Abstract
Introduction
Implantable cardioverter-defibrillators improve mortality in selected high risk patients, yet population based data regarding utilization of these devices, particularly in the elderly, are limited.
Methods
To address this, we reviewed all ICD implantations performed in Olmsted County, MN, a geographically defined population, between December 1989 and December 2004.
Results
The study population comprised 179 patients (147 male, 82%, mean age 65 ± 14 years). Baseline ejection fraction and creatinine were 35% ± 16% and 1.38 ± 1.08 mg/dL, respectively. Over the study period, the incidence of congestive heart failure in patients undergoing ICD implantation and referrals for primary prevention ICDs increased, while baseline ejection fraction and etiology of cardiomyopathy remained unchanged. The incidence of ICD implantations increased significantly in the elderly (p<0.001) and especially in male patients when compared to female patients (p<0.001).
Conclusions
Age of patients undergoing ICD implantation is increasing. However, fewer females compared to males are undergoing ICD implantation, suggesting a gender bias in ICD therapy and utilization.
Keywords: Implantable cardioverter defibrillator utilization, gender differences; outcomes; elderly
1 Introduction
The efficacy of implantable cardioverter-defibrillator (ICD) therapy to prevent sudden cardiac death is well established in high risk patients 1,2. The Multicenter Automatic Defibrillator Implantation Trial II (MADIT II) and Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) have both demonstrated the benefit of prophylactic ICD implantation in primary prevention of sudden cardiac death in patients with left ventricular dysfunction 3,4. Population-based data regarding trends in ICD utilization in a community setting are limited and difficult to obtain due to lack of uniform follow up.
Other studies have shown gender differences and bias in the treatment of other cardiovascular diseases 5-7. More recent evidence has emerged from Medicare and American Heart Association databases that also suggests gender bias in ICD utilization 8-10. Whether similar gender and age biases also occur in community based practices, however, remains unknown.
Therefore to determine this, we undertook to examine trends in ICD utilization in a population-based study. Residents of Olmsted County represent a geographically defined group who are followed primarily at the Mayo Clinic and Olmsted Medical Center. All ICD implantations in Olmsted County are performed at the Mayo Clinic, providing an ideal setting to observe temporal trends in ICD utilization in a community based practice.
This study is important since previous studies have frequently failed to include patients >65 years old or female patients. Since age and gender bias have been demonstrated in other cardiovascular diseases, whether the findings of ICD clinical trials translate into the community setting is unknown.
2 Materials and Methods
2.1 Study Population
All new ICD implantations in Olmsted County, MN residents from December 1989-December 2004 were included. ICD generator replacement implantations were excluded. Clinical data were prospectively entered into a centralized clinical record and retrospectively analyzed. Follow-up data and death notification were obtained from the clinical record and the National Death Registry. Elderly patients were defined as patients who were 70-79 years old and very elderly patients were defined as patients who were ≥ 80 years old.
ICD implantation data, including defibrillation threshold (DFT) testing, was obtained from operative notes. DFT testing was performed at the time of ICD implantation in most patients. In most cases, ventricular fibrillation was induced on two occasions and a first shock programmed at either 14J or 21J. If 14J was successful at restoring sinus rhythm a second shock at 14 J was performed. If 14J was unsuccessful a second shock at 21J was attempted. In most cases, a “step down to failure” approach was not used. DFT was considered high if ≥ 15 J.
2.2 Case-control analysis
Mayo Clinic is a tertiary referral center with a large referral practice both within the United States and internationally. Since the primary aim of this study was to describe temporal trends in ICD utilization in a community based practice, to adjust for referral bias we conducted a case-control analysis between our referral and community based ICD practice to determine if trends observed in our community based practice are broadly applicable to the general population of ICD patients. We compared a random selection of our study group (Olmsted County residents) to randomly selected age and sex matched non-resident controls from our referral practice (i.e. non-resident controls) that underwent ICD implantation at Mayo Clinic, during the study period. Non-resident controls were also matched by year of ICD implantation. Clinical and follow up data, death notification and ICD implantation data were obtained from the National Death Registry and from the same centralized clinical record as for the study population. Differences in means were compared using a Wilcoxon rank-sum tests. Differences in patient characteristics between control and study subjects amongst three defined five year periods (1989-1994, 1995-1999, 2000-2004) were compared using a Kruskal-Wallis test. A p value of <0.05 was considered significant.
2.3 Incidence rates
Olmsted County residents undergoing ICD implantation were identified using the resources of the Rochester Epidemiology Project (REP), a medical records linkage system designed to capture data on any patient-physician encounter in Olmsted County, Minnesota 11,12. The population of this upper Midwest community of the United States (106,470 in 1990) is relatively isolated from other urban areas, and virtually all medical care is provided to county residents by Mayo Clinic or Olmsted Medical Group and their affiliated hospitals 11,12.
Annual age- and gender- specific incidence rates were constructed using the age and gender specific population figures for Olmsted County, Minnesota from the United States census. Age-and gender- specific denominators for individual years were generated from linear interpolation of the 1970, 1980, 1990, and 2000 census figures. The 95% confidence intervals were calculated with assumptions based on the Poisson distribution. Trends over time, by age, and between genders were investigated using Poisson regression models. A p value of <0.05 was considered significant.
3 Results
3.1 Study Population
A total of 179 Olmsted County residents underwent ICD implantation during the study period. Baseline characteristics and implant indications are summarized in Tables 1 and 2. There were 147 (82%) males and 32 (18%) females, mean age 65 ±14 years. Underlying cardiac disease was ischemic in 128 (72%) patients and non-ischemic in 51 (28%) patients. Mean ejection fraction was 35% ± 16%, 38 (22%) patients had a prior history of congestive heart failure and 53 (30%) had a history of atrial fibrillation at the time of ICD implantation. Medications, including anti-arrhythmic drugs, are shown in Table 1. Initial ICD implant indication was primary prevention in 42 (23%) patients and secondary prevention for sustained ventricular arrhythmias or sudden cardiac death in 137 (77%) patients. ICD implant indications changed during the study period. In the first and second five year periods (1989-1994, 1995-1999), all ICDs (n= 19 and n= 43, respectively) were implanted for secondary prevention. In the last five year period (2000-2004), 42 (36%) patients underwent ICD implantation for primary prevention, and 75 (64%) for secondary prevention. A dual chamber ICD was implanted in 91 (51%) patients; of these, 22 patients (24%) had high grade atrio-ventricular block, 9 patients (10%) had sinus node dysfunction, and 60 patients (66%) had conduction system disease demonstrated by invasive electrophysiology testing. A cardiac resynchronization therapy device was implanted in 14 (8%) patients for medically refractory heart failure.
Table 1. Patient Characteristics.
| Olmsted County residents n = 179* | |
|---|---|
| Age | 65 ± 14 years |
| Gender (Male) | 147 (82%) |
| Ejection fraction (n= 177) | 35% ±16% |
| Ischemic cardiomyopathy | 128 (72%) |
| DFT testing at implant | 163 (91%) |
| Atrial fibrillation | 53 (30%) |
| CHF (n= 176) | 38 (22%) |
| Creatinine (n= 176) | 1.38 ±1.08 mg/dL |
| Medications (n= 176) | |
| ACE Inhibitors or ARB | 108 (61%) |
| Beta Blockers | 83 (47%) |
| Digoxin | 60 (34%) |
| Diuretic | 85 (48%) |
| Calcium Channel Blockers | 19 (11%) |
| Class IA Anti-arrhythmic Drugs | 3 (2%) |
| Class IB Anti-arrhythmic Drugs | 3 (2%) |
| Class III Anti-arrhythmic Drugs | 12 (7%) |
unless otherwise noted, DFT= defibrillation threshold, CHF= congestive heart failure, Angiotensin receptor blockers
Table 2. Implant Indication.
| Implant Indications | n=179 |
|---|---|
| Primary prevention | 42 (23%) |
| Secondary prevention | 137 (77%) |
| Dual chamber ICD | 91 (51%) |
| CHB / High grade AV block | 22 (24%) |
| Sinus node dysfunction | 9 (10%) |
| Conduction system disease by EP study | 60 (66%) |
| CRT | 14 (8%) |
ICD = implantable cardioverter defibrillator, CHB = complete heart block, EP = electrophysiology, CRT = cardiac resynchronization therapy
3.2 Case Control Analysis
Comparison of baseline characteristics and implant indications of 47 randomly selected age and sex matched controls with 47 study patients are summarized in Tables 3 and 4. Ischemic cardiomyopathy was the underlying etiology in 31 (66%) study patients versus 30 (65%) controls (p= 0.94). Mean ejection fraction was not different in study patients versus controls (p=0.79). Medication use in study patients and control patients are shown in Table 3. Anti-arrhythmic drug use was similar in the study group when compared to controls. There was no difference in the proportion of study patients who had a history of congestive heart failure or atrial fibrillation at the time of ICD implantation when compared to controls. Olmsted County residents were more likely to receive an ICD for secondary prevention than controls, 36 patients (77%) versus 26 patients (56%), respectively (p= 0.04).
Table 3. Case-control Analysis-Baseline Characteristics.
| Olmsted County residents n=47 | Control n=47 | p value | |
|---|---|---|---|
| Ejection fraction | 33% ± 16% | 33% ± 18% | 0.79 |
| Ischemic cardiomyopathy | 31 (66%) | 30 (65%) | 0.94 |
| DFT testing at implant | 43 (91%) | 44 (94%) | 0.69 |
| Atrial fibrillation | 16 (34%) | 12 (27%) | 0.44 |
| CHF | 8 (17%) | 14 (31%) | 0.13 |
| Creatinine | 1.28 ± 0.66 mg/dL | 1.37 ± 0.59 mg/dL | 0.27 |
| Medications | |||
| ACE Inhibitors or ARB | 25 (54%) | 27 (60%) | 0.59 |
| Beta Blockers | 18 (39%) | 21 (47%) | 0.47 |
| Digoxin | 18 (39%) | 14 (31%) | 0.42 |
| Diuretic | 20 (43%) | 29 (64%) | 0.04 |
| Calcium Channel Blockers | 8 (17%) | 3 (7%) | 0.12 |
| Class IA Anti-arrhythmic Drugs | 1 (2%) | 1 (2%) | 0.99 |
| Class IB Anti-arrhythmic Drugs | 1 (2%) | 2 (4%) | 0.54 |
| Class III Anti-arrhythmic Drugs | 3 (7%) | 5 (11%) | 0.44 |
DFT= defibrillation threshold, CHF= congestive heart failure
Table 4. Case-control Analysis-Implant Indications.
| Olmsted County residents n=47 | Control n=47 | p value | |
|---|---|---|---|
| Primary Prevention | 11 (23%) | 20 (43%) | 0.04 |
| Secondary Prevention | 36 (77%) | 26 (56%) | 0.04 |
| Dual chamber ICD * | 25 (53%) | 21 (47%) | 0.53 |
| Pacing indication | 10 (21%) | 6 (13%) | 0.32 |
| CRT † | 4 (9%) | 2 (4%) | 0.43 |
ICD = implantable cardioverter defibrillator, CRT = cardiac resynchronization therapy
3.3 Patient Characteristics and Changes Over Time
The number of study patients who underwent ICD implantation increased over the study period, with 19 patients undergoing ICD implantation between 1989 and 1994, 43 patients between 1995 and 1999, and 117 patients between 2000 and 2004. Baseline characteristics of the study patients in each of the five year periods are summarized in Table 5, and differences compared with a Kruskal-Wallis or Chi-square test. Over the study period, ICD implant indications, incidence of congestive heart failure, and medical therapy changed significantly. During the first ten years of the study period, all patients underwent ICD implantation for secondary prevention. In the last five years of the study, 42 (36%) of patients were referred for placement of a prophylactic ICD (p<0.01). The incidence of congestive heart failure (p=0.02) increased, as did use of beta blockers (p<0.01) and angiotensin-converting enzyme inhibitors and angiotensin receptor blockers, although this change was not statistically significant (p= 0.12). There was no change in baseline ejection fraction or etiology of underlying cardiac disease during the study period.
Table 5. Patient Characteristics by Year Group.
|
1989-1994 n = 19 |
1995-1999 n = 43 |
2000-2004 n = 117 |
p value | |
|---|---|---|---|---|
| Ejection fraction | 35% ± 15% | 35% ±17% | 35% ±16% | 0.99 |
| Primary Prevention | 0 | 0 | 42 (36%) | <0.01 |
| Ischemic cardiomyopathy | 13 (68%) | 32 (74%) | 83 (71%) | 0.98 |
| DFT * testing at implant | 16 (84%) | 41 (95%) | 106 (91%) | 0.35 |
| DFT (J) | 13 ± 5 | 12 ± 6 | 13 ± 4 | 0.25 |
| Atrial fibrillation | 3 (16%) | 13 (30%) | 37 (32%) | 0.45 |
| CHF | 3 (16%) | 2 (5%) | 33 (28%) | 0.02 |
| Creatinine | 1.78 ± 2.40 mg/dL | 1.18 ± 0.29 mg/dL | 1.39 ± 0.95 mg/dL | 0.15 |
| Beta Blockers | 5 (26%) | 12 (28%) | 66 (56%) | <0.01 |
| ACE Inhibitors or ARB | 8 (42%) | 23 (53%) | 77 (66%) | 0.12 |
DFT = defibrillation threshold, CHF= congestive heart failure
3.4 Incidence of ICD Implantations
The incidence of ICD implantation per 100,000 in each of the five year periods of males and females are summarized in Table 6 and shown in Figures 1 and 2. Over the entire study period, the incidence of ICD implantations increased in both males and females. However, a greater increase in the incidence of ICD implantations was observed in males when compared to females (Figure1). Specifically, between 1989 and 1994, the incidence of ICD implantations was 1.18 (95% confidence interval (CI); 0 -2.51) in females versus 7.45 (95% CI; 3.72-11.20) in males, compared with 7.14 (95% CI; 3.91-10.60) versus 42.63 (95% CI; 34.00-51.30), respectively, in 2000-2004 (p<0.01). The incidence of ICD implantations increased with age (p<0.01), with the greatest increase in elderly (70-79 years) and very elderly (≥ 80 years) male patients (Figure 2). From 1989-1994, the ICD incidence rates were 52.59 (95% CI; 19.30-114.60) in elderly males, compared with 186.43 (95% CI; 119.50-277.80) in 2000-2004 (p<0.01). Similarly, incidence rates in very elderly males increased from none in 1989-1994 to 204.74 (95% CI; 108.90-350.10) in 2000-2004. While incidence rates also increased in elderly and very elderly females during the study period, none versus 65.80 (95% CI; 32.80-117.80) and none versus 7.07 (95% CI; 0.18-39.40), respectively, the increase in incidence rates was significantly less than that in elderly and very elderly males (p<0.01).
Table 6. Incidence of ICD Implantations per 100,000.
| 1989-1994 | 1995-1999 | 2000-2004 | |
|---|---|---|---|
| Males (total - age adjusted) | 7.45 (3.72-11.20)* | 16.58 (10.80-22.40) | 42.63 (34.00-51.30) |
| Females (total - age adjusted) | 1.18 (0 -2.51) | 3.80 (1.43-6.17) | 7.14 (3.91-10.60) |
| Males 70-79 yrs old | 52.59 (19.30-114.60) | 87.21 (41.90-160.50) | 186.43 (119.50-277.80) |
| Females 70-79 yrs old | 0 | 12.90 (1.56-46.60) | 65.80 (32.80-117.80) |
| Males ≥80 yrs old | 0 | 72.25 (19.70-185.00) | 204.74 (108.90-350.10) |
| Females ≥ 80 yrs old | 0 | 15.47 (1.87-55.90) | 7.07 (0.18-39.40) |
95% confidence interval
Figure 1.
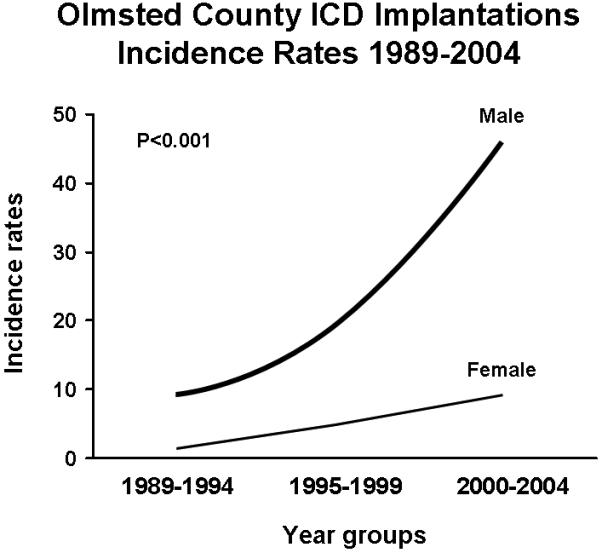
Incidence of ICD implantations over the study period by year groups. Incidence per 100,000 in males and females are shown.
Figure 2.
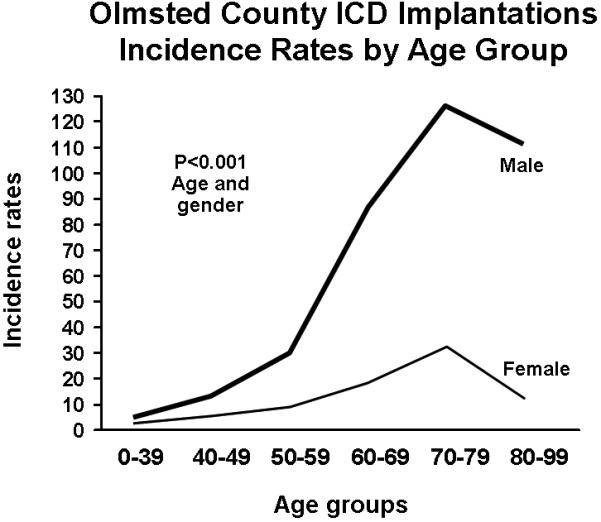
Incidence of ICD implantations by age groups. Incidence per 100,000 in males and females are shown.
4 Discussion
The major finding of this study is that the rate of ICD implantation in this geographically defined population has increased significantly over the past fifteen years. In particular, the numbers of elderly and very elderly patients receiving an ICD has increased. An unexpected finding was that ICD implantation rates increased disproportionately in males when compared to females.
ICD implant indications have evolved over the fifteen year study period, following the MADIT II trial which demonstrated the efficacy of prophylactic ICD implantation in patients with ischemic cardiomyopathy and left ventricular dysfunction 3. Our finding that incidence rates increased most markedly in the last five years of our study period likely reflects this change in indication for prophylactic ICD implantations. In the first ten years of our study period, no patients in our study group underwent ICD implantation for primary prevention. Conversely, in the last five years of our study period (2000-2004), during which the MADIT II data was published, more than one-third of patients underwent ICD implantation primary prevention of sudden cardiac death. Therefore, although the largest proportion (77%) of our study patients underwent ICD implantation for secondary prevention, we believe that the significant increase in incidence of ICD implantation during the latter part of the study period most likely reflects increased referrals for prophylactic ICD implantations.
Since elderly and very elderly patients comprise a large proportion of patients with ischemic cardiomyopathy and left ventricular dysfunction, it is not surprising that the highest increase in incidence of ICD implantation was observed in the elderly and very elderly.
The other changes observed in baseline characteristics, including increasing incidence of congestive heart failure and use of beta blockers, likely also reflect the evolution in ICD implant indications during the fifteen year study period and adoption of clinical trial data, especially pertaining to treatment of congestive heart failure, in the community. However, other baseline characteristics, including ejection fraction and underlying etiology of cardiac disease, have been stable over the study period.
Since our aim was to determine the impact of clinical trial data on a community based population, we accounted for probable referral bias by performing a case-control analysis comparing our community based practice to our referral (non-Olmsted County residents) practice. Our study population was similar to the referral population. Underlying etiology of cardiac disease and baseline characteristics of Olmsted County residents were not different than non-residents referred for ICD implantation at the Mayo Clinic, although Olmsted County residents were more likely to receive an ICD for secondary prevention than non-resident controls. The similarities suggest that although the Mayo Clinic is a tertiary care center with a referral based practice, temporal trends observed in our geographically defined study population may reflect general temporal trends in ICD implantation.
A surprising finding was that the increase in the incidence of ICD implantation over the study period was significantly higher in males than females. Specifically, the incidence of ICD implantation between 2000 and 2004 was six times higher in males than females. This difference was most marked in very elderly patients, with an incidence of ICD implantation 29 times higher in very elderly males compared to very elderly females. Similar gender disparities in ICD utilization have been observed in managed care and Medicare database analyses, and more recently in an American Heart Association survey of patients hospitalized for heart failure as well as a large multi-center registry (National Registry to Advance Heart Health) 9,10,13,14. While the reasons for gender based differences in ICD utilization are unclear, our data suggests that the discrepancy also exists in a community-based practice.
Our finding that the incidence of ICD implantation is lower in females is consistent with previous studies showing gender differences in treatment for other cardiovascular diseases 5-7,15. Females may be referred later and less often for coronary artery bypass grafting or cardiac catheterization, resulting in higher mortality from coronary artery disease 6,7,15. Similar findings have been shown for medical therapy for myocardial infarctions; females receive less aggressive medical therapy, both acutely and at the time of discharge 5.
One other explanation could be gender differences in the underlying etiology of cardiomyopathy and left ventricular dysfunction. Whether the recent addition of SCD-HeFT criteria to include prophylactic ICD implantation for patients with non-ischemic cardiomyopathy 4 will affect gender differences in the incidence of ICD implantation, remains to be seen. Further investigation is required to determine if this reflects gender differences in patient perceptions of ICD therapy, or physician referral bias.
5 Conclusions
The incidence of ICD implantation is increasing, with the greatest increase in the elderly and very elderly. Despite proven efficacy of ICD therapy, males are increasingly more likely to undergo ICD implantation than females, with this difference being more marked in the elderly and very elderly. These data suggest that ICD therapy is underutilized in females.
Acknowledgments
Financial Support: This study was not supported by any financial grants.
ABBREVIATIONS
- ICD
implantable cardioverter defibrillator
- DFT
defibrillation threshold
- MADIT II
Multi-center Automatic Defibrillator Implantation Trial II
- SCD-HeFT
Sudden Cardiac Death in Heart Failure Trial
- REP
Rochester Epidemiology Project
- EP
electrophysiology
- CHF
congestive heart failure
- CRT
cardiac resynchronization therapy
Footnotes
Financial Disclosures: Dr. Hayes has the following financial disclosures: Educational speaking; Medtronic, Guidant, St. Jude Medical, Sorin/ELA, Sponsored research; Medtronic, Guidant, St. Jude Medical, Steering committee; Medtronic, Advisory board; Guidant, Sorin/ELA, St. Jude Medical. None of the other authors have any conflicts.
REFERENCES
- 1.The Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators A Comparison of Antiarrhythmic-Drug Therapy with Implantable Defibrillators in Patients Resuscitated from Near-Fatal Ventricular Arrhythmias. N Engl J Med. 1997;337:1576–1584. doi: 10.1056/NEJM199711273372202. [DOI] [PubMed] [Google Scholar]
- 2.Moss AJ, Hall WJ, Cannom DS, Daubert JP, Higgins SL, Klein H, Levine JH, Saksena S, Waldo AL, Wilber D, Brown MW, Heo M, The Multicenter Automatic Defibrillator Implantation Trial Investigators Improved Survival with an Implanted Defibrillator in Patients with Coronary Disease at High Risk for Ventricular Arrhythmia. N Engl J Med. 1996;335:1933–1940. doi: 10.1056/NEJM199612263352601. [DOI] [PubMed] [Google Scholar]
- 3.Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, Daubert JP, Higgins SL, Brown MW, Andrews ML, the Multicenter Automatic Defibrillator Implantation Trial II Investigators Prophylactic Implantation of a Defibrillator in Patients with Myocardial Infarction and Reduced Ejection Fraction. N Engl J Med. 2002;346:877–883. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 4.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH, the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 5.Blomkalns AL, Chen AY, Hochman JS, Peterson ED, Trynosky K, Diercks DB, Brogan J, Gerard X, Boden WE, Roe MT. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: Large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol. 2005;45:832–837. doi: 10.1016/j.jacc.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 6.Chandra NC, Ziegelstein RC, Rogers WJ, Tiefenbrunn AJ, Gore JM, French WJ, Rubison M. Observations of the treatment of women in the United States with myocardial infarction: a report from the National Registry of Myocardial Infarction-I. Arch Intern Med. 1998;158:981–988. doi: 10.1001/archinte.158.9.981. [DOI] [PubMed] [Google Scholar]
- 7.Khan SS, Nessim S, Gray R, Czer LS, Chaux A, Matloff J. Increased mortality of women in coronary artery bypass surgery: evidence for referral bias. Ann Intern Med. 1990;112:561–567. doi: 10.7326/0003-4819-112-8-561. [DOI] [PubMed] [Google Scholar]
- 8.Ruskin JN, Camm AJ, Zipes DP, Hallstrom AP, McGrory-Usset ME. Implantable cardioverter defibrillator utilization based on discharge diagnoses from Medicare and managed care patients. Journal Of Cardiovascular Electrophysiology. 2002;13:38–43. doi: 10.1046/j.1540-8167.2002.00038.x. [DOI] [PubMed] [Google Scholar]
- 9.Curtis LH, Al-Khatib SM, Shea AM, Hammill BG, Hernandez AF, Schulman KA. Sex Differences in the Use of Implantable Cardioverter-Defibrillators for Primary and Secondary Prevention of Sudden Cardiac Death. [DOI] [PubMed] [Google Scholar]
- 10.Hernandez AF, Fonarow GC, Liang L, Al-Khatib SM, Curtis LH, LaBresh KA, Yancy CW, Albert NM, Peterson ED. Sex and Racial Differences in the Use of Implantable Cardioverter-Defibrillators Among Patients Hospitalized With Heart Failure. [DOI] [PubMed] [Google Scholar]
- 11.Kurland L, Molgard C. The Patient Record in Epidemiology. Sci Am. 1981;245:54–63. doi: 10.1038/scientificamerican1081-54. [DOI] [PubMed] [Google Scholar]
- 12.Melton L. History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–74. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 13.Gauri AJ, Davis A, Hong T, Burke MC, Knight BP. Disparities in the Use of Primary Prevention and Defibrillator Therapy Among Blacks and Women. Am J Med. 2006;119:167.e17–167.e21. doi: 10.1016/j.amjmed.2005.08.021. [DOI] [PubMed] [Google Scholar]
- 14.El-Chami MF, Hanna IR, Bush H, Langberg JJ. Impact of race and gender on cardiac device implantations. Heart Rhythm. 2007;4:1420–1426. doi: 10.1016/j.hrthm.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 15.Ayanian JZ, Epstein AM. Differences in the use of procedures between women and men hospitalized for coronary heart disease. N Engl J Med. 1991;325:221–225. doi: 10.1056/NEJM199107253250401. [DOI] [PubMed] [Google Scholar]


