Hb electrophoresis an unusually high proportion of HbA (HbF 82.7%, HbA 15.9%, HbA2 1.4%). A Coombs test was negative as were tests for CMV, Herpes and Parvo virus. The karyotype was normal. The extended test for immunization was normal and no fetomaternal transfusion was identified. The finding of microcytic anemia in the fetus and the history of microcytic, hypochromic anemia in the father, led us to consider a hereditary anemia.
The fetus underwent 6 cordocenteses and blood transfusions over the following weeks, up to 34 weeks gestation. After the 4th transfusion, nine days following the first, the ascites and pericardial fluid disappeared, the heart normalized but hepatomegaly remained. A female infant was delivered by Caesarian section at 36 weeks’ gestation with a (transfused) Hb level of 13.6–14.1 g/dL over the first few days and a significantly enlarged liver. By one month of age her Hb had dropped to 8.8 g/dL, with MCV 78 fL, MCH 26 pg and platelets 706×109/L. She was transfused at this stage and at about two months; subsequently her Hb has been stable at about 9 g/dL. Her physical and neurological development has been normal and at two years she is healthy with a stable microcytic anemia. Her most recent blood count showed a Hb of 9.8 g/dL, MCV 55 fl, MCH 19 pg.
Family studies
The mother was a primagravida of pure Norwegian heritage. Hematologic studies showed normal red cell morphology, a normal blood count (Hb 11.3 g/dL, MCV 86 fL, MCH 29 pg), and normal Hb electrophoresis (HbA2=2.5%, HbF=0.5%). The father, of Swedish/Norwegian ancestry, had a microcytic hypochromic blood picture and blood tests at various times revealed a Hb of 12.9–13.5 g/dL, MCV=60–62 fL, MCH = 19–20 pg, a slightly raised reticulocte count (0.147×1012/L) and a platelet count of 321×109/L. On hemoglobin electrophoresis his HbA2 was normal at 3.0% as was his HbF of <0.5%. He had a serum iron of 23.6 mg/dL, TIBC 54 mg/dL and a normal ferritin level (187 ng/mL). His bone marrow was hypercellular with an increased erythroid component, a normal number of megakaryocytes and the absence of ring sideroblasts.
Further checking revealed that the father was anemic and severely thrombocytopenic at birth with hepatosplenomegaly, requiring transfusions at four days and two months. These symptoms had resolved by four months and further development was normal although the microcytic anemia persisted and its cause remained undiagnosed. None of his 5 siblings or their 10 offspring had any signs of anemia.
Molecular studies
The phenotype of a thalassemic picture with normal Hb A2 levels is characteristic of α thalassemia. To examine this possibility in the present family, PCR analysis of the common deletion alleles excluded the presence of the α-3.7, α-4.2, α-20.5, α-SEA, α-MED, α-FIL and αTHAI alleles. The absence of any α gene deletion was confirmed by MLPA.
A normal HbA2 thalassemia picture is also the phenotype of the ɛγγδβ thalassemias. Furthermore, this condition is frequently associated with quite severe anemia in infancy that spontaneously resolves during early childhood,2 similar to that seen in the proband and her father. As ɛγγδβ thalassemias are due to deletions that remove either the whole of the β globin cluster or at least the 5’ end that contains the LCR, we used MLPA to determine if the cluster was intact.
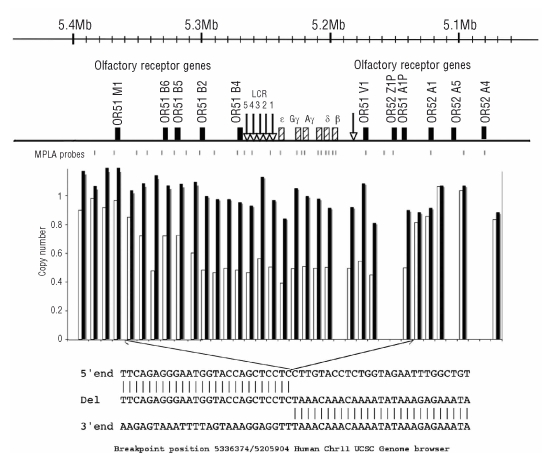
By using two sets of probe pairs spanning the cluster, a deletion was detected that started upstream in a region containing a series of olfactory receptor (OR) genes. The 5’ end of the deletion lay between OR5 1B6 and OR5 1M1. The deletion extended into the globin gene cluster with the 3’ end lying between the δ and β genes. It removed the LCR, the ɛ, Gγ, Aγ and δ globin genes sparing the β globin gene itself (Figure 1).
Figure 1.
Diagram to illustrate the structure of the β globin gene cluster and its surroundings together with the positions of all the MPLA probes used in the analysis. Below are the results of the relevant MLPA probes on the mother (black bars) and the propositus (white bars); note the 5’ end of the deletion was clearer on other MLPA analyses of both the propositus and her father. Bottom: the sequence of the junction fragment.
Southern blotting with a β globin gene probe narrowed the 3’ breakpoint to a region between the Hind II and Bgl II restriction sites while probe 45 from the 5’ breakpoint region showed the start point to lie between the MfeI and NheI restriction sites. PCR primers were chosen in the intact regions at both ends close to the suspected breakpoints and a 321bp fragment was amplified and directly sequenced. This demonstrated the 5’ breakpoint to lie at position 5336374 and the 3’ break at 5205904 of the UCSC human chromosome 11 genome browser, a deletion of 130.470kb. The 5’ breakpoint lay in an L1 repeat with no obvious homology to the 3’ breakpoint and no orphan nucleotides were present (Figure 1).
Analysis of the daughter’s DNA by MPLA and Southern blotting confirmed that she had inherited the deletion chromosome from her father.
Results and Discussion
ɛγγδβ thalassemia is a rare disorder with an adult phenotype of β thalassemia trait but with normal rather than elevated levels of HbA2. Many (14/18) of the previously published families3 have been described in Northern Europeans but this almost certainly reflects ascertainment bias, with such cases standing out in populations where the common forms of thalassemia are not prevalent.
The clinical presentation of ɛγγδβ thalassemia may be variable but marked neonatal anemia is the norm and neonatal transfusions are frequently required.4–6 The variable severity is likely to be influenced by other genetic and environmental factors, as shown by variability within a family, with one case requiring neonatal transfusion while 2 others had uneventful neonatal periods.5 In the present case, the severe and potentially life-threatening anemia was detected early and treated with intrauterine transfusions. Intrauterine transfusions were also given in 2 infants from a Chilean family6 and in a Dutch case.7 The severe presentation in the neonatal period that resolves during early childhood may reflect a limited response to anemia at this stage of development. It is also possible that neonatal red cell membranes are more susceptible to damage by excess α globin chains than adult membranes. This has not been directly examined but a more severe course in the neonatal period may also occur in some hereditary spherocytosis patients with spectrin and other membrane protein defects.8
The Norwegian deletion, like almost half of the previously described ɛγγδβ thalassemia cases, spares the β globin gene itself but the loss of the LCR leaves the gene inactive. The molecular deletion in each has been unique to the family in which it was found1,3 and the Norwegian case is no exception. This makes it likely that the condition is maintained by recurrent mutation and hence is a potential diagnosis even in populations not normally associated with thalassemia.
In prenatal cases, a thorough family history is important in that it may provide the suspicion of the potential diagnosis. Intrauterine transfusions should always be considered in cases with fetal anemia of unknown etiology while further investigation is being performed. A correct diagnosis not only provides a probable prognosis but also allows early prenatal diagnosis and optimal surveillance in future pregnancies.
Footnotes
Authorship and Disclosures
AB and SH-EN were responsible for the clinical investigation and clinical management of the patients, NR and CF carried out the molecular analyses under the supervision of WGW; AB, SE and WGW wrote the paper.
The authors reported no potential conflicts of interest.
References
- 1.Harteveld CL, Voskamp A, Phylipsen M, Akkermans N, den Dunnen JT, White SJ, et al. Nine unknown rearrangements in 16p13.3 and 11p15.4 causing α- and β-thalassaemia characterised by high resolution multiplex ligation-dependent probe amplification. J Med Genet. 2005;42:922–31. doi: 10.1136/jmg.2005.033597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weatherall DJ, Clegg JB. The thalassaemia syndromes. Blackwell Science; Oxford: 2001. [Google Scholar]
- 3.Rooks H, Bergounioux J, Game L, Close JP, Osborne C, Best S, et al. Heterogeneity of the ɛγδβ-thalassaemias: characterization of three novel English deletions. Br J Haematol. 2005;128:722–9. doi: 10.1111/j.1365-2141.2005.05368.x. [DOI] [PubMed] [Google Scholar]
- 4.Kan YW, Forget BG, Nathan DG. γ-β thalassemia: a cause of hemolytic disease of the newborn. N Engl J Med. 1972;286:129–34. doi: 10.1056/NEJM197201202860304. [DOI] [PubMed] [Google Scholar]
- 5.Trent RJ, Williams BG, Kearney A, Wilkinson T, Harris PC. Molecular and hematologic characterization of Scottish-Irish type (ɛγδβ)0 thalassemia. Blood. 1990;76:2132–8. [PubMed] [Google Scholar]
- 6.Game L, Bergounioux J, Close JP, Marzouka BE, Thein SL. A novel deletion causing (ɛγδβ) degrees thalassaemia in a Chilean family. Br J Haematol. 2003;123:154–9. doi: 10.1046/j.1365-2141.2003.04564.x. [DOI] [PubMed] [Google Scholar]
- 7.Harteveld CL, Osborne CS, Peters M, van der Werf S, Plug R, Fraser P, et al. Novel 112 kb (ɛGγAγ)δβ thalassemia deletion in a Dutch family. Br J Haematol. 2003;122:855–8. doi: 10.1046/j.1365-2141.2003.04505.x. [DOI] [PubMed] [Google Scholar]
- 8.Iolascon A, Avvisati RA. Genotype/phenotype correlation in hereditary spherocytosis. Haematologica. 2008;93:1283–8. doi: 10.3324/haematol.13344. [DOI] [PubMed] [Google Scholar]