Abstract
Background
The length of hospice stay, as an indicator of timing of hospice referral, is an important outcome to examine in end-of-life care because it is relevant to the quality and cost efficiency of end-of-life care that patients receive. Although the majority receives nonmedical care from informal caregivers, many elderly hospice users rely on paid caregivers or staff of residential facilities.
Objective
This study examined whether availability of informal primary caregiver interact with ethnicity to affect length of hospice stay.
Design
A retrospective cross-sectional study.
Setting/subjects
Data on 3024 hospice patients aged 65 and older discharged between 1997 and 2000 was extracted from the National Center for Health Statistics' National Home and Hospice Care Survey (NHHCS).
Measurements
Length of hospice stay prior to death or discharge.
Results
Survival analysis revealed that among patients with formal caregivers, minority patients were likely to have significantly shorter hospice stays than non-Hispanic whites. There were no significant ethnic differences in length of stay among patients with informal caregivers.
Conclusions
Our findings suggest that ethnic differences in length of stay should be discussed in terms of type of caregiver, not just type of setting, since patients in residential facilities can have informal primary caregivers who are vigilant advocates for their dying relatives. We discuss possible reasons for the influence of having formal caregivers on length of stay of minority elders.
INTRODUCTION
MEDICARE ADDED THE Hospice Benefit (MHB) in 1983 to provide comprehensive palliative and supportive services to dying patients and their families.1 In spite of a rapid increase in MHB utilization, there has been growing concern among service providers and policy makers that many patients are enrolling in hospice too late for optimal benefits.2 The median stay declined from 26 days in 1992 to 15 days in 2002.1,3 Dying in less than a week is not rare: from 1998 to 2002, more than one in four MHB beneficiaries stayed for less than a week.4 When enrollment occurs too close to death, hospice providers may have inadequate time to establish relationships with the dying patient and family members, to address pain and suffering, and to provide complex and intensive services, such as continuous home care. It is therefore important to identify populations who are at risk of being referred to hospice care at a less than optimal length of time prior to death. Despite overall increase in the number of hospice users, the gap between white and minority patients in utilizing hospice care has remained little changed.4 Reasons offered for this underutilization include a lack of knowledge in the minority community of the availability and benefits of hospice care, among others. In addition, many eligible persons do not receive hospice care because of an unwillingness on their part, their caregiver's part, and/or their physician's part, to accept and discuss end-of-life care.3,5 Although the same reasons for the underutilization are also offered for late referrals to hospice,3 previous studies report rather opposite finding, that is, that there is a longer stay among minority patients than among white patients.6-8
To determine the difference in length of stay between whites and minority hospice decedents, this study decided to examine the potentially intermediary effect of the availability of informal caregiver, a key component in end of life care of dying elderly and in more general long-term care of frail elderly.9,10 The majority of hospice patients have informal (i.e., unpaid) primary caregivers, who are bound to them by ties of commitment and considered as family. Informal caregivers' roles and tasks change as illness progresses and the setting for care changes. They provide vital assistance with activities of daily living and carry out most treatment recommendations for patients living in private residences. When patients move from their home to facilities, these caregivers become less responsible for around-the-clock supervision and hands-on care, but instead provide companionship and assume an executive functioning role to uphold patients' wishes and manage patients' total needs.11,12 Even for individuals dying in a hospital from serious and life-threatening illnesses, family caregiving is typically at the core of what sustains them until the end of life.13 They frequently handle difficult tasks of final decision making, such as withdrawal of life support13 or enrollment in hospice and discontinuation of curative treatment.14
Lack of an informal caregiver is a barrier to receipt of hospice care for individuals in private residences, thus increasing the likelihood of delayed access to hospice. Some hospice programs limit participation to beneficiaries who have a caregiver in their homes.15 Therefore, to receive hospice care, elders who do not have informal caregivers may need to move to more expensive facilities.16 In spite of the seeming importance of primary caregiving for receipt of hospice care, little study has been done on whether the availability of informal caregiving differently affects the timing of referral between minority patients and white patients. Previous studies8,17 examining length of stay between a nursing home versus home setting of hospice care are likely to lead one to assume that, once a patient moves to health facilities including nursing homes, there would be no informal caregiver present for the individual. This assumption prevents one from distinguishing patients for whom informal caregivers play roles from those for whom informal caregivers do not exist or do not assume roles as primary caregivers. Such distinction is necessary because the latter elders are most likely to report a staff member as a primary caregiver, unlike their counterparts who would probably report family members as primary caregivers even though they reside in health facilities. Our study addressed the following question: does relationship between race/ethnicity and length of elders' stay in hospice vary by primary caregiving status (having an informal primary caregiver versus having a formal primary caregiver such as a staff member)?
METHODS
Data source
The study used hospice discharge data from the 1998 and 2000 National Center for Health Statistics' National Home and Hospice Care Survey (NHHCS), the fifth and sixth in a series of surveys conducted by the National Center for Health Statistics (NCHS).18 The respondent providing information for each discharged person was the staff member most familiar with that person's care. Respondents referred to patient medical records and other records as necessary. We pooled data from the 2 years to solve the problem of small sample size resulting from the categorization of subjects into four combinations of caregiver type (informal versus formal) and ethnicity (white versus nonwhite). We excluded younger hospice users because caregiver issues tend to be less serious among them than among elders. Younger hospice users are more likely than older counterparts to have relatives such as parents or spouses than the MHB elderly population, which is becoming increasingly older.19 Detailed information on NHHCS is available elsewhere.5,18
Variables
Length of stay
Length of stay in hospice was measured by days from date of hospice enrollment until termination of hospice care.
Caregiver type
Caregiver type (or “caregiver group”) referred to whether the hospice patient had an informal primary caregiver or formal primary caregiver prior to hospice discharge. A primary care-giver was defined as an individual who was responsible for providing personal care assistance, companionship, and/or supervision to the patient. The patient's caregiver type was identified by answers to two survey questions: (1) “Did she/he have a primary caregiver outside of this hospice?” and (2) “What was the relationship of the primary caregiver to the patient?” (asked if the answer to the first question was yes). If the answer was yes, information from the follow-up question was used to identify the patient's caregiver as either an unpaid, informal caregiver (if the caregiver was reported as spouse, child, sister/brother, other relative, or friend /neighbor) or a paid, formal caregiver (if the caregiver was reported as paid help or a staff member in a facility where the patient resided).
Race/ethnicity (referred to henceforth as “ethnicity”)
The interview questionnaire asks two questions: the first regarding Hispanic origin and the second regarding specific racial backgrounds. A person who was not reported as being of Hispanic origin and whose race was reported as white was categorized as non-Hispanic white (referred to as “white” hereafter). All others were categorized as minority ethnic status. Inadequate sample size precluded further breakdown of ethnicity beyond “white” and all others, whom we considered ethnic minority population.
Control variables/covariates
Other variables included as control variables in our analyses included survey year and five characteristics of the patient: age, gender, diagnosis at admission, having a hospital referral source, and living status (living alone or with others). A dichotomous variable was created to indicate whether the patient was referred from a hospital or not. Hospital referral indicates that the patient experienced hospitalization immediately before moving to hospice.
The principal diagnosis at admission was categorized as one of the following: cancer, dementia, heart disease, stroke, chronic obstructive pulmonary disease (COPD), or other. Unlike cancer where the trajectory to disease is relatively simple, noncancerous diseases may involve multiple crises before death, thus complicating the decision of when to enter hospice.20
Finally, we included the dummy variable whether or not a patient lived alone at the time of discharge, because according to the 2000 NHHCS report,5 hospice patients who lived alone at the time of death had relatively long stays. Patients living alone reside in private/semi private residences or assisted living/residential facilities.
Statistical analyses
Despite long-standing concern about short lengths of stays, there is no widely accepted definition of what constitutes an acceptable minimum length of stay (i.e., a stay long enough for hospice care to be effective).21-23 Depending on the measures and definitions of acceptable minimum stay, different conclusions can be drawn because the criteria for “timely” access to hospice care is set differently. To address this issue, we used survival analysis to present a 6-month window of time for following patients from admission until death. Use of survival curves allowed for a full investigation less constrained by particular definitions of short stay, untimely access, or minimum acceptable length. The 6-month point reflects the MHB eligibility criterion of a prognosis of six months or less to live. The 6-month window of time also allowed us to examine survival at month 2, which reflects the end of the first MHB benefit period before recertification is required.
Time to death following hospice enrollment (measured in days) was compared between ethnic categories within each caregiver type separately. Specifically, based on Kaplan-Meier curves, survival rates at each point of time and their confidence intervals were estimated. Patients who left hospice for reasons other than death were treated as censored observations.
In addition to the univariate Kaplan-Meier method, multivariate analyses were conducted using Cox proportional hazard models to estimate death rates adjusted for possible confounding factors (the control variables described above). We first estimated Cox models with only one covariate at a time. Covariates whose p value is less than 0.2 in these unadjusted analyses were entered into the final model. To check if proportional hazards assumptions were met, we examined whether time interaction terms for the covariates had a p 0.05, suggesting no evidence of increasing or decreasing trends over time in the hazard ratio among levels of covariates. Tests of interactions with time indicated no significant lack of proportionality except for caregiver type. To avoid the violation of proportionality assumptions, we entered the caregiver type as a strata variable for the combined analysis, and separate Cox models were constructed for each caregiver group. Relative risks (hazard ratios), 95% confidence intervals, and p values were derived from the final multivariate Cox proportional hazards models. The final Cox proportional hazards model for each caregiver type was then used to generate survival curves corresponding to each ethnic category, varying only the category while holding other covariates constant. This enabled us to estimate the effect of race/ethnicity on length of stay, holding other confounders constant. The resulting predicted survival curves reflect the different underlying shapes across time for the two ethnic categories. Sampling weights were used for data analyses and all data analyses were done using SAS version 9.1 (SAS Institute Inc., Cary, NC).
RESULTS
The majority of our study hospice elders had informal primary caregivers (83%; Table 1). Minority elders accounted for 24% of the formal caregiver group, and 27% of the informal caregiver group. Compared to elders in the formal caregiver group, the informal caregiver group was more likely to die of cancer, with slightly more than 60% dying of cancer.
Table 1.
Comparison of Characteristics of Hospice Discharges by Caregiver Type
| Caregiver type |
|||
|---|---|---|---|
| Characteristic | Total | Informal | Formal |
| Sample size, No. (%) | |||
| Actual | 3,024 | 2,484 (82.14) | 540 (17.86) |
| Weighted | 767,051 | 634,420 (82.71) | 132,631 (17.29) |
| Death, % (SE) | 86.90 (1.68) | 87.09 (1.82) | 85.09 (4.01) |
| Age, mean, 95% CI | 79.36 (0.40) | 78.33 (0.39) | 84.00 (0.94) |
| Women, % (SE) | 52.17 (2.35) | 51.26 (2.44) | 58.38 (6.67) |
| Race/ethnicity: minority, % (SE) | 26.15 (1.82) | 27.61 (2.06) | 23.68 (5.48) |
| Diagnosis: noncancera | 44.23 (2.35) | 39.48 (2.46) | 61.18 (6.47) |
| Residence During Care: Facilitya,b | 34.58 (2.01) | 21.43 (2.05) | 90.85 (3.35) |
All figures are weighted.
p < 0.001.
Facility is defined as board and care, assisted living facility, residential care facility, and institutional setting such as nursing home, inpatient hospice unit, hospital hospice unit or psychiatric hospital.
SE, standard error; CI, confidence interval.
Almost 91% of the formal caregiver group resided in facilities defined as board and care, assisted living facilities, residential care facilities, and institutional settings including nursing homes, inpatient hospice units, hospital hospice units, or psychiatric hospitals. The remaining 9% of the formal caregiver group lived in their own private residences with assistance from paid caregivers. Although the formal caregiver type was significantly associated with living in a facility, hospice users in facilities did not necessarily have formal caregivers. Slightly more than 21% of the informal caregiver group, or 1 in 5, resided in facilities.
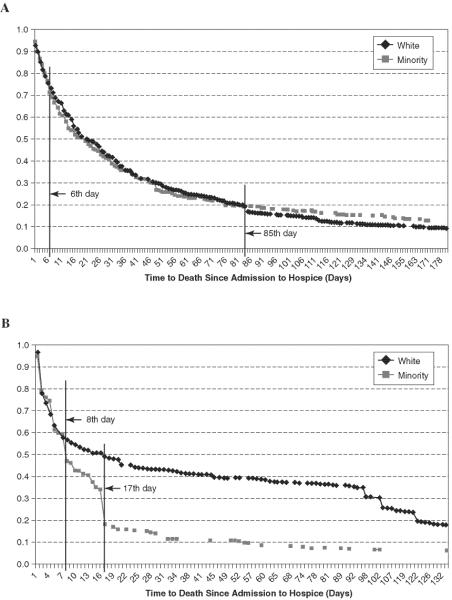
The Kaplan-Meier survival curves were plotted against days to death since enrollment—up to around 180 days (or about 6 months). Overall survival estimates for whites and for minorities in the informal caregiver group (Fig. 1A) were not significantly different. In contrast, the survival curve for the formal caregiver group (Fig. 1B) shows a significant difference between white and minority patients. During the first week, there was no clear difference in survival, but immediately after that, significantly more minorities than whites died.
FIG. 1.
Kaplan-Meier survival curves. A: Whites versus minority informal caregiver group. B: Whites versus minority formal caregiver group.
Whereas the Kaplan-Meier curves provide unadjusted hazards of dying, multivariate Cox proportional hazards models were constructed to estimate hazard ratios by ethnic status (minority survival rates relative to white rates) adjusted for potential confounders (age, gender, living arrangement during hospice care, diagnosis at admission, hospital referral, and survey year) (Table 2). A hazard ratio (HR) > 1.00 indicates shorter stays on average in hospice (thus a faster death rate) for minorities than for whites, and a ratio < 1.00 indicates a slower average death rate than for minorities than for whites.
Table 2.
Hazard Ratios for Length of Stay in Hospice by Caregiver Type
| Caregiver type |
|||
|---|---|---|---|
| Variable | All | Informal | Formal |
| Cancer | 0.89 | 0.81b | 1.67b |
| Dementia | 0.94 | 1.06 | 1.26 |
| Heart | 0.78a | 0.81a | 1.07 |
| Stroke | 1.34b | 1.12 | 1.62 |
| COPD | 0.68b | 0.61b | 1.30 |
| Hospital referral | 0.88 | 1.11 | 0.64b |
| Male | 1.20b | 1.13a | 1.66b |
| Age | 0.85b | 0.86b | 0.93 |
| Age | 1.00b | 1.00b | 1.00 |
| Alone | 0.54b | 0.57b | 1.17 |
| Year 2000 | 0.98 | 0.93 | 1.09 |
| Minority | 1.02 | 1.00 | 1.76b |
p < 0.05.
p < 0.01.
Reference group for cancer, dementia, heart, stroke, and COPD is all other diagnoses.
COPD, chronic obstructive pulmonary disease.
Using the entire sample, when we adjusted for potential confounders, there was no statistically significant difference between white and minority hospice patients (adjusted HR = 1.05; p = 0.29). However, ethnic patterns differed by caregiver type. There was no ethnic difference in length of stay among the informal caregiver group, but when patients had formal caregivers, minorities had significantly shorter stays in hospice than whites (adjusted HR=1.76; p < 0.001).
Figure 2 depicts four Cox proportional regression survival curves based on four hypothetical patients. The four patients differed only in ethnicity and care-giver type. They were identical in terms of the six covariates, set to: male, age 90, dementia as a primary diagnosis at admission, referral from hospital, not living alone during care, and died in survey year 2000. The two curves for the informal caregiver group overlap almost completely, indicating no ethnic differences in predicted survival. Among patients with formal caregivers with covariates held constant, minorities have a faster death rate than whites.
FIG. 2.
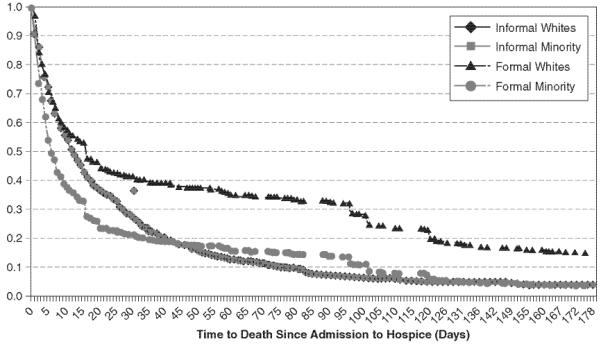
Cox survival curves by caregiver type: white versus minority.
DISCUSSION
Our major finding is that older hospice patients whose primary caregivers are paid caregivers or staff members in facilities where they reside have significantly shorter stays when they are ethnic minority patients. As displayed in Figure 2 above, this difference is of a significant magnitude (e.g., median survival of 7 days for minority patients compared to 16 days for whites with the particular covariate profile we selected). By contrast, minority group status appears to have no effect on length of stay for older adults with informal primary caregivers. These patterns hold true even after adjusting for other clinical and demographic factors.
Considering that many of the formal caregiver group were in nursing homes, these findings are consistent with previous research indicating racial disparity in the quality of nursing home care.24,25 Such racial disparity in access to quality nursing home care may impede enrollment in hospice among minority residents who lack informal caregivers, since they are likely to receive inadequate attention and advocacy from nursing home staff.12
In light of research associating nonwhite status with short life expectancy or poor health outcomes,26-28 one might suspect that minorities with formal caregivers have worse baseline health status to begin with than their white counterparts. However, if this were the case, then it would be highly likely that minorities with informal caregivers also have worse baseline health status than their white counterparts. Instead, we found no significant ethnic difference in survival duration among the informal caregiver group. Another possible explanation for the difference in length of stay between minorities and whites with formal caregivers is a differential hospice effect. That is, the difference could be that minorities with formal caregivers receive poorer care in hospice than whites and therefore die sooner (not that they enroll later).
Our discussion of the findings is tempered by several limitations. First, the NHHCS, the source of data for this study, may not provide a large enough sample to detect racial/ethnic disparities, even after combining all but non-Hispanic whites into one group. In addition, further breakdown of ethnic status, beyond “white” and all others, was not possible given the small size of subgroups in the sample. The makeup of our sample reflects the current Medicare population in general (whites account for more than 78%)29 and the current Medicare Hospice beneficiaries (whites accounts for approximately 90%).4 As previous researchers30 have noted, oversampling of minorities in federal survey data is needed in order to identify populations in greatest risk.
A second limitation is that classification of patients into caregiver groups was based on the subjective determination of the hospice worker as to whether an individual had an informal or formal caregiver. Although this may be a serious drawback of this study, MHB claim data or nursing home data do not provide the needed information. Interviewing this population, particularly those patients without involved family members, is a daunting job. This may explain why most studies exclusively rely on families of decedents, leaving little information on decedents without families. In that sense, this study may fill a void, although more rigorous studies should be undertaken.
A third limitation is the possibility that the findings were influenced by informative censoring of minorities in the survival analyses, particularly of African Americans. African Americans were more likely than whites and other ethnic groups to be discharged from hospice for reasons other than death. This was particularly true for African Americans whose primary caregiver was a formal caregiver, with almost 1 in 4 discharged before death. In the majority of cases, patients were discharged alive because their condition had stabilized, likely resulting in their loss of eligibility of MHB. Other patients were transferred to hospitals or nursing homes; suggesting voluntary disenrollment from hospice. Regardless of ethnicity, those discharged alive tended to stay much longer than their counterparts who died while in hospice care, and there was little difference between ethnic groups in time from enrollment to discharge for patients discharged alive. Therefore, excluding those discharged alive from our analysis would not have altered our major finding that older hospice patients whose primary caregivers are paid caregivers or staff members in facilities where they reside have significantly shorter stays when they are ethnic minority patients.
Finally the data set provided no indicators of socioeconomic status. We therefore were unable to control for variables such as education and income, which are related to ethnicity and may influence the relationship between caregiving and end-of-life care.
In spite of these limitations, our research breaks new ground in studying a previously uninvestigated relationship—the joint influence of ethnicity and caregiving on duration of hospice care. Our findings suggest that ethnic differences in length of stay should be discussed in terms of type of caregiver, not just type of setting, since patients in residential facilities can have informal primary caregivers who are vigilant advocates for their dying relatives. Relating to the interaction of ethnicity with type of caregiver, we have posed several possible explanations why referral to hospice for minorities with formal caregivers, possibly longstay residents in facilities, appears to be late compared to non-Hispanic whites in seemingly the same situation. However, there is a need for further research to understand the reasons for this apparent health disparity. Such research is particularly important when one considers that the magnitude of difference in length of stay was found to be quite large (HR = 1.76) and the difference mainly came from the first 3-week period after enrollment.
REFERENCES
- 1.Medicare Payment Advisory Commission . Report to the Congress: New Approaches in Medicare. MedPAC; Washington, D.C.: 2004. Hospice care in Medicare: Recent trends and a review of the issues. [Google Scholar]
- 2.Miller SC, Mor V, Teno J. Hospice enrollment and pain assessment and management in nursing homes. J Pain Symptom Manage. 2003;3:791–799. doi: 10.1016/s0885-3924(03)00284-7. [DOI] [PubMed] [Google Scholar]
- 3.U.S. General Accounting Office . Medicare: More Beneficiaries Use Hospice but for Fewer Days of Care. GAO-HEHS-00-182; Washington, D.C.: Sep, 2000. [Google Scholar]
- 4.Medicare Payment Advisory Commission . Report to the Congress: Increasing the Value of Medicare. MedPAC; Washington, DC: 2006. Medicare's hospice benefit: Recent trends and consideration of payment system refinements. [Google Scholar]
- 5.Haupt BJ. Vital Health Stat 13(154) National Center for Health Statistics; Atlanta, GA: 2003. Characteristics of hospice care discharges and their length of service: United States, 2000. [PubMed] [Google Scholar]
- 6.Christakis NA, Iwashyna TJ. Impact of individual and market factors on the timing of initiation of hospice terminal care. Med Care. 2000;38:528–541. doi: 10.1097/00005650-200005000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Somova MJ, Somov PG, Lawrence JC, Frantz TT. Factors associated with length of stay in a mid-sized, urban hospice. Am J Hosp Palliat Care. 2000;17:99–105. doi: 10.1177/104990910001700209. [DOI] [PubMed] [Google Scholar]
- 8.Miller SC, Weitzen S, Kinzbrunner B. Factors associated with the high prevalence of short hospice stays. J Palliat Med. 2003;6:725–736. doi: 10.1089/109662103322515239. [DOI] [PubMed] [Google Scholar]
- 9.Emanuel EJ, Fairclough DL, Slutsman J, Alpert H, Baldwin D, Emanuel LL. Assistance from family members, friends, paid care givers, and volunteers in the care of terminally ill patients. N Engl J Med. 1999;341:956–963. doi: 10.1056/NEJM199909233411306. [DOI] [PubMed] [Google Scholar]
- 10.Spillman BC, Pezzin LE. Potential and active family caregivers: Changing networks and the “sandwich generation.”. Milbank Q. 2000;78:347–374. doi: 10.1111/1468-0009.00177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hauser JM, Kramer BJ. Family caregivers in palliative care. Clin Geriatr Med. 2004;20:67–688. doi: 10.1016/j.cger.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 12.Port CL. Informal caregiver involvement and illness detection among cognitively impaired nursing home residents. J Gerontol A Biol Sci Med Sci. 2006;61:970–974. doi: 10.1093/gerona/61.9.970. [DOI] [PubMed] [Google Scholar]
- 13.Prendergast TJ, Puntillo KA. Withdrawal of life support: Intensive caring at the end of life. JAMA. 2002;288:2732–2740. doi: 10.1001/jama.288.21.2732. [DOI] [PubMed] [Google Scholar]
- 14.Chen H, Haley WE, Robinson BE, Schonwetter RS. Decisions for hospice care in patients with advanced cancer. J Am Geriatr Soc. 2003;51:789–797. doi: 10.1046/j.1365-2389.2003.51252.x. [DOI] [PubMed] [Google Scholar]
- 15.Enguidanos S, Yip J, Wilber K. Ethnic variation in site of death of older adults dually eligible for Medicaid and Medicare. J Am Geriatr Soc. 2005;53:1411–1416. doi: 10.1111/j.1532-5415.2005.53410.x. [DOI] [PubMed] [Google Scholar]
- 16.Miller SC, Gozalo P, Mor V. Use of Medicare's hospice benefit by nursing facility residents. In: Important questions for hospice in the next century. Washington, D.C.: U.S. Department of Health and Human Services, Office of Disability, Aging and Long-Term Care Policy and The Urban Institute. 2000 Contract No.:100-97-0010. www. aspe.hhs.gov/daltcp/reports/nufares.htm (Last accessed February 16, 2008)
- 17.Casarett DJ, Hirschman KB, Henry MR. Does hospice have a role in nursing home care at the end of life? J Am Geriatr Soc. 2001;49:1493–1498. doi: 10.1046/j.1532-5415.2001.4911242.x. [DOI] [PubMed] [Google Scholar]
- 18.Haupt BJ. Development of the National Home and Hospice Care Survey. Series 1: programs and collection procedures. Vital Health Stat 1. 1994;Sept(33):1–153. [PubMed] [Google Scholar]
- 19.Campbell DE, Lynn J, Louis TA, Shugarman LR. Medicare program expenditures associated with hospice use. Ann Intern Med. 2004;140:269–278. doi: 10.7326/0003-4819-140-4-200402170-00009. [DOI] [PubMed] [Google Scholar]
- 20.Fox E, Landrum-McNiff K, Zhong Z, Dawson NV, Wu AW, Lynn J. Evaluation of prognostic criteria for determining hospice eligibility in patients with advanced lung, heart, or liver disease. JAMA. 1999;282:1638–1645. doi: 10.1001/jama.282.17.1638. [DOI] [PubMed] [Google Scholar]
- 21.Emanuel LL, von Gunten CF, Ferris FD. Gaps in end-of-life care. Arch Fam Med. 2000;9:1176–1180. doi: 10.1001/archfami.9.10.1176. [DOI] [PubMed] [Google Scholar]
- 22.Lynn J. Serving patients who may die soon and their families: The role of hospice and other services. JAMA. 2001;285:925–932. doi: 10.1001/jama.285.7.925. [DOI] [PubMed] [Google Scholar]
- 23.Huskamp H, Beeuwkes-Buntin M, Wang V, Newhouse J. Providing care at the end of life: do Medicare rules impede good care? Health Aff (Millwood) 2001;20:204–211. doi: 10.1377/hlthaff.20.3.204. [DOI] [PubMed] [Google Scholar]
- 24.Howard DL, Sloane PD, Zimmerman S, Eckert JK, Walsh JF, Buie VC, Taylor PJ, Koch GG. Distribution of African Americans in residential care/assisted living and nursing homes: More evidence of racial disparity? Am J Public Health. 2002;92:1272–1277. doi: 10.2105/ajph.92.8.1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mor V, Zinn J, Angelelli J Teno JM, Miller SC. Driven to tiers: Socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82:227–256. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tan EJ, Lui LY, Eng C, Jha AK, Covinsky KE. Differences in mortality of black and white patients enrolled in the program of all-inclusive care for the elderly. J Am Geriatr Soc. 2003;51:246–251. doi: 10.1046/j.1532-5415.2003.51065.x. [DOI] [PubMed] [Google Scholar]
- 27.Moody-Ayers SY, Mehta KM, Lindquist K, Sands L, Covinsky KE. Black-white disparities in functional decline in older persons: the role of cognitive function. J Gerontol A Biol Sci Med Sci. 2005;60:933–939. doi: 10.1093/gerona/60.7.933. [DOI] [PubMed] [Google Scholar]
- 28.Sloan FA, Wang J. Disparities among older adults in measures of cognitive function by race or ethnicity. J Gerontol B Psychol Sci Soc Sci. 2005;60:242–250. doi: 10.1093/geronb/60.5.p242. [DOI] [PubMed] [Google Scholar]
- 29.Medicare Payment Advisory Commission . A Data Book: Health-care Spending and the Medicare Program. MedPAC; Washington, D.C.: 2006. Section 2: Medicare beneficiary demographics. www.medpac.gov/publications/congressional_reports/Jun06DataBookSec2.pdf (Last accessed February 16, 2008) [Google Scholar]
- 30. National Academy of Sciences: Eliminating health disparities: Measurement and data needs. The National Academies, Committee on National Statistics, National Research Council, Division of Behavioral and Social Sciences and Education, Committee on National Statistics, Panel on DHHS Collection of Race and Ethnicity Data, 2004.