Abstract
Recent guidelines recommending more aggressive blood pressure control in patients with chronic kidney disease have unknown impact. We assessed trends in and predictors of blood pressure control in 8,829 adult NHANES 1999–2006 participants with hypertension (self-report, measured blood pressure, or use of anti-hypertensive medications), without (n=7,178) and with (n=1,651) chronic kidney disease. Uncontrolled blood pressure was defined as: general definition, systolic blood pressure ≥140/diastolic blood pressure ≥90 mmHg; disease-specific definition, ≥130/≥85 (1999–2002) and ≥130/≥80 (2003–2006) mmHg for those with chronic kidney disease (estimated GFR <60 ml/min/1.73 m2) or diabetes (self-report). Proportions with uncontrolled blood pressure in 1999–2006 were greater in those with chronic kidney disease versus those without chronic kidney disease [51.5% vs. 48.7% (general definition, P=0.122) and 68.8% vs. 51.7% (disease-specific definition; P<0.001)]. In those with chronic kidney disease, there were significant decreases in uncontrolled blood pressure over time [55.9% to 47.8% (general definition, P=0.011)]. With adjustment for demographic, socioeconomic, and clinical variables, older age (P<0.001) and lack of anti-hypertensive treatment (P<0.001) were associated with uncontrolled blood pressure, regardless of chronic kidney disease status; non-white race (P=0.002) was associated in those without chronic kidney disease, whereas female sex (P=0.030) was associated in those with chronic kidney disease. Multiple medications (P<0.001) and angiotensin-converting enzyme inhibitors/angiotensin II receptor blockers (P=0.001) were associated with less uncontrolled blood pressure. Although some improvement has occurred over time, uncontrolled blood pressure remains highly prevalent, especially in chronic kidney disease and in non-whites, older persons, and females. Therapy appears suboptimal.
Keywords: blood pressure control, prevalence, trends, risk factors, treatment guidelines, chronic kidney disease
Introduction
Published guidelines for blood pressure (BP) control include lower BP targets among those with chronic kidney disease (CKD) or diabetes (1;2), compared to those without these conditions. Lower BP is generally well known to be associated with decreased risk of kidney disease progression, cardiovascular events, and death (3;4). Despite the recognized importance of controlling BP, control in the general population has previously been shown to be fairly poor, ranging from 29% to 60%, depending on age, sex, and race (5–7). Similarly, patients with CKD have also been shown to have low rates of BP control (6;8–10). It has been shown that BP control increased from 1988–1994 to 1999–2004 (11), but whether BP control has improved over recent years is unclear. Moreover, factors that predict uncontrolled BP, including guideline-concordant care, are not well-known in the setting of CKD.
Previous studies of BP control in persons with CKD were generally performed within subpopulations or in less representative cohort or screening studies. Using data from the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2006, we examined not only the extent of uncontrolled BP in the adult U.S. non-CKD and CKD populations but also whether uncontrolled BP improved over this period. We also compared the estimates obtained using both general and (more stringent) disease-specific guidelines for defining BP control. Additionally, we examined and compared potential treatment and risk factors for uncontrolled BP by CKD status.
Methods
Study Design
The NHANES surveys are currently conducted every 2 years by the National Center for Health Statistics to examine disease prevalence and trends over time in representative samples of non-institutionalized U.S. civilian residents (12). The survey consists of a standardized in-home interview and a physical examination and blood and urine collection at a mobile examination center (MEC), for which participants give informed consent. The protocol was approved by an institutional review board.
We examined combined data from the 1999–2000 (13), 2001–2002 (14), and 2003–2004 (15), and 2005–2006 (16) NHANES surveys. Our study was limited to 8,829 NHANES participants from 1999–2006 who were at least 20 years old, underwent a MEC exam, and had hypertension. Those participants without measured BP or with missing age, sex, race, or creatinine were excluded.
Measurements
A standardized protocol (17) for measurements of auscultatory BPs was executed during the MEC visit by a trained physician with a mercury sphygmomanometer using appropriate cuff sizes. Recorded systolic BP (SBP) and diastolic BP (DBP) are the mean of three measurements separated by 30 seconds following a 5-minute rest period. Averages of three (sometimes four) recordings were used; individual pulse pressures were calculated for each recording and averaged.
Self-reported information on demographics (age, sex, race), socioeconomic status (education, insurance, income), health conditions (hypertension, diabetes), health behaviors (smoking, obesity) and routine site of healthcare were obtained during the interview portions of the surveys. Additionally, prescription medication information was obtained during the interview, with the interviewer recording the names of medications from the bottles provided by the participant. Height and weight were measured during the MEC exam. Random spot urine samples were obtained, and urine albumin and creatinine were measured using frozen specimens. Urine albumin was measured using solid-phase fluorescence immunoassay; urine creatinine was measured using the modified Jaffe kinetic method in the same laboratory. Serum creatinine was measured by the modified kinetic method of Jaffe using different analyzers in different survey years.
Definitions
Uncontrolled BP was defined in those with hypertension two ways, per Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC) guidelines. By the general definition, BP was considered uncontrolled if SBP was ≥140 mmHg or DBP was ≥90 mmHg. By the disease-specific definition, BP was considered uncontrolled in those with CKD or diabetes if SBP was 130 mmHg or DBP was ≥85 (1999–2002) or ≥80 (2003–2006) mmHg, according to the JNC-VI (2) and JNC-VII (1) criteria, respectively; or, in those without these conditions, if SBP was ≥140 mmHg or DBP was ≥90 mmHg.
Hypertension was defined by self-reported hypertension, high measured BP, or use of antihypertensive medications. Self-reported hypertension was defined by answer of “yes” to the question “have you ever been told by a doctor or other health professional that you have hypertension, also called high blood pressure.” SBP ≥140 or DBP ≥90 mmHg was considered high measured BP. The use of hypertension medications was defined as any prescription for diuretics, angiotensin-converting enzyme (ACE) inhibitors, alpha- and/or beta-blockers, calcium channel blockers, angiotensin II receptor blockers (ARBs), central alpha-2 agonists, aldosterone receptor blockers, or direct vasodilators, prescribed either alone or in combination.
CKD was defined as estimated glomerular filtration rate (eGFR) >15 and <60 ml/min/1.73 m2 (stage 3 or 4 CKD according to the Kidney Disease Outcomes Quality Initiative guidelines (18)). CKD was limited to stages 3 and 4 to avoid potential misclassification due to short-term variability in microalbuminuria in stages 1 and 2 (19). eGFR was calculated according to the modified MDRD Study equation for calibrated creatinine: eGFR = 175 × [(calibrated serum creatinine in mg/dl)−1.154] × age−0.203 × (0.742 if female) × (1.210 if African-American) (20, 21). Serum creatinine was calibrated for adherence to the Cleveland Clinic protocol for the 1999–2000 and 2005–2006 surveys using regression formulas provided by NHANES; no correction was required for the 2001–2002 or 2003–2004 surveys (22). Diabetes was defined by answer of “yes” to the question “have you ever been told by a doctor or other health professional that you have diabetes, or sugar diabetes.” Albuminuria was considered to be present at urinary albumin-to-creatinine ratios of 30–299 mg/g (microalbuminuria) and ≥300 mg/g (macroalbuminuria).
Statistical Methods
The proportion with uncontrolled BP was calculated by the general and disease-specific definitions and by CKD status. Variance of proportions was estimated with Taylor series linearization. The proportion with uncontrolled BP was also calculated by patient characteristics and by survey year. These characteristics were examined in logistic models predicting uncontrolled BP, with adjustment for possible confounders, including demographics, socioeconomic status, diabetes, obesity, treatment with hypertension medications, and survey years (pre- and post-JNC-VII guidelines). Odds ratios and adjusted percentages were obtained from these models; only adjusted percentages are shown since the odds ratios are likely to overestimate the relative risk in the setting of a condition as common as uncontrolled BP.
All analyses were performed using the SVY commands in Stata v. 10.0 to account for study design weights, strata, and pseudostrata. Appropriate NHANES 8-year MEC weights were used; 8-year weights were calculated as: 8-year weight=1/2 × 4-year weight (if survey year = 1999–2002) and 8-year weight=1/2 × 2-year weight (if survey year = 2003–2006) (23).
Results
Participant Characteristics by CKD
Participants with hypertension who had CKD had higher SBP and lower DBP than those without CKD (Table 1). Those with CKD were also significantly older; more likely to be female or white, to have a lower income, to have diabetes and albuminuria, and to be treated with anti-hypertensive medications; and less likely to have a high school education and to be obese. Those with CKD were also more likely to be on multiple medications and to be on ACE inhibitors/ARBs or diuretics than those without CKD. The proportions on ACE inhibitors/ARBs increased from 1999–2002 to 2003–2006 (13.8% to 18.8%, P<0.001), while the proportion on other medications declined (3.6% to 2.2%, P<0.001). Among those on treatment in 1999–2006, a lower proportion of those with CKD (36.5%) were treated with ACE inhibitors/ARBs, compared to those without CKD (40.9%; P=0.035), but those with CKD were more likely to be on multiple anti-hypertensive medications (37.9% vs. 27.3%, P<0.001).
Table 1.
Characteristics of NHANES 1999–2006 participants with hypertension (self-reported hypertension, high measured BP, or use of antihypertensive medications), by presence of CKD (stages 3 and 4)
| Characteristic | No CKD | CKD | P |
|---|---|---|---|
| N | 7,178 | 1,651 | — |
| Mean Systolic Blood Pressure, mmHg | 135.9 (135.0–136.9) | 141.3 (139.7–142.9) | <0.001 |
| Mean Diastolic Blood Pressure, mmHg | 76.1 (75.4–76.8) | 67.5 (66.1–68.9) | <0.001 |
| Mean Pulse Pressure, mmHg | 59.8 (58.9–60.7) | 73.8 (71.6–75.9) | <0.001 |
| Survey Year | |||
| 1999–2002 | 46.4 (42.9–50.1) | 45.3 (39.9–50.8) | 0.623 |
| 2003–2006 | 53.6 (49.9–57.1) | 54.7 (49.2–60.2) | |
| Demographics | |||
| Age | |||
| 20–39 | 25.5 (23.5–27.8) | 3.6 (2.5–5.1) | <0.001 |
| 40–59 | 43.9 (42.0–45.7) | 18.5 (15.7–21.7) | |
| 60–69 | 15.3 (14.1–16.7) | 17.2 (15.0–19.7) | |
| 70+ | 15.3 (14.0–16.7) | 60.7 (57.3–64.1) | |
| Sex | |||
| Male | 49.3 (48.1–50.6) | 37.8 (35.6–40.2) | <0.001 |
| Female | 50.7 (49.4–51.9) | 62.2 (59.8–64.4) | |
| Race | |||
| Non-Hispanic White | 70.8 (67.4–73.9) | 83.9 (81.1–86.3) | <0.001 |
| Non-Hispanic Black | 13.3 (11.1–15.8) | 7.9 (6.4–9.8) | |
| Mexican-American | 6.2 (5.0–7.8) | 2.0 (1.3–3.1) | |
| Socioeconomic Status | |||
| Education | |||
| <High school | 21.6 (20.0–23.2) | 30.1 (26.7–33.7) | <0.001 |
| High school+ | 78.4 (76.8–80.0) | 69.9 (66.3–73.3) | |
| Household income | |||
| <$20,000 | 19.3 (17.8–20.8) | 33.6 (30.0–37.3) | <0.001 |
| $20–44,999 | 30.4 (28.9–32.1) | 34.1 (30.6–37.7) | |
| $45–74,999 | 24.6 (22.9–26.4) | 19.5 (16.1–23.3) | |
| $75,000+ | 25.7 (23.5–28.1) | 12.9 (10.3–16.0) | |
| Insurance | |||
| No | 14.7 (13.1–16.4) | 3.4 (2.3–5.1) | <0.001 |
| Yes | 85.4 (83.6–86.9) | 96.6 (94.9–97.7) | |
| Clinical Status | |||
| BMI | |||
| <30 | 58.6 (57.0–60.2) | 63.2 (60.0–66.3) | 0.007 |
| 30+ | 41.4 (39.8–43.0) | 36.8 (33.7–40.0) | |
| Diabetes | |||
| No | 88.8 (87.9–89.6) | 78.2 (74.9–81.2) | <0.001 |
| Yes | 11.2 (10.4–12.1) | 21.8 (18.8–25.1) | |
| Albuminuria | |||
| No | 87.2 (86.2–88.2) | 71.0 (67.9–73.9) | <0.001 |
| Yes | 12.8 (11.8–13.8) | 29.0 (26.1–32.1) | |
| Treatment Status | |||
| Any anti-hypertensive medication | |||
| No | 62.8 (60.4–65.1) | 33.6 (31.0–36.3) | <0.001 |
| Yes | 37.2 (34.9–39.7) | 66.4 (63.7–69.0) | |
| No. of anti-hypertensive medications | |||
| 0 | 62.8 (60.4–65.1) | 33.6 (31.0–36.3) | <0.001 |
| 1 | 27.1 (25.1–29.2) | 41.3 (38.2–44.3) | |
| 2+ | 10.2 (9.1–11.3) | 25.1 (22.7–27.7) | |
| ACE inhibitor or ARB | |||
| No | 84.8 (83.4–86.1) | 75.8 (73.4–78.1) | <0.001 |
| Yes | 15.2 (13.9–16.6) | 24.2 (21.9–26.6) | |
| Diuretic | |||
| No | 88.9 (87.5–90.2) | 81.5 (79.0–83.8) | <0.001 |
| Yes | 11.1 (9.8–12.5) | 18.5 (16.2–21.1) | |
| Other* anti-hypertensive medication | |||
| No | 97.3 (96.9–97.7) | 95.4 (94.1–96.4) | <0.001 |
| Yes | 2.7 (2.3–3.1) | 4.6 (3.6–5.9) | |
Including beta blockers and calcium channel blockers.
Uncontrolled Blood Pressure, Systolic Blood Pressure, and Diastolic Blood Pressure by CKD Status
Without adjustment, uncontrolled BP was greater in those with versus without CKD, by the general and disease-specific definitions (Figure 1). These differences remained after adjustment for adjustment for demographics, socioeconomic status, and clinical variables (Table 2; P<0.001 for no CKD vs. CKD by either definition). In a sensitivity analysis, with hypertension defined only by self-report and measured BP, the proportions with uncontrolled BP were similar: 51.2% and 54.1% for those without CKD and 55.4% and 72.1% for those with CKD, by the general and disease-specific definitions. Among the entire population (including those without hypertension), the proportions with BP exceeding the general and disease-specific guidelines were: 16.1% and 17.6% (without CKD) and 39.8% and 60.6% (with CKD).
Figure 1.
Unadjusted, weighted percentage of NHANES 1999–2006 participants with hypertension who have uncontrolled blood pressure, by CKD status.
Table 2.
Percentage of NHANES 1999–2006 participants with hypertension who have uncontrolled blood pressure, by presence of CKD (stages 3 and 4) and definition of uncontrolled blood pressure (general vs. disease-specific)
| % with Uncontrolled Blood Pressure (95% CI) |
||||||||
|---|---|---|---|---|---|---|---|---|
| General Definition (≥140/≥90 mmHg) |
Disease-specific Definition (≥130/≥85 [1999–2002] and ≥130/≥80 [2003–2006] mmHg for CKD & diabetes; otherwise ≥140/≥90 mmHg) |
|||||||
| No CKD (n=5163) | CKD (Stage 3 & 4; n=1330) | No CKD (n=5163) | CKD (Stage 3 & 4; n=1330) | |||||
| Subgroup | Unadjusted | Adjusted* | Unadjusted | Adjusted* | Unadjusted | Adjusted* | Unadjusted | Adjusted* |
| Overall | 48.7 (46.3–51.1) | 52.7 (50.4–55.0) | 51.5 (48.5–54.6) | 59.0 (56.2–61.7) | 51.7 (49.3–54.2) | 58.6 (56.3–60.9) | 68.8 (65.7–71.8) | 69.2 (66.6–71.7) |
| Survey Year | ||||||||
| 1999–2002 | 53.4 (50.0–56.7) | 56.3 (52.7–60.0) | 55.9 (51.3–60.3) | 59.2 (53.7–64.4) | 56.4 (53.0–59.7) | 60.8 (57.3–64.2) | 71.8 (67.5–75.8) | 74.7 (70.1–78.7) |
| 2003–2006 | 44.3 (41.1–47.6) | 50.0 (46.9–53.1) | 47.8 (43.7–52.0) | 50.9 (46.1–55.8) | 47.3 (44.1–50.6) | 54.1 (50.9–57.2) | 66.3 (61.6–70.6) | 70.7 (66.2–74.8) |
| P for trend | <0.001 | 0.011 | 0.011 | 0.027 | <0.001 | 0.007 | 0.073 | 0.204 |
| Demographics | ||||||||
| Age | ||||||||
| 20–39 | 38.5 (33.9–43.4) | 34.7 (31.3–38.2) | 49.9 (31.3–68.4) | 32.2 (21.9–44.7) | 39.7 (34.9–44.6) | 38.7 (35.2–42.3) | 69.7 (47.8–85.2) | 51.3 (37.2–65.2) |
| 40–59 | 46.0 (43.0–49.0) | 47.4 (44.8–50.0) | 37.2 (28.4–46.9) | 40.0 (32.5–49.2) | 49.0 (45.9–52.0) | 51.7 (49.2–54.2) | 54.7 (44.1–64.9) | 60.2 (51.2–68.5) |
| 60–69 | 51.7 (47.5–55.8) | 60.4 (58.0–62.9) | 46.4 (38.8–54.1) | 49.6 (44.7–54.4) | 57.0 (52.7–61.2) | 64.5 (62.1–66.8) | 66.8 (59.5–73.3) | 68.4 (64.2–72.3) |
| 70+ | 63.8 (60.0–67.4) | 72.1 (69.1–75.1) | 57.2 (58.5–60.8) | 58.5 (54.7–62.3) | 66.5 (63.0–69.9) | 75.5 (72.5–78.2) | 73.5 (69.8–76.8) | 75.6 (71.9–78.9) |
| P for trend | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | 0.002 | 0.002 |
| Sex | ||||||||
| Male | 47.7 (44.6–50.8) | 53.0 (49.9–56.1) | 46.5 (41.1–52.0) | 49.8 (43.9–55.6) | 50.3 (47.2–53.4) | 57.0 (53.7–60.2) | 64.5 (59.0–69.6) | 69.1 (63.7–74.0) |
| Female | 49.8 (47.1–52.5) | 52.8 (49.7–55.9) | 54.0 (50.5–58.6) | 58.4 (53.6–63.0) | 53.3 (50.6–55.9) | 57.4 (54.6–60.2) | 71.4 (67.1–75.5) | 75.1 (70.2–79.4) |
| P for trend | 0.212 | 0.921 | 0.028 | 0.030 | 0.071 | 0.811 | 0.060 | 0.119 |
| Race | ||||||||
| Non-Hispanic White | 46.7 (43.9–49.5) | 49.4 (46.6–52.1) | 51.4 (48.0–54.8) | 53.6 (49.6–57.6) | 49.3 (46.4–52.2) | 53.4 (50.7–56.1) | 67.8 (64.4–71.1) | 70.1 (66.8–73.3) |
| Non-Hispanic Black | 53.6 (50.6–56.6) | 53.5 (51.0–56.0) | 52.0 (44.4–59.5) | 55.3 (50.4–60.1) | 57.5 (54.3–60.6) | 57.8 (55.4–60.2) | 70.5 (63.3–76.8) | 74.5 (70.7–78.5) |
| Mexican- American | 53.3 (49.3–57.3) | 57.5 (53.3–61.7) | 51.0 (37.7–64.1) | 56.9 (47.9–65.5) | 57.6 (53.6–61.4) | 62.0 (58.1–65.8) | 64.0 (51.0–75.2) | 79.0 (72.1–84.5) |
| P for trend | <0.001 | 0.002 | 0.986 | 0.509 | <0.001 | 0.001 | 0.609 | 0.020 |
| Socioeconomic Status | ||||||||
| Education | ||||||||
| <High school | 55.8 (52.6–59.0) | 54.7 (51.3–57.9) | 51.4 (45.5–57.3) | 52.4 (46.1–58.7) | 59.7 (56.5–62.9) | 58.7 (55.4–62.0) | 69.3 (63.6–74.4) | 70.2 (64.7–75.2) |
| High school+ | 46.7 (44.0–49.4) | 52.0 (48.8–55.2) | 51.5 (47.5–55.5) | 55.6 (50.6–60.5) | 49.5 (46.7–52.3) | 56.4 (53.2–59.6) | 68.6 (64.1–72.8) | 73.6 (68.8–77.9) |
| P for trend | <0.001 | 0.263 | 0.981 | 0.459 | <0.001 | 0.347 | 0.863 | 0.384 |
| Household income | ||||||||
| <$20,000 | 53.4 (49.1–57.5) | 54.7 (51.1–58.3) | 55.6 (49.8–61.2) | 56.3 (50.8–61.7) | 57.6 (53.9–61.2) | 59.5 (55.8–63.0) | 71.8 (66.5–76.7) | 74.3 (69.8–78.4) |
| $20–44,999 | 50.0 (46.6–53.5) | 53.4 (50.9–55.8) | 50.5 (43.2–57.8) | 54.5 (50.8–58.1) | 54.1 (50.4–57.7) | 57.8 (55.3–60.2) | 69.9 (63.3–75.7) | 72.4 (69.3–75.4) |
| $45–74,999 | 48.4 (43.8–52.9) | 52.0 (49.1–54.9) | 49.6 (42.5–56.7) | 52.6 (46.8–58.4) | 50.0 (45.6–54.4) | 56.0 (53.3–58.7) | 66.5 (58.2–73.8) | 70.4 (65.6–74.8) |
| $75,000+ | 41.3 (37.0–45.8) | 50.7 (46.2–55.1) | 43.7 (32.7–55.3) | 50.8 (41.2–60.2) | 43.4 (39.0–47.9) | 54.3 (50.0–58.5) | 59.0 (47.7–69.4) | 68.4 (60.3–75.5) |
| P for trend | <0.001 | 0.222 | 0.305 | 0.397 | <0.001 | 0.107 | 0.170 | 0.235 |
| Insurance | ||||||||
| No | 48.4 (45.9–50.9) | 52.9 (50.3–55.6) | 51.4 (48.3–54.6) | 54.4 (50.7–58.1) | 51.6 (49.0–54.2) | 57.4 (54.6–60.1) | 68.7 (65.5–71.6) | 72.2 (69.1–75.2) |
| Yes | 50.5 (44.7–56.3) | 52.7 (46.0–59.4) | 46.8 (27.5–67.2) | 54.8 (29.1–78.2) | 52.6 (46.8–58.2) | 56.2 (49.4–62.7) | 68.9 (47.7–84.3) | 76.6 (52.6–90.6) |
| P for trend | 0.488 | 0.954 | 0.668 | 0.978 | 0.744 | 0.759 | 0.980 | 0.672 |
| Clinical Status | ||||||||
| BMI | ||||||||
| <30 | 51.5 (48.4–54.5) | 52.7 (49.5–55.9) | 53.7 (49.6–57.7) | 54.8 (50.4–59.1) | 52.9 (50.0–55.9) | 56.5 (53.5–59.4) | 69.9 (66.0–73.6) | 72.3 (68.3–76.0) |
| 30+ | 45.1 (42.1–48.0) | 53.2 (50.0–56.2) | 48.8 (43.2–54.6) | 53.8 (47.0–60.5) | 50.0 (46.8–53.2) | 58.2 (54.9–61.4) | 67.0 (62.1–71.5) | 72.5 (67.6–77.0) |
| P for trend | <0.001 | 0.845 | 0.193 | 0.821 | 0.119 | 0.424 | 0.286 | 0.941 |
| Diabetes | ||||||||
| No | 40.9 (36.9–45.1) | 46.0 (41.6–50.6) | 52.3 (44.8–59.7) | 61.2 (53.0–68.9) | 65.4 (60.1–70.4) | 72.8 (68.1–77.0) | 66.0 (58.9–72.4) | 72.4 (65.5–78.3) |
| Yes | 49.9 (47.4–52.4) | 54.1 (51.6–56.5) | 51.5 (47.9–55.2) | 52.2 (48.0–56.4) | 49.9 (47.4–57.4) | 54.3 (51.9–56.6) | 69.4 (65.6–72.9) | 72.4 (68.3–76.2) |
| P for trend | <0.001 | 0.001 | 0.868 | 0.059 | <0.001 | <0.001 | 0.404 | 0.989 |
| Albuminuria | ||||||||
| No | 47.0 (44.4–49.5) | 49.3 (46.6–52.0) | 46.7 (42.6–50.5) | 47.0 (42.6–51.4) | 49.6 (46.9–52.3) | 53.8 (51.0–56.6) | 64.0 (59.9–68.0) | 65.5 (61.8–69.3) |
| Yes | 63.1 (59.6–66.4) | 65.5 (61.6–69.2) | 66.7 (60.1–72.8) | 68.2 (42.6–51.3) | 68.8 (65.5–72.0) | 67.0 (62.6–70.9) | 81.8 (76.9–85.8) | 83.2 (78.1–87.4) |
| P for trend | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Treatment Status Any anti-hypertensive | ||||||||
| No | 59.3 (56.7–61.9) | 64.4 (61.6–67.2) | 71.1 (64.4–77.1) | 73.4 (66.6–79.2) | 61.2 (58.5–63.8) | 68.4 (65.8–71.0) | 84.0 (79.0–88.0) | 84.7 (79.7–88.7) |
| Yes | 35.8 (32.9–38.7) | 35.2 (32.0–38.5) | 43.1 (39.5–46.7) | 44.9 (41.1–48.8) | 40.2 (37.1–43.4) | 38.9 (35.7–42.3) | 62.3 (58.8–65.7) | 65.1 (61.5–68.4) |
| P for trend | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Number of anti- hypertensives | ||||||||
| 0 | 59.3 (56.7–61.9) | 61.3 (58.4–64.1) | 71.1 (64.4–77.1) | 68.0 (62.9–72.7) | 61.2 (58.5–63.8) | 75.1 (68.1–80.9) | 84.0 (79.0–88.0) | 80.4 (76.7–83.8) |
| 1 | 33.9 (30.5–37.5) | 43.6 (40.8–46.5) | 44.4 (39.4–49.5) | 53.1 (49.7–56.7) | 37.7 (34.2–41.3) | 64.4 (57.4–70.9) | 63.4 (58.9–67.7) | 71.3 (68.3–74.1) |
| 2+ | 40.9 (35.5–46.4) | 27.4 (23.1–32.2) | 40.9 (35.5–46.5) | 37.8 (33.0–42.8) | 47.0 (41.5–52.6) | 52.2 (43.6–60.6) | 60.4 (54.4–66.1) | 59.9 (54.6–65.0) |
| P for trend | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| ACE inhibitors/ARBs | ||||||||
| No | 52.2 (49.7–54.6) | 54.8 (52.0–57.5) | 55.6 (51.6–59.5) | 56.5 (52.4–60.7) | 54.7 (52.3–57.0) | 67.3 (59.9–74.0) | 72.0 (67.8–75.8) | 73.2 (69.1–76.8) |
| Yes | 33.1 (29.0–37.6) | 35.2 (30.6–40.1) | 39.6 (34.5–45.0) | 43.3 (37.5–49.3) | 38.6 (34.1–43.3) | 57.5 (49.1–65.4) | 59.6 (53.9–65.1) | 64.1 (58.6–69.3) |
| P for trend | <0.001 | <0.001 | <0.001 | 0.001 | <0.001 | 0.016 | 0.002 | 0.016 |
| Diuretic | ||||||||
| No | 50.9 (48.5–53.2) | 53.3 (50.7–55.8) | 53.1 (49.8–56.4) | 54.5 (51.0–58.0) | 53.8 (51.4–56.3) | 66.1 (59.0–72.5) | 70.0 (66.6–73.2) | 71.8 (68.2–75.1) |
| Yes | 34.8 (30.3–39.6) | 36.9 (32.2–41.8) | 45.2 (39.4–51.2) | 47.1 (39.5–54.7) | 38.0 (33.3–43.0) | 60.5 (50.4–69.7) | 64.1 (56.7–70.8) | 66.6 (59.0–73.5) |
| P for trend | <0.001 | <0.001 | 0.016 | 0.076 | <0.001 | 0.219 | 0.115 | 0.219 |
| Other† anti-hypertensive | ||||||||
| No | 49.0 (46.6–51.4) | 51.4 (49.0–54.0) | 51.3 (48.1–54.5) | 52.6 (49.2–56.1) | 52.0 (49.6–54.5) | 64.8 (57.9–71.1) | 69.0 (65.6–72.1) | 70.8 (67.6–73.7) |
| Yes | 40.4 (31.4–50.1) | 39.1 (29.2–50.2) | 56.5 (45.9–66.6) | 61.7 (47.9–73.8) | 43.8 (34.5–53.5) | 65.7 (50.3–78.4) | 66.2 (55.5–75.4) | 71.6 (58.0–82.2) |
| P for trend | 0.084 | 0.026 | 0.347 | 0.208 | 0.099 | 0.894 | 0.603 | 0.894 |
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker.
Adjusted for all of the following except the subgroup being examined: survey year, age, sex, race, education, income, insurance, obesity, diabetes, and treatment with any anti-hypertensive.
Includes beta and calcium channel blockers.
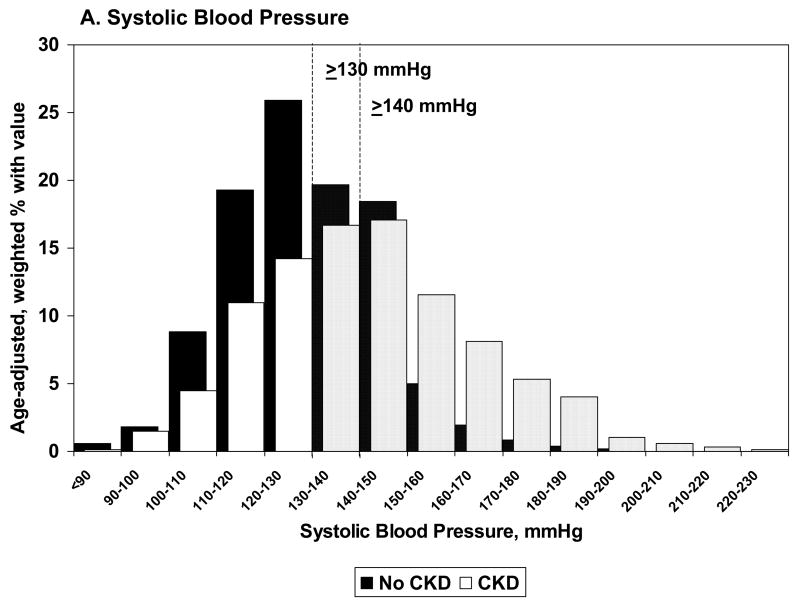
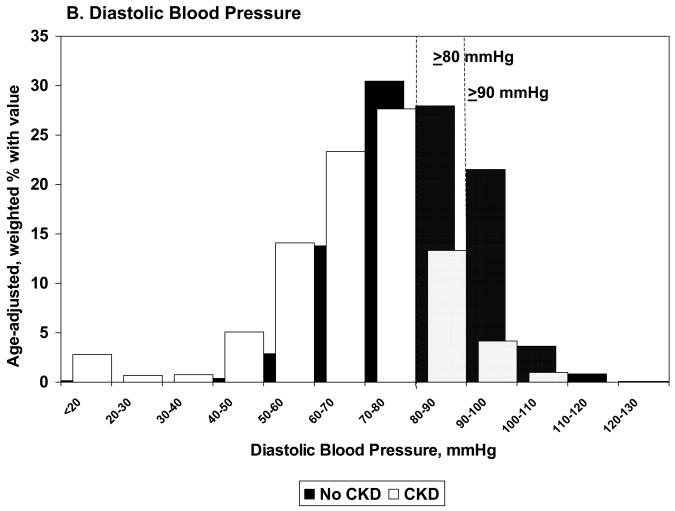
The vast majority of uncontrolled BP could be attributed to high SBP (87.0% general definition; 94.2% disease-specific definition) rather than high DBP, regardless of CKD status. The distributions of age-adjusted BP among those with CKD were more right-skewed (Figure 2, A and B), indicating that these participants are more likely to have extremely high BPs than those without CKD. The proportions of participants with CKD who had BPs above the thresholds were higher for SBP and lower for DBP, relative to those without CKD.
Figure 2.
Weighted, age-adjusted distributions of systolic (A) and diastolic (B) blood pressure among NHANES 1999–2006 participants with hypertension, by CKD status.
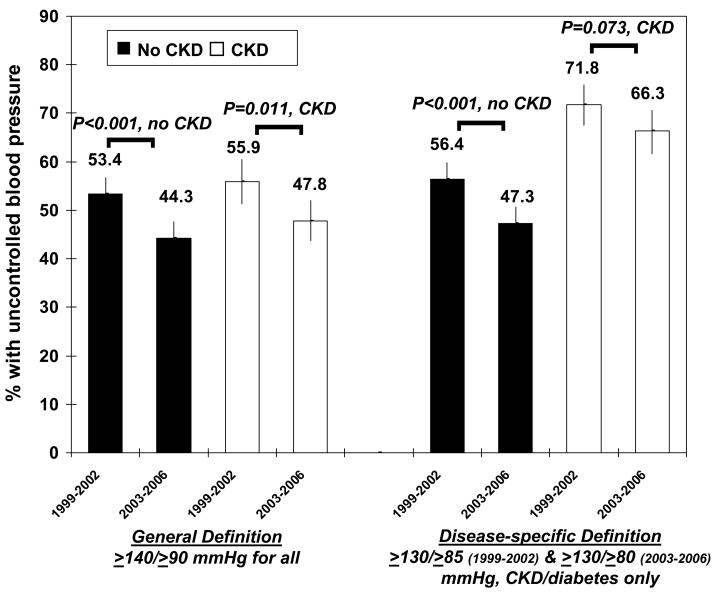
Trends in Uncontrolled Blood Pressure
For those without CKD, prevalence of uncontrolled BP by both definitions decreased between 1999–2002 and 2003–2006 (Figure 3); similar decreases were seen for those with CKD, although the trend did not reach statistical significance by the disease-specific definition. With adjustment, results were similar (Table 2). Significant decreasing trends were also seen for proportions with stage II uncontrolled BP (P=0.002 and 0.037 for no CKD and CKD, respectively).
Figure 3.
Percentage of NHANES 1999–2006 participants with hypertension who have uncontrolled blood pressure, by CKD status and by year: 1999–2002 (pre-JNC-7 guidelines) and 2003–2006 (post-JNC-7 guidelines).
Predictors of Uncontrolled Blood Pressure
Demographics
After adjustment, participants who did not have CKD and who were older and of non-Hispanic black race were significantly more likely than their younger and white counterparts to have uncontrolled BP by the general definition (Table 2). There was no difference by sex in those without CKD, regardless of adjustment. For those with CKD, older age and female sex were both associated with higher rates of uncontrolled BPs by the same definition, with or without adjustment, whereas uncontrolled BP did not differ by race in those with CKD, using the general definition. Interaction analyses showed that, after adjustment, sex remained a possible effect modifier of risk of uncontrolled BP by CKD status (P=0.045 and 0.061, general and disease-specific definitions, respectively). Regardless of CKD status, participants who were 70 or older had proportions of uncontrolled BP that were ~2-fold those in participants aged 20–39 by this definition.
Socioeconomic Factors
Participants without CKD who had lower education and lower income were significantly more likely than their counterparts to have uncontrolled BP by either definition (Table 2); however, neither factor remained significantly associated after adjustment. For those with CKD, there were no statistically significant socioeconomic predictors of uncontrolled BP.
Clinical Factors
Participants without CKD who were not obese and had diabetes were all significantly more likely than their counterparts to have uncontrolled BP by the general definition (Table 2); only diabetes status remained associated after adjustment and showed evidence of significant interactions with CKD status (P=0.003 and 0.006, general and disease-specific definitions). By the disease-specific definition, those without diabetes were more likely to have uncontrolled BP. Albuminuria was associated with greater prevalence of uncontrolled blood pressure regardless of CKD status or definition used.
Treatment Status
Regardless of definition of uncontrolled BP or CKD status, use of a single anti-hypertensive agent was associated with lower unadjusted rates of uncontrolled BP, whereas the use of multiple medications was associated with slightly higher rates; however, with adjustment for potential confounders, uncontrolled BP decreased with increasing numbers of medications used (Table 2). ACE inhibitors/ARBs were associated with lower rates of uncontrolled BP for all participants, whereas diuretics and other medications were significant only for those without CKD, using the general definition. Of those with CKD and uncontrolled blood pressure (disease-specific definition), 21.8% were on ACE inhibitors/ARBs and 23.1% were on multiple medications. There was also evidence of effect modification by CKD status with medications (ACE inhibitors/ARBs, P=0.097, and other medications, P=0.047, general definition only; diuretics, P=0.050, disease-specific definition only).
Discussion
In this national survey, 49% and 52% of the participants with hypertension who did not have CKD had uncontrolled BP by the general and disease-specific guidelines, respectively. Uncontrolled BP was more prevalent in the CKD population, with 52% and 69%, respectively, having uncontrolled BP by the general and disease-specific guidelines. These estimates were not substantially lower than the rates of uncontrolled BP (62–70%) reported in CKD stage 5 patients treated with hemodialysis (24, 25).
The substantially higher prevalence of uncontrolled BP in those with CKD relative to those without CKD are likely due to difficulties associated with controlling BP in those with CKD. The JNC-7 guidelines (1) recommend that patients with CKD, the vast majority of whom have hypertension, receive aggressive management, including the use of three or more medications at increasing doses; in fact, consensus evidence shows that an average of more than three medications are needed to control BP in CKD (26). We found that one-third of those with CKD and hypertension were not treated with medications; of those on treatment, only 37% and 28% of those with CKD and hypertension were on ACE inhibitors/ARBs and diuretics, respectively. Moreover, despite their association with a lower likelihood of uncontrolled BP, only 22% of those with CKD and uncontrolled blood pressure were on ACE inhibitors/ARBs. Similarly, after adjustment, only 23% were on multiple medications. This is despite our findings that uncontrolled BP rates in CKD were lowest in those on two or more agents, but only after adjustment for factors contributing to the indication for treatment (i.e., factors associated with poor control requiring multiple medications). Although this study was not conducted in a healthcare setting, these results suggest that there may be an educational deficit in the community with regard to optimal care of hypertension.
Both patient and provider factors could play a role in the lack of BP control among those with CKD. Patient factors that may impede BP control in those with CKD include the lack of a primary care provider or non-adherence to medications and dietary guidelines. Non-adherence may result from a lack of understanding of the importance of BP for preventing progression and complications of CKD; cognitive difficulties associated with CKD (27); fear or intolerance of medication side effects; and the cost of medications, especially multiple medications. Hypervolemia and/or increased arterial stiffness, suggested by the substantially higher pulse pressure we found in those with CKD, may also make BP control very difficult among these patients, even with primary care and adherence.
The provider’s role in controlling BP in CKD involves both recognizing CKD and knowing and adhering to CKD-specific guidelines. Previous surveys have shown that primary care physicians may be unlikely to recognize some risk factors (28) and may only recognize CKD upon testing at rates of 59–78% (29). A 2007 survey (30) showed that physicians in training (internal medicine residents) selected a BP target of 130/80 or less for patients with CKD nearly 90% of the time, and 98% identified ACE inhibitors/ARBs as part of the treatment plan, indicating that knowledge of CKD guidelines may be improving.
We also found evidence that uncontrolled BP decreased in both those without and with CKD from 1999–2002 to 2003–2006, coincident with the release of new hypertension guidelines in 2003 (1). This may be due to greater physician knowledge of and adherence to the revised guidelines or to a greater availability of multiple medications for aggressive treatment of BP in CKD. In fact, ACE inhibitors/ARBs were used more frequently in more recent survey years. However, despite this evidence of a downward trend in uncontrolled BP, control remains poor, by any definition, in both the non-CKD and CKD populations.
We also found that BP control was often associated with demographic characteristics. As with previous studies (6, 8, 31), we found that older age (usually associated with arterial stiffness) was strongly associated with uncontrolled BP in those with and without CKD, regardless of the definition used. Although a previous study using the NHANES population-based survey data showed an increased risk of uncontrolled BP in males in the general population (5), a more recent study by Ostchega et al. (6) showed that females were more likely to have uncontrolled BP. We found that females with CKD were at greater risk for uncontrolled BP, in agreement with a previous study of volunteers with CKD (32), but only using the general definition. Non-whites with CKD were at greater risk for uncontrolled BP, which has been shown previously (5, 6), possibly due to greater medication nonadherence and worry about hypertension (33).
Socioeconomic factors, including higher level of education, insured status, and high income, were not associated with risk of uncontrolled BP after adjustment for demographics and clinical characteristics, suggesting that physiologic factors dominate socioeconomic influence on BP control in the CKD population. This finding highlights the necessity of better professional and broad-based patient education in efforts to improve BP control. As expected, diabetes (34) was associated with uncontrolled BP in the non-CKD population but not in those with CKD. This is likely a reflection of the physiological mechanisms (e.g., salt and water retention due to reduced kidney function, aldosterone excess, or sympathetic overactivity) that lead to hypertension once CKD develops, regardless of the underlying causes of the disease. Interestingly, regardless of CKD status (i.e., kidney function), presence of albuminuria was strongly associated with increased prevalence of uncontrolled blood pressure, as has been reported previously in CKD populations (8, 35).
There are some limitations of the study that deserve mention. First, although we chose to examine CKD stage 3 and 4 only to minimize the error associated with single albuminuria measurements, we almost certainly have some misclassification of CKD stage 1 and 2 as “non-CKD,” which may have attenuated some of our comparisons between the two populations. However, because these early stages are currently neither well-recognized nor universally accepted (36), we believe that many of these participants are likely to be treated as “non-CKD” in the treatment of their hypertension. Second, information on treatment nonadherence, which may be differential by either CKD status or other patient characteristics (such as age or race), was not available. Additionally, we did not have enough observations to examine various combinations of medications as predictors of uncontrolled BP. Third, as with any observational study, there may be unknown or unmeasured factors that affect BP control for which we could not account. For example, psychosocial reasons such as hopelessness, frustration with treatment, and anxiety, have been proposed as predisposing factors for poor BP control (37). Fourth, although the method of blood pressure measurement (office BP at a single point in time) in NHANES was the only practical means of assessing BP in a large national survey, it may not have captured all the uncontrolled BP in the population, particularly in those with CKD whose BP may be elevated outside the clinic setting (e.g., at home or during routine daily activities) and could be captured with ambulatory BP monitoring. A recent study (38) found that white-coat hypertension and masked hypertension, particularly, were prevalent among those with CKD; this phenomenon may have further attenuated the differences between participants with and without that we observed here. Finally, changes in therapy or other patient characteristics cannot be assessed over time in a cross-sectional survey. Additionally, provider knowledge of BP control guidelines in CKD and the general population and quality of patient-provider communication may play a significant role in BP control and could not be ascertained here.
Perspectives
Uncontrolled BP is common in the U.S. CKD population, especially using the newer (more stringent) BP control guidelines. We showed that, although there was improvement in rates of uncontrolled BP over time in those without and with CKD, control remains poor overall. Use of ACE inhibitors/ARBs and multiple medications was associated with better BP control, but these therapies may be underutilized in those with uncontrolled BP. Non-whites, older persons, and females with CKD, who are most likely to have uncontrolled BP, should be targeted with more aggressive efforts to control BP.
Acknowledgments
We thank the participants and staff of the NHANES survey.
Funding Source: This project was supported under a cooperative agreement from the Centers for Disease Control and Prevention through the Association of American Medical Colleges, grant number U36/CCU319276, AAMC ID number MM-0997-07/07. Report contents are solely the responsibility of the authors and do not necessarily represent the official views of the AAMC or CDC. Members of the CKD Surveillance Project: Johns Hopkins University Neil Powe, Laura Plantinga, L. Ebony Boulware, Josef Coresh, Edgar Miller III, Andrew Levey, Lesley Stevens, Deidra Crews, April Lawner; University of Michigan Rajiv Saran, Elizabeth Hedgeman, Brenda Gillespie, William Herman, Friedrich Port, Bruce Robinson, Vahakn Shahinian, Jerry Yee, Eric Young, Meggy Yin; Centers for Disease Control and Prevention Desmond Williams, Sabitha Desari, Mark Eberhardt, Paul Eggers, Nicole Flowers, Linda Geiss, Sue Hailpern, Regina Jordan, Juanita Mondeshire, Bernice Moore, Gary Myers, Meda Pavkov, Nilka Rios-Burrows, Deborah Rolka, Sharon Saydah, Anton Schoolwerth, Rodolfo Valdez, Larry Waller. Dr. Powe is partially supported by grant K24DK02643 and Dr. Stevens is partially supported by grant K23DK081017-01, both from the National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD.
Footnotes
Conflicts of Interest: None.
References
- 1.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ the National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 2.The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1997;157:2413–2446. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- 3.Stamler J, Stamler R, Neaton JD. Blood pressure, systolic and diastolic, and cardiovascular risks. US population data. Arch Intern Med. 1993;153:598–615. doi: 10.1001/archinte.153.5.598. [DOI] [PubMed] [Google Scholar]
- 4.Vasan RS, Larson MG, Leip EP, Evans JC, O’Donnell CJ, Kannel WB, Levy D. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345:1291–1297. doi: 10.1056/NEJMoa003417. [DOI] [PubMed] [Google Scholar]
- 5.Burt VL, Cutler JA, Higgins M, Horan MJ, Labarthe D, Whelton P, Brown C, Roccella EJ. Trends in the prevalence, awareness, treatment, and control of hypertension in the adult US population. Data from the health examination surveys, 1960 to 1991. Hypertension. 1995;26:60–69. doi: 10.1161/01.hyp.26.1.60. [DOI] [PubMed] [Google Scholar]
- 6.Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S. Trends in hypertension prevalence, awareness, treatment, and control in older u.s. Adults: data from the national health and nutrition examination survey 1988 to 2004. J Am Geriatr Soc. 2007;55:1056–1065. doi: 10.1111/j.1532-5415.2007.01215.x. [DOI] [PubMed] [Google Scholar]
- 7.Psaty BM, Manolio TA, Smith NL, Heckbert SR, Gottdiener JS, Burke GL, Weissfeld J, Enright P, Lumley T, Powe N, Furberg CD. Time trends in high blood pressure control and the use of antihypertensive medications in older adults: the Cardiovascular Health Study. Arch Intern Med. 2002;162:2325–2332. doi: 10.1001/archinte.162.20.2325. [DOI] [PubMed] [Google Scholar]
- 8.Peralta CA, Hicks LS, Chertow GM, Ayanian JZ, Vittinghoff E, Lin F, Shlipak MG. Control of hypertension in adults with chronic kidney disease in the United States. Hypertension. 2005;45:1119–1124. doi: 10.1161/01.HYP.0000164577.81087.70. [DOI] [PubMed] [Google Scholar]
- 9.Sarafidis PA, Li S, Chen SC, Collins AJ, Brown WW, Klag MJ, Bakris GL. Hypertension awareness, treatment, and control in chronic kidney disease. Am J Med. 2008;121:332–340. doi: 10.1016/j.amjmed.2007.11.025. [DOI] [PubMed] [Google Scholar]
- 10.Rao MV, Qiu Y, Wang C, Bakris G. Hypertension and CKD: Kidney Early Evaluation Program (KEEP) and National Health and Nutrition Examination Survey (NHANES), 1999–2004. Am J Kidney Dis. 2008;51:S30–S37. doi: 10.1053/j.ajkd.2007.12.012. [DOI] [PubMed] [Google Scholar]
- 11.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008;52:818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics: Plan and operation of the Third National Health and Nutrition Examination Survey, 1988–1994. Series 1: Program and collection procedures. Vital Health Stat. 1994;32:1–407. [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention, National Center for Health Statistics. National Health and Nutrition Examination Survey Data, 1999–2000. Hyattsville, MD: U.S.Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. Available at: http://www.cdc.gov/nchs/about/major/nhanes/nhanes1999-2000/nhanes99_00.htm. [Google Scholar]
- 14.Centers for Disease Control and Prevention, National Center for Health Statistics. National Health and Nutrition Examination Survey Data, 2001–2002. Hyattsville, MD: U.S.Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. Available at: http://www.cdc.gov/nchs/about/major/nhanes/nhanes2001-2002/nhanes01_02.htm. [Google Scholar]
- 15.Centers for Disease Control and Prevention, National Center for Health Statistics. National Health and Nutrition Examination Survey Data, 2003–2004. Hyattsville, MD: U.S.Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. Available at: http://www.cdc.gov/nchs/about/major/nhanes/nhanes2003-2004/nhanes03_04.htm. [Google Scholar]
- 16.Centers for Disease Control and Prevention, National Center for Health Statistics. National Health and Nutrition Examination Survey Data, 2005–2006. Hyattsville, MD: U.S.Department of Health and Human Services, Centers for Disease Control and Prevention; 2008. Available at: http://www.cdc.gov/nchs/about/major/nhanes/nhanes2005-2006/nhanes05_06.htm. [Google Scholar]
- 17.National Health and Nutrition Examination Survey. Physician Examination Procedures Manual. Hyattsville, MD: National Center for Health Statistics; 2003. Available at: http://www.cdc.gov/nchs/data/nhanes/nhanes_05_06/PE.pdf. [Google Scholar]
- 18.National Kidney Foundation. Kidney Disease Outcomes Quality Initiative (K/DOQI) National Kidney Foundation. 2005 Available at: http://www.kidney.org/professionals/doqi.
- 19.Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2003;41:1–12. doi: 10.1053/ajkd.2003.50007. [DOI] [PubMed] [Google Scholar]
- 20.Levey AS, Coresh J, Greene T, Marsh J, Stevens LA, Kusek J, Van Lente F. Expressing the MDRD study equation for estimating GFR with IDMS traceable(gold standard) serum creatinine values [Abstract] J Am Soc Nephrol. 2005;16:69A. [Google Scholar]
- 21.Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, Kusek JW, Van Lente F. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145:247–254. doi: 10.7326/0003-4819-145-4-200608150-00004. [DOI] [PubMed] [Google Scholar]
- 22.Selvin E, Manzi J, Stevens LA, Van Lente F, Lacher DA, Levey AS, Coresh J. Calibration of serum creatinine in the National Health and Nutrition Examination Surveys (NHANES) 1988–1994, 1999–2004. Am J Kidney Dis. 2007;50:918–926. doi: 10.1053/j.ajkd.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics. Analytic and reporting guidelines: the National Health and Nutrition Examination Survey (NHANES) National Center for Health Statistics. 2007 Available at: http//www.cdc.gov/nchs/data/nhanes/nhanes_03_04/nhanes_analytic_guidelines_dec_2005.pdf.
- 24.Rahman M, Dixit A, Gupta S, Hanslik T, Lacson E, Ogundipe A, Weigel K, Smith MC. Factors associated with inadequate blood pressure control in hypertensive hemodialysis patients. Am J Kidney Dis. 1999;33:498–506. doi: 10.1016/s0272-6386(99)70187-3. [DOI] [PubMed] [Google Scholar]
- 25.Agarwal R, Nissenson AR, Batelle D, Coyne DW, Trout JR, Warnock DG. Prevalence, treatment, and control of hypertension in chronic hemodialysis patients in the United States. Am J Med. 2003;115:291–297. doi: 10.1016/s0002-9343(03)00366-8. [DOI] [PubMed] [Google Scholar]
- 26.Bakris GL, Williams M, Dworkin L, Elliott WJ, Epstein M, Toto R, Tuttle K, Douglas J, Hsueh W, Sowers J. Preserving renal function in adults with hypertension and diabetes: a consensus approach. National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group. Am J Kidney Dis. 2000;36:646–661. doi: 10.1053/ajkd.2000.16225. [DOI] [PubMed] [Google Scholar]
- 27.Kurella TM, Wadley V, Yaffe K, McClure LA, Howard G, Go R, Allman RM, Warnock DG, McClellan W. Kidney function and cognitive impairment in US adults: the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study. Am J Kidney Dis. 2008;52:227–234. doi: 10.1053/j.ajkd.2008.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lea JP, McClellan WM, Melcher C, Gladstone E, Hostetter T. CKD risk factors reported by primary care physicians: do guidelines make a difference? Am J Kidney Dis. 2006;47:72–77. doi: 10.1053/j.ajkd.2005.09.027. [DOI] [PubMed] [Google Scholar]
- 29.Boulware LE, Troll MU, Jaar BG, Myers DI, Powe NR. Identification and referral of patients with progressive CKD: a national study. Am J Kidney Dis. 2006;48:192–204. doi: 10.1053/j.ajkd.2006.04.073. [DOI] [PubMed] [Google Scholar]
- 30.Agrawal V, Ghosh AK, Barnes MA, McCullough PA. Awareness and knowledge of clinical practice guidelines for CKD among internal medicine residents: a national online survey. Am J Kidney Dis. 2008;52:1061–1069. doi: 10.1053/j.ajkd.2008.06.022. [DOI] [PubMed] [Google Scholar]
- 31.Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med. 2001;345:479–486. doi: 10.1056/NEJMoa010273. [DOI] [PubMed] [Google Scholar]
- 32.Duru OK, Li S, Jurkovitz C, Bakris G, Brown W, Chen SC, Collins A, Klag M, McCullough PA, McGill J, Narva A, Pergola P, Singh A, Norris K. Race and sex differences in hypertension control in CKD: results from the Kidney Early Evaluation Program (KEEP) Am J Kidney Dis. 2008;51:192–198. doi: 10.1053/j.ajkd.2007.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bosworth HB, Powers B, Grubber JM, Thorpe CT, Olsen MK, Orr M, Oddone EZ. Racial differences in blood pressure control: potential explanatory factors. J Gen Intern Med. 2008;23:692–698. doi: 10.1007/s11606-008-0547-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Geiss LS, Rolka DB, Engelgau MM. Elevated blood pressure among U.S. adults with diabetes, 1988–1994. Am J Prev Med. 2002;22:42–48. doi: 10.1016/s0749-3797(01)00399-3. [DOI] [PubMed] [Google Scholar]
- 35.Agarwal R, Andersen MJ. Correlates of systolic hypertension in patients with chronic kidney disease. Hypertension. 2005;46:514–520. doi: 10.1161/01.HYP.0000178102.85718.66. [DOI] [PubMed] [Google Scholar]
- 36.Bauer C, Melamed ML, Hostetter TH. Staging of chronic kidney disease: time for a course correction. J Am Soc Nephrol. 2008;19:844–846. doi: 10.1681/ASN.2008010110. [DOI] [PubMed] [Google Scholar]
- 37.Jokisalo E, Enlund H, Halonen P, Takala J, Kumpusalo E. Factors related to poor control of blood pressure with antihypertensive drug therapy. Blood Press. 2003;12:49–55. [PubMed] [Google Scholar]
- 38.Pogue VA, Rahman M, Lipkowitz M, Toto RD, Miller ER, III, Faulkner M, Rostand SG, Hiremath L, Sika M, Kendrick C, Hu B, Greene T, Appel LJ, Philips RA. Disparate estimates of hypertension control from ambulatory and clinic blood pressure measurements in hypertensive kidney disease: results from the AASK cohort study. Hypertension. 2009 doi: 10.1161/HYPERTENSIONAHA.108.115154. in press. [DOI] [PubMed] [Google Scholar]