Abstract
Walking Forward is a community-based participatory research program in western South Dakota funded by the National Cancer Institute (NCI). The primary goal of this initiative is to address the high and ominously increasing cancer mortality rates among American Indians by facilitating access to innovative clinical trials, behavioral and genetic research and tailored patient navigation. The critical outcomes include: an unprecedented accrual rate of 25 percent in clinical trials, including cancer treatment and cancer control trials; a significant reduction in the number of missed treatment days among navigated American Indian cancer patients undergoing radiation therapy; and most importantly, establishment of trusting partnerships with the American Indian communities as reflected in enrollment in a genetic study involving the ataxia telangiectasia mutated gene. The results indicate that the Walking Forward approach presents an effective strategy to overcome the barriers to cancer care in this underserved community.
Introduction
The Cancer Disparities Research Partnership (CDRP) program of the National Cancer Institute (NCI) seeks to reduce cancer disparities observed among underserved sections of United States population. American Indians bear a disproportionate burden of disease, injury, death, and disability.1 Although the cancer mortality among this population is lower as compared to other races, there are some significant regional differences.2 The cancer mortality rates for American Indians served by the Billings, Aberdeen and Bemidji Areas of the Indian Health Services (IHS), which include western South Dakota, are approximately 30 percent higher than that of the overall U.S. population.3 These disparities could be attributed to low rates of cancer screening,2 4–9 and higher likelihood of being diagnosed at advanced stages of disease.2,4,10–12 Furthermore, the interval between diagnosis and treatment is longer for American Indians,12–13 ensued by low five-year survival rates.4 In 2002, Rapid City Regional Hospital (RCRH) was awarded a CDRP grant to address cancer-related health disparities among America Indians in western South Dakota (Principal Investigator Daniel Petereit, MD). As a result, a community-based participatory program, regionally called the Walking Forward program, was developed and implemented.
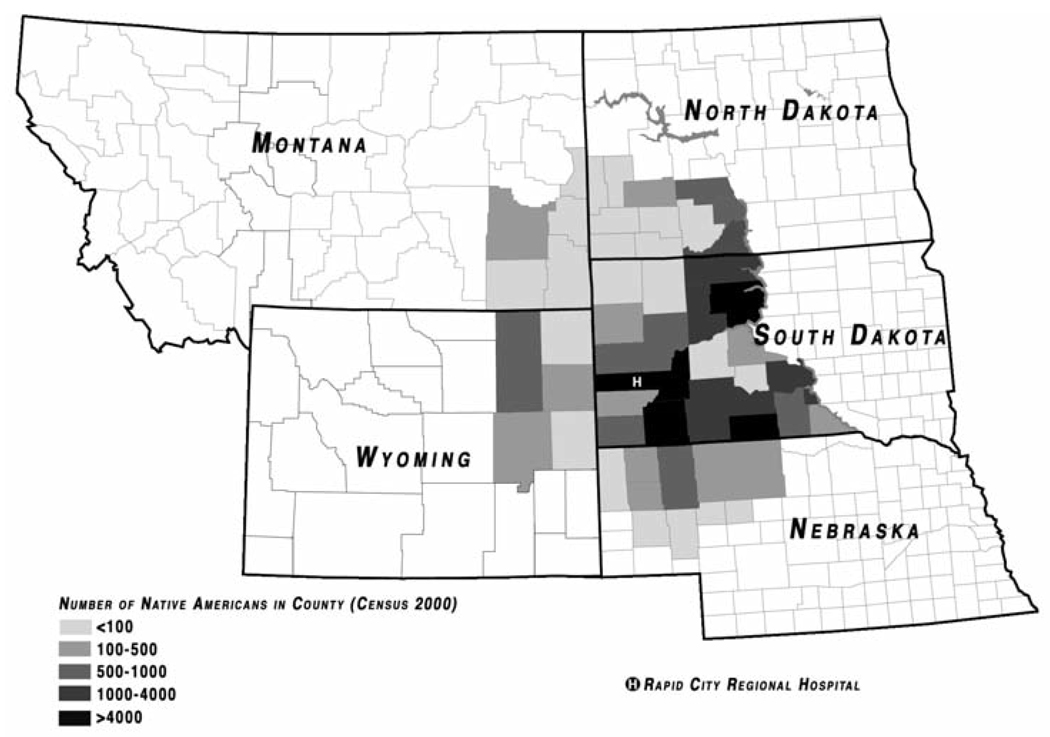
RCRH serves all of western South Dakota and parts of the adjacent states of Wyoming and Nebraska (Figure 1). Its service basin incorporates a geographic area of 250,000 square miles with a population base of 350,000. It is the sole secondary and tertiary oncology care provider to a large population (~60,000) of American Indians in this area. The Walking Forward program specifically serves the American Indian community members from the Cheyenne River Sioux Tribe, Rosebud Sioux Tribe and Oglala Sioux Tribe, as well as the urban American Indians living in and around Rapid City.
Figure 1.
American Indian population, by county for the region using Rapid City Regional Hospital’s John T Vucurevich Cancer Care Institute {Rapid City, SD(H)}. Reprinted with permission. ©2008 American Society of Clinical Oncology. All rights reserved.10
A primary goal of the Walking Forward program is to enroll American Indians in cancer treatment clinical trials to ultimately decrease cancer mortality rates. This was primarily achieved by: a) identifying the barriers to cancer care; b) implementing an effective patient navigation program; c) enhanced recruitment of cancer patients into clinical trials; and d) conducting translational research, including genetic studies.
All activities undertaken as a part of the Walking Forward program were approved by the RCRH and Aberdeen Area IHS Institutional Review Boards (IRB) prior to initiation of the study. As a requirement for IRB approval, the Aberdeen Area IHS IRB also required tribal council approvals from all three participating tribes and their respective IHS Hospital chief executive officers, as well as from the Rapid City Sioux San IHS Hospital that serves the urban American Indian community in Rapid City. Additionally, the genetic study involving the ataxia telangiectasia mutated gene was also approved by the University of Wisconsin IRB. Informed consent was obtained from all participants prior to collecting any data. This article describes the Walking Forward program and its outcomes.
Implementation and Outcomes
Identifying Barriers to Health Care: Results from a Survey among Community Members and Cancer Patients
Factors contributing to health care disparities are complex and include patient-, physician- or system-related barriers. To identify the barriers to timely cancer diagnosis and treatment, community and cancer patient surveys were developed through a collaborative process employing a community-based participatory research (CBPR) method-ology.14 Survey development progressed through an iterative process with critical input from community members and was designed to understand cancer-related behavior and barriers to cancer care in this population. The community survey was implemented among 984 American Indians in the target communities, while the cancer patient survey was implemented prospectively among 165 newly diagnosed cancer patients at RCRH’s Cancer Care Institute (CCI), of which 52 were American Indians.
A significant proportion (47 percent) of the respondents to the community survey identified lack of transportation as one of the most common barriers to accessing care. Given that most of the American Indian communities reside in rural locations, distance and transportation present significant barriers to accessing specialized health care such as that provided at the RCRH CCI. For example, 75 percent of respondents reported traveling more than 50 miles for tertiary medical care. American Indians seeking cancer treatment at RCRH travel an average of 140 miles one way. Other related barriers also include cost of transportation, food and lodging. While 75 percent of the respondents reported traveling less than 25 miles to access primary care, the quality of primary care is compromised due to staffing shortages. IHS clinics in rural areas find recruiting providers challenging and are chronically short-staffed,15 which negatively impacts the delivery of quality primary care,16 thus instilling dissatisfaction.
The respondents of the community survey also identified lack of satisfaction in interactions with medical providers and a lack of confidence in their abilities as additional barriers to care. The cancer patient survey utilized a novel scale for medical mistrust and satisfaction with health care.17 American Indian cancer patients exhibited a significantly higher mistrust (p=.0001) and lower satisfaction (p=.0001) with health care than Whites.
Additional barriers specific to accessing cancer-related health care, including cancer screening, were identified through both surveys. Overall, only 43 percent of participants reported ever having had any cancer screening tests. Analysis of cancer-specific screening rates showed the following percentages: cervical 48 percent (n=596), breast 59 percent (n=369), prostate 34 percent (n=115), and colorectal 20 percent (n=56). These rates are significantly lower than the published rates for not only U.S. non-Hispanic Whites, but also for American Indians, specifically the Northern Plains American Indian population.2 Importantly, 87 percent responded “no” when asked whether their doctor or nurse had ever recommended a cancer screening test. Furthermore, the cancer patient survey revealed that American Indian cancer patients presented with higher rates of advanced-stage disease for screen detectable cancers, consistent with results from other similar studies in American Indians.2,4,18 Possible reasons for low screening rates could be lower health literacy and lack of encouragement for cancer screening by health professionals and other access barriers, including lack of transportation, that present challenges in these communities.19 These findings underscore the need for a targeted cancer education and intervention program.
Patient Navigation: A Model for Success in American Indian Communities
Patient Navigation is an emerging and promising concept to enhance health care. As discussed in the previous section, the Walking Forward program identified key barriers to cancer care in the American Indian community. A process map for patient navigation was developed to overcome the identified barriers and build trust within the community. Although this model shared similar characteristics to the one developed by Dr. Harold Freeman, Director of the Center to Reduce Cancer Health Disparities, our model was tailored to meet the needs of our population.
A core feature of the Walking Forward navigation program is ensuring cultural competency of the navigators. The process of achieving cultural competence for the Walking Forward staff has been previously described.20 Establishing local community representation, as well as employing hospital- based navigators with ties to the communities, has contributed to the success of this program. Cultural competence of the patient navigators fostered the establishment of a partnership based on trust between Walking Forward staff and American Indian communities, including tribal administration. Lack of trust for research in American Indian communities, especially with genetic studies, is well documented.21,22 This breeds a culture of resistance to research and is a barrier to receiving health care and to participation in clinical trials. Adapting care and patient/family health care education with culturally sensitive staff who can communicate in Native languages are important steps to delivering higher quality care and a more satisfying, less threatening health care experience.
The Walking Forward patient navigation program includes services for cancer patients and a community outreach component. Cancer patients are assisted by hospital-based patient navigators to overcome barriers and facilitate cancer-related care and follow-up assessment. Additionally, the patient navigators assist with financial, social and emotional support to these patients. The community research representatives (CRR), based in their respective communities, facilitate an education and outreach component. These CRRs promote early detection through screening and raise awareness of the clinical trials by implementing culturally relevant education modules. The success of the Walking Forward patient navigation program is demonstrated in increased patient enrollment in clinical trials and increased adherence to the prescribed cancer treatment regimen.
A retrospective analysis determined that Walking Forward-navigated patients undergoing radiation therapy had better completion rates compared to non-navigated patients. For patients who receive potentially curative chemotherapy and radiation for cervical and head and neck cancers, each day of treatment prolongation increases the risk of a recurrence by 1 percent. For example, if a patient with either one of the above malignancies delays the completion of radiation by 10 days, the chance for cure decreases by 10 percent.23 On average, navigated patients had a delay of 1.5 days versus 4.5 days (the equivalent of one week of treatment) for non- navigated patients.20 (Table 1) The ability to reduce treatment delays and increase completion rates is a critical measure of program efficacy.
Table 1.
Impact of Patient Navigation on Treatment Interruptions. (Reprinted with permission. ©2008 Association of Community Cancer Centers. All rights reserved.)
| Control Group (curative radiation/not navigated during treatment) |
74 | 4.45 | 1.132 | 4.855 | 0.002 |
| Experimental Group (curative radiation/ navigated during treatment) |
42 | 1.45 |
Participation of American Indians in Cancer Clinical Trials
The rationale for clinical trial participation includes the following: access to state-of-the-art therapy; safe and effective treatments that are closely monitored; and the potential for improved clinical outcomes, including quality of life. The rate of accrual in clinical trials among minority, rural and lower socioeconomic subpopulations is low in the U.S. and is approximately 1 percent.24–26 This could be a result of numerous barriers to accessing health care that could potentially exacerbate known cancer-related health disparities among underserved populations.27–29 The low participation rates among minorities also limit the treatment implications of data derived from clinical trials. RCRH CCI has access to clinical trials through several cooperative group mechanisms.
Since American Indians live an average of 140 miles from the cancer center in Rapid City, a hypothesis of the project was to determine if a shorter course of radiation could potentially address this barrier by using innovative technologies as part of a clinical trial. For example, Phase II trials using brachytherapy and intensity modulated radiotherapy (IMRT) were initiated for prostate and breast cancer. Earlier-stage breast cancer patients are eligible for breast brachytherapy where the treatment duration is decreased from six weeks to one week. Two methods of brachytherapy are used: the intracavity and interstitial approach. To date, 26 patients have been enrolled on this study, including four American Indians.
Early stage prostate cancer patients are offered a variety of radiation options, including brachytherapy (permanent seed implantation) or external beam radiation using IMRT via tomotherapy. The conventional number of external beam treatments is 38, in order to deliver a potentially tumoricidal dose of 76 Gy. A Phase II multi-institutional IMRT trial is open, where the number of treatments are decreased from 22 (2.94 Gy per fraction) to 16 (3.63 Gy) to 12 (4.3 Gy) by increasing the daily dose of radiation. These schedules were designed to give an equivalent dose of 76 Gy in 38 treatments. This trial has accrued 270 patients nationwide with 50 accrued in Rapid City. The current dose level is 3.63 Gy × 16 over four weeks. No significant toxicities have been encountered to date.
Two additional Phase II clinical trials were open for intermediate- and high-risk prostate cancer patients (non-metastatic). Intermediate patients are offered a short course of IMRT (2.2 Gy × 16), followed by a permanent seed implant boost. The rationale for this method of dose escalation is based upon emerging data demonstrating higher cure rates compared to conventional radiation.30 To date, six patients have been enrolled in this study. Finally, for the high-risk patients, the pelvic lymph nodes are treated to 56 Gy and the prostate is treated to 70 Gy in 28 fractions in order to decrease the overall treatment time from eight weeks to six weeks by using IMRT. So far, 18 patients have been enrolled on this study, of which eight are from Rapid City. No significant toxicities have been observed. The theme of these trials is to reduce the barrier of distance and time away from home while maintaining or improving the therapeutic window.
RCRH currently has approximately 69 active clinical trials, including trials for cancer control. RCRH received a CTOC (Clinical Trials Operating Committee) supplement grant from the NCI in September 2006. The goal was to increase patient recruitment (for both non-American Indian and American Indian) to clinical trials. This enabled RCRH to hire dedicated nursing staff and a research associate in an effort to expand current outreach programs for clinical trial accrual.
The clinical trial enrollment rate among all cancer patients presenting to CCI is about 7.4 percent. While this is still a relatively low percentage of all new patients evaluated, it is more than twofold higher than the rate of trial accrual reported nationally by other investigators.24,25 Furthermore, we have achieved a clinical treatment trial accrual incidence of 7 percent among new American Indian cancer patients. The rates of accrual to a race-specific non-treatment cancer control trial, the ATM gene mutation study (described below), is 18 percent, leading to a total enrollment rate of 25 percent among American Indians.31 This compares favorably with other studies that have reported American Indian trial participation rates of less than 1 percent.24,26,32,33
The reasons for non-participation in clinical trials are numerous. They include lack of availability of protocols for common cancer sites, restricted eligibility due to stringent inclusion criteria, patient medical co-morbidities and patient presentation with advanced stages of disease.31 These issues become acute among our large American Indian patient population, as they are more likely to present with advanced-stage disease and have multiple medical co-morbidities, thus making them ineligible for most available protocols.5,28,34 Similarly, protocol inclusion criteria restrictiveness has also been shown by other investigators to be a significant barrier to trial participation, especially among underrepresented populations.35 The cooperative groups sponsored by the NCI need to be cognizant of these factors when designing clinical trials and eligibility criteria. There is a great need to design trials for common disease sites which represent the majority of patients seen in a typical cancer center. By increasing trial eligibility, a greater percentage of the oncology population would benefit from advances in cancer treatment, similar to the pediatric oncology population.
Future Directions
Genetic Polymorphism in Ataxia Telangiectasia Mutated (ATM) Gene and Radiogenomics
Fractionated radiotherapy has an established role in the management of human cancer. However, loco-regional control rates, which ultimately influence overall cure rates, are limited by tumor radioresistance and normal tissue tolerance.36 Individual variability in normal tissue response to fractionated radiotherapy has been observed in both clinical and laboratory studies.37–39
The American Indian patient population in western South Dakota appears to be more sensitive to the effects of radiation therapy. In a retrospective analysis of 61 American Indians undergoing definitive radiotherapy at RCRH CCI, 50 percent of patients experienced G2 (grade 2 toxicities), and 17 percent experienced G3 (grade 3 toxicities). The majority of these toxicities were skin reactions in patients with breast and colorectal cancer.11,40 This is manifested as more severe than expected skin reactions ranging from a mild skin erythema to a patchy moist desquamation with moderate edema and eventually progressing to a confluent moist desquamation. Fear of this treatment-related side effect could potentially contribute to the commonly observed treatment delays observed in this patient population. In an analysis from RCRH, 28 percent had delays greater than six or more days, and 15 percent had delays of greater than 11 days, which could lead to compromised tumor control.40,41
Genetic polymorphism in DNA repair genes has been indicated in modulating the clinical response to radiotherapy and influence normal tissue tolerance during radiation therapy. We are currently studying the ataxia telangiecta-sia mutated gene (ATM) in the American Indian population for any known or new polymorphism that may predispose them to such toxicities. ATM is an important cell cycle checkpoint kinase. Thus, it functions as a regulator of a wide variety of downstream proteins, including tumor suppressor proteins such as p53 and BRCA1. Homozygosity of mutations in ATM leads to extreme hypersensitivity to radiation,42,43 while heterozygosity may be associated with an increased risk for developing cancer and radiation induced toxicities.44 Studying the ATM gene in American Indians will provide a better understanding of the underlying molecular mechanism for the observed higher incidence of toxicities in this population. To date, 59 American Indians and 52 non-American Indians have participated in the ATM study. Variants were identified in 18 of 62 sequenced exons. Once a total of 200 patients have undergone gene sequencing, radiation toxicities will be correlated to ATM polymorphisms.45
As an extension of the ATM study, we will also investigate the genetic risk profiles of individuals by identifying genes through DNA microarrays that might predict response to treatment and ultimately guide therapy. Several retrospective studies have demonstrated that fibroblasts derived from patients with unusually sensitive skin responses are radiosensitive in vitro. Patients’ survival parameters have been measured in dermal fibroblast derived from patients that exhibited severe acute or late effects associated with radiation therapy to determine whether the radiation response in vitro correlated with the clinical normal tissue reactions.42,43,46 In addition, an association of radiation sensitivity of fibroblasts and genetic variants in DNA-damage response genes has been shown.47 Similarly, use of gene expression analysis to evaluate the response of lymphocytes to irradiation was investigated.48 The results indicate that lymphocyte is a valid system to identify genetic responses to radiation that could be predictive of adverse responses in vivo. We will be investigating a similar expression pattern by conducting a match-pair analysis for American Indians who did and did not develop significant radiation complications. The ultimate goal is to identify markers that could be used to identify patients that might have an adverse response prior to treatment and to determine whether the causes of susceptibility of American Indians and other populations are similar or different. Such tailored treatment can potentially result in better local control and survival rates. For example, if a patient with prostate cancer has a genetic profile that would predict for developing a significant radiation complication, he would probably be better served by a radical prostatectomy, rather than external beam irradiation – particularly a treatment schedule where larger doses of radiation are given. A similar scenario would unfold for a woman with breast cancer who is contemplating whether or not to have a mastectomy. In both cases, brachytherapy might be a reasonable option if surgery was declined.
Increasing Cancer Screening Rate among American Indians
A review of the RCRH tumor registry (1990–2000) reveals that a higher percentage of American Indians present with Stage III–IV breast, colorectal, prostate, cervical or lung cancer, compared to the non-American Indian population.11,40 (Table 2) This disparity persists as indicated in a prospective survey of newly diagnosed cancer patients at RCRH.14 This could be attributed to the low screening rates in this population. The Walking Forward Program has received supplemental funding from the NCI to provide cancer education in American Indian communities, with the goal of increasing screening rates for screen-detectable cancers. We have developed culturally responsive cancer education modules in collaboration with Dr. Linda Burhansstipanov from Native American Cancer Research. These will be implemented in all four Walking Forward communities. As a result of increasing screening rates and detecting cancer earlier, stage migration should result, i.e. presentation at earlier stages of disease. This should ultimately lead to increased treatment options and better outcomes for the patients.
Table 2.
Cancer Stage at Presentation at RCRH Among American Indians. (Reprinted with permission. © 2008 American Society of Clinical Oncology. All rights reserved.10)
| Site | Stage III & IV American Indian |
Stage III & IV White |
|---|---|---|
| Lung | 72% (92/127) | 68% (669/989) |
| Breast | 16% (12/75) | 10% (111/1127) |
| Colorectal | 48% (26/54) | 40% (298/739) |
| Prostate | 44% (22/50) | 30% (281/945) |
| Cervix | 53% (8/15) | 26% (13/51) |
Next Steps
Enhancing the Patient Navigation Program
The existing Walking Forward patient navigation program utilizes a hospital-based patient navigator for delivery of services. While this approach has been very successful at working with cancer patients during their treatment within the hospital, we believe that a comprehensive model involving coordinated efforts of both hospital-based and community-based patient navigators offers the advantages of: (a) increased visibility and accessibility in the community; (b) the ability to provide assistance and problem solve on-site in the local clinics and IHS facilities; and (c) the ability to provide individual health care counseling and emotional support to patients through home visits and other personal connections. This comprehensive model is likely to be more effective by optimizing the specific services needed for each individual patient and will better address geographical distance and associated barriers to cancer treatment access. Such a system will potentially include both individual patient services and a community outreach component.
Providing Palliative Care
Palliative care relieves suffering and improves quality of life for cancer patients.49–52 Medical facilities in rural areas, such as IHS, often lack such specialized services due to challenges pertaining to environment, infrastructure and resources. In a survey of tribal health directors, 70 percent of the respondents indicated an urgent need for pain management, while 50 to 60 percent reported a need for advance care planning, traditional medicine, physical therapy and other indicators of palliative care.53 Several of the Walking Forward patients who live on reservations are in urgent need of palliative care. Such services are often available only in distant facilities like RCRH. Lack of transportation, large distances, little knowledge in the community about palliative care and lack of awareness among medical personnel are barriers to palliative care on rural reservations. Effective use of new technologies, such as telemedicine, can elude barriers of time and distance, thereby providing a more equitable healthcare distribution.54 We are currently in planning stages of leveraging existing telemedicine facilities to provide palliative care on the reservation. This will be a coordinated effort between the oncologists at RCRH, the Walking Forward staff, South Dakota State University’s College of Nursing and the Tribes.
Telesynergy® is a linked medical consultation workstation at the Pine Ridge IHS Hospital and the RCRH CCI. Both systems were obtained through the CDRP grant and are HIPAA-compliant. Telesynergy® consists of a PC-based videoconferencing system, which includes tools such as a diagnostic-quality microscope, a patient exam camera, a color video printer, radiology monitors and a document camera. The workstation integrates all of these imaging capabilities into one system and allows them to be used together during a videoconference. Compatible telemedicine capabilities are also available at the Rosebud Sioux reservation. This infrastructure will facilitate the delivery of comprehensive palliative care services administered through dialogues between oncologists and nurses at RCRH and the cancer patients on the reservations. It will include patient consultation for cancer-related symptom and pain management and caregiver education. Caregivers of these patients will be provided culturally relevant education on issues related to palliative and end-of-life care needs of cancer patients. Such interventions will equip them with the critical knowledge, skills and attitudes to better understand the patient’s condition and needs and to more fully participate in meaningful caregiving.
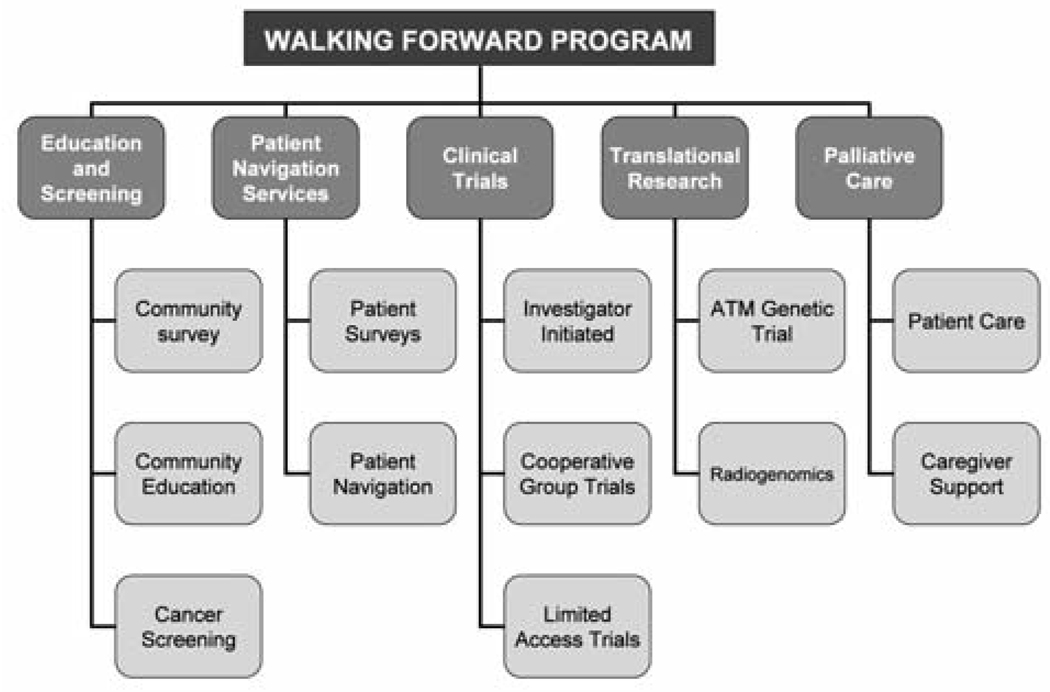
In conclusion, we believe that these comprehensive and coordinated efforts of the Walking Forward program will eventually have a positive effect on population-based measures of cancer-related health outcomes in American Indian communities in Western South Dakota. As illustrated in Figure 2, our next project will address the spectrum of cancer care from screening and education to palliation. The ultimate goal is to influence the stage of cancer at presentation where patients are seen at a much earlier stage of disease and, as a result, have a better chance for cure. American Indians will then have the opportunity to “walk forward” in good health and thereby lead healthier and longer lives.
Figure 2.
Walking Forward Approach to Cancer Care among American Indians in South Dakota.
Acknowledgements
This project has been funded in part with federal funds from the National Cancer Institute, National Institutes of Health, under contract No. N01-CO-12400 and NIH grant RFA IU56CA99010-01 (to D.G.P).
Footnotes
Disclaimer:
The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the Indian Health Service, National Cancer Institute, or the National Institutes of Health.
The authors have no potential conflict of interest.
Please note: Due to limited space, we are unable to list all 58 references. You may contact South Dakota Medicine at 605.336.1965 for a complete listing.
Contributor Information
Shalini Kanekar, Program Director for Walking Forward Program at the John T. Vucurevich Regional Cancer Care Institute at Rapid City Regional Hospital..
Daniel Petereit, a radiation oncologist at the John T. Vucurevich Cancer Care Institute at Rapid City Regional Hospital and with the Department of Human Oncology at the University of Wisconsin-Madison..
REFERENCES
- 1.Jones DS. The Persistence of American Indian Health Disparities. American Journal of Public Health. 2006 Dec;96(12):2122–2134. doi: 10.2105/AJPH.2004.054262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Espey DK, Wu X, Swan J, et al. Annual Report to the Nation on the Status of Cancer, 1975-2004, Featuring Cancer in American Indians and Alaska Natives. Cancer. 2007 Nov 15;110(10):2119–2152. doi: 10.1002/cncr.23044. [DOI] [PubMed] [Google Scholar]
- 3.Haverkamp D, Espey D, Paisano R, Cobb N. Rockville, MD: Indian Health Service; Cancer Mortality among American Indians and Alaska Natives: Regional Differences. 2008 February;:1999–2003.
- 4.Ward E, Jemal A, Cokkinides V, et al. Cancer Disparities by Race/Ethnicity and Socioeconomic Status. A Cancer Journal for Clinicians. 2004;54(2):278–293. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- 5.Giuliano A, Papenfuss M, de Guernsey de Zapien J, Tilousi S, Nuvayestewa L. Breast cancer screening among Southwest American Indian women living on-reservation. Prev Med. 1998;27(1):135–143. doi: 10.1006/pmed.1997.0258. [DOI] [PubMed] [Google Scholar]
- 6.Risendal B, Roe D, DeZapien J, Papenfuss M, Giuliano A. Influence of health care, cost, and culture on breast cancer screening: issues facing urban American Indian women. Preventive Medicine. 1999 Dec;29(6 Pt 1):501–509. doi: 10.1006/pmed.1999.0564. [DOI] [PubMed] [Google Scholar]
- 7.Coughlin SS, Uhler RJ, Blackman DK. Breast and cervical cancer screening practices among American Indian and Alaska Native women in the United States, 1992-1997. Preventive Medicine. 1999 Oct;29(4):287–295. doi: 10.1006/pmed.1999.0537. [DOI] [PubMed] [Google Scholar]
- 8.Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer screening practices in the United States: results from the 2000 National Health Interview Survey. Cancer. 2003;97(6):1528–1540. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- 9.Gilliland FD, Rosenberg RD, Hunt WC, Straubler P, Key CR. Patterns of mammog-raphy use among Hispanic, American Indian, and non-Hispanic White women in New Mexico, 1994-1997. American Journal of Epidemiology. 2000;152(5):432–437. doi: 10.1093/aje/152.5.432. [DOI] [PubMed] [Google Scholar]
- 10.Petereit DG, Rogers D, Govern F, et al. Increasing Access to Clinical Cancer Trials and Emerging Technologies for Minority Populations: The Native American Project. Journal of Clinical Oncology. 2004 Nov 15;22(22):4452–4455. doi: 10.1200/JCO.2004.01.119. [DOI] [PubMed] [Google Scholar]
- 11.Rogers D, Petereit DG. Cancer Disparities Research Partnership in Lakota Country: Clinical Trials, Patient Services and Community Education for the Oglala, Rosebud and Cheyenne River Sioux Tribes. American Journal of Public Health. 2005 Dec;95(12):1–4. doi: 10.2105/AJPH.2004.053645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson RT, Adams-Cameron M, Burhansstipanov L, Roubideaux Y, Cobb N, Lynch CF. Disparities in breast cancer treatment among American Indian, Hispanic, and non-Hispanic White women enrolled in Medicare. Journal of Health Care for the Poor and Underserved. 2007;18:648–664. doi: 10.1353/hpu.2007.0071. [DOI] [PubMed] [Google Scholar]
- 13.Caplan LS, May DS, Richardson LC. Time to Diagnosis and Treatment of Breast Cancer: Results from the National Breast and Cervical Cancer Early Detection Program, 1991-1995. American Journal of Public Health. 2000;90(1):130–134. doi: 10.2105/ajph.90.1.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guadagnolo BA, Cina K, Helbig P, et al. Assessing Cancer Stage and Screening Disparities Among Native American Cancer Patients. When Free Primary Care is not Enough. Public Health Reports. 2009 Jan-Feb;124:79–89. doi: 10.1177/003335490912400111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Washington, DC: National Cancer Institute, DHHS/NIH/NCI; Facing Cancer in Indian Country: The Yakama Nation and Pacific Northwest Tribes. 2002
- 16.Indian Health Service. U.S. Senate; Health Care Services Are Not Always Available to Native Americans: United States Government Accountability Office. Report to the Committee on Indian Affairs. 2005 Aug;
- 17.Guadagnolo BA, Cina K, Helbig P, et al. Medical Mistrust and Less Satisfaction with Health Care among Native Americans Presenting for Cancer Treatment. J Health Care for Poor and Underserved. 2009 Feb;20(1):210–226. doi: 10.1353/hpu.0.0108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilson RT, Adams-Cameron M, Burhansstipanov L, et al. Disparities in Breast Cancer Treatment Among American Indian, Hispanic and Non-Hispanic White Women Enrolled in Medicare. Journal of Health Care for the Poor and Underserved. 2007;18:648–664. doi: 10.1353/hpu.2007.0071. [DOI] [PubMed] [Google Scholar]
- 19.Hodge FS, Fredericks L, Rodriguez B. American Indian women's talking circle: A cervical cancer screening and prevention project. Cancer. 1996;78(7 Suppl):1592–1597. [PubMed] [Google Scholar]
- 20.Molloy K, Reiner M, Ratteree K, et al. Patient Navigation and Cultural Competency in Cancer Care. Association of Community Cancer Centers Oncology Issues. 2007 Sept/Oct;22(5):38–41. [Google Scholar]