Abstract
Radiation therapy continues to be one of the more popular treatment options for localized prostate cancer. One major obstacle to radiation therapy is that there is a limit to the amount of radiation that can be safely delivered to the target organ. Emerging evidence suggests that therapeutic agents targeting specific molecules might be combined with radiation therapy for more effective treatment of tumors. Recent studies suggest that modulation of these molecules by a variety of mechanisms (e.g., gene therapy, antisense oligonucleotides, small interfering RNA) may enhance the efficacy of radiation therapy by modifying the activity of key cell proliferation and survival pathways such as those controlled by Bcl-2, p53, Akt/PTEN and cyclooxygenase-2. In this article, we summarize the findings of recent investigations of radiosensitizing agents in the treatment of prostate cancer.
Review
Radiotherapy as a single modality has a limited but important role in the overall treatment of solid tumors, specifically prostate cancer. One major difficulty with radiation therapy is that there is a limit to the amount of radiation that can be safely delivered to the target organ [1,2]. For prostate cancer, radiation doses are generally limited to < 80 Gy because of the increased risk of toxicity at higher doses and the lack of clinical evidence that doses > 80 Gy improve local tumor control. Unfortunately, at these dosing levels a significant proportion of tumors are resistant to radiotherapy – either they do not respond to radiotherapy or they recur after treatment. It has become clear that the resistance of human cancers to radiation correlates with the expression of several key genes that regulate different steps of the apoptotic and cell cycle pathway. Thus, the strategy of targeting distinct molecular pathways may translate into higher efficacy, resulting in better survival. Radiation therapy combined with these targeted therapies may exert enhanced antitumor activity through synergic action. The combination treatment could also decrease the toxicity caused by radiation therapy if lower doses could be employed. In this article, we review the current literature on key molecules that have been associated with the development of radiation resistant prostate cancer and discuss novel ways to modulate these molecules to sensitize these tumors to the killing effects of radiation.
In the clinical arena, disease relapse after definitive radiation therapy (i.e., brachytherapy, external beam radiation therapy and proton therapy) is usually identified by an elevated or rising prostate-specific antigen (PSA) profile. Due to the controversy that surrounds identifying disease relapse, a consensus panel was formed to define radiation failure [3]. In addition to the debate about defining failure, controversy exists as to whether this new disease is persistent disease that was inadequately treated or recurrent disease that is refractory to therapy. It is difficult to distinguish persistent disease from recurrent disease. It is possible that persistent disease may have a genotype and phenotype different to recurrent disease since the organ has been exposed to radiation, albeit subtherapeutic doses.
Depending on the initial serum PSA level, Gleason score on biopsy, or clinical stage, 33–85% of patients undergoing external beam radiotherapy (XRT) for localized prostate cancer are biochemically disease-free 5 years after initial radiation therapy [1,2,4-8]. Tumor response to radiation is dependent on the total dose of radiation that can be safely delivered. Prostate tumors are notoriously resistant to total doses of 75 to 80 Gy, but higher doses are not generally administered because of the increased risk of toxicity. Because improved local tumor control is a therapeutic goal for most cancers, various strategies for sensitizing tumors to radiation have been tested over the last 20 years [9-13]. All of these strategies have involved the systemic administration of drugs or other agents that have specific toxicities of their own, which almost always limits pharmacological doses to levels below what is needed to sensitize tumors. The only successful sensitizing strategy thus far has been hormonal deprivation in combination with radiation therapy, which has been demonstrated to improve cause-specific survival in men with advanced prostate cancer [14,15], but still hormonal therapy in this setting is not the panacea. Perhaps molecular targets identified in in vitro and in vivo work could help improve the efficacy of radiotherapy above and beyond what we see with hormonal therapy. Despite ongoing clinical trials, no sensitizing strategies are currently available for widespread use.
Various genetic abnormalities have been associated with radiation-resistant prostate cancer [16]. Table 1 lists some of the more common genetic abnormalities associated with prostatic disease relapse after definitive radiation therapy [17-25]. The four most common genetic abnormalities reported in the literature, p53, Bcl-2, COX and Akt/PTEN will be reviewed in detail.
Table 1.
Genes associated with radiation resistant prostate cancer
| Major | Mechanism |
|---|---|
| Bcl-2 | Mitochondrial membrane protein that blocks the apoptotic death of cells |
| P53 | Protein which responds to diverse cellular stresses, regulating cell cycle arrest, apoptosis, senescence, DNA repair, or changes in metabolism |
| pAkt | Protein responsible for cell survival, proliferation, metabolism and angiogenesis |
| COX-2 | Enzyme responsible for prostaglandin production which is involved in cellular inflammation and mitogenesis |
| Minor | |
| Heat shock proteins 27, 90 [17-20] | Family of proteins whose expression is increased when cells are exposed to external stresses (e.g., infection, inflammation, hypoxia) and can inhibit apoptosis and activate proteosomes |
| Caspase-1 [21] | Protein which is a member of the cysteine-aspartic acid protease (caspase) family and is central to cell apoptosis as well as inflammation, septic shock, and wound healing |
| MDM2 [22] | Protein with an autoregulatory negative feedback loop p53 effecting cell cycle, apoptosis and tumorigenesis |
| Clusterin [23,24] | Glycoprotein observed to have both pro- and antiapoptotic functions |
| Ras [25] | Family of proteins responsible for signal transduction and cell to cell communication |
PI3K/Akt/PTEN
PI3K is a lipid kinase that can generate phosphatidylinositol-3,4,5-trisphosphate (PI(3,4,5)P3) which has a broad array of functions including inositol phosphate metabolism, phosphatidylinositol signaling system, p53 signaling pathway, cellular proliferation and survival, focal adhesion, and cell-cell communication. PI3K is regulated by its upstream growth factor receptor tyrosine kinases (e.g., EGFR family receptors). In addition, there is cross talk between the PI3K/Akt pathway and mitogen-activated protein kinases (MAP Kinase) pathway, mTOR pathway, and protein kinase A, B and C (PKA, PKB, PKC) pathways [26-29]. Phosphatase and tensin homolog (PTEN), the major negative regulator of the PI3K/Akt pathway, is a tumor suppressor gene that is localized on chromosome l0q23. PTEN is dual specific phosphatase that is involved in controlling cell cycle and apoptosis [30]. The PI3K signaling pathway is frequently aberrantly activated in tumors by mutation or loss of the 3'phospholipid phosphatase. Activation of the PI3K/Akt pathway is associated with three major radioresistance mechanisms: intrinsic radioresistance; tumor-cell proliferation; and hypoxia [31].
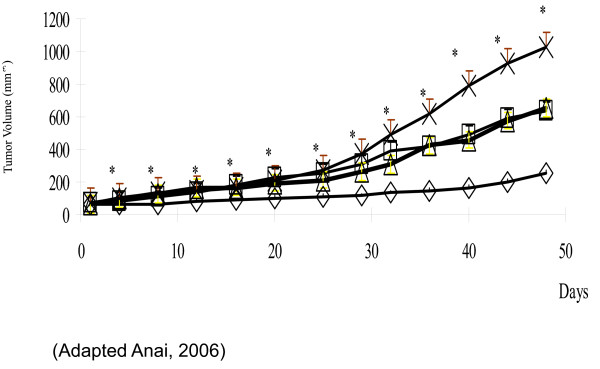
Forty-two percent of prostatic tumors have abnormal PTEN/Akt expression [32]. The human prostate cancer cell lines, PC-3, DU-145 and LNCaP are known to be resistant to radiation and thus are widely used in clonogenic radiation assays [33]. One of the cell lines, PC-3, was stably transfected to overexpress Bcl-2 which generated a cell line even more resistant to radiation than its parental lines [34]. Of the above cell lines, only DU-145 has wild-type PTEN and thus suppressed Akt expression (Table 2). Utilizing gene therapy, overexpression of PTEN resulted in down regulation of Akt. PTEN restoration caused significant G1 phase arrest in PC-3 cells. Morphologic changes, most notably apoptotic bodies and reduction in cellular proliferation, were evident in all cell lines. In addition, a reduction in the surviving fractions after 2 Gy of radiation was evident in the majority of cells assayed: PC-3-Bcl-2, reduction from 60.5% to 3.6%; PC-3-Neo, no reduction; LNCaP, reduction from 29.6% to 16.3%; and DU-145, reduction from 32.7% to 25.7%. Thus in select cells, PTEN restoration sensitized these cells to the killing effects of radiation [34]. PTEN restoration was tested in a xenograft model using the human prostate cancer cell line, PC-3-Bcl-2. PTEN expression inhibited xenograft tumor growth, however PTEN expression plus radiation (5 Gy) reduced tumor size to 75% of the untreated tumor (Figure 1). Combination treatment also enhanced apoptosis, inhibited cellular proliferation, and inhibited tumor-induced neovascularity [35].
Table 2.
Prostate cancer cell lines phenotype
| Cell Line | p53 status | Bcl-2 status | PTEN status |
|---|---|---|---|
| PC-3-Bcl-2 | Mutant | Overexpression | Deleted |
| PC-3-Neo | Mutant | Expression | Deleted |
| DU145 | Mutant | Wild type | Wild type |
| LNCaP | Wild type | Overexpression | Deleted |
Figure 1.
Effect of PTEN expression and radiation therapy on the growth of human prostate cancer xenograft tumors. In PC-3 Bcl-2 tumors, a modest, but significant, inhibition of tumor growth was demonstrated in Ad-PTEN alone. Compared to other treatment groups, the addition of irradiation to Ad-PTEN therapy further inhibited tumor growth. mock no XRT, X; mock + XRT, open square; AdPTEN no XRT, open triangle; AdPTEN + XRT, open diamond. (Adapted from Anai, 2006).
As the next section will illustrate, Bcl-2 expression can result in the development of radiation-resistant cancers. It is interesting that Huang and colleagues demonstrated that PTEN down regulation results in upregulation of Akt and Bcl-2, thus illustrating the possible cross-talk between the Bcl-2 and PI3K/Akt pathway [36].
Unlike for the other molecules we will discuss, limited clinical information is available regarding PI3K/Akt/PTEN conferring radiation resistance in actual human samples. Thus, further studies correlating abnormalities in the PI3K/Akt/PTEN pathway and the development of radiation-resistant disease are needed. If this correlation can be demonstrated clinically, the PI3K/Akt/PTEN pathway may prove to be a desirable therapeutic target that could be used combination with radiation therapy.
Bcl-2
After p53 the next most commonly discussed genetic aberration associated with radiation resistance is overexpression of Bcl-2. Bcl-2 is the founding member of a protein family composed of regulators of programmed cell death in both normal and abnormal cells. Bcl-2 is a pro-survival multidomain protein that regulates apoptosis by preventing the release of pro-apoptotic factors from mitochondria (e.g., cytochrome c) and subsequent activation of a caspase cascade [37-39]. The role of Bcl-2 as an antiapoptotic molecule is significant in prostate cancer because of the level of tenacity and resistance it grants to a tumor. As a result of these characteristics, it is associated with tumor aggressiveness [40-43].
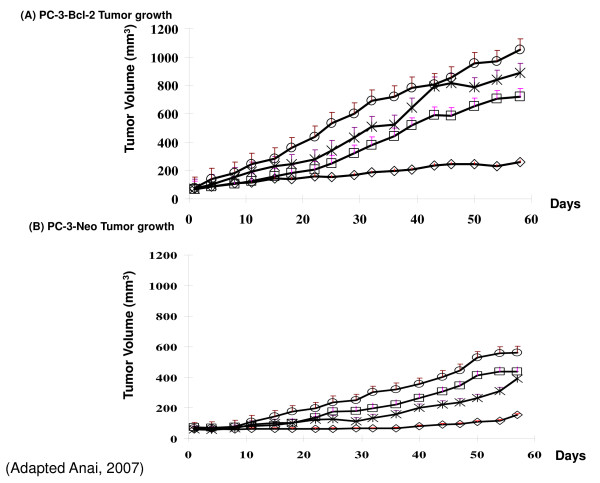
In vitro, exposure of cancer cells to low, non-toxic doses of radiation resulted in the up regulation of Bcl-2, indicating these cells were attempting to adapt to the harmful environment. To confirm that Bcl-2 expression is associated with radiation resistance, human prostate cancer cells PC-3 were stably transfected to express Bcl-2 and subjected to 0–6 Gy radiation. The Bcl-2 expressing clone grew more colonies at higher doses of radiation than the control clones (Figure 2). Utilizing these same cell lines, our group down regulated Bcl-2 expression in this model and studied its effects with and without radiation in vitro and in vivo. Solely targeting Bcl-2 produced no cytotoxic effects and was associated with G1 cell cycle arrest. The combination of knock-down of Bcl-2 with irradiation sensitized the cells to the killing effects of radiation. In addition, both PC-3-Bcl-2 and PC-3-Neo xenografts in mice treated with the combination of targeting Bcl-2 and irradiation were >3 times smaller by volume than were xenografts in mice treated with either modality alone (Figure 3). The combination therapy was also associated with increased rates of apoptosis, decreased rates of angiogenesis, and decreased rates of proliferation [44].
Figure 2.
Clonogenic assay of a panel of human prostate cancer cell lines subjected to irradiation. Utilizing clonogenic assay, gold standard for monitoring cell survival after irradiation, it was demonstrated that PC-3 cells that overexpressed Bcl-2 were the most radioresistant cells assayed.
Figure 3.
Effect of Bcl-2 targeted therapy in combination with radiation therapy on the growth of human prostate cancer xenograft tumors. (A) In PC-3 Bcl-2 tumors, growth inhibition was present with antisense Bcl-2 oligonucleotide (ASO) alone or radiation alone. Combining ASO and radiation significantly inhibited of tumor growth compared to other treatment groups. (B) In PC-3-Neo tumors, similar results were evident with combinational therapy resulting in an additive effect with irradiation. mock no XRT, open circle; mock + XRT, X; ASO no XRT, open square; ASO + XRT, open diamond. (Adapted from Anai, 2007).
Resistance to radiation therapy in human prostate cancers has been strongly linked to Bcl-2 [45-47]. In a study including 20 men who were radio-naïve and underwent prostatectomy for prostate cancer, no patient in this group was Bcl-2 positive. Among 20 men in the same study who were radio-recurrent and underwent prostatectomy for prostate cancer, 55% of the tumors were Bcl-2 immunopositive (p = 0.0004) [48]. Further evidence as to the importance of the expression of key proteins in the Bcl-2 family comes from a prospective, randomized, radiation dose escalation trial that treated 305 men with localized prostate cancer with either 70 or 78 Gy. Tumors were stained using a panel of markers from the Bcl-2 family of proteins including Bcl-2, Bcl-x (antiapoptotic Bcl-2 family member) and Bax (proapoptotic Bcl-2 family member). In the cohort, overexpression of Bcl-2 was observed in 16% of patients; altered Bax expression was observed in 23% of patients; and altered Bcl-x expression was observed in 53% of patients. Kaplan-Meier survival estimates of freedom from biochemical failure (bNED) and the log-rank tests revealed significantly lower rates in association with positive Bcl-2 and altered Bax staining. No correlation was observed between Bcl-x staining; and bNED. Cox proportional hazards multivariate analysis confirmed that Bcl-2 and Bax were independent of pretreatment PSA level, Gleason score and disease stage in predicting bNED [49]. Recently Khor and associates reported on the immunohistochemical results for Bcl-2 in 586 high-risk prostate cancer patients prospectively randomized to the Radiation Therapy Oncology Group (RTOG) trial 92-02 in which XRT was given in conjunction with a short course (STAD) or long course (LTAD) of androgen deprivation therapy. Bcl-2 was positive in 45.6% cases, and Bax expression altered in 53.9% cases. Bcl-2 overexpression was not independently related to biochemical failure, local failure, distant metastasis, cause-specific mortality or overall mortality, although the relative risks (RR) for failure were higher for overall mortality, cause-specific mortality, distant metastasis, and local failure, 1.24 (0.96–1.60), 1.24 (0.79–1.94), 1.37 (0.90–2.08) and 1.27 (0.78–2.07), respectively. In univariate analyses, altered Bax expression was not significantly associated with any of the end points tested either, although there was a trend for treatment failure (RR, 1.30; 95% CI, 0.97–1.73; p = 0.0806). However in the multivariate analyses, abnormal Bax expression was significantly associated with overall failure (RR, 1.43; 95% CI, 1.05–1.95; p = 0.0226) and marginally with biochemical failure (RR, 1.37; 95% CI, 0.96–1.97; p = 0.0851) [50].
Furthermore, the most common practice treatment for patients with locally advanced prostate is radiation therapy in conjunction with androgen deprivation therapy (ADT). ADT treatment triggers an overexpression of Bcl-2 which can lead to androgen independence, a condition associated with advanced prostate cancer [51]. The compelling data presented above illustrates the significance of the Bcl-2 family in conferring radiation resistance in prostatic tumors. Strategies designed to favorably alter this family of survival proteins to enhance the antitumor effect of radiation warrant further clinical evaluation.
p53
The importance of TP53 (p53) gene as a molecular marker in cancer is demonstrated by the finding that mutations of p53 occur in approximately half of all human malignancies [52]. p53 is a well known protein that acts as a "master watchman" in cell-cycle arrest, programmed cell death, and DNA repair [53-55]. Though some researchers have reported the response to radiation is independent of the cell's p53 status [56], numerous reports are available that demonstrated increased cell kill with irradiation in cells expressing p53 [57].
Gene therapy strategies based on p53 have been shown to reduce tumorigenicity and promote apoptosis in a variety of cell lines and xenograft tumors including colon, head and neck, ovary, and brain [58-66]. Resistance to apoptosis due to cell-cycle disruption has been found to be variably dependent on the existence of p53. p53 is therefore an important protein in the sensitization of prostate cancer to radiation therapy. In an elegant experiment by researchers at MD Anderson Cancer Center, the effects of adenoviral-mediated p53 transgene expression on the radiation response of two human prostate cancer cell lines, LNCaP and PC3 lines, was examined. After correcting for the effect of Ad5-p53 on plating efficiency, the surviving fraction after 2 Gy of radiation was reduced more than 2.5-fold, from 0.187 to 0.072, with transgene p53 expression in the LNCaP cell line. Surviving fraction after 4 Gy was reduced greater than 4.5-fold, from 0.014 to 0.003, after Ad5-p53 treatment. In the PC3 cell line, Ad5-p53 reduced surviving fraction after 2 Gy 1.9-fold from 0.708 to 0.367 and 6-fold at the surviving fraction after 4 Gy from 0.335 to 0.056. Lastly in both cell lines, the combination of Ad5-p53 plus radiation (2 Gy) resulted in supra-additive apoptosis (approximately 20% for LNCaP and approximately 15% for PC3 at 50 MOI) above that seen from the controls [67]. Other groups have been able to corroborate the results of this in vitro experiment in human prostate cancer cells [68]. In a follow-up to that study, Cowen presented the in vivo results in PC3 and LNCaP xenograft model treated with intratumoral p53 injection and 5 Gy radiation. The time for the PC3 tumors to reach 500 mm3 were calculated as 10.7 days (+/- 0.7) for the saline control, 15.6 days (+/- 1.6) for Ad5-p53, 14.6 days (+/- 1.5) radiation therapy, and 31.4 days (+/- 5.3) for Ad5-p53 plus XRT. Thus, Ad5-p53 plus radiation significantly retarded the growth of xenograft prostate tumors. Furthermore in LNCaP xenograft tumors where serum PSA levels were used to judge treatment efficacy, treatment with Ad5-p53 plus 5 Gy resulted in significantly fewer PSA failures (<30%), as compared with failures with Ad5-p53 alone (64–73%) and the other controls (approximately 80–100%) [69]. These studies indicate that prostatic tumor growth could be inhibited with the over expression of p53 in combination with radiation therapy.
Several small, retrospective studies in men with prostate cancer have suggested that abnormal p53 expression is associated with poor outcomes [70-74]. In addition, prospective clinical trials have clearly demonstrated the prognostic implications of abnormally expressed p53 in men treated with XRT. For example, tissue samples from 777 men enrolled in RTOG 92-02, the seminal study that compared STAD with XRT to LTAD + XRT, with locally-advanced prostate cancer were analyzed for p53 expression. Abnormal p53 expression was defined as 20% or more tumor cells with positive nuclei. Abnormal p53 was detected in 168 (21.6%) of 777 cases and was significantly associated with cause-specific mortality (adjusted hazard ratio [HR] = 1.89; 95% confidence interval [CI] 1.14 – 3.14; p = 0.014) and distant metastasis (adjusted HR = 1.72; 95% CI 1.13–2.62; p = 0.013). When patients were divided into subgroups according to assigned treatment, only the subgroup of patients who underwent STAD + RT showed significant correlation between p53 status and cause-specific mortality (adjusted HR = 2.43; 95% CI = 1.32–4.49; p = 0.0044). This increase in cause-specific mortality could be reduced with LTAD [73]. Similarly, in RTOG 86-10, a phase III trial of Zoladex and flutamide in locally advanced carcinoma of the prostate treated with definitive radiotherapy, patients were assessed for the prognostic significance of abnormal p53 expression. One hundred twenty-nine (27%) of the 471 patients entered in the trial had sufficient tumor material for analysis. Abnormal p53 protein expression was detected in the tumors of 23 (18%) of these 129 patients. Statistically significant associations were found on a multivariate analysis between the presence of abnormal p53 protein expression and increased incidence of distant metastases, decreased progression-free survival, and decreased overall survival. No association was found between abnormal p53 protein expression and the time to local progression [75].
In addition, D'Amico reported the results of CALGB 9682 in which 180 men with clinical stage T1c-T3cN0M0 adenocarcinoma of the prostate. They were treated with ADT and assessed with endorectal magnetic resonance imaging (eMRI) for change in tumor volume (TV) and associated PSA outcome. Of these subjects, 141 had sufficient tissue to assess p53 expression. After a median follow-up of 6.9 years and adjusting for PSA level, Gleason score, clinical stage, and change in tumor volume, men with abnormal p53 expression compared with normal were at increased risk of PSA failure (hazard ratio [HR]: 2.8; 95% confidence interval [CI]) [76].
Knowing the significance of p53 expression, the next hurdle is whether we can manipulate p53 expression to obtain more favorably outcomes. Researchers studying other tumor types have published on the success of this approach [77]. For prostate cancer, only one significant trial stands out. In a phase I/II clinical trial, investigators at MD Anderson Cancer Center, administered intraprostatic injections of Ad-p53 on three separate occasions prior to radical prostatectomy in subjects with high-risk localized prostate cancer. There were no grade 3 or 4 adverse events related to p53 administration. Of the 11 patients with negative baseline immunostaining for p53 protein, 10 had positive p53 immunostaining after the administration of p53, and 8 had an increase in apoptotic cells [78]. Though adenoviral gene therapy has its limitations, this study is an excellent example of proof of the concept that p53 expression may restore the cell's normal function which can then assist in the eradication of the tumor. Further research is needed to explore targeting p53 in conjunction with radiation therapy in the treatment of prostate cancer.
COX-2
Cyclooxygenase is a family of isozymes that convert arachidonic acid to prostaglandins and other eicosanoids. COX-1, ubiquitously expressed in almost all tissue, is important for the maintenance of homeostatic function [79]. COX-2 has been well-characterized as a key component in the inflammatory pathway of such disorders as rheumatoid arthritis and Parkinson's Disease [80,81]. In addition, COX-2 is overexpressed in 80% of cancers of the breast, colon, esophagus, liver, lung, pancreas, cervix, head and neck, and prostate [82-85]. COX-2 is induced by growth factors, tumor promoters, and cytokines and is subject to transcriptional and translational regulation and degradation [86]. Thus, COX-2 is another important cell survival factor. Overexpression of COX-2 or its related products confers resistance to cells undergoing chemotherapy or radiation therapy induced apoptosis.
Similar to what was reported for Bcl-2, cancer cells exposed to low doses of radiation up-regulated COX-2 expression as a possible means to survive the radiation exposure [87]. As described above, therapeutic gamma radiation exerts its effect on the function and/or survival of cells by interacting with biologically important molecules, either directly or indirectly. Exposure to radiation can directly affect DNA structure, which can in turn influence the subtle balance of the expression of genes whose products are involved in promoting cell survival or triggering cell death. Interestingly, other environmental stressors, including hypoxia and acidosis, resulted in an up-regulation of COX-2 expression [87].
In a series of in vitro clonogenic assays, the human prostate cancer cell line LNCaP was stably transfected to overexpress COX-2. LNCaP-COX-2 cells were significantly more resistant to radiation therapy compared to LNCaP-Neo cells. However, the addition of celecoxib, a selective COX-2 inhibitor that blocks the production of prostaglandins primarily via inhibition of cyclooxygenase-2, sensitized LNCaP-COX-2 cells to the cytocidal effects of radiation. Moreover, we confirmed that COX-2 overexpression was associated with overexpression of pAkt and CA IX, two key genes associated with poor tumor response to radiation [87]. Other preclinical reports have confirmed that COX-2 overexpression and/or subsequently targeting COX-2 with these COX-2 inhibitors may render cells susceptible to the killing effects of the radiation [88-91].
Although limited in vivo data are available as to the significance of COX-2 overexpression as related to its ability to confer radiation resistance, recently Khor and colleagues reported the immunohistochemical results for COX-2 in 586 patients enrolled in Radiation Therapy Oncology Group (RTOG) 92-02. As previously stated, in the RTOG 92-02 trial patients were randomly assigned to treatment with STAD plus radiotherapy or LTAD plus radiotherapy. In multivariate analyses, the intensity of COX-2 staining as a continuous covariate was an independent predictor of distant metastasis (hazard ratio [HR] 1.181; 95% CI 1.077–1.295); biochemical failure (HR 1.073 [1.014–1.134]); and any failure (HR 1.068 [1.015–1.124]) [92].
Both the Bcl-2 pathway and COX-2 pathway overlap at phosphatidylinositol 3-kinase (PI3K)/Akt, making these molecules attractive targets. The above data support a pivotal role for COX-2 expression in tumors treated with irradiation and thus justify studies to evaluate the clinical application of targeting COX-2 in patients undergoing radiation therapy as a treatment for prostate cancer.
Future Directions
The expression of the aforementioned genes has been reliably linked to the development of radiation-resistance cancers. It is feasible to conclude that a litany of other survival genes may be associated with the development of radiation resistant cancers. Limited data are available from the use of high throughput technology (e.g., genomic and proteomic) in the discovery of new biomarkers of which influence resistance to radiation in prostate tumors. As is clearly evident here, no single molecule is responsible for the development and growth of radiation-resistance prostate cancer. As is common in the development of primary tumors, multiple genes are aberrant. The importance of the redundancy in the aberrant genes is that they are likely to ensure the survival of tumors. The ability to target more than one gene is an attractive approach. The recent flourish in the clinical development of more than 30 targeted protein kinase inhibitors designed to inhibit angiogenesis, tumor growth and progression attests to this [93,94]. Specifically, Imatinib mesylate [95], Sorafenib [96], Sunitinib malate [97], and Temsirolimus [98] have demonstrated efficiency in solid tumors including renal cell carcinoma. Due to the multiple targets inhibited by these multikinase inhibitors, effects in different tumor types are likely to be mediated through a variety of mechanisms. Limited forays combining these inhibitors with radiation therapy in a variety of tumor types have produced encouraging results [99]. We clearly recognize the roadblocks in designing clinical trials to test new agents for radiosensitizing since it is difficult to obtain tissue after radiation therapy for prostate cancer. However, the question begs consideration, can targeted therapy effectively treat these cancers? Similar to what we have seen in other cancers (e.g., testis, lymphoma, colon), optimal therapy will consist of a therapeutic 'cocktail' involving traditional chemotherapy and the new targeted therapies in conjunction with radiation therapy, which has also evolved over the past decade.
The importance of incorporating these targeted therapies may be similar to incorporating ADT with radiation therapy. Preclinical studies have demonstrated that ADT can induce apoptosis and inhibit angiogenesis [100]; outcomes that may be potentitated by radiation therapy. These preclinical studies subsequently were translated into a clinical therapeutic advantage in men with high risk localized prostate cancer. Only four targeted therapeutic trials are currently open (Table 3) in men with high risk prostate cancer treated with radiation therapy. A more concerted attempt must be made to bring promising targeted therapeutics to clinical trial to determine treatment efficacy.
Table 3.
Accruing Clinical Trials Combining Targeted Therapy with radiation Therapy
| Agent | Institute |
|---|---|
| Sunitinib | MD Anderson Cancer Center |
| SU5416 | University of Chicago |
| Bevacizumab | 1) Benaroya Research Institute 2) Virginia Mason |
| RAD001 | Shelba Medical Center |
Conclusion
Radiation therapy continues to be one of the more popular treatment options for localized prostate cancer. However, recent studies suggest that abnormal expression of Bcl-2, p53, Akt/PTEN and cyclooxygenase-2 may render tumors resistant to the killing effects of radiation. However modulation of these molecules by a variety of mechanisms (e.g., gene therapy, antisense oligonucleotides, small interfering RNA) may enhance the efficacy of radiation therapy by modifying the activity of these key cell proliferation and survival pathways.
List of abbreviations
MOI: Multiplicity Of Infection; Ad: adenovirus; PTEN: Phosphatase and tensin; PI3K: Phosphatidylinositol 3 kinase; MAP kinase: mitogen-activated protein kinases; PKA, PKB, PKC: protein kinase A, B and C; RTOG: Radiation Therapy Oncology Group; STAD: short course of androgen deprivation therapy; LTAD: long course of androgen deprivation therapy; eMRI: endorectal magnetic resonance imaging (eMRI); TV: tumor volume; Gy: Gray; PSA: prostate specific antigen; XRT: radiation therapy; bNED: biochemical no evidence of disease; ADT: androgen deprivation therapy; HR: hazard rates; CI: confidence interval.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MG collected data and drafted the manuscript. SP assisted in collecting data and revising the manuscript. CJR conceived the project, and participated in its design and coordination. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Contributor Information
Charles J Rosser, Email: charles.rosser@urology.ufl.edu.
Micah Gaar, Email: mgaar@fsu.edu.
Stacy Porvasnik, Email: stacy.porvasnik@ufl.edu.
Acknowledgements
Joanne Clarke for her review and editing of the manuscript.
References
- Kuban DA, El-Mahdi AM, Schellhammer PF. Effect of local tumor control on distant metastasis and survival in prostatic adenocarcinoma. Urology. 1987;30:420–6. doi: 10.1016/0090-4295(87)90372-4. [DOI] [PubMed] [Google Scholar]
- Pollack A, Zagars GK, Smith LG, Lee JJ, von Eschenbach AC, Antolak JA, Starkschall G, Rosen I. Preliminary results of a randomized radiotherapy dose-escalation study comparing 70 Gy with 78 Gy for prostate cancer. J Clin Oncol. 2000;18:3904–11. doi: 10.1200/JCO.2000.18.23.3904. [DOI] [PubMed] [Google Scholar]
- Roach M 3rd, Hanks G, Thames H Jr, Schellhammer P, Shipley WU, Sokol GH, Sandler H. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys. 2006;65(4):965–74. doi: 10.1016/j.ijrobp.2006.04.029. [DOI] [PubMed] [Google Scholar]
- Bagshaw MA, Kaplan ID, Cox RC. Prostate cancer. Radiation therapy for localized disease. Cancer. 1993;71:939–52. doi: 10.1002/1097-0142(19930201)71:3+<939::aid-cncr2820711409>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Pollack A, Zagars GK, Starkschall G, Childress CH, Kopplin S, Boyer AL, rosen II. Conventional vs. conformal radiotherapy for prostate cancer. Preliminary results of dosimetry and acute toxicity. Int J Radiat Oncol Biol Phys. 1996;34:555–64. doi: 10.1016/0360-3016(95)02103-5. [DOI] [PubMed] [Google Scholar]
- Shipley WU, Verhey LJ, Munzenrider JE, Suit HD, Urie MM, McManus PL, Young RH, Shipley JW, Zietman AL, Biggs PG, Heney NM, Goitein M. Advanced prostate cancer: the results of a randomized comparative trial of high dose irradiation boosting with conformal protons compared with conventional dose irradiation using photons alone. Int J Radiat Oncol Biol Phys. 1995;32:3–12. doi: 10.1016/0360-3016(95)00063-5. [DOI] [PubMed] [Google Scholar]
- Zagars GK, von Eschenbach AC, Johnson DE, Oswald MJ. Stage C adenocarcinoma of the prostate. An analysis of 551 patients treated with external beam radiation. Cancer. 1987;60:1489–99. doi: 10.1002/1097-0142(19871001)60:7<1489::aid-cncr2820600715>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- Pollack A, Zagars GK, Antolak JA, Kuban DA, Rosen II. Prostate biopsy status and PSA nadir level as early surrogates for treatment failure: analysis of a prostate cancer randomized radiation dose escalation trial. Int J Radiat Oncol Biol Phys. 2002;54(3):677–85. doi: 10.1016/s0360-3016(02)02977-2. [DOI] [PubMed] [Google Scholar]
- Chinnaiyan P, Huang S, Vallabhaneni G. Mechanisms of enhanced radiation response following epidermal growth factor receptor signaling inhibition by erlotinib (Tarceva) Cancer Res. 2005;65:3328–35. doi: 10.1158/0008-5472.CAN-04-3547. [DOI] [PubMed] [Google Scholar]
- Chendil D, Ranga RS, Meigooni D, Sathishkumar S, Ahmed MM. Curcumin confers radiosensitizing effect in prostate cancer cell line PC-3. Oncogene. 2004;23:1599–607. doi: 10.1038/sj.onc.1207284. [DOI] [PubMed] [Google Scholar]
- Husbeck B, Peehl DM, Knox SJ. Redox modulation of human prostate carcinoma cells by selenite increases radiation-induced cell killing. Free Radic Biol Med. 2005;38:50–7. doi: 10.1016/j.freeradbiomed.2004.09.022. [DOI] [PubMed] [Google Scholar]
- Wang H, Oliver P, Zhang Z, Agrawal S, Zhang R. Chemosensitization and radiosensitization of human cancer by antisense anti-MDM2 oligonucleotides: in vitro and in vivo activities and mechanisms. Ann N Y Acad Sci. 2003;1002:217–35. doi: 10.1196/annals.1281.025. [DOI] [PubMed] [Google Scholar]
- Lapidus RG, Dang W, Rosen DM. Anti-tumor effect of combination therapy with intratumoral controlled-release paclitaxel (PACLIMER microspheres) and radiation. Prostate. 2004;58:291–8. doi: 10.1002/pros.10331. [DOI] [PubMed] [Google Scholar]
- Bolla M, Gonzalez D, Warde P. Improved survival in patients with locally advanced prostate cancer treated with radiotherapy and goserelin. N Engl J Med. 1997;337:295–300. doi: 10.1056/NEJM199707313370502. [DOI] [PubMed] [Google Scholar]
- Lawton CA, Winter K, Murray K, Machtay M, Mesic JB, Hanks GE, Coughlin CT, Pilepich MV. Updated results of the phase III Radiation Therapy Oncology Group (RTOG) trial 85-31 evaluating the potential benefit of androgen suppression following standard radiation therapy for unfavorable prognosis carcinoma of the prostate. Int J Radiat Oncol Biol Phys. 2001;49(4):937–46. doi: 10.1016/s0360-3016(00)01516-9. [DOI] [PubMed] [Google Scholar]
- Peters LJ. Inherent radiosensitivity of tumor and normal tissue cells as a predictor of human tumor response. Radiother Oncol. 1990;17:177–190. doi: 10.1016/0167-8140(90)90202-8. [DOI] [PubMed] [Google Scholar]
- Bull EE, Dote H, Brady KJ, Burgan WE, Carter DJ, Cerra MA, Oswald KA, Hollingshead MG, Camphausen K, Tofilon PJ. Enhanced tumor cell radiosensitivity and abrogation of G2 and S phase arrest by the Hsp90 inhibitor 17-(dimethylaminoethylamino)-17-demethoxygeldanamycin. Clin Cancer Res. 2004;10(23):8077–84. doi: 10.1158/1078-0432.CCR-04-1212. [DOI] [PubMed] [Google Scholar]
- Dote H, Cerna D, Burgan WE, Camphausen K, Tofilon PJ. ErbB3 expression predicts tumor cell radiosensitization induced by Hsp90 inhibition. Cancer Res. 2005;65(15):6967–75. doi: 10.1158/0008-5472.CAN-05-1304. [DOI] [PubMed] [Google Scholar]
- Teimourian S, Jalal R, Sohrabpour M, Goliaei B. Down-regulation of Hsp27 radiosensitizes human prostate cancer cells. Int J Urol. 2006;13(9):1221–5. doi: 10.1111/j.1442-2042.2006.01483.x. [DOI] [PubMed] [Google Scholar]
- Aloy MT, Hadchity E, Bionda C, Diaz-Latoud C, Claude L, Rousson R, Arrigo AP, Rodriguez-Lafrasse C. Protective role of Hsp27 protein against gamma radiation-induced apoptosis and radiosensitization effects of Hsp27 gene silencing in different human tumor cells. Int J Radiat Oncol Biol Phys. 2008;70(2):543–53. doi: 10.1016/j.ijrobp.2007.08.061. [DOI] [PubMed] [Google Scholar]
- Winter RN, Rhee JG, Kyprianou N. Caspase-1 enhances the apoptotic response of prostate cancer cells to ionizing radiation. Anticancer Res. 2004;24(3a):1377–86. [PubMed] [Google Scholar]
- Stoyanova R, Hachem P, Hensley H, Khor LY, Mu Z, Hammond ME, Agrawal S, Pollack A. Antisense-MDM2 sensitizes LNCaP prostate cancer cells to androgen deprivation, radiation, and the combination in vivo. Int J Radiat Oncol Biol Phys. 2007;68(4):1151–60. doi: 10.1016/j.ijrobp.2007.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zellweger T, Kiyama S, Chi K, Miyake H, Adomat H, Skov K, Gleave ME. Overexpression of the cytoprotective protein clusterin decreases radiosensitivity in the human LNCaP prostate tumour model. BJU Int. 2003;92(4):463–9. doi: 10.1046/j.1464-410x.2003.04349.x. [DOI] [PubMed] [Google Scholar]
- Zellweger T, Chi K, Miyake H, Adomat H, Kiyama S, Skov K, Gleave ME. Enhanced radiation sensitivity in prostate cancer by inhibition of the cell survival protein clusterin. Clin Cancer Res. 2002;8(10):3276–84. [PubMed] [Google Scholar]
- Kim BY, Kim KA, Kwon O, Kim SO, Kim MS, Kim BS, Oh WK, Kim GD, Jung M, Ahn JS. NF-kappaB inhibition radiosensitizes Ki-Ras-transformed cells to ionizing radiation. Carcinogenesis. 2005;26(8):1395–403. doi: 10.1093/carcin/bgi081. [DOI] [PubMed] [Google Scholar]
- Franke TF. PI3K/Akt getting it right matters. Oncogene. 2008;27(50):6473–88. doi: 10.1038/onc.2008.313. [DOI] [PubMed] [Google Scholar]
- Carnero A, Blanco-Aparicio C, Renner O, Link W, Leal JF. The PTEN/PI3K/AKT signalling pathway in cancer, therapeutic implications. Curr Cancer Drug Targets. 2008;8(3):18–98. doi: 10.2174/156800908784293659. [DOI] [PubMed] [Google Scholar]
- Steelman LS, Stadelman KM, Chappell WH, Horn S, Bäsecke J, Cervello M, Nicoletti F, Libra M, Stivala F, Martelli AM, McCubrey JA. Akt as a therapeutic target in cancer. Expert Opin Ther Targets. 2008;12(9):1139–65. doi: 10.1517/14728222.12.9.1139. [DOI] [PubMed] [Google Scholar]
- Osaki M, Oshimura M, Ito H. PI3K-Akt pathway: its functions and alterations in human cancer. Apoptosis. 2004;9(6):667–76. doi: 10.1023/B:APPT.0000045801.15585.dd. [DOI] [PubMed] [Google Scholar]
- Steelman LS, Bertrand FE, McCubrey JA. The complexity of PTEN: mutation, marker and potential target for therapeutic intervention. Expert Opin Ther Targets. 2004;8:537–550. doi: 10.1517/14728222.8.6.537. [DOI] [PubMed] [Google Scholar]
- Bussink J, Kogel AJ van der, Kaanders JH. Activation of the PI3-K/AKT pathway and implications for radioresistance mechanisms in head and neck cancer. Lancet Oncol. 2008;9(3):288–96. doi: 10.1016/S1470-2045(08)70073-1. [DOI] [PubMed] [Google Scholar]
- Teng DH, Hu R, Lin H, Davis T, Iliev D, Frye C, Swedlund B, Hansen KL, Vinson VL, Gumpper KL, Ellis L, El-Naggar A, Frazier M, Jasser S, Langford LA, Lee J, Mills GB, Pershouse MA, Pollack RE, Tornos C, Troncoso P, Yung WK, Fujii G, Berson A, Steck PA. MMAC1/PTEN mutations in primary tumor specimens and tumor cell lines. Cancer Res. 1997;57(23):5221–5. [PubMed] [Google Scholar]
- Bromfield GP, Meng A, Warde P, Bristow RG. Cell death in irradiated prostate epithelial cells: role of apoptotic and clonogenic cell kill. Prostate Cancer Prostatic Dis. 2003;6(1):73–85. doi: 10.1038/sj.pcan.4500628. [DOI] [PubMed] [Google Scholar]
- Rosser CJ, Tanaka M, Pisters LL, Tanaka N, Levy LB, Hoover DC, Grossman HB, McDonnell TJ, Kuban DA, Meyn RE. Adenoviral-mediated PTEN transgene expression sensitizes Bcl-2-expressing prostate cancer cells to radiation. Cancer Gene Ther. 2004;11(4):273–9. doi: 10.1038/sj.cgt.7700673. [DOI] [PubMed] [Google Scholar]
- Anai S, Goodison S, Shiverick K, Iczkowski K, Tanaka M, Rosser CJ. Combination of PTEN gene therapy and radiation inhibits the growth of human prostate cancer xenografts. Hum Gene Ther. 2006;17(10):975–84. doi: 10.1089/hum.2006.17.975. [DOI] [PubMed] [Google Scholar]
- Huang H, Cheville JC, Pan Y, Roche PC, Schmidt LJ, Tindall DJ. PTEN induces chemosensitivity in PTEN-mutated prostate cancer cells by suppression of Bcl-2 expression. J Biol Chem. 2001;276(42):38830–6. doi: 10.1074/jbc.M103632200. [DOI] [PubMed] [Google Scholar]
- Lucken-Ardjomande S, Martinou JC. Regulation of Bcl-2 proteins and of the permeability of the outer mitochondrial membrane. C R Biol. 2005;328:616–31. doi: 10.1016/j.crvi.2005.05.002. [DOI] [PubMed] [Google Scholar]
- Reed JC. Bcl-2 and the regulation of programmed cell death. J Cell Biol. 1994;124(1–2):1–6. doi: 10.1083/jcb.124.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang E, Korsmeyer S. Molecular thanatopsis A discourse on the BCL2 family and cell death. Blood. 1996;88(2):386–401. [PubMed] [Google Scholar]
- Stattin P, Damber JE, Karlberg L, Nordgren H, Bergh A. Bcl-2 immunoreactivity in prostate tumorigenesis in relation to prostatic intraepithelial neoplasia, grade, hormonal status, metastatic growth and survival. Urol Res. 1996;24(5):257–264. doi: 10.1007/BF00304774. [DOI] [PubMed] [Google Scholar]
- Bubendorf L, Sauter G, Moch H, Jordan P, Blochlinger A, Gasser TC, Mihatsch MJ. Prognostic significance of Bcl-2 in clinically localized prostate cancer. Am J Pathol. 1996;148(5):1557–1565. [PMC free article] [PubMed] [Google Scholar]
- Lipponen P, Vesalainen S. Expression of the apoptosis suppressing protein bcl-2 in prostatic adenocarcinoma is related to tumor malignancy. Prostate. 1997;32(1):9–15. doi: 10.1002/(sici)1097-0045(19970615)32:1<9::aid-pros2>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Tsuji M, Murakami Y, Kanayama H, Sano T, Kagawa S. Immunohistochemical analysis of Ki-67 antigen and Bcl-2 protein expression in prostate cancer: effect of neoadjuvant hormonal therapy. Br J Urol. 1998;81:116–21. doi: 10.1046/j.1464-410x.1998.00492.x. [DOI] [PubMed] [Google Scholar]
- Anai S, Goodison S, Shiverick K, Hirao Y, Brown BD, Rosser CJ. Knock-down of Bcl-2 by antisense oligodeoxynucleotides induces radiosensitization and inhibition of angiogenesis in human PC-3 prostate tumor xenografts. Mol Cancer Ther. 2007;6(1):101–11. doi: 10.1158/1535-7163.MCT-06-0367. [DOI] [PubMed] [Google Scholar]
- Huang A, Gandour-Edwards R, Rosenthal SA. p53 and Bcl-2 immunohistochemical alterations in prostate cancer treated with radiation therapy. Urology. 1998;51:346–351. doi: 10.1016/s0090-4295(97)00636-5. [DOI] [PubMed] [Google Scholar]
- Rakozy C, Grignon DJ, Sarkar FH. Expression of Bcl-2, p53, and p21 in benign and malignant prostatic tissue before and after radiation therapy. Mod Pathol. 1998;11:892–899. [PubMed] [Google Scholar]
- Scherr DS, Vaughn ED, Wei J. Bcl-2 and p53 expression in clinically localized prostate cancer predicts response to external beam radiotherapy. J Urol. 1999;162:12–17. doi: 10.1097/00005392-199907000-00003. [DOI] [PubMed] [Google Scholar]
- Rosser CJ, Reyes AO, Vakar-Lopez F, Levy LB, Kuban DA, Hoover DC, Lee AK, Pisters LL. Bcl-2 is significantly overexpressed in localized radio-recurrent prostate carcinoma, compared with localized radio-naive prostate carcinoma. Int J Radiat Oncol Biol Phys. 2003;56(1):1–6. doi: 10.1016/s0360-3016(02)04468-1. [DOI] [PubMed] [Google Scholar]
- Pollack A, Cowen D, Troncoso P, Zagars GK, von Eschenbach AC, Meistrich ML, McDonnell T. Molecular markers of outcome after radiotherapy in patients with prostate carcinoma: Ki-67, bcl-2, bax, and bcl-x. Cancer. 2003;97(7):1630–8. doi: 10.1002/cncr.11230. [DOI] [PubMed] [Google Scholar]
- Khor LY, Moughan J, Al-Saleem T, Hammond EH, Venkatesan V, Rosenthal SA, Ritter MA, Sandler HM, Hanks GE, Shipley WU, Pollack A. Bcl-2 and Bax expression predict prostate cancer outcome in men treated with androgen deprivation and radiotherapy on radiation therapy oncology group protocol 92-02. Clin Cancer Res. 2007;13(12):3585–90. doi: 10.1158/1078-0432.CCR-06-2972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonnell TJ, Troncoso P, Brisbay SM. Expression of the protooncogene bcl-2 in the prostate and its association with emergence of androgen-independent prostate cancer. Cancer. 1992;52:Res6940–4. [PubMed] [Google Scholar]
- Hollstein M, Hergenhahn M, Yang Q, Bartsch H, Wang ZQ, Hainaut P. New approaches to understanding p53 gene tumor mutation spectra. Mutat Res. 1999;431:199–209. doi: 10.1016/s0027-5107(99)00162-1. [DOI] [PubMed] [Google Scholar]
- Yonish-Rouach E, Resnitzky D, Rotem J. Wild-type p53 induces apoptosis of myeloid leukemic cells that is inhibited by interleukin-6. Nature. 1991;352:345–347. doi: 10.1038/352345a0. [DOI] [PubMed] [Google Scholar]
- Kastan MB, Onyekwere O, Sidransky D. Participation of p53 protein in the cellular response to DNA damage. Cancer Res. 1992;51:6304–6311. [PubMed] [Google Scholar]
- Lowe SW, Schmitt EM, Smith SW. p53 is required for radiation-induced apoptosis in mouse thymocytes. Nature. 1993;362:847–485. doi: 10.1038/362847a0. [DOI] [PubMed] [Google Scholar]
- Kyprianou N, Rock S. Radiation-induced apoptosis of human prostate cancer cells is independent of mutant p53 overexpression. Anticancer Res. 1998;8:897–906. [PubMed] [Google Scholar]
- Nagasawa H, Li C-Y, Maki CG. Relationship between radiation-induced G1 phase arrest and p53 function in human tumor cells. Cancer Res. 1995;55:1842–1846. [PubMed] [Google Scholar]
- Spitz FR, Nguyen D, Skibber JM. Adenoviral-mediated wild-type p53 gene expression sensitizes colorectal cancer cells to ionizing radiation. Clin Cancer Res. 1996;2:1665–1671. [PubMed] [Google Scholar]
- Spitz FR, Nguyen D, Skibber JM, Cusack J, Roth JA, Cristiano RJ. In vivo adenoviral-mediated p53 tumor suppressor gene therapy for colorectal cancer. Anticancer Res. 3422;16:3415–1996. [PubMed] [Google Scholar]
- Pirollo KF, Hao Z, Rait A, Jang, Fee WE, Ryan P, Chiang Y, Chang EH. p53 mediated sensitization of squamous cell carcinoma of the head and neck radiotherapy. Oncogene. 1746;14:1735–1997. doi: 10.1038/sj.onc.1201116. [DOI] [PubMed] [Google Scholar]
- Pirollo KF, Hao Z, Rait A. p53 mediated sensitization of squamous cell carcinoma of the head, and neck radiotherapy. Oncogene. 1996;14:1735–1746. doi: 10.1038/sj.onc.1201116. [DOI] [PubMed] [Google Scholar]
- Lang FF, Yung WKA, Raju U. Enhancement of radiosensitivity of wild-type p53 human glioma cells by adenovirus-mediated delivery of the p53 gene. J Neurosurg. 1998;89:125–132. doi: 10.3171/jns.1998.89.1.0125. [DOI] [PubMed] [Google Scholar]
- Badie B, Goh CS, Klaver J. Combined radiation and p53 gene therapy of malignant glioma cells. Cancer Gene Ther. 1999;6:155–162. doi: 10.1038/sj.cgt.7700009. [DOI] [PubMed] [Google Scholar]
- Kock H, Harris MP, Anderson SC, Machemer T, Hancock W, Sutjipto S, Wills KN, Gregory RJ, Shepard HM, Westphal M, Maneval DC. Adenovirus mediated p53 gene transfer suppresses growth of human glioblastoma cells in vitro and in vivo. Int J Cancer. 1996;67:808–815. doi: 10.1002/(SICI)1097-0215(19960917)67:6<808::AID-IJC9>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- Li JH, Lax SA, Kim J. The effects of ionizing radiation and adenoviral p53 therapy in nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 1999;43:607–616. doi: 10.1016/s0360-3016(98)00432-5. [DOI] [PubMed] [Google Scholar]
- Gallardo D, Drazan KE, McBride WH. Adenovirus-based transfer of wild-type p53 gene increases ovarian tumor radiosensitivity. Cancer Res. 1996;56:4891–4893. [PubMed] [Google Scholar]
- Colletier PJ, Ashoori F, Cowen D, Meyn RE, Tofilin P, Meistrich ME, Pollack A. Adenoviral-mediated p53 transgene expression sensitizes both wild-type and null p53 prostate cancer cells in vitro to radiation. Int J Radiation Oncology Biol Phys. 2000;48(5):1507–1512. doi: 10.1016/s0360-3016(00)01409-7. [DOI] [PubMed] [Google Scholar]
- Srivastava S, Katayose D, Tong YA, Craig CR, Mcleod DG, Moul JW, Cowan KH, Seth P. Recombinant adenovirus vector expressing wild-type p53 is a potent inhibitor of prostate cancer cell proliferation. Urology. 1995;46:843–848. doi: 10.1016/S0090-4295(99)80355-0. [DOI] [PubMed] [Google Scholar]
- Cowen D, Salem N, Ashoori F, Meyn R, Meistrich ML, Roth JA, Pollack A. Prostate Cancer Radiosensitization in Vivo with Adenovirus mediated p53. Gene Therapy 4402. 2000;6:4402–4408. [PubMed] [Google Scholar]
- Rakozy C, Grignon DJ, Li YW. p53 gene alterations in prostate cancer after radiation failure, and the association with clinical outcome. A molecular and immunohistochemical analysis. Pathol Res Pract. 1999;195:129–135. doi: 10.1016/S0344-0338(99)80024-7. [DOI] [PubMed] [Google Scholar]
- Cheng L, Sebo TJ, Cheville JC. p53 protein overexpression is associated with increased cell proliferation in patients with locally recurrent prostate carcinoma after radiation therapy. Cancer. 1999;85:1293–1299. [PubMed] [Google Scholar]
- Grossfield GD, Olumi AF, Connolly JA. Locally recurrent prostate tumors following either radiation therapy or radical prostatectomy have changes in Ki-67 labeling index, p53 and Bcl-2 immunoreactivity. J Urol. 1998;159:1437–1443. doi: 10.1097/00005392-199805000-00004. [DOI] [PubMed] [Google Scholar]
- Prendergast NJ, Atkins MR, Schatte EC. p53 immunohistochemical and genetic alterations are associated at high incidence with post-irradiated locally persistent prostate carcinoma. J Urol. 1996;155:1685–1692. [PubMed] [Google Scholar]
- Che M, DeSilvio M, Pollack A, Grignon DJ, Venkatesan VM, Hanks GE, Sandler HM. RTOG. Prognostic value of abnormal p53 expression in locally advanced prostate cancer treated with androgen deprivation and radiotherapy: a study based on RTOG 9202. Int J Radiat Oncol Biol Phys. 2007;69(4):1117–23. doi: 10.1016/j.ijrobp.2007.04.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grignon DJ, Caplan R, Sarkar FH, Lawton CA, Hammond EH, Pilepich MV, Forman JD, Mesic J, Fu KK, Abrams RA, Pajak TF, Shipley WU, Cox JD. p53 status and prognosis of locally advanced prostatic adenocarcinoma: a study based on RTOG 8610. J Natl Cancer Inst. 1997;89(2):158–65. doi: 10.1093/jnci/89.2.158. [DOI] [PubMed] [Google Scholar]
- D'Amico AV, Halabi S, Vollmer R, Loffredo M, McMahon E, Sanford B, Archer L, Vogelzang NJ, Small EJ, Kantoff PW. Cancer and Leukemia Group B. p53 protein expression status and recurrence in men treated with radiation and androgen suppression therapy for higher-risk prostate cancer: a prospective phase II Cancer and Leukemia Group B Study (CALGB 9682) Urology. 2008;71(5):933–7. doi: 10.1016/j.urology.2007.11.005. [DOI] [PubMed] [Google Scholar]
- Swisher SG, Roth JA, Komaki R, Gu J, Lee JJ, Hicks M, Ro JY, Hong WK, Merritt JA, Ahrar K, Atkinson NE, Correa AM, Dolormente M, Dreiling L, El-Naggar AK, Fossella F, Francisco R, Glisson B, Grammer S, Herbst R, Huaringa A, Kemp B, Khuri FR, Kurie JM, Liao Z, McDonnell TJ, Morice R, Morello F, Munden R, Papadimitrakopoulou V, Pisters KM, Putnam JB Jr, Sarabia AJ, Shelton T, Stevens C, Shin DM, Smythe WR, Vaporciyan AA, Walsh GL, Yin M. Induction of p53-regulated genes and tumor regression in lung cancer patients after intratumoral delivery of adenoviral p53 (INGN 201) and radiation therapy. Clin Cancer Res. 2003;9(1):93–101. [PubMed] [Google Scholar]
- Pisters LL, Pettaway CA, Troncoso P, McDonnell TJ, Stephens LC, Wood CG, Do KA, Brisbay SM, Wang X, Hossan EA, Evans RB, Soto C, Jacobson MG, Parker K, Merritt JA, Steiner MS, Logothetis CJ. Evidence that transfer of functional p53 protein results in increased apoptosis in prostate cancer. Cancer Res. 2004;10(8):2587–93. doi: 10.1158/1078-0432.ccr-03-0388. [DOI] [PubMed] [Google Scholar]
- Smith WL, DeWitt DL, Garavito MG. Cyclooxygenases: structure, cellular, and molecular biology. Annu Rev Biochem. 2000;69:145–182. doi: 10.1146/annurev.biochem.69.1.145. [DOI] [PubMed] [Google Scholar]
- Teismann P, Tieu K, Choi DK, Wu DC, Naini A, Hunot S, Vila M, Jackson-Lewis V, Przedborski S. Cyclooxygenase-2 is instrumental in Parkinson's disease neurodegeneration. Proc Natl Acad Sci USA. 2003;100(9):5473–8. doi: 10.1073/pnas.0837397100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karim A, Tolbert DS, Hunt TL, Hubbard RC, Harper KM, Geis GS. Celecoxib, a specific COX-2 inhibitor, has no significant effect on methotrexate pharmacokinetics in patients with rheumatoid arthritis. J Rheumatol. 1999;26(12):2539–43. [PubMed] [Google Scholar]
- Wang MT, Honn KV, Nie D. Cyclooxygenases, prostanoids, and tumor progression. Cancer Metastasis Rev. 2007;26(3–4):525–34. doi: 10.1007/s10555-007-9096-5. [DOI] [PubMed] [Google Scholar]
- Nasir A, Fernandez PM, Chughtai OR, Kaiser HE. COX-2, NSAIDs and human neoplasia. Part I: Colorectal neoplasms. In Vivo. 2002;16(6):501–9. [PubMed] [Google Scholar]
- Singh-Ranger G, Mokbel K. The role of cyclooxygenase-2 (COX-2) in breast cancer, and implications of COX-2 inhibition. Eur J Surg Oncol. 2002;28(7):729–37. doi: 10.1053/ejso.2002.1329. [DOI] [PubMed] [Google Scholar]
- Dixon DA. Regulation of COX-2 expression in human cancers. Prog Exp Tumor Res. 2003;37:52–71. doi: 10.1159/000071363. [DOI] [PubMed] [Google Scholar]
- Inoue H, Yokoyama C, Hara S, Tone Y, Tanabe T. Transcriptional regulation of human prostaglandin-endoperoxide synthase-2 gene by lipopolysaccaride and phorbol ester in vascular endothelial cells. J Biol Chem. 1995;270(42):24965–71. doi: 10.1074/jbc.270.42.24965. [DOI] [PubMed] [Google Scholar]
- Anai S, Tanaka M, Shiverick KT, Kim W, Takada S, Boehlein S, Goodison S, Mizokami A, Rosser CJ. Increased Expression of Cyclooxygenase-2 Correlates With Resistance to Radiation in Human Prostate Adenocarcinoma Cells. The Journal of Urology. 2007;177:1913–1917. doi: 10.1016/j.juro.2007.01.019. [DOI] [PubMed] [Google Scholar]
- Kirschenbaum A, Liu X, Yao S, Levine AC. The role of cyclooxygenase-2 in prostate cancer. Urology. 2001;58:127. doi: 10.1016/s0090-4295(01)01255-9. [DOI] [PubMed] [Google Scholar]
- Rubin DB, Drab EA, Ts'ao CH, Gardner D, Ward WF. Prostacyclin synthesis in irradiated endothelial cells cultured from bovine aorta. J Appl Physiol. 1985;58:592. doi: 10.1152/jappl.1985.58.2.592. [DOI] [PubMed] [Google Scholar]
- Eisen V, Walker DI. Effect of ionizing radiation on prostaglandin 15-OH-dehydrogenase (PGDH) [proceedings] Br J Pharmacol. 1978;62:461. [PMC free article] [PubMed] [Google Scholar]
- Choy H, Milas L. Enhancing radiotherapy with cyclooxygenase-2 enzyme inhibitors: a rational advance? J Natl Cancer Inst. 2003;95:1440. doi: 10.1093/jnci/djg058. [DOI] [PubMed] [Google Scholar]
- Khor LY, Bae K, Pollack A, Hammond ME, Grignon DJ, Venkatesan VM, Rosenthal SA, Ritter MA, Sandler HM, Hanks GE, Shipley WU, Dicker AP. COX-2 expression predicts prostate-cancer outcome: analysis of data from the RTOG 92-02 trial. Lancet Oncol. 2007;8(10):912–20. doi: 10.1016/S1470-2045(07)70280-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dancey J, Sausville EA. Issues and progress with protein kinase inhibitors for cancer treatment. Nat Rev Drug Discov. 2003;2:296–313. doi: 10.1038/nrd1066. [DOI] [PubMed] [Google Scholar]
- Manning G, Whyte DB, Martinez R, Hunter T, Sudarsanam S. The protein kinase complement of the human genome. Science. 2002;298:1912–34. doi: 10.1126/science.1075762. [DOI] [PubMed] [Google Scholar]
- Wilhelm SM, Adnane L, Newell P, Villanueva A, Llovet JM, Lynch M. Preclinical overview of sorafenib, a multikinase inhibitor that targets both Raf and VEGF and PDGF receptor tyrosine kinase signaling. Mol Cancer Ther. 2008;7(10):3129–40. doi: 10.1158/1535-7163.MCT-08-0013. [DOI] [PubMed] [Google Scholar]
- Ryan C, Bukowski R, Figlin R. The Advanced Renal Cell Carcinoma Sorafenib (ARCCS) expanded access trial: Long-term outcomes in first-line patients (pts) J Clin Oncol. 2007;25:5096. [Google Scholar]
- Motzer RJ, Rini BI, Bukowski RM. Sunitinib in patients with metastatic renal cell carcinoma. JAMA. 2006;295:2516–2524. doi: 10.1001/jama.295.21.2516. [DOI] [PubMed] [Google Scholar]
- Hudes G, Carducci M, Tomczak P. Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. N Engl J Med. 2007;356:2271–2281. doi: 10.1056/NEJMoa066838. [DOI] [PubMed] [Google Scholar]
- Dobelbower MC, Russo SM, Raisch KP, Seay LL, Clemons LK, Suter S, Posey J, Bonner JA. Epidermal growth factor receptor tyrosine kinase inhibitor, erlotinib, and concurrent 5-fluorouracil, cisplatin and radiotherapy for patients with esophageal cancer: a phase I study. Anticancer Drugs. 2006;17(1):95–102. doi: 10.1097/01.cad.0000185178.26862.4c. [DOI] [PubMed] [Google Scholar]
- Kyprianou N, lsaacs JT. Activation of programmed cell death in rat ventral prostate following castration. Endocrinology. 1988;22:552–562. doi: 10.1210/endo-122-2-552. [DOI] [PubMed] [Google Scholar]