Abstract
Approximately seven million people were prescribed a treatment for attention deficit hyperactivity disorder (ADHD) between November, 2006, and October, 2007: 3.8 million ages 0 to 17 years and 3.2 million age 18 years and older. To investigate prescribing trends, we obtained monthly total prescriptions from January, 2003, through October, 2007, for two age groups: patients under 18 years and patients age 18 years and older. The 0 to 17 years age group has demonstrated significant seasonality with total monthly prescription volume dropping between 22 and 29 percent between May and July, depending on the year. In contrast, prescribing trends for adults age 18 years and older have been steadily growing over the time period and do not exhibit any seasonal variation. Interestingly, in July, 2007, for the first time, ADHD total prescriptions for adults were larger than total prescriptions for children.
Keywords: ADHD, children, adolescents, adults, prescription, seasonailty
Introduction
Approximately 7 million people were prescribed a treatment for attention deficit hyperactivity disorder (ADHD) between November, 2006, and October, 2007: 3.8 million ages 0 to 17 years and 3.2 million age 18 years and older. In this paper, we investigate the trends in ADHD prescribing over the past six years overall and at the monthly level to investigate whether there is any monthly variation, especially in the summer season.
Methods
We obtained data from Verispan’s Vector One National (VONA), which captures nearly half of all prescription activity in the US. Because the prescription data is age specific, we were able to examine monthly total prescriptions from January, 2003, to October, 2007, for two age groups: 0 to 17 years and 18 years and over.
Results
Figure 1 displays monthly total prescriptions for ADHD therapies in the 0 to 17 years and 18 years and over age groups. As seen in the figure, the 0 to 17 years age group shows a significant dip in total prescriptions for the summer months. The seasonality observed ranges from a 22- to 29-percent decrease in monthly total prescriptions from May to July depending upon the year. In contrast, total monthly prescriptions in the 18 years and older age group have been steadily increasing over the January, 2003, to October, 2007, time period and the trend does not exhibit any seasonal differences in product use. Interestingly, in July, 2007, for the first time, there were more ADHD prescriptions filled for adults than children.
Figure 1.
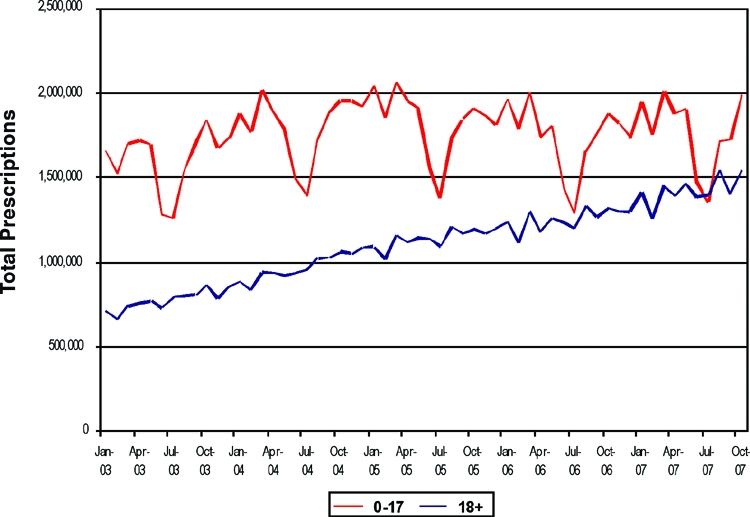
Monthly total prescriptions of ADHD products ages 0–17 years and 18 years and older. Source: Verispan VONA, total prescriptions ADHD therapies, January, 2003, through September, 2007: Ages 0–17 years and 18 years and older.
Expert Commentary
by Richard H. Weisler, MD
This prescription information for ADHD medications highlights some very important observations about US prescribing patterns. The seasonal trends over years provide convincing evidence of the use of ADHD medications only during the school year for many children and adolescents. The school-year–only dosing pattern may even be more significant than reflected in this prescribing data as many K–12 students in the US now are on a year-round school calendar. On a year-round school calendar, children or their parents may be discontinuing ADHD medications for multiple 2- to 3-week periods throughout the calendar year when on school breaks rather than just over the summer school holiday as is reflected in the Verispan data.
While school-year–only dosing of ADHD medications may be acceptable for some, the vast majority of both children and adolescents clearly do best when they take their ADHD medications regularly. For example, many older adolescents also drive vehicles, and it has been shown that driving performance improves and accident rates decrease with ADHD treatment.1 It is common for substance abuse and ADHD to co-occur and adversely impact each other. When ADHD goes untreated, the core symptoms of ADHD appear to increase the risk for substance use disorders and antisocial behavior.2,3 Substance abuse also negatively impacts the core symptoms of ADHD leading to more functional impairment. Episodic dosing further exacerbates adherence problems like that seen in a recent analysis, which revealed that only approximately 50 percent of patients on long-term stimulants are still taking their ADHD medication 3 to 5 months into treatment. A 15-month study of prescription data, which differentiated between two different preparations of methylphenidate as well as mixed amphetamine salts and atomoxetine, showed that only approximately 20 percent of patients were still taking their medications.4 Unfortunately, patients’ and/or parents’ efforts to minimize time spent on ADHD medications require their starting and stopping ADHD medications repeatedly, which may actually have the paradoxical effect of increasing the overall side-effect burden for patients. Intermittent dosing of ADHD medication can lead to problems from both the frequent need to redevelop initial medication tolerance and to reaccommodate to adverse events. Moreover, discontinuation-related adverse events from stimulants and atomoxetine treatment can be problematic for some as ADHD medications are repeatedly started and stopped by patients or their parents in relation to the school year and for many even just for the weekends. Efficacy is negatively impacted by intermittent dosing, especially in the case of atomoxetine. There are significant life impairments seen in surveyed adults with ADHD in the Biederman and Faraone study.5 Their survey results revealed that during their late adolescent years, relationship, self esteem, substance abuse, work, and other problems secondary to having had ADHD as a child, which would often be unrelated to the school year calendar academic issues. Consistent treatment of most chronic medical illnesses usually gives patients and those who are treating them better results than employing episodic medication management. Prescription data showing yearly wide seasonal swings as children are tracked out of school each summer demonstrates the need for additional patient, parent, and medical education. More ADHD treatment and outcome research is also needed to provide families and clinicians with a clearer understanding of potential short- and long-term negative and positive impact that is associated with the intermittent and seasonal dosing of ADHD medications in children.
Additionally, the sharp increase over the period of this analysis in prescriptions of medication for the treatment of adult ADHD is striking. With the FDA approval of atomoxetine in late 2002, mixed amphetamine salts XR in 2004, and dexmethylphenidate XR in 2005, US clinicians for the first time ever have agents that are approved for the treatment of adults with ADHD from which to choose. The national comorbidity study by Kessler6 revealed that 4.4 percent of adults had ADHD, and that only 10.9 percent of those adults had received any medication treatment in the last year. We also know that many adults with ADHD have gone undiagnosed, and even the vast majority of adults with ADHD who have been diagnosed are still medically untreated. Given the recognition that ADHD significantly impairs 40 to 60 percent of adults who, by definition, had ADHD as a child (up to 10% of the child population),7 it is very likely that significant future increases in adult prescriptions of medications for ADHD will be seen. As there are roughly about 230,000,0000 adults and 72,000,000 children ages 0 to 17 years in the US, one could easily imagine in the not too distant future a time when ADHD medication prescription volume for adults could ultimately be two or more times greater than the volume for children and adolescents.
Contributor Information
Elisa Cascade, Ms. Cascade is Vice President, Strategic Research and Safety, Quintiles Inc., Falls Church, Virginia.
Amir H. Kalali, Dr. Kalali is Vice President, Global Therapeutic Group Leader CNS, Quintiles Inc., San Diego, California, and Professor of Psychiatry, University of California, San Diego.
Richard H. Weisler, Dr. Weisler is an Adjunct Professor of Psychiatry at the University of North Carolina, Chapel Hill and Adjunct Associate Professor of Psychiatry at Duke University, Durham, North Carolina.
Susan Lenderts, Ms. Lenderts is with Quintiles, Inc..
References
- 1.Barkley RA, Murphy KR, Dupaul GI, Bush T. Driving in young adults with attention deficit hyperactivity disorder: knowledge, performance, adverse outcomes, and the role of executive functioning. J Int Neuropsychol Soc. 2002;8(5):655–672. doi: 10.1017/s1355617702801345. [DOI] [PubMed] [Google Scholar]
- 2.Wilens TE, Upadhyaya HP. Impact of substance use disorder on ADHD and its treatment. J Clin Psychiatry. 2007;68(8):e20. doi: 10.4088/jcp.0807e20. [DOI] [PubMed] [Google Scholar]
- 3.Wilens TE, Faraone SV, Biederman J, Gunawardene S. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;111(1):179–185. doi: 10.1542/peds.111.1.179. [DOI] [PubMed] [Google Scholar]
- 4.Capone NM, McDonnell T, Buse J, Kochhar A. Persistence with common pharmacologic treatments for ADHD. Annual International Conference of Children and Adults with Attention Deficit/Hyperactivity Disorder; October 27, 2005; Dallas, TX. Poster presented at: [Google Scholar]
- 5.Biederman J, Faraone SV, Spencer TJ, et al. Functional impairments in adults with self-reports of diagnosed ADHD: A controlled study of 1001 adults in the community. J Clin Psychiatry. 2006;67(4):524–540. doi: 10.4088/jcp.v67n0403. [DOI] [PubMed] [Google Scholar]
- 6.Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: Results from the National Comorbidity Survey Replication. Am J Psychiatry. 2006;163(4):716–723. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rowland AS, Umbach DM, Stallone L, et al. Prevalence of medication treatment for attention deficit-hyperactivity disorder among elementary school children in Johnston County, North Carolina. Am J Public Health. 2002;92(2):231–234. doi: 10.2105/ajph.92.2.231. [DOI] [PMC free article] [PubMed] [Google Scholar]


