Abstract
A continuing challenge in weight loss treatment is attaining maintenance of weight loss. The goal of this study was to develop a counseling method that would assist African American breast cancer survivors with weight loss maintenance. In this pilot study, 31 obese breast cancer survivors were recruited. Individualized, dietitian-led counseling by telephone and free Weight Watchers coupons were provided to all participants for 18 months. At the 6-month time point, women were randomized to receive spirituality counseling or not in addition to the standard program. The spirituality counseling was delivered via telephone using an 8-step framework. Subjects were asked to utilize daily meditation or prayer, daily readings, and the recording of thoughts in a journal. Mean weight loss from baseline to 6 months was a modest 2.0% of baseline weight. From 6 to 18 months, there was no further weight change in the spirituality arm and a gain of 0.7% in the dietitian only arm. Despite little effect on weight loss, it did appear that spirituality counseling positively affected spiritual well-being (FACIT-Sp) scores and dietary quality. The spirituality counseling framework therefore may be further refined and useful for other health promotion studies with African American populations.
Keywords: spirituality, obesity, breast cancer, weight loss, quality of life
INTRODUCTION
Breast cancer in African-American (AA) women appears to follow different patterns than in European American (EA) women, with a relatively higher risk of recurrence and shorter survival in AA women.1,2 Weight gain and obesity negatively affect prognosis after a breast cancer diagnosis, but it is still unclear whether obesity affects prognosis in AA women as it does EA women.3–5 Effects of body weight on health in survivorship are still an issue, however, as cancer survivors bear a disproportionate burden of illness and lost productivity versus the general population that is still present many years post diagnosis.6 Byers and Sedjo have argued that diet, physical activity and weight management trials in breast cancer survivors may best focus on endpoints that are more prevalent in survivors than recurrence such as risks of cardiovascular disease and diabetes, and preservation of quality of life.7 In AA breast cancer survivors, this is compounded by the overall greater incidence of obesity, insulin-resistance, and diabetes in AAs as compared with EAs.8–10 AA women have been shown to gain twice as much weight after a diagnosis of breast cancer as EA women.11 Design of effective weight loss interventions in obese AA breast cancer survivors is therefore needed.
There have been a number of studies comparing weight loss interventions in AAs and EAs. Most of these studies used group approaches and indicated that weight loss can be achieved in AAs, but typically the extent of weight loss has been less than in EAs.12, 13 A review of weight loss interventions for AA women has identified several important components of successful interventions.14 Group sessions appeared to be essential, but individual-centered programs led to more enthusiastic participation and more sustained weight loss. Programs that utilized a counselor to provide individualized guidance were more effective.14, 15 Finally, there is growing evidence that an approach utilizing spirituality may help AA women adhere to weight loss and other health behaviors.16–22 Spirituality therefore might be useful for maintenance of weight loss after the intensive phase of weight loss counseling is over, at which time weight regain typically occurs.
Spirituality is an integral part of human existence that defines the basic value around which all other values are focused. Most Americans believe that spirituality gives meaning to life, aids in decision making, and is a necessary component of health.23 Spirituality and religiosity are conceptually linked, but they are not the same.24 Religiosity generally does have a spiritual component, but it also encompasses the personal practices related to both communal faith and group rituals as well as the communications stemming from shared conviction. Spirituality is defined as “the propensity to find meaning through a sense of relatedness to dimensions that transcend the self in such a way that empowers and does not devalue the individual. This relatedness may be experienced intra-personally (as a connectedness within oneself), interpersonally (in the context of others and the natural environment), and trans-personally (referring to a sense of relatedness to the unseen, God, or power greater than the self and ordinary resources)”.25 Individuals can be spiritual without a focus on a Higher Power. These individuals “are able to feel a sense of spiritual connectedness within themselves through memory or imagination; they also experience integrative powers of spirituality in their relationships with others and the world”. 26
The spiritual approach may be especially relevant to weight loss in AA women. In a large study of persons with chronic illnesses, AAs had significantly higher spirituality scores than Latinos or EAs using the Cella Well-Being Spirituality sub-scale (FACIT-Sp).27 AAs also are more likely than EAs to use spirituality to cope with adversity, including the stress associated with the diagnosis of breast cancer.28–31 Studies of breast cancer survivors report that religious beliefs, prayer and meditation are powerful coping forces within their lives. 32 The “connectedness” of social support associated with religion and spirituality has been shown to improve quality of life and even survival in breast cancer patients.33, 34 One study found that 36% of AA breast cancer survivors used spiritual healing.35 Spiritual strategies also were shown to be effective for cardiovascular health promotion in AA women,22, 36 and spiritual themes were used in culturally-tailored materials developed to promote healthy eating and physical activity in a church-based program.37
This literature therefore indicates that utilizing spiritual influences to foster motivation for acquiring and maintaining better health behaviors might be an important long-term weight management strategy. We hypothesized that spirituality would help breast cancer survivors maintain weight loss. We therefore conducted a randomized, culturally-tailored clinical trial of spirituality counseling for weight management in AA breast cancer survivors. Both study arms received individualized dietary and exercise counseling combined with Weight Watchers for 18 months, and at the 6-month time point women were randomized to also receive spirituality counseling or not. A framework was developed for non-denominational spirituality counseling utilizing each participant’s own relationship to a higher power.
METHODS
Subject recruitment and trial design
The Lifestyle Improvement with Food and Exercise (LIFE) Study was approved by the Human Investigation Committee of Wayne State University. The main sources of subject recruitment in the greater Detroit area were direct solicitation of clinic patients by their providers, presentations and mailings to an AA breast cancer support group, community advertising through a local newspaper, and brochures placed in the Karmanos Cancer Institute breast care clinic. Females who had been diagnosed with stage I, II or IIIA breast cancer within the last 10 years and who identified themselves as African American were eligible. After 10 years, risk of breast cancer approaches the general population risk.38 Other eligibility criteria included: BMI 30–45 kg/m2; completed chemo- or radiation therapy at least 3 months previous (with the exception of tamoxifen); age 18–70; willing and able to follow diet and exercise recommendations; and having spiritual influences in their lives as determined from a spirituality index screening questionnaire. The spirituality index screening questionnaire was designed to exclude those with no personal conceptualization of spirituality.32 The screening measure consisted of six items. A low score on 3 or more of the items would disqualify a potential subject, and nobody was disqualified because of a low score on this index. Women with a recurrence, a second primary tumor or other history of malignant tumors were not eligible. Eligible women were not presently on a special diet for a medical condition (e.g., Type 1 diabetes) or currently participating in a formal weight reduction program.
Interested women were invited to meet with the study coordinator to learn more about the study and to determine eligibility. Potential participants were asked to keep 3-day food records (one weekend and two week days). Subjects were required to bring these food records to the baseline appointment as a final element of eligibility that would also alert the women to the record-keeping requirements of the study. The dietary data that obese persons provide on records is known to be under-reported,39 but it did provide the dietitian with information on the food preferences and eating patterns of the participants and was used during the counseling.
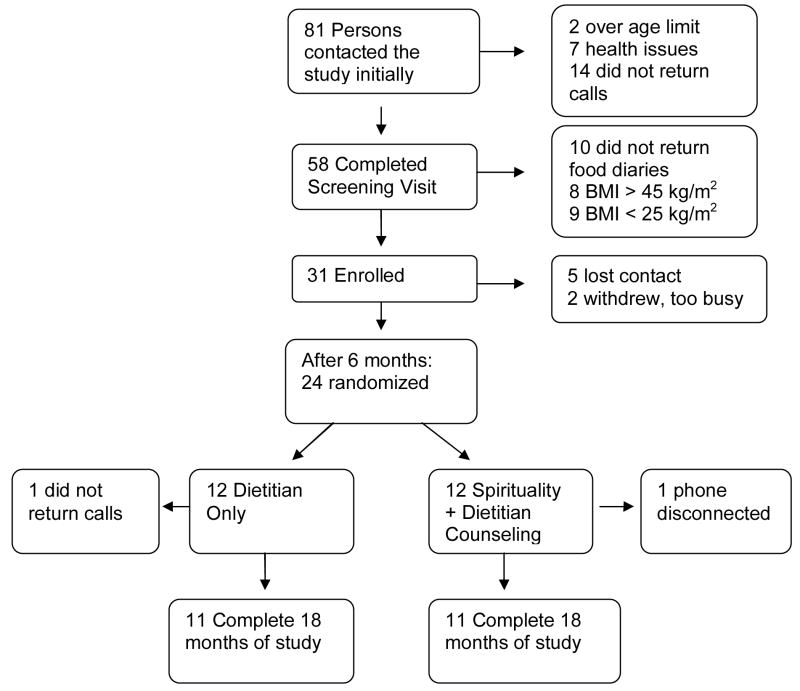
Randomization was conducted after 6 months of standard weight loss counseling (Figure 1). At this time, the dietary counseling became less frequent (see description under “Dietitian-led counseling”), making addition of spiritual counseling feasible. Based on our previous study, it was planned that most women would be entering a weight maintenance phase after 6 months. Stratification was by weight loss of 5% or more versus less than 5% weight loss, relative to baseline. The randomization to the dietitian-only group, which was to continue with dietitian-led counseling, or to the spirituality group, which added spirituality counseling to the standard program, was accomplished using a block size of four. Study assessment visits were conducted every 6 months (baseline, 6, 12 and 18 months). The baseline visit lasted about two hours since the program materials were reviewed at that time, and the other visits lasted about one hour.
Figure 1.
Study enrollment and subject flow shown using the format provided by the Consolidated Standards of Reporting Trials (CONSORT). Randomization occurred after 6 months of dietitian-led weight loss counseling.
Dietitian-led Counseling
Individualized counseling led by a registered dietitian was provided to all study participants for 18 months. The counseling was done in person at the baseline, 6, and 12 month visits with interim contacts by telephone. The aim was to provide weekly contacts for the first 3 months, biweekly for months 3–6 and monthly thereafter. If a subject was not available at the appointed time for the call, a message was left. The goal was to attain a weight loss of 10% of initial weight using realistic short-term goals that included exercise and dietary energy control using balanced diet plans. The dietitian-led counseling approach utilized the theoretical framework of Bandura’s social cognitive theory.40 Weight Watchers coupons also were provided for free weekly attendance throughout the study since we found previously that Weight Watchers increased early weight loss success over individualized counseling alone.41, 42 Weight Watchers pre-packaged meals were not recommended by the dietitian. A monthly newsletter included topics on environmental control, goal setting, negative/positive thinking, body image, self-monitoring, social support, and time management.
Counseling for the weight loss goal of 10% of baseline body weight targeted a 1 to 2 pound/week weight loss using the American Dietetic Association dietary exchange list diet method.43 The recommendation was for a deficit of 500 to 1000 kcal per day below the calculated. maintenance intake for a given body weight (using an estimate of 11 kcal/pound needed for maintenance).44 Subjects were asked to decrease fat to 20–25% of calories, to keep protein at about 20% of calories, to use whole grains for at least half of their daily grain intake, and include at least 6–8 servings of fruits and vegetables each day, depending on energy intake (with an emphasis on variety). The exchange list method was chosen since it accommodates individual food preferences, which appears important for AA women.45
In addition to control of caloric intake, study participants were asked to exercise at least 30 minutes most days each week (at least 5), in accord with currently accepted guidelines,46 using their preferred mode of exercise. Subjects were given pedometers for self-monitoring, and instructed that 10,000 steps each day is a desirable goal. Lists of local resources such as mall walking clubs, biking clubs, library exercise videos and community facilities near their place of work or home were provided. Subjects were asked to keep a log of time spent on exercise together with their dietary exchange log in the same weekly self-monitoring booklet. Envelopes with postage were provided for mailing this log to the dietitian before the scheduled call. This method was successful in our previous study of breast cancer survivors.47 In addition, a pilot study with 12 AA obese breast cancer survivors showed that this published dietitian-led approach resulted in a mean loss of 9.8% of baseline weight over 6 months (unpublished data).
Spirituality Counseling
The spirituality approach was selected based on two focus groups that we conducted with 15 women before we initiated this study. The focus groups indicated that overweight and obese AA breast cancer survivors were attracted to an approach that uses spirituality to help them incorporate and follow new lifestyle patterns for maintenance of a lower body weight. The spirituality counseling was aimed at addressing the following areas which we identified as important to weight loss maintenance: 1) coping in a crisis; 2) setting priorities; 3) dealing with emotional issues which trigger old behavior patterns; and 4) developing accountability for following desired diet and exercise behaviors. The most common cause of relapse during behavior change attempts has been identified as distress. Other causes of relapse include social pressure from a social network, and lifestyle issues where time is a factor in accomplishing desired diet and exercise goals.48
Spirituality is thought to build the inner strength that is necessary to reduce stress and to prioritize one’s own needs, both of which are important in weight management.49 Connectedness with others and a higher power (key elements of spirituality) also can be used to create accountability outside of one’s own self for maintaining weight loss behaviors. The goal of the spiritual counseling therefore was to strengthen and utilize spiritual ties to incorporate healthy lifestyle behaviors into each woman’s own value system. Some participants already had strong spiritual ties that could be applied towards weight loss behaviors while others needed to first build their spiritual ties before they could be used to foster healthy lifestyle behaviors.
A spiritual counselor with a Master’s degree in Counseling Psychology and a certification in Biblical Counseling conducted this intervention. Contacts with the spiritual counselor were exclusively by telephone. These contacts were scheduled to be weekly for 3 months, biweekly for the next 3 months, and then monthly, with flexibility for each individual based on need. The frequency of contacts was documented. The spiritual counselor also discussed the progress of each participant with the dietitian, so that the counseling was coordinated.
Counseling Framework
The spirituality counseling framework was based loosely on 12-step strategies such as Alcoholics Anonymous, Overeaters Anonymous, and the Renfrew Perspective for eating disorders and behavioral dependencies. These programs are widely used in the community, and are documented to be effective for addictive behaviors related to drug and alcohol abuse.50, 51 Some of the steps in these programs were not applicable to weight control or to women who might have low-self esteem at the outset. For example, many 12-step programs were developed for men with addictive behaviors who suffer from egotistical tendencies.52 Overeaters Anonymous utilizes a 12-step program for weight loss which suggests that compulsive over-eating is beyond a person’s power to overcome; therefore, one must surrender to a Higher Power.53 Several of the steps refer to personal shortcomings, defects in character, and making amends to persons harmed by one’s behavior.54 These steps therefore had to be revised for a more acceptable program that women interested in weight loss and health could use to empower themselves with the strength needed to make lifestyle changes. The 8-step framework and the implementation plan are shown in Tables 1 and 2.
Table 1.
8-Component Theoretical Framework for Spiritual Counseling on Weight Loss
|
Table 2.
Implementation Plan for Spirituality Counseling.
| Ask the subject to identify the issues in their own life that contribute to overweight and obesity (step #5). | The counselor will help assess the problem by listening attentively, being non-judgmental, allowing the expression of feelings, and being warmly supportive, as is recommended for spiritual counseling in general. 75 Asking participants to summarize thoughts from their reflections journal can also help participants become aware of problem areas. |
| Ask for specific definition of the way in which the subject feels powerless over the situation or condition (step #3). | Careful analysis of the contributing problems can identify areas that may be truly out of a person’s hands, and those areas may need to be surrendered (steps #7). Efforts can then be concentrated on the areas that can be modified. |
| Ask in what way a higher Power or connections with others can help (step #2). | The counselor asks questions to help subjects uncover spiritual influences that can be useful in coping with events or experiences that interfere with maintaining weight loss behaviors. These spiritual connections can provide empowerment over problems that are difficult or impossible to address alone (step #1). Some study participants will already have strong spiritual connections while others will require specific readings and meditations to first strengthen those connections (step #2). Other readings and meditations will help subjects understand how these connections support a healthy lifestyle (step #3). |
| Identify character traits that contribute to the problem such as seeking approval, seeking control, obsessive/compulsive behavior, rescuing, taking inappropriate responsibility, hiding feelings, fear of abandonment or authority (step#4). | For example, often time demands stand in the way of exercising daily and preparing healthier foods. The spiritual counselor works to help the participant value herself, using assigned readings and meditations. These will reaffirm the value of each person in the eyes of her Higher Power. The participant can then allow her Higher Power to help re-prioritize her time demands, with the knowledge that if she does not take care of herself she may not be able to fulfill the role her Higher Power has for her, such as the care of others. |
| Confess the behavior (step #1). | Admitting the problem is needed before one can work to address the problem (step #4). This can be revealed by open-ended questioning from the counselor and by use of the reflections journal to become aware of underlying causes of difficult situations. |
| Get ready to work in partnership with your Higher Power to remove this behavior (step #6). | Participants will require varying amounts of counseling before they will be ready to allow a Higher Power to guide them toward a healthier lifestyle. For example, readings can help strengthen the connections needed and can demonstrate how partnership with a Higher Power can help minimize the stress of life’s demands. Using a Higher Power for guidance can help minimize distress from difficult situations. |
| Through prayer or meditation ask for knowledge of your Higher Power’s will for you (steps #8, #3). | Daily prayer or meditation will be an important component of the program to help participants bring their Higher Power into their new, healthier lifestyle. Accountability is a key element of weight loss, and weight gain is generally observed when counseling contacts stop. 76 If accountability can be transferred to a Higher Power through daily prayer or meditation, weight loss maintenance may improve. |
Specific tools
Subjects were taught to use daily meditation, daily readings, and the recording of thoughts in a journal. It has been suggested that in order to achieve a greater spiritual influence in one’s life, time and space must be found for “exercises” that heighten awareness of one’s actions and feelings. 55 Existing weight loss programs conducted in the community through churches, such as Faithful Fitness and First Place: A Christ-centered Health Program, utilize motivational readings from the Bible organized around specific topics relevant to weight loss such as “Value Your Body (your body …..God’s temple)”, “On loan from God”, “Going God’s Way” and “Practical love with difficult people”. 56, 57 The spiritual counselor offered guidance to study participants on developing meditations that helped them observe their own actions and build better behaviors. For some participants, Scripture or prayer was preferred. The book “Walk Tall: Affirmations for People of Color” (C. Brice, RPI Publishing: San Diego, 1994) was given to all participants since it provides daily inspirational readings, generally given as quotes from prominent figures. In addition, subjects were given the book “God Just Showed Up” (L. Watkins, Moody Press: Chicago, 2001).
A reflection journal was used to develop an understanding between experiences and feelings and making sense of those feelings, which can affect faith.55 These reflections were a step towards identifying gainful engagement, and the counselor could be consulted for development of engagement strategies that lead to behavior change. Ongoing questions suggested for reflection in the journal were: 1) How does this experience or event help me discern the presence or absence of a Higher Power in my life? 2) What insights do these events/experiences offer into myself as a person? 3) How does this help me respond to and with others who seek to involve a Higher Power in our lives as part of the community?55
Assessments
Subjects were asked to come to the study office for assessments at 0, 6, 12 and 18 months, and they were provided with $20 for each assessment visit. Body weight was measured to the nearest quarter pound in light clothing without shoes using a Health-o-Meter Professional Beam Scale, model 402KLS (Bridgeview, Illinois). Height was measured without shoes while standing on a level, hard surface with a stadiometer. Hip and waist measures were obtained without restrictive garments to the nearest 0.1cm with a flexible tape measure. A Health Status Questionnaire captured demographic information, gynecological history, medical history (including breast cancer treatment), and body weight history at baseline. Cancer diagnosis and treatment information was obtained from the oncologist’s note. At subsequent visits (6, 12 and 18 months), a Health Update Questionnaire was administered to capture any changes in medications, stress levels, and overall health. Physical activity patterns were captured using the Stanford 7-day Physical Activity Recall, which is based on self-reported typical activity patterns, and the results were calculated in metabolic equivalents.58
Aspects of spirituality were measured by several instruments. The Spiritual Well-Being Questionnaire was a 12-item spiritual well-being scale from the Functional Analysis of Chronic Illness and Therapy Spiritual subscale or FACIT-Sp. This spiritual scale has been validated in persons with chronic illnesses and has two sub-scales: Faith and Meaning/Peace. The Faith subscale is associated with religion, whereas the Meaning/Peace subscale measures a dimension that is independent of any religion or specific belief.27 Subjects were also asked to keep a log of all spiritual influences not related to the study (church attendance, bible study groups, spiritual radio shows, talking with friends for support in life’s challenges etc.) for the week before the assessment visits at 6, 12 and 18 months. The Brief Multidimensional Measure of Religiousness/Spirituality: 1999 from the Fetzer Spirituality Resource Manual was administered at baseline and 18 months.59 This instrument consists of 40 items to calculate 10 scales, assess overall self-ranking and identify religious affiliation. Three of the scales appeared to capture elements of the spiritual counseling in this study most closely: 1) Daily Spiritual Experiences which is derived from 6 items; 2) Private Spiritual Practice which contains 5 items including praying, meditating, saying grace, reading, and watching/listening to religious programs; and 3) Spiritual Coping which includes 7 items and emphasizes the extent of support from a Higher Power in coping.
At the beginning and end of the study, the Block’98 Food Frequency Questionnaire was administered (NutritionQuest, Berkeley, CA). This Food Frequency Questionnaire compared well with food records for assessment of usual fat and fruit-vegetable intakes of women in our previous studies. 60 This questionnaire was first developed using a population sample in the suburban Detroit area (Ypsilanti, MI) that included African Americans.61
Statistical Methods
To assess pre/post-intervention changes within a single group, Wilcoxon matched pairs tests were used. For comparing continuous variables between the two study groups, the Mann-Whitney test or the Wilcoxon matched pairs test was used, as appropriate. For comparisons of continuous variables across three groups, the Kruskal-Wallis test was used. To compare categorical variables across the three groups of subjects, Fisher’s exact test was used. Spearman rank correlations were computed between select pairs of continuous variables. To control Type I error rates, the nominal 0.05 significance level was adjusted via the multiple comparisons procedure of Benjamini and Hochberg.62 This false discovery rate procedure was applied to related sets of comparisons which are specified in footnotes of the data tables.
RESULTS
Demographic and Clinical Characteristics
Subjects were enrolled into the study from 7/22/2004 to 4/7/2005. The flow of subjects from initial contact to study completion is shown in Figure 1. Screening excluded 10 women who failed to return 3-day food diaries, and 17 women were excluded because their BMI was either below or above the inclusion range. Only four of the 31 women enrolled were still premenopausal (three in the dietitian arm and one in the spirituality arm). Almost all of the women had chemotherapy as part of their breast cancer treatment (27 of 31). Only three were currently taking tamoxifen and one was currently taking letrozole.
There were seven women who withdrew prior to randomization and two women who withdrew after randomization. The seven women who withdrew from the study early on were, on average, a little younger, less educated, had later stage cancer and were within a shorter time frame since their initial diagnosis than the women who completed at least 6 months on study. These and other demographic and clinical characteristics did not differ statistically between the seven women who withdrew in the first 6 months, the subjects randomized to the dietitian only arm, and the subjects who received the spirituality counseling (Table 3).
Table 3.
Characteristics of Subjects at Study Enrollment (mean and SD, or number of subjects and percentage of total)
| Characteristic | Dietitian only group n = 12 | Spirituality group n=12 | Un-assigned Subjectsa, n=7 | P-Valueb |
|---|---|---|---|---|
| Demographic Characteristics | ||||
| Weight (kg) | 94.9, 14.8 | 93.8, 11.3 | 95.8, 11 | 0.891 |
| BMI (kg/m2) | 36, 5 | 36, 3 | 37, 5 | 0.947 |
| Weight at age 18 (kg) | 55.2, 5.5 | 59.7, 10.7 | 58.4, 10.3 | 0.460 |
| Age at study Enrollment (years) | 56, 10 | 55, 8 | 50, 7 | 0.305 |
| Married (number, %) | 5 (42%) | 3 (25%) | 3 (43%) | 0.704 |
| College graduate | 6 (50%) | 8 (67%) | 1 (14%) | 0.107 |
| Work outside the Home | 10 (83%) | 5 (42%) | 5 (71%) | 0.119 |
| Live alone | 5 (42%) | 5 (42%) | 1 (14%) | 0.560 |
| Household income<$30,000/year | 3 (25%) | 3 (25%) | 3 (42%) | 0.688 |
| Family history of breast cancerc | 4 (33%) | 2 (17%) | 2 (29%) | 0.678 |
| Clinical Characteristics | ||||
| Age at diagnosis | 51, 9 | 49, 6 | 47, 7 | 0.496 |
| Years since diagnosis | 5.6, 4.3 | 5.7, 3.3 | 2.8, 1.1 | 0.074 |
| Stage I (number, %) | 5 (42%) | 6 (50%) | 0 (0%) | |
| Stage II (number, %) | 3 (25%) | 5 (42%) | 4(57%) | 0.104d |
| Stage III (number, %) | 4 (33%) | 1 (8%) | 3 (43%) | |
| Hormonal Therapye | 5 (42%) | 8 (67%) | 6 (86%) | 0.204. |
| Spirituality and Depression Scalesf | ||||
| FACIT-Sp | ||||
| Overall | 40.8, 6.5 | 41.7, 5.7 | 35.9, 3.6 | 0.056 |
| Faith | 14.2, 2.9 | 15.1, 2.0 | 12.0, 2.4 | 0.012 |
| Meaning | 26.7, 4.3 | 26.6, 4.3 | 23.9, 4.1 | 0.335 |
| CES-D | 11, 8 | 6, 7 | 12, 9 | 0.201 |
| Daily Spiritual Experiences | 30, 3 | 31, 4 | 30, 4 | 0.625 |
| Spiritual Coping | 24, 3 | 24, 3 | 23, 2 | 0.691 |
| Private Spiritual Experiences | 26, 6 | 26, 5 | 26, 6 | 0.992 |
Un-assigned subjects withdrew from the study before the 6-month randomization appointment.
The p-values shown are from Kruskal-Wallis tests for comparison of the three groups with regard to data from scales and for continuous variables. For variables for which numbers of women are reported, the p-value is from Fisher’s Exact test.
Breast cancer in first-degree relatives.
From testing the distribution of stage (3 groups) over the 3 subject categories using Fisher’s Exact test.
Use of hormonal therapy for breast cancer now or in the past. Two women in the un-assigned group and one woman in the spirituality group were taking tamoxifen at the time of enrollment. One woman in the un-assigned group was currently taking letrozole. All but three women in the spirituality arm and one woman in the dietitian only arm had chemotherapy as part of their breast cancer treatment.
The FACIT-Sp is the spiritual sub-scale of the Functional Assessment of Chronic Illness Therapy well-being scale.27 The CES-D is the Center of Epidemiological Studies Depression scale.77 The other four scales are from the Multidimensional Measure of Spirituality compiled by the Fetzer Institute.59 None of these 7 comparisons are significant at the 0.05 level in the multiple comparisons sense, after applying the Benjamini and Hochberg procedure.62
Compliance to Spirituality Counseling
Spirituality counseling was conducted for the 12 subjects randomized to the spirituality arm. The number of calls completed per subject was 2 to 26 (median 11 calls). When subjects were not home for their counseling appointment, a message was left on the answering machine or with a household member. Most often the same subjects who were difficult for the dietitian to contact were also difficult for the spirituality counselor to contact. The total time spent on spiritual counseling of each subject ranged from 70 to 608 minutes (median 279 minutes), with 17 to 45 minutes per call (median 25.8 minutes). The correlation between number of calls and minutes of total time counseling was high (r = 0.967, p<0.0001). There was no appreciable correlation between number of spirituality counseling calls completed and weight change in the spirituality group (r < 0.2 with weight change at 18 months from either baseline or 6 months).
Dietary Intakes and Physical Activity
The Block’98 Food Frequency Questionnaire was administered at baseline and after 18 months (Table 4). This questionnaire is designed to capture dietary intakes over the past 12 months. At baseline, mean fat intake for all 31 women was about 39.3% of calories (SD 6.7), which is somewhat above national averages of 35% calories from fat for females age 50–59.63 Reported baseline fruit and vegetable intakes of 4.2 servings/day (SD 2.5, n=31) were also above national averages of 3.04 servings/day in the National Health and Nutrition Examination Survey (NHANES) 1999–2002 dataset.64 At baseline, Healthy Eating Index (HEI) scores ranged from 36 to 76 (mean 57, SD 11, n=30). HEI scores take into account the degree to which diet conforms to the Food Guide Pyramid, along with intakes of fat, cholesterol and sodium and a factor for dietary variety.65 Scores of 51–80 on the HEI are classified as “needs improvement”, and scores above 80 are classified as “good”. In the NHANES data from 1999–2000, mean HEI score in non-Hispanic blacks was 61.1, which is a few points above the mean score of 57 for women in this study.66 Both study groups exhibited reductions in fat intake with time, and improvement in the HEI (Table 4). Fruit intakes in the spirituality group increased significantly both with time and relative to the dietitian only group. None of these comparisons were significant at the 0.05 level in the multiple comparisons sense after applying the Benjamini and Hochberg procedure to control the Type I error rate, although the fruit intake comparisons were of borderline statistical significance even after that adjustment.
Table 4.
Dietary Intakes from the Block’98 Food Frequency Questionnaires (mean, SD, n)
| Intake | Baseline | 18 Months | Change | P-value for difference | |
|---|---|---|---|---|---|
| With timea | between groupsb | ||||
| Un-assigned Group | |||||
| Fat, % of calories | 41, 7, 7 | - | - | ||
| Fruit, servings per 1000 kcal | 1.0, 1.0, 7 | - | - | ||
| Vegetables, servings per 1000 kcal | 2.0, 0.7, 7 | - | - | ||
| Healthy Eating Index | 54, 13, 7 | - | - | ||
| Physical Activity, Mcal/week | 26.7, 5.3, 7 | - | - | ||
| Dietitian Only Group | |||||
| Fat, % of calories | 40, 7, 12 | 36, 5, 11 | −7.8, 12.7, 11 | 0.054 | |
| Fruit, servings per 1000 kcal/day | 0.9, 0.7, 12 | 1.1, 0.6, 11 | 0.3, 0.7, 11 | 0.206 | |
| Vegetables, servings per 1000 kcal/day | 1.8, 1.5, 12 | 2.4, 1.3, 11 | 0.5, 0.8, 11 | 0.042 | |
| Healthy Eating Index | 56, 10, 12 | 61, 11, 11 | 6, 11, 11 | 0.100 | |
| Physical Activity, Mcal/week | 24.4, 5.1, 12 | 26.5, 8.3, 11 | 2.4, 8.1, 11 | 0.278 | |
| Spirituality Group | |||||
| Fat, % of calories | 37, 6, 12 | 33, 7, 11 | −5.6, 7.3, 11 | 0.042 | 0.896 |
| Fruit, servings per 1000 kcal/day | 1.3, 0.8, 12 | 2.5, 0.9, 11 | 1.2, 0.8, 11 | 0.007 | 0.013 |
| Vegetables, servings per 1000 kcal/day | 2.9, 2.6, 12 | 3.3, 1.7, 11 | 0.2, 2.6, 11 | 0.465 | 0.895 |
| Healthy Eating Index | 59, 10, 11 | 70, 15, 11 | 12, 14, 10c | 0.036 | 0.418 |
| Physical Activity, Mcal/week | 25.1, 4.3, 12 | 25.4, 4.2, 11 | 0.0, 5.6, 11 | 0.966 | 0.555 |
The p-values for changes with time within each group are from Wilcoxon matched pairs tests using data at 0 and 18 months. None of these 10 comparisons are significant at the 0.05 level in the multiple comparisons sense, after applying the Benjamini and Hochberg procedure.62
The p-values for the difference between the dietitian-only and spirituality groups are from Mann-Whitney tests. None of these 5 comparisons are significant at the 0.05 level in the multiple comparisons sense, after applying the Benjamini and Hochberg procedure.
One subject reported too few foods eaten at baseline to calculate a Healthy Eating Index score. The mean intakes at baseline and changes in dietary intakes were similar with that subject excluded.
Physical activity was assessed by the Stanford 7-day recall.58 These data were used to calculate energy expenditure per week using MET values of 1 for sleep, 1.5 for light activity, 4 for moderate activity, 6 for hard activity and 10 for very hard activities. Mean energy expenditure per week did not change appreciably in either study group (Table 4). Since the intervention targeted moderate exercise, this was examined separately in hours per week. Moderate activities per week increased from baseline to 6 months before randomization (mean 3.9 hours/week, SD 10, n=24), and this increased further from 6 to 18 months in the dietitian only group (mean 2.4 hours/week, SD 13.8, n=11) and the spirituality group (mean 1.3 hours/week, SD 12.5, n=11). Variability in these data was large and none of the changes in physical activity were statistically significant at the 0.05 level in the multiple comparisons sense, after applying the Benjamini and Hochberg multiple comparisons procedure.62
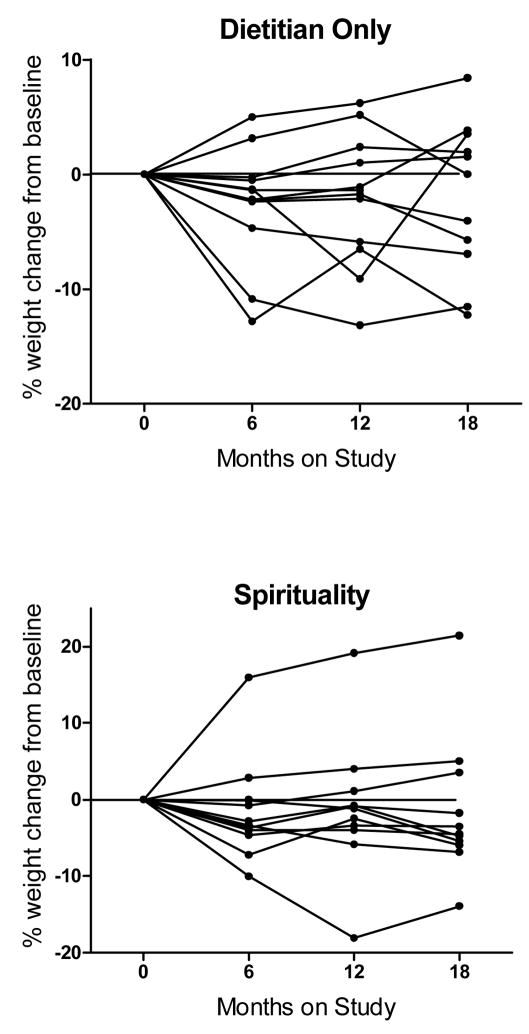
Weight Loss
Weight loss in the study was modest with a mean loss of 2% of baseline weight at 6 months (SD 5.7, n=24), and weight loss from baseline to 6 months did not differ significantly by diet arm assignment being 2.5% in the dietitian only arm and 1.5% in the spirituality arm (Table 5, Figure 2). At 18 months, mean weight loss, as a percentage of baseline weight, was 1.9% in the dietitian-only arm and 1.5% in the combination arm. Weight change from 6 to 18 months indicated a slight regain of 0.7 % (SD 3.3, 0.4 kg regain, n=11) in the dietitian only arm and no regain in the spirituality arm (SD 3.4, n=11), and this difference between the two groups was not statistically significant. There was one woman in the spirituality arm who gained 19 kg from baseline to 6 months and then gained at a slower rate afterwards (Figure 2). Excluding that subject, mean weight loss in the spirituality arm at 18 months was 3.2% of baseline weight. At the 18-month time point, five of 11 women exhibited weight loss, relative to baseline, in the dietitian-only arm and eight of 11 women exhibited weight loss in the spirituality arm (Figure 2).
Table 5.
Changes in weight, spirituality and depression from baseline to 6 months and from 6 months to 18 months (mean, SD and n)
| Measure | Dietitian only group | Spirituality group | P-value for comparison between groupsa | ||
|---|---|---|---|---|---|
| 0 to 6 mos. | 6 to 18 mos. | 0 to 6 mos. | 6 to 18 mos. | ||
| % weight changeb | −2.5, 5.1, 12 | 0.7, 3.3, 11 | −1.5, 6.5, 12 | 0.0, 3.4, 11 | 0.555 |
| change in weight (kg) | −2.6, 4.7, 12 | 0.4, 3.0, 11 | −1.0, 7.0, 12 | 0.3, 3.4, 11 | 0.922 |
| FACIT-Sp Score | |||||
| Total | 0.7, 4.3, 12 | −3.3, 3.9, 11 | 0.2, 2.2, 12 | −0.2, 3.2, 11 | 0.024 |
| Meaning | 1.1, 3.6, 12 | −2.5, 2.8, 11 | 0.3, 2.5, 12 | −0.2, 3.3, 11 | 0.146 |
| Faith | −0.4, 1.4, 12 | −0.8, 3.1, 11 | −0.1, 0.5, 12 | 0.0, 0.6, 11 | 0.451 |
| CES-D score | −0.3, 9.0, 12 | −0.9, 7.7, 11 | −1.0, 7.0, 12 | −1.7, 5.6, 11 | 0.646 |
P-values shown are from Mann-Whitney tests for the difference between dietitian only versus spirituality groups for the change from 6 to 18 months since randomization occurred at 6 months. None of these 6 comparisons are significant at the 0.05 level in the multiple comparisons sense, after applying the Benjamini and Hochberg procedure.
The percent change in weight was calculated from either baseline or 6 months, as appropriate.
Figure 2.
Percent weight change from baseline for each woman randomized to spirituality counseling or not.
Spirituality
Several scales were used to assess spirituality in the subject’s lives. The spirituality sub-scale of the Well-Being Questionnaire (or Functional Analysis of Chronic Illness Therapy, FACIT-Sp) indicated that the mean overall score at baseline for spirituality in this study (mean 40.0, SD 5.9, n=31), and there was no significant difference in mean score by diet arm assignment (Table 3). These scores are very similar to that reported by Peterman et al. for a sample of breast cancer patients of mixed ethnicity and race (mean score 39.9).27 After 18 months, there was a decrease in spiritual well-being in the dietitian only arm (from a mean score of 41 at baseline to a mean score of 38 at 18 months), and there was no change in FACIT-Sp score of 42 in the spirituality arm. The mean changes in spiritual well-being from 6 to 18 months are shown in Table 5 since subjects were randomized at 6 months, and the score decreased in both diet arms. The decrease in the FACIT-Sp score from 6 to 18 months was greater in the dietitian-only arm (−3.3 points) versus the spirituality arm (−0.2 points), as shown in Table 5. The change in FACIT-Sp score from 6 to 18 months for the spirituality arm was also significantly and positively correlated with total minutes of spirituality counseling time (r = 0.704, p = 0.008) and almost significantly associated with number of calls (r = 0.599, p = 0.026), but the number of women was small (n=11).
The Fetzer “Multidimensional Measure of Spirituality” instrument was also administered 0 and 18 months. 59 This instrument yields 12 scales. Five of the scales refer to religiosity and therefore were not entirely relevant to this study, but it is interesting to note that all but 6 of 31 women attended church at least once a month at baseline. Eight women were non-denominational, 12 Baptist, 1 Mormon, 3 Catholic, and 7 belonged to other Protestant religions. The changes in the three scales most relevant to spirituality counseling were small and not statistically significant (p>0.35 in each case comparing the two study arms). These were: 1) An increase in the Daily Spiritual Experiences scale in the spirituality arm (mean 0.2, SD 2.7) and in the dietitian only arm (mean 1.5, SD 3.2); 2) Increases in the private spiritual experiences scale of 1.7 (SD 2.9) in the spirituality arm and 1.4 (SD 5.1) in the dietitian only arm; and 3) For spiritual coping, there was an increase in the spirituality arm (mean 0.5, SD 2.5) and a decrease in the dietitian-only arm (mean −0.6, SD 3.5). The other spiritually-relevant scales in the Fetzer Measure had little inter-individual variation in responses. For the 2-item Meaning scale, all but three women agreed or strongly agreed that their lives unfold according to a greater plan and that they had a sense of mission in their life. The scales of Forgiveness (3 items) and Values/beliefs (2 items) also had little intra-individual variability with 28 of 31 women scoring either “often” or “always” for forgiveness and all either agreed or strongly agreed that a “higher power watches over me”. Overall self-ranking on the Fetzer Measure was very high, with only one woman who was “slightly spiritual” at baseline; the rest of the subjects were all moderately or very religious.
The spirituality counseling included recommendations to spend time each day on spiritual activities to enforce the requested lifestyle changes. Subjects were asked to keep a log of daily spiritual experiences for the week preceding their study visits at 6, 12 and 18 months. Most of the logs were returned. In the dietitian only arm, the mean private time spent on spiritual activities (meditation, prayer, readings) increased from 177 min/week at 6 months (SD 81, n=10) to 256 min/week at 18 months (SD 227, n=11) and total time sent on spiritual activities (which adds attending church, talking to others, listening or watching spiritual programs) increased from 679 to 904 min/week. Neither of these increases was significant (p>0.6 using Wicoxon matched pairs tests). In the spirituality arm, the mean private time increased from 226 min/week at 6 months (SD 221, n=9) to 384 min/week at 18 months (SD 499, n=11), not including time spent on phone counseling (p=0.081). Total time increased from 590 min/week (SD 342, n=9) at 6 months to 871 min/week (SD 665, n=11) at 18 months, which was of borderline significance p=0.048.
Depression
Depression scores, as measured by the CES-D questionnaire, indicated that six of 31 women had clinically-meaningful impairment at baseline (scores higher than 16). In the 22 women who finished 18 months on study, four had scores of 16 or greater at baseline and only one still had a score above 16 at 18 months. Mean CES-D scores improved in both study arms (indicated by a lower score), with a slightly greater improvement in the spirituality arm versus the dietitian only arm as shown in Table 5. Subjects in the spirituality arm did have a lower mean CES-D score at baseline than the subjects assigned to the dietitian only arm. Since a previous study indicated that CES-D scores were inversely related to Healthy Eating Index scores in breast cancer survivors67, we also examined this relationship and found that at baseline there was a negative correlation between HEI and CES-D, but this was of borderline significance in our sample of 31 women (r = −0.343, p=0.064).
DISCUSSION
As cancer treatments have improved over the years, there are now approximately 2 million breast cancer survivors in the United States.68 This makes health in survivorship an important issue, and obesity is of particular relevance because of rising weight levels in the population and obesity is a known risk factor for many chronic diseases. Attempts at prevention of weight gain and obesity in breast cancer survivors, however, may be accompanied by unique psychosocial and biological factors that might not be present in persons who have never been diagnosed with cancer. Our previous trial of weight loss in breast cancer survivors (73% of whom were Caucasian), called the Weight Loss After Breast Cancer Study, provided data on the effectiveness of an individualized, dietitian-led weight loss counseling approach combined with Weight Watchers over 24 months.41, 42 The majority of the weight loss with this combination approach occurred during the first 6 months, resulting in a loss of 10% of initial body weight at that time point. From 6 to 18 months, mean weight regain of 4% of initial body weight occurred (9 pounds), followed by stabilization of mean body weight from 18 to 24 months. After 6 months, the dietitian-led counseling frequency diminishes, making institution of additional counseling feasible. The 6-month time point was therefore chosen for randomization to spirituality counseling or not.
The present study targeted AA breast cancer survivors. AAs as a group seem to suffer disproportionately from cardiovascular disease and diabetes and therefore may benefit from weight control to promote health in survivorship.69 In addition, AA women have a worse prognosis after a diagnosis of breast cancer than EA women.1, 2 A number of weight loss studies have been conducted among AA women, and in general the literature indicates that weight loss occurs at a slower rate in this population group.70 We therefore sought to design a culturally-tailored approach towards weight loss that would help breast cancer survivors incorporate a healthy lifestyle into their own value system and prioritize their own health. Fitzgibbon et al. examined a faith-based weight loss intervention using group sessions in overweight and obese AA women. There was slightly more weight loss in the faith-based group that received scripture readings versus the control group that received a culturally-tailored weight intervention without a faith-based component (2.4% versus 1.7% in 12 weeks).16 Karanja et al. also achieved modest weight loss of 3.7 kg over 6 months in AA women (3.5% of baseline weight), again using group sessions for the intervention.17 There is in fact growing evidence that spirituality may be an important consideration in the design of effective strategies for weight control as well as for other health-promoting behaviors in AAs.18–22 For breast cancer survivors, a spirituality approach is particularly attractive since connections with others (i.e. social support) have been shown to reduce stress in breast cancer survivors,34, 71 and stress is a frequent cause of relapse in weight loss treatment.48 Spirituality has been shown to improve both quality of life and coping in breast cancer survivors.72–74
Despite the fact that there was little influence of spirituality counseling on weight loss in this pilot study, there did appear to be a positive effect on spiritual well-being (FACIT-Sp), which is an encouraging finding relevant to quality of life. In addition, the Healthy Eating Index improved by 12 points in the spirituality arm, which may be important for weight control over longer periods of time. Although there were few statistically significant findings in this study, there may be certain individuals who benefit to a relatively greater extent with this type of weight control approach. Limitations of the study include the small sample size and very modest initial weight loss, which made examination of weight loss maintenance difficult. Generalizing this program to community settings might be difficult since the women in the study were fairly well educated overall and there would be costs associated with use of the Weight Watchers program and the professional counselors. Another limitation is that the spirituality counseling was administered by telephone, which may be less efficacious than in-person counseling. The framework developed for spirituality counseling may, however, be useful for further methods development, especially in longer-term studies targeting improved health in AA cancer survivors.
Acknowledgments
We thank the women who took the time to participate in this study. We thank Cheryl Miree for assisting with study set-up, and we thank Gwen Traylor and Kelly Brittain for assisting with subject recruitment.
Financial Support. This study was supported by NCI-CAM grant 1R21 CA100720, the Weight Watchers Group, (Farmington Hills, MI), and NCI Cancer Center Support Grant CA-22453.
References
- 1.Bowen RL, Stebbing J, Jones LJ. A review of the ethnic differences in breast cancer. Pharmacogenomics. 2006;7:935–942. doi: 10.2217/14622416.7.6.935. [DOI] [PubMed] [Google Scholar]
- 2.Rose DP, Royak-Schaler R. Tumor biology and prognosis in black breast cancer patients: a review. Cancer Detect Prev. 2001;25:16–31. [PubMed] [Google Scholar]
- 3.Chlebowski RT, Aiello E, McTiernan A. Weight loss in breast cancer patient management. J Clin Oncol. 2002;20:1128–1143. doi: 10.1200/JCO.2002.20.4.1128. [DOI] [PubMed] [Google Scholar]
- 4.Cleveland RJ, Eng SM, Abrahamson PE, et al. Weight gain prior to diagnosis and survival from breast cancer. Cancer Epidemiol Biomarkers Prev. 2007;16:1803–1811. doi: 10.1158/1055-9965.EPI-06-0889. [DOI] [PubMed] [Google Scholar]
- 5.Palmer JR, Adams-Campbell LL, Boggs DA, et al. A prospective study of body size and breast cancer in black women. Cancer Epidemiol Biomarkers Prev. 2007;16:1795–1802. doi: 10.1158/1055-9965.EPI-07-0336. [DOI] [PubMed] [Google Scholar]
- 6.Yabroff KR, Lawrence WF, Clauser S, et al. Burden of illness in cancer survivors: findings from a population-based national sample. J Natl Cancer Inst. 2004;96:1322–1330. doi: 10.1093/jnci/djh255. [DOI] [PubMed] [Google Scholar]
- 7.Byers T, Sedjo RL. A weight loss trial for breast cancer recurrence: pre-menopausal, post-menopausal, both, or neither? Cancer Causes Control. 2006;17:1–3. doi: 10.1007/s10552-005-0547-4. [DOI] [PubMed] [Google Scholar]
- 8.Mokdad AH, Serdula MK, Dietz WH, et al. The spread of the obesity epidemic in the United States, 1991–1998. JAMA. 1999;282:1519–1522. doi: 10.1001/jama.282.16.1519. [DOI] [PubMed] [Google Scholar]
- 9.Davidson MB. The disproportionate burden of diabetes in African-American and Hispanic populations. Ethn Dis. 2001;11:148–151. [PubMed] [Google Scholar]
- 10.Okosun IS. Racial differences in rates of type 2 diabetes in American women: how much is due to differences in overall adiposity? Ethn Health. 2001;6:27–34. doi: 10.1080/13557850120040379. [DOI] [PubMed] [Google Scholar]
- 11.Rock CL, Flatt SW, Newman V, et al. Factors associated with weight gain in women after diagnosis of breast cancer. Women’s Healthy Eating and Living Study Group. J Am Diet Assoc. 1999;99:1212–1221. doi: 10.1016/s0002-8223(99)00298-9. [DOI] [PubMed] [Google Scholar]
- 12.Kumanyika SK. Obesity in African Americans: biobehavioral consequences of culture. Ethn Dis. 1998;8:93–96. [PubMed] [Google Scholar]
- 13.Kumanyaka (sic) SK, Obarzanek E, Stevens VJ, et al. Weight-loss experience of black and white participants in NHLBI-sponsored clinical trials. Am J Clin Nutr. 1991;53:1631S–1638S. doi: 10.1093/ajcn/53.6.1631S. [DOI] [PubMed] [Google Scholar]
- 14.Bronner Y, Boyington JEA. Developing weight loss intervention for African-American women: elements of successful models. J Natl Med Assoc. 2002;94:224–235. [PMC free article] [PubMed] [Google Scholar]
- 15.Kaul L, Nidiry JJ. Management of obesity in low-income African Americans. J Natl Med Assoc. 1999;91:139–143. [PMC free article] [PubMed] [Google Scholar]
- 16.Fitzgibbon ML, Stolley MR, Ganschow P, et al. Results of a faith-based weight loss intervention for black women. J Natl Med Assoc. 2005;97:1393–1402. [PMC free article] [PubMed] [Google Scholar]
- 17.Karanja N, Stevens VJ, Hollis JF, et al. Steps to soulful living (steps): a weight loss program for African-American women. Ethn Dis. 2002;12:363–371. [PubMed] [Google Scholar]
- 18.Drayton-Brooks S, White N. Health promoting behaviors among African American women with faith-based support. ABNF J. 2004;15:84–90. [PubMed] [Google Scholar]
- 19.Kumanyika SK, Whitt-Glover MC, Gary TL, et al. Expanding the obesity research paradigm to reach African American communities. Prev Chronic Dis. 2007;4:A112. [PMC free article] [PubMed] [Google Scholar]
- 20.Chester DN, Himburg SP, Weatherspoon LJ. Spirituality of African-American women: correlations to health-promoting behaviors. J Natl Black Nurses Assoc. 2006;17:1–8. [PubMed] [Google Scholar]
- 21.Reicks M, Mills J, Henry H. Qualitative study of spirituality in a weight loss program: contribution to self-efficacy and locus of control. J Nutr Educ Behav. 2004;36:13–15. doi: 10.1016/s1499-4046(06)60123-1. [DOI] [PubMed] [Google Scholar]
- 22.Yanek LR, Becker DM, Moy TF, et al. Project Joy: faith based cardiovascular health promotion for African American women. Public Health Rep. 2001;116 (Suppl 1):68–81. doi: 10.1093/phr/116.S1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moberg DO. The reality and centrality of spirituality. In: Moberg DO, editor. Aging and Spirituality. Binghamton, NY: Haworth Pastoral Press; 2001. pp. 3–20. [Google Scholar]
- 24.Mickley JR, Soeken K, Belcher A. Spiritual well-being, religiousness and hope among women with breast cancer. Image J Nurs Sch. 1992;24:267–272. doi: 10.1111/j.1547-5069.1992.tb00732.x. [DOI] [PubMed] [Google Scholar]
- 25.Brewer EDC. Life stages and well-being. In: Moberg DO, editor. Spiritual Well-Being: Sociological Perspectives. Washington D.C: University Press; 1979. pp. 99–111. [Google Scholar]
- 26.Baker D, Nussbaum P. Religious practice and spirituality - Then and now: A retrospective study of spiritual dimensions of residents residing at a continuum care retirement community. J Relig Gerontol. 1997;10:33–44. [Google Scholar]
- 27.Peterman AH, Fitchett G, Brady MJ, et al. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy--Spiritual Well-being Scale (FACIT-Sp) Ann Behav Med. 2002;24:49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 28.Samuel-Hodge CD, Headen SW, Skelly AH, et al. Influences on day-to-day self-management of type 2 diabetes among African-American women: Spirituality, the multi-caregiver role, and other social context factors. Diabetes Care. 2000;23:928–933. doi: 10.2337/diacare.23.7.928. [DOI] [PubMed] [Google Scholar]
- 29.Lackey NR, Gates MF, Brown G. African American women’s experiences with the initial discovery, diagnosis, and treatment of breast cancer. Oncol Nurs Forum. 2001;28:519–527. [PubMed] [Google Scholar]
- 30.Koenig HG, McCullough ME, Larson DB. Handbook of Religion and Health. New York: Oxford University Press; 2001. [Google Scholar]
- 31.Potts RG. Spirituality and the experience of cancer in an African-American community: implications for psychological oncology. J Psych Oncol. 1996;14:1–19. [Google Scholar]
- 32.Post-White J, Ceronsky C, Kreitzer M, et al. Hope, spirituality, sense of coherence, and quality of life in patients with cancer. Oncol Nurs Forum. 1996;23:1571–1579. [Google Scholar]
- 33.Weihs KL, Enright TM, Simmens SJ. Close relationships and emotional processing predict decreased mortality in women with breast cancer: preliminary evidence. Psychosom Med. 2008;70:117–124. doi: 10.1097/PSY.0b013e31815c25cf. [DOI] [PubMed] [Google Scholar]
- 34.Lee CO. Quality of life and breast cancer survivors. Psychosocial and treatment issues. Cancer Pract. 1997;5:309–316. [PubMed] [Google Scholar]
- 35.Lee MM, Lin SS, Wrensch MR, et al. Alternative therapies used by women with breast cancer in four ethnic populations. J Natl Cancer Inst. 2000;92:42–47. doi: 10.1093/jnci/92.1.42. [DOI] [PubMed] [Google Scholar]
- 36.Ruesch AC, Gilmore GD. Developing and implementing a Healthy Heart program for women in a parish setting. Holist Nurs Pract. 1999;13:9–18. doi: 10.1097/00004650-199907000-00004. [DOI] [PubMed] [Google Scholar]
- 37.Resnicow K, Campbell MK, Carr C, et al. Body and soul. A dietary intervention conducted through African-American churches. Am J Prev Med. 2004;27:97–105. doi: 10.1016/j.amepre.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 38.Saphner T, Tormey DC, Gray R. Annual hazard rates of recurrence for breast cancer after primary therapy. J Clin Oncol. 1996;14:2738–2746. doi: 10.1200/JCO.1996.14.10.2738. [DOI] [PubMed] [Google Scholar]
- 39.Hill RJ, Davies PS. The validity of self-reported energy intake as determined using the doubly labelled water technique. Br J Nutr. 2001;85:415–430. doi: 10.1079/bjn2000281. [DOI] [PubMed] [Google Scholar]
- 40.Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- 41.Djuric Z, DiLaura N, Jenkins I, et al. Weight loss in obese breast cancer survivors: novel strategies. Breast Cancer Res Treat. 2000;64:49. [Google Scholar]
- 42.Djuric Z, Uhley V, Lababidi S, et al. Effect of low-fat and/or low-energy diets on anthropometric measures in participants of the Women’s Diet Study. J Am Coll Nutr. 2002;21:38–46. doi: 10.1080/07315724.2002.10719192. [DOI] [PubMed] [Google Scholar]
- 43.American Diabetes Association, American Dietetic Association. Exchange Lists for Meal Planning. Alexandria, VA and Chicago, IL: American Diabetes Association & American Dietetic Association; 1986. [Google Scholar]
- 44.Ainsworth BE, Haskell WL, Leon AS, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993:71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 45.Dacosta KO, Wilson JF. Food preferences and eating attitudes in three generations of black and white women. Appetite. 1996;27:183–191. doi: 10.1006/appe.1996.0044. [DOI] [PubMed] [Google Scholar]
- 46.American College of Sports Medicine. ACSM position stand on the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness and flexibility in adults. Med Sci Sports Exerc. 1998;30:975–991. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]
- 47.Djuric Z, DiLaura NM, Jenkins I, et al. Combining weight-loss counseling with the Weight Watchers plan for obese breast cancer survivors. Obes Res. 2002;10:657–665. doi: 10.1038/oby.2002.89. [DOI] [PubMed] [Google Scholar]
- 48.Prochanska JO, Norcross JC, Diclements CC. Changind for Good. New York: Avon Books; 1994. [Google Scholar]
- 49.Gandy DJ. Sacred Pampering Principles. New York: William Morrow and Company; 1997. [Google Scholar]
- 50.McGee EM. Alcoholics Anonymous and nursing. Lessons in holism and spiritual care. J Holist Nurs. 2000;18:11–26. doi: 10.1177/089801010001800104. [DOI] [PubMed] [Google Scholar]
- 51.Siqueland L, Crits-Christoph P. Current developments in psychosocial treatments of alcohol and substance abuse. Curr Psychiatry Rep. 1999;1:179–184. doi: 10.1007/s11920-999-0029-6. [DOI] [PubMed] [Google Scholar]
- 52.Morgan OJ. Addiction and spirituality in context. In: Morgan OJ, Jordan MR, editors. Addiction and Spirituality. St. Louis, MO: Chalice Press; 1999. pp. 3–31. [Google Scholar]
- 53.Weiner S. The addiction of overeating: self-help groups as treatment models. J Clin Psychol. 1998;54:163–167. doi: 10.1002/(sici)1097-4679(199802)54:2<163::aid-jclp5>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 54.Overeater’s Anonymous Inc. [Accessed 02/05/2003]; http://www.overeatersanonymous.org/twelve_steps.html.
- 55.Dash MIN, Jackson J, Rasor SC. Hidden Wholeness: An African American Spirituality for Individuals and Communities. Cleveland, OH: United Church Press; 1997. [Google Scholar]
- 56.Lewis C, Smith K. First Place: A Christ-Centered Health Program. Houston, TX: First Baptists Church; 1984. [Google Scholar]
- 57.Lewis C. Choosing to Change: The First Place Change. Nashville: Lifeway Press; 1996. [Google Scholar]
- 58.Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 59.Fetzer Institute. Multidimensional Measurement of Religiousness/Spirituality for Use in Health Research: A report of the Fetzer Institute and the National Institute on Aging Working Group. Kalamazoo, MI: Fetzer Institute; 1999. [Google Scholar]
- 60.Radakovich K, Heilbrun LK, Venkatranamamoorthy R, et al. Women participating in a dietary intervention trial maintain dietary changes without much effect on household members. Nutr Cancer. 2006;55:44–52. doi: 10.1207/s15327914nc5501_6. [DOI] [PubMed] [Google Scholar]
- 61.Block G, Woods M, Potosky A, et al. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43:1327–1335. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 62.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Royal Stat Soc. 1995;57:289–300. [Google Scholar]
- 63.Agricultural Research Service. [Accessed May 1, 2008];Nutrient intakes from food: mean amounts and percentages of calories from protein, carbohydrate, fat and alcohol, one day, 2003–2004. www.ars.usda.gov/ba/bhnrc/fsrg.
- 64.Casagrande SS, Wang Y, Anderson C, et al. Have Americans increased their fruit and vegetable intake? The trends between 1988 and 2002. Am J Prev Med. 2007;32:257–263. doi: 10.1016/j.amepre.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 65.Kennedy ET, Ohls J, Carlson S, et al. The Healthy Eating Index: design and applications. J Am Diet Assoc. 1995;95:1103–1108. doi: 10.1016/S0002-8223(95)00300-2. [DOI] [PubMed] [Google Scholar]
- 66.Basiotis PP, Carlson A, Gerrior SA, et al. Vol CNPP-12: Center for Nutrition Policy and Promotion. U.S. Department of Agriculture; 2002. The Healthy Eating Index: 1999–2000. [Google Scholar]
- 67.Tangney CC, Young JA, Murtaugh MA, et al. Self-reported dietary habits, overall dietary quality and symptomatology of breast cancer survivors: a cross-sectional examination. Breast Cancer Res Treat. 2002;71:113–123. doi: 10.1023/a:1013885508755. [DOI] [PubMed] [Google Scholar]
- 68.Cancer Facts and Figures. Atlanta, GA: American Cancer Society; 2006. [Google Scholar]
- 69.Underwood SM, Buseh AG, Canales MK, et al. Nursing contributions to the elimination of health disparities among African-Americans: review and critique of a decade of research. J Natl Black Nurses Assoc. 2004;15:48–62. [PubMed] [Google Scholar]
- 70.Yancey AK, Miles OL, McCarthy WJ, et al. Differential response to targeted recruitment strategies to fitness promotion research by African-American women of varying body mass index. Ethn Dis. 2001;11:115–123. [PubMed] [Google Scholar]
- 71.Bloom JR, Stewart SL, Johnston M, et al. Sources of support and the physical and mental well-being of young women with breast cancer. Soc Sci Med. 2001;53:1513–1524. doi: 10.1016/s0277-9536(00)00440-8. [DOI] [PubMed] [Google Scholar]
- 72.Henderson PD, Gore SV, Davis BL, et al. African American women coping with breast cancer: a qualitative analysis. Oncol Nurs Forum. 2003;30:641–647. doi: 10.1188/03.ONF.641-647. [DOI] [PubMed] [Google Scholar]
- 73.Leak A, Hu J, King CR. Symptom distress, spirituality, and quality of life in African American breast cancer survivors. Cancer Nurs. 2008;31:E15–E21. doi: 10.1097/01.NCC.0000305681.06143.70. [DOI] [PubMed] [Google Scholar]
- 74.Morgan PD, Gaston-Johansson F, Mock V. Spiritual well-being, religious coping, and the quality of life of African American breast cancer treatment: a pilot study. ABNF J. 2006;17:73–77. [PubMed] [Google Scholar]
- 75.Moberg DO. The spiritual life review. In: Moberg DO, editor. Aging and Spirituality. Binghamton, NY: Haworth Pastoral Press; 2001. pp. 159–175. [Google Scholar]
- 76.Foreyt JP, Goodrick GK. Factors common to successful therapy for the obese patient. Med Sci Sports Exerc. 1991;23:292–297. [PubMed] [Google Scholar]
- 77.Radloff LS. The CES-D Scale: A self-report measure for research in the general population. Appl Psychol Measurement. 1977;1:385–401. [Google Scholar]