Abstract
Purpose
To determine the optimal sequence of combining anti-IGF1R antibodies with chemotherapeutic drugs in cancer cells in vitro and in vivo.
Experimental design
MCF-7 and LCC6 cells were treated with sub-cytotoxic concentrations of doxorubicin (DOX) with or without anti-IGF1R antibodies (scFv-Fc or EM164 and its humanized version AVE1642). Treatments were given simultaneously, DOX followed by anti-IGF1R antibody, or anti-IGF1R antibody followed by DOX, with measurement of in vitro proliferation, apoptosis, and anchorage-independent growth. Effects of sequencing on LCC6 xenograft growth and metastasis were studied.
Results
DOX followed by anti-IGF1R antibody (scFv-Fc or EM164) was the most effective combination strategy to inhibit cell monolayer growth and anchorage-independent growth. This sequential combination triggered increased Poly (ADP-ribose) polymerase (PARP) cleavage compared to other treatment sequences. The reverse sequence, antibody followed by DOX treatment, protected cells from chemotherapy by decreasing apoptosis, arresting cells in S phase, and inhibiting the level and activity of topoisomerase IIα. Finally, our in vivo data show that recovery of IGF1R prior to DOX therapy resulted in the best therapeutic responses. Low doses of AVE1642 that allowed IGF1R expression to recover at one week were more effective in combination with DOX than higher antibody doses.
Conclusion
The timing of IGF1R inhibition affects responses to chemotherapy. The optimal sequence was DOX followed by anti-IGF1R antibody, while the opposite sequence inhibited DOX effects. Thus, dose and sequencing of anti-IGF1R therapies should be considered in the design of future clinical trials.
Keywords: Type I IGF receptor, breast cancer, chemotherapy
Introduction
Although chemotherapy produces objective responses in patients with breast cancer, it is far from completely effective. Cytotoxic agents also may cause severe and dose-limiting systemic toxicities. Thus, identifying new methods to enhance the beneficial effects of chemotherapy while decreasing systemic toxicities are clearly needed (1, 2). Recent progress suggests that combination of chemotherapy with targeted therapy is superior to either one alone. For example, patients with metastatic colon cancer treated with both the anti-EGFR antibody, cetuximab, and the chemotherapy drug irinotecan have superior results, even if the patients progressed on irinotecan alone (3). In addition, trastuzumab (Herceptin), an anti-HER2 antibody, is widely used to treat patients overexpressing the HER2 growth factor receptor in combination with chemotherapeutic drugs (4, 5).
Among the new potential cancer targets, the type I insulin-like growth factor receptor (IGF1R) has emerged as a relevant pathway. Population, preclinical, and research findings suggest that the insulin-like growth factor (IGF) system functions to maintain the malignant phenotype in cancer (6). Disruption of IGF1R activation has been shown to inhibit cancer cell growth and motility in vitro and in vivo (7-9). Various approaches of disrupting IGF1R activity have been developed as potential interventions in the treatment of malignancies in the past several years. Antibodies that disrupt IGF1R function have been developed. scFv-Fc, a chimeric humanized single chain antibody, causes initial receptor biochemical signaling followed by receptor down-regulation, and exhibits dose-dependent growth inhibition of some breast cancer cell lines (10, 11). EM164, a full antagonistic anti-IGF1R antibody, did not stimulate IGF1R autophosphorylation, but downregulated IGF1R in vitro and in vivo. It also displays inhibitory activity against IGF-I and IGF-II induced survival of MCF-7 breast cancer cell (12). The humanized version of EM164, AVE1642 (sanofi-aventis) is currently in clinical trials against various type of solid cancer.
Several studies have shown that activation of IGF1R protects breast cancer cells from apoptosis induced by chemotherapy and radiation, and receptor activation mediates resistance to chemotherapy and radiation (13-15). Therefore, inhibiting IGF1R signaling may enhance the sensitivity of cancer cells to chemotherapy. Indeed, several groups have shown that combining anti-IGF1R antibody with chemotherapy enhances chemotherapy responses in human cancer cells (12, 16, 17).
Recent findings suggest that combination of chemotherapy and targeted therapy may be sequence-dependent. A large cooperative group trial demonstrated an estimated disease-free survival advantage of 18% for sequential rather than concurrent chemotherapy and tamoxifen treatment when given in the adjuvant setting (18). In addition, inhibition of HER2 by trastuzumab first, but not in the reverse order, increased paclitaxel resistance of ovarian cancer cells (19). Since several anti-IGF1R antibodies are being evaluated in phase I /II/III clinical trials, some in combination with cytotoxic chemotherapy, it is be important to determine the optimal schedule for the antibodies in combination with chemotherapy.
The work presented here describes the in vitro and in vivo activity of anti-IGF1R antibody in combination with several chemotherapeutic drugs delivered concurrently or sequentially in human cancer cell lines. We have determined the optimal sequence of anti-IGF1R antibodies in combination with commonly used chemotherapeutic drugs. Our results support the idea that sequencing of anti-IGF1R therapy with chemotherapy can optimize the anti-tumor effect and have significant implications for the clinical development of this strategy.
Materials and Methods
Reagents
All reagents and chemicals were purchased from Sigma (St. Louis, MO), and cell culture reagents were from Invitrogen/Life Technologies, Inc. (Rockville, MD) unless otherwise noted. IGF-I was purchased from Novozyme (Adelaide, Australia). The anti-IGF1R antibody scFv-Fc was engineered and purified as described previously (20). EM164 and AVE1642 (a humanized EM164) antibody were previously reported(12). Antibodies against ERK1/ERK2 were purchased from Cell Signaling (Beverly, MA). The polyclonal antibodies against IGF1R α and ß subunits were from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA). The anti-ß-actin was from Sigma-Aldrich (St.Louis, MO). Anti-Topo IIα antibody was from TopoGEN (Columbus, OH). Anti-rabbit and anti-mouse secondary antibodies conjugated to HRP were from GE Biosciences (Piscataway, NJ).
Cell Lines and Culture
MCF-7 cells were originally obtained from Dr. C. Kent Osborne (Baylor College of Medicine, Houston, TX) and were routinely maintained in Iscove’s modified essential medium (IMEM) with Zinc Option (Richter’s modification) with 5% fetal bovine serum, 11.25 nM human insulin (Eli Lilly, Indianapolis, IN), 50 units/ml penicillin, and 50 μg/ml streptomycin. LCC6 cells were obtained from Dr. Robert Clarke (Georgetown University, Washington D. C.). LCC6 cells were routinely maintained in Dulbecco’s modified Eagle’s medium with 10% fetal bovine serum, 11.25 nM human insulin, 50 units/ml penicillin and 50μg/ml streptomycin.
Proliferation Assay
MCF-7 cells were plated in triplicate in 24 well tissue culture plates at a density of 20,000 cells per well in growth media. After 24 hours, cells were switched to serum free medium (SFM) for 24 hours and then treated according to the following schedules: (1) doxorubicin (DOX) alone for 72 hours; (2) DOX and antibody simultaneously for 72 hours; (3) pretreatment with DOX for 24 hours followed by antibody treatment for 48 hours; (4) pretreatment with antibody for 24 hours followed by DOX treatment for another 48 hours. Cell number was estimated using the 3-[4,5-Dimethylthiazol 2-yl]2,5-diphenyltetrazolium bromide (MTT) assay as described previously(21). 60 μl of 5 mg/ml MTT reagent in PBS was added to each well and plates were incubated for 3 hours at 37°C. Wells were aspirated and 0.5 ml of solubilizing solution (95% DMSO + 5% IMEM) was added to solubilize the formazan crystals. Absorbance was measured at 570nm using a 670nm differential filter.
Anchorage-independent Growth
Anchorage-independent growth assays were performed as follows. A bottom agar was prepared by solidifying 1 ml of 0.8% SeaPlaque agarose (BioWhitaker, Rockland, ME) in 2% FBS-containing growth media in each well of a 6-well plate. The bottom agar was overlaid with 800 μl of a 0.45% top agar mixture containing 10,000 LCC6 cells per well in the presence of DOX, scFv-Fc, EM164, or DOX and anti-IGF1R antibody. The plates were incubated at 37°C for 24 hours, then growth media with or without DOX and antibody was added to the top of agar. After 9-10 days, colonies were counted using a light microscope with an ocular grid. Only colonies larger than two-thirds of a grid square were counted. Five random fields were counted for each well and the average number of colonies per well is shown. Results are representative of one experiment performed in triplicate for each treatment.
Western Blotting
LCC6 cells were grown to 70% confluence, incubated in SFM overnight, and treated with the same schedule as described for MTT assays. Cells were lysed in TNESV buffer and 40 μg of total cellular proteins were separated by SDS-PAGE on 8% gels. Proteins were transferred to nitrocellulose and immunoblotted with the anti-Poly (ADP-Ribose) polymerase (PARP) antibody (Santa Cruz, CA). Enhanced chemiluminescence was performed according to manufacturer’s instructions (Pierce). For studies on the effect of combining the anti-IGF1R antibody with doxorubicin on topo IIα protein levels, nuclear extracts were prepared from LCC6 cells treated with AVE1642, doxorubicin, or AVE1642 combined with doxorubicin concurrently or sequentially. Nuclear extracts were purified by lysis of cells with a high-salt buffer [100 mM NaCl, 20 mM KCl, 20 mM Tris, and 0.5 mM Na2HPO4 (pH 7.4)] containing 0.5% Triton X-100 and 1% NP40. Nuclei were pelleted, and the nuclear proteins were solubilized by sonication in 1% SDS. After quantification, 50 μg of nuclear proteins were loaded and separated by 8% SDS-PAGE, transferred onto nitrocellulose, and incubated with an anti-human topo IIα rabbit polyclonal antibody (TopoGEN, Inc., Columbus, OH).
Annexin V Analysis of Apoptosis
The annexin V-APC-labeled Apoptosis Detection Kit I (BD Biosciences, San Diego, CA) was used to detect apoptosis by flow cytometry according to the manufacturer’s instructions. LCC6 cells (4 × 105 cells/well) were seeded in 60-mm dishes and cultured overnight in serum-free DMEM medium. The next day, cells were treated according to the following schedule: (1) 1% FBS; (2) DOX (100 ng/ml) 48 hours; (3) scFv-Fc (30 μg/ml) or EM164 (15 μg/ml) 48 hours; (4) DOX in combination with scFv-Fc or EM164 simultaneously for 48 hours; (5) DOX 24 hours followed by scFv-Fc or EM164 for another 24 hours; (6) Pretreated with scFv-Fc or EM164 for 24 hours and followed by DOX for another 24 hours. Cells were harvested in cold PBS after treatment. Heat shocked cells (cells were incubated in 56°C water bath for 1 min) were used as positive control. Cells were then resuspended at a density of 1 × 106 cells/ml in 1x binding buffer (HEPES, 10 mM, pH 7.4, 150 mM NaCl, 5 mM KCl, 1 mM MgCl2, and 1.8 mM CaCl2) and stained simultaneously with APC-labeled annexin V (25 ng/mL) and 7-AAD (50 ng/mL). 7-AAD was used as a cell viability marker. Cells were analyzed using a fluorescence-activated cell sorter (FACS) flow cytometer (Becton Dickinson, San Jose, CA), and the data were analyzed with CellQuest software.
Cell Cycle Analysis
Confluent LCC6 cells were trypsinized and plated at a density of 5× 105 cells per 60 mm dish. After 24 hours, cells were switched to SFM for 24 hours. Cells were then treated as it is described above. Cells were collected on ice in 1 ml of 1x PBS, and stained with propidium iodide (Sigma-Aldrich Corp. St. Louis, MO). Cells were analyzed for phase of the cell cycle by flow cytometry. Results were analyzed using Modfit software.
Topoisomerase II Decatenation Assay
The assay was performed according to manufacturer’s instructions (TopoGen, Inc., Port Orange, FL). LCC6 cells were treated with doxorubicin, AVE1642, or doxorubicin with AVE1642 simultaneously or sequentially. Nuclear extracts were prepared as noted above. The total reaction volume was held at 20 μl. Assay buffer (120 mM KCL, 50 mM Tris-HCl, 10 mM MgCl2, 0.5 mM dithiothreitol, 0.5 mM ATP, and 30 μg/mL BSA) containing 100 ng of catenated kinetoplast DNA (kDNA) and 2 μg LCC6 nuclear extract was incubated for 30 min at 37°C. The reaction was stopped upon addition of 4 μl of stop buffer (4% glyceol, 1% sarkosyl, and 0.025% bromphenol blue), and then analyzed by 1% agarose gel electrophoresis.
Tumor Growth in Athymic Mice and Tumor Extract Analyses
Four week-old female athymic mice were used for in vivo study. To study the effect of AVE1642 dose on IGF1R downregulation in vivo, 5 × 106 LCC6 cells were injected into the mammary fat pads on each side of each mouse. When tumor volume reached 100 mm3, AVE1642 was injected intraperitoneally (i.p). Tumors from the left side of all mice were surgically resected and snap-frozen in liquid nitrogen two days after AVE1642 treatment. The tumors on the right side of the mouse were collected and frozen after another 7 days. Tumors were homogenized and blotted for IGF1Rβ as noted above.
For the tumor growth study, 5 × 106 LCC6 cells in serum-free IMEM were injected into the mammary fat pad of the mice. Tumor growth was measured every 3 days and tumor volume was estimated from bidirectional measurements using the formula length × breadth2 / 2. When the tumors reached volume of ∼80 mm3, the mice were randomized into 5 groups of 5 animals each. The dose of AVE1642 was based on the findings from the previous experiment. Mice were treated with PBS, DOX (3 mg/kg body weight/week), AVE1642 (50 μg/week), DOX followed 24 hours later by AVE1642 (50 μg/week) or DOX followed 24 hours later by AVE1642 (800 μg/week) by intraperitoneal injection. Treatment was given weekly for 4 weeks. Twenty four hours after the final treatment, mice were sacrificed. The lungs of the mice were harvested, fixed, embedded, sectioned and stained with hematoxylin and eosin, and examined microscopically for micro-metastatic deposits. In the second set of experiments, the mice were sacrificed one week after the final treatment. Tumors were harvested, nap-frozen and homogenized. Tissue homogenates were suspended in 500 μl TNESV lysis buffer. 100 μg of each tumor extract were subjected to 8% SDS-PAGE followed by immunoblotting for the level of IGF1R. Total levels of MAPK were used as loading control. All the animal protocols were approved by the University of Minnesota’s Institutional Animal Case & Use Committee (IACUC).
Statistical Tests
Statistical significance between means of control and antibody in combination with doxorubicin was assayed using Student’s t test; 95% confidence interval (P< 0.05) was considered significant. For comparisons between more than two treatments in the xenograft experiments, One-way ANOVA analysis was performed. If not otherwise indicated, error bars in all experiments represent the SD.
Results
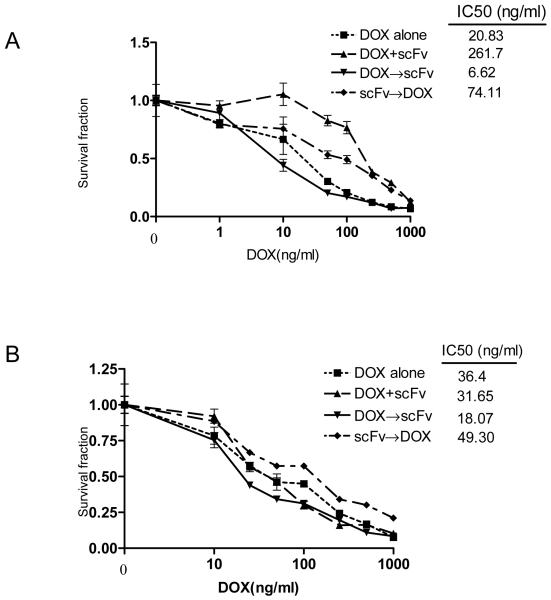
Sequence-dependent anti-proliferation effects of combining scFv-Fc or AVE1642 with doxorubicin in MCF-7 cells
To assess whether the IGF1R antibody, scFv-Fc can synergize or inhibit the cytotoxicity of doxorubicin, the IC50 of doxorubicin were studied in a monolayer growth using MTT assays (Fig.1). These assays were done in the absence (1%FBS) or presence of IGF-I (5 nM). Whether in the presence of IGF-I or in the 1% FBS condition, simultaneous treatment with scFv-Fc and doxorubicin or the sequence of scFv-Fc followed by doxorubicin, decreased cytotoxicity was observed (Fig.1A, B). The IC50 of doxorubicin was increased when antibody was given before or simultaneously with the drug. Interestingly, doxorubicin followed by scFv-Fc, resulted in enhanced doxorubicin cytotoxicity and the IC50 2-4 times lower in MCF-7 cells.
Figure 1. Sequence-dependent anti-proliferation effect of combining scFv-Fc or AVE1642 with doxorubicin in MCF-7 cells.
MCF-7 cells grown in 5 nM IGF-I (A,C) or 1% FBS condition (B,D) were treated with different concentration of doxorubicin (DOX), scFv-Fc (scFv, 30 μg/ml) or AVE1642 (AVE, 15μg/ml) simultaneously or sequentially as following: (1) doxorubicin (DOX) alone for 72 hours; (2) DOX and antibody simultaneously for 72 hours; (3) pretreatment with DOX for 24 hours followed by antibody treatment for 48 hours; (4) pretreatment with antibody for 24 hours followed by DOX treatment for another 48 hours. MTT assay were performed over 72 hours. Cell survival is displayed as a percentage of growth over non-DOX treated control. The experiment was repeated three times; a representative experiment is shown.
It was evident that the magnitude of the effect of sequencing was different between the two culture conditions. Since scFv-Fc stimulated biochemical activity of the receptor, the effects were less marked in cells cultured in the presence of IGF-I as the agonist effect of scFv-Fc was masked by the presence of IGF-I. In order to address whether the sequence-dependent inhibition was affected by the agonistic properties of scFv-Fc, we examined the effect of doxorubicin in combination with EM164. This antibody does not stimulate IGF1R biochemical activation and displayed potent inhibitory activity against IGF-I, IGF-II and serum stimulated proliferation of diverse cancer cell lines (12). As shown in Figure 1C and D, similar results were obtained, as the sequence of doxorubicin followed by EM164 significantly inhibited the cell proliferation in MCF-7 cells. These results suggest that the cytotoxic effects of combining doxorubicin with scFv-Fc or EM164 are sequence-dependent with doxorubicin followed by antibody demonstrating the optimal anti-proliferative effect.
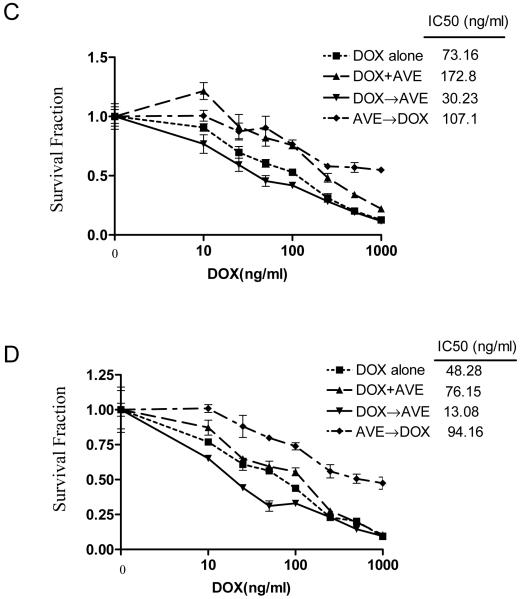
Doxorubicin, but not 5-FU, followed by scFv-Fc or EM164, significantly inhibited the anchorage-independent growth of LCC6 cells
In MCF-7 cells, IGF1R activation stimulates proliferation complicating the interpretation of this type of sequencing experiment (22). In order to further evaluate the effects of inhibition of IGF1R on chemotherapy and confirm the sequence-dependent inhibition effects, without the added complexity of the growth regulatory effects of IGF1R on the cell, we concentrated on the LCC6 cell line in anchorage-independent growth assays. This cell line, derived from the MDA-MB-435 cell line, expresses IGF1R yet is not growth regulated by its activation (23). Recently, this cell line has been shown to originate from a malignant melanoma cell (24), but still is an excellent model for studying the effects of IGF1R inhibition on cancer cell biology.
In this experiment, we used a dose of doxorubicin (100 ng/ml) that by itself, it did not inhibit colony formation. Cells were either treated simultaneously with doxorubicin and scFv-Fc or treated sequentially. As shown in Fig. 2A, similar to the result of the MTT assay in MCF-7 cells, the sequential treatment of doxorubicin followed by scFv-Fc significantly inhibited colony growth compared to the other sequences (Fig.2A). Since scFv-Fc is a partial agonistic antibody of IGF1R, we examined the effect of doxorubicin in combination with EM164 in anchorage-independent growth. As shown in Figure 2B, similar results were obtained, as the sequence of doxorubicin followed by EM164 significantly inhibited the colony growth in LCC6 cells.
Figure 2. Doxorubicin, but not 5-FU, followed by scFv-Fc or EM164 significantly inhibited the anchorage-independent growth of LCC6 cells.
Cells incubated with or without antibodies (scFv-Fc (scFv) or EM164 (EM)), and/or cytotoxic drugs, (A, B) doxorubicin (DOX) and (C,D) 5-fluorouracil (5-FU), in the presence of 2% FBS were mixed with 0.45% agarose and overlaid over 0.8% bottom agar in 6-well plates and incubate for 24 hours. If a second treatment was needed (shown by the arrow), it was added as a solution to the top agar with continued incubation for 9-10 days. Five randomly selected fields were counted for each well. Each treatment was done in triplicate, and the results are shown as the average number of colonies ± SE. The experiment was repeated three times with similar results, and a representative experiment is shown. * P<0.05 vs 5-FU alone; ** P<0.01 vs DOX alone; *** P<0.001 vs DOX alone. The abbreviations used are: scFv, scFv-Fc (30 μg/ml); EM, EM164 (15 μg/ml); DOX, doxorubicin (100 ng/ml); 5-FU, 5-fluorouracil (2.5μM).
Rochester et al. showed that silencing of the IGF1R gene enhances sensitivity to DNA damaging agents in human prostate cancer cells, but not with other cytotoxic agents (25). Doxorubicin is a toposomerase II inhibitor and also intercalates into DNA to cause DNA damage (26). To investigate whether the sequence-dependent inhibition of doxorubicin in combination with anti-IGF1R antibodies was specific to DNA damaging drugs, the effect of combining anti-IGF1R antibodies with etoposide and 5-FU were examined. Etoposide is another topoisomerase II inhibitor and induces double strand DNA breaks (27), while 5-FU is an anti-metabolite which undergoes biotransformation to 5-fluoro-2′-deoxyuridine- 5′-phosphate and forms a covalently bound ternary complex with the enzyme thymidylate synthase and its cofactor to inhibit DNA synthesis (28). As expected, etoposide followed by scFv-Fc or EM164 significantly inhibited colony growth (data not shown). In contrast, sequence-dependent inhibition was not observed with 5-FU in combination with scFv-Fc or EM164 (Fig. 2C, D).
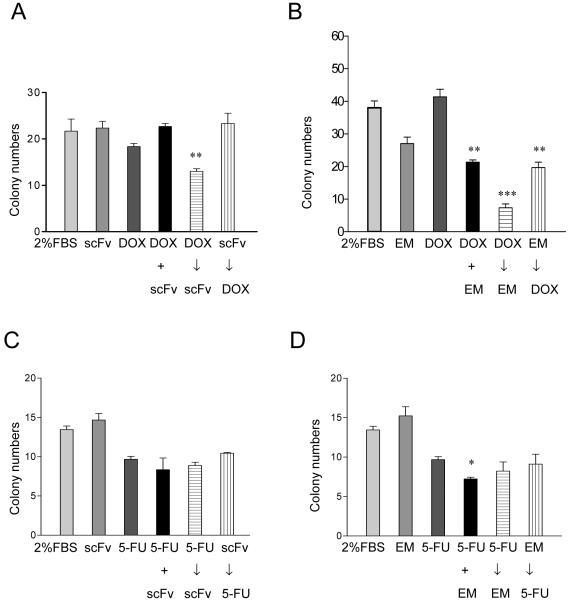
Doxorubicin followed by scFv-Fc or AVE1642 increased PARP cleavage and pretreatment with scFv-Fc or EM164 rendered cell resistant to doxorubicin induced apoptosis
IGF-I protects MCF-7 breast cancer cells from doxorubicin and paclitaxel by induction of proliferation and inhibition of apoptosis (22). In LCC6 cells, mono-layer cell growth is not affected by IGF-I; we used these cells to examine whether anti-IGF1R antibody scFv-Fc or AVE1642 sequencing affected doxorubicin induced apoptosis in LCC6 cells. LCC6 cells were treated with doxorubicin and scFv-Fc or AVE1642 simultaneously or sequentially. After treatment, both adherent and nonadherent cells were collected and subjected to Western blotting with antibodies to PARP, a caspase substrate that is cleaved in cells undergoing apoptosis. In Fig. 3A, doxorubicin followed by scFv-Fc or AVE1642, but not in other sequences, significantly increased DOX (500 ng/ml) induced PARP cleavage. Neither antibody by itself induced PARP cleavage.
Figure 3. Doxorubicin followed by scFv-Fc or EM164 increased PARP cleavage and pretreatment with antibody rendered cell resistant to doxorubicin induced apoptosis.
A, Serum starved LCC6 cells were treated with 1%FBS (control), doxorubicin, scFv-Fc, AVE1642 or antibody in combination with DOX simultaneously or sequentially for 48 hours totally. PARP cleavage was determined by Western blot analysis of whole cell lysates as described under “Materials and Methods.” The abbreviations used are: scFv, scFv-Fc (30 μg/ml); AVE, AVE1642 (20 μg/ml); DOX1000 (doxorubicin at 1000 ng/ml); DOX 500 (doxorubicin at 500 ng/ml). B and C, LCC6 cells were treated with different compounds alone or in combination with DOX simultaneously or sequentially, and then cell were collected and stained with APC-Annexin V and 7-AAD and analyzed by flow cytometry. The experiment was repeated three times with similar results; a representative experiment is shown for cells of apoptosis (percentage of all cells that were apoptotic). * P< 0.05 vs DOX alone.
To address whether these changes in PARP cleavage reflected an increase in induction of apoptosis by chemotherapy, we measured annexin-V staining by flow cytometry analysis. LCC6 cells were treated with doxorubicin in combination with scFv-Fc or EM164 concurrently or sequentially for 48 h, the adherent and nonadherent cells were analyzed. In this assay, pre-treatment with EM164 significantly decreased the doxorubicin induced apoptosis (Fig. 3B). We did not see DOX followed by EM164 increased cell apoptosis in this experiment. However, these data indicate that if IGF1R was inhibited prior to doxorubicin exposure, then cells were protected from the effects of doxorubicin.
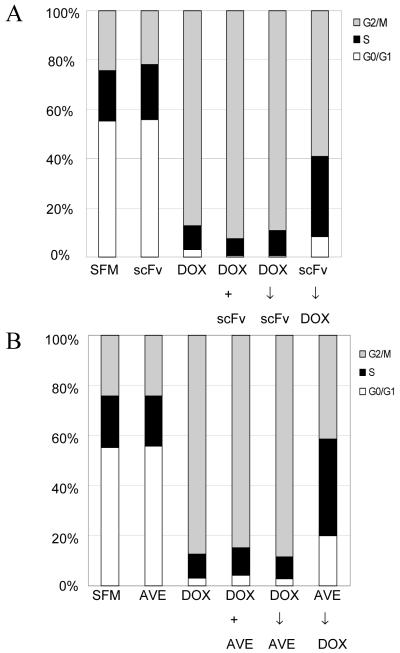
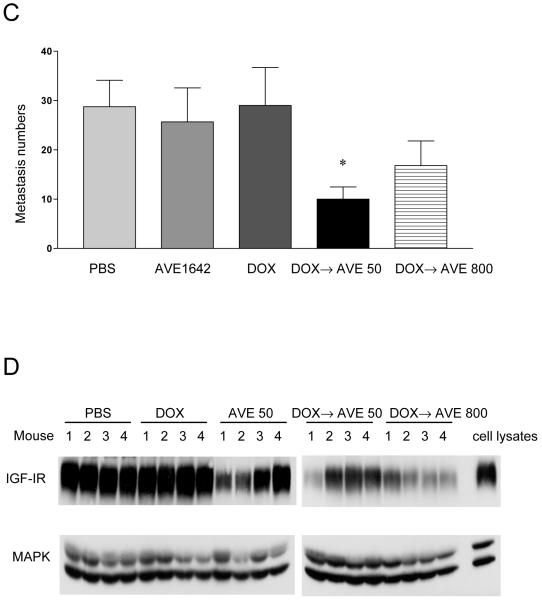
Pretreatment with scFv-Fc or AVE1642 followed by doxorubicin arrested LCC6 cells in S phase
To investigate the potential mechanism of this sequence-dependent effect of doxorubicin in combination with anti-IGF1R antibodies, we studied the cell cycle profile of LCC6 cells treated with doxorubicin and scFv-Fc or AVE1642. In these cells, the antibodies did not affect cell cycle distribution of LCC6 cells (Figure 4). Consistent with previous report, doxorubicin treated cells were arrested in G2-M phase (29). Simultaneous exposure to scFv-Fc /AVE1642 and doxorubicin, doxorubicin followed by scFv-Fc or AVE1642, showed similar effects to doxorubicin alone. In contrast, cells pre-treated with antibody followed by doxorubicin decreased G2-M arrest with an increase in G1 and S-phase fraction (Fig. 4A, B). These data suggested that inhibition of IGF1R prior to doxorubicin exposure blunted the effects of doxorubicin as reflected by effects on the cell cycle.
Figure 4. Pretreatment with scFv-Fc or EM164 followed by doxorubicin prevented G2-M phase arrest.
LCC6 cells were seeded in 60-mm plates at a density of 4× 105 per plate. After 24 hours serum starving, the cells were treated with 100 ng/ml doxorubicin, 30 μg/ml scFv-Fc (A), 20 μg/ml AVE1642 (B) or antibodies in combination with DOX simultaneously or sequentially for 48 hours as described under Material and Methods, and then cells were stained with propidium iodide and analyzed by flow cytometry. The experiment was repeated three times with similar results, and a representative experiment is shown.
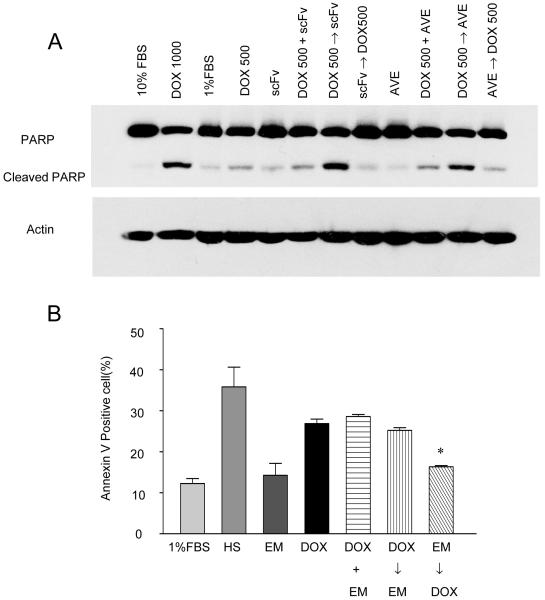
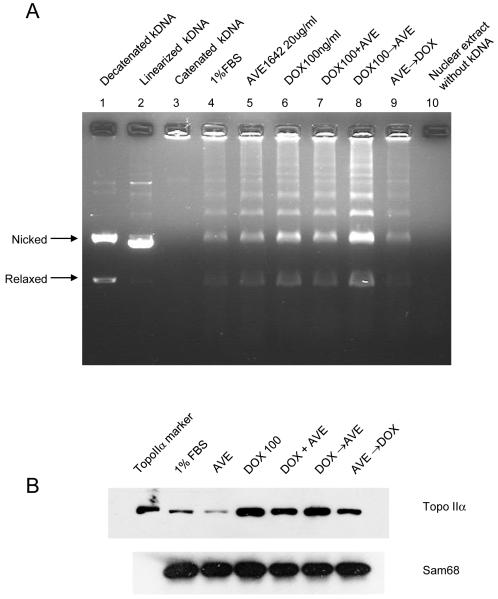
Pretreatment of AVE1642 followed by doxorubicin decreased topoisomerase II activity and protein level
Since the effects of sequencing were seen with drugs that affect topoisomerase II (topo II), such as doxorubicin and etoposide, we hypothesized that blockade of IGF1R may affect topo II activity. We measured topo II activity in nuclear extracts by the decatenation of kDNA assay. This assay measures the ability of topo II to catalyze strand passage between two double-stranded DNA segments. Topo II decatenation activity (per identical amounts of nuclear extract proteins) was approximately 5-fold lower in the sequence AVE1642 followed by doxorubicin extracts as compared with doxorubicin alone (Figure 5A, lane 6 versus lane 9). In contrast, nuclear extracts from cells, with sequential treatment of doxorubicin followed by AVE1642, had significantly increased topo II activity (Fig. 5A lane 6 versus lane 8). To determine if the altered topo II activity was related to level of topo II protein, we determined topo II levels in cellular extracts by immunoblotting. AVE1642 followed by doxorubicin caused a 2-fold decrease in Topo II levels (Figure 5B). Taken together, these data suggest that decreased topo II activity by pretreatment with AVE1642 led directly to a decreased sensitivity of LCC6 cells to topo II poisons like doxorubicin. In contrast, post-doxorubicin blockade of IGF1R increased the activity of topo II and increased sensitivity of LCC6 cells to doxorubicin.
Figure 5. Pretreatment of AVE1642 followed by doxorubicin decreased topoisomerase II activity and protein level.
A, Decatenation assay. LCC6 cells were starved in serum-free media for 24 hours and then treated with AVE1642 (20μg/ml), DOX (100ng/ml) alone or in combination simultaneously or sequentially for 48 hours. Nuclear extracts were incubated with kinetoplast DNA at 37°C for 15 min. After gel electrophoresis in 1% agarose, the decatenated products containing nicked circular and relaxed circular DNA were determined. B, Topo IIα protein levels. Nuclear extracts were prepared for LCC6 cell treated with AVE1642 (20μg/ml), DOX (100ng/ml) alone or in combination simultaneously or sequentially for 48 hours. After quantification, 50 μg of nuclear extract were immunoblotted for topoIIα with purified topoIIα control. Sam 68 is the loading control.
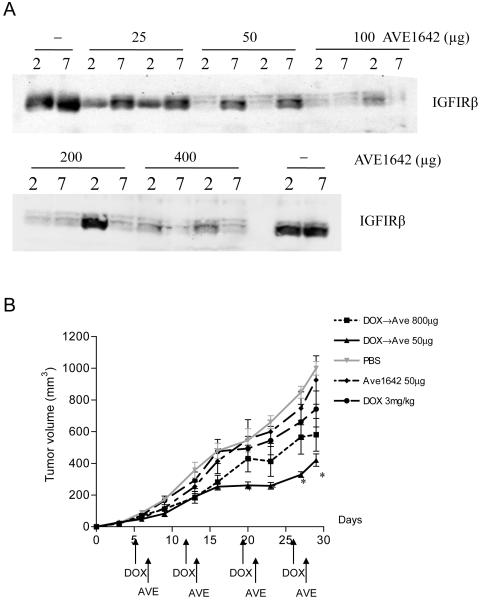
Sequential treatment of doxorubicin followed by a low dose of AVE1642 significantly inhibited xenograft tumor growth and metastasis
Our in vitro data suggest that blockade of IGF1R after doxorubicin was the most effective combination. Moreover, inhibition of IGF1R prior to doxorubicin might interfere with the cytotoxic effects of topo II inhibitors. Since antibodies have a very long half-life in vivo, we next explored whether low doses of antibody would allow IGF1R to recover over the course of a week. Mice bearing two xenograft tumors implanted in the mammary fat pad of opposite sides were studied. When xenograft tumors were formed, mice were treated with varying doses of AVE1642 by intraperitoneal injection. Tumors were removed from mice at 2 and 7 days after AVE1642 treatments. Fig. 6A shows that all doses of AVE1642 suppressed IGF1R levels at 2 days after treatment. Low doses of antibody (25 and 50 μg/mouse) allowed IGF1R to recover to pre-treatment levels at 7 days. While some individual variation was seen at day 2 (200μg dose), higher doses of antibody (100, 200 and 400 μg/mouse) suppressed IGF1R levels for the entire 7 days.
Figure 6. Sequential treatment of doxorubicin followed by a low dose of AVE1642 significantly inhibited mice xenografts growth and metastasis.
A, AVE1642 dose dependently decreased the IGFIR levels in vivo. Female athymic mice were injected with LCC6 cells in opposite mammary fat pads to form xenograft tumors. When tumors had reached a volume of ∼80 mm3, mice were treated with AVE1642. Tumors were dissected 2 and 7 days after AVE1642 treatment. A total of 100 μg of tumor extracts were immunoblotted for total IGF-1Rß levels. B, Established breast cancer xenografts (100 mm3) were treated with PBS, DOX (3 mg/kg/week each, i.p.), AVE1642 (50 μg/mouse/week, i.p.), DOX 24 hours followed by AVE1642 50 μg or DOX 24 hours followed by AVE1642 800 μg four times at a 7 day interval. Tumors were measured every 3 days. C, Analysis of lung micrometastatic deposits. 24 hours after the final treatment with AVE1642 and doxorubicin, mice were sacrificed. The lung of each mouse was fixed, embedded, sectioned, and stained with hematoxylin and eosin, and examined microscopically for metastatic deposits. Results are presented as mean ± S.E. (n=5) *P<0.05 vs DOX alone. D, Seven days after the final treatment, mice were sacrificed, and tumor samples were frozen in liquid nitrogen and homogenized in TNESV buffer. A total of 100 μg of tumor extract and 40 μg of LCC6 cell lysates were immunoblotted for IGF-IR, and MAPK.
Since low doses of AVE1642 suppressed IGF1R expression immediately after dosing, but allowed recovery after 7 days, we used a low and high dose of antibody to model our in vitro findings showing that IGF1R suppression at the time of doxorubicin was deleterious. As shown in Figure 6B, doxorubicin and AVE1642 alone had little effect on LCC6 xenograft growth. A low dose (50 μg/mouse) and a high dose (800 μg/mouse) of AVE1642 were used in combination with doxorubicin. This high dose of AVE1642 was based on our previously published results demonstrating tumor inhibition of MCF-7 cells (30). Doxorubicin followed with the low dose of AVE1642 (four repeated weekly cycles) best resembled the in vitro optimal sequence and was most effective in vivo. Since high dose of AVE1642 (>100 μg/mouse) resulted in sustained IGF1R downregulation, repeated 4 cycles of doxorubicin followed by 800 μg/mouse AVE1642 mimicked the in vitro sequence of antibody pretreatment followed by doxorubicin. This higher dose of antibody was superior to doxorubicin alone, but less effective than the low dose of AVE1642.
It has been reported that IGF1R is involved in invasion and metastasis in several tumor types (23, 31, 32). LCC6 has been reported to metastasize from the mammary fat pad to the lungs of mice (23). We investigated whether the sequential combination doxorubicin with AVE1642 influenced lung metastasis in vivo. At the end of the treatment period, lungs were harvested and examined by histological examination for metastases. Figure 6C demonstrates that the numbers of pulmonary metastases were reduced in the doxorubicin plus low dose AVE1642 treated animals.
Anti-IGF1R antibodies commonly downregulate receptor levels and it is felt that this is a common mechanism of action (10). To determine if our dosing scheme affected IGF1R levels in a manner we expected, we examined tumor IGF1R levels one week after treatment. Fig. 6D showed that IGF1R levels were not affected in control and doxorubicin treated animals; 50 μg AVE1642 only mildly inhibited the IGF1R levels 7 days after treatment and doxorubicin followed by 800 μg AVE1642 dramatically inhibited the IGF1R for at least 7 days. Since the sequence of doxorubicin followed 50 μg AVE1642 showed a better anti-tumor effect compared with 800 μg AVE1642, chronic downregulation of IGF1R by high-doses of antibody may not be the optimal strategy when combining with DNA damaging agents.
Discussion
Several lines of experimental evidence validate IGF1R signaling blockade as an important anticancer target that may prove clinically useful in combination with chemotherapy. Treatment with αIR3 has been shown to enhance the effect of chemotherapeutic agent doxorubicin and vincristine against Ewing’s sarcoma cells (33). An almost complete inhibition of non small lung cancer cells (A549) xenograft growth was observed when mice were treated with anti-IGF1R antibody H7C10 combined with vinorelbine (17). Another human anti-IGF1R antibody CP-751,871 was shown to enhance the anti-tumor growth effect of chemotherapy in several different cell lines (16). Hug et. al reported that tamoxifen (TAM) protected cells from the cytotoxicity of both chemotherapy agents 5-fluorouracil and doxorubicin (34). Data from recent randomized trials also demonstrated a clinically antagonistic effect of TAM on concurrent cytotoxic chemotherapy and beneficial effect of sequential chemotherapy and TAM (18, 35). Similarly, inhibition of HER2 by trastuzumab followed by paclitaxel increased resistance (19). These preclinical and clinical studies demonstrated that sequencing need to be considered when combined the chemotherapy with target therapy. Several anti-IGF1R antibodies are currently being evaluated in phase I or II clinical trials (36). Although it is possible that combination of anti-IGF1R antibodies with cytotoxic chemotherapy might be more beneficial than single agents alone, it is also possible that disruption of IGF1R signaling might interfere with the cytotoxic effects. Thus, the optimal schedule for the combination therapy remains to be established.
Our study assesses the effect of two anti-IGF1R antibodies, scFv-Fc and EM164 (humanized version, AVE1642) given concurrently or sequentially, in combination with several widely used cytotoxic drugs. Our study demonstrates several significant considerations for combination therapy. First, there are important sequence dependent effects when combining some types of chemotherapy with anti-IGF1R antibodies, with drug followed by anti-IGF1R antibody as the best sequence. Second, low doses of antibody may be more effective by simulating this sequence dependent effect in vivo. Third, inhibition of IGF1R prior to exposure to doxorubicin may interfere with the cytotoxic effects of the drug.
Doxorubicin exerts its effects on cancer cells via two different mechanisms: first, it intercalates between the bases of DNA and blocks DNA synthesis and transcription; second, it inhibits the activity of topoisomerase II and leads to breaks in the genomic DNA (37). Topo II has two isoforms, IIα and IIβ, and the topo IIα exhibiting cell cycle regulation of its expression that is elevated during S phase and that peaks at G2/M phase (38). Furthermore, tumor cell sensitivity to topo II inhibitors has been positively correlated with increased nuclear topo IIα levels (39, 40). Our cell cycle analysis revealed that, when cells were treated with doxorubicin at sub-toxic concentration, most cells accumulated in the G2-M phase reflecting doxorubicin’s mechanism of action; in contrast, pretreatment with scFv-Fc and AVE1642 caused an increase in G0/G1 and S phase accumulation (Fig. 4). Since topo IIα expression is regulated by cell cycle and relates to drug sensitivity, we measured the topo IIα expression and activity of different groups. Our experiments demonstrated that pretreatment with anti-IGF1R antibodies decreased both topo IIα level and enzymatic activity, and decreased sensitivity to doxorubicin. In contrast, the sequence doxorubicin followed by AVE1642 increased the topo II activity and was associated with increased sensitivity of doxorubicin (Fig.5). The sequence of pretreatment with anti-IGF1R antibodies resulted in fewer cells in G2/M phase compared with other sequences, consistent with the reduction in topo IIα levels. Son et. al. showed that the activity of topo II was reduced in a doxorubicin-resistant human stomach cancer cell lines (41). Another report showed that cytotoxicity of doxorubicin was inhibited by anti-ErbB2 antibody trastuzumab and caused by a decrease of topo II protein and activity (42). These data underscore the correlation of topo II protein level with doxorubicin sensitivity; increases in topo IIα expression is associated with sensitivity to the doxorubicin presumably due to increased target on which the drug acts. Although, a direct mechanism between IGF signaling and topo II has not been demonstrated, our results suggest that alteration in topo II activity may be one possible mechanism to explain the sequence-dependent effect in combination of anti-IGF1R antibody with doxorubicin.
Down-regulation of IGF1R expression by monoclonal antibodies has been shown in vitro and in vivo (30). Our in vitro data suggested that down-regulation of the receptor before chemotherapy would attenuate the cytotoxicity of doxorubicin. Extending these findings to an in vivo mouse model, LCC6 xenograft growth was significantly inhibited with doxorubicin followed by AVE1642 compared with either treatment alone (Fig. 6B). As predicted by the in vitro data, a lower dose of AVE1642 was more effective in combination with doxorubicin than the higher dose. Our data show that transient downregulation of receptor by the low dose of antibody was associated with a more substantial tumor inhibition in combination with doxorubicin. Previous data from our laboratory showed that inhibition of IGF1R may prevent metastases to lung in LCC6 cells xenograft tumor. Here, we tested effectiveness of combined therapy against lung metastasis. Similar to the growth of the xenograft tumor, the best results were obtained with doxorubicin followed by transient downregulation of IGF1R. One hypothesis to explain the lack of benefit for the sustained downregulation of receptor might be the decreased topoisomerase II protein and activity in vivo seen in these experimental conditions. Our data show that sustained downregulation of IGF1R impairs sensitivity of doxorubicin by lowering topo IIα level. The status of topoismoerase II in combination therapy also needs further in-depth investigation. It is noteworthy that not all chemotherapies show this sequence dependency. Furthermore, it is uncertain if cells dependent on IGF1R for proliferation would also have similar sequence-dependent effects. Cohen at al. demonstrated that low doses of a monoclonal antibody were ineffective at suppressing growth of a mouse fibroblast cell line transfected with IGF1R (16). These data have been taken to suggest that continuous suppression of IGF1R is necessary for single agent activity, but lower doses of IGF1R inhibitors with chemotherapy have not been studied in IGF1R-dependent cells. Further in vivo modeling of these sequence effects with additional classes of chemotherapy and cell lines need to be pursued.
In summary, our studies have important implications for IGF1R targeted cancer therapy. First, downregulation of IGF1R may not affect tumor growth but could sensitize cells to apoptotic insults. Secondly, the sequencing of IGF1R inhibition with chemotherapy may distinguish between synergy and interference. This observation is important, as several anti-IGF1R antibodies including AVE1642 are being evaluated in phase I /II clinical trials as single agents and in combination with chemotherapy. The antibody dosages used in these trials will likely result in sustained downregulation of IGF1R. While this should clearly extinguish IGF1R signaling, the effects on the response to DNA damaging agents might be counterproductive. Third, given the potential toxicity on glucose metabolism of chronic IGF1R inhibition, it is possible that low doses of antibodies might have reduced toxicity. Our study suggests that careful consideration of sequencing and dose is necessary when considering combining anti-IGF1R strategies with chemotherapy.
Acknowledgments
We thank Yoko Fujita-Yamaguchi for providing the hybridoma that produces scFv-Fc.
Grant support: This work was supported by: NIH grant RO1 CA74285 (D. Yee) and USPHS Cancer Center Support grant P30 CA77398 from the National Cancer Institute.
Footnotes
Statement of Translational Relevance
Disruption of type I insulin-like growth factor receptor (IGF1R) signaling has emerged as an important target in cancer therapy. While interruption of receptor signaling may have single agent activity, combining this strategy with other cytotoxic agents has appeal. These data demonstrate that the sequencing of IGF1R blockade plays a critical role in determining efficacy. Optimal anti-cancer effects were seen when chemotherapy was given prior to exposure to an anti-IGF1R monoclonal antibody. Moreover, lower doses of antibody, which resulted in transient receptor suppression in vivo, were more effective than continuous receptor suppression caused by higher antibody doses. Thus, sequencing of cytotoxic chemotherapy with IGF1R blockade should be considered in the design of clinical trials.
Reference
- 1.Hortobagyi GN. Opportunities and challenges in the development of targeted therapies. Semin Oncol. 2004;31:21–7. doi: 10.1053/j.seminoncol.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Zeng X, Yee D. Insulin-like growth factors and breast cancer therapy. Adv Exp Med Biol. 2007;608:101–12. doi: 10.1007/978-0-387-74039-3_7. [DOI] [PubMed] [Google Scholar]
- 3.Wong SF. Cetuximab: an epidermal growth factor receptor monoclonal antibody for the treatment of colorectal cancer. Clin Ther. 2005;27:684–94. doi: 10.1016/j.clinthera.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 4.Pegram MD, Konecny GE, O’Callaghan C, Beryt M, Pietras R, Slamon DJ. Rational combinations of trastuzumab with chemotherapeutic drugs used in the treatment of breast cancer. J Natl Cancer Inst. 2004;96:739–49. doi: 10.1093/jnci/djh131. [DOI] [PubMed] [Google Scholar]
- 5.Viani GA, Afonso SL, Stefano EJ, De Fendi LI, Soares FV. Adjuvant trastuzumab in the treatment of her-2-positive early breast cancer: a meta-analysis of published randomized trials. BMC Cancer. 2007;7:153. doi: 10.1186/1471-2407-7-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pollak MN, Schernhammer ES, Hankinson SE. Insulin-like growth factors and neoplasia. Nat Rev Cancer. 2004;4:505–18. doi: 10.1038/nrc1387. [DOI] [PubMed] [Google Scholar]
- 7.Byron SA, Yee D. Potential therapeutic strategies to interrupt insulin-like growth factor signaling in breast cancer. Semin Oncol. 2003;30:125–32. doi: 10.1053/j.seminoncol.2003.08.014. [DOI] [PubMed] [Google Scholar]
- 8.Wu JD, Odman A, Higgins LM, et al. In vivo effects of the human type I insulin-like growth factor receptor antibody A12 on androgen-dependent and androgen-independent xenograft human prostate tumors. Clin Cancer Res. 2005;11:3065–74. doi: 10.1158/1078-0432.CCR-04-1586. [DOI] [PubMed] [Google Scholar]
- 9.Sachdev D, Yee D. Disrupting insulin-like growth factor signaling as a potential cancer therapy. Mol Cancer Ther. 2007;6:1–12. doi: 10.1158/1535-7163.MCT-06-0080. [DOI] [PubMed] [Google Scholar]
- 10.Sachdev D, Li SL, Hartell JS, Fujita-Yamaguchi Y, Miller JS, Yee D. A chimeric humanized single-chain antibody against the type I insulin-like growth factor (IGF) receptor renders breast cancer cells refractory to the mitogenic effects of IGF-I. Cancer Res. 2003;63:627–35. [PubMed] [Google Scholar]
- 11.Ye JJ, Liang SJ, Guo N, et al. Combined effects of tamoxifen and a chimeric humanized single chain antibody against the type I IGF receptor on breast tumor growth in vivo. Horm Metab Res. 2003;35:836–42. doi: 10.1055/s-2004-814145. [DOI] [PubMed] [Google Scholar]
- 12.Maloney EK, McLaughlin JL, Dagdigian NE, et al. An anti-insulin-like growth factor I receptor antibody that is a potent inhibitor of cancer cell proliferation. Cancer Res. 2003;63:5073–83. [PubMed] [Google Scholar]
- 13.Dunn SE, Hardman RA, Kari FW, Barrett JC. Insulin-like growth factor 1 (IGF-1) alters drug sensitivity of HBL100 human breast cancer cells by inhibition of apoptosis induced by diverse anticancer drugs. Cancer Res. 1997;57:2687–93. [PubMed] [Google Scholar]
- 14.Lu Y, Zi X, Pollak M. Molecular mechanisms underlying IGF-I-induced attenuation of the growth-inhibitory activity of trastuzumab (Herceptin) on SKBR3 breast cancer cells. Int J Cancer. 2004;108:334–41. doi: 10.1002/ijc.11445. [DOI] [PubMed] [Google Scholar]
- 15.Yu D, Watanabe H, Shibuya H, Miura M. Redundancy of radioresistant signaling pathways originating from insulin-like growth factor I receptor. J Biol Chem. 2003;278:6702–9. doi: 10.1074/jbc.M209809200. [DOI] [PubMed] [Google Scholar]
- 16.Cohen BD, Baker DA, Soderstrom C, et al. Combination therapy enhances the inhibition of tumor growth with the fully human anti-type 1 insulin-like growth factor receptor monoclonal antibody CP-751,871. Clin Cancer Res. 2005;11:2063–73. doi: 10.1158/1078-0432.CCR-04-1070. [DOI] [PubMed] [Google Scholar]
- 17.Goetsch L, Gonzalez A, Leger O, et al. A recombinant humanized anti-insulin-like growth factor receptor type I antibody (h7C10) enhances the antitumor activity of vinorelbine and anti-epidermal growth factor receptor therapy against human cancer xenografts. Int J Cancer. 2005;113:316–28. doi: 10.1002/ijc.20543. [DOI] [PubMed] [Google Scholar]
- 18.Pierce LJ, Hutchins LF, Green SR, et al. Sequencing of tamoxifen and radiotherapy after breast-conserving surgery in early-stage breast cancer. J Clin Oncol. 2005;23:24–9. doi: 10.1200/JCO.2005.01.198. [DOI] [PubMed] [Google Scholar]
- 19.Abuharbeid S, Apel J, Zugmaier G, et al. Inhibition of HER-2 by three independent targeting strategies increases paclitaxel resistance of SKOV-3 ovarian carcinoma cells. Naunyn Schmiedebergs Arch Pharmacol. 2005;371:141–51. doi: 10.1007/s00210-004-1016-4. [DOI] [PubMed] [Google Scholar]
- 20.Li SL, Liang SJ, Guo N, Wu AM, Fujita-Yamaguchi Y. Single-chain antibodies against human insulin-like growth factor I receptor: expression, purification, and effect on tumor growth. Cancer Immunol Immunother. 2000;49:243–52. doi: 10.1007/s002620000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Twentyman PR, Luscombe M. A study of some variables in a tetrazolium dye (MTT) based assay for cell growth and chemosensitivity. Br J Cancer. 1987;56:279–85. doi: 10.1038/bjc.1987.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gooch JL, Van Den Berg CL, Yee D. Insulin-like growth factor (IGF)-I rescues breast cancer cells from chemotherapy-induced cell death--proliferative and anti-apoptotic effects. Breast Cancer Res Treat. 1999;56:1–10. doi: 10.1023/a:1006208721167. [DOI] [PubMed] [Google Scholar]
- 23.Sachdev D, Hartell JS, Lee AV, Zhang X, Yee D. A dominant negative type I insulin-like growth factor receptor inhibits metastasis of human cancer cells. J Biol Chem. 2004;279:5017–24. doi: 10.1074/jbc.M305403200. [DOI] [PubMed] [Google Scholar]
- 24.Rae JM, Creighton CJ, Meck JM, Haddad BR, Johnson MD. MDA-MB-435 cells are derived from M14 melanoma cells--a loss for breast cancer, but a boon for melanoma research. Breast Cancer Res Treat. 2007;104:13–9. doi: 10.1007/s10549-006-9392-8. [DOI] [PubMed] [Google Scholar]
- 25.Rochester MA, Riedemann J, Hellawell GO, Brewster SF, Macaulay VM. Silencing of the IGF1R gene enhances sensitivity to DNA-damaging agents in both PTEN wild-type and mutant human prostate cancer. Cancer Gene Ther. 2005;12:90–100. doi: 10.1038/sj.cgt.7700775. [DOI] [PubMed] [Google Scholar]
- 26.Muller I, Niethammer D, Bruchelt G. Anthracycline-derived chemotherapeutics in apoptosis and free radical cytotoxicity (Review) International journal of molecular medicine. 1998;1:491–4. doi: 10.3892/ijmm.1.2.491. [DOI] [PubMed] [Google Scholar]
- 27.Baldwin EL, Osheroff N. Etoposide, topoisomerase II and cancer. Curr Med Chem Anticancer Agents. 2005;5:363–72. doi: 10.2174/1568011054222364. [DOI] [PubMed] [Google Scholar]
- 28.Longley DB, Harkin DP, Johnston PG. 5-fluorouracil: mechanisms of action and clinical strategies. Nat Rev Cancer. 2003;3:330–8. doi: 10.1038/nrc1074. [DOI] [PubMed] [Google Scholar]
- 29.Bar-On O, Shapira M, Hershko DD. Differential effects of doxorubicin treatment on cell cycle arrest and Skp2 expression in breast cancer cells. Anticancer Drugs. 2007;18:1113–21. doi: 10.1097/CAD.0b013e3282ef4571. [DOI] [PubMed] [Google Scholar]
- 30.Sachdev D, Singh R, Fujita-Yamaguchi Y, Yee D. Down-regulation of insulin receptor by antibodies against the type I insulin-like growth factor receptor: implications for anti-insulin-like growth factor therapy in breast cancer. Cancer Res. 2006;66:2391–402. doi: 10.1158/0008-5472.CAN-05-3126. [DOI] [PubMed] [Google Scholar]
- 31.Manara MC, Landuzzi L, Nanni P, et al. Preclinical in vivo study of new insulin-like growth factor-I receptor--specific inhibitor in Ewing’s sarcoma. Clin Cancer Res. 2007;13:1322–30. doi: 10.1158/1078-0432.CCR-06-1518. [DOI] [PubMed] [Google Scholar]
- 32.Samani AA, Yakar S, LeRoith D, Brodt P. The role of the IGF system in cancer growth and metastasis: overview and recent insights. Endocr Rev. 2007;28:20–47. doi: 10.1210/er.2006-0001. [DOI] [PubMed] [Google Scholar]
- 33.Benini S, Manara MC, Baldini N, et al. Inhibition of insulin-like growth factor I receptor increases the antitumor activity of doxorubicin and vincristine against Ewing’s sarcoma cells. Clin Cancer Res. 2001;7:1790–7. [PubMed] [Google Scholar]
- 34.Hug V, Hortobagyi GN, Drewinko B, Finders M. Tamoxifen-citrate counteracts the antitumor effects of cytotoxic drugs in vitro. J Clin Oncol. 1985;3:1672–7. doi: 10.1200/JCO.1985.3.12.1672. [DOI] [PubMed] [Google Scholar]
- 35.Pico C, Martin M, Jara C, et al. Epirubicin-cyclophosphamide adjuvant chemotherapy plus tamoxifen administered concurrently versus sequentially: randomized phase III trial in postmenopausal node-positive breast cancer patients. A GEICAM 9401 study. Ann Oncol. 2004;15:79–87. doi: 10.1093/annonc/mdh016. [DOI] [PubMed] [Google Scholar]
- 36.Haluska P, Shaw HM, Batzel GN, et al. Phase I dose escalation study of the anti insulin-like growth factor-I receptor monoclonal antibody CP-751,871 in patients with refractory solid tumors. Clin Cancer Res. 2007;13:5834–40. doi: 10.1158/1078-0432.CCR-07-1118. [DOI] [PubMed] [Google Scholar]
- 37.Binaschi M, Bigioni M, Cipollone A, et al. Anthracyclines: selected new developments. Curr Med Chem Anticancer Agents. 2001;1:113–30. doi: 10.2174/1568011013354723. [DOI] [PubMed] [Google Scholar]
- 38.Woessner RD, Mattern MR, Mirabelli CK, Johnson RK, Drake FH. Proliferation- and cell cycle-dependent differences in expression of the 170 kilodalton and 180 kilodalton forms of topoisomerase II in NIH-3T3 cells. Cell Growth Differ. 1991;2:209–14. [PubMed] [Google Scholar]
- 39.Asano T, Kleinerman ES, Zwelling LA, Zhou Z, Fukunaga Y. Adenovirus-mediated human topoisomerase IIalpha gene transfer increases the sensitivity of etoposide-resistant human and mouse breast cancer cells. Acta oncologica (Stockholm, Sweden) 2005;44:240–7. doi: 10.1080/02841860510029653. [DOI] [PubMed] [Google Scholar]
- 40.Dingemans AM, Witlox MA, Stallaert RA, van der Valk P, Postmus PE, Giaccone G. Expression of DNA topoisomerase IIalpha and topoisomerase IIbeta genes predicts survival and response to chemotherapy in patients with small cell lung cancer. Clin Cancer Res. 1999;5:2048–58. [PubMed] [Google Scholar]
- 41.Son YS, Suh JM, Ahn SH, et al. Reduced activity of topoisomerase II in an Adriamycin-resistant human stomach-adenocarcinoma cell line. Cancer Chemother Pharmacol. 1998;41:353–60. doi: 10.1007/s002800050751. [DOI] [PubMed] [Google Scholar]
- 42.Harris LN, Yang L, Liotcheva V, et al. Induction of topoisomerase II activity after ErbB2 activation is associated with a differential response to breast cancer chemotherapy. Clin Cancer Res. 2001;7:1497–504. [PubMed] [Google Scholar]