This report characterizes the molecular genetic alterations harbored by neoplastic B cells in primary effusion lymphoma. By studying both cell lines and primary tumor samples, the authors show that mutations in P53 and CDKN2A/ARF although uncommon in clinical material, are associated with an EBV-negative immunophenotype
Keywords: human herpesvirus 8, non-Hodgkin’s lymphoma, primary effusion lymphoma, tumor suppressor gene, mutations
Abstract
Human herpesvirus 8 (HHV-8)-associated primary effusion lymphoma is a rare non-Hodgkin’s lymphoma often associated with Epstein-Barr virus (EBV) infection. Mutations in TP53, PTEN, PIK3CA, CTNNB1/β-catenin genes and deletion of CDKN2A-ARF (p14ARF-p16NK4a I ) locus were investigated in sixteen primary primary effusion lymphoma tumors and seven primary effusion lymphoma cell lines using PCR and sequencing. TP53 mutations were detected in one primary primary effusion lymphoma tumor (6.2%) and two primary effusion lymphoma cell lines (28.6%). BC-3 and BCP-1 cell lines showed PTEN gene mutations, associated with a loss of PTEN protein expression in both cases. No mutations were detected in PIK3CA and CTNNB1/β-catenin hotspot sequences. Only BC-3 contained a homozygous deletion of CDKN2A-ARF locus. Although detected at a higher frequency in primary effusion lymphoma cell lines than in primary primary effusion lymphoma tumors, TP53 and/or PTEN mutations, as well as deletion of CDKN2A-ARF locus are uncommon in primary effusion lymphoma, and are found to correlate with the EBV-negative status of primary effusion lymphoma tumors.
Introduction
Somatic mutations of tumor suppressor genes and oncogenes are among the most common genetic alterations found in human malignancies. Moreover, single nucleotide polymorphisms (SNP) in genes involved in apoptosis or cell cycle regulation have been shown to correlate with an increased risk of cancer development, an accelerated cancer onset, a poor response to treatment or a shorter survival. In this setting, a common SNP (rs1042522) in exon 4 of the TP53 gene, resulting in either Arginine or Proline at codon 72 of the proline-rich domain, has been reported to influence the ability of TP53 protein to induce apoptosis, the Arg72 variant being the most efficient apoptosis inducer.1 The SNP309 t/g (rs2279744) polymorphism identified in the promoter of MDM2 oncogene, which encodes the negative regulator of TP53, has been shown to influence DNA binding affinity of the transcriptional activator Sp1, leading to changes in MDM2 expression levels and attenuation of TP53 response. In sporadic cancers, including diffuse large B-cell lymphomas (DLBCL), the SNP309 g/g genotype has been found to correlate with an earlier age of tumor onset in female patients.2 In other studies however, neither MDM2 SNP309 nor TP53 SNP72 have been found to be associated with survival or age of tumor onset in patients with non-Hodgkin’s lymphoma (NHL).3,4
Primary effusion lymphoma (PEL) is a rare NHL which usually develops as lymphomatous effusions in the serous cavities of immunocompromised patients, especially Human Immunodeficiency Virus type-1 (HIV-1)-infected individuals and solid organ transplant recipients.5,6 PEL tumor cells display pleiomorphic morphology and frequently lack B-cell lineage antigen expression, despite their B-cell monoclonal origin. These cells are latently infected with HHV-8, and are in most cases co-infected with Epstein-Barr virus (EBV).7,8 The phosphatidylinositol 3’-kinase (PI3K)/AKT cascade has been identified as constitutively activated in PEL and critical for cell survival.9 This pathway is negatively regulated by the non-redondant lipid phosphatase PTEN (phosphatase and tensin homolog deleted on chromosome 10). Among the best known genetic alterations leading to the constitutive activation of PI3K/AKT cascade, the loss of PTEN tumor suppressor gene and the activating mutations of the p110 catalytic subunit of PI3K (PIK3CA) have been reported in many cancers including NHL.10–13 PEL tumor cells have been shown to express high levels of β-catenin, which is a downstream activator of the Wnt signaling pathway.14 Mutations in exon 3 of the CTNNB1/β-catenin gene resulting in the accumulation of β-catenin in the cytoplasm, have been found in several cancer types, including lymphoproliferative disorders developed in renal transplant recipients.15 A loss of CDKN2A/p16NK4a I protein expression has been reported in all primary PEL isolates analyzed. However, the molecular events leading to CDKN2A/p16INK4a gene silencing have only been identified in a few PEL cell lines.16 Since mutations of PTEN, PIK3CA, CTNNB1/β-catenin genes and deletion of CDKN2A-ARF (p14ARF-p16INK4a) locus had not been previously investigated in primary PEL tumors, we performed an extensive molecular analysis of mutations and SNP in a large series of PEL samples.
Design and Methods
The study included seven PEL cell lines and sixteen primary tumor samples (seven pleural effusions, eight ascites, one pericardial effusion) collected from 12 HIV-1-infected patients, 2 HIV-1-negative elderly individuals and 2 renal transplant recipients with HHV-8-associated PEL. All patients samples (Tables 1 and 2) were collected in accordance with the ethical regulations of our institution, as indicated in our previous studies.5,6 The clinical data were collected from the patients’ records by the same examiner (EB). Human acute lymphoblastic leukemia (ALL) cell lines of T (CEM) and B [DAUDI, RAJI, REH, RS(4;11)] cell lineage origins, and peripheral blood mononuclear cells (PBMCs) from Caucasian healthy donors, were used as controls. Mutations of TP53 (exons 4–11), PTEN (exons 1–9), PIK3CA (exons 9 and 20), CTNNB1/β-catenin (exon 3) genes and deletion of CDKN2A-ARF (p14ARF-p16INK4a) locus were detected by PCR and direct sequencing. SNP in several genes involved in apoptosis and cell cycle regulation including SNP72 and ins16bp in TP53, SNP309 in MDM2, S31R and 3'UTR (c70t) in CDKN1A/p21Cip1, V109G and 5'UTR (c79t) in CDKN1B/p27Kip1, g870a in CCND1/cyclin D1, A259S in CCND3/cyclin D3, F31I (t91a) in STK15/aurora A, R70C in CDC25C, A655V in CDC2L1 and I441V in CDC6 genes, were assessed by PCR.
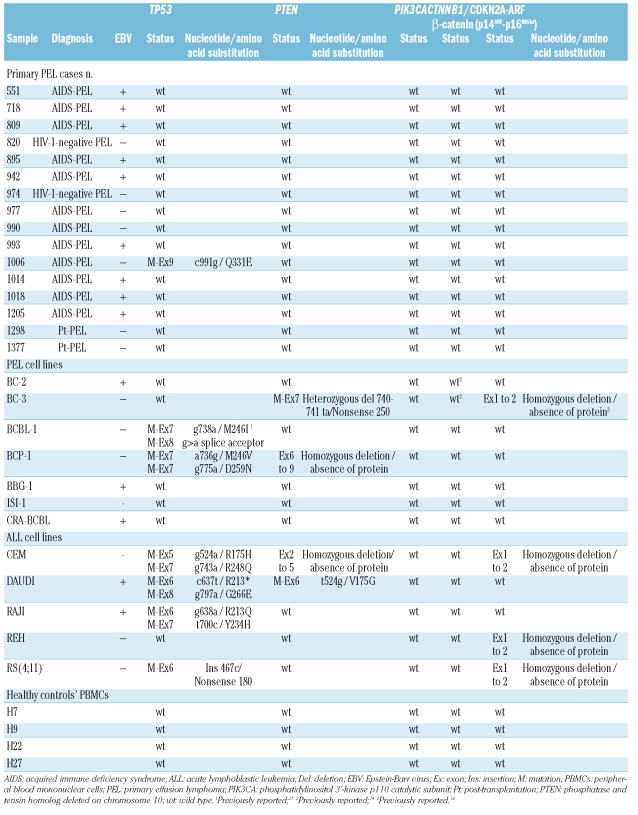
Table 1.
Analysis of mutations in oncogenes and tumor suppressor genes.
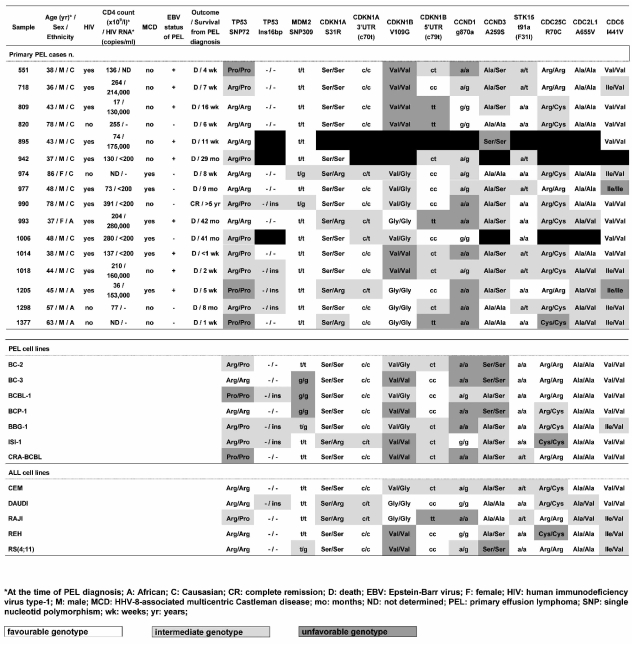
Table 2.
Analysis of single nucleotide polymorphisms in several genes involved in cell cycle regulation.
Results and Discussion
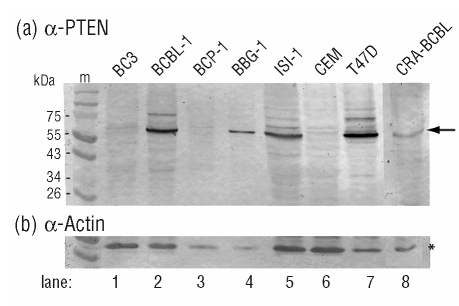
As previously observed,7,8 the frequency of TP53 gene mutations in PEL was found to be low, as they were detected in only one out of sixteen (6.2%) tumor samples and in two out of seven cell lines (28.6%, Table 1). In accordance with previous reports,17 BCBL-1 was found to harbor a heterozygous M246I mutation of TP53. BCP-1 contained two missense mutations leading to single nucleotide changes (M246V and D259N) in both alleles of exon 7. Only BC-3 contained a homozygous deletion of CDKN2A-ARF locus, in agreement with previous reports.16 No mutations were found in PIK3CA and CTNNB1/β-catenin hotspot sequences. PTEN gene alterations were identified in two PEL cell lines (Table 1). BC-3 carried a monoallelic 2 bp-deletion in exon 7 leading to a frameshift at codon 247 followed by a stop at codon 250, whereas BCP-1 harbored a homozygous deletion of PTEN exons 6 through 9. In both cases, these mutations resulted in the loss of PTEN protein expression (Figure 1). Approximately 20% of high-grade B-cell NHL have TP53 mutations18 whereas the reported rates of PTEN and PIK3CA mutations are around 5%10,11 and from 1 to 8%,12,13 respectively. By contrast, CTNNB1/β-catenin gene mutations occur more frequently in T-cell or NK/T-cell NHL from Asian patients than in B-cell NHL.15 Our results indicated that these genetic alterations occur at a lower frequency in PEL than in other subtypes of B-cell NHL, and suggested that other mechanisms may be relevant in activating oncogenic pathways.
Figure 1.
PTEN expression in PEL cell lines. Lysates from BC-3 (lane 1), BCBL-1 (lane 2), BCP-1 (lane 3), BBG-1 (lane 4), ISI-1 (lane 5) and CRA-BCBL (lane 8) cell lines were analyzed by Western blot for PTEN (A) and actin (B) protein expression. The T-ALL CEM (lane 6) and breast adenocarcinoma T47D (lane 7) cell lines served as negative and positive controls, respectively. Sodium dodecyl sulfate (SDS)-denatured cellular proteins were separated by SDS-polyacrylamide gel electrophoresis (PAGE) in 10% acrylamide gels using a discontinuous buffer system (Laemmli, U.K., 1970). The transfer of proteins onto nitrocellulose membranes (Hybond ECL, Amersham Biosciences) was carried out using a semi-dry blotting system. Blots were blocked with skimmed milk in TNT buffer (20 mM Tris-HCl pH 7.5, 150 mM NaCl, 0.05% Tween-20) and developed after successive incubation with anti-human PTEN rabbit antibody (R&D Systems) and alkaline phosphatase-labeled goat anti-rabbit IgG conjugate (Sigma-Aldrich).
Among HHV-8 lytic proteins with transforming potential, G-protein coupled receptor (vGPCR)19 and K120 have been shown to constitutively activate the PI3K/AKT pathway, and viral interferon regulatory factor 1 (vIRF1) to inhibit TP53 function.21 LANA-1, which is constitutively expressed in tumor PEL cells, is able to suppress TP53 function and to induce β-catenin accumulation by trapping the glycogen synthase kinase-3b (GSK-3b) into the nucleus.14 Beside genetic alterations of coding sequences, additional mechanisms might participate in the loss of tumor suppressor gene function such as epigenetic silencing. In BCBL-1, BCP-1 and ISI-1 cell lines, gene hypermethylation has been identified as underlying the loss of CDKN2A/p16INK4a locus expression.16 Post-translational modifications like phosphorylation can lead to PTEN inactivation, as observed in Hodgkin’s lymphoma cell lines.22 Because K1 expression has been shown to increase PTEN phosphorylation in transfected BJAB cells, it might contribute to the constitutive activation of PI3K/AKT pathway observed in PEL.20 Like in DLBCL and Burkitt’s lymphomas, TP53 and PTEN gene alterations occurred at a higher frequency in PEL cell lines (3/7) than in primary tumors (1/16). Considering both PEL cell lines and primary PEL tumors, the mutation rate was found to be significantly higher in EBV-negative PEL (4/11) compared to EBV-positive PEL (0/12, p=0.037, Fisher’s test). However, this difference was not significant when only the primary PEL cases were analyzed. A similar correlation between the presence of TP53 gene mutations and the absence of EBV has been reported in Hodgkin’s lymphomas,23 although this result could not be confirmed by further studies.24
Considering the 16 patients with PEL (Table 2), the CDKN1A/p21Cip1 S31R, CDKN1B/p27Kip1 V109G and CDC2L1 A655V polymorphims were found to be significantly associated with an African origin (p=0.033, 0.002 and 0.007, respectively), the CDKN1A/p21Cip1 c70t polymorphism with the presence of an HHV-8-associated multicentric Castleman disease (p=0.015) and the CCND3 A259S polymorphism with HIV-1 infection and EBV status of PEL (p=0.001 and 0.015, respectively). However, no correlation could be found between these SNP, the age of patients at the time of PEL diagnosis and their survival from the date of PEL diagnosis.
Our results confirm that mutations of TP53 and PTEN tumor suppressor genes, as well as deletion of CDKN2A-ARF locus, are uncommon in PEL, although they were detected at a higher frequency in PEL cell lines than in primary PEL tumors. Moreover, these genetic alterations were found to be restricted to EBV-negative PEL tumors. No mutations were detected in PIK3CA and CTNNB1/β-catenin hotspot sequences, suggesting that other mechanisms are involved in the pathogenesis of HHV-8-associated PEL.
Acknowledgments
the authors would like to thank Dr. Félix Agbalika (Service de Microbiologie, Hôpital Saint-Louis and EA3963, Université Paris 7, Paris, France), Dr. Chris Boshoff (Wolfson Institute for Biomedical Research, University College London, UK), Dr. Renaud Mahieux (Unité d'Epidémiologie et de Physiopathologie des Virus Oncogènes, Institut Pasteur, Paris, France) and Dr. Elizabeth Macintyre (Laboratoire d’Hématologie, Hôpital Necker Enfants Malades, Paris, France) for providing us with ISI-1, BCP-1, BC-2, BC-3, BCBL-1, BBG-1, CRA-BCBL, CEM, DAUDI, RAJI, RS(4;11) and REH cell lines. We would also like to thank Prof. Pierre Boulanger (Faculté de Médecine Laennec, Lyon, France) for critical reading of our manuscript.
Footnotes
Authorship and Disclosures
EB was the principal investigator and takes primary responsibility for the paper. EB recruited the patients. EB, AM, SSH and PP performed the laboratory work for the study. EB and PP performed the statistical analyses and wrote the paper.
The authors reported no potential conflicts of interest.
Funding: this work was supported by a grant from the French Ligue Nationale contre le Cancer. EB was supported by the French Association pour la Recherche sur le Cancer (ARC).
References
- 1.Dumont P, Leu JI, Della Pietra AC, 3rd, George DL, Murphy M. The codon 72 polymorphic variants of p53 have markedly different apoptotic potential. Nat Genet. 2003;33:357–65. doi: 10.1038/ng1093. [DOI] [PubMed] [Google Scholar]
- 2.Bond GL, Hirshfield KM, Kirchhoff T, Alexe G, Bond EE, Robins H, et al. MDM2 SNP309 accelerates tumor formation in a gender-specific and hormone-dependent manner. Cancer Res. 2006;66:5104–10. doi: 10.1158/0008-5472.CAN-06-0180. [DOI] [PubMed] [Google Scholar]
- 3.Bittenbring J, Parisot F, Wabo A, Mueller M, Kerschenmeyer L, Kreuz M, et al. MDM2 gene SNP309 T/G and p53 gene SNP72 G/C do not influence diffuse large B-cell non-Hodgkin lymphoma onset or survival in central European Caucasians. BMC Cancer. 2008;8:116. doi: 10.1186/1471-2407-8-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zainuddin N, Berglund M, Wanders A, Ren ZP, Amini RM, Lindell M, et al. TP53 mutations predict for poor survival in de novo diffuse large B-cell lymphoma of germinal center subtype. Leuk Res. 2009;33:60–6. doi: 10.1016/j.leukres.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 5.Boulanger E, Duprez R, Delabesse E, Gabarre J, Macintyre E, Gessain A. Mono/oligoclonal pattern of Kaposi Sarcoma-associated herpesvirus (KSHV/HHV-8) episomes in primary effusion lymphoma cells. Int J Cancer. 2005;115:511–8. doi: 10.1002/ijc.20926. [DOI] [PubMed] [Google Scholar]
- 6.Boulanger E, Afonso PV, Yahiaoui Y, Adle-Biassette H, Gabarre J, Agbalika F. Human herpesvirus-8 (HHV-8)-associated primary effusion lymphoma in two renal transplant recipients receiving rapamycin. Am J Transplant. 2008;8:707–10. doi: 10.1111/j.1600-6143.2007.02110.x. [DOI] [PubMed] [Google Scholar]
- 7.Nador RG, Cesarman E, Chadburn A, Dawson DB, Ansari MQ, Sald J, et al. Primary effusion lymphoma: a distinct clinicopathologic entity associated with the Kaposi’s sarcoma-associated herpes virus. Blood. 1996;88:645–56. [PubMed] [Google Scholar]
- 8.Carbone A, Gloghini A, Vaccher E, Zagonel V, Pastore C, Dalla Palma P, et al. Kaposi's sarcoma-associated herpesvirus DNA sequences in AIDS-related and AIDS-unrelated lymphomatous effusions. Br J Haematol. 1996;94:533–43. doi: 10.1046/j.1365-2141.1996.d01-1826.x. [DOI] [PubMed] [Google Scholar]
- 9.Uddin S, Hussain AR, Al-Hussein KA, Manogaran PS, Wickrema A, Gutierrez MI, et al. Inhibition of phosphatidylinositol 3’-kinase/AKT signaling promotes apoptosis of primary effusion lymphoma cells. Clin Cancer Res. 2005;11:3102–8. doi: 10.1158/1078-0432.CCR-04-1857. [DOI] [PubMed] [Google Scholar]
- 10.Gronbaek K, Zeuthen J, Guldberg P, Ralfkiaer E, Hou-Jensen K. Alterations of the MMAC1/PTEN gene in lymphoid malignancies. Blood. 1998;91:4388–90. [PubMed] [Google Scholar]
- 11.Sakai A, Thieblemont C, Wellmann A, Jaffe ES, Raffeld M. PTEN gene alterations in lymphoid neoplasms. Blood. 1998;92:3410–5. [PubMed] [Google Scholar]
- 12.Abubaker J, Bavi PP, Al-Harbi S, Siraj AK, Al-Dayel F, Uddin S, et al. PIK3CA mutations are mutually exclusive with PTEN loss in diffuse large B-cell lymphoma. Leukemia. 2007;21:2368–70. doi: 10.1038/sj.leu.2404873. [DOI] [PubMed] [Google Scholar]
- 13.Baohua Y, Xiaoyan Z, Tiecheng Z, Tao Q, Daren S. Mutations of the PIK3CA gene in diffuse large B cell lymphoma. Diagn Mol Pathol. 2008;17:159–65. doi: 10.1097/PDM.0b013e31815d0588. [DOI] [PubMed] [Google Scholar]
- 14.Fujimuro M, Wu FY, ApRhys C, Kajumbula H, Young DB, Hayward GS, et al. A novel viral mechanism for dysregulation of beta-catenin in Kaposi’s sarcoma-associated herpesvirus latency. Nat Med. 2003;9:300–6. doi: 10.1038/nm829. [DOI] [PubMed] [Google Scholar]
- 15.Hoshida Y, Hongyo T, Nakatsuka S, Nishiu M, Takakuwa T, Tomita Y, et al. Gene mutations in lymphoproliferative disorders of T and NK/T cell phenotypes developing in renal transplant patients. Lab Invest. 2002;82:257–64. doi: 10.1038/labinvest.3780419. [DOI] [PubMed] [Google Scholar]
- 16.Platt G, Carbone A, Mittnacht S. p16INK4a loss and sensitivity in KSHV associated primary effusion lymphoma. Oncogene. 2002;21:1823–31. doi: 10.1038/sj.onc.1205360. [DOI] [PubMed] [Google Scholar]
- 17.Katano H, Sato Y, Sata T. Expression of p53 and human herpesvirus-8 (HHV-8)-encoded latency-associated nuclear antigen with inhibition of apoptosis in HHV-8-associated malignancies. Cancer. 2001;92:3076–84. doi: 10.1002/1097-0142(20011215)92:12<3076::aid-cncr10117>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 18.Imamura J, Miyoshi I, Koeffler HP. p53 in hematologic malignancies. Blood. 1994;84:2412–21. [PubMed] [Google Scholar]
- 19.Montaner S. Akt/TSC/mTOR activation by the KSHV G protein-coupled receptor: emerging insights into the molecular oncogenesis and treatment of Kaposi’s sarcoma. Cell Cycle. 2007;6:438–43. doi: 10.4161/cc.6.4.3843. [DOI] [PubMed] [Google Scholar]
- 20.Tomlinson CC, Damania B. The K1 protein of Kaposi’s sarcoma-associated herpesvirus activates the Akt signaling pathway. J Virol. 2004;78:1918–27. doi: 10.1128/JVI.78.4.1918-1927.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seo T, Park J, Lee D, Hwang SG, Choe J. Viral interferon regulatory factor 1 of Kaposi’s sarcoma-associated herpesvirus binds to p53 and represses p53-dependent transcription and apoptosis. J Virol. 2001;75:6193–8. doi: 10.1128/JVI.75.13.6193-6198.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Georgakis GV, Li Y, Rassidakis GZ, Medeiros LJ, Mills GB, Younes A. Inhibition of the phosphatidylinositol-3 kinase/Akt promotes G1 cell cycle arrest and apoptosis in Hodgkin lymphoma. Br J Haematol. 2006;132:503–11. doi: 10.1111/j.1365-2141.2005.05881.x. [DOI] [PubMed] [Google Scholar]
- 23.Chen WG, Chen YY, Kamel OW, Koo CH, Weiss LM. p53 mutations in Hodgkin’s disease. Lab Invest. 1996;75:519–27. [PubMed] [Google Scholar]
- 24.Maggio EM, Stekelenburg E, Van den Berg A, Poppema S. TP53 gene mutations in Hodgkin lymphoma are infrequent and not associated with absence of Epstein-Barr virus. Int J Cancer. 2001;94:60–6. doi: 10.1002/ijc.1438. [DOI] [PubMed] [Google Scholar]