Abstract
Tumors are complex collections of heterogeneous cells with recruited vasculature, inflammatory cells, and stromal elements. Neoplastic cells frequently display a hierarchy in differentiation status. Recent studies suggest that brain tumors have a limited population of neoplastic cells called cancer stem cells with the capacity for sustained self-renewal and tumor propagation. Brain tumor stem cells contribute to therapeutic resistance and tumor angiogenesis. In this minireview, we summarize recent data regarding critical signaling pathways involved in brain tumor stem cell biology and discuss how targeting these molecules may contribute to the development of novel anti-glioma therapies.
Cancers can be considered organ systems with aberrant activation of developmental and wound response pathways. Recent evidence suggests that within some tumors there is a cell subpopulation with the special capacity for sustained self-renewal and tumor propagation in vivo. Cells fulfilling these criteria were originally reported in acute myeloid leukemia (1), but similar populations were soon successively identified within various solid tumors (2). The proper terminology regarding these cells remains unsettled, with most groups using terms such as CSCs,2 tumor-initiating/propagating cells, and stem-like cancer cells. Although CSCs are a source of controversy, the concept recognizes the well described heterogeneity of tumor cells. Many critics contest the hypothesis on the grounds of a potential stem cell origin, challenge of current markers, or CSC frequency, none of which are implicit requirements of the CSC hypothesis (3).
Malignant gliomas are essentially universally lethal despite conventional therapy, with surgical resection and chemoradiation limited to palliation. Glioma CSCs were among the first solid tumor CSCs described (4) and remain one of the most widely used CSC models. Glioma CSCs share significant similarities with normal NSCs, including the expression of stem cell markers (CD133, Nestin, Musashi, and Sox2) and the capacity to differentiate into multiple lineages (5), but the overlap is incomplete. Notably, glioma CSCs are also highly resistant to chemoradiotherapies (5, 6), underscoring the importance of developing more efficient therapies against CSCs and prompting researchers to elucidate the molecular mechanisms regulating CSCs. Here, we summarize recent findings regarding the signaling pathways that are critical to glioma CSC biology.
Signaling from the Outside In
CSC behaviors are constantly affected by external signals from their niche, including neighboring stromal, immune, and non-stem tumor cells. Extracellular and paracrine effects are mediated commonly from cell-surface ligand-receptor systems. Accumulating evidence has demonstrated that multiple glioma CSC functions hinge on major receptor-mediated pathways (Fig. 1).
FIGURE 1.
Complex signaling pathways and cellular factors regulate glioma CSCs. Glioma CSCs are controlled at multiple levels by complicated regulatory networks. Signals initiated by RTKs, BMPRs, Hedgehog, and Notch result in complicated intracellular events to help balance self-renewal and differentiation of CSCs as well as the promotion of cell survival and proliferation. Intracellular regulators, including transcriptional factors (Olig2, Myc, Oct4, etc.), epigenetic modifiers (Bmi1), and miRNAs, are also highly potent in maintaining CSC population due to their ability to regulate massive downstream targets simultaneously. FGF, fibroblast growth factor; PDGF, platelet-derived growth factor; IGF, insulin-like growth factor; PIP2, phosphatidylinositol 4,5-bisphosphate; PIP3, phosphatidylinositol 1,4,5-trisphosphate; PI3K, phosphoinositide 3-hydroxykinase; GSK, glycogen synthase kinase; PKA, protein kinase A; NICD, Notch intracellular domain.
Receptor Tyrosine Kinases
The RTK family mediates the effects of multiple oncogenic growth factor pathways, among which the EGFR is one of the best characterized in gliomas. Malignant glioma cells frequently have increased EGFR signaling as a result of either amplified EGFR copy number or expression of the constitutively active variant EGFRvIII. Transduction of murine Nestin+ NSCs with EGFRvIII induces glioma-like lesions (7). Similarly, a recent publication showed that the combination of AKT/phosphoinositide 3-hydroxykinase activation and constitutive EGFR activity is sufficient to transform murine NSCs (8). Although the origin of glioma CSCs is under study (9), these data suggest a possible role for EGFR pathways in glioma and possibly CSC biology. In cell culture studies, the proliferation and neurosphere generation (an in vitro assay to assess the self-renewal of CSCs) of human glioma CSCs were dependent on the EGFR (10), like NSCs.
The signal initiated by RTKs is transduced and amplified through downstream molecule cascades, such as the pro-survival AKT/phosphoinositide 3-hydroxykinase pathway. Upon activation by RTK pathways, AKT promotes survival, proliferation, invasion, and secretion of pro-angiogenic factors. We recently demonstrated that glioma CSCs are more dependent on AKT signals than matched non-stem glioma cells (54). Pharmacologic inhibitors of AKT attenuate glioma CSC neurosphere formation, induce apoptosis, and substantially delay intracranial tumor formation. These data suggest that AKT inhibition may specifically target the CSC population to reduce tumor malignancy.
Bone Morphogenetic Proteins
BMPs are a family of growth factors named for their central roles in bone and cartilage formation (11). Most BMPs elicit their actions through binding to cell-surface receptor kinases (the BMPRs). The canonical effectors of BMPRs are the Smad proteins. Activating phosphorylation of receptor Smad1/5/8 enables these proteins to bind to the co-activator Smad4, translocate into the nucleus, and regulate transcription. BMPs are crucial factors that regulate proliferation and apoptosis in NSCs and usually promote the differentiation of NSCs (12). Interestingly, a prodifferentiation BMP response mechanism seems to be preserved in some glioma CSCs, as CSCs express BMPRs, and BMPs inhibit the proliferation of these cells (13). BMP ligands deplete the CSC population by inducing the differentiation of CSCs into astroglial and neuron-like cells. Treating CSCs with BMPs in vivo markedly delays tumor growth and reduces tumor invasion. These data suggest that selective activation of BMP pathways may reduce the tumorigenic capacity of CSCs.
Similar to the previous report, Lee et al. (14) reported that glioma CSCs differentiate upon BMP treatment. However, CSCs from one patient displayed enhanced proliferation rather than differentiation upon BMP treatment. This CSC sample displayed a fetal BMPR expression pattern due to epigenetic silencing of Bmpr1b. Restoration of BMPR1B expression sensitized CSCs to BMP-mediated differentiation, suggesting that the expression pattern of BMPR may determine BMP-mediated CSC behavior. Thus, an individual tumor's genomic and epigenetic characteristics may determine the response to anti-CSC treatment.
Hedgehog
The binding of Hedgehog ligands to their receptors activates transducers termed GLIs (named for their discovery in gliomas), which then translocate into the nucleus to activate or repress downstream targets. The Hedgehog pathway is one of the key regulators of embryogenesis and is critical for several different types of normal stem cells, including NSCs (15, 16). Mutations in the Hedgehog pathway are associated with medulloblastomas, primary brain tumors common in children, and several genetic medulloblastoma models incorporate aberrant Hedgehog signaling. Hedgehog signaling is also active in gliomas and contributes to CSC function (17–19). Hedgehog ligands are required for CSC self-renewal as well as tumorigenesis. Treatment of glioma CSCs with the Hedgehog inhibitor cyclopamine or transduction with GLI RNA interference inhibits proliferation and self-renewal while increasing apoptosis. The importance of Hedgehog signaling is further underscored by the observation that Hedgehog inhibition augments the efficacy of the standard-of-care chemotherapy agent temozolomide to abolish CSC proliferation and induce cell death. In vivo, Hedgehog pathway inhibition blocks CSC tumor growth (18). Bar et al. (19) also showed that cyclopamine treatment depletes CSCs, as viable cells after treatment failed to propagate tumors in vivo. In agreement with our study (5), they found that CSCs respond poorly to radiotherapy. However, cyclopamine treatment improves the effects of radiation on CSC survival (19). Together, these data suggest that the Hedgehog pathway is important for glioma CSCs and that pharmacologic inhibitors may improve traditional therapy efficiency against gliomas.
Notch
Notch proteins are single-pass transmembrane receptors that mediate cell-cell communication. Upon ligand binding, Notch is cleaved by the γ-secretase complex to release its intracellular domain from the cell membrane. Cleaved Notch translocates into the nucleus to function as a transcription factor. The importance of the Notch signaling pathway is evident by its high conservation throughout evolution. During development, Notch promotes the proliferation of normal NSCs while suppressing their differentiation (20, 21). Notch is required for neural progenitors both in vitro and in vivo (22). Notch signaling has been implicated in brain tumor biology as well. Expression of Notch-1 and its ligands Delta-like-1 and Jagged-1 is critical to high grade gliomas and medulloblastomas (23–25). The potential role of Notch signaling in brain tumor CSCs was first studied in medulloblastomas, with CSCs expressing high levels of Notch and displaying sensitivity to Notch pathway inhibitors (26). Notch functions were later linked to glioma CSCs, as Notch signaling increases expression of the stem cell marker Nestin in gliomas. Notch expression in a K-Ras-induced mouse glioblastoma model generates proliferative lesions in the NSC-rich subependymal zone, ultimately leading to glioma formation (27). In addition, activation of Notch signaling in the glioma cell lines increases the formation of neurosphere-like colonies (28).
On the Inside
Transcription factors, epigenetic regulators, and miRNAs are extremely powerful regulators of normal cells and cancer cells. They are capable of simultaneous regulation of multiple downstream targets and are implicated in glioma CSC survival, proliferation, and maintenance (Fig. 1).
c-Myc
The c-Myc oncoprotein has been extensively studied for its instrumental role in the proliferation of both normal stem cells and tumor cells. Recently, inducible pluripotent stem cells were generated from differentiated cells through the introduction of several transcription factors, including c-myc (29), supporting a role in core stem cell machinery. c-Myc may thus serve as a critical link between “stemness” and malignancy. c-Myc expression correlates with the grade of malignancy in gliomas (30). We recently determined that glioma CSCs express elevated levels of c-Myc and that c-Myc is required both for maintenance of glioma CSCs in vitro and for their tumorigenic capacity in vivo (31). These data derived from human patient samples are supported by mouse glioma models. Conditional overexpression of c-Myc in mouse astroglia (a subtype of NSCs) results in growing tumors that resemble human gliomas (32). c-Myc additionally prevents differentiation and promotes self-renewal of tumor neurospheres derived from a p53/Pten double knock-out mouse model (33).
Octomer 4 (Oct4)
Oct4, along with Sox2 and Nanog, is believed to be a core component in controlling the balance between self-renewal and differentiation in embryonic stem cells. Oct4 is also one of the factors that generates inducible pluripotent stem cells (29). Oct4 is highly expressed in many human glioma specimens and cell lines, and its expression correlates with glioma grade (34). The direct role of Oct4 in glioma CSCs is not well understood, but overexpression of Oct4 in rat C6 glioma cells increases the expression level of the stemness marker Nestin. These data suggest that Oct4 may inhibit the differentiation of glioma CSCs (34) and contribute to CSC maintenance.
Olig2
Olig2 is a transcription factor that is almost exclusively expressed in the central nervous system. During brain development, Olig2 is expressed in neural progenitor cells that give rise to oligodendrocytes and certain neuronal subtypes (35–38). Pathological analysis revealed that Olig2 is expressed in almost all adult astrocytomas and is required for tumor initiation, suggesting a link to gliomas and CSCs (39, 40). Functionally, Olig2 is required in both normal NSCs and glioma CSCs. Olig2 sustains the replication-competent state of neural progenitors and is necessary for the multilineage differentiation potential of neural progenitors (38, 41). Olig2 function is mediated through the proliferative regulation of glioma CSCs in part through suppression of p21WAF1/CIP1 (40).
Bmi1
bmi1 belongs to the Polycomb group genes, which usually function as epigenetic silencers. Bmi1 has been implicated in determining stem cell fate in multiple tissues and is a positive regulator of NSC self-renewal (42). bmi1 is also a known oncogene that is frequently overexpressed in many cancer types, including gliomas. Using cells from wild-type and bmi1 knock-out mice, researchers demonstrated that Bmi1 is required for transforming both differentiated astrocytes and NSCs (43). Whereas transformed wild-type NSCs give rise to high grade gliomas in vivo, bmi1-deficient NSCs are able to initiate only less malignant tumors. bmi1-deficient tumors have fewer cells expressing the NSC marker Nestin, implying that they may have fewer CSCs. Both transformed and non-transformed bmi1-deficient NSCs demonstrate impaired capability of neurogenesis, highlighting a role of Bmi1 in controlling differentiation of normal and malignant stem cells. Although it remains unclear whether Bmi1 is also critical for CSCs derived from human gliomas, Bmi1 helps to maintain CSCs from hepatocellular carcinoma (44).
miRNAs
miRNAs are small noncoding RNAs that can silence target genes through post-transcriptional mechanisms on target mRNAs. miRNAs are powerful intracellular regulators because a single miRNA can regulate many distinct mRNAs. In cancer biology, miRNAs can function as “oncogenes,” e.g. the miR-17–92 polycistron, or “tumor suppressors,” e.g. the miR-15/miR-16 cluster. miRNA regulation appears to be critically important in glioma cell behaviors. For instance, miRNA-21 was shown to be significantly overexpressed in glioblastomas, and inhibition of its function induces apoptosis (45).
Two recent reports directly investigated the roles of miRNAs in glioma CSCs. The levels of miR-124 and miR-137 are reduced in grade III and IV malignant gliomas in comparison with normal brain (46). Overexpression of these two miRNAs inhibits proliferation while inducing differentiation of glioma CSCs, indicating a tumor suppressor role for these two miRNAs in CSCs. Similarly, another miRNA, miR-451, is expressed at lower levels in CD133+ glioma CSCs in comparison with CD133− non-stem glioma cells (47). External expression of miR-451 inhibits the growth of glioma CSCs and disrupts neurosphere formation.
Inside Out and Back Again
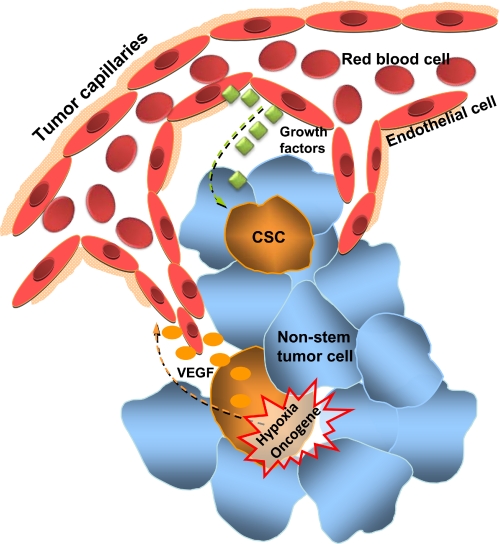
The relationship between CSCs and their microenvironment is reciprocal. CSCs not only receive signals from extracellular sources through receptors but also actively transmit signals to manipulate the environment. In this way, CSCs are able to modulate the same microenvironment that produces signals regulating CSCs. Angiogenesis is the best studied example of such cross-talk (Fig. 2).
FIGURE 2.
Glioma stem cells reside within a perivascular niche. Regulated by oncogene activation or microenvironment conditions such as hypoxia, CSCs are strongly capable of stimulating the growth of the neovasculature by expressing high levels of pro-angiogenic factors such as VEGF. On the other hand, blood vessels create a vascular niche to help maintain CSC population. Such reciprocal relationships between glioma CSCs and blood vessels enable rapid and sustained tumorigenesis.
Vascular Endothelial Growth Factor and Other Angiogenic Factors
Active angiogenesis is a hallmark of solid tumors and plays a key role in providing oxygen and nutrition as well as facilitating metastasis. Malignant gliomas are characterized by florid angiogenesis, with neovascularization significantly correlated with enhanced tumor aggressiveness, degree of tumor malignancy, and poor clinical prognosis. Given the importance of CSCs in glioma maintenance, it is not surprising that CSCs and angiogenesis are tightly connected. We showed that, in comparison with matched non-stem cancer cells, glioma CSCs have a stronger capacity for promoting angiogenesis, partially through amplified secretion of VEGF, one of the most important pro-angiogenic factors (48). Treating glioma CSCs with the VEGF-neutralizing antibody bevacizumab attenuates their ability to promote angiogenesis both in vitro and in vivo, which in turn markedly inhibits the tumorigenesis of CSCs. The mechanism underlying the specific up-regulation of VEGF in CSCs is still unclear, but it has been suggested that environmental factors such as hypoxia and acidosis play important roles in this process. Alternatively, VEGF could also be induced by oncogene activation, e.g. the loss of PTEN and/or activation of EGFR could result in high VEGF expression in gliomas.
Vascular Niche
The extraordinary pro-angiogenic influence of CSCs is likely critical for their maintenance not only because blood vessels provide oxygen and nutrition but also because, like normal NSCs, glioma CSCs are situated in “vascular niches.” Both normal NSCs and CSCs are believed to be physically located in specialized microenvironmental niches, which regulate self-renewal and differentiation. NSCs are located in niches defined by the vasculature (49, 50), and this property is shared by medulloblastoma CSCs (51). Co-injection of CSCs and endothelial cells accelerates tumor initiation and growth. This reciprocal relationship between angiogenesis and glioma CSCs may help explain the preliminary success of anti-angiogenesis therapy on malignant gliomas. Clinical trials of anti-angiogenic drugs like bevacizumab and cediranib have demonstrated promising preliminary results in glioblastoma patients (52, 53). It is possible that these drugs might directly disrupt the maintenance of CSCs, thus effectively eliminating the roots of tumor progression.
Conclusion
The existence of glioma CSCs prompts a refocusing of our views of cancer biology. Rather than a bulk of equally potent neoplastic cells, gliomas appear to have a cellular hierarchy. Within this hierarchy, glioma CSCs represent cells with an extraordinary capacity for tumorigenesis, making them attractive targets for anti-glioma therapies. Unfortunately, glioma CSCs are also highly resistant to traditional therapies, making the development of novel treatments against CSCs an urgent task. Remarkable insights have been gained through recent studies of signaling pathways that are differentially regulated in CSCs and non-stem cancer cells. In addition to the signaling discussed above, other oncogenic signals (e.g. Ras/mitogen-activated protein kinase (MAPK) pathway) or tumor suppressors (e.g. p53) may play important roles in glioma CSCs. CSCs may be more dependent on oncogenic signaling motifs, so selectively and effectively targeting these oncogenes may be a promising anti-CSC therapeutic strategy. Blood vessels provide not only nutrition/oxygen to cancer cells but also a favorable microenvironment for the maintenance of CSCs. Thus, anti-angiogenic agents appear promising because they may inhibit tumor growth in two ways: 1) direct interruption of nutrient-supplying vasculature and 2) indirect CSC inhibition by disruption of vascular niches.
As the current methods of CSC identification improve and studies of CSCs in both glioma and non-glioma cancers advance, we anticipate that CSC-directed cancer therapeutics will be a useful component of multipronged anticancer treatment regimens. Further investigations into the molecular underpinnings of glioma CSC biology may not only inform us of the biology of these cells and the tumor as a whole but may also allow a starting ground for rational drug development to improve the prognosis of patients with a variety of cancers.
Supplementary Material
This work was supported, in whole or in part, by National Institutes of Health Grants CA129958, CA116659, and NS054276. This work was also supported by the Damon Runyon Cancer Research Foundation, the Goldhirsh Foundation, and the Brain Tumor Society. This minireview will be reprinted in the 2009 Minireview Compendium, which will be available in January, 2010.
- CSC
- cancer stem cell
- NSC
- neural stem cell
- RTK
- receptor tyrosine kinase
- EGFR
- epidermal growth factor receptor
- BMP
- bone morphogenetic protein
- BMPR
- BMP receptor
- miRNA
- microRNA
- VEGF
- vascular endothelial growth factor.
REFERENCES
- 1.Bhatia M., Wang J. C., Kapp U., Bonnet D., Dick J. E. ( 1997) Proc. Natl. Acad. Sci. U. S. A. 94, 5320– 5325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cho R. W., Clarke M. F. ( 2008) Curr. Opin. Genet. Dev. 18, 48– 53 [DOI] [PubMed] [Google Scholar]
- 3.Jordan C. T. ( 2009) Cell Stem Cell 4, 203– 205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh S. K., Hawkins C., Clarke I. D., Squire J. A., Bayani J., Hide T., Henkelman R. M., Cusimano M. D., Dirks P. B. ( 2004) Nature 432, 396– 401 [DOI] [PubMed] [Google Scholar]
- 5.Bao S., Wu Q., McLendon R. E., Hao Y., Shi Q., Hjelmeland A. B., Dewhirst M. W., Bigner D. D., Rich J. N. ( 2006) Nature 444, 756– 760 [DOI] [PubMed] [Google Scholar]
- 6.Ma S., Lee T. K., Zheng B. J., Chan K. W., Guan X. Y. ( 2008) Oncogene 27, 1749– 1758 [DOI] [PubMed] [Google Scholar]
- 7.Bachoo R. M., Maher E. A., Ligon K. L., Sharpless N. E., Chan S. S., You M. J., Tang Y., DeFrances J., Stover E., Weissleder R., Rowitch D. H., Louis D. N., DePinho R. A. ( 2002) Cancer Cell 1, 269– 277 [DOI] [PubMed] [Google Scholar]
- 8.Li L., Dutra A., Pak E., Labrie J. E., III, Gerstein R. M., Pandolfi P. P., Recht L. D., Ross A. H. ( 2009) Neuro-oncology 11, 9– 21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alcantara Llaguno S., Chen J., Kwon C. H., Jackson E. L., Li Y., Burns D. K., Alvarez-Buylla A., Parada L. F. ( 2009) Cancer Cell 15, 45– 56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Soeda A., Inagaki A., Oka N., Ikegame Y., Aoki H., Yoshimura S.-i., Nakashima S., Kunisada T., Iwama T. ( 2008) J. Biol. Chem. 283, 10958– 10966 [DOI] [PubMed] [Google Scholar]
- 11.Reddi A. H. ( 1997) Cytokine Growth Factor Rev. 8, 11– 20 [DOI] [PubMed] [Google Scholar]
- 12.Panchision D. M., McKay R. D. ( 2002) Curr. Opin. Genet. Dev. 12, 478– 487 [DOI] [PubMed] [Google Scholar]
- 13.Piccirillo S. G., Reynolds B. A., Zanetti N., Lamorte G., Binda E., Broggi G., Brem H., Olivi A., Dimeco F., Vescovi A. L. ( 2006) Nature 444, 761– 765 [DOI] [PubMed] [Google Scholar]
- 14.Lee J., Son M. J., Woolard K., Donin N. M., Li A., Cheng C. H., Kotliarova S., Kotliarov Y., Walling J., Ahn S., Kim M., Totonchy M., Cusack T., Ene C., Ma H., Su Q., Zenklusen J. C., Zhang W., Maric D., Fine H. A. ( 2008) Cancer Cell 13, 69– 80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park Y., Rangel C., Reynolds M. M., Caldwell M. C., Johns M., Nayak M., Welsh C. J., McDermott S., Datta S. ( 2003) Dev. Biol. 253, 247– 257 [DOI] [PubMed] [Google Scholar]
- 16.Wechsler-Reya R. J., Scott M. P. ( 1999) Neuron 22, 103– 114 [DOI] [PubMed] [Google Scholar]
- 17.Dahmane N., Sanchez P., Gitton Y., Palma V., Sun T., Beyna M., Weiner H., Ruiz i, Altaba A. ( 2001) Development (Camb.) 128, 5201– 5212 [DOI] [PubMed] [Google Scholar]
- 18.Clement V., Sanchez P., de Tribolet N., Radovanovic I., Ruiz i, Altaba A. ( 2007) Curr. Biol. 17, 165– 172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bar E. E., Chaudhry A., Lin A., Fan X., Schreck K., Matsui W., Piccirillo S., Vescovi A. L., DiMeco F., Olivi A., Eberhart C. G. ( 2007) Stem Cells 25, 2524– 2533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gaiano N., Fishell G. ( 2002) Annu. Rev. Neurosci. 25, 471– 490 [DOI] [PubMed] [Google Scholar]
- 21.Solecki D. J., Liu X. L., Tomoda T., Fang Y., Hatten M. E. ( 2001) Neuron 31, 557– 568 [DOI] [PubMed] [Google Scholar]
- 22.Androutsellis-Theotokis A., Leker R. R., Soldner F., Hoeppner D. J., Ravin R., Poser S. W., Rueger M. A., Bae S. K., Kittappa R., McKay R. D. ( 2006) Nature 442, 823– 826 [DOI] [PubMed] [Google Scholar]
- 23.Purow B. W., Haque R. M., Noel M. W., Su Q., Burdick M. J., Lee J., Sundaresan T., Pastorino S., Park J. K., Mikolaenko I., Maric D., Eberhart C. G., Fine H. A. ( 2005) Cancer Res. 65, 2353– 2363 [DOI] [PubMed] [Google Scholar]
- 24.Fan X., Mikolaenko I., Elhassan I., Ni X., Wang Y., Ball D., Brat D. J., Perry A., Eberhart C. G. ( 2004) Cancer Res. 64, 7787– 7793 [DOI] [PubMed] [Google Scholar]
- 25.Hallahan A. R., Pritchard J. I., Hansen S., Benson M., Stoeck J., Hatton B. A., Russell T. L., Ellenbogen R. G., Bernstein I. D., Beachy P. A., Olson J. M. ( 2004) Cancer Res. 64, 7794– 7800 [DOI] [PubMed] [Google Scholar]
- 26.Fan X., Matsui W., Khaki L., Stearns D., Chun J., Li Y. M., Eberhart C. G. ( 2006) Cancer Res. 66, 7445– 7452 [DOI] [PubMed] [Google Scholar]
- 27.Shih A. H., Holland E. C. ( 2006) Neoplasia 8, 1072– 1082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang X. P., Zheng G., Zou L., Liu H. L., Hou L. H., Zhou P., Yin D. D., Zheng Q. J., Liang L., Zhang S. Z., Feng L., Yao L. B., Yang A. G., Han H., Chen J. Y. ( 2008) Mol. Cell. Biochem. 307, 101– 108 [DOI] [PubMed] [Google Scholar]
- 29.Takahashi K., Yamanaka S. ( 2006) Cell 126, 663– 676 [DOI] [PubMed] [Google Scholar]
- 30.Herms J. W., von Loewenich F. D., Behnke J., Markakis E., Kretzschmar H. A. ( 1999) Surg. Neurol. 51, 536– 542 [DOI] [PubMed] [Google Scholar]
- 31.Wang J., Wang H., Li Z., Wu Q., Lathia J. D., McLendon R. E., Hjelmeland A. B., Rich J. N. ( 2008) PLoS ONE 3, e3769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jensen N. A., Pedersen K. M., Lihme F., Rask L., Nielsen J. V., Rasmussen T. E., Mitchelmore C. ( 2003) J. Biol. Chem. 278, 8300– 8308 [DOI] [PubMed] [Google Scholar]
- 33.Zheng H., Ying H., Yan H., Kimmelman A. C., Hiller D. J., Chen A. J., Perry S. R., Tonon G., Chu G. C., Ding Z., Stommel J. M., Dunn K. L., Wiedemeyer R., You M. J., Brennan C., Wang Y. A., Ligon K. L., Wong W. H., Chin L., DePinho R. A. ( 2008) Nature 455, 1129– 1133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Du Z., Jia D., Liu S., Wang F., Li G., Zhang Y., Cao X., Ling E.-A., Hao A. ( 2008) Glia 57, 724– 733 [DOI] [PubMed] [Google Scholar]
- 35.Lu Q. R., Sun T., Zhu Z., Ma N., Garcia M., Stiles C. D., Rowitch D. H. ( 2002) Cell 109, 75– 86 [DOI] [PubMed] [Google Scholar]
- 36.Novitch B. G., Chen A. I., Jessell T. M. ( 2001) Neuron 31, 773– 789 [DOI] [PubMed] [Google Scholar]
- 37.Takebayashi H., Yoshida S., Sugimori M., Kosako H., Kominami R., Nakafuku M., Nabeshima Y. ( 2000) Mech. Dev. 99, 143– 148 [DOI] [PubMed] [Google Scholar]
- 38.Zhou Q., Anderson D. J. ( 2002) Cell 109, 61– 73 [DOI] [PubMed] [Google Scholar]
- 39.Ligon K. L., Alberta J. A., Kho A. T., Weiss J., Kwaan M. R., Nutt C. L., Louis D. N., Stiles C. D., Rowitch D. H. ( 2004) J. Neuropathol. Exp. Neurol. 63, 499– 509 [DOI] [PubMed] [Google Scholar]
- 40.Ligon K. L., Huillard E., Mehta S., Kesari S., Liu H., Alberta J. A., Bachoo R. M., Kane M., Louis D. N., DePinho R. A., Anderson D. J., Stiles C. D., Rowitch D. H. ( 2007) Neuron 53, 503– 517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee S. K., Lee B., Ruiz E. C., Pfaff S. L. ( 2005) Genes Dev. 19, 282– 294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dirks P. ( 2007) Cancer Cell 12, 295– 297 [DOI] [PubMed] [Google Scholar]
- 43.Bruggeman S. W., Hulsman D., Tanger E., Buckle T., Blom M., Zevenhoven J., van Tellingen O., van Lohuizen M. ( 2007) Cancer Cell 12, 328– 341 [DOI] [PubMed] [Google Scholar]
- 44.Chiba T., Miyagi S., Saraya A., Aoki R., Seki A., Morita Y., Yonemitsu Y., Yokosuka O., Taniguchi H., Nakauchi H., Iwama A. ( 2008) Cancer Res. 68, 7742– 7749 [DOI] [PubMed] [Google Scholar]
- 45.Chan J. A., Krichevsky A. M., Kosik K. S. ( 2005) Cancer Res. 65, 6029– 6033 [DOI] [PubMed] [Google Scholar]
- 46.Silber J., Lim D. A., Petritsch C., Persson A. I., Maunakea A. K., Yu M., Vandenberg S. R., Ginzinger D. G., James C. D., Costello J. F., Bergers G., Weiss W. A., Alvarez-Buylla A., Hodgson J. G. ( 2008) BMC Med. 6, 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gal H., Pandi G., Kanner A. A., Ram Z., Lithwick-Yanai G., Amariglio N., Rechavi G., Givol D. ( 2008) Biochem. Biophys. Res. Commun. 376, 86– 90 [DOI] [PubMed] [Google Scholar]
- 48.Bao S., Wu Q., Sathornsumetee S., Hao Y., Li Z., Hjelmeland A. B., Shi Q., McLendon R. E., Bigner D. D., Rich J. N. ( 2006) Cancer Res. 66, 7843– 7848 [DOI] [PubMed] [Google Scholar]
- 49.Tavazoie M., Van der Veken L., Silva-Vargas V., Louissaint M., Colonna L., Zaidi B., Garcia-Verdugo J. M., Doetsch F. ( 2008) Cell Stem Cell 3, 279– 288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shen Q., Wang Y., Kokovay E., Lin G., Chuang S. M., Goderie S. K., Roysam B., Temple S. ( 2008) Cell Stem Cell 3, 289– 300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Calabrese C., Poppleton H., Kocak M., Hogg T. L., Fuller C., Hamner B., Oh E. Y., Gaber M. W., Finklestein D., Allen M., Frank A., Bayazitov I. T., Zakharenko S. S., Gajjar A., Davidoff A., Gilbertson R. J. ( 2007) Cancer Cell 11, 69– 82 [DOI] [PubMed] [Google Scholar]
- 52.Vredenburgh J. J., Desjardins A., Herndon J. E., 2nd, Dowell J. M., Reardon D. A., Quinn J. A., Rich J. N., Sathornsumetee S., Gururangan S., Wagner M., Bigner D. D., Friedman A. H., Friedman H. S. ( 2007) Clin. Cancer Res. 13, 1253– 1259 [DOI] [PubMed] [Google Scholar]
- 53.Batchelor T. T., Sorensen A. G., di Tomaso E., Zhang W. T., Duda D. G., Cohen K. S., Kozak K. R., Cahill D. P., Chen P. J., Zhu M., Ancukiewicz M., Mrugala M. M., Plotkin S., Drappatz J., Louis D. N., Ivy P., Scadden D. T., Benner T., Loeffler J. S., Wen P. Y., Jain R. K. ( 2007) Cancer Cell 11, 83– 95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Eyler C. E., Foo W. C., LaFiura K. M., McLendon R. E., Hjelmeland A. B., Rich J. N. ( 2008) Stem Cells 26, 3027– 3036 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.