Abstract
Gait modification offers a non-invasive option for offloading the medial compartment of the knee in patients with knee osteoarthritis. While gait modifications have been proposed based on their ability to reduce the external knee adduction moment, no gait pattern has been proven to reduce medial compartment contact force directly. This study used in vivo contact force data collected from a single subject with a force-measuring knee replacement to evaluate the effectiveness of two gait patterns at achieving this goal. The first was a “medial thrust” gait pattern that involved medializing the knee during stance phase, while the second was a “walking pole” gait pattern that involved using bilateral walking poles commonly used for hiking. Compared to the subject's normal gait pattern, medial thrust gait produced a 16% reduction and walking pole gait a 27% reduction in medial contact force over stance phase, both of which were statistically significant based on a two-tailed Mann-Whitney U-test. While medial thrust gait produced little change in lateral and total contact force over the stance phase, walking pole gait produced significant 11% and 21% reductions, respectively. Medial thrust gait may allow patients with knee osteoarthritis to reduce medial contact force using a normal-looking walking motion requiring no external equipment, while walking pole gait may allow patients with knee osteoarthritis or a knee replacement to reduce medial, lateral, and total contact force in situations where the use of walking poles is possible.
Keywords: Knee osteoarthritis, rehabilitation, gait retraining, biomechanics
INTRODUCTION
Articular cartilage overloading is believed to contribute to the development of medial compartment knee osteoarthritis (OA)1. Consequently, joint-sparing treatments are often aimed at reducing medial compartment contact force2. For example, high tibial osteotomy (HTO) surgery seeks to achieve this goal by correcting varus malalignment3. For some patients, the surgery results in decreased pain, improved function, and a decreased rate of disease progression3-5, supporting the hypothesis that reducing medial compartment contact force has disease modifying potential.
Gait modification may offer a non-invasive alternative for achieving the same goal. However, assessment of effectiveness is difficult since medial compartment contact force cannot be measured in vivo under normal circumstances. To address this limitation, researchers have identified the external knee adduction moment as a surrogate measure for medial compartment contact force6-8. The peak value of this moment during stance phase has been correlated with poorer outcomes following HTO surgery7,8 as well as with pain9,10, disease severity11, and the rate of disease progression12 in non-operated patients. Thus, if gait modification can reduce the peak knee adduction moment, it may provide one of the few conservative treatment options with disease modifying potential. Furthermore, it could fill an important treatment “hole” for patients in their 40's and 50's, who no longer achieve sufficient pain relief through pharmacological means and yet want to delay a total knee replacement.
A variety of gait patterns have been investigated based on their potential to reduce the external knee adduction moment. These include toeing out6,8,13, walking more slowly or with decreased stride length8,14, walking with increased medial-lateral trunk sway15,16, using lateral heel wedges9,17, walking with a cane2, or walking with medialized knees (i.e., “medial thrust” gait)18-21. Medial thrust gait is advantageous since it maintains a patient's normal walking speed, does not require special shoes or inserts, and utilizes a walking motion that looks “normal” to the casual observer. Similar to walking with a cane, walking with hiking poles may also be advantageous by providing a stabilizing moment in the frontal plane. While the external knee adduction moment is highly correlated with medial compartment contact force22, the ultimate test for any gait pattern is to demonstrate experimentally that it reduces medial compartment contact force directly.
This study evaluates the ability of two gait patterns to reduce medial compartment contact force in the knee. The two patterns investigated were a “medial thrust” gait involving knee medialization during stance phase18-20 and a “walking pole” gait involving bilateral walking poles commonly used by hikers23. The effectiveness of both gait patterns was evaluated using internal contact force data collected from a single patient with a force-measuring knee replacement. Since walking poles provide external force inputs, we hypothesized that walking pole gait would be more effective than medial thrust gait at reducing medial compartment contact force. We also hypothesized that both gait patterns would produce the largest reductions in medial compartment contact force near 25% and 75% of stance phase, the locations of peak contact force.
METHODS
One patient with a force-measuring knee replacement (male, right knee, age 83, mass 68 kg, height 1.7 m, body mass index 23.5, implanted contralateral knee) performed overground gait with simultaneous collection of internal knee contact force and external ground reaction force data. The patient was tested 3½ years after implantation for primary knee osteoarthritis. Institutional review board approval was obtained, and the subject provided informed consent. The patient's implant utilized a custom tibial prosthesis instrumented with four uniaxial force transducers, a microtransmitter, and an antenna, where the transducers measured compressive force at the four corners of the tibial tray24.
The subject performed five trials for each of three different gait patterns (normal, medial thrust, and walking pole; Fig. 1) at his self-selected walking speed of 1.23 m/s. The subject was given approximately 10 minutes of verbal instruction and training to learn each of the modified gait patterns. For medial thrust gait, he was instructed to bring his stance leg knee toward the midline of his body by increasing his knee flexion slightly19,20 and internally rotating his hip slightly18. The goal was to reduce the moment arm of the ground reaction force vector about the knee center. For walking pole gait, the subject used two Leki Makalu Tour walking poles with rubber tips (LEKI Lenhart GmbH, Kirchheim, Germany). Pole height was adjusted based on the manufacturer's recommendations, and the subject was instructed to place the contralateral pole on the ground opposite his stance leg heel at the instant of heel strike.
Figure 1.
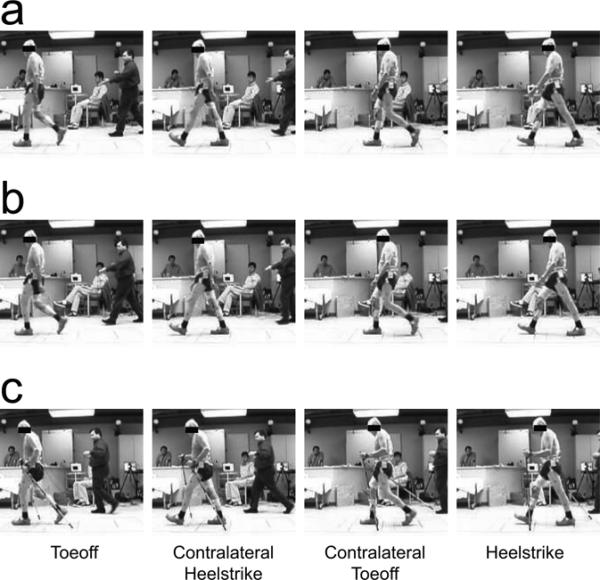
Photos of ground contact events for the subject performing (a) normal gait, (b) medial thrust gait, and (c) walking pole gait.
The effectiveness of medial thrust and walking pole gait was evaluated by comparing medial, lateral, and total tibial contact forces with those generated by the patient's normal gait pattern. For each trial, stance phase was identified using the time frames for which the vertical ground reaction force was non-zero. Force transducer data from the instrumented implant were converted into medial, lateral, and total contact force data using a previously validated regression equation developed for the same patient and instrumented implant25. Tibial contact force changes were quantified at 25%, 50%, and 75% of stance phase and for the mean value over all of stance phase (i.e., 0 to 100%). These locations were selected since no clear peaks existed in some of the contact force data, making it impossible to analyze changes in peak values, and since peaks and troughs in contact force normally occur near 25%, 50%, and 75% of stance phase. Medial, lateral, and total contact force changes between the three gait patterns were analyzed using a two-tailed non-parametric Mann-Whitney U-test with the level of significance set at 0.05. Changes in speed, cadence, and average vertical ground reaction force were also analyzed statistically to investigate whether changes in medial contact force could be attributed to these sources.
RESULTS
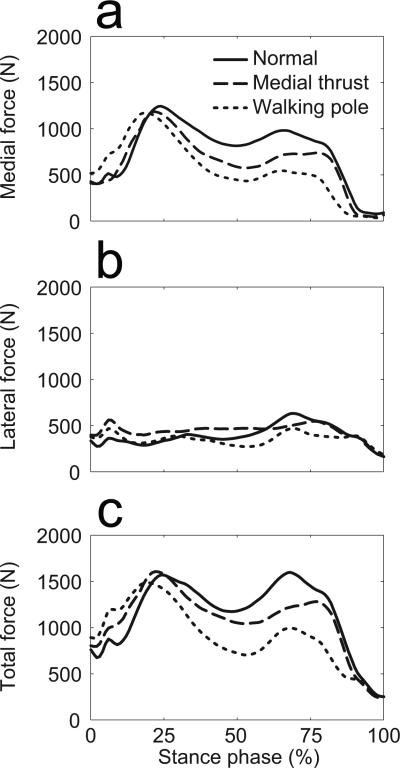
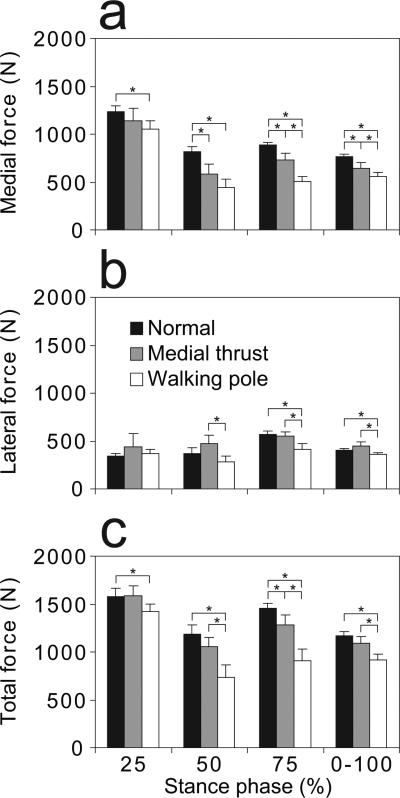
Medial thrust gait and walking pole gait both produced significant reductions in medial tibial contact force during stance phase, with walking pole gait being the most effective (Figs. 2a and 3a; Table 1). For both gait patterns, most quantified changes in medial contact force were statistically significant. Relative to normal gait, medial thrust gait reduced medial tibial contact force between 7% (90 N) and 28% (229 N) at various points during stance phase, while walking pole gait produced reductions of between 15% (181 N) and 45% (369 N). The largest reductions occurred during mid and late stance with little reduction occurring in the first peak during early stance. Walking speed and cadence were not significantly different between the three gait patterns, while the average vertical ground reaction force over stance phase was not significantly different between normal and medial thrust gait, but was different between normal and walking pole gait.
Figure 2.
Mean curves for (a) medial, (b) lateral, and (c) total knee contact force during stance phase from five trials each of normal gait (solid line), medial thrust gait (dashed line), and walking pole gait (dotted line).
Figure 3.
Mean and standard deviation of (a) medial, (b) lateral, and (c) total knee contact force at 25%, 50%, 75% and 0 through 100% of stance phase from five trials each of normal gait (black bars), medial thrust gait (grey bars), and walking pole gait (white bars). Stars (*) indicate significant differences (p < 0.05).
Table 1.
Mean changes in medial contact force between the three gait patterns. Stars (*) indicate significant differences (p < 0.05).
| Gait Cycle | Normal to Medial Thrust |
Normal to Walking Pole |
Medial Thrust to Walking Pole |
|||
|---|---|---|---|---|---|---|
| Relative (%) | Absolute (N) | Relative (%) | Absolute (N) | Relative (%) | Absolute (N) | |
| 25% | −7 | −90 | −15* | −181* | −8 | −91 |
| 50% | −28* | −229* | −45* | −369* | −24 | −140 |
| 75% | −17* | −155* | −43* | −384* | −31* | −229* |
| 0−100% | −16* | −122* | −27* | −205* | −13* | −83* |
In contrast, only walking pole gait produced significant reductions in lateral tibial contact force over stance phase (Figs. 2b and 3b; Table 2). Though medial thrust gait produced no significant changes in lateral tibial contact force relative to normal gait, there was a trend toward an increase of between 11% (45 N) and 29% (100 N), with a small decrease at 75% of stance phase. When walking pole gait was compared to the other two gait patterns, most quantified lateral contact force changes were significant except at 25% of stance phase. Relative to normal gait, walking pole gait reduced lateral tibial contact force between 11% (44 N) and 29% (163 N), with a small increase at 25% of stance phase.
Table 2.
Mean changes in lateral contact force between the three gait patterns. Stars (*) indicate significant differences (p < 0.05).
| Gait Cycle | Normal to Medial Thrust |
Normal to Walking Pole |
Medial Thrust to Walking Pole |
|||
|---|---|---|---|---|---|---|
| Relative (%) | Absolute (N) | Relative (%) | Absolute (N) | Relative (%) | Absolute (N) | |
| 25% | 29 | 98 | 8 | 26 | −17 | −72 |
| 50% | 27 | 100 | −24 | −88 | −40* | −188* |
| 75% | −4 | −23 | −29* | −163* | −26* | −140* |
| 0−100% | 11 | 45 | −11* | −44* | −20* | −88* |
In a similar manner, walking pole gait, but not medial thrust gait, produced significant reductions in total tibial contact force over stance phase (Figs. 2c and 3c; Table 3). Medial thrust gait produced no significant changes in total contact force relative to normal gait except at 75% of stance phase, with a trend toward decreased total contact force of between 7% (77 N) and 12% (177 N). In contrast, walking pole gait produced significant changes in nearly all total contact force quantities relative to the other two gait patterns. Reductions relative to normal gait were between 10% (155 N) and 39% (457 N).
Table 3.
Mean changes in total contact force between the three gait patterns. Stars (*) indicate significant differences (p < 0.05).
| Gait Cycle | Normal to Medial Thrust |
Normal to Walking Pole |
Medial Thrust to Walking Pole |
|||
|---|---|---|---|---|---|---|
| Relative (%) | Absolute (N) | Relative (%) | Absolute (N) | Relative (%) | Absolute (N) | |
| 25% | 1 | 8 | −10* | −155* | −10 | −163 |
| 50% | −11 | −129 | −39* | −457* | −31* | −328* |
| 75% | −12* | −177* | −38* | −547* | −29* | −369* |
| 0−100% | −7 | −77 | −21* | −248* | −16* | −172* |
DISCUSSION
This study investigated the effectiveness of two gait patterns for reducing medial compartment contact force in the knee. Both gait patterns produced significant reductions throughout stance phase, though walking pole gait was the most effective, and reductions in the first peak were limited. Since the subject trained with each modified gait pattern for only 10 minutes before testing, larger reductions in the first peak in particular might have been achieved with further habituation. Most quantified changes relative to normal gait were statistically significant, and their magnitudes suggest that they may be clinically significant as well.
Possible explanations exist for the reduced medial contact force achieved by both modified gait patterns. For medial thrust gait, the reduction was not due to placing an increased load on the contralateral leg, as no change in average vertical ground reaction force was observed between normal and medial thrust gait. The trend toward increased lateral contact force suggests that medial thrust gait shifted a portion of the medial contact force to the lateral compartment, similar to what one would expect from HTO surgery. This shift was achieved without an increase in total contact force, which could have occurred if muscle co-contraction had increased. Instead, a trend toward decreased total contact force was observed. Thus, medial thrust gait appears to shift a portion of the contact load to the lateral compartment while simultaneously decreasing total contact force slightly, possibly due to a more favorable geometric configuration of the leg or reduced muscle co-contraction. Whether or not the increase in lateral contact force would be detrimental to the lateral compartment articular cartilage requires further investigation, but the effect is likely to be comparable to that of HTO surgery.
For walking pole gait, the most likely explanation for reduced medial contact force is that some of the ground reaction force was transferred through the contralateral walking pole. This explanation is supported by a reduction in average vertical ground reaction force for walking pole gait compared to normal gait23. This ground reaction force reduction translated into significant medial (27%, 205 N) and lateral (11%, 44 N) contact force reductions over stance phase. The fact that the largest reduction occurred in the medial compartment is likely due to the contralateral walking pole counteracting the external knee adduction moment. These observations suggest that walking poles offload both compartments of the tibiofemoral joint via two mechanisms: 1) bearing a portion of the external axial force, and 2) bearing a portion of the external adduction moment.
Despite good overall reduction in medial contact force, both modified gait patterns were relatively ineffective at reducing the first peak in medial contact force near 25% of stance phase. It is not known whether medial thrust and walking pole gait could be modified so as to achieve significant medial contact force reductions at this point as well. Medial thrust gait was originally designed using a patient-specific computational model that predicted gait alterations to minimize the external knee adduction moment19,20. If internal knee contact force data from the present subject could be accurately fitted as a function of the subject's external knee loads (three forces and three torques) calculated from inverse dynamics, then a similar computational approach could be used to predict further gait refinements to minimize medial contact force directly. Applying a similar computational methodology to walking pole gait would be difficult without having contact force measurements between the walking poles and the floor. Conceptually, placing the contralateral walking pole on the ground slightly before heel strike may increase knee offloading during early stance phase, though the resulting phase shift in arm motion may be difficult to achieve from a coordination perspective.
The large percent changes in lateral contact force produced by medial thrust gait and walking pole gait need to be interpreted in light of the corresponding absolute changes. The largest changes in lateral contact force were a 29% increase due to medial thrust gait (25% of stance phase) and a 29% decrease due to walking pole gait (75% of stance phase). These percent changes correspond to absolute changes of 98 N and 163 N, respectively. At the same points during stance phase, medial thrust gait decreased medial contact force by 7% (90 N), while walking pole gait decreased it by 15% (181 N) – much smaller values percent-wise, but comparable values on an absolute scale. Thus, since medial contact forces were significantly larger than lateral contact forces, large percent changes in lateral contact force correspond to much smaller percent changes in medial contact force.
The primarily limitation of this study is the use of only a single subject with a force-measuring knee replacement. To date, only four patients in the United States have been implanted for force-measuring knee replacements. Thus, the opportunity to obtain in vivo knee contact force data for different gait patterns is highly limited. Use of a subject with a total knee replacement is also a limitation, as the subject's normal, medial thrust, and walking pole gait patterns may differ from those of subjects with healthy natural knees. We have compared our subject's ground reaction force curves with data from normal subjects reported in the literature26 and found good agreement. Our subject's self-selected walking speed was also within the range observed for normal subjects27. Furthermore, the subject's gait pattern appeared visually “normal,” which is not always the case for older subjects with a joint replacement. Based on these observations, it is unlikely that our subject's normal gait pattern was highly aberrant. Though further investigation with additional instrumented knee patients is needed to determine the extent to which these results can be generalized, this study is the first to validate clinically promising gait patterns using in vivo tibial contact force data.
Another limitation of this study is that the external knee adduction moment was not calculated to examine its ability to predict the measured changes in medial contact force. A recent study reported that one's interpretation of the effectiveness of a gait modification at reducing the external knee adduction moment is highly dependent on how the knee adduction moment is calculated28. Researchers have used different reference frames (i.e., the laboratory, the tibia, the femur, and a floating reference frame) and different directions within those reference frames to calculate the knee adduction moment, with different methods yielding different results. Which calculation method (if any) yields knee adduction moment results that accurately predict changes in medial contact force produced by different gait patterns is unknown.
An important issue for clinical implementation of medial thrust gait is whether knee OA patients can both achieve and maintain this gait pattern. An advantage of medial thrust gait compared to other gait modifications is that it looks natural to the naked eye. Since no external devices are required, it also has the advantage of being usable anywhere and at any time. These characteristics make it a good contender for clinical implementation. However, it is unknown how quickly and easily knee OA patients can achieve a medial thrust gait pattern, and consequently, whether they can ingrain it so that it becomes second nature. These issues are the topic of ongoing investigation. A previous study used gait retraining to treat hip dysplasia, and those subjects maintained their modified gait pattern for at least a year following the end of retraining29. Athletes are successful at learning new ways of running, kicking, jumping, and throwing so as to improve athletic performance. These movement modifications must become second nature to be useful during competition. Thus, it is reasonable to believe that at least some patients with knee OA would be motivated enough to learn and ingrain a modified gait pattern if it provided significant pain relief.
In summary, this study used in vivo contact force measurements from an instrumented knee implant to investigate the effectiveness of two gait patterns for reducing medial compartment contact force in the knee. Both the medial thrust gait pattern and the walking pole gait pattern produced statistically, and possibly clinically, significant reductions in medial compartment contact force throughout stance phase, though reductions in the first peak near 25% of stance phase were the smallest. The walking pole gait pattern also produced significant reductions in lateral compartment contact force. For individuals with total knee replacements, use of walking poles may significantly reduce the development of wear, while for individuals with medial compartment knee osteoarthritis, use of medial thrust gait or walking poles may minimize further damage to the articular surfaces.
Acknowledgments
This work was supported by an NSF CAREER award and by NIH National Center for Medical Rehabilitation Research grant 1R21HD053490 to B.J. Fregly, by the Shiley Center for Orthopaedic Research & Education at Scripps Clinic in La Jolla, CA, and by the University of Florida.
REFERENCES
- 1.Maly MR. Abnormal and cumulative loading in knee osteoarthritis. Current Opinions in Rheumatology. 2008;20:547–552. doi: 10.1097/BOR.0b013e328307f58c. [DOI] [PubMed] [Google Scholar]
- 2.Kemp G, Crossley KM, Wrigley TV, Metcalf BR, Hinman RS. Reducing joint loading in medial knee osteoarthritis: shoes and canes. Arthritis & Rheumatism. 2008;59:609–614. doi: 10.1002/art.23578. [DOI] [PubMed] [Google Scholar]
- 3.Briem K, Ramsey DK, Newcomb W, Rudolph KS, Snyder-Mackler L. Effects of the amount of valgus correction for medial compartment knee osteoarthritis on clinical outcome, knee kinetics and muscle co-contraction after opening wedge high tibial osteotomy. Journal of Orthopaedic Research. 2007;25:311–318. doi: 10.1002/jor.20326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Habata T, Uematsu K, Hattori K, Kasanami R, Takakura Y, Fujisawa Y. High tibial osteotomy that does not cause recurrence of varus deformity for medial gonarthrosis. Knee Surgery, Sports, Traumatoloy, and Arthroscopy. 2006;14:962–967. doi: 10.1007/s00167-006-0077-y. [DOI] [PubMed] [Google Scholar]
- 5.Majima T, Yasuda K, Katsuragi R, Kaneda K. Progression of joint arthrosis 10 to 15 years after high tibial osteotomy. Clinical Orthopaedics and Related Research. 2000:177–184. doi: 10.1097/00003086-200012000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Andriacchi TP. Dynamics of knee malalignment. Orthopedic Clinics of North America. 1994;25:395–403. [PubMed] [Google Scholar]
- 7.Prodromos CC, Andriacchi TP, Galante JO. A relationship between gait and clinical changes following high tibial osteotomy. Journal of Bone and Joint Surgery. 1985;67A:1188–1194. [PubMed] [Google Scholar]
- 8.Wang JW, Kuo KN, Andriacchi TP, Galante JO. The influence of walking mechanics and time on the results of proximal tibial osteotomy. Journal of Bone and Joint Surgery. 1990;72A:905–909. [PubMed] [Google Scholar]
- 9.Hinman RS, Payne C, Metcalf BR, Wrigley TV, Bennell KL. Lateral wedges in knee osteoarthritis: what are their immediate clinical and biomechanical effects and can these predict a three-month clinical outcome? Arthritis & Rheumatism. 2008;59:408–415. doi: 10.1002/art.23326. [DOI] [PubMed] [Google Scholar]
- 10.Thorp LE, Sumner DR, Wimmer MA, Block JA. Relationship between pain and medial knee joint loading in mild radiographic knee osteoarthritis. Arthritis & Rheumatism. 2007;57:1254–1260. doi: 10.1002/art.22991. [DOI] [PubMed] [Google Scholar]
- 11.Sharma L, Hurwitz DE, Thonar EJ-MA, Sum JA, Lenz ME, Dunlop DD, Schnitzer TJ, Kirwan-Mellis G, Andriacchi TP. Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis & Rheumatism. 1998;41:1233–1240. doi: 10.1002/1529-0131(199807)41:7<1233::AID-ART14>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 12.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Annals of the Rheumatic Diseases. 2002;61:617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guo M, Axe MJ, Manal K. The Influence of foot progression angle on the knee adduction moment during walking and stair climbing in pain free individuals with knee osteoarthritis. Gait and Posture. 2007;26:436–441. doi: 10.1016/j.gaitpost.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 14.Mündermann A, Dyrby CO, Hurwitz DE, Sharma L, Andriacchi TP. Potential strategies to reduce medial compartment loading in patients with knee osteoarthritis of varying severity. Arthritis & Rheumatism. 2004;50:1172–1178. doi: 10.1002/art.20132. [DOI] [PubMed] [Google Scholar]
- 15.Mündermann A, Asay JL, Mündermann L, Andriacchi TP. Implications of increased medio-lateral trunk sway for ambulatory mechanics. Journal of Biomechanics. 2008;41:165–170. doi: 10.1016/j.jbiomech.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 16.Hunt MA, Birmingham TB, Bryant D, Jones I, Giffin JR, Jenkyn TR, Vandervoort AA. Lateral trunk lean explains variation in dynamic knee joint load in patients with medial compartment knee osteoarthritis. Osteoarthritis and Cartilage. 2008;16:591–599. doi: 10.1016/j.joca.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 17.Kakihana W, Akai M, Nakazawa K, Takashima T, Naito K, Torii S. Effects of laterally wedged insoles on knee and subtalar joint moments. Archives of Physical Medicine and Rehabilitation. 2005;86:1465–1471. doi: 10.1016/j.apmr.2004.09.033. [DOI] [PubMed] [Google Scholar]
- 18.Barrios JA, Davis IS. A gait modification to reduce the external knee adduction moment at the knee: a case study.. Proceedings of the 31st Annual Meeting of the American Society of Biomechanics.; Stanford, CA. 2007. paper #219. [Google Scholar]
- 19.Fregly BJ, Reinbolt JA, Rooney KL, Mitchell KH, Chmielewski TL. Design of patient-specific gait modifications for knee osteoarthritis rehabilitation. IEEE Transactions on Biomedical Engineering. 2007;54:1687–1695. doi: 10.1109/TBME.2007.891934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fregly BJ, Rooney KL, Reinbolt JA. Predicted gait modifications to reduce the peak knee adduction torque.. Proceedings of the XXth Congress of the International Society of Biomechanics.; Cleveland, OH. 2005. p. 283. [Google Scholar]
- 21.Fregly BJ. Computational assessment of combinations of gait modifications for knee osteoarthritis rehabilitation. IEEE Transactions on Biomedical Engineering. 2008;55:2104–2106. doi: 10.1109/TBME.2008.921171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao D, Banks SA, Mitchell KH, D'Lima DD, Colwell CW, Fregly BJ. Correlation between the knee adduction torque and medial contact force for a variety of gait patterns. Journal of Orthopaedic Research. 2007;25:789–797. doi: 10.1002/jor.20379. [DOI] [PubMed] [Google Scholar]
- 23.Willson J, Torry MR, Decker MJ, Kernozek T, Steadman JR. Effects of walking poles on lower extremity gait mechanics. Medicine and Science in Sports and Exercise. 2001;33:142–147. doi: 10.1097/00005768-200101000-00021. [DOI] [PubMed] [Google Scholar]
- 24.D'Lima DD, Townsend CP, Arms SW, Morris BA, Colwell CWJ. An implantable telemetry device to measure intra-articular tibial forces. Journal of Biomechanics. 2005;38:299–304. doi: 10.1016/j.jbiomech.2004.02.011. [DOI] [PubMed] [Google Scholar]
- 25.Zhao D, Banks SA, D'Lima DD, Colwell CW, Fregly BJ. In vivo medial and lateral tibial loads during dynamic and high flexion activities. Journal of Orthopaedic Research. 2007;25:593–602. doi: 10.1002/jor.20362. [DOI] [PubMed] [Google Scholar]
- 26.Chao EY, Laughman RK, Schneider E, Stauffer RN. Normative data of knee joint motion and ground reaction forces in adult level walking. Journal of Biomechanics. 1983;16:219–233. doi: 10.1016/0021-9290(83)90129-x. [DOI] [PubMed] [Google Scholar]
- 27.Andriacchi TP, Galante JO, Fermier RW. The influence of total knee-replacement design on walking and stair-climbing. Journal of Bone and Joint Surgery. 1982;64A:1328–1335. [PubMed] [Google Scholar]
- 28.Schache AG, Fregly BJ, Crossley KM, Hinman RS, Pandy MG. The effect of gait modification on the external knee adductor moment is reference frame dependent. Clinical Biomechanics. 2008;23:601–608. doi: 10.1016/j.clinbiomech.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 29.Schröter J, Güth V, Overbeck M, Rosenbaum D, Winkelmann W. The ‘Entlastungsgang’. A hip unloading gait as a new conservative therapy for hip pain in the adult. Gait and Posture. 1999;9:151–157. doi: 10.1016/s0966-6362(99)00007-7. [DOI] [PubMed] [Google Scholar]