Abstract
Aims
The aim of this study was to examine the explanatory power of intelligence (IQ) compared with traditional cardiovascular disease (CVD) risk factors in the relationship of socio-economic disadvantage with total and CVD mortality, that is the extent to which IQ may account for the variance in this well-documented association.
Methods and results
Cohort study of 4289 US male former military personnel with data on four widely used markers of socio-economic position (early adulthood and current income, occupational prestige, and education), IQ test scores (early adulthood and middle-age), a range of nine established CVD risk factors (systolic and diastolic blood pressure, total blood cholesterol, HDL cholesterol, body mass index, smoking, blood glucose, resting heart rate, and forced expiratory volume in 1 s), and later mortality. We used the relative index of inequality (RII) to quantify the relation between each index of socio-economic position and mortality. Fifteen years of mortality surveillance gave rise to 237 deaths (62 from CVD and 175 from ‘other’ causes). In age-adjusted analyses, as expected, each of the four indices of socio-economic position was inversely associated with total, CVD, and ‘other’ causes of mortality, such that elevated rates were evident in the most socio-economically disadvantaged men. When IQ in middle-age was introduced to the age-adjusted model, there was marked attenuation in the RII across the socio-economic predictors for total mortality (average 50% attenuation in RII), CVD (55%), and ‘other’ causes of death (49%). When the nine traditional risk factors were added to the age-adjusted model, the comparable reduction in RII was less marked than that seen after IQ adjustment: all-causes (40%), CVD (40%), and ‘other’ mortality (43%). Adding IQ to the latter model resulted in marked, additional explanatory power for all outcomes in comparison to the age-adjusted analyses: all-causes (63%), CVD (63%), and ‘other’ mortality (65%). When we utilized IQ in early adulthood rather than middle-age as an explanatory variable, the attenuating effect on the socio-economic gradient was less pronounced although the same pattern was still present.
Conclusion
In the present analyses of socio-economic gradients in total and CVD mortality, IQ appeared to offer greater explanatory power than that apparent for traditional CVD risk factors.
Keywords: Cardiovascular disease, IQ, Socio-economic status
Introduction
Socio-economic inequalities in health, as exemplified by cardiovascular disease (CVD), are essentially universal: with the exception of very few outcomes, poorer health is more common in the disadvantaged.1 Reducing these differentials is a priority for many governments, including those of the UK2,3 and USA,4 and for the World Health Organization, which has launched the Global Commission on Social Determinants of Health.5,6 For interventions to exert an effect, it is first crucial to understand the underlying causes of these inequalities.7
Explanations for how socio-economic disadvantage might lead to CVD and other chronic diseases include access to resources (e.g. education and income), environmental exposures (e.g. housing conditions), and, most obviously, health-related behaviours (e.g. tobacco smoking, physical activity, and diet) and their physiological correlates (e.g. obesity, and raised levels of blood pressure and high cholesterol).6,8 That controlling for preventable behavioural and physiological risk factors attenuates but fails to eliminate socio-economic gradients in health, particularly CVD,9,10 raises the possibility that as yet unmeasured psychological factors need to be considered. One such characteristic is intelligence or cognitive function (denoted here as IQ) which is strongly related to socio-economic position11 and, in a recent series of studies, consistently reveals inverse associations with total mortality12,13 and CVD14–17 mortality, such that higher scores appear to confer protection.
The extent to which IQ may ‘explain’ socio-economic inequalities in health—that is the degree to which it may account for the variance in this association—can be tested by simply adjusting the relationship between socio-economic position and a given health outcome for this psychological characteristic. In the only two reports of which we are aware,18,19 although IQ did not offer full explanatory power, there was evidence of marked attenuation of the socio-economic–illness gradient. This was particularly apparent when total and CVD mortality were the outcomes of interest.18 However, importantly, because these studies were either not well characterized for classic risk factors for premature mortality and CVD (raised blood cholesterol and blood glucose),18 or did not have sufficient numbers of CVD deaths,19 they could not provide a comparison between the explanatory power of IQ with that seen for established risk indices in the socio-economic-mortality gradient. This is possible in the present study which holds extensive data on IQ, four markers of socio-economic position, a wide range of risk indices, and cause-specific mortality.
Methods
Background
Following concerns that the health of Vietnam veterans may have been detrimentally affected by their military experiences, the US congress directed that a series of epidemiological studies be conducted. One such investigation was the Vietnam Experience Study (VES). The VES has been described in detail elsewhere20–24 and has recently been used to examine the predictive capacity of pre-morbid IQ for a range of health outcomes.16,25–27 The study was established retrospectively in the early 1980s when 18 313 former US army personnel—entering the service between 1965 and 1971—qualified for inclusion in the cohort.
Data collection at army entry
Army income based on 1964 pay scales (≤85, 86–98, 99–119, 120–144, and ≥145 USD/month) was extracted from service records when the men were around 20 years of age. On enlistment, recruits also took a general aptitude test: the Army General Technical Test (AGTT).28 This consists of two subtests, verbal and arithmetic reasoning. Scores on the AGTT correlate highly with those on standard tests of intelligence,28 including, in this cohort, the Wechsler Adult Intelligence Scale.25,27 Data retrieved from service records are described herein as being from ‘wave 1’.
Data collection in middle-age
At around 38 years of age (in 1985/86), 15 288 men (85.6% of those surviving from the original cohort) participated in a telephone survey during which smoking habits and socio-economic position were assessed using years of completed education (range: 1–18 years in 1-year increments), pre-tax total household income (range: <5000 to >50 000 USD/year, generally in 10 000 increments), and a continuous index of occupational prestige in which a higher score denoted increased social status (range: 11.8–88.5, SD 19).29,30 To facilitate analyses, data on education (Grades ≤11, 12, and ≥13), and mid-life (≤20 000, 20 001–40 000, and >40 000 USD/year) and army income (83–119, 120–144, and 145 USD/month) were collapsed into a smaller number of categories.
A random sample of these respondents (n = 6443) were invited to attend a 3-day medical examination; 4462 (69%) did so. Data were collected using standard protocols for the period.20,21 In short, after an overnight fast, blood was drawn and analysed for levels of triglycerides and cholesterol fractions were ascertained using a Kodak Ektachem 700 autoanalyzer.20,21 Serum glucose level was determined with a standard adaptation of the glucose oxidase–peroxidase–chromogen-coupled system for glucose determination in biologic fluids.20,21 With the participant in a sitting position, blood pressure was measured twice in the right arm using a standard mercury sphygmomanometer; for the purposes of analyses, an average was computed. Resting heart rate, an indicator of cardiorespiratory fitness and therefore a proxy for regular physical activity,31,32 was also recorded. Lung function, as indexed by forced expiratory volume in 1 s, was determined using spirometry. Measured height and weight were used to calculate body mass index (kg/m2). Finally, the study participants again completed the AGTT, exactly as administered at wave 1 some 20 years previously. The telephone survey and medical exam are collectively referred to as ‘wave 2’ herein.
Ascertainment of mortality
Vital status of men between army discharge and 31 December 1983 (the date the cohort was established) was ascertained by cross-checking against a variety of mortality databases supplied by the US army, the Veterans Administration (Beneficiary Identification and Records Locator Subsystem), the Social Security Administration, the Internal Revenue Service, and the National Center for Health Statistics (National Death Index). All potential matches were manually reviewed. Study participants were followed for mortality experience for a mean of 15.1 years. Follow-up time was taken from the medical examination until death or 31 December 2000, whichever came first.
Statistical analyses
Given that the different markers of socio-economic position have different coding structures, a direct comparison of the magnitude of the relation of each with mortality is problematic. For this reason, we used the relative index of inequality (RII) to quantify this association as we18 and others19 have done previously. First, we reversed scores for income, occupational prestige, and education so that higher scores represented greater disadvantage (risk). The RII was then derived by ranking the subjects on each of the socio-economic variables and then dividing this rank score by the sample size to yield a value between 0 and 1. When included in the Cox proportional hazard models33 with mortality as the outcome, the estimates for the RII can be interpreted as the mortality hazard for the disadvantaged end of the socio-economic distribution relative to the advantaged. Thus, an RII of 2.0 indicates that the mortality hazard between the extreme ends of the socio-economic distribution is twice as high for the most disadvantaged (greatest risk) compared with the most advantaged (lowest risk).
In these models, we adjusted for age throughout. Our aim in these analyses was to assess whether controlling for IQ and, separately, the nine classic risk factors measured in the study had an impact on each of the associations between the socio-economic variables and mortality. Thus, first, we added IQ to the age-adjusted model. Secondly, we added the group of nine classic risk factors to the age-adjusted model. By comparing the RII produced from these two models with those from the age-adjusted analyses, we were able to calculate a percentage change in RII and therefore gauge the impact, if any, of these statistical controls on the socio-economic gradient in mortality. Finally, in order to ascertain whether IQ added any explanatory power above that offered by the risk factor-adjusted model, we added IQ to it. Analyses throughout were based on 4289 respondents with complete data. We have previously shown that this group is representative of the original sample of study participants.25
Results
In Table 1, we present the relation of IQ score, as ascertained from the AGTT at both wave 1 and wave 2, with the four indicators of socio-economic disadvantage across the adult life course. Throughout, higher IQ scores from both tests were associated with more favourable social circumstances. Unsurprisingly, the strongest correlations were seen for education (r = 0.55 and 0.53 for IQ at wave 1 and wave 2, respectively), followed by occupational prestige (0.44 and 0.43), family income (0.39 and 0.40), and army income (0.30 and 0.28).
Table 1.
IQ in relation to indicators of socio-economic status in the VES (n = 4289)
| No. of men | AGTT (wave 1) |
AGTT (wave 2) |
|||
|---|---|---|---|---|---|
| Mean (SD) | P-trend | Mean (SD) | P-trend | ||
| Army income (USD/month) | |||||
| 83–119 | 536 | 95.8 (18.5) | 100.6 (21.1) | ||
| 120–144 | 2121 | 103.1 (20.3) | 107.6 (22.2) | ||
| 145 | 1632 | 113.3 (18.7) | <0.001 | 118.0 (19.2) | <0.001 |
| Education attainment | |||||
| Grade ≤11 | 523 | 86.5 (16.4) | 90.0 (20.4) | ||
| Grade 12 | 1573 | 100.3 (17.1) | 104.5 (19.7) | ||
| Grade ≥13 | 2193 | 114.9 (18.6) | <0.001 | 120.0 (18.4) | <0.001 |
| Family income (USD/year) | |||||
| ≤20 000 | 1219 | 96.4 (19.8) | 99.8 (22.7) | ||
| 20 001–40 000 | 2141 | 106.4 (18.9) | 111.5 (20.0) | ||
| >40 000 | 929 | 117.9 (18.0) | <0.001 | 123.1 (17.0) | <0.001 |
| Occupational prestigea | |||||
| Q1 (lowest) | 990 | 96.9 (19.1) | 100.4 (21.7) | ||
| Q2 | 1151 | 99.4 (19.1) | 103.9 (21.7) | ||
| Q3 | 1046 | 108.5 (18.3) | 114.0 (18.9) | ||
| Q4 | 1102 | 119.0 (17.4) | <0.001 | 123.8 (16.5) | <0.001 |
aOccupational prestige is a continuous variable that was categorized here for ease of presentation.
After an average of 15.1 years of follow-up, there were 237 deaths (of which 62 were ascribed to CVD and 175 to ‘other’ causes). In Table 2, we summarize the relation of the four indicators of socio-economic position with three mortality outcomes across three regression models. As anticipated, for all mortality outcomes, socio-economic position was inversely associated with mortality risk such that the highest rates were apparent in the most disadvantaged men. Of the individual socio-economic indices, mid-life income revealed the strongest relation with mortality risk with army income, education, and occupational prestige of similar magnitude. When IQ of the men at around 18 years of age (wave 1) was added to the multivariable model, there was marked attenuation of the socio-economic gradient across socio-economic markers. Thus, in the IQ-adjusted analyses, the average per cent reduction in the RII across the four socio-economic predictors was 38% for total mortality, 34% for CVD, and 40% for other causes of death. When the nine classic risk factors were added to the age-adjusted model, the comparable attenuation was slightly higher across each outcome. Adding IQ to the model containing these classic risk factors appeared to add additional explanatory power for all-cause (40–55% reduction in RII) and ‘other’ mortality (43–61%), but for CVD, the difference between these two models was marginal (40–45%).
Table 2.
Relative index of inequality (95% confidence interval) for the relation of indicators of socio-economic position with mortality in the VES—controlling for IQ at wave 1 (AGTT) and established risk factors at wave 2 (n = 4289)
| Outcome (no. of deaths) | Age-adjusted | Adjusted for age plus IQ | % changea | Adjusted for age plus risk factorsb | % changec | Adjusted for age plus risk factors and IQ | % changed |
|---|---|---|---|---|---|---|---|
| All-cause mortality (237) | |||||||
| Army incomee | 3.24 (1.95, 5.41) | 2.38 (1.40, 4.05) | 38.4 | 2.46 (1.48, 4.12) | 34.8 | 2.10 (1.24, 3.58) | 50.9 |
| Occupation | 2.96 (1.88, 4.67) | 2.05 (1.24, 3.39) | 46.4 | 2.09 (1.31, 3.33) | 44.4 | 1.70 (1.03, 2.84) | 64.3 |
| Mid-life income | 7.34 (4.48, 12.0) | 5.91 (3.49, 10.0) | 22.6 | 5.08 (3.09, 8.37) | 35.6 | 4.69 (2.78, 7.93) | 41.8 |
| Education | 3.72 (2.31, 6.00) | 2.47 (1.42, 4.32) | 46.0 | 2.44 (1.49, 3.99) | 47.1 | 1.96 (1.11, 3.46) | 64.7 |
| 38.4f | 40.5 | 55.4 | |||||
| CVD mortality (62) | |||||||
| Army income | 2.52 (0.95, 6.72) | 1.88 (0.68, 5.21) | 42.1 | 2.06 (0.76, 5.63) | 30.3 | 1.90 (0.67, 5.37) | 40.8 |
| Occupation | 4.11 (1.68, 10.1) | 3.20 (1.20, 8.54) | 29.3 | 2.62 (1.04, 6.60) | 47.9 | 2.57 (0.94, 7.10) | 49.5 |
| Mid-life income | 6.48 (2.52, 16.7) | 5.36 (1.95, 14.7) | 20.4 | 5.17 (1.94, 13.8) | 23.9 | 5.26 (1.89, 14.7) | 22.3 |
| Education | 3.29 (1.31, 8.28) | 2.25 (0.76, 6.64) | 45.4 | 1.93 (0.75, 4.95) | 59.4 | 1.78 (0.58, 5.46) | 65.9 |
| 34.3 | 40.4 | 44.6 | |||||
| Remaining causes (175) | |||||||
| Army income | 3.56 (1.95, 6.49) | 2.60 (1.39, 4.85) | 37.5 | 2.57 (1.42, 4.67) | 38.7 | 2.14 (1.16, 3.98) | 55.5 |
| Occupation | 2.63 (1.55, 4.47) | 1.75 (0.97, 3.14) | 54.0 | 1.85 (1.07, 3.19) | 47.9 | 1.42 (0.79, 2.57) | 74.2 |
| Mid-life income | 7.68 (4.32, 13.7) | 6.13 (3.31, 11.3) | 23.2 | 5.00 (2.80, 8.94) | 40.1 | 4.46 (2.42, 8.22) | 48.2 |
| Education | 3.89 (2.23, 6.81) | 2.56 (1.34, 4.90) | 46.0 | 2.62 (1.47, 4.66) | 43.9 | 2.02 (1.05, 3.92) | 64.7 |
| 40.2 | 42.7 | 60.7 | |||||
aBased on a comparison of the age-adjusted RII with that for the IQ-adjusted RII using the formulae: ([RIIage-adjusted − 1] − [RIIIQ and/or risk factor-adjusted − 1]/[RIIage-adjusted − 1]) × 100%.
bSystolic and diastolic blood pressure, total cholesterol, HDL cholesterol, BMI, smoking, blood glucose, resting heart rate, and forced expiratory volume in 1 s.
cBased on a comparison of the age-adjusted RII with that for the risk factor-adjusted RII.
dBased on a comparison of the age-adjusted RII with that for the IQ- and risk factor-adjusted RII.
eResults are hazards ratio for a comparison of the most socio-economically disadvantaged men with the least disadvantaged.
fMean per cent change across the four socio-economic indices for each outcome.
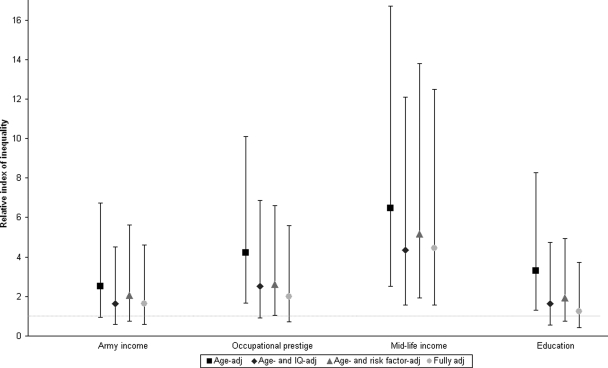
In Table 3, we report similar analyses to those given in Table 2, the exception being that the IQ measure was captured at wave 2 when the study participants were middle-aged. Although a similar pattern of association with that seen when adjustment was made for IQ at wave 1, the attenuating effect of controlling for IQ in middle-age was more marked and, for most socio-economic indices, exceeded that apparent following adjustment for the classic risk factors. Thus, in the IQ-adjusted analyses, the average per cent reduction in the RII across the four socio-economic predictors was 50% for total mortality, 55% for CVD, and 49% for other causes of death. When the risk factors were added separately to the age-adjusted model, the comparable attenuation was lower across each outcome: all-causes (41% reduction in RII); CVD (40%), and ‘other’ mortality (43%). Adding IQ to the latter model resulted in considerable additional explanatory power for all outcomes: all-causes (63% reduction in RII), CVD (63%), and ‘other’ mortality (65%). The total explanatory effect in this final model which contained IQ at wave 2 was markedly higher than that containing IQ at wave 1. The results for socio-economic status, IQ, and CVD mortality are depicted in Figure 1.
Table 3.
Relative index of inequality (95% confidence interval) for the relation of indicators of socio-economic position with mortality in the VES—controlling for IQ at wave 2 (AGTT) and established risk factors at wave 2 (n = 4289)
| Outcome (no. deaths) | Age adjusted | Adjusted for age plus IQ | % changea | Adjusted for age plus risk factorsb | % changec | Adjusted for age plus risk factors and IQ | % changed |
|---|---|---|---|---|---|---|---|
| All-cause mortality (237) | |||||||
| Army incomee | 3.24 (1.95, 5.41) | 2.21 (1.30, 3.76) | 46.0 | 2.46 (1.48, 4.12) | 34.8 | 1.97 (1.16, 3.34) | 56.7 |
| Occupation | 2.96 (1.88, 4.67) | 1.78 (1.07, 2.95) | 60.2 | 2.09 (1.31, 3.33) | 44.4 | 1.52 (0.91, 2.54) | 73.5 |
| Mid-life income | 7.34 (4.49, 12.0) | 5.24 (3.09, 8.89) | 33.1 | 5.08 (3.09, 8.37) | 35.6 | 4.30 (2.54, 7.29) | 47.9 |
| Education | 3.72 (2.31, 6.00) | 2.06 (1.19, 3.58) | 61.0 | 2.44 (1.49, 3.99) | 47.1 | 1.67 (0.95, 2.94) | 75.4 |
| 50.1f | 40.5 | 63.4 | |||||
| CVD mortality (62) | |||||||
| Army income | 2.52 (0.95, 6.72) | 1.63 (0.59, 4.52) | 58.6 | 2.06 (0.76, 5.63) | 30.3 | 1.63 (0.58, 4.60) | 58.6 |
| Occupation | 4.12 (1.68, 10.1) | 2.53 (0.93, 6.85) | 51.0 | 2.62 (1.04, 6.60) | 47.9 | 2.01 (0.72, 5.60) | 67.6 |
| Mid-life income | 6.48 (2.52, 16.7) | 4.35 (1.57, 12.1) | 38.9 | 5.17 (1.94, 13.8) | 23.9 | 4.44 (1.57, 12.5) | 37.2 |
| Education | 3.29 (1.31, 8.28) | 1.62 (0.56, 4.74) | 72.9 | 1.93 (0.75, 4.95) | 59.4 | 1.24 (0.41, 3.74) | 89.5 |
| 55.3 | 40.4 | 63.2 | |||||
| Remaining causes (175) | |||||||
| Army income | 3.56 (1.95, 6.49) | 2.47 (1.32, 4.61) | 42.6 | 2.57 (1.42, 4.67) | 38.7 | 2.07 (1.12, 3.83) | 58.2 |
| Occupation | 2.63 (1.55, 4.47) | 1.57 (0.87, 2.83) | 65.0 | 1.85 (1.07, 3.19) | 47.9 | 1.33 (0.73, 2.40) | 79.6 |
| Mid-life income | 7.68 (4.32, 13.7) | 5.61 (3.02, 10.4) | 31.0 | 5.00 (2.80, 8.94) | 40.1 | 4.22 (2.28, 7.82) | 51.8 |
| Education | 3.89 (2.23, 6.81) | 2.25 (1.18, 4.28) | 56.7 | 2.62 (1.47, 4.66) | 43.9 | 1.85 (0.96, 3.56) | 70.6 |
| 48.8 | 42.7 | 65.1 | |||||
aBased on a comparison of the age-adjusted RII with that for the IQ-adjusted RII using the formulae: ([RIIage-adjusted − 1] − [RIIIQ and/or risk factor-adjusted − 1]/[RIIage-adjusted − 1]) × 100%.
bSystolic and diastolic blood pressure, total cholesterol, HDL cholesterol, BMI, smoking, blood glucose, resting heart rate, and forced expiratory volume in 1 s.
cBased on a comparison of the age-adjusted RII with that for the risk factor-adjusted RII.
dBased on a comparison of the age-adjusted RII with that for the IQ- and risk factor-adjusted RII.
eResults are hazards ratio for a comparison of the most socio-economically disadvantaged men with the least disadvantaged.
fMean per cent change across the four socio-economic indices for each outcome.
Figure 1.
Relative index of inequality (95% confidence interval) for the relation of indicators of socio-economic position (disadvantaged vs. advantaged) with cardiovascular disease mortality in the VES—controlling for IQ at wave 2 (AGTT) and established risk factors at wave 2 (n = 4289). Full adjustment is adjustment for age, IQ, and all established CVD risk factors.
Discussion
The purpose of these analyses was to examine the degree to which IQ may account for the variance in the well-documented association between socio-economic position and mortality, including CVD, and the extent that IQ adds any explanatory power beyond that offered by adjusting for established risk factors. All the socio-economic mortality gradients were markedly attenuated when IQ was added to the univariate models, as they were when control was made for the nine classic risk factors. However, IQ appeared to offer some additional explanatory power above these latter adjustments, an effect that was most pronounced when the IQ measure from middle-age rather than early adulthood was utilized.
There are a number of explanations for mid-life IQ having a stronger attenuating effect on the socio-economic differentials in mortality than early measurement of this psychological characteristic. First, IQ may be, at least partially, a ‘record’ of bodily insults across the life course.34 Thus, IQ scores have been shown to be inversely correlated with important chronic diseases, such as hypertension,35 diabetes,36 and atherosclerosis;37 conditions that may remain hidden but nonetheless increase mortality risk. By the time of the later IQ assessment, the prevalence of such co-morbidities will have been higher than earlier in life. It may be, therefore, that low IQ test scores at this age already reflect deteriorating health, and therefore, adjustment for it may be partly controlling for subclinical health status when the study participants were examined in middle-age. We explored this issue by excluding deaths in the first 4 years of follow-up, reasoning that those dying from chronic disease during this period were likely to have the highest morbid load at study induction. Our results were little changed (tables not shown but available upon request). A second reason for the stronger attenuating effect of later life rather than earlier IQ may be the former's higher correlations with socio-economic position—if this was the case, we would anticipate greater attenuation offered by the contemporary IQ measure. However, mid-life IQ revealed very similar associations with mid-life socio-economic position to the correlations seen for early IQ.
Comparison with previous studies
As the first study to compare the explanatory power of IQ with well-established risk factors in the relation of socio-economic position with mortality, our study is very unusual. As such, there are few relevant reports with which to draw comparison. To our knowledge, only data from the Whitehall II of London-based civil servants19 and the West of Scotland ‘Twenty-0718’ population-based study have been explicitly utilized to examine the hypothesis that IQ may explain social inequalities in health. In these studies, for less objective measures of health—self-reported minor psychiatric illness, self-rated health, and self-reported long-term illness—the impact of adjusting for IQ appears to have a less pronounced impact on the socio-economic gradient than when CVD was the outcome of interest. No further adjustments were made in these investigations. The effect of controlling for measures of IQ on the socio-economic position–health relation in these analyses18,19 was more pronounced than adjustment for other psychological characteristics reported elsewhere such as job control38 and psychosocial stress.39
Study strengths and limitations
This study has a number of strengths, including the wide range of traditional risk factors for CVD and premature mortality collected and the complete mortality follow-up. It is not, however, without its shortcomings. First, the present analyses are based on a sample of men with complete information on IQ, covariates at telephone interview and medical exam, and mortality (n = 4289). This group represents 67% of the random subsample invited to the medical examination, that is 23% of persons originally enrolled in the study. Although the latter is based on a random sample of surviving men, concerns are nonetheless raised about selection bias, that is if the reported results differ markedly between persons included in the analyses and those not. As indicated above, there was generally little evidence of any systematic differences between the groups. This was confirmed when we computed the relation between army income ascertained at wave 1 with total mortality in men included in this analytical sample and, separately, those that were not. That the strength of this association (RIIdisdvantaged vs. advantaged; 95% CI) was similar in those included (3.24; 1.95, 5.41) and excluded (2.63; 2.02, 3.43) from the analyses (P-value for difference = 0.58) provides empirical support against selection bias. Secondly, because the risk factor data were mainly collected in the mid 1980s, we did not have information on emerging predictors such as inflammatory and thrombotic markers. We could not therefore examine their explanatory power for the socio-economic gradients in mortality.
A third limitation of the present study is that the verbal or written elements of the IQ tests were administered in English. In a previous study, we used reaction time scores, a culture-reduced indicator of cognitive ability, which is measured using a simple electronic device where the study participant merely responds as quickly as possible to a stimulus.18 Reaction time correlates moderately strongly with IQ test scores40 such that the longer the reaction time, the lower the mental ability. In that study,18 adjusting for reaction time scores also produced attenuation in the socio-economic health gradients that were comparable to those seen for a brief written test of IQ. Fourthly, the present study is limited by examining only men; it is uncertain to what extent these results are applicable to women—in studies which adjusted for IQ only, there was no evidence of a differential effect by gender, although, as discussed, there was no examination of the impact of control for traditional risk factors. Finally, it is plausible that the range of IQ scores in the present cohort may be narrower than in a population-based group, not only due to the occupational nature of the sample (the so called ‘healthy worker’ effect) but also because a criteria for study entry was that, on exiting the army, personnel had to have a rank corresponding to sergeant or below. However, because any reduced variance will apply to all variables in these analyses, we believe that the percentage reduction in the strength of the socio-economic position–mortality gradient should be the same as that seen in the general population.
Public health implications
Our findings suggest that measured IQ does not completely account for observed inequalities in health, but, probably through a variety of mechanisms, may quite strongly contribute to them. This implies that efforts to reduce inequalities should continue to be broadly based, including educational opportunities and interventions directed at early life.7,41 The latter may also elicit improvements in IQ, although results are mixed.42 Given that the general learning and reasoning ability captured by IQ tests may be important in the successful management of a person's health, it may be that individual cognition levels should be considered more carefully when preparing health promotion campaigns and in the health professional–client interaction.12
In conclusion, in this, the first study to examine the explanatory power of controlling for IQ on the socio-economic position–mortality gradient relative to adjustment for classic risk factors, IQ offered explanatory power above these traditional indices of risk. There is a need to advance the currently scant information about IQ and health, and explore how the links between low socio-economic status, low IQ, and poor health might be broken.
Funding
G.D.B. is a Wellcome Trust Fellow (WBS U.1300.00.006.00012.01). M.J.S. is funded by the British Heart Foundation and L.H.M. by The National Institute of Public Health, Denmark. The MRC Social and Public Health Sciences Unit receives funding from the UK Medical Research Council and the Chief Scientist Office at the Scottish Government Health Directorates. The Centre for Cognitive Ageing and Cognitive Epidemiology is supported by the Biotechnology and Biological Sciences Research Council, the Engineering and Physical Sciences Research Council, the Economic and Social Research Council, the Medical Research Council, and the University of Edinburgh as part of the cross-council Lifelong Health and Wellbeing initiative. Mortality surveillance of the cohort in the post-service VES was funded by the National Center for Environmental Health, Atlanta, USA.
Conflict of interest: none declared.
References
- 1.MacIntyre S. Social inequalities and health in the contemporary world: comparative overview. In: Strickland S, Shetty P, editors. Human Biology and Social Inequality (39th Symposium Volume of the Society for the Study of Human Biology) Cambridge: Cambridge University Press; 1998. [Google Scholar]
- 2.Chief Medical Officer. Health in Scotland 2004. Edinburgh: Scottish Executive; 2005. [Google Scholar]
- 3.Department of Health. Choosing Health: Making Healthy Choices Easier. London: The Stationery Office; 2004. [Google Scholar]
- 4.US Department of Health and Human Services. Healthy People 2010. Washington, DC: US Government Printing Office; 2000. [Google Scholar]
- 5.Marmot M. Social determinants of health inequalities. Lancet. 2005;365:1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 6.Wilkinson R, Marmot M. Social Determinants of Health: The Solid Facts. Copenhagen: World Health Organisation; 2003. [Google Scholar]
- 7.Acheson D. Independent Inquiry into Inequalities in Health: Report. London: TSO; 1998. [Google Scholar]
- 8.Gordon D, Shaw M, Dorling D, Davey Smith G. Inequalities in Health. Bristol: The Policy Press; 1999. [Google Scholar]
- 9.Yarnell JW. The PRIME study: classical risk factors do not explain the severalfold differences in risk of coronary heart disease between France and Northern Ireland. Prospective Epidemiological Study of Myocardial Infarction. QJM. 1998;91:667–676. doi: 10.1093/qjmed/91.10.667. [DOI] [PubMed] [Google Scholar]
- 10.Marmot MG, Shipley MJ, Rose G. Inequalities in death-specific explanations of a general pattern? Lancet. 1984;1:1003–1006. doi: 10.1016/s0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- 11.Neisser U, Boodoo G, Bouchard T, Jr, Boykin AW, Brody N, Ceci SJ, Halpern DF, Loehlin JC, Perloff R, Sternberg RJ, Urbina S. Intelligence: knowns and unknowns. Am Psychol. 1996;51:77–101. [Google Scholar]
- 12.Batty GD, Deary IJ, Gottfredson LS. Premorbid (early life) IQ and later mortality risk: systematic review. Ann Epidemiol. 2007;17:278–288. doi: 10.1016/j.annepidem.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 13.Hemmingsson T, Melin B, Allebeck P, Lundberg I. The association between cognitive ability measured at ages 18–20 and mortality during 30 years of follow-up—a prospective observational study among Swedish males born 1949–51. Int J Epidemiol. 2006;35:665–670. doi: 10.1093/ije/dyi321. [DOI] [PubMed] [Google Scholar]
- 14.Hart CL, Taylor MD, Davey Smith G, Whalley LJ, Starr JM, Hole DJ, Wilson V, Deary IJ. Childhood IQ, social class, deprivation, and their relationships with mortality and morbidity risk in later life: prospective observational study linking the Scottish Mental Survey 1932 and the Midspan studies. Psychosom Med. 2003;65:877–883. doi: 10.1097/01.psy.0000088584.82822.86. [DOI] [PubMed] [Google Scholar]
- 15.Batty GD, Mortensen EL, Nybo Andersen AM, Osler M. Childhood intelligence in relation to adult coronary heart disease and stroke risk: evidence from a Danish birth cohort study. Paediatr Perinat Epidemiol. 2005;19:452–459. doi: 10.1111/j.1365-3016.2005.00671.x. [DOI] [PubMed] [Google Scholar]
- 16.Batty GD, Shipley MJ, Mortensen L, Gale CR, Deary IJ. IQ in late adolescence/early adulthood, risk factors in middle-age, and later coronary heart disease mortality in men: the Vietnam Experience Study. Eur J Cardiovasc Prev Rehabil. 2008 doi: 10.1097/HJR.0b013e3282f738a6. (in press) [DOI] [PubMed] [Google Scholar]
- 17.Hemmingsson T, Essen JV, Melin B, Allebeck P, Lundberg I. The association between cognitive ability measured at ages 18–20 and coronary heart disease in middle age among men: a prospective study using the Swedish 1969 conscription cohort. Soc Sci Med. 2007 doi: 10.1016/j.socscimed.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 18.Batty GD, Der G, MacIntyre S, Deary IJ. Does IQ explain socioeconomic inequalities in health? Evidence from a population based cohort study in the west of Scotland. BMJ. 2006;332:580–584. doi: 10.1136/bmj.38723.660637.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh-Manoux A, Ferrie JE, Lynch JW, Marmot M. The role of cognitive ability (intelligence) in explaining the association between socioeconomic position and health: evidence from the Whitehall II prospective cohort study. Am J Epidemiol. 2005;161:831–839. doi: 10.1093/aje/kwi109. [DOI] [PubMed] [Google Scholar]
- 20.The Centers for Disease Control Vietnam Experience Study. Health status of Vietnam veterans. I. Psychosocial characteristics. JAMA. 1988;259:2701–2707. [PubMed] [Google Scholar]
- 21.The Centers for Disease Control Vietnam Experience Study. Health status of Vietnam veterans. II. Physical Health. JAMA. 1988;259:2708–2714. [PubMed] [Google Scholar]
- 22.The Centers for Disease Control Vietnam Experience Study. Health status of Vietnam veterans. III. Reproductive outcomes and child health. JAMA. 1988;259:2715–2719. [PubMed] [Google Scholar]
- 23.The Centers for Disease Control Vietnam Experience Study. Postservice mortality among Vietnam veterans. JAMA. 1987;257:790–795. [PubMed] [Google Scholar]
- 24.Boehmer TK, Flanders WD, McGeehin MA, Boyle C, Barrett DH. Postservice mortality in Vietnam veterans: 30-year follow-up. Arch Intern Med. 2004;164:1908–1916. doi: 10.1001/archinte.164.17.1908. [DOI] [PubMed] [Google Scholar]
- 25.Batty GD, Shipley MJ, Mortensen LH, Boyle SH, Barefoot J, Gronbaek M, Gale CR, Deary IJ. IQ in late adolescence/early adulthood, risk factors in middle age and later all-cause mortality in men: the Vietnam Experience Study. J Epidemiol Community Health. 2008;62:522–531. doi: 10.1136/jech.2007.064881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Batty GD, Mortensen L, Gale CR, Deary IJ. Is low IQ related to risk of death by homicide? Testing an hypothesis using data from the Vietnam Experience Study. Psychiatry Research. 2008;161:112–115. doi: 10.1016/j.psychres.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 27.Batty GD, Gale CR, Mortensen LH, Langenberg C, Shipley MJ, Deary IJ. Pre-morbid intelligence, the metabolic syndrome and mortality: the Vietnam Experience Study. Diabetologia. 2008;51:436–443. doi: 10.1007/s00125-007-0908-5. [DOI] [PubMed] [Google Scholar]
- 28.Montague EK, Williams HL, Lubin A, Gieseking CF. Army tests for assessment of intellectual deficit. US Armed Forces Med J. 1957;8:883–892. [PubMed] [Google Scholar]
- 29.Duncan O. A Socioeconomic Index for All Occupations. New York: Free Press; 1961. [Google Scholar]
- 30.Stevens G, Cho J. Socioeconomic Indexes and the New 1980 Census Occupational Classification Scheme. Soc Sci Res. 1985;14:142–168. [Google Scholar]
- 31.Blair SN, Kannel WB, Kohl HW, Goodyear N, Wilson PWF. Surrogate measures of physical activity and physical fitness. Am J Epidemiol. 1989;129:1145–1156. doi: 10.1093/oxfordjournals.aje.a115236. [DOI] [PubMed] [Google Scholar]
- 32.Davey Smith G, Shipley MJ, Batty GD, Morris JN, Marmot M. Physical activity and cause-specific mortality in the Whitehall study. Public Health. 2000;114:308–315. doi: 10.1038/sj.ph.1900675. [DOI] [PubMed] [Google Scholar]
- 33.Cox DR. Regression models and life-tables. J R Stat Soc (Ser B) 1972;34:187–220. [Google Scholar]
- 34.Whalley LJ, Deary IJ. Longitudinal cohort study of childhood IQ and survival up to age 76. BMJ. 2001;322:1–5. doi: 10.1136/bmj.322.7290.819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Manolio TA, Olson J, Longstreth WT. Hypertension and cognitive function: pathophysiologic effects of hypertension on the brain. Curr Hypertens Rep. 2003;5:255–261. doi: 10.1007/s11906-003-0029-6. [DOI] [PubMed] [Google Scholar]
- 36.Awad N, Gagnon M, Messier C. The relationship between impaired glucose tolerance, type 2 diabetes, and cognitive function. J Clin Exp Neuropsychol. 2004;26:1044–1080. doi: 10.1080/13803390490514875. [DOI] [PubMed] [Google Scholar]
- 37.Gale CR, Deary IJ, Batty GD. Intelligence and carotid atherosclerosis in older people: cross-sectional study. J Am Geriatr Soc. 2008;56:769–771. doi: 10.1111/j.1532-5415.2008.01616.x. [DOI] [PubMed] [Google Scholar]
- 38.Bosma H, Schrijvers C, Mackenbach JP. Socioeconomic inequalities in mortality and importance of perceived control: cohort study. BMJ. 1999;319:1469–1470. doi: 10.1136/bmj.319.7223.1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Metcalfe C, Davey Smith G, Sterne JA, Heslop P, Macleod J, Hart CL. Cause-specific hospital admission and mortality among working men: association with socioeconomic circumstances in childhood and adult life, and the mediating role of daily stress. Eur J Public Health. 2005;15:238–244. doi: 10.1093/eurpub/cki063. [DOI] [PubMed] [Google Scholar]
- 40.Deary IJ, Der G, Ford G. Reaction times and intelligence differences: a population-based cohort study. Intelligence. 2001;29:389–399. [Google Scholar]
- 41.Black D, Morris J, Smith C, Townsend P. Inequalities in Health: Report of a Working Party. London: Department of Health and Social security; 1980. [Google Scholar]
- 42.Mackintosh N. IQ and Human Intelligence. Oxford: Oxford University Press; 1998. [Google Scholar]