Monoclonal gammopathy of undetermined significance (MGUS) is one of the most common pre-malignant disorders in western countries with a prevalence of 3.2% in the Caucasian general population 50 years of age or older.1 It is characterized by the presence of a monoclonal immunoglobulin (M-protein) in individuals lacking evidence of multiple myeloma (MM) or other lymphoproliferative malignancies.2 Long-term follow-up of MGUS patients reveals an average 1% annual risk of developing a lymphoproliferative malignancy.3,4 Although the etiology of MM and MGUS is unknown, there is emerging evidence to support a role for genetic factors. For example, familial aggregation of both MM and MGUS has been observed.5 Also racial disparities in incidence patterns for MGUS and MM support a role for germline genes in the etiology of MM.6 Recently, we found first-degree relatives of MGUS patients to have an increased risk of MGUS, MM, lymphoplasmacytic lymphoma/Waldenström’s macroglobulinemia, and chronic lymphocytic leukemia, supporting a role for shared common germline susceptibility genes in these disorders.5 Furthermore, in two recent studies an excess of certain solid tumors among blood relatives to MM patients was reported.7,8
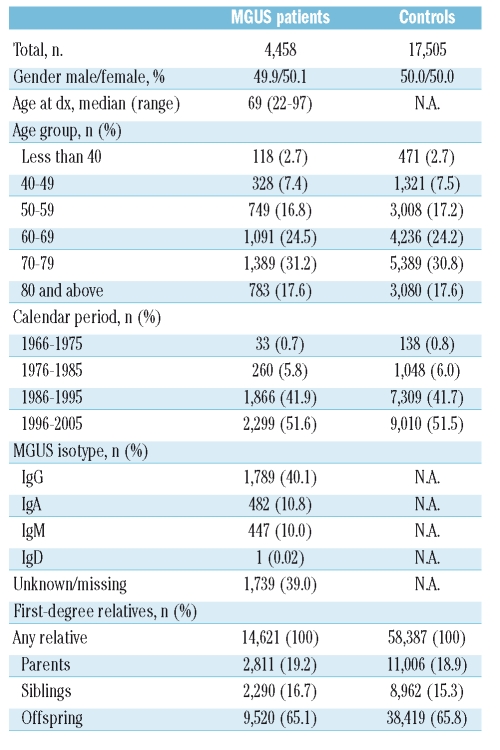
To improve our understanding in this area, we have, to the best of our knowledge, conducted the first population-based study to evaluate familial aggregation patterns of 27 solid tumors and all myeloid hematologic malignancies among first-degree blood relatives of MGUS patients. Using high-quality population-based data from Sweden, we identified 4,458 MGUS patients and 17,505 controls, as well as all linkable first-degree relatives of patients (n=14,621) and controls (n=58,387) (Table 1). We used χ2 models to calculate relative risks (RR) and 95% confidence intervals (CI) as measures of familial aggregation.
Table 1.
Characteristics of MGUS patients and matched controls.
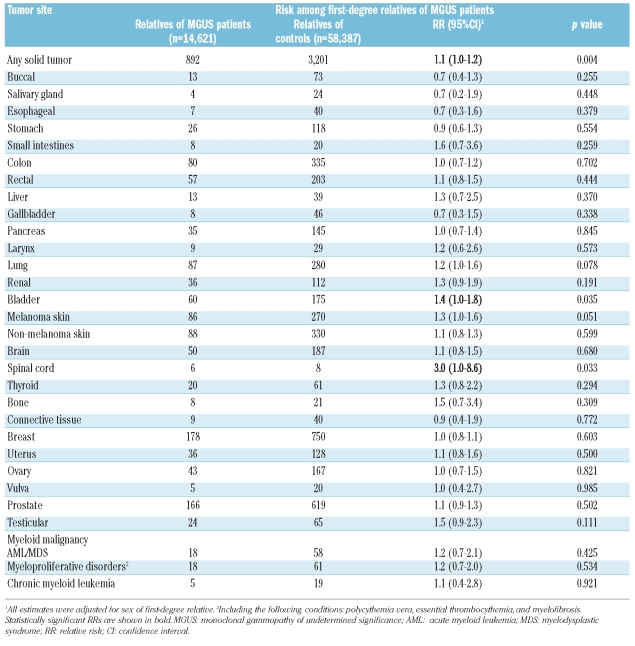
Table 2.
Relative risk of solid tumors and hematologic myeloid malignancies among first-degree relatives of MGUS patients.
Compared to relatives of controls, first-degree relatives of MGUS patients had a borderline increased risk of any solid tumor (RR=1.1; 95% CI 1.04–1.21; p=0.004). When we assessed individual tumor sites, we found evidence of a significantly increased risk for bladder cancer (RR=1.4; 95% CI 1.02–1.84; p=0.035) and, based on small numbers, a 3.0-fold (95% CI 1.04–8.64; p=0.033) increased risk for spinal cancer. We also found borderline increased risks for malignant melanoma (RR=1.3; 95% CI 1.00–1.62; p=0.051) and lung cancer (RR=1.2; 95% CI 0.98–1.58; p=0.078). No significantly increased risk was found for any of the other solid tumor sites (Table 1). Neither did we find relatives of MGUS patients to have a significantly increased risk for myeloid hematologic malignancies (Table 1). In analyses stratified by MGUS isotype, the risks were essentially the same (data not shown).
The observed increased risk for bladder cancer among relatives of MGUS patients agrees with a prior study showing evidence of co-aggregation of MM and bladder cancer.9 Furthermore, in a study based on patients with a coexisting MGUS and a solid tumor, 24% had bladder cancer.10 Also in agreement with a previous study by Camp et al.,7 we found first-degree relatives of MGUS cases to have a borderline increased risk of malignant melanoma. These findings are further supported by a prior genotyping study, suggesting that germline mutations in the CDKN2A gene may predispose to both MM and malignant melanoma.11 Our finding of a borderline increased risk of lung cancer among relatives of MGUS patients needs to be confirmed by other studies. However, one small study found family history of lung cancer to be associated with an increased risk of MM in elderly patients,12 a finding not observed in our previous Swedish MM study.6 In contrast to two prior studies focusing on solid cancers in MM families, 7,8 we did not find a significantly increased risk of prostate cancer among MGUS relatives. Based on small numbers, we found excess risk of spinal cancer among MGUS relatives. Because we evaluated a large number of malignancies, it cannot be ruled out that this finding is due to chance. Finally, we did not find an increased risk of myeloid malignancies among first-degree relatives suggesting that myeloid and lymphoid hematologic malignancies have different mechanisms with regard to etiology. Our study has several strengths, including its large size as well as the application of high-quality data. The use of the nationwide register-based case-control design ruled out recall-bias, ensured a population-based setting, and generalizability of our findings. The nature of this study is hypothesis-generating and one has to interpret our findings with caution due to the large number of tested malignancies.
Our findings support a role for a shared susceptibility (genetic, environmental, or both) that predisposes to MGUS and certain solid tumors, supporting the application of gene mapping and candidate gene approaches in high-risk families and case-control studies.
Acknowledgments
the authors thank Ms. Shiva Ayobi, The National Board of Health and Welfare, Stockholm, Sweden; Ms. Susanne Dahllöf, Statistics Sweden, Orebro, Sweden; Ms. Charlotta Ekstrand, Ms. Molly Collin and Ms. Lisa Camner, Karolinska Institutet, Stockholm, Sweden, for invaluable ascertainment of MGUS data; and Ms. Emily Steplowski, Information Management Services, Silver Spring, MD, for important efforts in the development of this database. The authors have no conflict of interest to declare.
Footnotes
Funding: This research was supported by grants from the Swedish Cancer Society, Stockholm County Council, the Karolinska Institutet Foundations, and the Intramural Research Program of the NIH, NCI.
References
- 1.Kyle RA, Therneau TM, Rajkumar SV, Larson DR, Plevak MF, Offord JR, et al. Prevalence of monoclonal gammopathy of undetermined significance. N Engl J Med. 2006;354:1362–9. doi: 10.1056/NEJMoa054494. [DOI] [PubMed] [Google Scholar]
- 2.Anonymous Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group. Br J Haematol. 2003;121:749–57. [PubMed] [Google Scholar]
- 3.Kyle RA, Therneau TM, Rajkumar SV, Offord JR, Larson DR, Plevak MF, et al. A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N Engl J Med. 2002;346:564–9. doi: 10.1056/NEJMoa01133202. [DOI] [PubMed] [Google Scholar]
- 4.Kyle RA, Therneau TM, Rajkumar SV, Remstein ED, Offord JR, Larson DR, et al. Long-term follow-up of IgM monoclonal gammopathy of undetermined significance. Blood. 2003;102:3759–64. doi: 10.1182/blood-2003-03-0801. [DOI] [PubMed] [Google Scholar]
- 5.Landgren O, Kristinsson SY, Goldin LR, Caporaso NE, Blimark C, Mellqvist UH, et al. Risk of plasma-cell and lymphoproliferative disorders among 14,621 first-degree relatives of 4,458 patients with monoclonal gammopathy of undetermined significance (MGUS) in Sweden. Blood. 2009 doi: 10.1182/blood-2008-12-191676. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Landgren O, Linet MS, McMaster ML, Gridley G, Hemminki K, Goldin LR. Familial characteristics of autoimmune and hematologic disorders in 8,406 multiple myeloma patients: a population-based case-control study. Int J Cancer. 2006;118:3095–8. doi: 10.1002/ijc.21745. [DOI] [PubMed] [Google Scholar]
- 7.Camp NJ, Werner TL, Cannon-Albright LA. Familial myeloma. N Engl J Med. 2008;359:1734–5. doi: 10.1056/NEJMc081677. [DOI] [PubMed] [Google Scholar]
- 8.Lynch HT, Ferrara K, Barlogie B, Coleman EA, Lynch JF, Weisenburger D, et al. Familial myeloma. N Engl J Med. 2008;359:152–7. doi: 10.1056/NEJMoa0708704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Plna K, Hemminki K. Familial bladder cancer in the National Swedish Family Cancer Database. J Urol. 2001;166:2129–33. [PubMed] [Google Scholar]
- 10.Anagnostopoulos A, Galani E, Gika D, Sotou D, Evangelopoulou A, Dimopoulos MA. Monoclonal gammopathy of undetermined significance (MGUS) in patients with solid tumors: effects of chemotherapy on the monoclonal protein. Ann Hematol. 2004;83:658–60. doi: 10.1007/s00277-004-0896-1. [DOI] [PubMed] [Google Scholar]
- 11.Dilworth D, Liu L, Stewart AK, Berenson JR, Lassam N, Hogg D. Germline CDKN2A mutation implicated in predisposition to multiple myeloma. Blood. 2000;95:1869–71. [PubMed] [Google Scholar]
- 12.Bourguet CC, Grufferman S, Delzell E, DeLong ER, Cohen HJ. Multiple myeloma and family history of cancer. A case-control study. Cancer. 1985;56:2133–9. doi: 10.1002/1097-0142(19851015)56:8<2133::aid-cncr2820560842>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]