Abstract
We investigated total prescription and new prescription trends before and after the economic slowdown beginning in September 2008. Over the July to November timeframe, both total prescriptions and new prescriptions for sleep aids, benzodiazepines, and antidepressants increased. There appears to be a small spike in the number of total and new prescriptions following September 2008, although this increase was not enough to cause a statistically significant change in the overall rate of increase of prescriptions over time. Discussion of data is provided.
Keywords: sleep aids, benzodiazepines, antidepressants, economy, prescription trends
Introduction
Recognizing that decreases in financial wealth and increases in unemployment are often associated with stress, anxiety, and depression, we investigated trends in prescribing of sleep aids, benzodiazepines (BZDs), and antidepressants prior to and following the economic slowdown in September 2008.
Methods
Specifically, we examined retail pharmacy prescription data from SDI/Verispan, which captures more than 1.4 billion patient-centric prescriptions per year, nearly half of all prescription activity in the US. This data set includes prescriptions from a variety of retail channels (e.g., national retail chains, mass merchandisers) from a near-census of US pharmacies. The SDI/Verispan retail pharmacy database also captures information from all payer types, including cash. Prescription data were analyzed on a four-week rolling basis to smooth out some of the variation observed with weekly prescription data (e.g., due to holidays).
Results
Figure 1 displays total prescription trends for four different therapeutic groups: sleep aids, BZDs, all antidepressants, and selective serotonin reupake inhibitor (SSRI)/serotonin norephinephrine reuptake inhibitor (SNRI) antidepressants. As seen in Figure 1, total prescriptions for all therapeutic groups have increased over the study timeframe. Although not enough to cause a statistically significant change in the rate of increase over time, there appears to be a small spike in the number of total prescriptions following September 2008.
FIGURE 1.
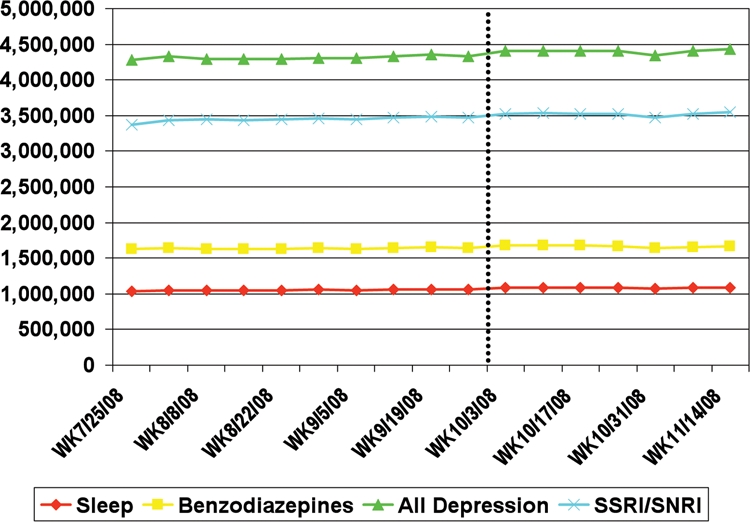
Rolling four-week total prescriptions
Source: SDI/Verispan VONA, TRx: sleep aid market, benzodiazepine class, and antidepressant market
New prescriptions have also increased over the past four months (Figure 2). Similar to the trends in total prescriptions, there has been some increase in new prescriptions following the September economic slowdown, although not enough to significantly affect the rate of increase over time.
FIGURE 2.
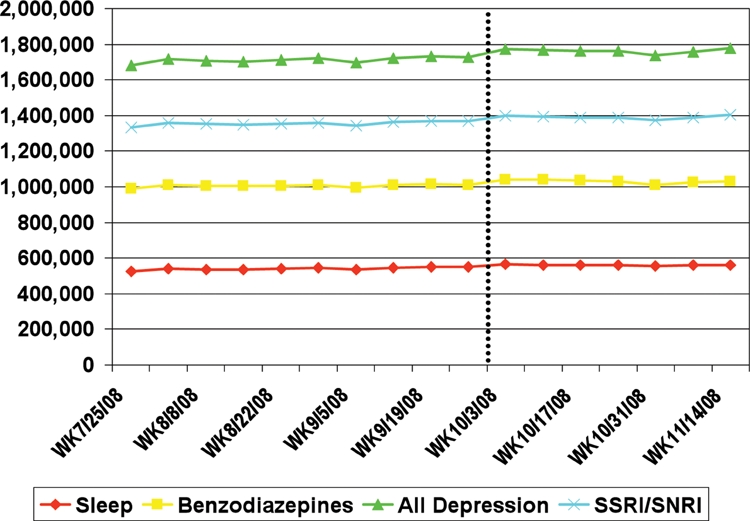
Rolling four-week new prescriptions
Source: SDI/Verispan VONA, NRx: sleep aid market, benzodiazepine class, and antidepressant market
Expert Commentary
by Joseph A. Kwentus, MD
The drugs described in this data are used to treat anxiety and depression. The recent economic downturn has produced significant stress, but it is not possible to determine from the data whether anxiety or depression is more prevalent.
The financial crisis has made millions of Americans anxious. The anxious person typically complains about tension, worry, and physical distress. Many people who have anxiety symptoms do not meet formal Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for an anxiety disorder and they often do not get their care from a psychiatrist. Even when someone meets formal criteria for an anxiety disorder, anxiety levels usually wax and wane. BZD therapy is one of the more common interventions for acute anxiety.
The approach that practitioners take to BZD therapy varies considerably. However, the intensity and duration of therapy will always be tailored to the course of the underlying illness. Although some patients require chronic therapy, the majority of people who use these medications use them intermittently.
The efficacy of BZDs in the treatment of anxiety has been established for almost 50 years. However, BZDs have not been evaluated by modern standards. The first BZD, chlordiazepoxide, was released during the days of DSM-I, and criteria for the diagnosis have changed significantly since those early years.
Dosing was poorly studied in the early BZD trials. Today’s practitioner still struggles with appropriate dosing decisions. Reports of newer meta-analysis have attempted to minimize the role of BZDs on anxiety syndromes. However, the sheer volume of BZD use in the face of the virtual absence of any marketing effort by the pharmaceutical industry would argue that these compounds have a profound effect on their targeted symptoms.
BZDs act on major inhibitory neuronal receptors in the mammalian brain, the gamma-aminobutyric acid type A (GABA (A)) receptors. Modulation of GABA-gated chloride channels is the basis of their anxiolytic, hypnotic, and anticonvulsant properties. The α subunit is the main determinant of selectivity at the GABA (A) receptor. The α1 subtype is proposed to be responsible for the sedative action; the α2 and/or the α3 subtypes are thought to mediate the anxiolytic properties and the muscular effects; and the α5 subtype is associated with cognition. There has been considerable effort to improve the selectivity of the BZDs. The non-BZD hypnotics have increased selectivity at the α1 subtype. Drugs with increased selectivity at other receptor subtypes are currently under investigation.
People who use BZDs tend to develop tolerance to the side effects rather than to the anxiolytic effects. Even so, adverse effects can be significant. Major adverse effects created by BZDs include abuse, dependency, cognitive disorders, and motor impairment. BZDs may contribute to motor vehicle and industrial accidents when used in combination with other sedatives or in the presence of certain medical disorders, such as sleep apnea. While BZD abusers constitute a small group that usually has a history of abuse of other substances, the prescriber must remain ever vigilant for misuse and diversion.
It is generally accepted that anxiety disorders are commonly undertreated and that the people who should benefit from BZDs are not receiving them. Nonetheless, there are many others who are receiving BZDs that do not really need them.
Depression may also be an anticipated outcome of the trauma associated with the economic downturn. Many antidepressants have been shown to be extremely effective for anxiety as well as depression. Still, antidepressants are not as valuable for relieving anxiety in a crisis as they are for treating long-standing depression and chronic anxiety. The most common drugs used today to treat depression and anxiety impact the brain chemicals serotonin, norepinephrine, and dopamine. The major limitation to these interventions includes low response rate, long response lag, and high rates of relapse.
Increasing evidence indicates that other targets may prove beneficial. The hypothalamic pituitary axis and specifically corticotropin-releasing factor (CRF) have gotten some attention. It has been known for a long time that abnormally high levels of this stress hormone are frequently present in those with depression. Drugs that block CRF or its effects may have the potential to lift the mood of depressed people. A variety of CRF-blocking drugs and drugs that affect the hypothalamic pituitary axis are currently in development.
A major recent advance in neuroscience is the growing appreciation of the role that neuroplasticity plays in the adult brain. The growth factor brainderived neurotrophic factor (BDNF) has been extensively studied with respect to the pathophysiology of depression. Chronic social stress may impact BDNF in selective brain areas. There is evidence that stress is associated with increased levels of glutamatergic activation in several important areas of the brain. There are many lines of research that are dedicated to finding new avenues of intervention in glutamatergic transmission.
A brief discussion cannot do justice to such an enormous topic. Hopefully the economic downturn will not be as deep or as extensive as has been expected. Perhaps the next time we track drug utilization during a crisis, we will have more effective and safer drugs to deal with the aftermath.
Contributor Information
Elisa Cascade, Ms. Cascade is Vice President, Quintiles Inc./iGuard, Falls Church, Virginia.
Amir H. Kalali, Dr. Kalali is Vice President, Global Therapeutic Group Leader CNS, Quintiles Inc., San Diego, California, and Professor of Psychiatry, University of California, San Diego.
Joseph A. Kwentus, Dr. Kwentus is Professor, Department of Psychiatry and Human Behavior, University of Mississippi Medical Center, Jackson, Mississippi.
Murtuza Bharmal, Dr. Bharmal is Associate Director, Medical Affairs, Epidemiology and Outcomes Research, Quintiles, Inc., Falls Church, Virginia.


