Abstract
The primary purpose of this survey was to assess the interest and concerns of a group of cancer complementary and alternative medicine (CAM) practitioners regarding CAM research issues. These issues include the CAM modalities used most often by CAM practitioners in the treatment of cancer patients, cancer CAM practitioners’ perceptions of the most promising areas of cancer CAM research, the perceived obstacles to carrying out research objectives in the emerging field of cancer CAM research, the extent of awareness of the National Cancer Institute (NCI) Best Case Series Program, and CAM practitioners’ level of interest in research collaboration with CAM researchers. A cross-sectional survey of a convenience sample of cancer CAM practitioners was conducted. One hundred thirty-four respondents completed the survey. About 72% of the respondents were involved in the care of cancer patients, and these were considered the informative respondents. All results were from the informative respondent group. Respondent practitioners provided care using interventions from all seven of the predefined CAM categories. This care was provided to improve both quality of life and survival. Over two-thirds of the respondents rated research in pharmacologic and biologic treatments, alternative medical systems and nutritional therapeutics for cancer treatment, and symptom/side-effect management as high-priority areas. Although no single obstacle to research predominated as the most significant, the most frequently encountered obstacle was lack of awareness of appropriate funding sources (75.4%). More than 83% of respondents expressed some interest in or willingness to establish research collaboration with a cancer researcher. The results from this survey indicate that many cancer CAM practitioners have shared interests, perceived obstacles, and desired research opportunities. Despite a small sample size and lack of a feasible process for random sampling, this survey highlights avenues to promote and support collaborative research. The NCI/Office of Cancer Complementary and Alternative Medicine will continue to respond to the concerns elucidated by the survey by developing strategies for future program opportunities within the NCI.
Keywords: cancer complementary and alternative medicine practitioners, complementary and alternative medicine (CAM), practitioner survey
The Office of Cancer Complementary and Alternative Medicine (OCCAM) was established to coordinate and enhance the National Cancer Institute’s (NCI) activities in the arena of complementary and alternative medicine (CAM). OCCAM’s goals are to increase the amount of high-quality information and research on the use of CAM and CAM-related approaches for the diagnosis, prevention, and treatment of cancer and cancer-related symptoms; furthermore, OCCAM provides NCI with an interface to the general public, health practitioner, and research communities regarding cancer CAM issues.
To further these goals, OCCAM staff designed and commissioned the conduct of two surveys, one of cancer researchers with an interest in CAM research and the other of CAM practitioners. Through the surveys, we sought to assess the interest and concerns of practitioners and researchers regarding research opportunities of various CAM approaches to the care of cancer patients. This information would be used to inform new program development and implementation. The results of the survey of researchers have been previously reported.1 This article focuses on the results of the survey of CAM practitioners. Both surveys were conducted by Westat of Rockville, Maryland, through a subcontract from Matthews Media Group.
The main research questions guiding the practitioner study were as follows:
What CAM modalities are used most often by CAM practitioners in the treatment of cancer patients?
What are perceived as the most promising areas of cancer CAM research?
What are the perceived obstacles to conducting CAM research?
To what extent are CAM practitioners aware of the NCI Best Case Series (BCS) Program?
To what extent are practitioners interested in partnering with CAM researchers to evaluate CAM?
Methods
Respondents
The population of CAM practitioners is diverse and possesses little cohesiveness or cross-disciplinary organizing structure. Consequently, it was not feasible to comprehensively identify members of this group and generate a random sample for participation in the survey. Therefore, we identified several sources of potential respondents, defined as those individuals who met any of the following criteria:
OCCAM contacts from the NCI BCS Program
Practitioners who advertise cancer therapies in CAM periodicals
Authors of cancer CAM literature
This process identified 374 potential respondents, identified in the order of the criteria listed above. All persons on the list were included in the survey; as such, no sampling was conducted.
Survey Questionnaire
For the purpose of this survey, cancer CAM research was defined to include scientific investigations across a variety of fields. These included alternative medical systems, energy therapies, manipulative and body-based methods, mind-body interventions, movement therapies and unconventional physical therapies, nutritional therapeutics, and pharmacologic and biologic treatments. The CAM fields were the same as those used in the survey of cancer researchers.1
The survey questionnaire was created by OCCAM staff with support from Westat. It was pilot-tested with three practitioners, who received a participation incentive of $50 (US). In addition to completing the survey, the pilot practitioners completed a form on which they indicated any questions they found difficult to answer. Furthermore, they were asked to specify the reason for the difficulty, terms that should have been defined, and any other comments or suggestions regarding the survey. In follow-up telephone calls, they were asked to describe the thought process they used to understand survey instructions, interpret survey items, and select survey responses. The survey was then revised based on their answers. The final version of the survey consisted of 39 questions and took approximately 30 minutes to complete. Approval of the survey was obtained from the Office of Management and Budget through NCI’s Office of Communication’s existing pretest and formative research clearance.
Data Collection
When an e-mail address was available for a potential respondent, the survey was sent as an attachment to a message with the instruction to return the completed survey by toll-free fax. Alternatively, the survey was sent via postal mail with a postage-paid return envelope and instructions for returning the survey form by toll-free fax. For both delivery methods, a cover letter from the OCCAM director (J.D.W.), which described the purpose of the study, accompanied the survey. The letter also indicated that the identity of the respondents would be kept confidential and not disclosed, except as required by law. Furthermore, identifying information would be kept in a separate database from survey responses, not allowing for an association.
Respondents were asked to return their survey forms within 2 weeks of receipt. To encourage a high response rate and prompt return of the surveys, respondents were offered an incentive of $25. All postmaster returns designated as undeliverable were processed, and tracings were conducted for these cases. Surveys were remailed by postal service to potential respondents for whom an “undeliverable” e-mail message was received and to those for whom a current address was obtained through tracing. One week after the questionnaires were sent by e-mail, a prompt was e-mailed to all non-respondents. Nonrespondents in the postal mail group were prompted by telephone 2 weeks after the mailing. One week after the prompts, experienced telephone interviewers attempted to contact all non-respondents by telephone and offered to fax or mail another survey form or administer the survey by telephone.
Interviewers received 3 hours of training on administering the survey prior to beginning telephone follow-up. A maximum of 12 telephone prompts were made. Interviewers also called respondents to retrieve key data items that were missing or unclear. No additional follow-up was done for persons who declined to complete the survey when contacted by telephone. Data collection occurred over a 4-month period in 2004.
The survey was designed such that in the beginning, the respondent was asked some questions about his or her background and practice. If the respondent either did not self-identify as a CAM practitioner or did not provide care to cancer patients, he or she was deemed to be a noninformative respondent and thus was shunted to the end of the survey without answering the remaining questions. Therefore, all of the presented data are from informative respondents.
Response Rate
Of the 374 potential respondents, 21 were ineligible because they were deceased, retired, or not located in the United States. Of the 353 practitioners on the adjusted list, completed surveys were received from 134 (38%). Seventy-four potential respondents could not be located, and 103 received the maximum number of telephone calls. When these two groups were excluded from the calculation, the response rate was 76.1%. Since no information was known about the non-respondents, weighting to adjust for nonresponse was not possible.
Results
Demographics
About two-thirds (67.0%) of the practitioners responding to the survey were male. Educational degrees held by at least 5% of the practitioners are shown in Table 1. More than half (53.2%) of the respondents held MD degrees, and about one-fifth (19.2%) held PhDs. Although 42.6% of respondents reported that they had a bachelor’s degree, this percentage is probably low since most people with MD or PhD degrees also have a bachelor’s degree.
Table 1.
Practitioners Holding Various Degrees (%)
| Degree | % of Practitioners |
|---|---|
| Medical doctor (MD) | 53.2 |
| Bachelor of arts/bachelor of science (BA/BS) | 42.6 |
| Master of arts/master of science (MA/MS) | 20.2 |
| Doctor of philosophy (PhD) | 19.2 |
| Naturopathic doctor (ND) | 12.8 |
| Oriental medical doctor/doctor of oriental medicine (OMD/DOM) | 8.5 |
Certificates or licenses relating to CAM practice held by practitioners are shown in Table 2. The most frequently held license was licensed acupuncturist (LAc), held by 18.1% of the practitioners. All of the other certificates listed on the survey were held by less than 10% of the respondents. Additional certificates were named by 41.5% of the respondents. Although the exact name of most of these other certificates varied, the areas in which three or more practitioners had certificates were naturopathy, homeopathy, acupuncture, holistic medicine, herbal medicine, and chelation.
Table 2.
Practitioners Holding Various Certificates or Licenses Relating to CAM Practice (%)
| Certificate/License | % of Practitioners |
|---|---|
| Licensed acupuncturist (LAc) | 18.1 |
| Certified nutritional consultant (CNC) | 7.5 |
| Certified hypnotherapist/certified medical hypnotherapist (CHt/CMHt) | 5.3 |
| Certified massage therapist | 3.2 |
| Certified healing touch practitioner | 2.1 |
| Other | 41.5 |
CAM = complementary and alternative medicine.
Patient Care
There were 134 respondents; 96 (72%) of the respondents were involved in the care of cancer patients. Of these 96, 27% cared for 1 to 10 cancer patients per year, 36% cared for 11 to 50, 11% cared for 51 to 100 patients, and another 25% cared for more than 100 cancer patients per year. Ninety-eight percent of the respondents reported that they provided CAM for their cancer patients and/or referred their cancer patients to other health care providers for CAM treatments.
Referral Practices
Practitioners were asked about the location of other health care providers to whom they referred either some or all of their cancer patients for CAM treatment. Forty-four percent made referrals both within and outside their practice, and another 34% made referrals solely outside of their practice. Finally, 5.3% of the respondents did not make any referrals to other health care providers for CAM treatment (Table 3). The survey specifically addressed the question of the various modalities of CAM treatment that the practitioner either provided or referred his patients to. More specifically, for each CAM modality, it was asked whether the practitioner was either providing or referring for the purpose of improvement of quality of life or increased survival. For each CAM modality, the percentage of practitioners providing it for each purpose was similar (Table 4). For example, nutritional therapeutics was provided by 84.0% of the practitioners for the purpose of improving quality of life and by 83.0% for increasing survival; however, the types of CAM provided by the practitioners showed considerable variation. Nutritional therapeutics (84.0%) and alternative medical systems (68.1%) were prescribed most frequently. Movement and unconventional physical therapies (22.3%) and manipulative and body-based methods (27.7%) were prescribed the least frequently for improving quality of life.
Table 3.
Location of Other Health Care Professionals to Whom Practitioners Referred Some or All of Their Cancer Patients for CAM Treatment
| Location of Other Health Care Professionals | % of Practitioners |
|---|---|
| Both within and outside their practice | 43.6 |
| Outside their practice | 34.0 |
| Within their practice | 5.3 |
| Do not make referrals for CAM treatment | 5.3 |
| Not ascertained | 11.7 |
CAM = complementary and alternative medicine.
Table 4.
Practitioners Providing and Making Referrals for Various CAM Treatment Categories for the Purposes of Improving Quality of Life and Increasing Survival (%)
| Provide | Refer | |||
|---|---|---|---|---|
| CAM Treatment Category | Improving Quality of Life | Increasing Survival | Improving Quality of Life | Increasing Survival |
| Alternative medical systems (and some specific components) | 68.1 | 63.8 | 51.1 | 40.4 |
| Energy therapies | 41.5 | 37.2 | 44.7 | 36.2 |
| Manipulative and body-based methods | 27.7 | 23.4 | 58.5 | 43.6 |
| Mind-body interventions | 61.7 | 57.5 | 55.3 | 45.7 |
| Movement therapies and unconventional physical therapies | 22.3 | 22.3 | 43.6 | 36.2 |
| Nutritional therapeutics | 84.0 | 83.0 | 42.6 | 45.7 |
| Pharmacologic and biologic treatments | 57.5 | 57.5 | 46.8 | 45.7 |
CAM = complementary and alternative medicine.
A somewhat different pattern emerged for referrals. For most modalities of CAM, more practitioners made referrals for the purpose of improving quality of life than for increasing survival. At the same time, there was less variation in the distribution across the CAM modalities with respect to referrals. This included referrals for purposes of increased survival, as well as improving quality of life. The percentage of practitioners making referrals to other health practitioners for the purposes of improved quality of life ranged from 42.6% for nutritional therapeutics to 58.5% for manipulative and body-based methods, with the other CAM modalities lying within this range.
The types of CAM treatments that the practitioners provided themselves differed from the types for which they made referrals. For example, although about one-fourth of the practitioners provided manipulative or body-based methods for improving quality of life (27.7%) or increasing survival (23.4%), they were more apt to make referrals for this type of treatment, with almost three-fifths (58.5%) making referrals for improving the quality of life. On the other hand, more than four-fifths of the practitioners provided nutritional therapeutics for improving the quality of life (84.0%) and increasing survival (83.0%) and were less likely to make referrals for this type of CAM treatment.
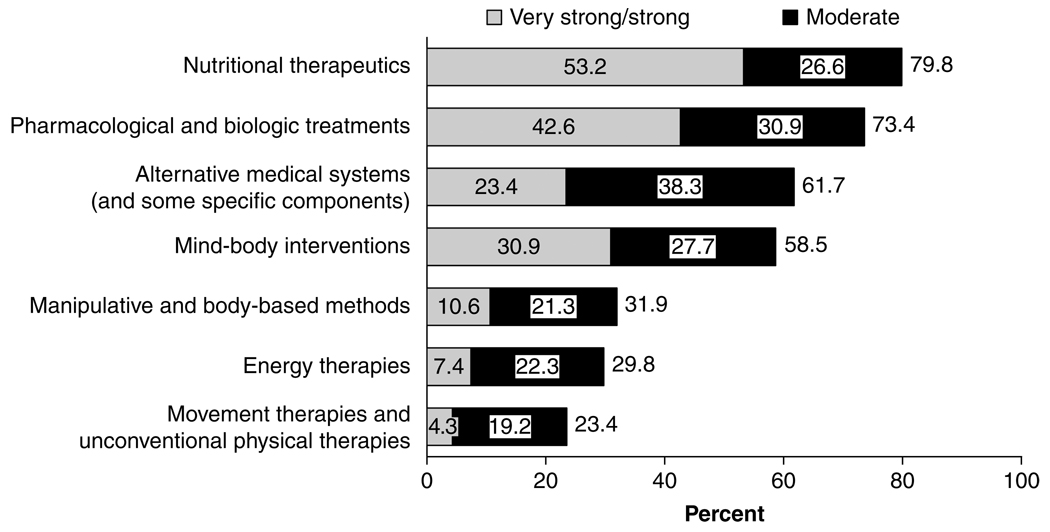
Strength of Research Evidence
Practitioners were asked to rate the strength of the research evidence supporting the efficacy of several categories of CAM used as a cancer treatment (Figure 1). Nutritional therapeutics was the only CAM category for which more than half of the respondents (53.2%) said that there was very strong or strong evidence. However, when very strong, strong, and moderate evidence responses were combined, four categories of CAM were considered to have supporting research evidence by more than half of the respondents: nutritional therapeutics (79.8%), pharmacologic and biologic treatments (73.4%), alternative medical systems and some specific components (61.7%), and mind-body interventions (58.5%).
Figure 1.
Percentage of respondents saying that there was very strong, strong, or moderate evidence supporting the efficacy of CAM categories used as a cancer treatment. (Details may not add to totals because of rounding)
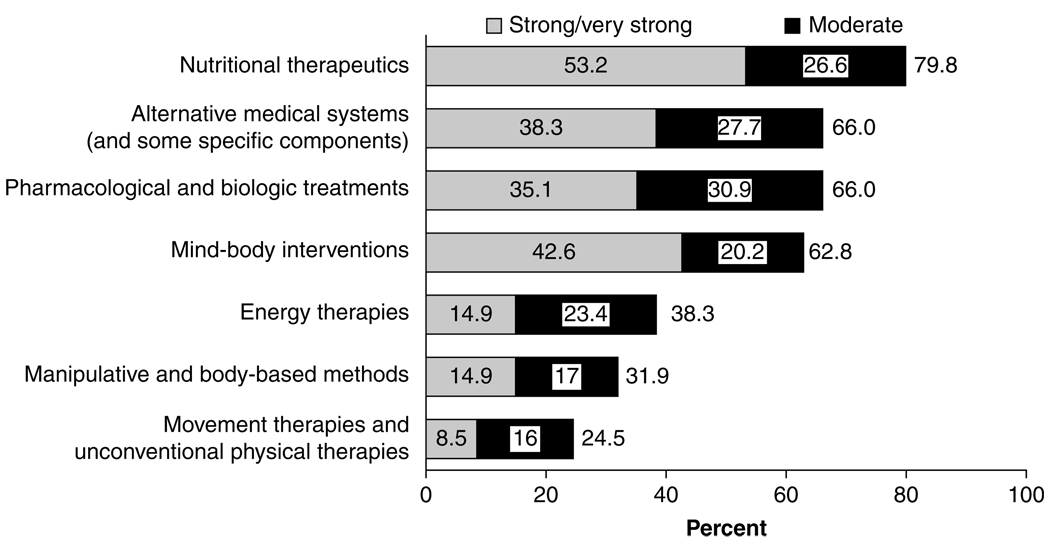
The practitioners were also asked to rate the strength of the research evidence supporting the efficacy of several categories of CAM used in symptom/side-effect management. The percentages of respondents indicating that there was very strong, strong, or moderate evidence were similar to the results for the CAM as cancer treatment section. Nutritional therapeutics was the only CAM category for which more than half of the respondents (53.2%) said that there was very strong or strong evidence for use as symptom/side-effect management; however, when very strong, strong, and moderate evidence responses were combined, four categories of CAM considered to have supporting research evidence emerged: nutritional therapeutics (79.8%), alternative medical systems (66%), pharmacologic and biologic treatments (66%), and mind-body interventions (62.8%) (Figure 2).
Figure 2.
Percentages of respondents saying that there was strong, very strong, or moderate evidence supporting the efficacy of CAM categories used in symptom or side-effect management.
Research Priorities
Practitioners were asked to rate the priority they would give to conducting research on various CAM categories used either for cancer treatments or symptom/side-effect management (Table 5). For cancer treatment, 85.1% of the practitioners gave high priority to research of nutritional therapeutics. Alternative medical systems and pharmacologic/biologic treatments were both given high priority by 69.2% of respondents. Finally, mind-body interventions were given a high priority by 52.1% of those responding. These four categories were also those for which the majority of respondents thought there was very strong, strong, or moderate evidence supporting their efficacy as cancer treatments (see Figure 1). These same categories were given high priority for research in symptom/side-effect management by the greatest percentage of practitioners (83%, 73.4%, 69.2%, and 62.8%, respectively). With regard to the categories of energy therapies, manipulative and body-based methods, and movement and unconventional physical therapies, respondents were more inclined to give research priority to symptom/side-effect management than cancer treatment.
Table 5.
Practitioners Giving High Priority to Research Regarding the Use of Various CAM Treatment Categories for Cancer Treatment and Symptom/Side-Effect Management (%)
| CAM Treatment Category | Cancer Treatment | Symptom/Side-Effect Management |
|---|---|---|
| Nutritional therapeutics | 85.1 | 83.0 |
| Alternative medical systems (and some specific components) | 69.2 | 73.4 |
| Pharmacologic and biologic treatments | 69.2 | 69.2 |
| Mind-body interventions | 52.1 | 62.8 |
| Energy therapies | 33.0 | 50.0 |
| Manipulative and body-based methods | 18.1 | 31.9 |
| Movement therapies and unconventional physical therapies | 13.8 | 26.6 |
CAM = complementary and alternative medicine.
Research Collaboration
Practitioners were asked to indicate the CAM categories in which they were interested for collaborative research (Table 6). More than half of the practitioners expressed an interest in nutritional therapeutics (72.4%), pharmacologic and biologic treatments (71.1%), and the alternative medical systems (60.5%). The category eliciting the least amount of interest for collaborative research was manipulative and body-based methods (18.4%).
Table 6.
Practitioners Indicating They Were Interested in Various CAM Categories for Collaborative Research (%)
| CAM Category | % Interested |
|---|---|
| Nutritional therapeutics | 72.4 |
| Pharmacologic and biologic treatments | 71.1 |
| Alternative medical systems (and some specific components) | 60.5 |
| Mind-body interventions | 44.7 |
| Energy therapies | 36.8 |
| Movement therapies and unconventional physical therapies | 26.3 |
| Manipulative and body-based methods | 18.4 |
CAM = complementary and alternative medicine.
Obstacles Related to Conducting CAM Research
All respondents who were interested in participating in cancer CAM research in the future (n = 79) were asked a series of questions about NCI’s grant application process.
The practitioners who had considered participating in CAM research projects were asked to identify the obstacles to research that they had previously encountered (Table 7). The most frequently encountered obstacle was lack of awareness of appropriate funding sources, cited by three-fourths (75.4%) of the practitioners. Furthermore, of those who encountered this obstacle, 10% felt that it was the most significant in hindering CAM research. Many practitioners (72.1%) also cited lack of access to appropriate cancer research collaborators as a hindrance to conducting CAM research, with 11.7% indicating it to be the most significant. Other obstacles mentioned by at least 50% of the respondents included difficulty in designing a CAM research study that meets grant requirements (excluding placebo-related problems) (60.7%), lack of time (59.0%), lack of institutional support (55.7%), Institutional Review Board issues/regulations (54.1%), lack of success in receiving funds for CAM research (52.5%), and Food and Drug Administration issues/regulations (50.8%). Although no single obstacle predominated as the most significant, four were cited most frequently: lack of awareness of funding sources (10%), lack of access to cancer research collaborators (11.7%), lack of time (11.7%), and lack of success in receiving funds for CAM research (11.7%).
Table 7.
Practitioners Who Encountered Various Obstacles in the Conduct of Cancer CAM Research Projects and Who Indicated that the Obstacle Was the Most Significant (%)
| Obstacle | % Encountering the Obstacle | % Indicating It Was Most Significant |
|---|---|---|
| Lack of awareness of appropriate funding sources | 75.4 | 10.0 |
| Lack of access to appropriate cancer research collaborators | 72.1 | 11.7 |
| Difficulty in designing a CAM research study that meets grant requirements (excluding placebo-related problems) |
60.7 | 8.3 |
| Lack of time | 59.0 | 11.7 |
| Lack of institutional support | 55.7 | 8.3 |
| Institutional Review Board issues/regulations | 54.1 | 3.3 |
| Lack of success in receiving funds for CAM research | 52.5 | 11.7 |
| Food and Drug Administration issues/regulations | 50.8 | 5.0 |
| Nonacceptance of research reports for journal publication | 45.9 | 5.0 |
| Negative perceptions among peers regarding the acceptability of CAM research |
44.3 | 5.0 |
| Lack of access to appropriate CAM practitioners | 31.2 | 0.0 |
| Difficulty in identifying an appropriate placebo | 31.2 | 0.0 |
| Difficulty in obtaining a sufficient number of patients | 29.5 | 1.7 |
| Other obstacle | 13.1 | 8.3 |
CAM = complementary and alternative medicine.
NCI BCS Program
The survey contained a description of the NCI’s BCS Program, which is a process for evaluating case report information from practitioners that involves the same rigorous scientific methods used to evaluate treatment responses with conventional medicine. The program is an opportunity for cancer CAM practitioners to share their well-documented cases, with the goal of assessing whether sufficient evidence is available for NCI-initiated prospective research. Respondents were asked if they knew about the NCI BCS Program prior to receiving the survey. Fifty-six respondents (71%) had heard about the program. Of those 56, about 48% became aware of the program through a conference presentation, 27% through OCCAM’s Web site, and 23% through a letter from the director of OCCAM. Twelve of the 56 responding practitioners had submitted cases for review. The remaining 44 practitioners had not submitted cases and cited several reasons. These included lack of time necessary to compile case study material, lack of support staff and resources to compile case study material, and lack of a program information packet. Some of the practitioners felt that the effort required to compile case studies was not worthwhile. Other reasons included lack of access to patient records and lack of cases that meet eligibility requirements.
Discussion
The primary purpose of this survey was to assess the patterns of a cohort of CAM practitioners as they relate to their general clinical practice, referrals, reliance on research findings, research priorities, and interest in partnering with cancer researchers. To our knowledge, this report is the first to detail the practices, interests, and concerns of cancer CAM practitioners with regard to these issues. Although limited in number, other cancer CAM practitioner surveys have been undertaken and published.2,3 Despite a variation in survey focus and data acquisition techniques in comparison with the previous studies, our study achieved a similar response rate of only 38%. This leads one to speculate that if surveys of this type are to be undertaken in the future, thought must be given to developing new approaches to improve participation. For example, development of innovative techniques of participant identification, survey administration, and follow-up may be warranted.
To encourage a high response rate within this diverse population of practitioners, various strategies were employed. For example, potential respondents were offered financial incentives and follow-up telephone calls were made when necessary. Despite these measures, the final sample size was relatively small, restricting our ability to generalize the data to all CAM practitioners. Nevertheless, inherent value remains in the information in laying the groundwork for future successful collaborations.
Practitioners were queried with regard to the location and purpose of cancer CAM delivery. Ninety-eight percent of the practitioners within the survey population either provided CAM to cancer patients within their clinical setting or referred the patients to other CAM providers. The survey indicated that the practitioner’s rationale for providing CAM to their patients was for both the purposes of improving quality of life and increasing survival. This care delivery premise matches that of patients’ beliefs that certain CAM modalities can improve quality of life and are effective in minimizing the discomforts associated with treatment.4 Understandably, the types of CAM modalities that practitioners provided differed with the types for which they made referrals. For example, nutritional therapeutics, alternative medical systems, and pharmacologic/biologic treatments were the most frequently provided treatment categories; however, manipulative and body-based methods and movement therapies elicited a higher percentage of referrals. One can speculate that the latter categories require a certain degree of specialization that was not common among the cohort and were therefore provided by fewer practitioners. Most interestingly, the three categories of cancer CAM that practitioners were providing themselves matched the top three categories that were cited as needing the highest priority for research. One must consider that these categories of intervention may be the most highly sought after by patients, thus stimulating a desire in the practitioner to deliver better quality of care. However, another possibility is that these are the treatments that the practitioners themselves consider to be the most promising and therefore promote them to patients.
The NCI had also commissioned a simultaneous survey targeting cancer researchers for the primary purpose of assessing their perceptions of promising areas of cancer CAM research. In addition, we were interested in elucidating the level of interest that existed among the researchers for potential collaborations with the CAM practitioners as a way to scientifically advance the field. Although the viewpoints differed on which modalities possessed greater evidence, both researchers and practitioners agreed that high-priority research for cancer treatment should involve nutritional therapeutics and pharmacologic/biologic treatments and were interested in research partnership in these areas.1
In any setting, the partnering of those with a highly unique set of skills and knowledge leads to greater chances for ultimate success. This formula for success is no less important for advancing the science of cancer CAM; however, at present, these partnerships are more the exception than the rule in academia, clinical trials, and community settings. More recently, however, practitioners and researchers alike are finding increasing value in partnering efforts. In the NCI surveys, both groups were queried as to their interest in clinical research partnerships. The CAM categories in which most practitioners and researchers were interested in collaborative research were nutritional therapeutics, pharmacologic/ biologic treatments, and alternative medical systems. Interestingly, these modalities were also identified as those being most commonly provided by the practitioners. One could presumably conclude that practitioners are self-providing modalities that are of the most interest to patients. As such, fuel for interest in specific types of research by the practitioner may be patient driven to a certain extent. With respect to the researcher, pharmacologic/biologic and nutritional modalities were cited as the two CAM categories with the most evidence supporting their use as a cancer treatment. 1 This basis may provide researchers with the incentive to further the science in these modalities.
The practitioner’s survey brought forth valuable information for consideration with regard to establishing successful clinical research partnerships. In response to these data, the NCI further examined the dynamics of collaboration during the conference Cancer Researcher & CAM Practitioners: Fostering Collaborations; Advancing the Science (National Institutes of Health, October 2007). The conference fostered interaction and dialogue between both groups with regard to priorities in CAM clinical cancer research. Examples of successful partnerships were highlighted at the meeting, providing incentive for other future endeavors. The current survey indicates that 22% of researchers and 31% of practitioners felt that lack of access to appropriate collaborators was a hindrance to CAM research. In response, the NCI has built a directory of cancer CAM researchers to allow individuals working in this field to identify others with similar or related research interests (<http://www.cancer.gov/cam/research_directory.html>).
The researcher and practitioner surveys brought forth other concerns with regard to either the lack of access and/or awareness of funding sources as a deterrent to CAM research. For both groups, this was the obstacle encountered by the greatest percentage of respondents.1 The NCI/OCCAM has taken measures to address these concerns. For example, a Broad Agency Announcement (BAA) was initiated in 2005 for contracts to support preparation of a case series or projects in which CAM practitioners and researchers would work together. Second, the NCI/OCCAM has undertaken the development of a funding directory designed to assist researchers in locating sources of money to support cancer CAM research projects. Currently, the database consists of foundations, advocacy groups, non–federal government organizations, and private sector organizations that have expressed an interest in funding cancer CAM research. Contact information and specific areas of CAM interest are provided in the directory, located at <http://www.cancer.gov/cam/research_funding_directory.html>.
The NCI BCS Program
Since 1991, the NCI has had a process for evaluating data submitted by cancer CAM practitioners. This process, the NCI BCS Program, provides an independent review of medical records, radiographic imaging, and pathologic specimens involving cancer patients treated with CAM therapies. As such, gathering and submitting the required documentation are the responsibility of the practitioner. The primary goal of this program is to obtain and review sufficient information to determine if NCI-initiated research on a specific CAM intervention is warranted.
The current survey has revealed that despite knowledge of the program, few practitioners had submitted cases for review. The survey identified lack of time, resources, and uncertainty of the value as the main reasons for not pursuing submissions to the program (data not shown). In response to this information, the NCI/OCCAM has made efforts to assist practitioners in the submission process. Examples include on-site visits, group discussion of potential cases, assistance with acquisition of data associated with cases of interest, and the covering of mailing expenses. Although case reports are generally considered the lowest level of evidence, they may be the only obtainable or realistic information in support of a CAM therapy.
Conclusion
NCI/OCCAM’s program goals are to increase the amount of high-quality information and research on the use of CAM and CAM-related approaches for the diagnosis, prevention, and treatment of cancer and related symptoms. Despite a small sample size and lack of a feasible process for random sampling, this survey highlights avenues to promote and support collaborative research. The survey solicited a review of obstacles within and among the practitioner and researcher communities, laying the groundwork for future steps forward in the process of establishing successful collaborative research partnerships. The lack of organizational structure to cancer CAM practitioners is a significant impediment to identifying comprehensive solutions to the issues identified in the survey. Thus, we hope that the publication of this article may play a small role in catalyzing greater cohesiveness of this community. NCI/OCCAM will continue to respond to the concerns elucidated by the survey by developing strategies for future program opportunities within the NCI.
Acknowledgment
Financial disclosure of authors: Funding for this paper was provided by the National Cancer Institute.
Footnotes
Presented in part at the Second International Meeting of the Society for Integrative Oncology, San Diego, CA, November 11, 2005.
Financial disclosure of reviewers: None reported.
Contributor Information
C.D.R. Colleen Lee, Office of Cancer Complementary and Alternative Medicine, National Cancer Institute, National Institutes of Health, Department of Health and Human Services, Bethesda, MD.
Farah Zia, Office of Cancer Complementary and Alternative Medicine, National Cancer Institute, National Institutes of Health, Department of Health and Human Services, Bethesda, MD.
Oluwadamilola Olaku, Kelly Services Incorporated, Rockville, MD.
Joan Michie, Westat, Rockville, MD..
Jeffrey D. White, Office of Cancer Complementary and Alternative Medicine, National Cancer Institute, National Institutes of Health, Department of Health and Human Services, Bethesda, MD;.
References
- 1.Smith WB, Olaku O, Michie J, et al. Survey of cancer researchers regarding complementary and alternative medicine. J Soc Integr Oncol. 2008;6:2–12. [PubMed] [Google Scholar]
- 2.Cassileth BR, Lusk EJ, Strouse TB, et al. Contemporary unorthodox treatments in cancer medicine. A study of patients, treatments, and practitioners. Ann Intern Med. 1984;101:105–112. doi: 10.7326/0003-4819-101-1-105. [DOI] [PubMed] [Google Scholar]
- 3.Berman BM, Singh BB, Hartnoll SM, et al. Primary care physicians and complementary-alternative medicine: training, attitudes, and practice patterns. J Am Board Fam Pract. 1998;11:272–281. doi: 10.3122/jabfm.11.4.272. [DOI] [PubMed] [Google Scholar]
- 4.Sparber A, Bauer L, Curt G, et al. Use of complementary medicine by adult patients participating in cancer clinical trials. Oncol Nurs Forum. 2000;27:623–630. [PubMed] [Google Scholar]