Abstract
This randomized controlled trial tested an intervention, Sharing Patients’ Illness Representations to Increase Trust (SPIRIT), designed to enhance communication regarding end-of-life care between African Americans with end-stage renal disease (ESRD) and their chosen surrogate decision makers (N = 58 dyads). We used surveys and semi-structured interviews to determine the feasibility, acceptability, and preliminary effects of SPIRIT on patient and surrogate outcomes at 1 week and 3 months post-intervention. We also evaluated patients’ deaths and surrogates’ end-of-life decision making to assess surrogates’ perceptions of benefits and limitations of the SPIRIT while facing end-of-life decisions. We found that SPIRIT promoted communication between patients and their surrogates and was effective and well received by the participants.
Keywords: end-stage renal disease (ESRD), African American, end-of-life care, decision making, representational intervention
Randomized Controlled Trial of SPIRIT: An Effective Approach to Preparing African American Dialysis Patients and Families for End-of-Life
Advances in medicine may extend life but often with decreasing quality and escalating dependence on medical technologies (Blank & Merrick, 2005). End-stage renal disease (ESRD) is an example of a chronic illness wherein a technology, dialysis, significantly extends patients’ lives but does not necessarily improve the quality of that prolonged survival. The annual mortality rate in this population is high; of 450,000 patients with ESRD, more than 79,000 died in the United States in 2004 (U.S. Renal Data System, 2007). The Renal Physicians Association and American Society of Nephrology (2000) recommend that clinicians initiate timely and continuous discussions with dialysis patients and their families to assist them in expressing wishes about options in managing their illness and end of life. However, many such discussions are delayed until near death and are narrowly targeted to completion of advance directives (Cherlin, et al., 2005; Covinsky, et al., 2000) despite the widely documented limitations associated with advance directives (Fagerlin & Schneider, 2004; Perkins, 2007).
Several factors contribute to the lack of timely end-of-life discussions. Patients and their families may not foresee that death is approaching. This lack of foresight may be due to patients’ vacillating between focusing on the illness (having kidney disease) or on the relative wellness they experience from dialysis. Once acclimated to a life on dialysis, patients and their families may have a perspective of wellness in the foreground; they focus on being as well as possible until the need for hospitalization arises (Paterson, 2001). This perspective may forestall engaging in end-of-life discussions. Or they may be unwilling to believe that they or their loved ones will die (Carr & Khodyakov, 2007a; Morrison, Zayas, Mulvihill, Baskin, & Meier, 1998). Aversions to preparing for hard decisions about dying are difficult to overcome, and such decisions are left to physicians, families, or fate (Cherlin, et al., 2005).Physicians and families often have inadequate intimate knowledge of patients’ wishes (Houts, Smucker, Jacobson, Ditto, & Danks, 2002; Sulmasy, Haller, & Terry, 1994; Uhlmann, Pearlman, & Cain, 1988). Without adequate training, clinicians may have poor communication skills and may lack confidence in conducting end-of-life discussions (Tulsky, 2005; Tulsky, Chesney, & Lo, 1995). Families are not well prepared for end-of-life decision making, particularly in complex and traumatic circumstances and are emotionally unprepared for the decision making process, which typically entails conflicting interests, disagreements, blame, uncertainty, alienation, and feelings of loss (Braun, Beyth, Ford, & McCullough, 2008). There is little congruence between dialysis patients’ preferences for continuation of hemodialysis and their spouses’ judgments on this matter (r < .40) and patients’ thoughts of withdrawing from dialysis are rarely discussed with their spouses (Pruchno, Lemay, Feild, & Levinsky, 2005, 2006).
In any group of patients, wishes regarding end-of-life treatment are far too personal and value-driven for families and clinicians to understand unless they have had sufficient discussion. The lack of timely discussions is particularly problematic in the care of African Americans. ESRD is 4 times more common in African Americans than in Caucasians and is accompanied by a high incidence of co-morbidities (U.S. Renal Data System, 2007). African Americans prefer to have end-of-life discussions with family members rather than with physicians (Hines, et al., 1999) and compared to Caucasians, generally are thought to prefer more aggressive treatment at the end of life (Hopp & Duffy, 2000; McKinley, Garrett, Evans, & Danis, 1996). Little has been done to develop and test approaches for clarifying African Americans’ treatment preferences and values and preparing patients and their families for future crises (Perry, et al., 2005).
The present study tested an intervention, Sharing Patients’ Illness Representations to Increase Trust (SPIRIT), designed to enhance communication regarding end-of-life care between African Americans with ESRD and their chosen surrogate decision makers. The guiding theory of SPIRIT is the representational approach to patient education (Donovan & Ward, 2001; Donovan, et al., 2007). The representational approach is based on Leventhal’s common sense model and the conceptual change model. The first theory purports that individuals have their own representations of their illness or health problems, which consist of five dimensions: identity, cause, consequences, timeline, and cure/control (Leventhal & Diefenback, 1991; Leventhal, Nerenz, & Steele, 1984). These representations serve as a cognitive framework in which new information is processed. The conceptual change model (Hewson, 1993) proposes that the likelihood of learning increases when an opportunity is given to reflect and comment on current ideas and their consequences, when the individual is dissatisfied with current ideas or recognizes the limitations of the ideas, and when alternative information is seen as beneficial (Donovan & Ward; Donovan, et al.; Hewson). In an intervention using the representational approach, the clinician first explores patient’s existing representations to encourage him or her to examine those beliefs carefully. This process provides the opportunity for the patient and the clinician to recognize gaps or confusions in the patient’s understandings. The clinician can then provide new information that is highly individualized and likely to be accepted by the patient (Donovan & Ward; Donovan, et al.).
Using the representational approach, SPIRIT establishes an understanding of the cognitive, emotional, and spiritual aspects of the patient’s representation of his or her illness. These understandings serve as a foundation for the clinician to provide individualized health care information and to assist the patient in examining his or her own values and thresholds related to life-sustaining treatment at the end of life. By including a chosen surrogate in the discussion, SPIRIT offers the surrogate an opportunity to better understand the patient’s illness experiences and values and to be prepared for the responsibility and emotional turmoil that can arise during end-of-life decision making. An earlier intervention entitled Patient-Centered Advance Care Planning (PC-ACP), an intervention based on the representational approach and on the Respecting Choices® program (Hammes & Briggs, 2000), was efficacious in Caucasian patients undergoing major cardiovascular surgery (Song, Kirchhoff, Douglas, Ward, & Hammes, 2005). SPIRIT evolved from PC-ACP with the goal of addressing the particular needs and concerns of African Americans with ESRD.
The purposes of this study were to: (a) determine the feasibility and acceptability of the SPIRIT in African Americans with ESRD and their surrogate decision makers; and (b) examine the preliminary effects of SPIRIT on patient-surrogate congruence in goals of care, patients’ decisional conflict, surrogate decision making confidence, and participants’ psychosocial-spiritual well-being at 1 week and 3 months post-intervention. In addition, we evaluated patients’ deaths and surrogates’ end-of-life decision making to assess surrogates’ perceptions of the benefits and limitations of the SPIRIT while facing end-of-life decisions.
Method
Study Design
This study was a randomized controlled, pre-posttest, design wherein participants (patient-surrogate dyads) were stratified by type of dialysis (hemodialysis vs. peritoneal) and then randomized with equal allocation to the SPIRIT intervention or to usual care control, using permuted block randomization (Pocock, 1979; Rudy, Vaska, Daly, Happ, & Shiao, 1993). The assignment was implemented using sequential, opaque (security lined), numbered envelopes. We determined the sample size based on the feasibility to recruit and retain participants in the project time (1.5 years) given that 11% attrition (drop-out or death) was expected based on the latest census data at the study sites. We obtained measures at baseline (T1), 1 week (T2), and 3 months (T3) following intervention. When death occurred, medical record reviews and a semi-structured interview were conducted with the bereaved surrogate within 2 weeks of the death. Data were collected from January 2007 to June 2008.
Participants and Setting
Patients were deemed eligible if they met the following criteria: self-identified African American, receiving dialysis for at least 3 months prior to enrollment, availability of a surrogate chosen by the patient who could be present during the intervention, over 18 years of age, and able to read, write, and speak English. Social workers at the dialysis clinics approached 125 African Americans from six out-patient dialysis clinics in western Pennsylvania to assess their eligibility. Subsequently, the research staff approached patients who indicated an interest in the study for informed consent and a cognitive function test, the 10-item Short Portable Mental Status Questionnaire (SPMSQ; Pfeiffer, 1975). Patients with > 2 errors on the SPMSQ were deemed ineligible. Upon patients’ consent, the research staff contacted their surrogates and invited them to join the study if they were over 18 years old, able to read, write, and speak English, and willing to participate in the intervention with the patients.
Experimental Protocols
SPIRIT intervention
SPIRIT was an approximately 1-hour, single session, interview with a patient-surrogate dyad, delivered by a trained nurse interventionist who had completed 3.5 days of training. The training was a competency based program using training manuals and it relied primarily on role playing and skill demonstration (Baer, et al., 2007; Carroll, et al., 2000; Dumas, Lynch, Laughlin, Phillips, & Prinz, 2001; Hammes & Briggs, 2000; Miller, Moyers, Arciniega, Ernst, & Forcehimes, 2005). The nurse interventionist was not African American and had 13 years of clinical experience in medical/surgical nursing. The intervention consisted of five elements as summarized in Table 1 The intervention took place in a private room at the dialysis clinic either before or after dialysis or on a non-dialysis day depending on the dyad’s preference. For peritoneal dialysis patients, intervention sessions were delivered after their clinic appointment.
Table 1.
Elements and Goals of the SPIRIT Intervention
| Element | Goal |
|---|---|
| 1. Representational assessment | Both patient and surrogate describe illness representations along with the following dimensions: identity, timeline, consequences, controllability, and spiritual and emotional representations. The goal for all parties is to achieve a deeper understanding of patient’s illness experience and the surrogate’s experience with his/her loved one’s illness. |
| 2. Identifying and exploring gaps and concerns |
The interventionist identifies and explores gaps and concerns the dyad may have regarding illness progression, life- sustaining treatment and decision making. The goal for each member of the dyad is to exchange own values and concerns about life-sustaining treatment at the end-of-life. |
| 3. Creating conditions for conceptual change |
The interventionist encourages the dyad to share their views and ideas about death and dying and end-of-life care. She assists the patient to identify his/her threshold for unacceptable outcomes of life-sustaining treatment. The goal is to gain a good understanding of the dyad’s values of treatment outcomes and concerns. |
| 4. Introducing replacement Information |
The interventionist presents end-of-life scenarios and encourages the patient to clarify goals of care and express concerns. The interventionist assists the surrogate to examine her/his willingness to take the responsibility to act on them and to appreciate surrogate roles. |
| 5. Summary | The interventionist summarizes the value of the discussion and the need for future discussions. She also assesses any additional support they need such as consultation with social worker at the clinic and spiritual advisor. |
Every intervention session was audio-recorded and periodically reviewed as part of quality monitoring. We developed and used intervention manuals that clearly described the operationalized theoretical components of the intervention for training and assessment of interventionist’s performance. We periodically monitored content fidelity (the extent to which each of the 5 key components of the intervention was delivered) and process fidelity (the extent to which the prescribed communication skills were used; Dumas, et al., 2001) throughout the study using an investigator-developed fidelity evaluation tool. Every intervention session was audio-recorded for periodic review of 10 randomly selected intervention sessions. These sessions were evaluated for the interventionist’s adherence to the protocol for intervention delivery. Any detected problems in conducting sessions and drift from protocol were discussed with the interventionist and targeted re-training was provided if necessary.
Usual care
A social worker at each dialysis clinic provided written information on advance directives and the patient’s right to have an advance directive to every patient on the first day of dialysis treatment. The social worker encouraged patients to complete an advance directive and addressed their individual questions about life-sustaining treatment options. If completed, the advance directive was placed in the medical record. Questions about their medical condition and related end-of-life treatment options were referred to their physicians. Typically, this usual care is a one-time service provided on admission to the dialysis clinic unless the patient expresses his or her desire for a Do-Not-Resuscitate order. Although the POLST (Physician Orders for Life-Sustaining Treatment; Hickman, Sabatino, Moss, & Nester, 2008) has been used in some western Pennsylvania counties, the participating dialysis clinics were not using this program.
Measures
Feasibility
We assessed feasibility of recruiting African Americans with ESRD by tracking the proportion of dyads who agreed to participate among those who were eligible for the study and their reason for refusal. The feasibility of conducting SPIRIT was assessed by the proportion of consented dyads that completed the study in each group (control and intervention) and the mean and median minutes that were required for the nurse interventionist to complete the intervention.
Acceptability
The Patient-Clinician (or Interventionist) Interaction Index (Saha, Arbelaez, & Cooper, 2003) consists of 5 questions about specific clinician behaviors indicative of quality interactions. Patients and surrogates each completed a survey at 1 week and 3 months. They responded on a 4-point scale from 1 (A great deal) to 5 (None at all) regarding clinician behaviors (listening, explaining, participatory decision making, time spent, and respect). A data collector who was not an interventionist administered the surveys with instructions for the participant to think about the social worker who provided usual care (for the control group) or the interventionist (for the intervention group). A sum of the items, ranging 5 to 20, was used as a quality interaction index, with lower scores indicating better interaction (Cronbach’s α = .93).
The Quality of Patient-Clinician (or interventionist) Communication about End-of-Life Care
(Curtis, Patrick, Caldwell, Greenlee, & Collier, 1999) consists of 4 items to determine the quality of communication. The items ask participants’ perceptions regarding the attitudes and amount of attention given by the clinician (control group) or interventionist (intervention group) and whether they felt their end-of-life wishes were known after a discussion (Cronbach’s α = .90). Items are rated on a 3-point scale from 1 (No) to 3 (Definitely Yes). Because a summed score (ranging from 4 to 12) is used in analyses, it is recommended that all missing values be identified prior to data analyses. There were no missing values among those who completed the present study. Higher scores indicate better interactions.
Semi-structured interview
To obtain further information about how the dyads in the intervention group perceived the SPIRIT intervention, we conducted semi-structured interviews with each member of the dyad at 1 week and 3 months post-intervention. A trained data collector (who was not the interventionist) conducted brief interviews by telephone with the intervention group dyads to explore the acceptability of the intervention. The data collector asked each member of the dyads separately about their experience with the intervention; for example, “Tell me about your experience with the SPIRIT intervention,” “What did you like/dislike about it?”, “What was the most difficult part of participating in the intervention?”, “How would you describe the intervention to other dialysis patients/families?”, and “What suggestions would you like to make for us to improve the intervention?”. Each interview took approximately 10 minutes and was audio-recorded and transcribed.
Outcome Measures
Patient-surrogate congruence in goals of care was assessed using responses on the Goals of Care document wherein two scenarios specific to the patient’s medical condition were presented. Each member of dyad independently chose one of three options: “the goals of care should be focused on delaying my death and thus I want to continue life-sustaining treatment,” “the goals of care should be focused on my comfort and peace, and thus I do not want life-sustaining treatment, including dialysis,” and “I am not sure.” The responses were stratified into continue in both scenarios, mixed, and comfort care only in both scenarios” and compared between patient and surrogate for congruence.
The 13-item Decisional Conflict Scale (Song & Sereika, 2006) was used to assess patient’s level of difficulty in making choices. Patients responded on a 5-point scale from 1 (Strongly Agree) to 5 (Strongly Disagree). A mean of the 13 items was used in analyses, and a score ≥ 2 indicates difficulty in making choices (Cronbach’s α = .91).
The Decision-Making Confidence Scale (Song, et al., in press) was used to measure surrogate’s confidence in decision making. The instrument consists of five items with response options from 0 (Not Confident At All) to 4 (Very Confident), reflecting an individual’s level of comfort in the role of surrogate. A mean of the 5 items was used in analyses (Cronbach’s α = .85).
The 28-item Self-Perception and Relationship Tool (S-PRT) was used to measure psychosocial-spiritual well-being (Atkinson, Wishart, Wasil, & Robinson, 2004). The measure includes three dimensions: intrapersonal, interpersonal, and spiritual well-being. Each item is scored with a 7-point rating scale (+3 to −3) based on how frequently the individual experiences the sentiment presented in the word pairs. For example, “Universal beliefs or a divine presence helps me feel I am”: Nearly Always Comforted (+3) – Nearly Always Troubled (−3). Each dimensional score is a mean score of the corresponding items, and a total score is a mean score of the 28 items (Cronbach’s α = .98). Total scores were used in the analyses.
Other Descriptive Measures
The 30-item Dialysis Symptom Index was used to assess the presence (yes/no) of and distress associated with physical or emotional symptoms experienced during the previous 7 days (Weisbord, et al., 2004). Each item is rated on a 5-point Likert type scale from 1(not at all bothersome) to 5(bothered very much) to assess level of distress of each symptom. A total symptom distress score is calculated by summing distress scores for individual symptoms. Symptoms that are not endorsed by the patient as present are scored zero for distress scores so that those symptoms do not contribute to symptom distress scores.
The SF12v2® Health Survey was used to assess patient’s health-related quality of life (Ware, Kosinski, Turner-Bowker, & Gandek, 2002). The survey includes 2 summary measures, Physical Component Summary (PCS) and Mental Component Summary (MCS). Reported 2-week test-retest reliabilities for PCS and MCS are .89 and .76, respectively (Ware, et al., 2002).
Other descriptive data included age, gender, education, employment status, annual household income, health insurance, and religious preference, the important of religion or spirituality in life on a 4-point scale from 1 (not at all important) to 4 (extremely important), duration of dialysis, and the Charlson Comorbidity Index (CCI; Fried, Bernardini, & Piraino, 2001).
Medical record review
We reviewed medical records of the deceased patients to collect information about the last hospitalization, withdrawal of dialysis or other life-sustaining treatment, length of hospital stay, and location of death.
Semi-structured interview
The purpose of this telephone interview was to assess the surrogate’s experiences with the patient’s last hospitalization and end-of-life decision making. Example questions included in the interview guide were “Tell me about his/her last hospitalization,” “How was the decision made?”, “What helped you make the decision?”, and “How difficult was it for you to make the decision?”. These interviews took 15 – 20 minutes, were audio-recorded and transcribed.
Procedures
Study procedures were approved by the University of Pittsburgh Institutional Review Board. At baseline, each member of the dyad separately completed the descriptive and outcome measures at the dialysis clinic. Immediately after baseline data collection, dyads randomized to the intervention group participated in the SPIRIT intervention. At 1 week and 3 months post-baseline, dyads completed the outcome measures as well as the acceptability surveys over the telephone. The intervention dyads additionally completed the acceptability interview over the telephone. Surrogates received $25 at baseline for transportation. At completion of 1 week and 3 months follow-ups, each member of dyad received $25. After 3 months follow-up, the research staff contacted each dialysis clinic at least every 2 weeks to determine if any of the patients who had agreed to remain on study had been hospitalized. If death occurred at any point after baseline, the research staff reviewed the patient’s medical record and scheduled an interview with the surrogate. A trained data collector conducted a semi-structured interview over the telephone with the surrogate 2 weeks after the patient’s death. Although researchers have chosen various times to interview bereaved families (Gelfman, Meier, & Morrison, 2008; Teno, Clarridge, Casey, Edgman-Levitan, & Fowler, 2001), we chose 2 weeks after the patient’s death because it was a time that balanced respect for the acute grieving period with the need to minimize the effects of time on the surrogate’s recall regarding decision making. In addition, based on the rapport that had been established with surrogates through multiple previous contacts (the intervention and the telephone data collection), telling the story of their experiences with the loved one’s end of life has been shown to be therapeutic (Dyregrov, 2004).
Statistical Analyses
To test immediate and delayed effects of the intervention on patient and surrogate outcomes (i.e., congruence, decisional conflict, decision making confidence and psychosocial-spiritual well-being), changes between T1 (baseline) and T2 (1 week) and between T1 and T3 (3 months) were compared between the two groups using t-tests. Dichotomized variables (e.g., congruence) were analyzed using Fisher’s exact tests. Five (8.6%) of 58 dyads (1 surrogate at 1 week, 2 patients and 2 surrogates at 3 months) had missing data on the outcome variables. For binary variables (e.g., congruence), extreme case analysis approach (Sackett, Richardson, Rosenberg, & Haynes, 1997) was used. For example, dyads lost to the group that fared better were assigned a poor outcome; dyads lost to the group that fared worse were assigned a better outcome. For continuous variables (e.g., decision making confidence), a mean of the two available scores was computed for the missing value. Acceptability measures were analyzed using Mann-Whitney U tests because of not meeting the assumptions for a parametric test.
Analysis of the transcribed interviews
The analysis used basic qualitative description to achieve thematic analysis (Sandelowski, 2001). The initial coding procedure involved line by line examination, labeling, and organizing the textual data into segments (Strauss & Corbin, 1998). The research team developed a coded index of topics addressed in the interviews. Initial coding focused on preserving as much detail as possible in the words of the participants. Codes and definitions were revised by the team and applied to the subsequent interviews. Frequently occurring codes were grouped into fewer categories or general themes. Themes from the acceptability interview were then organized as process or outcome evaluation of the SPIRIT intervention by participant.
Results
Feasibility Evaluation
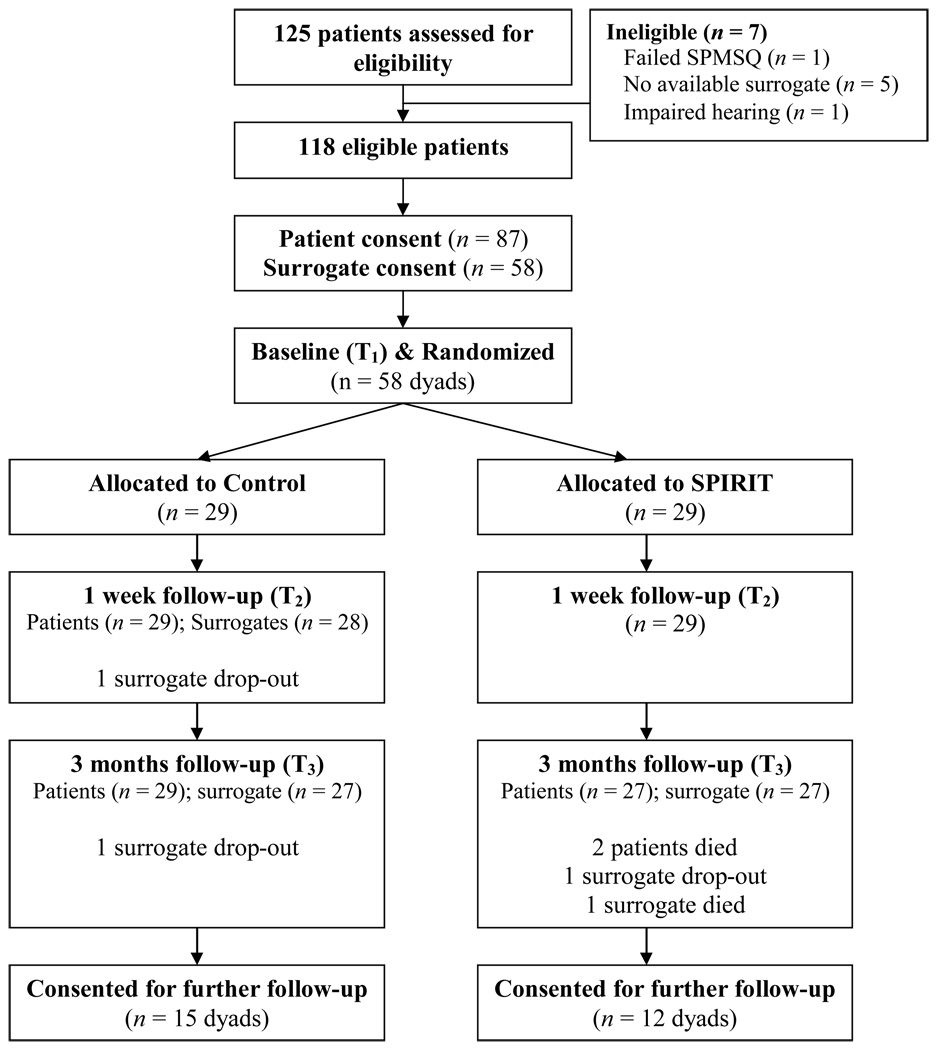
Of the 118 eligible patients, 87 (73.72%) consented; however, only 58 of their chosen surrogates (66.6%) agreed to participate. The most common reasons for patient refusal were “too much going on,” “too tired,” and “not interested in a research study.” Surrogates’ reasons were similar; “interested but can’t find a time” or “having health problems.” Sixteen surrogates verbally agreed initially but never responded to our attempt to schedule an appointment. The progress of the 58 patient-surrogate dyads (116 individuals) that were randomized is presented in Figure 1. The reasons for the surrogates’ withdrawal from the study were marital problems (n = 2) and death (n = 1). The mean and median minutes needed to deliver the SPIRIT sessions were 75.97 (SD = 19.98) and 79, respectively. All but two sessions were accomplished in a single session; there were two occasions where the intervention sessions were interrupted and split into two; one occasion was due to the patient’s fatigue after hemodialysis and one dyad had another appointment that was scheduled too closely to the intervention session. All but the last 8 dyads were invited to remain in the study for further contact; the last 8 were not invited because there was too little time left before the study end date. Twenty-seven dyads (27/50, 54%) agreed.
Figure 1.
Study Participants’ Progress in the Study
Table 2 displays the characteristics of the sample. The patients reported more than 11 bothersome symptoms on average. Their average CCI score was ≥ 6, predicting a mortality rate per patient-year of 27% (Cohen, Moss, Weisbord, & Germain, 2006). The mean PCS of the SF12 revealed our sample to have somewhat worse physical health related quality of life than the 50th percentile for the U.S. kidney disease population of a similar age (44.82), but the mean MCS revealed somewhat higher mental health related quality of life (Ware, et al.). The two groups (intervention and control) did not differ with respect to demographic and clinical characteristics.
Table 2.
Demographic and Clinical Variables at Baseline by Group
| Control (n = 29) n (%) |
SPIRIT (n = 29) n (%) |
|
|---|---|---|
| Patient | ||
| Age, M (SD) | 57.55 (12.2) | 58.31 (11.8) |
| Male | 14 (48.3) | 19 (65.5) |
| Married or living with partner | 14 (48.3) | 8 (27.5) |
| Completed high school | 24 (82.8) | 26 (89.7) |
| Protestant, Religious affiliation | 21 (72.4) | 22 (75.9) |
| Religious involvement | ||
| Frequently or always | 20 (69.0) | 16 (55.2) |
| Importance of spirituality in life | ||
| Extremely important | 20 (69.0) | 16 (55.2) |
| Annual household income | ||
| < $13,000 | 12 (41.4) | 12 (41.4) |
| $13,000 - $29,000 | 9 (31.0) | 8 (27.6) |
| > $29,000 | 8 (27.6) | 9 (31.0) |
| Medicare, Insurance | 24 (82.8) | 22 (75.9) |
| Time on dialysis in year, Median | 2.08 | 2.58 |
| Number of Dialysis symptoms Experiencing, M (SD) | 13.8 (6.4) | 11.8 (6.2) |
| CCI, M (SD) | 6.5 (2.2) | 6.1 (2.1) |
| SF12 PCS, M (SD) | 33.3 (9.8) | 36.6 (10.0) |
| MCS, M (SD) | 48.6 (14.3) | 46.8 (10.4) |
| Surrogate | ||
| Age, M (SD) | 48.9 (12.9) | 49.9 (12.8) |
| Male | 8 (27.6) | 6 (20.7) |
| White | 3 (10.3) | 0 |
| Completed high school | 23 (79.3) | 27 (93.1) |
| Relationship to patient | ||
| Spouse or partner | 10 (34.5) | 8 (27.6) |
| Parent | 5 (17.2) | 6 (20.7) |
| Sibling | 4 (13.8) | 10 (34.5) |
| Child | 3 (10.3) | 1 (3.4) |
| Other relative or frienda | 7 (24.1) | 4 (13.8) |
| Protestant, Religious affiliation | 23 (79.3) | 19 (65.5) |
| Religious involvement | ||
| Frequently or always | 22 (75.9) | 19 (65.5) |
| Importance of spirituality in life | ||
| Extremely important | 24 (82.8) | 22 (75.9) |
CCI: Charlson Comorbidity Index.
including ex-wives, in-laws, grandchildren, and nieces.
Preliminary Intervention Effects
Table 3 presents the outcome variables for the two groups over time. Intervention dyads’ congruence at T2 was significantly improved from baseline (χ2 [1, n = 57] = 4.29, p = .04, odds ratio = 3.30). However, dyads’ congruence at T3 was not significantly improved from baseline (χ2 [1, n = 54] = 2.64, p = .10). Patients’ decisional conflict did not change over time; there were no group differences in changes (T1 - T2 & T1 - T3). Surrogates’ decision making confidence and both patients and surrogates psychosocial-spiritual well-being in the two groups improved over time, but there were no differences between the groups on these measures.
Table 3.
Patient Decisional Conflict and Participant Well-Being over Time by Group.
| T1 |
T2 |
T3 |
|||||
|---|---|---|---|---|---|---|---|
| Variable | Ctrl | SPIRIT | Ctrl | SPIRIT | Ctrl | SPIRIT | |
| Patient Decisional Conflict (1 – 5)a |
M (SD) | 1.98 (.56) | 2.14 (.38) | 2.05 (.44) | 2.12 (.31) | 1.94 (.55) | 1.88 (.37) |
| Patient well- being −3 - +3) |
M (SD) | 1.65 (.91) | 1.37(1.05) | 1.67 (.79) | 1.71 (.76) | 1.95 (.81) | 1.68(1.03) |
| Surrogate well-being |
M (SD) | 1.81(1.16) | 1.47(1.10) | 1.79 (.97) | 1.51 (.90) | 1.84 (.98) | 1.65 (.99) |
Higher scores indicate greater decisional conflict.
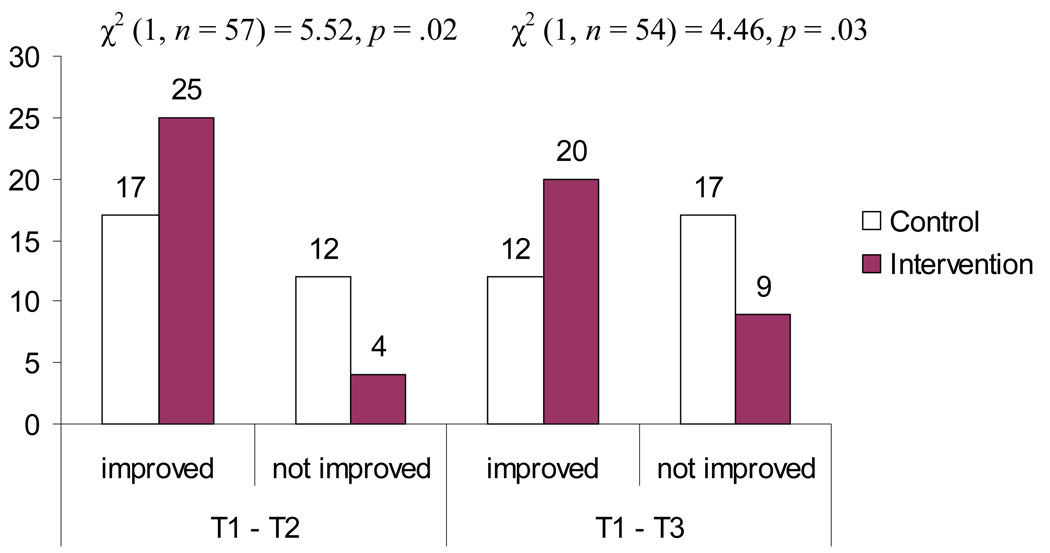
Because surrogates could be highly confident even if they in fact misunderstood patients’ wishes, we examined congruence and surrogates’ decisional confidence jointly as follows. Dyads were categorized as “Improved” if the dyad was congruent based on the responses on the goals of care (either improved from baseline or continued to be congruent) and the surrogate had a decision making confidence score ≥ 3 out of 4. Dyads were categorized as “Not Improved” if the dyad was incongruent (remained incongruent or became incongruent from baseline) and the surrogate had a decision making confidence score ≤ 2. Figure 2 presents the results of the analyses. The number of “Improved” dyads in the two groups significantly differed at T1 - T2 (χ2 [1, n = 57] = 5.52, p = .02, odds ratio = 4.40) and at T1 - T3 (χ2 [1, n = 54] = 4.46, p = .03, odds ratio = 3.17) favoring the SPIRIT intervention group.
Figure 2.
Number of Dyads Who Improved Dyad Congruence and Surrogate Decision Making Confidence by Group
Note. “Improved” included the combination of congruent dyad + confident surrogate (score ≥ 3); “Not Improved” included three combinations, incongruent dyad + unconfident surrogate (score ≤ 2), incongruent dyad + confident surrogate, and congruent dyad + unconfident surrogate.
Acceptability of the SPIRIT Intervention
The analysis of acceptability included only the patients and surrogates who remained in the study at each follow-up (completers analyses; Table 4). The intervention patients’ quality of communication scores were significantly higher than the control group at T2 (U = 283.50, p = .03) and T3 (U = 165.00, p < .01). Similarly, the intervention surrogates’ quality of communication scores were significantly higher than the control group at T2 (U = 95.00, p < .01) and T3 (U = 139.00, p = .03). Compared to control patients, those in the intervention group reported better (lower scores) quality of the interaction during intervention at T2 (U = 180.00, p < U = 183.50, p < .01). Intervention surrogates, compared to control surrogates, reported better (lower scores) quality of the interaction with the interventionist at T2 (U = 139.00, p = .01), but U = 147.50, p = .08).
Table 4.
Comparisons of Acceptability Measures by Group
| T2 | T3 | |||
|---|---|---|---|---|
| Control (M ± SD) |
SPIRIT (M ± SD) |
Control (M ± SD) |
SPIRIT (M ± SD) |
|
|
Quality of Patient-Clinician (or Interventionist) Communication about End- of-Life Care | ||||
| Patient | 8.83 ± 3.55 | 11.18 ± 1.12 | 7.52 ± 3.66 | 11.30 ± 1.41 |
| Surrogate | 6.79 ± 3.57 | 11.68 ± 0.55 | 10.22 ± 2.49 | 11.58 ± 0.72 |
|
Quality of Interaction with Clinician (or Interventionist)a | ||||
| Patient | 7.29 ± 3.42 | 5.56 ± 0.90 | 7.29 ± 2.65 | 5.68 ± 0.77 |
| Surrogate | 7.12 ± 3.39 | 5.39 ± 0.96 | 6.93 ± 3.04 | 5.46 ± 0.59 |
Lower scores indicate better interactions.
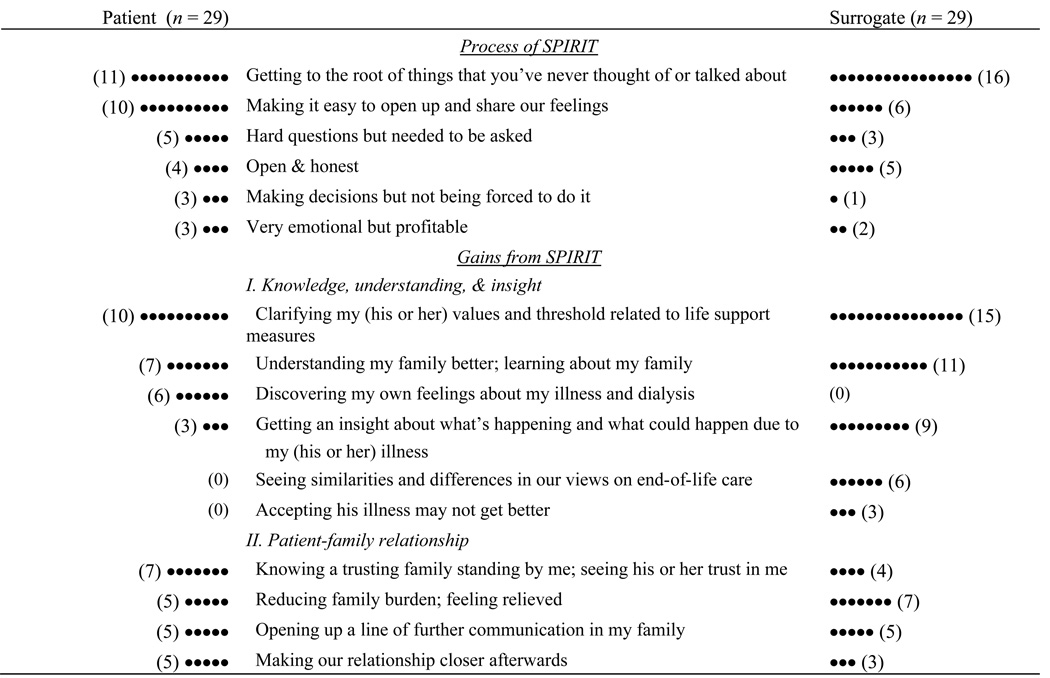
Interview data on participants’ experiences in the intervention process and gains from SPIRIT are summarized in Figure 3 in a stem leaf plot. The following quotation from a surrogate, a brother of a 43-year-old man who had been on hemodialysis for 8 months, represents what most participants reported as one of the gains from SPIRIT:
Figure 3.
Participants’ Experiences with SPIRIT Described During Acceptability Interviews
Note. Each description was counted only once even if the individual mentioned it more than once.
I learned about how his illness affected him and what point and how far he wanted to go to stay alive, which I didn’t know before, he said that he didn’t want dialysis, you know and I, I didn’t know that. Most of that stuff was new. We had touched on it before but we didn’t really discuss it. But, this time it was like, we really got to go into the bottom of it, how he would really feel about, uh, being kept alive, or, you know at what point he would want somebody to intercede. This was just much deeper than anything we’ve discussed.
The most frequently stated learning for the surrogates included: dialysis is a life support measure; patients with ESRD often die from cardiovascular complications, not from kidney failure; the patient had been suffering or struggling with dialysis in silence; and the patient’s values of life support measures differed from the surrogate’s. Most of the feedback about the intervention was highly positive. While 27 patients and 23 surrogates stated that there was no difficulty participating in SPIRIT, 2 patients and 4 surrogates said that facing death and dying was difficult, 2 surrogates said that hearing that the patient’s illness is not going to be cured from the patient was hard. One patient and 1 surrogate mentioned that finding time for the intervention was difficult. Finally, 4 surrogates commented that another subsequent session would be helpful to decide what needs to be done to ensure the patient’s wishes are known to others.
Summary of Deaths during the Study
During the study period, 5 patients died (1 in the control group and 4 in SPIRIT). The control patient’s death, which occurred after 3 months follow-up, was not reviewed because the dyad had not consented for further contact. The remaining patients who had consented for further contact were surviving at the end of study. All 4 of these patients were admitted to the ICU and received mechanical ventilation and other life support measures. Except for Dyad 3, all surrogates made various difficult end-of-life decisions for their loved ones. These 3 surrogates repeatedly expressed how beneficial it was to have had the intervention before their loved ones’ deaths. For example, although Dyad 4 appeared to have been prepared for the patient’s death before the SPIRIT intervention, the interview with the patient’s niece illustrates how the SPIRIT helped her in making those decisions:
I thought we had previously discussed EVERYTHING. But until we had that interview at the dialysis clinic, we never discussed how far you want them to go medically and how you would feel about that… So, I was really glad that we had the discussion. I knew what she honestly felt and tried to follow whatever she wanted. So … I told them, you know, I really would appreciate if you would make her comfortable and leave her alone. So, they gave her some medication to make her comfortable …
Discussion
The goal of the SPIRIT intervention tested in this study was to promote cognitive and emotional preparation for future crises that African Americans with ESRD and their chosen surrogate decision makers may face near end-of-life. We demonstrated that SPIRIT was effective in improving dyad congruence regarding goals of care and surrogate decision making confidence over time and that SPIRIT was well received by this sample of African Americans. Furthermore, data from the post-intervention and after-death interviews enhance our understanding of what they valued most about the intervention.
Some facets of SPIRIT should be highlighted. Each element of the intervention was designed to enhance exchanges of experiences with illness and values between the patient and chosen surrogate. During this process, the patient discovered his or her own representations about illness and dialysis and examined threshold/conditions for life support measures. At the same time, the surrogate gained understanding of the patient’s illness experience and began to see his or her limited life expectancy. The surrogate also validated similarities or differences with the patient regarding life support measures and examined his or her ability to follow through with the patient’s wishes. The interventionist invested significant time and effort during early steps of SPIRIT to establish a foundation for the all parties to see the relevance of and need for discussing end-of-life issues. Exploring the dyad’s representations of illness prepared the dyad for transitioning to more difficult topics of end-of-life care in later steps. Nearly every intervention dyad characterized their experiences with SPIRIT as open, honest, relieving, unrushed, unforced, and enlightening.
Researchers have demonstrated that patient and family emotions are fundamentally related to their experiences at end-of-life and communication with clinicians (Braun, et al., 2008; Cohen, Germain, Woods, Mirot, & Burleson, 2005; Moss, 1998). Our findings suggest the element that the intervention dyads most valued was the opportunity to share their emotions and beliefs about illness and end-of-life. This process should be considered critical in preparing patients and their families for end-of-life decision making (Braun, et al.). However, the importance of such an emotional preparation has not been fully appreciated by clinicians (Hebert, Schulz, Copeland, & Arnold, 2009).
In general, intervention patients’ choices as expressed in the Goals of Care document did not shift from T2 (1 week) to T3 (3 months). This result is consistent with previous studies demonstrating that end-of-life treatment preferences when they are elicited based on the patient’s values tend to be stable over time (Danis, Garrett, Harris, & Patrick, 1994; Ditto, et al., 2003; Wittink, et al., 2008). Such consistency is particularly true of dialysis patients (Pruchno, Rovine, Cartwright, & Wilson-Genderson, 2008).
The considerable heterogeneity in surrogate selection in this study should be noted. Previous studies of surrogate decision making have primarily focused on spouses (Ditto, et al., 2001; Hopp, 2000; Pruchno, et al., 2006; Uhlmann, et al., 1988). However, the selection of surrogates can be influenced by personal experiences, familial structures, or culture and may not be consistent with the order of the hierarchical compensatory model, which proposes most adults would turn first to their spouse, followed by their children and other relatives for receiving assistance from others (Carr & Khodyakov, 2007b; Noelker & Bass, 1994). Clinicians and future studies should be aware that patients’ preferences in surrogate selection may vary and the hierarchy may not represent the patient’s best interest or wishes.
It may appear time consuming for clinicians to conduct all SPIRIT steps at once, but it could perhaps be implemented over time. The steps of SPIRIT are explicit and may be carried out in dialysis units by nurses or social workers after appropriate training. The major barrier for surrogates was time. However, we feel that this barrier can be overcome outside a study setting in which patients and family members are familiar and comfortable with the dialysis unit staff. Clinicians must recognize the complexity of communicating effectively and appropriately about end-of-life care, which requires time investment and coordination. Future studies should test the efficacy of SPIRIT in a larger sample and its effects when implemented in practice.
Study limitations include the relatively small number of dyads studied; however, the sample size was determined based on the feasibility. We believe that the recruitment and retention was successful considering the triple challenge of recruiting patients with serious illness, who are African American and who have a surrogate willing to join the study. Another limitation is that the lack of intervention effect on decisional conflict could be due to a need for more than a one-time intervention. Because only a small number of deaths occurred during the study, we were unable to examine surrogates’ experiences during the time of actual end-of-life decision making. Finally, the lack of intervention effect on psychosocial-spiritual well-being could suggest the need for further evaluation of the instrument’s validity when used with African American samples. Its lack of variability and high baseline scores might have resulted in ceiling effects and limited sensitivity to change over time.
In summary, we found SPIRIT to promote communication between African American dialysis patients and their chosen surrogates was effective and well received. A subsequent session may help patients and their surrogates make practical plans to communicate patients’ wishes with others (e.g., other family members, spiritual advisors, and healthcare providers). Our findings from the 4 patient deaths suggest further tests of SPIRIT to examine its efficacy in reducing surrogate difficulties in end-of-life decision making and potential benefits on bereavement.
Acknowledgement
Support and Financial Disclosure Declaration
Supported by NIH, NINR Grant No. 1R21NR009662 (M. Song)
The authors sincerely thank the medical directors, administrators, social workers, and nursing staff at the participating dialysis clinics who provided significant supports in participant recruitment.
References
- Atkinson MJ, Wishart PM, Wasil BI, Robinson JW. The Self-Perception and Relationships Tool (S-PRT): A novel approach to the measurement of subjective health-related quality of life. Health and Quality Life Outcomes. 2004;2(1):36–50. doi: 10.1186/1477-7525-2-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer JS, Ball SA, Campbell BK, Miele GM, Schoener EP, Tracy K. Training and fidelity monitoring of behavioral interventions in multi-site addictions research. Drug & Alcohol Dependence. 2007;87(2–3):107–118. doi: 10.1016/j.drugalcdep.2006.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blank RH, Merrick JC. End-of-life decision making: A cross-national study. Cambridge, MA: The MIT Press; 2005. [Google Scholar]
- Braun UK, Beyth RJ, Ford ME, McCullough LB. Voices of African American, Caucasian, and Hispanic surrogates on the burdens of end-of-life decision making. Journal of General Internal Medicine. 2008;23(3):267–274. doi: 10.1007/s11606-007-0487-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr D, Khodyakov D. End-of-life health care planning among young-old adults: An assessment of psychosocial influences. Journal of Gerontology. 2007a;62(2):S135–S141. doi: 10.1093/geronb/62.2.s135. [DOI] [PubMed] [Google Scholar]
- Carr D, Khodyakov D. Health care proxies: Whom do young old adults choose and why? Journal of Health and Social behavior. 2007b;48(2):180–194. doi: 10.1177/002214650704800206. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Sifry RL, Nuro KF, Frankforter TL, Ball SA, et al. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug & Alcohol Dependence. 2000;57(3):225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- Cherlin E, Fried T, Prigerson HG, Schulman-Green D, Johnson-Hurzeler R, Bradley EH. Communication between physicians and family caregivers about care at the end of life: When do discussions occur and what is said? Journal of Palliative Medicine. 2005;8(6):1176–1185. doi: 10.1089/jpm.2005.8.1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen LM, Germain MJ, Woods AL, Mirot A, Burleson JA. The family perspective of ESRD deaths. American Journal of Kidney Disease. 2005;45(1):154–161. doi: 10.1053/j.ajkd.2004.09.014. [DOI] [PubMed] [Google Scholar]
- Cohen LM, Moss AH, Weisbord SD, Germain MJ. Renal palliative care. Journal of Palliative Medicine. 2006;9(4):977–992. doi: 10.1089/jpm.2006.9.977. [DOI] [PubMed] [Google Scholar]
- Covinsky KE, Fuller JD, Yaffe K, Johnston CB, Hamel MB, Lynn J, et al. Communication and decision-making in seriously ill patients: Findings of the SUPPORT project. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Journal of the American Geriatrics Society. 2000;48(5Suppl):S187–S193. doi: 10.1111/j.1532-5415.2000.tb03131.x. [DOI] [PubMed] [Google Scholar]
- Curtis JR, Patrick DL, Caldwell E, Greenlee H, Collier AC. The quality of patient-doctor communication about end-of-life care: A study of patients with advanced AIDS and their primary care clinicians. AIDS. 1999;13(9):1123–1131. doi: 10.1097/00002030-199906180-00017. [DOI] [PubMed] [Google Scholar]
- Danis M, Garrett J, Harris R, Patrick DL. Stability of choices about life-sustaining treatments. Annals of Internal Medicine. 1994;120(7):567–573. doi: 10.7326/0003-4819-120-7-199404010-00006. [DOI] [PubMed] [Google Scholar]
- Ditto PH, Danks JH, Smucker WD, Bookwala J, Coppola KM, Dresser R, et al. Advance directives as acts of communication: A randomized controlled trial. Archives of Internal Medicine. 2001;161(3):421–430. doi: 10.1001/archinte.161.3.421. [DOI] [PubMed] [Google Scholar]
- Ditto PH, Smucker WD, Danks JH, Jacobson JA, Houts RM, Fagerlin A, et al. Stability of older adults' preferences for life-sustaining medical treatment. Health Psychology. 2003;22(6):605–615. doi: 10.1037/0278-6133.22.6.605. [DOI] [PubMed] [Google Scholar]
- Donovan HS, Ward S. A representational approach to patient education. Journal of Nursing Scholarship. 2001;33(3):211–216. doi: 10.1111/j.1547-5069.2001.00211.x. [DOI] [PubMed] [Google Scholar]
- Donovan HS, Ward SE, Song MK, Heidrich SM, Gunnarsdottir S, Phillips CM. An update on the representational approach to patient education. Journal of Nursing Scholarship. 2007;39(3):259–265. doi: 10.1111/j.1547-5069.2007.00178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumas JE, Lynch AM, Laughlin JE, Phillips SE, Prinz RJ. Promoting intervention fidelity. Conceptual issues, methods, and preliminary results from the EARLY ALLIANCE prevention trial. American Journal of Preventive Medicine. 2001;20(1 Suppl):38–47. doi: 10.1016/s0749-3797(00)00272-5. [DOI] [PubMed] [Google Scholar]
- Dyregrov K. Bereaved parents' experience of research participation. Social Science & Medicine. 2004;58(2):391–400. doi: 10.1016/s0277-9536(03)00205-3. [DOI] [PubMed] [Google Scholar]
- Fagerlin A, Schneider CE. Enough. The failure of the living will. Hastings Center Report. 2004;34(2):30–42. [PubMed] [Google Scholar]
- Fried L, Bernardini J, Piraino B. Charlson comorbidity index as a predictor of outcomes in incident peritoneal dialysis patients. American Journal of Kidney Disease. 2001;37(2):337–342. doi: 10.1053/ajkd.2001.21300. [DOI] [PubMed] [Google Scholar]
- Gelfman LP, Meier DE, Morrison RS. Does palliative care improve quality? A survey of bereaved family members. Journal of Pain and Symptom Management. 2008;36(1):22–28. doi: 10.1016/j.jpainsymman.2007.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammes BJ, Briggs L. La Crosse, WI: Gundersen Lutheran Medical Foundation; 2000. Respecting choices: Advance care planning facilitator manual. [Google Scholar]
- Hebert RS, Schulz R, Copeland VC, Arnold RM. Preparing family caregivers for death and bereavement. Insights from caregivers of terminally ill patients. Journal of Pain and Symptom Management. 2009;37(1):3–12. doi: 10.1016/j.jpainsymman.2007.12.010. [DOI] [PubMed] [Google Scholar]
- Hewson M. Patient education through teaching for conceptual change. Journal of General Internal Medicine. 1993;8(7):393–398. doi: 10.1007/BF02600081. [DOI] [PubMed] [Google Scholar]
- Hickman SE, Sabatino CP, Moss AH, Nester JW. The POLST (Physician Orders for Life-Sustaining Treatment) paradigm to improve end-of-life care: Potential state legal barriers to implementation. Journal of Law, Medicine, and Ethics. 2008;36(1):119–140. doi: 10.1111/j.1748-720X.2008.00242.x. [DOI] [PubMed] [Google Scholar]
- Hines SC, Glover JJ, Holley JL, Babrow AS, Badzek LA, Moss AH. Dialysis patients' preferences for family-based advance care planning. Annals of Internal Medicine. 1999;130(10):825–828. doi: 10.7326/0003-4819-130-10-199905180-00016. [DOI] [PubMed] [Google Scholar]
- Hopp FP. Preferences for surrogate decision makers, informal communication, and advance directives among community-dwelling elders: Results from a national study. Gerontologist. 2000;40(4):449–457. doi: 10.1093/geront/40.4.449. [DOI] [PubMed] [Google Scholar]
- Hopp FP, Duffy SA. Racial variations in end-of-life care. Journal of American Geriatric Society. 2000;48(6):658–663. doi: 10.1111/j.1532-5415.2000.tb04724.x. [DOI] [PubMed] [Google Scholar]
- Houts RM, Smucker WD, Jacobson JA, Ditto PH, Danks JH. Predicting elderly outpatients' life-sustaining treatment preferences over time: The majority rules. Medical Decision Making. 2002;22(1):39–52. doi: 10.1177/0272989X0202200104. [DOI] [PubMed] [Google Scholar]
- Leventhal H, Diefenback M. The active side of illness cognition. In: Skelton JA, Croyle RT, editors. Mental representation in health and illness. New York, NY: Spinger-Verlag; 1991. pp. 245–271. [Google Scholar]
- Leventhal H, Nerenz D, Steele DS. Illness representations and coping with health threats. In: Baum A, Singer JE, editors. Handbook of psychology and health. Vol. IV. New York, NY: Erlbaum; 1984. pp. 221–252. [Google Scholar]
- McKinley ED, Garrett JM, Evans AT, Danis M. Differences in end-of-life decision making among black and white ambulatory cancer patients. Journal of General Internal Medicine. 1996;11(11):651–656. doi: 10.1007/BF02600155. [DOI] [PubMed] [Google Scholar]
- Miller WR, Moyers TB, Arciniega L, Ernst D, Forcehimes A. Training, supervision and quality monitoring of the COMBINE Study behavioral interventions. Journal of Studies on Alcohol. 2005;(Suppl 15):188–195. doi: 10.15288/jsas.2005.s15.188. [DOI] [PubMed] [Google Scholar]
- Morrison RS, Zayas LH, Mulvihill M, Baskin SA, Meier DE. Barriers to completion of healthcare proxy forms: A qualitative analysis of ethnic differences. Journal of Clinical Ethics. 1998;9(2):118–126. [PubMed] [Google Scholar]
- Moss AH. ‘At least we do not feel guilty’: Managing conflict with families over dialysis discontinuation. American Journal of Kidney Disease. 1998;31(5):868–883. doi: 10.1016/s0272-6386(98)70061-7. [DOI] [PubMed] [Google Scholar]
- Noelker L, Bass D. Relationships between the frail elderly’s informal and formal helpers. In: Kahana E, Beigel DE, Wykle M, editors. Family caregiving across the lifespan. Thousand Oaks, CA: Sage; 1994. pp. 356–385. [Google Scholar]
- Paterson BL. The shifting perspectives model of chronic illness. Journal of Nursing Scholarship. 2001;33(1):21–26. doi: 10.1111/j.1547-5069.2001.00021.x. [DOI] [PubMed] [Google Scholar]
- Perkins HS. Controlling death: The false promise of advance directives. Annals of Internal Medicine. 2007;147(1):51–57. doi: 10.7326/0003-4819-147-1-200707030-00008. [DOI] [PubMed] [Google Scholar]
- Perry E, Swartz J, Brown S, Smith D, Kelly G, Swartz R. Peer mentoring: A culturally sensitive approach to end-of-life planning for long-term dialysis patients. American Journal of Kidney Disease. 2005;46(1):111–119. doi: 10.1053/j.ajkd.2005.03.018. [DOI] [PubMed] [Google Scholar]
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of American Geriatric Society. 1975;23(10):433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Pocock SJ. Allocation of patients to treatment in clinical trials. Biometrics. 1979;35(1):183–197. [PubMed] [Google Scholar]
- Pruchno RA, Lemay EP, Jr, Feild L, Levinsky NG. Spouse as health care proxy for dialysis patients: whose preferences matter? Gerontologist. 2005;45(6):812–819. doi: 10.1093/geront/45.6.812. [DOI] [PubMed] [Google Scholar]
- Pruchno RA, Lemay EP, Jr, Feild L, Levinsky NG. Predictors of patient treatment preferences and spouse substituted judgments: The case of dialysis continuation. Medical Decision Making. 2006;26(2):112–121. doi: 10.1177/0272989X06286482. [DOI] [PubMed] [Google Scholar]
- Pruchno RA, Rovine MJ, Cartwright F, Wilson-Genderson M. Stability and change in patient preferences and spouse substituted judgments regarding dialysis continuation. Journal of Gerontology. 2008;63(2):S81–S91. doi: 10.1093/geronb/63.2.s81. [DOI] [PubMed] [Google Scholar]
- Renal Physicians Association and American Society of Nephrology. Shared decision-making in the appropriate initiation of and withdrawal from dialysis: Clinical practice guideline No.2. Washington, D.C: Renal Physicians Association; 2000. [DOI] [PubMed] [Google Scholar]
- Rudy EB, Vaska PL, Daly BJ, Happ MB, Shiao P. Permuted block design for randomization in a nursing clinical trial. Nursing Research. 1993;42(5):287–289. [PubMed] [Google Scholar]
- Sackett DL, Richardson WS, Rosenberg WS, Haynes RB. Evidence-based medicine. New York, NY: Churchill Livingstone; 1997. [Google Scholar]
- Saha S, Arbelaez JJ, Cooper LA. Patient-physician relationships and racial disparities in the quality of health care. American Journal of Public Health. 2003;93(10):1713–1719. doi: 10.2105/ajph.93.10.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandelowski M. Real qualitative researchers do not count: The use of numbers in qualitative research. Research in Nursing & Health. 2001;24(3):230–240. doi: 10.1002/nur.1025. [DOI] [PubMed] [Google Scholar]
- Song M, Donovan H, Piraino B, Choi J, Bernardini J, Verosky D, et al. Effects of an intervention to improve communication about end-of-life care among African Americans with chronic kidney disease: A pilot study. Applied Nursing Research. doi: 10.1016/j.apnr.2008.05.002. in press. [DOI] [PubMed] [Google Scholar]
- Song MK, Kirchhoff KT, Douglas J, Ward S, Hammes BJ. A randomized, controlled trial to improve advance care planning among patients undergoing cardiac surgery. Medical Care. 2005;43(10):1049–1053. doi: 10.1097/01.mlr.0000178192.10283.b4. [DOI] [PubMed] [Google Scholar]
- Song MK, Sereika SM. An evaluation of the Decisional Conflict Scale for measuring the quality of end-of-life decision making. Patient Education and Counseling. 2006;61(3):397–404. doi: 10.1016/j.pec.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Strauss A, Corbin J. Basics of qualitative research: Techniques and procedures for developing grounded theory. 2nd ed. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Sulmasy DP, Haller K, Terry PB. More talk, less paper: Predicting the accuracy of substituted judgments. American Journal of Medicine. 1994;96(5):432–438. doi: 10.1016/0002-9343(94)90170-8. [DOI] [PubMed] [Google Scholar]
- Teno JM, Clarridge B, Casey V, Edgman-Levitan S, Fowler J. Validation of Toolkit After-Death Bereaved Family Member Interview. Journal of Pain and Symptom Management. 2001;22(3):752–758. doi: 10.1016/s0885-3924(01)00331-1. [DOI] [PubMed] [Google Scholar]
- Tulsky JA. Beyond advance directives: Importance of communication skills at the end of life. JAMA. 2005;294(3):359–365. doi: 10.1001/jama.294.3.359. [DOI] [PubMed] [Google Scholar]
- Tulsky JA, Chesney MA, Lo B. How do medical residents discuss resuscitation with patients? Journal of General Internal Medicine. 1995;10(8):436–442. doi: 10.1007/BF02599915. [DOI] [PubMed] [Google Scholar]
- U.S. Renal Data System. Annual data report: Atlas of end-stage renal disease in the United States. Vol. 2007. Bethesda, MD: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2007. USRDS 2007. [Google Scholar]
- Uhlmann RF, Pearlman RA, Cain KC. Physicians' and spouses' predictions of elderly patients' resuscitation preferences. Journal of Gerontology. 1988;43(5):M115–M121. doi: 10.1093/geronj/43.5.m115. [DOI] [PubMed] [Google Scholar]
- Ware J, Jr, Kosinski M, Turner-Bowker DM, Gandek B. How to score version 2 of the SF-12 Health Survey (with a supplement documenting version 1) Lincon, RI: QualityMetric Inc; 2002. [Google Scholar]
- Weisbord SD, Fried LF, Arnold RM, Rotondi AJ, Fine MJ, Levenson DJ, et al. Development of a symptom assessment instrument for chronic hemodialysis patients: the Dialysis Symptom Index. Journal of Pain and Symptom Management. 2004;27(3):226–240. doi: 10.1016/j.jpainsymman.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Wittink MN, Morales KH, Meoni LA, Ford DE, Wang NY, Kalg MJ, et al. Stability of preferences for end-of-life treatment after 3 years of follow-up. Archives of Internal Medicine. 2008;168(19):2125–2130. doi: 10.1001/archinte.168.19.2125. [DOI] [PMC free article] [PubMed] [Google Scholar]